15c8f52e79fb614d948caefd1bc2e845.ppt
- Количество слайдов: 30
Lakes District Health Board Surgical Services Improvement Journey Improving the System - Meeting the Challenge – April 2012 Greg Vandergoot – Service Manager, Surgical & Elective Services Martin Thomas – Clinical Director Surgical & Elective Services Healthy Communities – Mauriora!
Overview § § § Lakes District Health Board Background Project Outcomes Ongoing Work Healthy Communities – Mauriora!
Lakes District Health Board l Population base (incorporating Lakes District) 108, 000 Operates from two sites, Rotorua and Taupo Rotorua theatre capacity three elective, one acute and endoscopy unit Taupo day-case theatre with an endoscopy facility l Ageing facilities l Surgical & Elective Services covers the following specialties: Ear, Nose, and Throat (ENT) General Surgery Orthopaedics Ophthalmology (Provided through Lakes Ophthalmic Services Ltd (LOSL) Plastic Surgery (outpatients provided though Health Waikato) Urology (Provided through Venturo Subcontract) Vascular Surgery as part of General Surgery Audiology l l l Healthy Communities – Mauriora!
Service Improvement Project Background § Issues regarding theatre throughput and utilisation raised by medical and clinical staff 2005 § Some work done historically to address issues but found that it was too complex and required sound project methodology § Recognised the need to set up as a project to ensure a sustainable outcome. Project Team established 2006 Healthy Communities – Mauriora!
Over-arching Issues l l l l l Improvement in Theatre Utilisation identified Reactive vs Proactive system Recruitment and Retention (Anaesthetics and Nursing) Patient complaints High hospital driven day of surgery cancellations Negative view of service and service performance Data rich, information poor Staff frustrated and felt disempowered Rationing of services Healthy Communities – Mauriora!
Project Principles l Patients at the Centre l Sustainability long term l Staff buy in and involvement l Short term and long terms Healthy Communities – Mauriora!
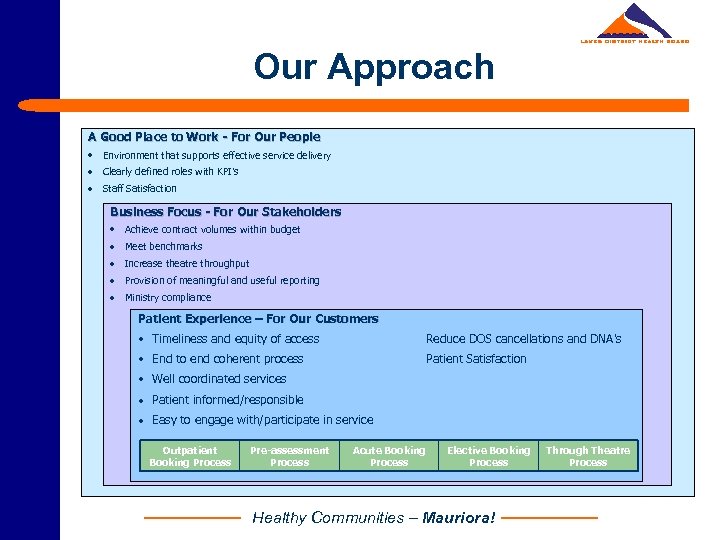
Our Approach A Good Place to Work - For Our People • Environment that supports effective service delivery · Clearly defined roles with KPI’s · Staff Satisfaction Business Focus - For Our Stakeholders • Achieve contract volumes within budget · Meet benchmarks · Increase theatre throughput · Provision of meaningful and useful reporting · Ministry compliance Patient Experience – For Our Customers • Timeliness and equity of access Reduce DOS cancellations and DNA’s • End to end coherent process Patient Satisfaction • Well coordinated services · Patient informed/responsible · Easy to engage with/participate in service Outpatient Booking Process Pre-assessment Process Acute Booking Process Elective Booking Process Healthy Communities – Mauriora! Through Theatre Process
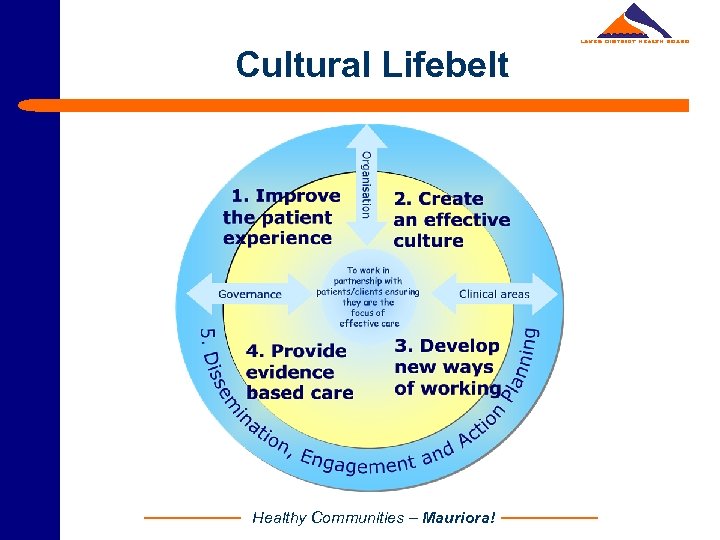
Cultural Lifebelt Healthy Communities – Mauriora!

Goals and Objectives l Quality care for patients l Improve efficiency and productivity within Surgical Service l Support Clinical Leadership l Redefine scheduling, reporting and rostering processes l Improve theatre roster co-ordination and communciation l Development of tools to ensure ongoing service improvement and decision making l To create an environment that supported and promoted staff involvement in service improvement Healthy Communities – Mauriora!
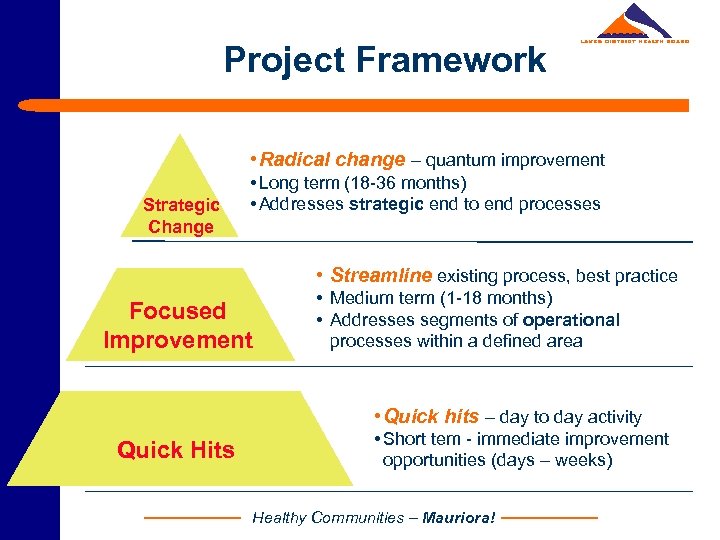
Project Framework • Radical change – quantum improvement Strategic Change • Long term (18 -36 months) • Addresses strategic end to end processes • Streamline existing process, best practice Focused Improvement • Medium term (1 -18 months) • Addresses segments of operational processes within a defined area • Quick hits – day to day activity Quick Hits • Short tem - immediate improvement opportunities (days – weeks) Healthy Communities – Mauriora!
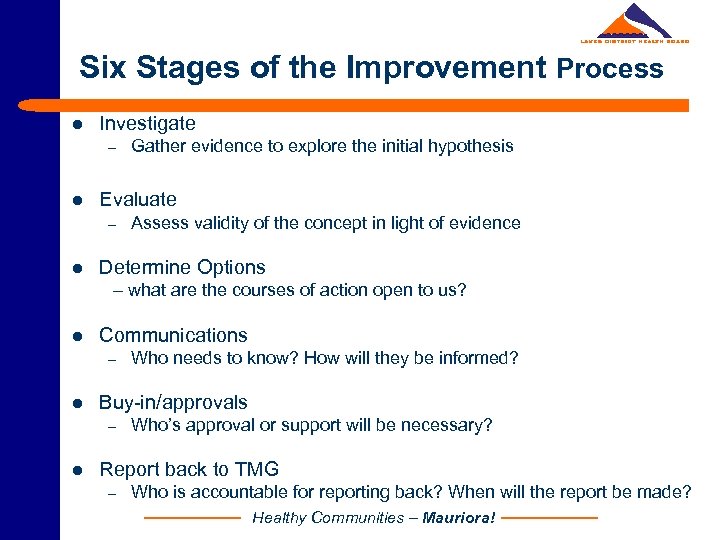
Six Stages of the Improvement Process l Investigate – l Evaluate – l Gather evidence to explore the initial hypothesis Assess validity of the concept in light of evidence Determine Options – what are the courses of action open to us? l Communications – l Buy-in/approvals – l Who needs to know? How will they be informed? Who’s approval or support will be necessary? Report back to TMG – Who is accountable for reporting back? When will the report be made? Healthy Communities – Mauriora!
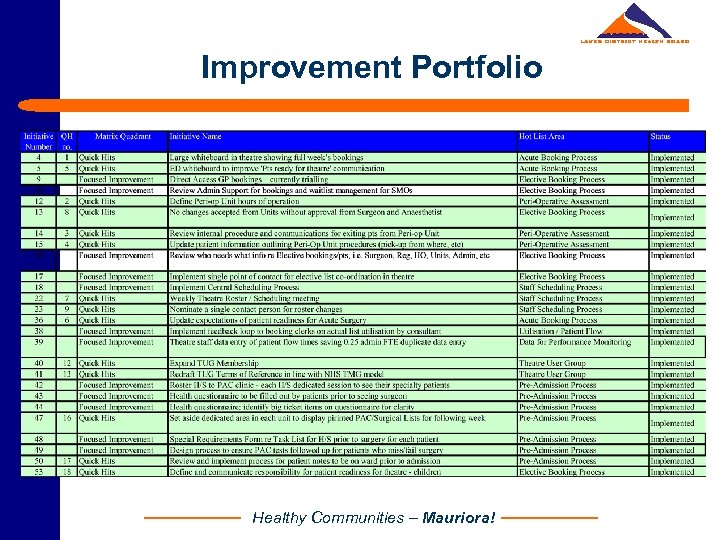
Improvement Portfolio Healthy Communities – Mauriora!
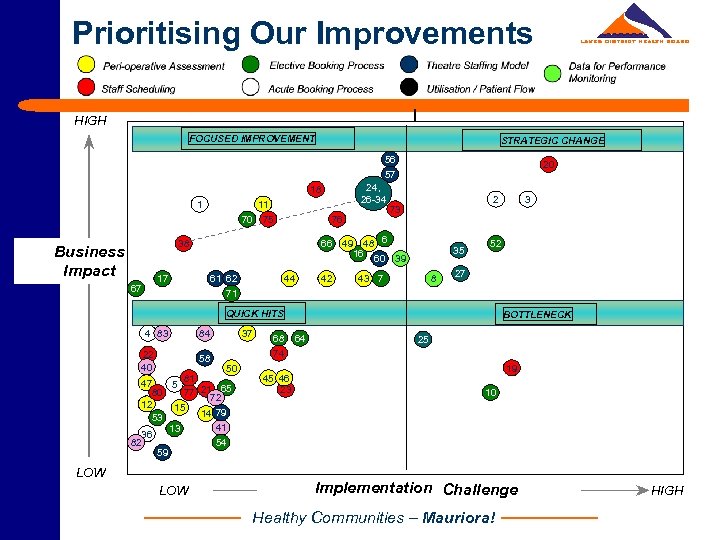
Prioritising Our Improvements HIGH FOCUSED IMPROVEMENT STRATEGIC CHANGE 56 57 24, 26 -34 18 1 11 70 75 76 38 Business Impact 17 67 66 61 62 71 44 42 20 2 73 49 48 6 16 60 39 35 43 7 8 52 27 QUICK HITS 4 83 22 40 84 58 50 81 47 5 80 77 21 65 72 12 15 14 79 53 41 13 36 82 54 59 LOW 37 68 64 74 45 46 23 3 BOTTLENECK 25 19 10 Implementation Challenge Healthy Communities – Mauriora! HIGH
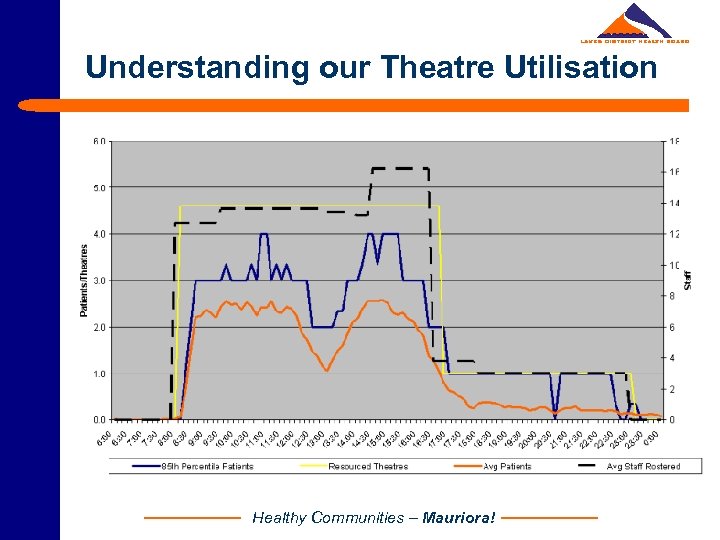
Understanding our Theatre Utilisation Healthy Communities – Mauriora!
Project Focus l Structure l Resourcing l Reporting l Theatre Roster & Schedule Analysis l Patient Journey Mapping & Detailed Process Mapping Healthy Communities – Mauriora!
What did we achieve? l Quick Hits – staff innovation and involvement l Establishment of a clinically led Theatre Management Group (TMG) – driver behind our improvement l Six weekly rolling theatre and anaesthetist roster sustained l Master Theatre Schedule Review l Introduction of flexible scheduling - sharing of lists within and across specialties l Re-designed theatre list formation and confirmation process – team focus Healthy Communities – Mauriora!

What did we achieve? l A sustainable increase in elective theatre utilisation and productivity l Theatre Dashboard Report l Specialty Procedure Times Report l Culture change – no cancellation of elective surgery l A better understanding of our business l Motivation to drive service improvement Healthy Communities – Mauriora!
General Surgery The Challenge l Unmanageable waitlist l ESPI non compliance l High cancellation of elective surgery l High number of patient complaints l Duplication of effort and rework l Clinician and staff dissatisfaction - couldn’t see the wood for the trees Addressing the Challenges l Validation of waitlist l Collaboration with private provider l Access criteria and thresholds l Business rules - clinic volumes and FSA: Follow up ratios l Pooling of patients l MDT fortnightly Scheduling Meeting Healthy Communities – Mauriora!
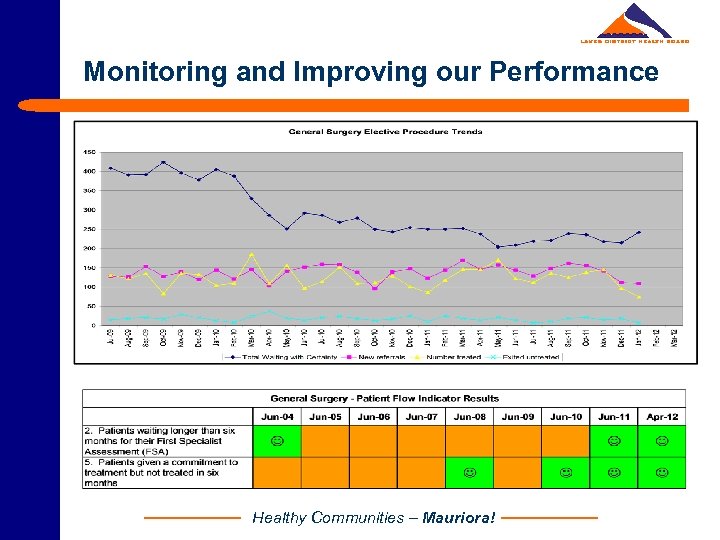
Monitoring and Improving our Performance Healthy Communities – Mauriora!
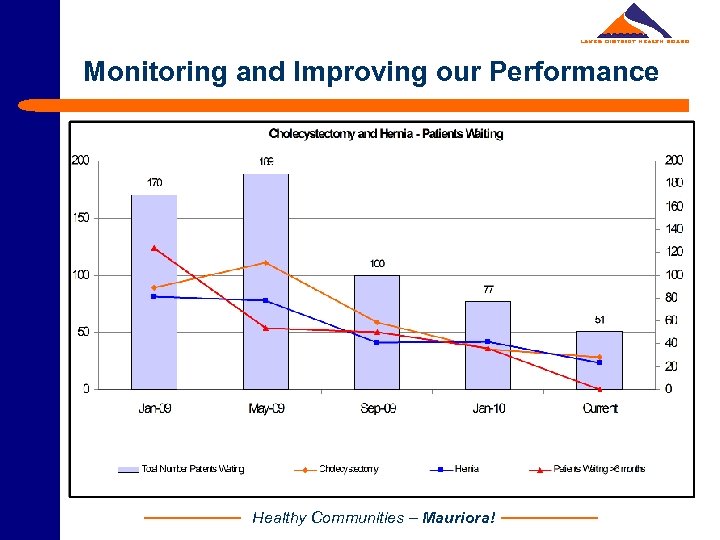
Monitoring and Improving our Performance Healthy Communities – Mauriora!
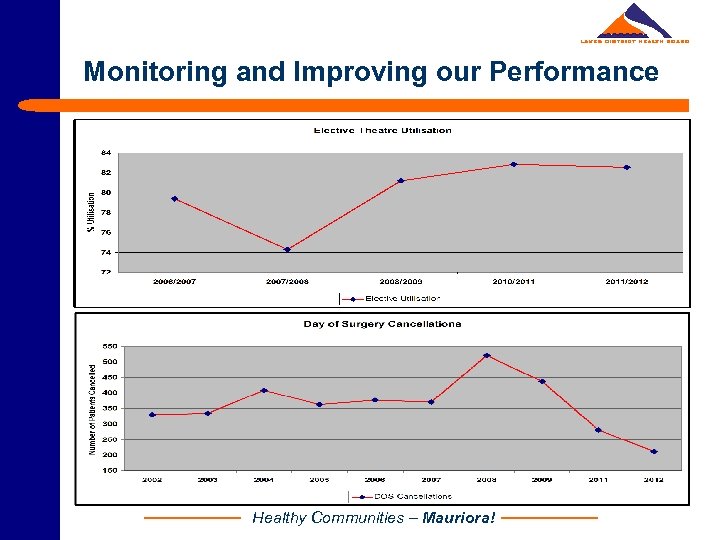
Monitoring and Improving our Performance Healthy Communities – Mauriora!
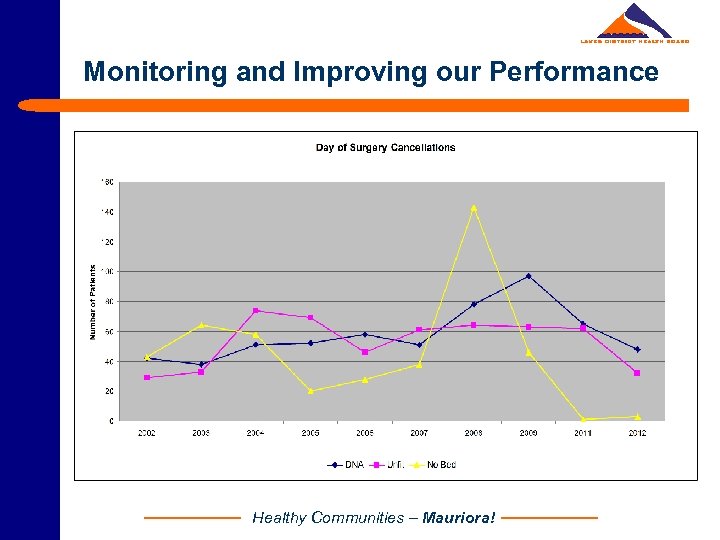
Monitoring and Improving our Performance Healthy Communities – Mauriora!
Service Changes l Strategic Planning l Service Improvement l Clinical Governance Model l Quality Focus l Balance Scorecard Healthy Communities – Mauriora!
Integration into Service Improvement l Embedded within Service Strategic Plan l TMG is fundamental to ongoing success of a Theatre Improvement Project l Needs buy in from Surgeons and other staff (clinical) l Maintaining engagement • • • l Ownership Delivery Evidence Concentrate on improvements but always reflect on successes Healthy Communities – Mauriora!
Surgical Strategic & Operational Plan Healthy Communities – Mauriora!
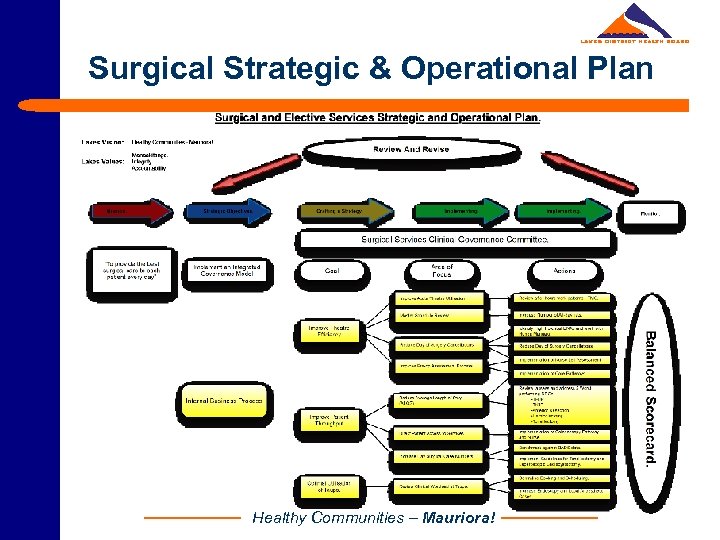
Surgical Strategic & Operational Plan Healthy Communities – Mauriora!
Key Learnings l The Service Improvement Process is ownership and accountability l Staff engagement l Leadership is key l Change is a difficult process l Perseverance and persistence can and does change culture l No quick fixes but a lack of action is not an option l Complex problems require a framework to address l Change is not a one time effort! Healthy Communities – Mauriora!
Making it Happen! l Enough need – a burning deck, a reason to change l Enough time – like a chronic disease, it’s a long journey l Enough money – waste reduction = resource gain l Enough knowledge / methodology l Enough support – at the right levels l Enough willingness, stamina and vision Healthy Communities – Mauriora!
Current Challenges l Ministry of Health Targets – Strategic Direction l Regional collaboration for Elective Surgery l Theatre Management Group maintaining impetus l Adherence to specialty business rules – eg entry and access criteria l Ongoing development of the Clinical Governance Framework l Facility redevelopment and co-location of service staff – management, administrators, clinicians l Resource efficiency vs funding constraints Healthy Communities – Mauriora!
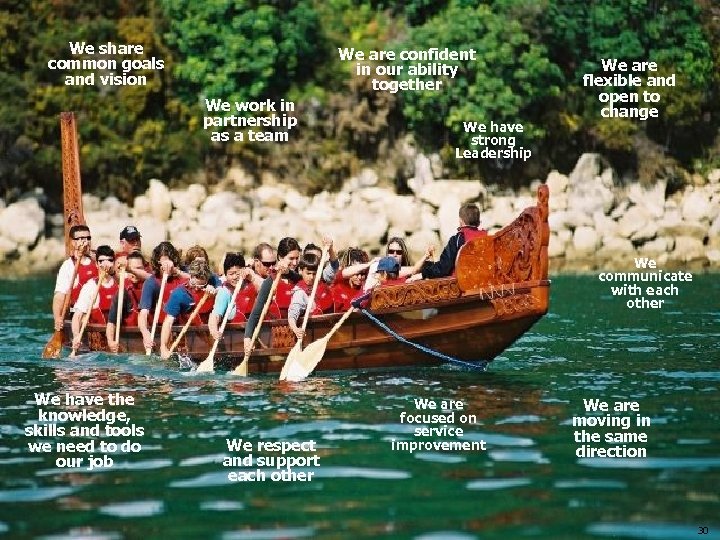
We share common goals and vision We are confident in our ability together We work in partnership as a team We have strong Leadership We are flexible and open to change We communicate with each other We have the knowledge, skills and tools we need to do our job We respect and support each other We are focused on service improvement We are moving in the same direction 30
15c8f52e79fb614d948caefd1bc2e845.ppt