28a8fcbdc5c6961810cf85ca147c11c7.ppt
- Количество слайдов: 47

Latest Advances In The Treatment Of Obsessive Compulsive And Related Disorders NA Fineberg, J Reid, R Ruparelia, R Sachdev, E Cinosi, D Mpavaenda Highly Specialised Service for Obsessive Compulsive and Related Disorders, Hertfordshire Partnership University NHS Foundation Trust, University of Hertfordshire, Rosanne House , Welwyn Garden City, Hertfordshire AL 8 6 HG March 2017

Declaration of interests I have received sponsorship for: • Consultancy work from Servier, Lundbeck, Glaxo-Smith Kline, Astra-Zeneca and Bristol-Myers Squibb. • Research support from Servier, Lundbeck • Educational work and lectures from Shire, Otsuka, Janssen, Lundbeck, Bristol-Myers Squibb, Wyeth, Servier.
Aims of lecture • Re-conceptualization of OCRDs • What are the first-line treatments? • Does pharmacotherapy improve health-related quality of life? • How long should treatment continue? • Can we predict treatment outcomes? • Management of treatment-refractory OCD • Novel targets and treatments
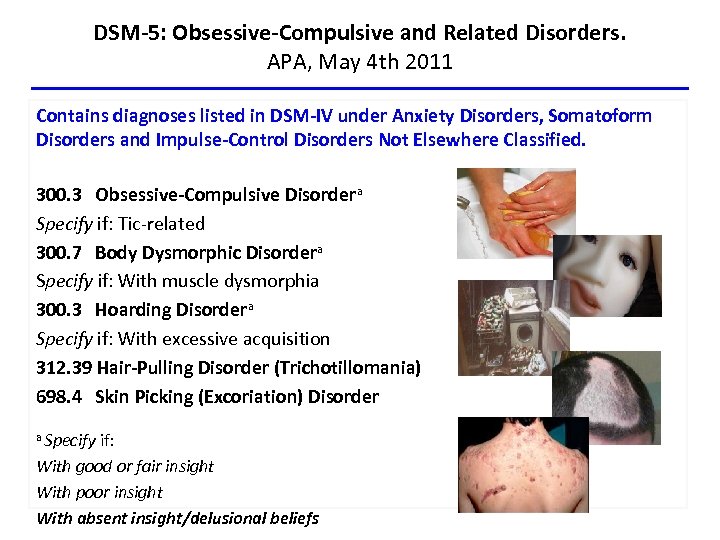
DSM-5: Obsessive-Compulsive and Related Disorders. APA, May 4 th 2011 Contains diagnoses listed in DSM-IV under Anxiety Disorders, Somatoform Disorders and Impulse-Control Disorders Not Elsewhere Classified. 300. 3 Obsessive-Compulsive Disordera Specify if: Tic-related 300. 7 Body Dysmorphic Disordera Specify if: With muscle dysmorphia 300. 3 Hoarding Disordera Specify if: With excessive acquisition 312. 39 Hair-Pulling Disorder (Trichotillomania) 698. 4 Skin Picking (Excoriation) Disorder a Specify if: With good or fair insight With poor insight With absent insight/delusional beliefs
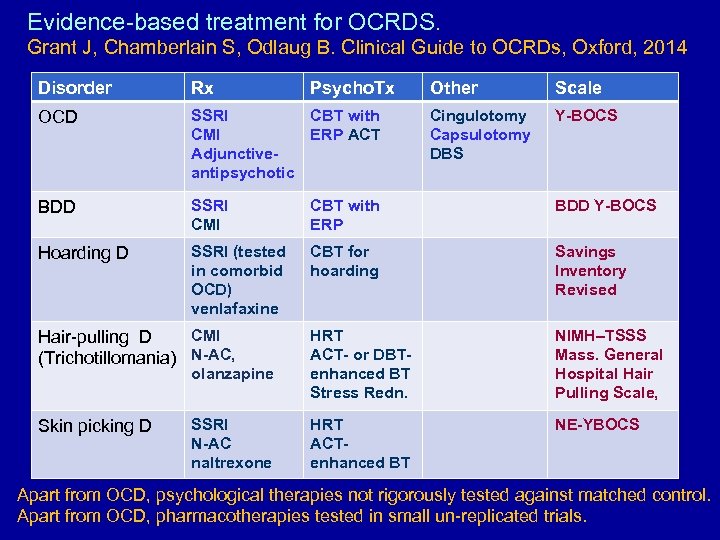
Evidence-based treatment for OCRDS. Grant J, Chamberlain S, Odlaug B. Clinical Guide to OCRDs, Oxford, 2014 Disorder Rx OCD SSRI CBT with CMI ERP ACT Adjunctiveantipsychotic BDD SSRI CMI CBT with ERP BDD Y-BOCS Hoarding D SSRI (tested in comorbid OCD) venlafaxine CBT for hoarding Savings Inventory Revised HRT ACT- or DBTenhanced BT Stress Redn. NIMH–TSSS Mass. General Hospital Hair Pulling Scale, HRT ACT- enhanced BT NE-YBOCS CMI Hair-pulling D (Trichotillomania) N-AC, olanzapine Skin picking D SSRI N-AC naltrexone Psycho. Tx Other Scale Cingulotomy Capsulotomy DBS Y-BOCS Apart from OCD, psychological therapies not rigorously tested against matched control. Apart from OCD, pharmacotherapies tested in small un-replicated trials.
Anxiety Disorders Guidelines covering OCD • International Consensus Group on Depression and Anxiety (2000, 2003) • World Federation of Societies of Biological Psychiatry (2002, 2008, 2012) • World Council on Anxiety Disorders (2003) • National Institute for Clinical Excellence (UK) (2006; Evidence Update 2013) (and BDD) • British Association for Psychopharmacology (2005, 2014) • American Psychiatric Association (2007, Guideline Watch update 2013) • ICOCS; Standards of Care (2016)
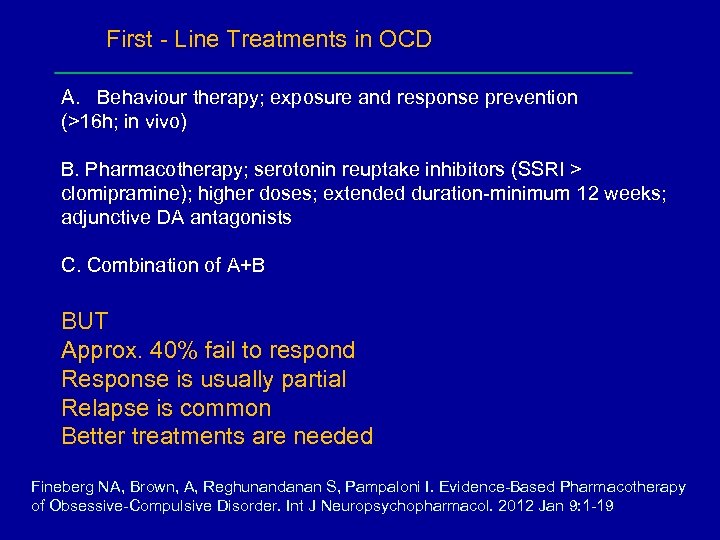
First - Line Treatments in OCD A. Behaviour therapy; exposure and response prevention (>16 h; in vivo) B. Pharmacotherapy; serotonin reuptake inhibitors (SSRI > clomipramine); higher doses; extended duration-minimum 12 weeks; adjunctive DA antagonists C. Combination of A+B BUT Approx. 40% fail to respond Response is usually partial Relapse is common Better treatments are needed Fineberg NA, Brown, A, Reghunandanan S, Pampaloni I. Evidence-Based Pharmacotherapy of Obsessive-Compulsive Disorder. Int J Neuropsychopharmacol. 2012 Jan 9: 1 -19
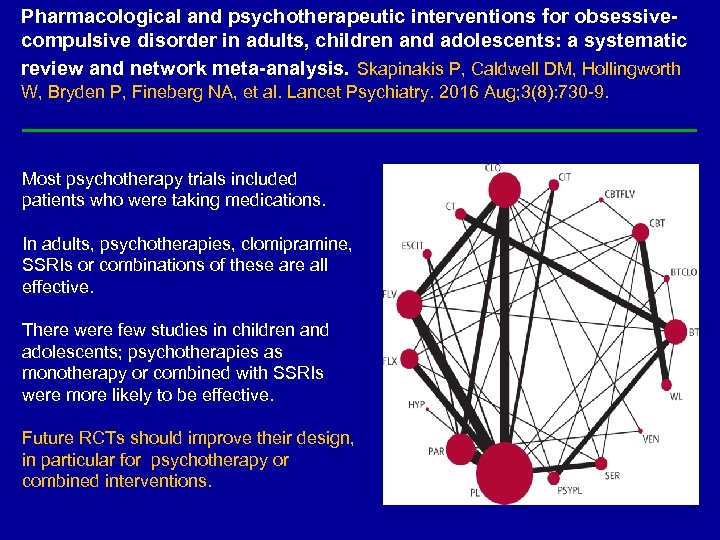
Pharmacological and psychotherapeutic interventions for obsessivecompulsive disorder in adults, children and adolescents: a systematic review and network meta-analysis. Skapinakis P, Caldwell DM, Hollingworth W, Bryden P, Fineberg NA, et al. Lancet Psychiatry. 2016 Aug; 3(8): 730 -9. Most psychotherapy trials included patients who were taking medications. In adults, psychotherapies, clomipramine, SSRIs or combinations of these are all effective. There were few studies in children and adolescents; psychotherapies as monotherapy or combined with SSRIs were more likely to be effective. Future RCTs should improve their design, in particular for psychotherapy or combined interventions.
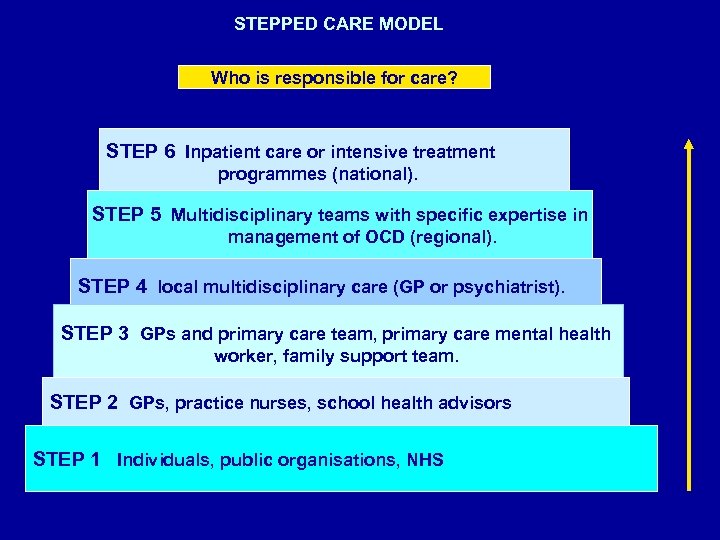
STEPPED CARE MODEL Who is responsible for care? STEP 6 Inpatient care or intensive treatment programmes (national). STEP 5 Multidisciplinary teams with specific expertise in management of OCD (regional). STEP 4 local multidisciplinary care (GP or psychiatrist). STEP 3 GPs and primary care team, primary care mental health worker, family support team. STEP 2 GPs, practice nurses, school health advisors STEP 1 Individuals, public organisations, NHS
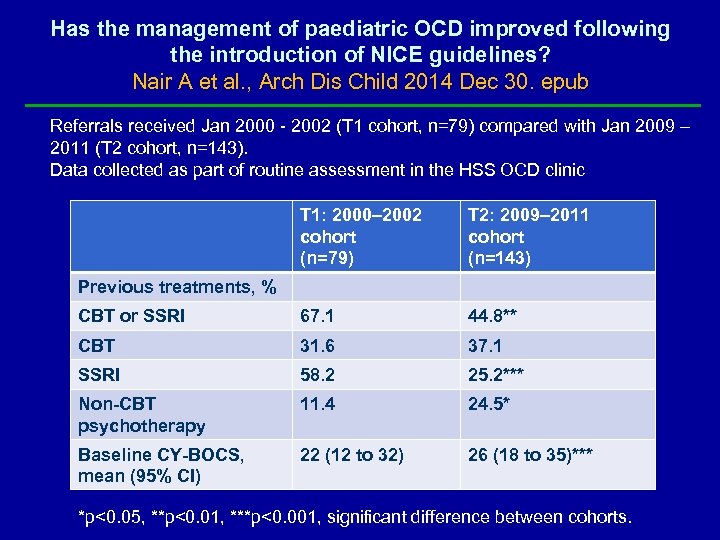
Has the management of paediatric OCD improved following the introduction of NICE guidelines? Nair A et al. , Arch Dis Child 2014 Dec 30. epub Referrals received Jan 2000 - 2002 (T 1 cohort, n=79) compared with Jan 2009 – 2011 (T 2 cohort, n=143). Data collected as part of routine assessment in the HSS OCD clinic T 1: 2000– 2002 cohort (n=79) T 2: 2009– 2011 cohort (n=143) CBT or SSRI 67. 1 44. 8** CBT 31. 6 37. 1 SSRI 58. 2 25. 2*** Non-CBT psychotherapy 11. 4 24. 5* Baseline CY-BOCS, mean (95% CI) 22 (12 to 32) 26 (18 to 35)*** Previous treatments, % *p<0. 05, **p<0. 01, ***p<0. 001, significant difference between cohorts.
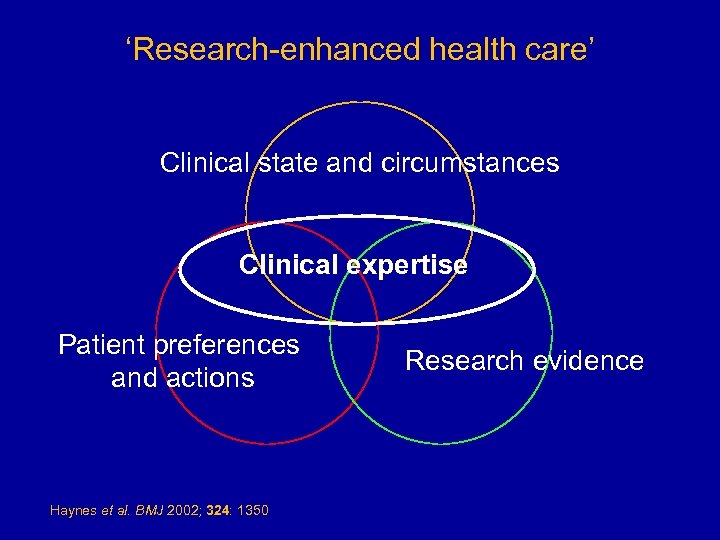
‘Research-enhanced health care’ Clinical state and circumstances Clinical expertise Patient preferences and actions Haynes et al. BMJ 2002; 324: 1350 Research evidence
Which dose?
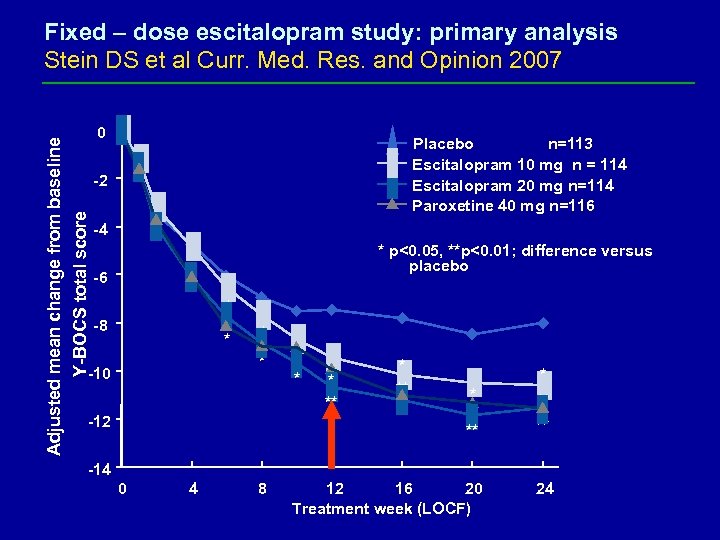
Adjusted mean change from baseline Y-BOCS total score Fixed – dose escitalopram study: primary analysis Stein DS et al Curr. Med. Res. and Opinion 2007 0 Placebo n=113 Escitalopram 10 mg n = 114 Escitalopram 20 mg n=114 Paroxetine 40 mg n=116 -2 -4 * p<0. 05, **p<0. 01; difference versus placebo -6 * -8 * * * -10 -12 * * ** ** ** 12 16 20 Treatment week (LOCF) 24 ** -14 0 4 8
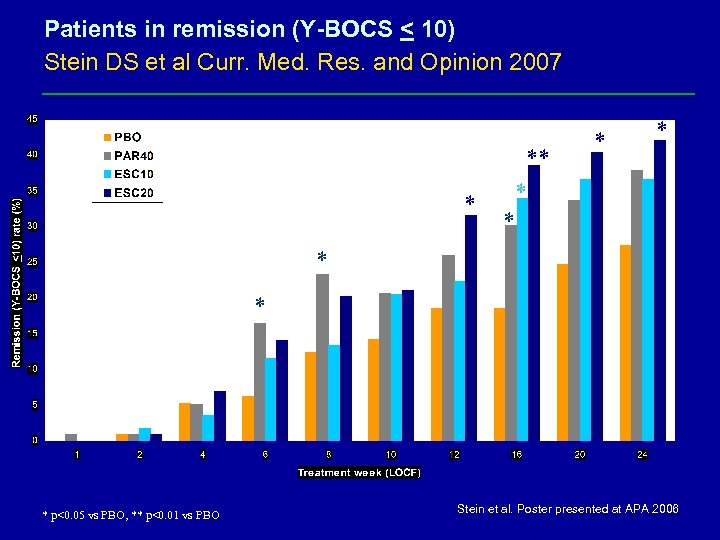
Patients in remission (Y-BOCS < 10) Stein DS et al Curr. Med. Res. and Opinion 2007 * ** * * * p<0. 05 vs PBO, ** p<0. 01 vs PBO Stein et al. Poster presented at APA 2006
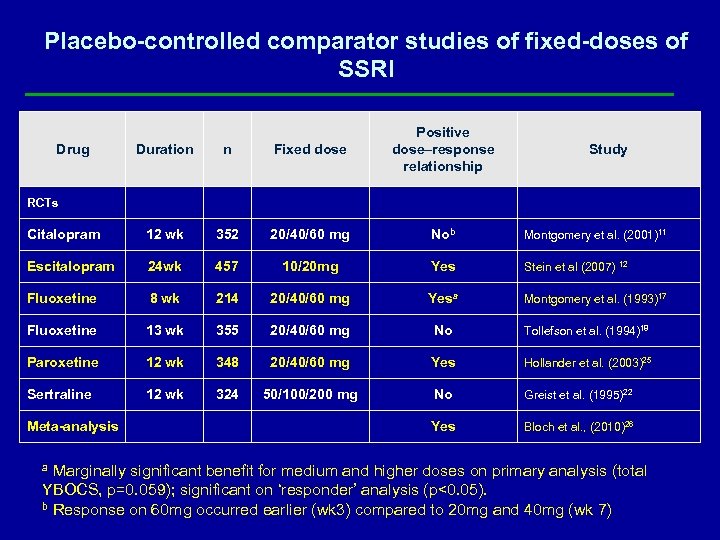
Placebo-controlled comparator studies of fixed-doses of SSRI Duration n Fixed dose Positive dose–response relationship Citalopram 12 wk 352 20/40/60 mg Nob Montgomery et al. (2001)11 Escitalopram 24 wk 457 10/20 mg Yes Stein et al (2007) 12 Fluoxetine 8 wk 214 20/40/60 mg Yesa Montgomery et al. (1993)17 Fluoxetine 13 wk 355 20/40/60 mg No Tollefson et al. (1994)18 Paroxetine 12 wk 348 20/40/60 mg Yes Hollander et al. (2003)25 Sertraline 12 wk 324 50/100/200 mg No Greist et al. (1995)22 Yes Bloch et al. , (2010)26 Drug Study RCTs Meta-analysis a Marginally significant benefit for medium and higher doses on primary analysis (total YBOCS, p=0. 059); significant on ‘responder’ analysis (p<0. 05). b Response on 60 mg occurred earlier (wk 3) compared to 20 mg and 40 mg (wk 7)
Does SSRI improve health related disability and quality of life?
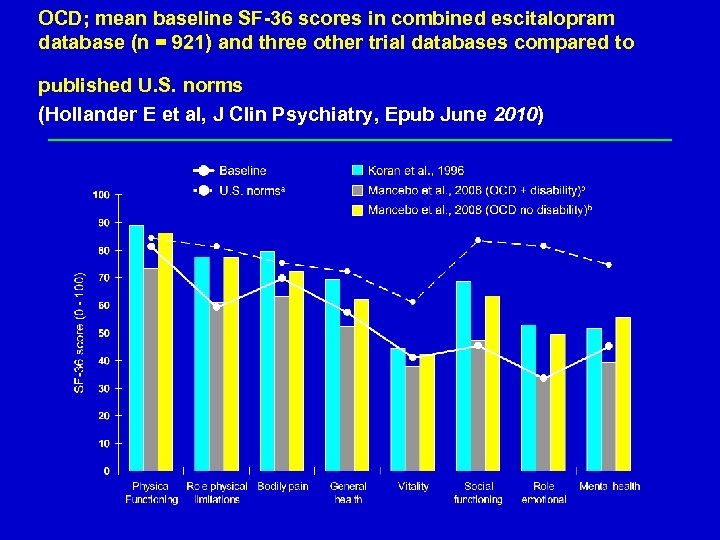
OCD; mean baseline SF-36 scores in combined escitalopram database (n = 921) and three other trial databases compared to published U. S. norms (Hollander E et al, J Clin Psychiatry, Epub June 2010) David Baldwin 17
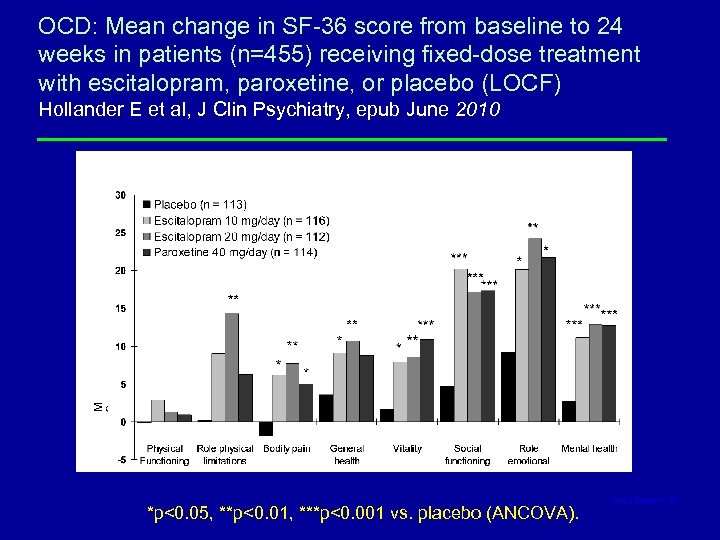
OCD: Mean change in SF-36 score from baseline to 24 weeks in patients (n=455) receiving fixed-dose treatment with escitalopram, paroxetine, or placebo (LOCF) Hollander E et al, J Clin Psychiatry, epub June 2010 *p<0. 05, **p<0. 01, ***p<0. 001 vs. placebo (ANCOVA). David Baldwin 18
Does combining medication and CBT improve outcomes?
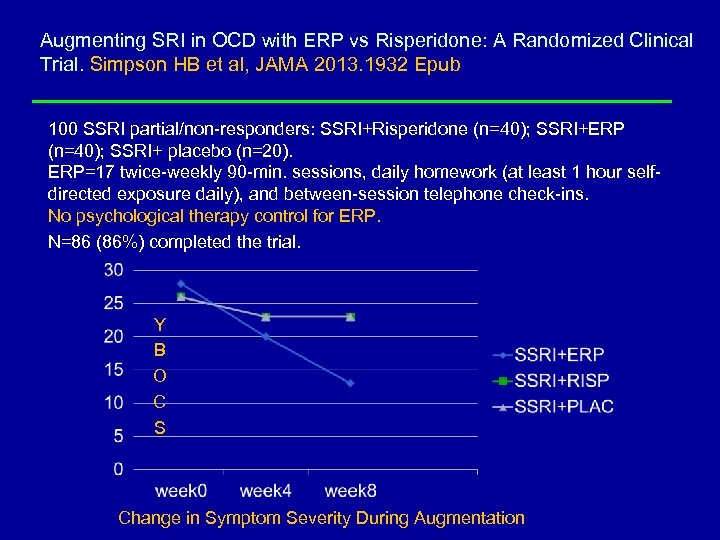
Augmenting SRI in OCD with ERP vs Risperidone: A Randomized Clinical Trial. Simpson HB et al, JAMA 2013. 1932 Epub 100 SSRI partial/non-responders: SSRI+Risperidone (n=40); SSRI+ERP (n=40); SSRI+ placebo (n=20). ERP=17 twice-weekly 90 -min. sessions, daily homework (at least 1 hour selfdirected exposure daily), and between-session telephone check-ins. No psychological therapy control for ERP. N=86 (86%) completed the trial. Y B O C S Change in Symptom Severity During Augmentation
Can we predict outcomes on an individual basis?
Early improvement as an indicator of treatment response in OCD? Implications for early-treatment decision-making. Da Conceicao DL 2013, J Psychiat Res Nov; 47(11): 1700 -7 A pragmatic naturalistic 12 -week SRI trial with 128 subjects. Early improvement (>= 20% reduction in baseline Y-BOCS) at 4 weeks was the best predictor of treatment response (>=35% Y-BOCS improvement) at 12 weeks (OR = 1. 05, p < 0. 0001). Only 20% of patients who did not improve at 4 weeks were responders after 12 weeks. But, only 55% who showed early improvement ended up responders at 12 weeks.
Five-year course of obsessive-compulsive disorder: predictors of remission and relapse. Eisen JL et al. , J Clin Psychiatry. 2013 Mar; 74(3): 233 -9. 213 adults with DSM-IV OCD Recruited between 2001 -6 OCD symptoms assessed annually over 5 -year follow-up - 39% participants entered either partial (22. 1%) or full (16. 9%) remission. - Obsessions regarding harm nearly twice as likely to remit (P <. 05) - Other positive predictors of remission included lower OCD severity (P < . 0001) and shorter duration of illness (P <. 0001) - Primary hoarding sig less likely to remit (2 of 21 participants (9. 5%). - 59% participants who remitted subsequently relapsed. - Participants with obsessive-compulsive personality disorder more than twice as likely to relapse (P <. 005). - Participants also more likely to relapse if they experienced partial remission versus full remission (70% vs 45%; P <. 05)
Long-term course of paediatric OCD: 3 years of prospective follow-up. Mancebo MC et al Compr Psychiatry. 2014 Oct; 55(7): 1498 -504. • 60 youth and their parents • Annual follow-up interviews for 3 years - 80% patients achieved either partial (53%) or full (27%) remission - Better functioning at intake and a shorter latency to initial OCD treatment were associated with faster onset of remission (P<. 001). - 21% of those who remitted subsequently relapsed (mean 88 wk f-up) CONCLUSIONS • Remission is more likely among youth versus adults with OCD. • Treatment early in the course of illness and before substantial impact on functioning predicts a better course.
How long to remain on treatment?
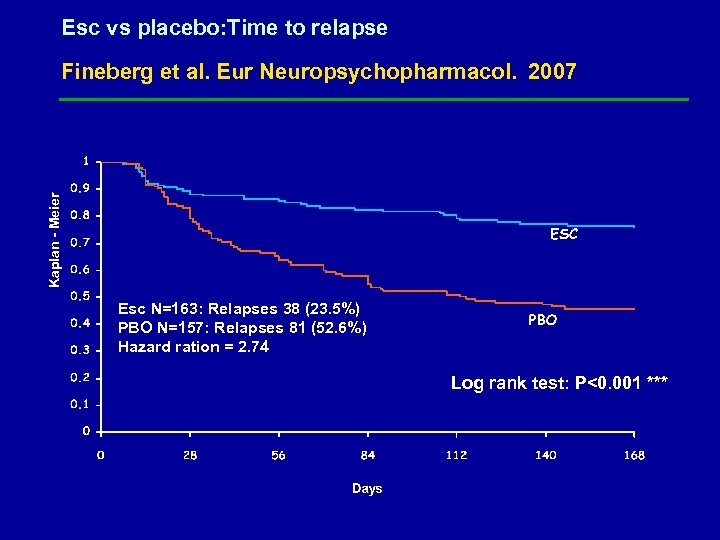
Esc vs placebo: Time to relapse Kaplan - Meier Fineberg et al. Eur Neuropsychopharmacol. 2007 Esc N=163: Relapses 38 (23. 5%) PBO N=157: Relapses 81 (52. 6%) Hazard ration = 2. 74 ESC N=163; Relapses: 38 (23. 5%) PBO N=157; Relapses: 81 (52. 6%) Hazard ratio = 2. 74 N=320 (ESC 163, PBO 157 ) Log rank test: P<0. 001 ***
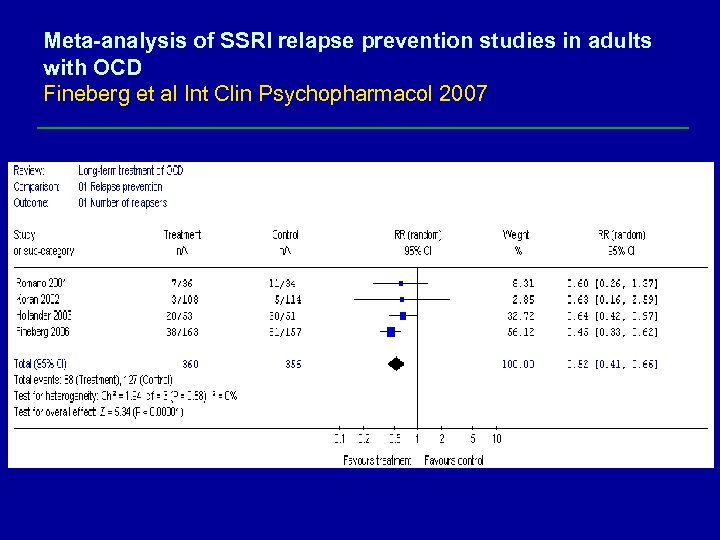
Meta-analysis of SSRI relapse prevention studies in adults with OCD Fineberg et al Int Clin Psychopharmacol 2007
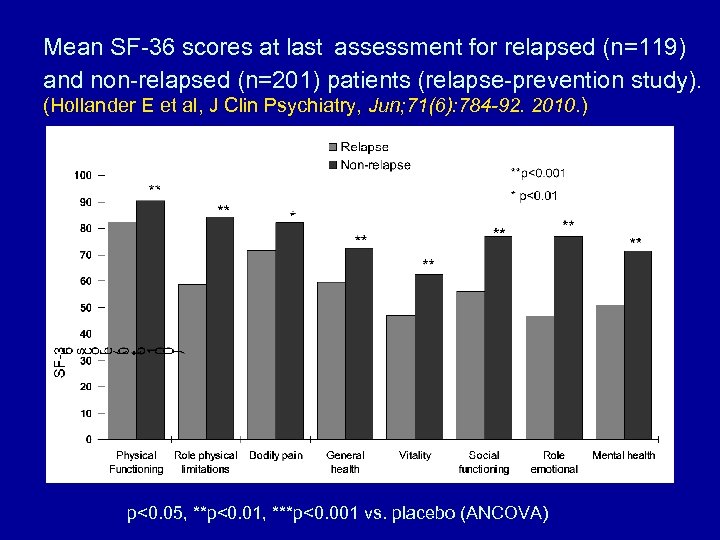
Mean SF-36 scores at last assessment for relapsed (n=119) and non-relapsed (n=201) patients (relapse-prevention study). (Hollander E et al, J Clin Psychiatry, Jun; 71(6): 784 -92. 2010. ) p<0. 05, **p<0. 01, ***p<0. 001 vs. placebo (ANCOVA)
How to treat resistant OCD?
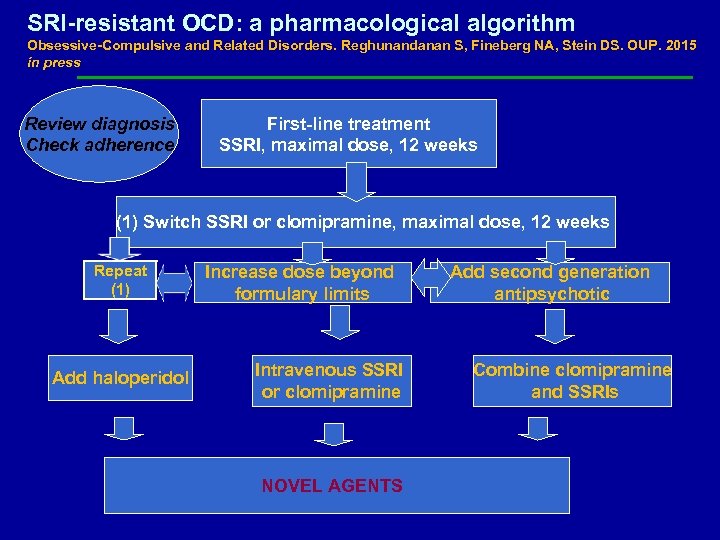
SRI-resistant OCD: a pharmacological algorithm Obsessive-Compulsive and Related Disorders. Reghunandanan S, Fineberg NA, Stein DS. OUP. 2015 in press Review diagnosis Check adherence First-line treatment SSRI, maximal dose, 12 weeks (1) Switch SSRI or clomipramine, maximal dose, 12 weeks Repeat (1) Add haloperidol Increase dose beyond formulary limits Intravenous SSRI or clomipramine NOVEL AGENTS Add second generation antipsychotic Combine clomipramine and SSRIs
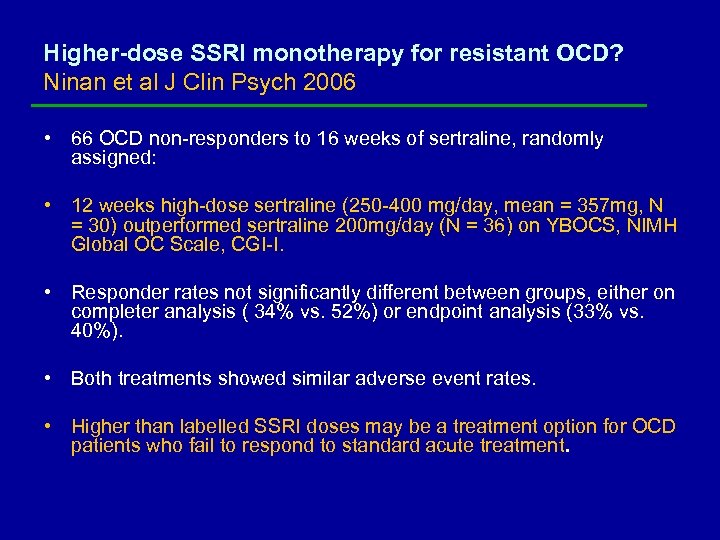
Higher-dose SSRI monotherapy for resistant OCD? Ninan et al J Clin Psych 2006 • 66 OCD non-responders to 16 weeks of sertraline, randomly assigned: • 12 weeks high-dose sertraline (250 -400 mg/day, mean = 357 mg, N = 30) outperformed sertraline 200 mg/day (N = 36) on YBOCS, NIMH Global OC Scale, CGI-I. • Responder rates not significantly different between groups, either on completer analysis ( 34% vs. 52%) or endpoint analysis (33% vs. 40%). • Both treatments showed similar adverse event rates. • Higher than labelled SSRI doses may be a treatment option for OCD patients who fail to respond to standard acute treatment.
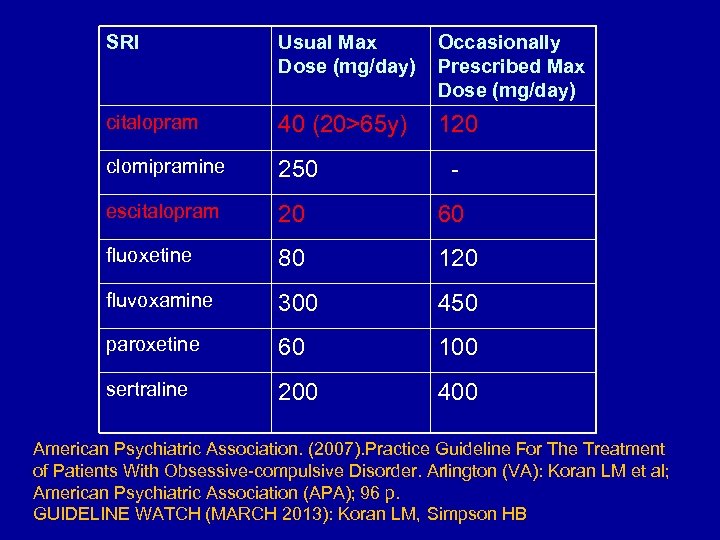
SRI Usual Max Dose (mg/day) Occasionally Prescribed Max Dose (mg/day) citalopram 40 (20>65 y) 120 clomipramine 250 - escitalopram 20 60 fluoxetine 80 120 fluvoxamine 300 450 paroxetine 60 100 sertraline 200 400 American Psychiatric Association. (2007). Practice Guideline For The Treatment of Patients With Obsessive-compulsive Disorder. Arlington (VA): Koran LM et al; American Psychiatric Association (APA); 96 p. GUIDELINE WATCH (MARCH 2013): Koran LM, Simpson HB
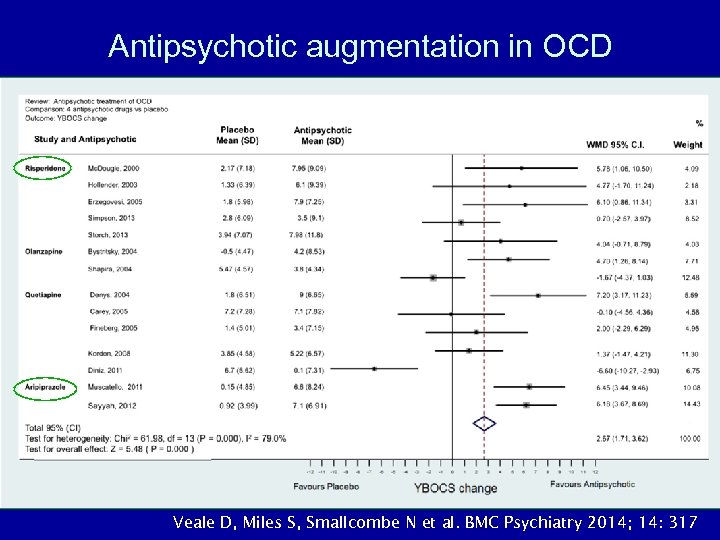
Antipsychotic augmentation in OCD Veale D, Miles S, Smallcombe N et al. BMC Psychiatry 2014; 14: 317

Effectiveness SMD YBOCS D 2 R and D 3 R ( but not 5 HTR) affinity predicts effectiveness of antipsychotic in OCD: a mixed model meta-regression analysis on 13 RCTs. Ducasse D et al, 2014 Psychopharmacology (Berl). 2014 Sep; 231(18): 3765 -70 Log Ki D 3 Log Ki D 2 NB: Studies are small in size and number (N=13), with varied methodologies and entry criteria
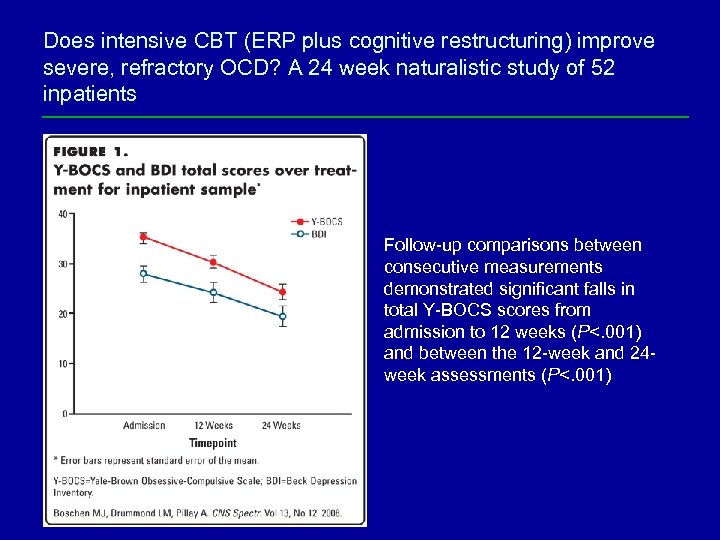
Does intensive CBT (ERP plus cognitive restructuring) improve severe, refractory OCD? A 24 week naturalistic study of 52 inpatients Follow-up comparisons between consecutive measurements demonstrated significant falls in total Y-BOCS scores from admission to 12 weeks (P<. 001) and between the 12 -week and 24 week assessments (P<. 001)
Novel treatment targets in OCD
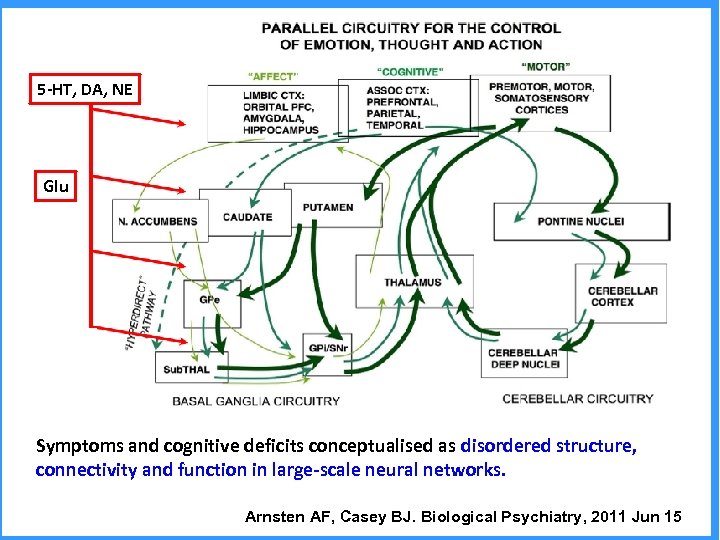
5 -HT, DA, NE Glu Symptoms and cognitive deficits conceptualised as disordered structure, connectivity and function in large-scale neural networks. Arnsten AF, Casey BJ. Biological Psychiatry, 2011 Jun 15
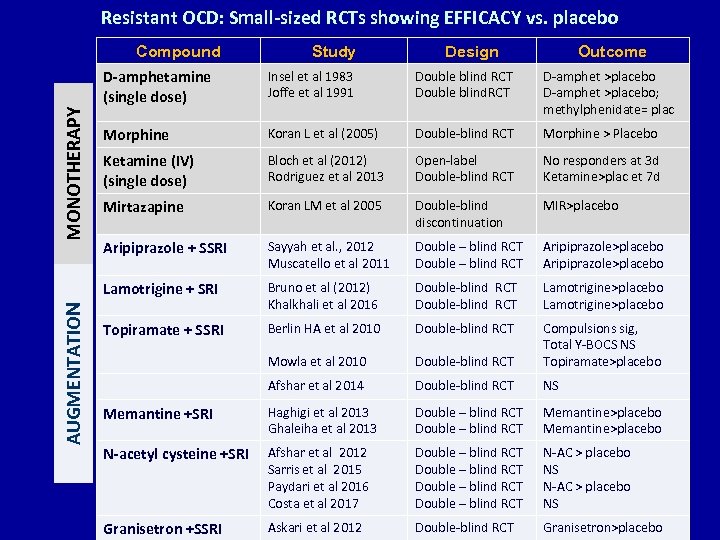
Resistant OCD: Small-sized RCTs showing EFFICACY vs. placebo Compound Study Design Outcome AUGMENTATION Insel et al 1983 Joffe et al 1991 Double blind RCT Double blind. RCT D-amphet >placebo; methylphenidate= plac Morphine Koran L et al (2005) Double-blind RCT Morphine > Placebo Ketamine (IV) (single dose) Bloch et al (2012) Rodriguez et al 2013 Open-label Double-blind RCT No responders at 3 d Ketamine>plac et 7 d Mirtazapine Koran LM et al 2005 Double-blind discontinuation MIR>placebo Aripiprazole + SSRI Sayyah et al. , 2012 Muscatello et al 2011 Double – blind RCT Aripiprazole>placebo Lamotrigine + SRI MONOTHERAPY D-amphetamine (single dose) Bruno et al (2012) Khalkhali et al 2016 Double-blind RCT Lamotrigine>placebo Topiramate + SSRI Berlin HA et al 2010 Double-blind RCT Mowla et al 2010 Double-blind RCT Compulsions sig, Total Y-BOCS NS Topiramate>placebo Afshar et al 2014 Double-blind RCT NS Memantine +SRI Haghigi et al 2013 Ghaleiha et al 2013 Double – blind RCT Memantine>placebo N-acetyl cysteine +SRI Afshar et al 2012 Sarris et al 2015 Paydari et al 2016 Costa et al 2017 Double – blind RCT N-AC > placebo NS Granisetron +SSRI Askari et al 2012 Double-blind RCT Granisetron>placebo
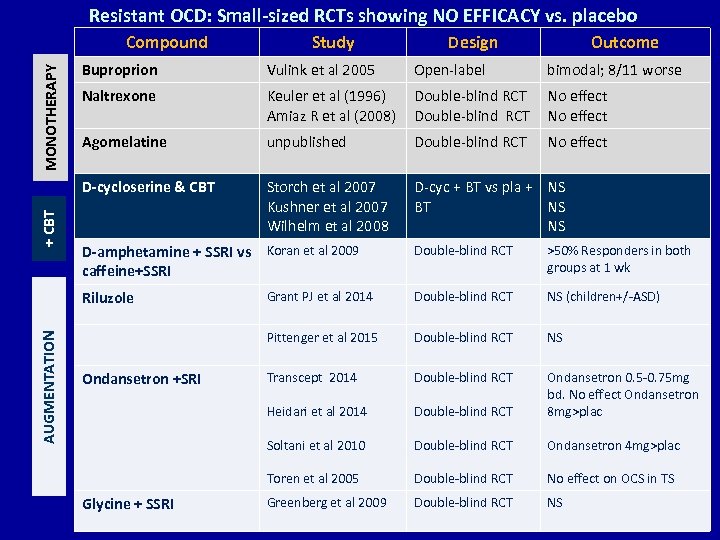
Resistant OCD: Small-sized RCTs showing NO EFFICACY vs. placebo Compound Study Design Outcome MONOTHERAPY Vulink et al 2005 Open-label bimodal; 8/11 worse Naltrexone Keuler et al (1996) Amiaz R et al (2008) Double-blind RCT No effect Agomelatine unpublished Double-blind RCT No effect D-cycloserine & CBT + CBT Buproprion Storch et al 2007 Kushner et al 2007 Wilhelm et al 2008 D-cyc + BT vs pla + NS BT NS NS Double-blind RCT >50% Responders in both groups at 1 wk Riluzole AUGMENTATION D-amphetamine + SSRI vs Koran et al 2009 caffeine+SSRI Grant PJ et al 2014 Double-blind RCT NS (children+/-ASD) Pittenger et al 2015 Double-blind RCT NS Transcept 2014 Double-blind RCT Heidari et al 2014 Double-blind RCT Ondansetron 0. 5 -0. 75 mg bd. No effect Ondansetron 8 mg>plac Soltani et al 2010 Double-blind RCT Ondansetron 4 mg>plac Toren et al 2005 Double-blind RCT No effect on OCS in TS Greenberg et al 2009 Double-blind RCT NS Ondansetron +SRI Glycine + SSRI
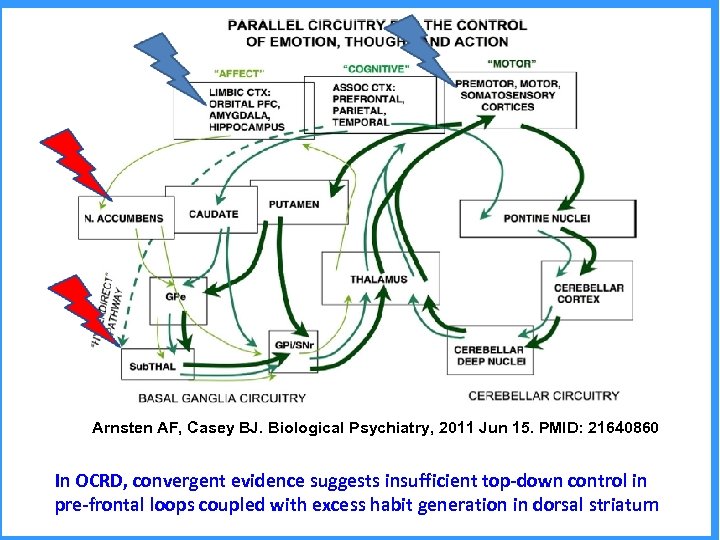
Arnsten AF, Casey BJ. Biological Psychiatry, 2011 Jun 15. PMID: 21640860 In OCRD, convergent evidence suggests insufficient top-down control in pre-frontal loops coupled with excess habit generation in dorsal striatum
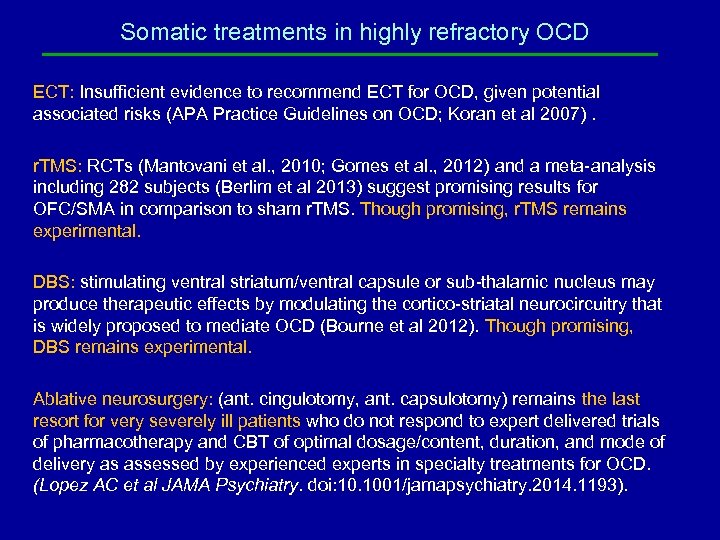
Somatic treatments in highly refractory OCD ECT: Insufficient evidence to recommend ECT for OCD, given potential associated risks (APA Practice Guidelines on OCD; Koran et al 2007). r. TMS: RCTs (Mantovani et al. , 2010; Gomes et al. , 2012) and a meta-analysis including 282 subjects (Berlim et al 2013) suggest promising results for OFC/SMA in comparison to sham r. TMS. Though promising, r. TMS remains experimental. DBS: stimulating ventral striatum/ventral capsule or sub-thalamic nucleus may produce therapeutic effects by modulating the cortico-striatal neurocircuitry that is widely proposed to mediate OCD (Bourne et al 2012). Though promising, DBS remains experimental. Ablative neurosurgery: (ant. cingulotomy, ant. capsulotomy) remains the last resort for very severely ill patients who do not respond to expert delivered trials of pharmacotherapy and CBT of optimal dosage/content, duration, and mode of delivery as assessed by experienced experts in specialty treatments for OCD. (Lopez AC et al JAMA Psychiatry. doi: 10. 1001/jamapsychiatry. 2014. 1193).
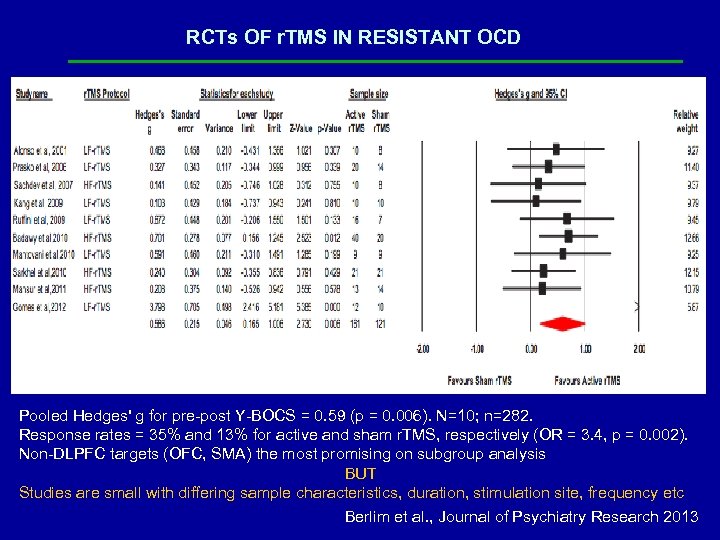
RCTs OF r. TMS IN RESISTANT OCD Pooled Hedges' g for pre-post Y-BOCS = 0. 59 (p = 0. 006). N=10; n=282. Response rates = 35% and 13% for active and sham r. TMS, respectively (OR = 3. 4, p = 0. 002). Non-DLPFC targets (OFC, SMA) the most promising on subgroup analysis BUT Studies are small with differing sample characteristics, duration, stimulation site, frequency etc Berlim et al. , Journal of Psychiatry Research 2013
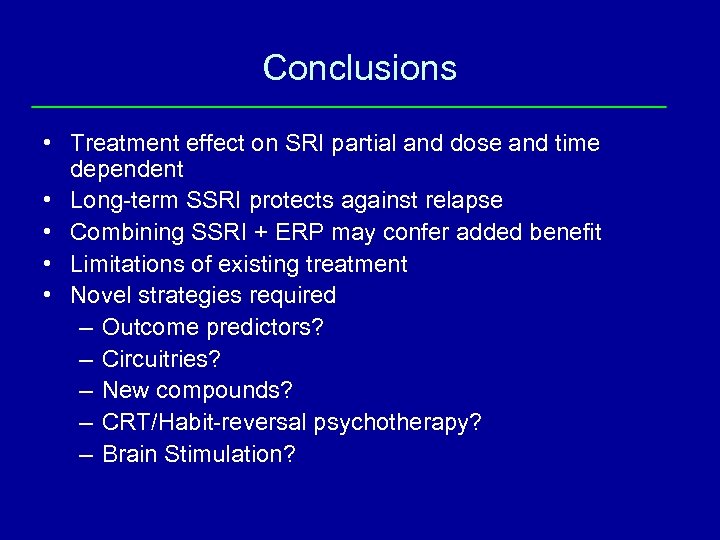
Conclusions • Treatment effect on SRI partial and dose and time dependent • Long-term SSRI protects against relapse • Combining SSRI + ERP may confer added benefit • Limitations of existing treatment • Novel strategies required – Outcome predictors? – Circuitries? – New compounds? – CRT/Habit-reversal psychotherapy? – Brain Stimulation?

THANK YOU
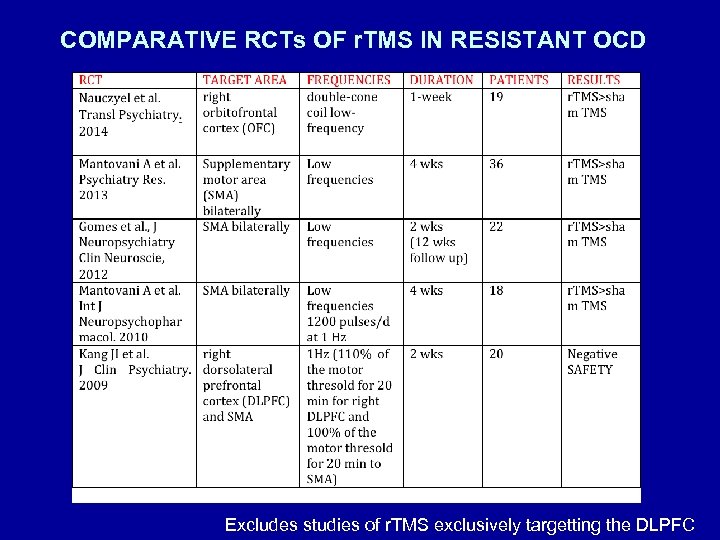
COMPARATIVE RCTs OF r. TMS IN RESISTANT OCD Excludes studies of r. TMS exclusively targetting the DLPFC
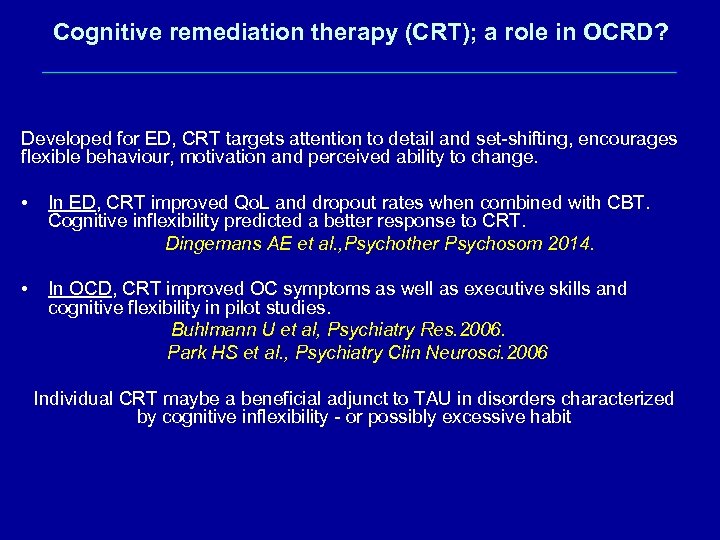
Cognitive remediation therapy (CRT); a role in OCRD? Developed for ED, CRT targets attention to detail and set-shifting, encourages flexible behaviour, motivation and perceived ability to change. • In ED, CRT improved Qo. L and dropout rates when combined with CBT. Cognitive inflexibility predicted a better response to CRT. Dingemans AE et al. , Psychother Psychosom 2014. • In OCD, CRT improved OC symptoms as well as executive skills and cognitive flexibility in pilot studies. Buhlmann U et al, Psychiatry Res. 2006. Park HS et al. , Psychiatry Clin Neurosci. 2006 Individual CRT maybe a beneficial adjunct to TAU in disorders characterized by cognitive inflexibility - or possibly excessive habit
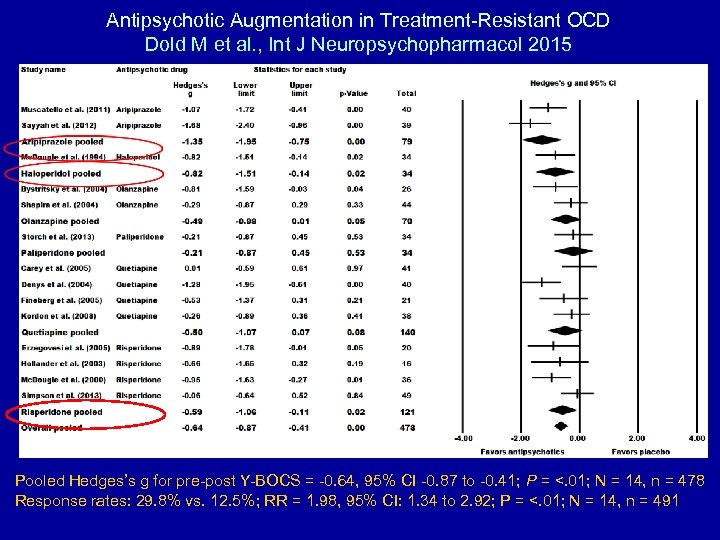
Antipsychotic Augmentation in Treatment-Resistant OCD Dold M et al. , Int J Neuropsychopharmacol 2015 Pooled Hedges’s g for pre-post Y-BOCS = -0. 64, 95% CI -0. 87 to -0. 41; P = <. 01; N = 14, n = 478 Response rates: 29. 8% vs. 12. 5%; RR = 1. 98, 95% CI: 1. 34 to 2. 92; P = <. 01; N = 14, n = 491
28a8fcbdc5c6961810cf85ca147c11c7.ppt