leg.pptx
- Количество слайдов: 137
 KURSK STATE MEDICAL UNIVERSITY DEPARTMENT OF TRAUMATOLOGY AND ORTHOPAEDICS SURGERY Injuries of a Leg
KURSK STATE MEDICAL UNIVERSITY DEPARTMENT OF TRAUMATOLOGY AND ORTHOPAEDICS SURGERY Injuries of a Leg
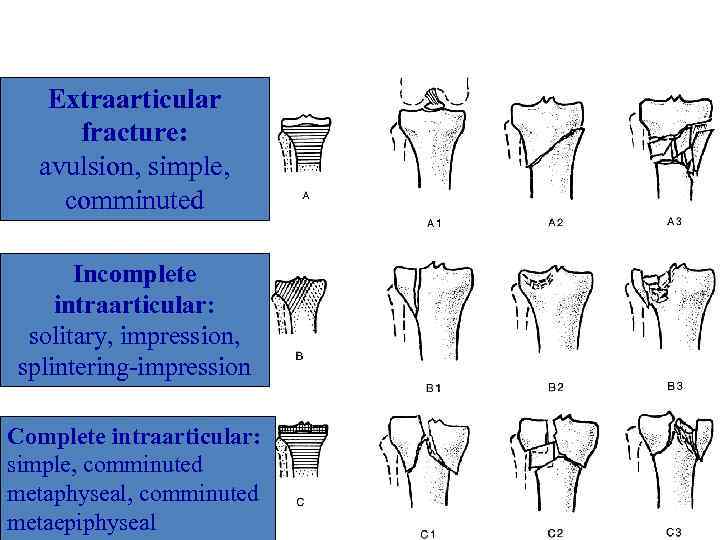 Classification AO of proximal part of leg’s bones Extraarticular fracture: avulsion, simple, comminuted Incomplete intraarticular: solitary, impression, splintering-impression Complete intraarticular: simple, comminuted metaphyseal, comminuted metaepiphyseal
Classification AO of proximal part of leg’s bones Extraarticular fracture: avulsion, simple, comminuted Incomplete intraarticular: solitary, impression, splintering-impression Complete intraarticular: simple, comminuted metaphyseal, comminuted metaepiphyseal
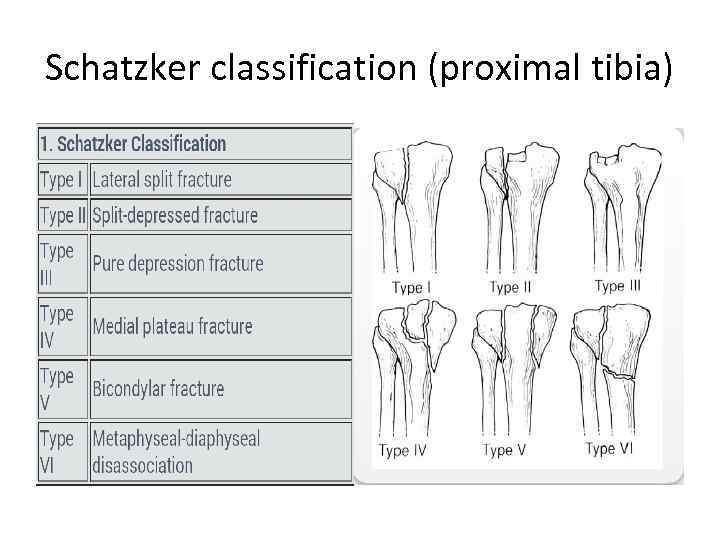 Schatzker classification (proximal tibia)
Schatzker classification (proximal tibia)
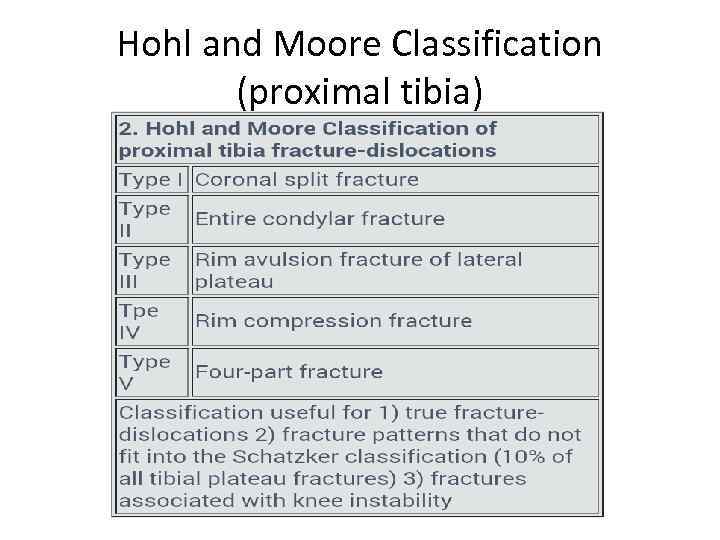 Hohl and Moore Classification (proximal tibia)
Hohl and Moore Classification (proximal tibia)
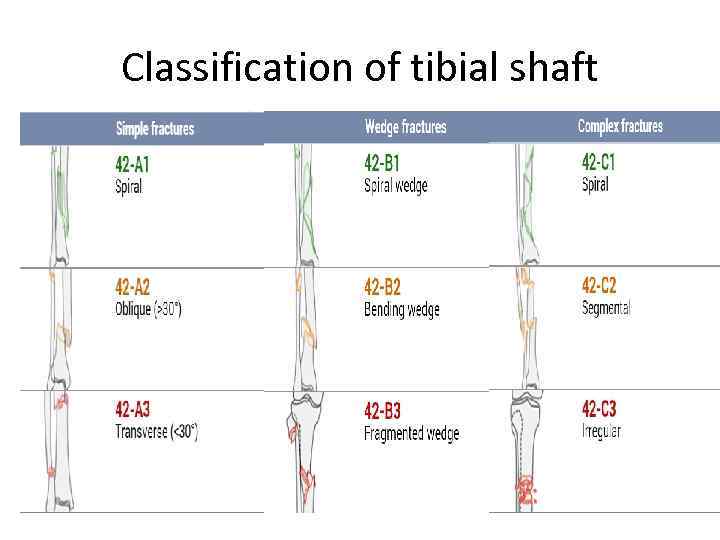 Classification of tibial shaft
Classification of tibial shaft
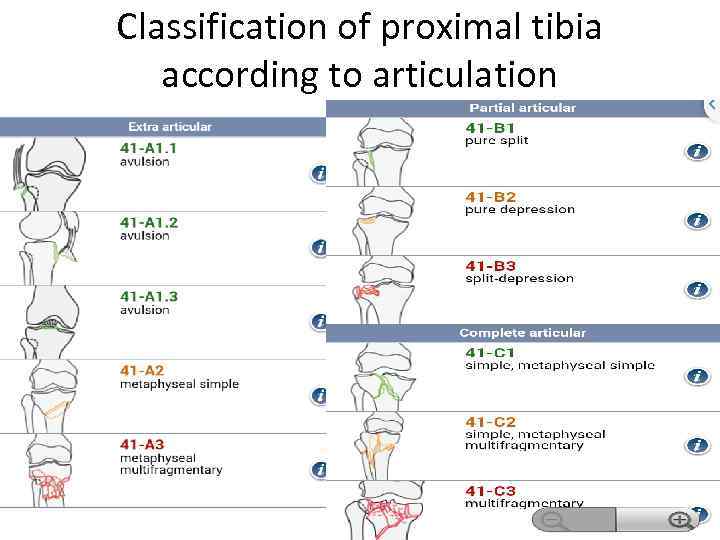 Classification of proximal tibia according to articulation
Classification of proximal tibia according to articulation
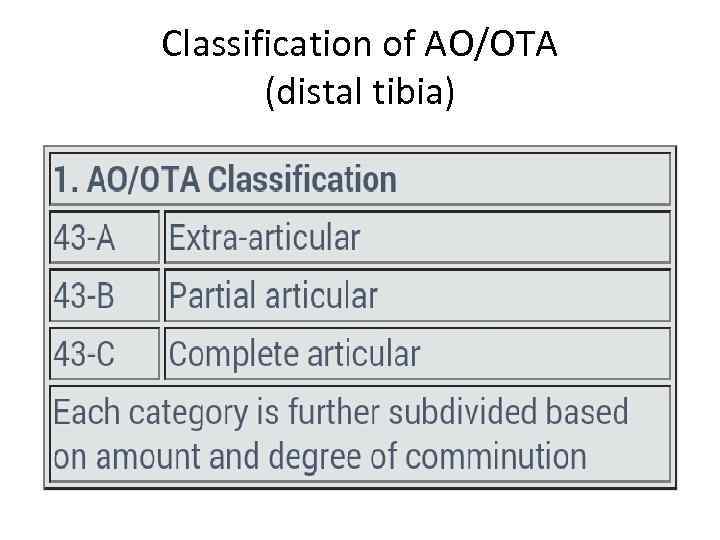 Classification of AO/OTA (distal tibia)
Classification of AO/OTA (distal tibia)
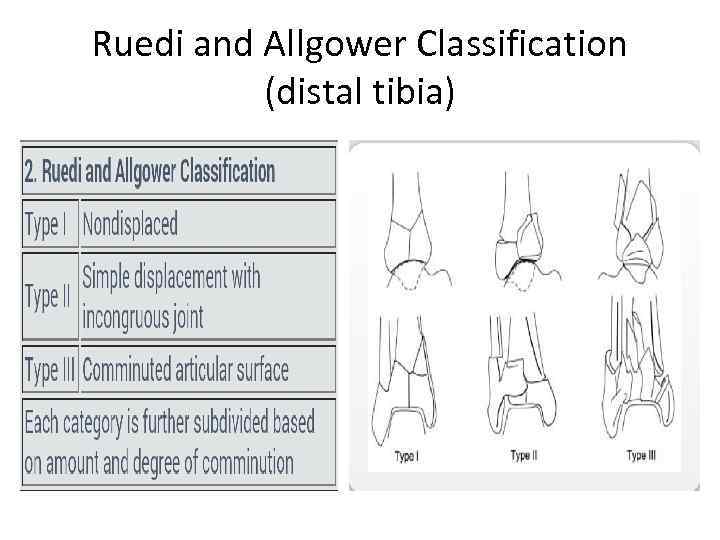 Ruedi and Allgower Classification (distal tibia)
Ruedi and Allgower Classification (distal tibia)
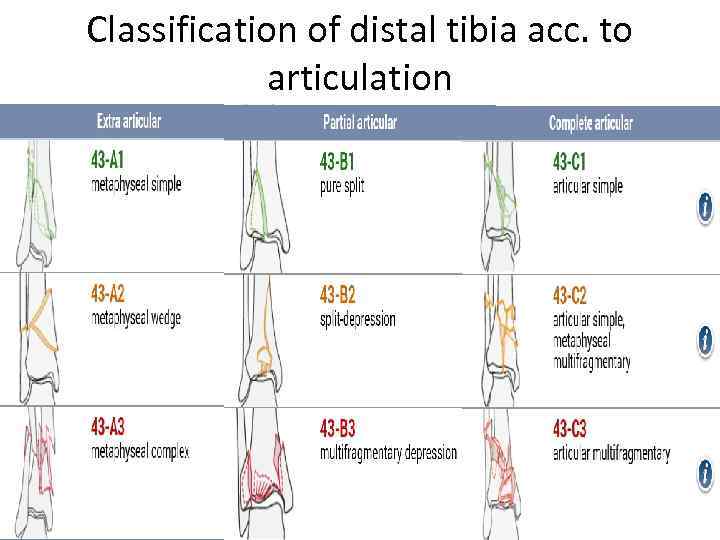 Classification of distal tibia acc. to articulation
Classification of distal tibia acc. to articulation
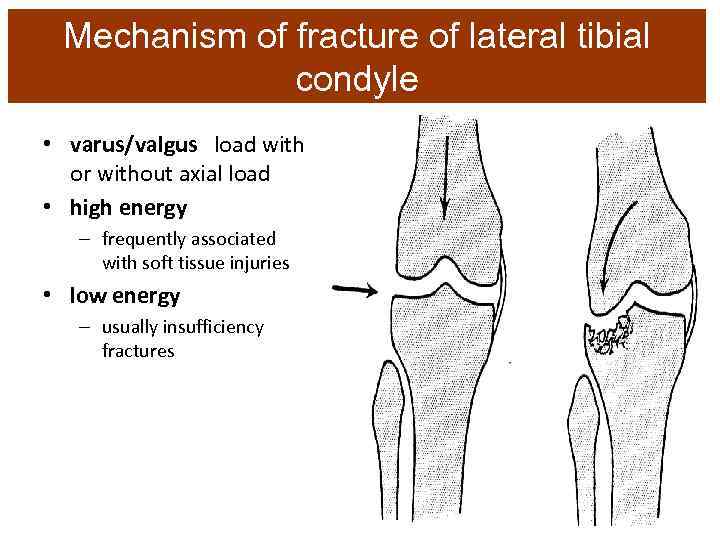 Mechanism of fracture of lateral tibial condyle • varus/valgus load with or without axial load • high energy – frequently associated with soft tissue injuries • low energy – usually insufficiency fractures
Mechanism of fracture of lateral tibial condyle • varus/valgus load with or without axial load • high energy – frequently associated with soft tissue injuries • low energy – usually insufficiency fractures
 First Aid • • Analgesics – Analgin (IM) Immobilization by kremer’s splint From gluteal fold to foot Transport to hospital
First Aid • • Analgesics – Analgin (IM) Immobilization by kremer’s splint From gluteal fold to foot Transport to hospital
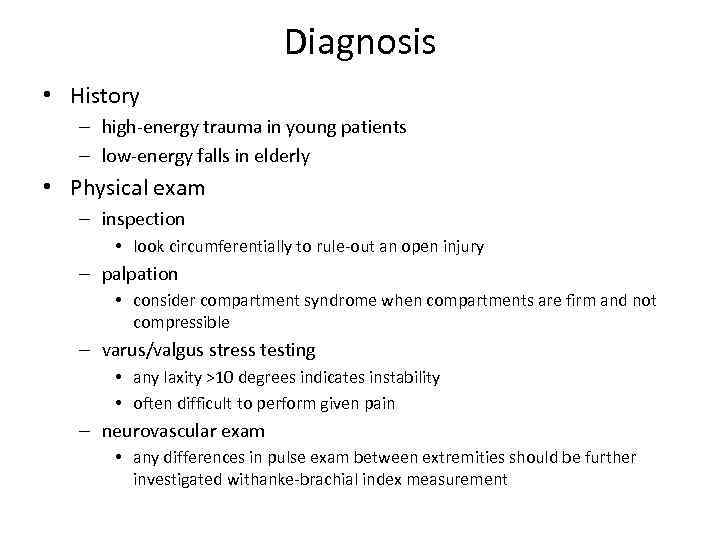 Diagnosis • History – high-energy trauma in young patients – low-energy falls in elderly • Physical exam – inspection • look circumferentially to rule-out an open injury – palpation • consider compartment syndrome when compartments are firm and not compressible – varus/valgus stress testing • any laxity >10 degrees indicates instability • often difficult to perform given pain – neurovascular exam • any differences in pulse exam between extremities should be further investigated withanke-brachial index measurement
Diagnosis • History – high-energy trauma in young patients – low-energy falls in elderly • Physical exam – inspection • look circumferentially to rule-out an open injury – palpation • consider compartment syndrome when compartments are firm and not compressible – varus/valgus stress testing • any laxity >10 degrees indicates instability • often difficult to perform given pain – neurovascular exam • any differences in pulse exam between extremities should be further investigated withanke-brachial index measurement
 В. 3. 3.
В. 3. 3.
 С. 3. 3.
С. 3. 3.


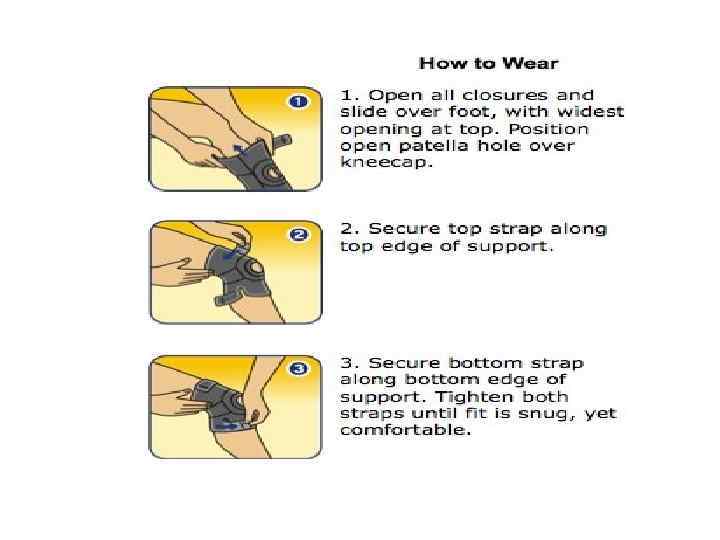
 Treatment of proximal part • Nonoperative – hinged knee brace, PWB for 812 weeks, and immediate passive ROM • indications – minimally displaced split or depressed fractures – low energy fracture stable to varus/valgus alignment – nonambulatory patients
Treatment of proximal part • Nonoperative – hinged knee brace, PWB for 812 weeks, and immediate passive ROM • indications – minimally displaced split or depressed fractures – low energy fracture stable to varus/valgus alignment – nonambulatory patients
 Operative §temporizing bridging external fixation w/ delayed ORIF • indications significant soft tissue injury polytrauma §external fixation with limited open/percutaneous fixation of articular segment • indications severe open fracture with marked contamination highly comminuted fractures where internal fixation not possible • outcomes similar to open reduction, internal fixation §open reduction, internal fixation • indications articular stepoff > 3 mm condylar widening > 5 mm varus/valgus instability all medial plateau fxs all bicondylar fxs • outcomes restoration of joint stability is strongest predictor of long term outcomes worse results with ligamentous instability meniscectomy alteration of limb mechanical axis > 5 degrees
Operative §temporizing bridging external fixation w/ delayed ORIF • indications significant soft tissue injury polytrauma §external fixation with limited open/percutaneous fixation of articular segment • indications severe open fracture with marked contamination highly comminuted fractures where internal fixation not possible • outcomes similar to open reduction, internal fixation §open reduction, internal fixation • indications articular stepoff > 3 mm condylar widening > 5 mm varus/valgus instability all medial plateau fxs all bicondylar fxs • outcomes restoration of joint stability is strongest predictor of long term outcomes worse results with ligamentous instability meniscectomy alteration of limb mechanical axis > 5 degrees
 External fixation (temporary) – technique • two 5 -mm half-pins in distal femur, two in distal tibia • axial traction applied to fixator • fixator is locked in slight flexion – advantages • allows soft tissue swelling to decrease before definitive fixation • decreases rate of infection and wound healing complications
External fixation (temporary) – technique • two 5 -mm half-pins in distal femur, two in distal tibia • axial traction applied to fixator • fixator is locked in slight flexion – advantages • allows soft tissue swelling to decrease before definitive fixation • decreases rate of infection and wound healing complications
 External Fixation
External Fixation
 External fixation with limited internal fixation (definitive) – technique • reduce articular surface either percutaneously or with small incisions • stabilize reduction with lag screws or wires – must keep wires >14 mm from joint • apply external fixator or hybrid ring fixation – post-operative care • begin weight bearing when callus is visible on radiographs • usually remain in place 2 -4 months – pros • minimizes soft tissue insult • permits knee ROM – cons • pin site complications
External fixation with limited internal fixation (definitive) – technique • reduce articular surface either percutaneously or with small incisions • stabilize reduction with lag screws or wires – must keep wires >14 mm from joint • apply external fixator or hybrid ring fixation – post-operative care • begin weight bearing when callus is visible on radiographs • usually remain in place 2 -4 months – pros • minimizes soft tissue insult • permits knee ROM – cons • pin site complications
 Open reduction, internal fixation – approach • lateral incision (most common) – straight or hockey stick incision anterolaterally from just proximal to joint line to just lateral to the tibial tubercle • midline incision (if planning TKA in future) – can lead to significant soft tissue stripping and should be avoided • posteromedial incision – interval between semimembranosus and medial head of gastrocnemius • dual surgical incisions with dual plate fixation – indications » bicondylar tibial plateau fractures • posterior – can be used for posterior shearing fractures –
Open reduction, internal fixation – approach • lateral incision (most common) – straight or hockey stick incision anterolaterally from just proximal to joint line to just lateral to the tibial tubercle • midline incision (if planning TKA in future) – can lead to significant soft tissue stripping and should be avoided • posteromedial incision – interval between semimembranosus and medial head of gastrocnemius • dual surgical incisions with dual plate fixation – indications » bicondylar tibial plateau fractures • posterior – can be used for posterior shearing fractures –
 • reduction – restore joint surface with direct or indirect reduction – fill metaphyseal void with autogenous, allogenic bone graft, or bone graft substitutes • calcium phosphate cement has high compressive strength for filling metaphyseal void
• reduction – restore joint surface with direct or indirect reduction – fill metaphyseal void with autogenous, allogenic bone graft, or bone graft substitutes • calcium phosphate cement has high compressive strength for filling metaphyseal void
 • internal fixation – absolute stability constructs should be used to maintain the joint reduction – screws • may be used alone for – simple split fractures – depression fractures that were elevated percutaneously – plate fixation • non-locked plates – non-locked buttress plates best indicated for simple partial articular fractures in healthy bone • locked plates – advantages » fixed-angle construct » less compression of periosteum and soft tissue
• internal fixation – absolute stability constructs should be used to maintain the joint reduction – screws • may be used alone for – simple split fractures – depression fractures that were elevated percutaneously – plate fixation • non-locked plates – non-locked buttress plates best indicated for simple partial articular fractures in healthy bone • locked plates – advantages » fixed-angle construct » less compression of periosteum and soft tissue
 • postoperative – hinged knee brace with early passive ROM • gentle mechanical compression on repaired osteoarticular segments improves chondrocyte survival – NWB or PWB for 8 to 12 weeks
• postoperative – hinged knee brace with early passive ROM • gentle mechanical compression on repaired osteoarticular segments improves chondrocyte survival – NWB or PWB for 8 to 12 weeks
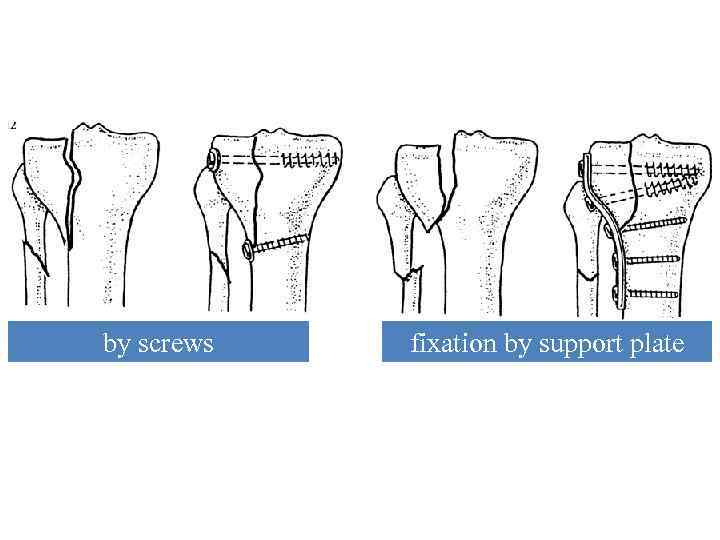 Variants of osteosynthesis at fractures of proximal part of bones‘ leg by screws fixation by support plate
Variants of osteosynthesis at fractures of proximal part of bones‘ leg by screws fixation by support plate
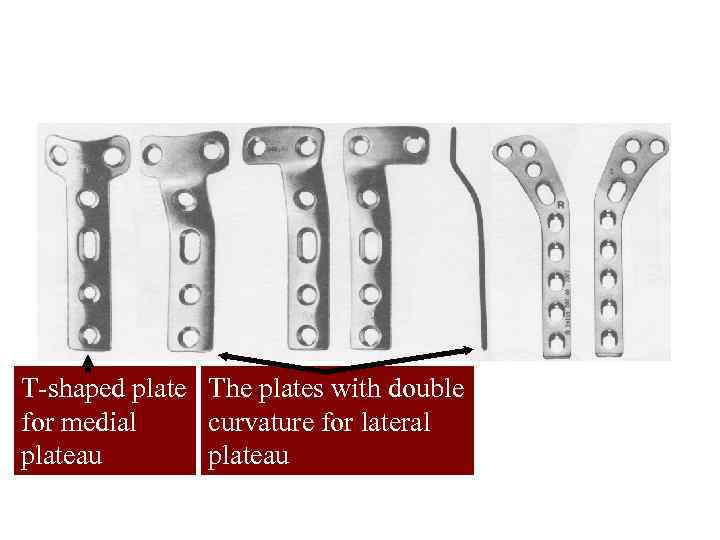 The types of supporting plates for fractures of a tibial plateau Т-shaped plate The plates with double for medial curvature for lateral plateau
The types of supporting plates for fractures of a tibial plateau Т-shaped plate The plates with double for medial curvature for lateral plateau
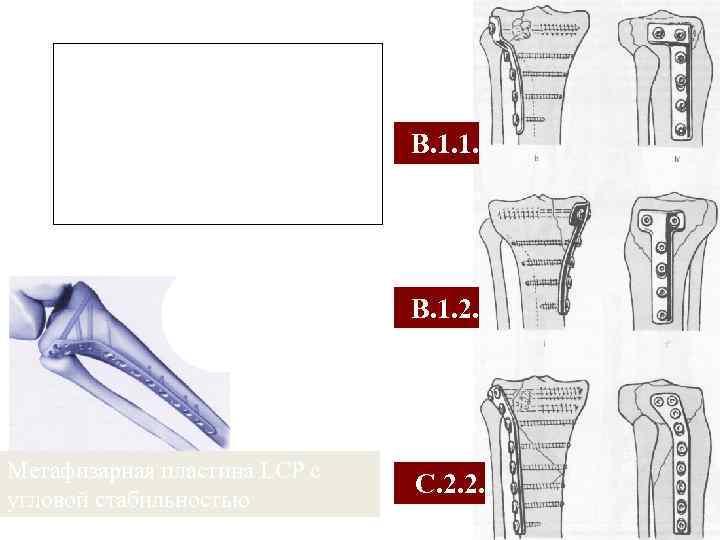 Different types of support plates for fractures of the tibial plateau В. 1. 1. В. 1. 2. Метафизарная пластина LCP с угловой стабильностью С. 2. 2.
Different types of support plates for fractures of the tibial plateau В. 1. 1. В. 1. 2. Метафизарная пластина LCP с угловой стабильностью С. 2. 2.
 LCP PTP 3, 5 мм
LCP PTP 3, 5 мм
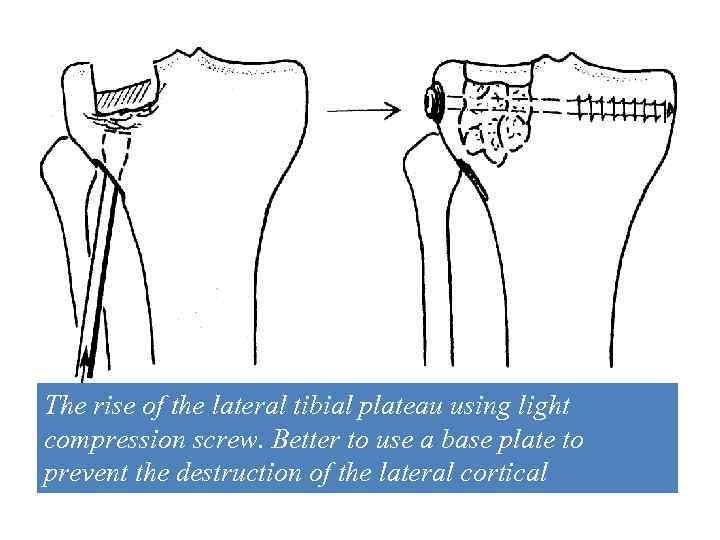 В. 2. 2. The rise of the lateral tibial plateau using light compression screw. Better to use a base plate to prevent the destruction of the lateral cortical
В. 2. 2. The rise of the lateral tibial plateau using light compression screw. Better to use a base plate to prevent the destruction of the lateral cortical
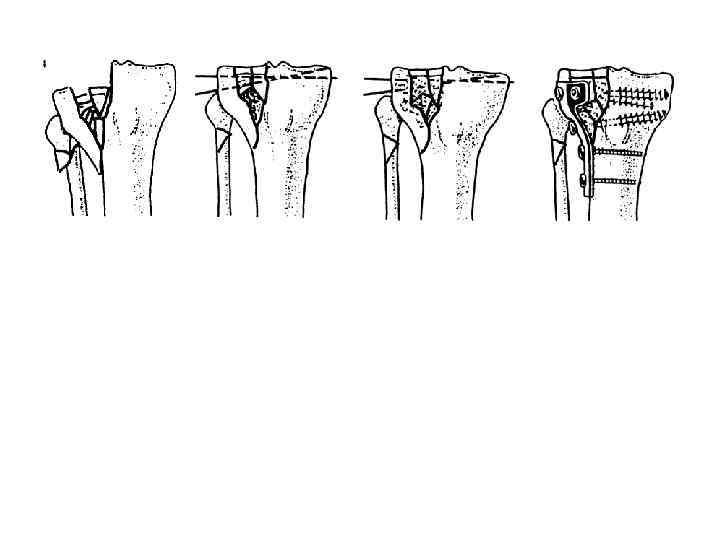 В. 3. 1. Reduction and temporary fixation Kirschner wires. Transplantation of cancellous bone. Fixing the base plate
В. 3. 1. Reduction and temporary fixation Kirschner wires. Transplantation of cancellous bone. Fixing the base plate
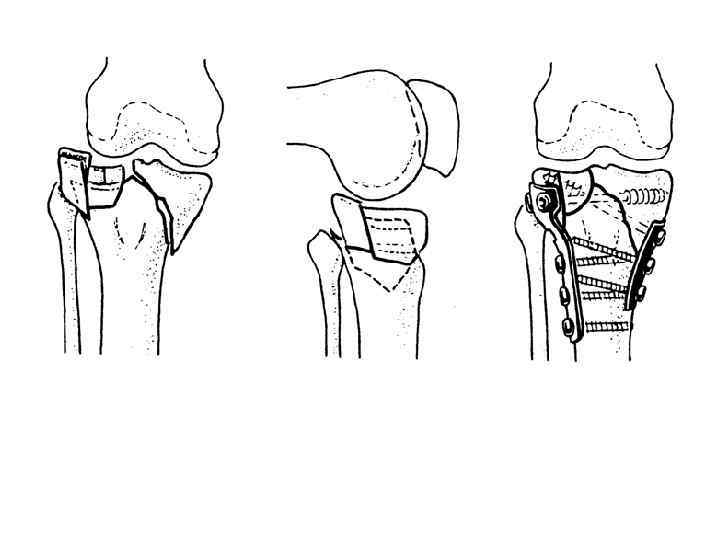 С. 3. 3. Fixing the two support plates
С. 3. 3. Fixing the two support plates
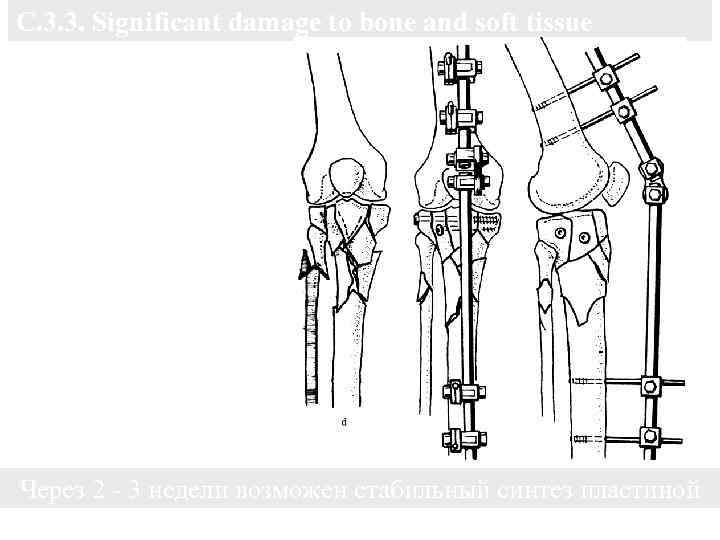 С. 3. 3. Significant damage to bone and soft tissue Reposition the result ligaments when distraction external fixation device. Fixing two cancellous screws Через 2 - 3 недели возможен стабильный синтез пластиной
С. 3. 3. Significant damage to bone and soft tissue Reposition the result ligaments when distraction external fixation device. Fixing two cancellous screws Через 2 - 3 недели возможен стабильный синтез пластиной
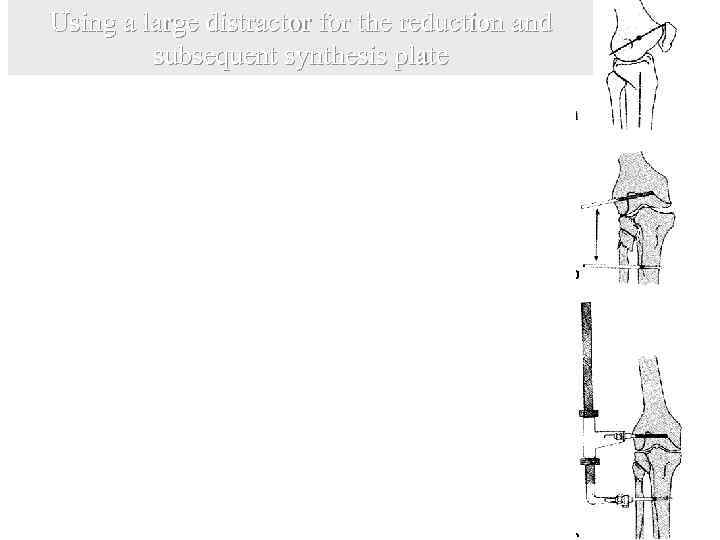 Using a large distractor for the reduction and subsequent synthesis plate The proximal screw inserted slightly anterior to the exposed point of the lateral condyle. The distal screws are inserted below the fracture so that it does not interfere with the installation plate. Intraarticular fragments raised and repositioned using special tools
Using a large distractor for the reduction and subsequent synthesis plate The proximal screw inserted slightly anterior to the exposed point of the lateral condyle. The distal screws are inserted below the fracture so that it does not interfere with the installation plate. Intraarticular fragments raised and repositioned using special tools
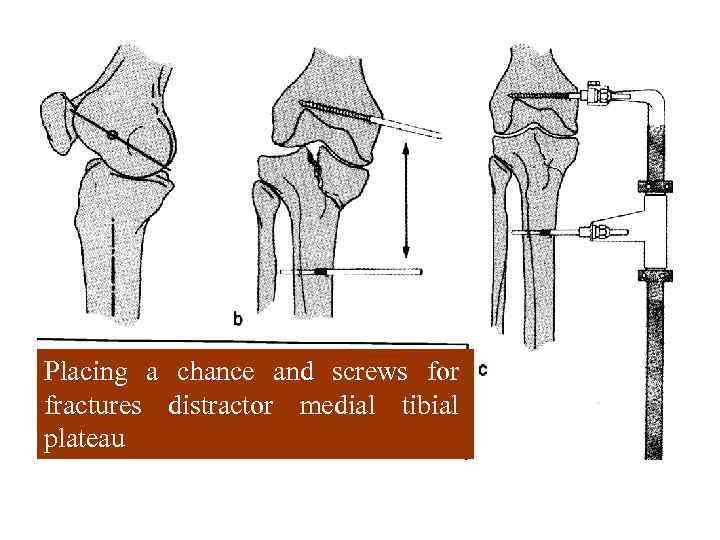 Placing a chance and screws for fractures distractor medial tibial plateau
Placing a chance and screws for fractures distractor medial tibial plateau
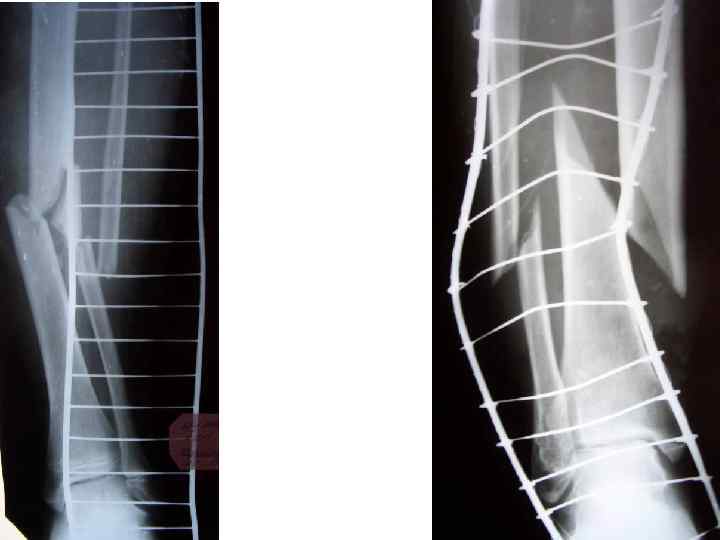
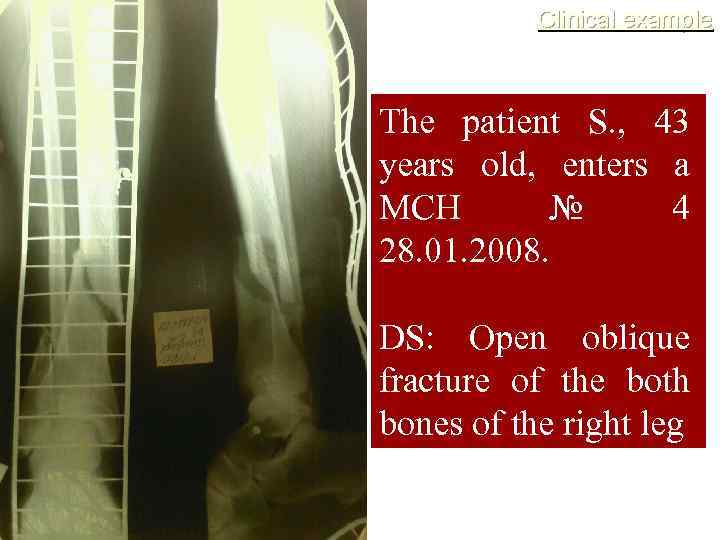 Clinical example The patient S. , 43 years old, enters a MCH № 4 28. 01. 2008. DS: Open oblique fracture of the both bones of the right leg
Clinical example The patient S. , 43 years old, enters a MCH № 4 28. 01. 2008. DS: Open oblique fracture of the both bones of the right leg
 28. 01. 2008 urgently operation is performed: PECVD wounds, reposition, MOS locking pin, flow-flushing drainage.
28. 01. 2008 urgently operation is performed: PECVD wounds, reposition, MOS locking pin, flow-flushing drainage.
 Treatment of shaft of tibia • Nonoperative o closed reduction / cast immobilization • indications – closed low energy fxs with acceptable alignment » < 5 degrees varus-valgus angulation » < 10 degrees anterior/posterior angulation » > 50% cortical apposition » < 1 cm shortening » < 10 degrees rotational alignment » if displaced perform closed reduction under general anesthesia • technique – place in long leg cast and convert to functional brace at 4 weeks • outcomes – high success rate if acceptable alignment maintained – risk of shortening with oblique fracture patterns – risk of varus malunion with midshaft tibia fractures and an intact fibula
Treatment of shaft of tibia • Nonoperative o closed reduction / cast immobilization • indications – closed low energy fxs with acceptable alignment » < 5 degrees varus-valgus angulation » < 10 degrees anterior/posterior angulation » > 50% cortical apposition » < 1 cm shortening » < 10 degrees rotational alignment » if displaced perform closed reduction under general anesthesia • technique – place in long leg cast and convert to functional brace at 4 weeks • outcomes – high success rate if acceptable alignment maintained – risk of shortening with oblique fracture patterns – risk of varus malunion with midshaft tibia fractures and an intact fibula
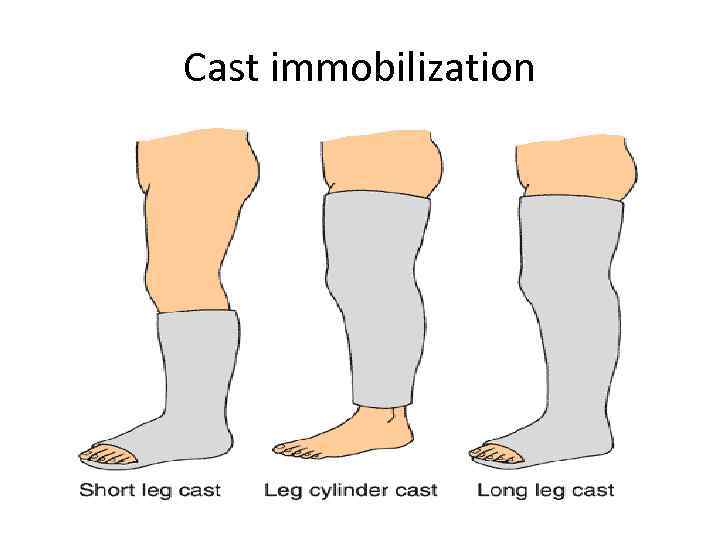 Cast immobilization
Cast immobilization
 • Operative o external fixation – indications • can be useful for proximal or distal metaphyseal fxs – complications • pin tract infections common – outcomes • higher incidence of malalignment compared to IM nailing
• Operative o external fixation – indications • can be useful for proximal or distal metaphyseal fxs – complications • pin tract infections common – outcomes • higher incidence of malalignment compared to IM nailing
 • IM Nailing – indications • • unacceptable alignment with casting soft tissue injury that will not tolerate casting segmental fx ipsilateral limb injury polytrauma bilateral tibia fx morbid obesity
• IM Nailing – indications • • unacceptable alignment with casting soft tissue injury that will not tolerate casting segmental fx ipsilateral limb injury polytrauma bilateral tibia fx morbid obesity
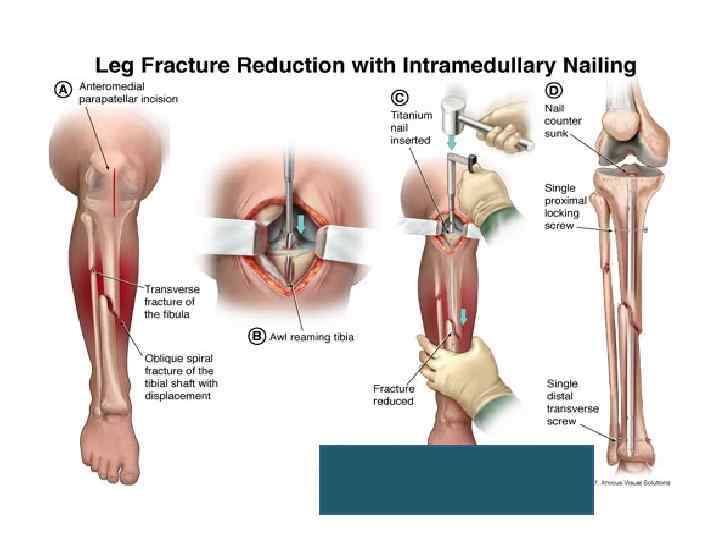
 – outcomes • IM nailing leads to (versus external fixation) – decreased malalignment • IM nailing leads to (versus closed treatment) – decrease time to union – decreased time to weight bearing • reamed vs. unreamed nails – reamed possibly superior to unreamed nails for treatment of closed tibia fxs for decrease in future bone grafting or implant exchange (SPRINT trial) – recent studies show no adverse effects of reaming (infection, nonunion) – reaming with use of a tourniquet is not associated with thermal necrosis of the tibial shaft – reamed nails associated with » decreased hardware failure » superior union rate » decrease time to union
– outcomes • IM nailing leads to (versus external fixation) – decreased malalignment • IM nailing leads to (versus closed treatment) – decrease time to union – decreased time to weight bearing • reamed vs. unreamed nails – reamed possibly superior to unreamed nails for treatment of closed tibia fxs for decrease in future bone grafting or implant exchange (SPRINT trial) – recent studies show no adverse effects of reaming (infection, nonunion) – reaming with use of a tourniquet is not associated with thermal necrosis of the tibial shaft – reamed nails associated with » decreased hardware failure » superior union rate » decrease time to union
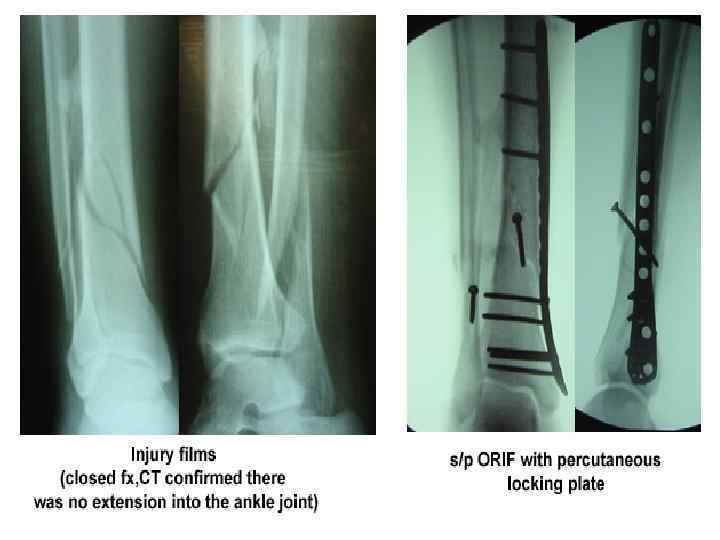
 • percutaneous locking plate – indications • proximal tibia fractures with inadequate proximal fixation from IM nailing • distal tibia fractures with inadequate distal fixation from IM nail – complications • long plates may place superficial peroneal nerve at risk
• percutaneous locking plate – indications • proximal tibia fractures with inadequate proximal fixation from IM nailing • distal tibia fractures with inadequate distal fixation from IM nail – complications • long plates may place superficial peroneal nerve at risk
 Treatment of open tibia fracture • Operative o antibiotics, I&D – indications • all open fractures require an emergent I&D – timing of I&D • surgical debridement 6 -8 hours after time of injury is preferred • grossly contaminated wounds are irrigated in emergency department – antibiotics • standard abx for open fractures (institution dependent) – cephalosporin given for 24 -48 hours in Grade I, II, and IIIA open fractures – aminoglycoside added in Grade IIIB injuries » minimal data to support this – penicillin administered in farm injuries » minimal data to support this • tetanus prophylaxis
Treatment of open tibia fracture • Operative o antibiotics, I&D – indications • all open fractures require an emergent I&D – timing of I&D • surgical debridement 6 -8 hours after time of injury is preferred • grossly contaminated wounds are irrigated in emergency department – antibiotics • standard abx for open fractures (institution dependent) – cephalosporin given for 24 -48 hours in Grade I, II, and IIIA open fractures – aminoglycoside added in Grade IIIB injuries » minimal data to support this – penicillin administered in farm injuries » minimal data to support this • tetanus prophylaxis
 • external fixation – indications • provisional external fixation an option for open fractures with staged IM nailing or plating • falling out of favor in last decade • indicated in children with open physis
• external fixation – indications • provisional external fixation an option for open fractures with staged IM nailing or plating • falling out of favor in last decade • indicated in children with open physis
 • IM Nailing – indications • most open fx can be treated with IM nail within 24 hours • contraindicated in children with open physis (use flexible nail, plate, or external fixation instead) – outcomes for open fxs • IM nailing vs. external fixation – no difference with respect to » infection rate » union rate » time to union – IM nailing superior with respect to » decreased malalignment » decreased secondary surgeries » shorter time to weight bearing • reamed nails vs. unreamed nails – reaming does not negatively affect union, infection, or need for additional surgeries in open tibia fractures – gapping at the fracture site is greatest risk for non-union
• IM Nailing – indications • most open fx can be treated with IM nail within 24 hours • contraindicated in children with open physis (use flexible nail, plate, or external fixation instead) – outcomes for open fxs • IM nailing vs. external fixation – no difference with respect to » infection rate » union rate » time to union – IM nailing superior with respect to » decreased malalignment » decreased secondary surgeries » shorter time to weight bearing • reamed nails vs. unreamed nails – reaming does not negatively affect union, infection, or need for additional surgeries in open tibia fractures – gapping at the fracture site is greatest risk for non-union
 • Amputation o indications – no current scoring system to determine if an amputation should be performed – relative indications for amputation include • significant soft tissue trauma • warm ischemia > 6 hrs • severe ipsilateral foot trauma • outcomes – LEAP study • most important predictor of eventual amputation is the severity of ipsilateral extremity soft tissue injury • most important predictor of infection other than early antibiotic administration is transfer to definitive trauma center • study shows no significant difference in functional outcomes between amputation and salvage • loss of plantar sensation is not an absolute indication for amputation
• Amputation o indications – no current scoring system to determine if an amputation should be performed – relative indications for amputation include • significant soft tissue trauma • warm ischemia > 6 hrs • severe ipsilateral foot trauma • outcomes – LEAP study • most important predictor of eventual amputation is the severity of ipsilateral extremity soft tissue injury • most important predictor of infection other than early antibiotic administration is transfer to definitive trauma center • study shows no significant difference in functional outcomes between amputation and salvage • loss of plantar sensation is not an absolute indication for amputation
 Treatment of distal tibia • Nonoperative – immobilization • indications – stable fracture patterns without articular surface displacement – critically ill or nonambulatory patients – significant risk of skin problems (diabetes, vascular disease, neuropathy) • technique – long leg cast for 6 weeks followed by fracture brace and ROM exercises – alternative treatment is with early ROM • outcomes – intra-articular fragments are unlikely to reduce with manipulation of displaced fractures – loss of reduction is common – inability to monitor soft tissue injuries is a major disadvantage
Treatment of distal tibia • Nonoperative – immobilization • indications – stable fracture patterns without articular surface displacement – critically ill or nonambulatory patients – significant risk of skin problems (diabetes, vascular disease, neuropathy) • technique – long leg cast for 6 weeks followed by fracture brace and ROM exercises – alternative treatment is with early ROM • outcomes – intra-articular fragments are unlikely to reduce with manipulation of displaced fractures – loss of reduction is common – inability to monitor soft tissue injuries is a major disadvantage
 • Operative o temporizing spanning external fixation across ankle joint – indications • acute management – provides stabilization to allow for soft tissue healing • fractures with significant joint depression or displacement • leave until swelling resolves (generally 10 -14 days)
• Operative o temporizing spanning external fixation across ankle joint – indications • acute management – provides stabilization to allow for soft tissue healing • fractures with significant joint depression or displacement • leave until swelling resolves (generally 10 -14 days)
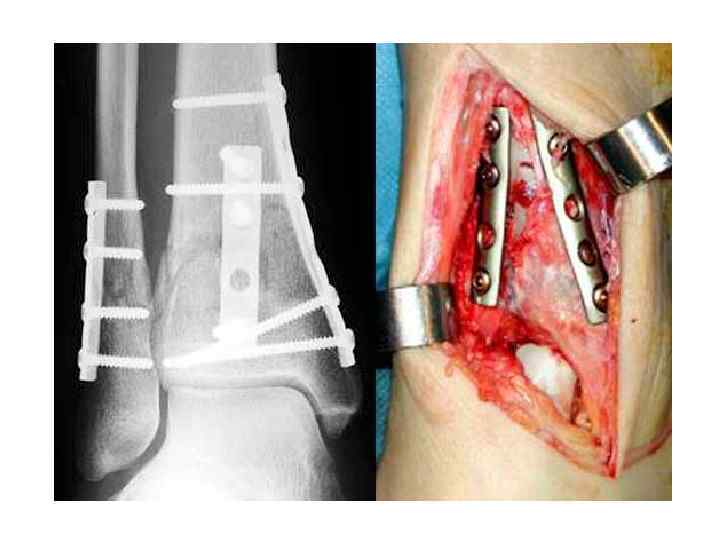
 • ORIF indications – definitive fixation for majority of pilon fractures – limited or definitive ORIF can be performed acutely with low complications in certain situations • outcomes – ability to drive • brake travel time returns to normal 6 weeks after weight bearing
• ORIF indications – definitive fixation for majority of pilon fractures – limited or definitive ORIF can be performed acutely with low complications in certain situations • outcomes – ability to drive • brake travel time returns to normal 6 weeks after weight bearing
 • external fixation alone – indications • may be indicated in select cases
• external fixation alone – indications • may be indicated in select cases
 References • https: //www 2. aofoundation. org/wps/portal/surgery? show. Page=diagnosis &bone=Tibia&segment=Proximal • http: //www. orthobullets. com/trauma/1044/tibial-plateau-fractures • https: //www 2. aofoundation. org/wps/portal/surgery? show. Page=diagnosis &bone=Tibia&segment=Shaft • http: //www. orthobullets. com/trauma/1045/tibia-shaft-fractures • https: //www 2. aofoundation. org/wps/portal/surgery? show. Page=diagnosis &bone=Tibia&segment=Distal • http: //www. orthobullets. com/trauma/1046/tibial-plafond-fractures
References • https: //www 2. aofoundation. org/wps/portal/surgery? show. Page=diagnosis &bone=Tibia&segment=Proximal • http: //www. orthobullets. com/trauma/1044/tibial-plateau-fractures • https: //www 2. aofoundation. org/wps/portal/surgery? show. Page=diagnosis &bone=Tibia&segment=Shaft • http: //www. orthobullets. com/trauma/1045/tibia-shaft-fractures • https: //www 2. aofoundation. org/wps/portal/surgery? show. Page=diagnosis &bone=Tibia&segment=Distal • http: //www. orthobullets. com/trauma/1046/tibial-plafond-fractures
 KURSK STATE MEDICAL UNIVERSITY DEPARTMENT OF TRAUMATOLOGY AND ORTHOPAEDICS SURGERY Injuries to Ankle
KURSK STATE MEDICAL UNIVERSITY DEPARTMENT OF TRAUMATOLOGY AND ORTHOPAEDICS SURGERY Injuries to Ankle
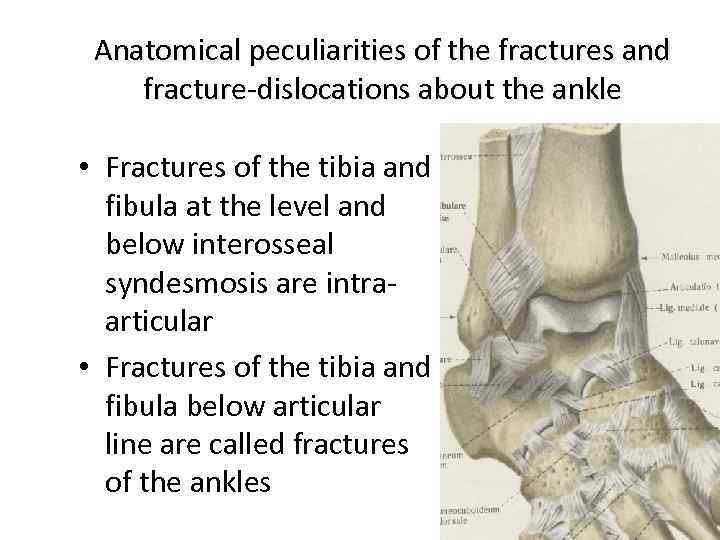 Anatomical peculiarities of the fractures and fracture-dislocations about the ankle • Fractures of the tibia and fibula at the level and below interosseal syndesmosis are intraarticular • Fractures of the tibia and fibula below articular line are called fractures of the ankles
Anatomical peculiarities of the fractures and fracture-dislocations about the ankle • Fractures of the tibia and fibula at the level and below interosseal syndesmosis are intraarticular • Fractures of the tibia and fibula below articular line are called fractures of the ankles
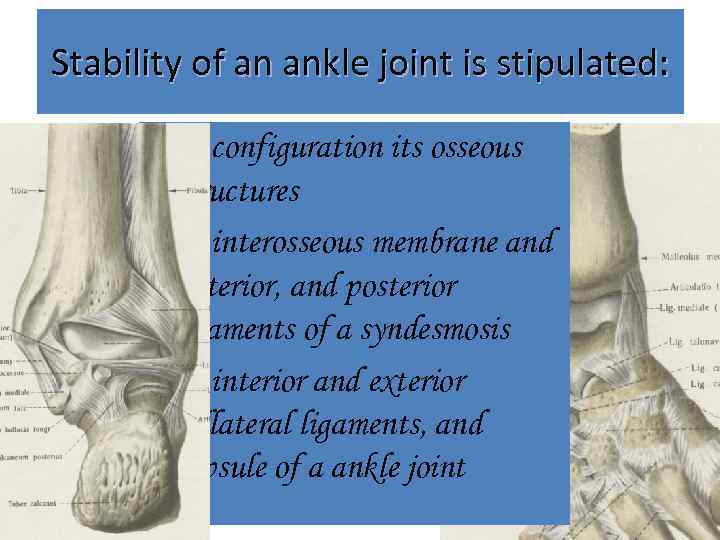 Stability of an ankle joint is stipulated: membrana • by configuration its osseous interossea cruris structures lig. tibiofibulare anterius & posterius • by interosseous membrane and lig. deltoideum: anterior, andanterior, tibiotalaris posterior tibionavicularis, ligaments of a syndesmosis tibiocalcanea, tibiotalaris posterior • by interior and exterior lig. talofibulare collateral ligaments, and anterius & posterius lig. calcaneofibulare capsule of a ankle joint
Stability of an ankle joint is stipulated: membrana • by configuration its osseous interossea cruris structures lig. tibiofibulare anterius & posterius • by interosseous membrane and lig. deltoideum: anterior, andanterior, tibiotalaris posterior tibionavicularis, ligaments of a syndesmosis tibiocalcanea, tibiotalaris posterior • by interior and exterior lig. talofibulare collateral ligaments, and anterius & posterius lig. calcaneofibulare capsule of a ankle joint
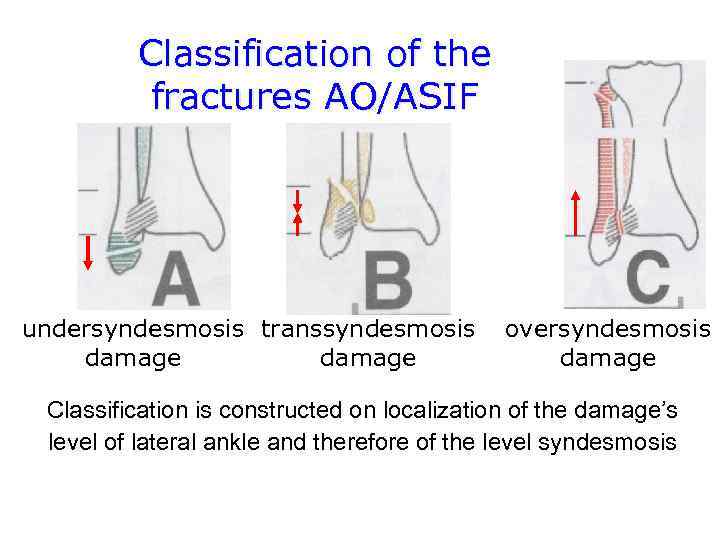 Classification of the fractures AO/ASIF undersyndesmosis transsyndesmosis damage oversyndesmosis damage Classification is constructed on localization of the damage’s level of lateral ankle and therefore of the level syndesmosis
Classification of the fractures AO/ASIF undersyndesmosis transsyndesmosis damage oversyndesmosis damage Classification is constructed on localization of the damage’s level of lateral ankle and therefore of the level syndesmosis
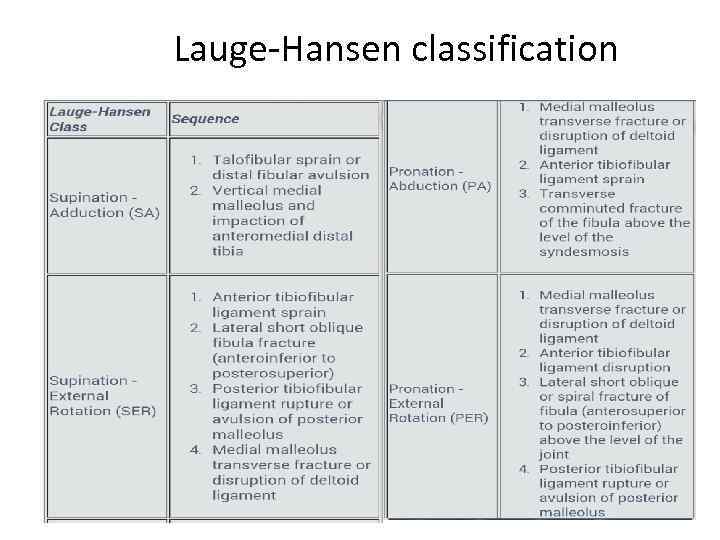 Lauge-Hansen classification
Lauge-Hansen classification
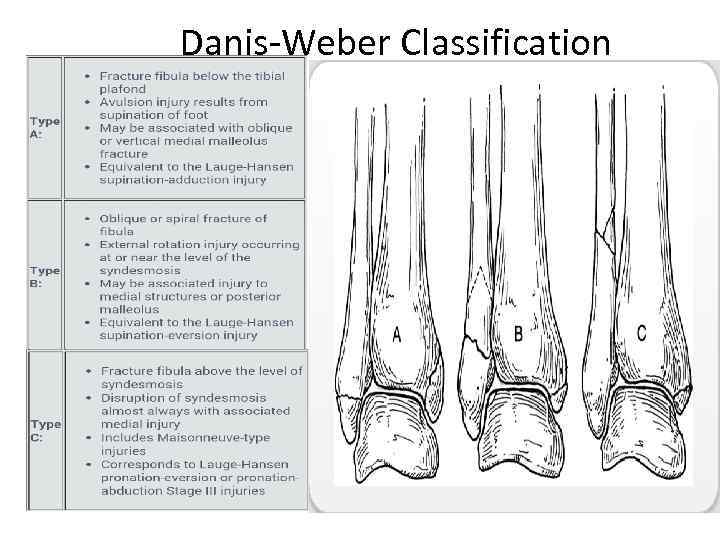 Danis-Weber Classification
Danis-Weber Classification
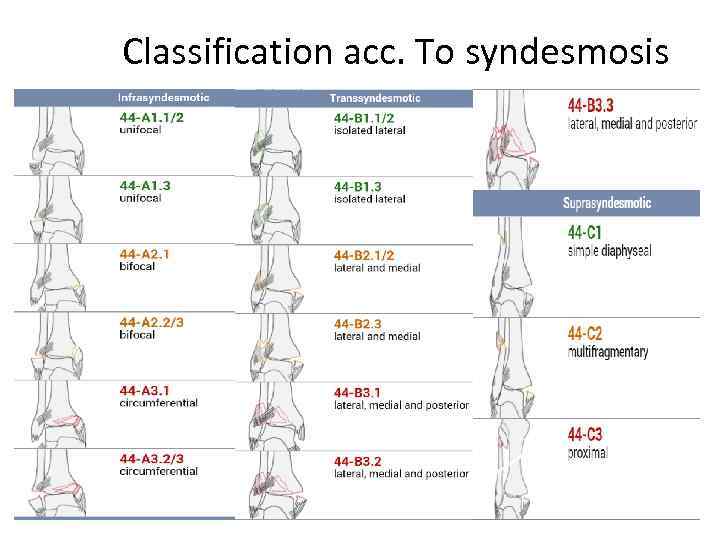 Classification acc. To syndesmosis
Classification acc. To syndesmosis
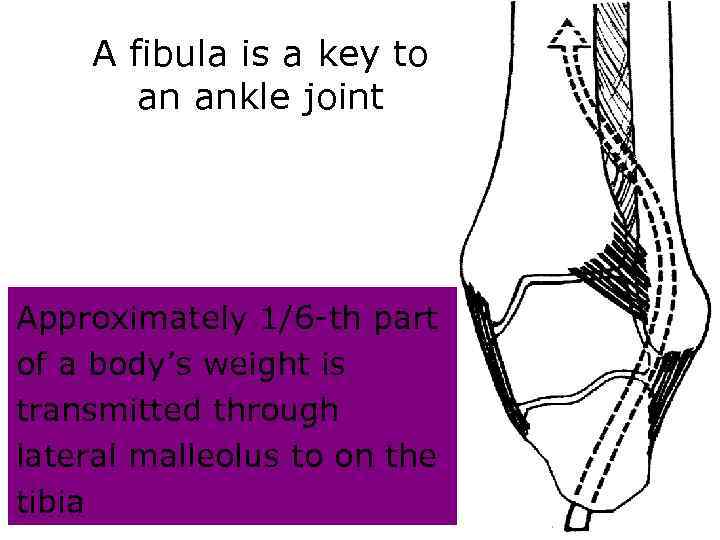 A fibula is a key to an ankle joint Approximately 1/6 -th part of a body’s weight is transmitted through lateral malleolus to on the tibia
A fibula is a key to an ankle joint Approximately 1/6 -th part of a body’s weight is transmitted through lateral malleolus to on the tibia
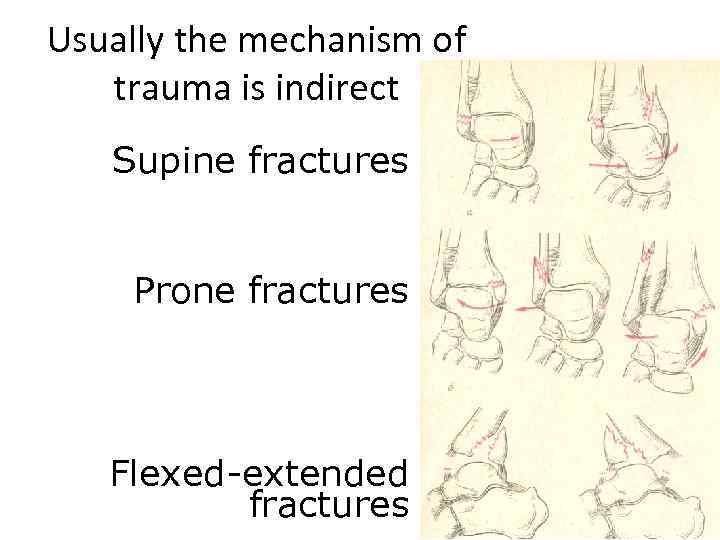 Usually the mechanism of trauma is indirect Supine fractures Prone fractures Flexed-extended fractures
Usually the mechanism of trauma is indirect Supine fractures Prone fractures Flexed-extended fractures
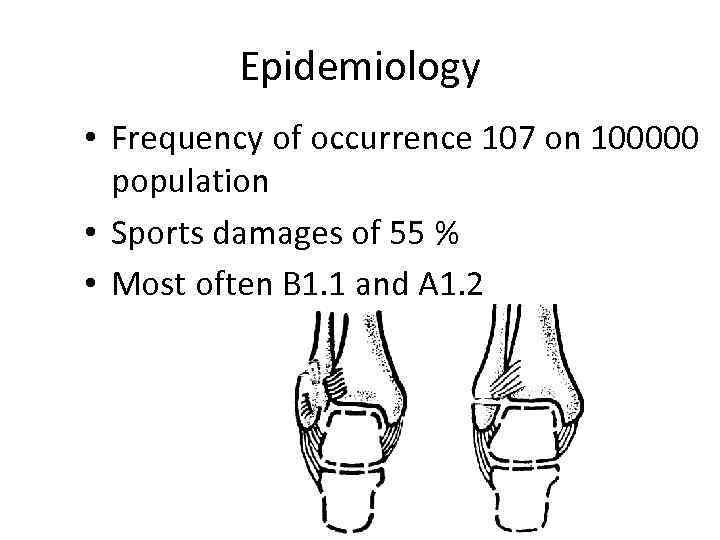 Epidemiology • Frequency of occurrence 107 on 100000 population • Sports damages of 55 % • Most often B 1. 1 and A 1. 2
Epidemiology • Frequency of occurrence 107 on 100000 population • Sports damages of 55 % • Most often B 1. 1 and A 1. 2
 Basic symptoms of the fractures of the ankles • The general symptoms of damage: a pain, a swelling, a bruise, increase of local temperature, lesion of function. • Authentic symptoms of fractures: pathological mobility of fragments, crepitus, deformation. Possible appearance of bone’s fragments in a wound for open penetrating fractures
Basic symptoms of the fractures of the ankles • The general symptoms of damage: a pain, a swelling, a bruise, increase of local temperature, lesion of function. • Authentic symptoms of fractures: pathological mobility of fragments, crepitus, deformation. Possible appearance of bone’s fragments in a wound for open penetrating fractures
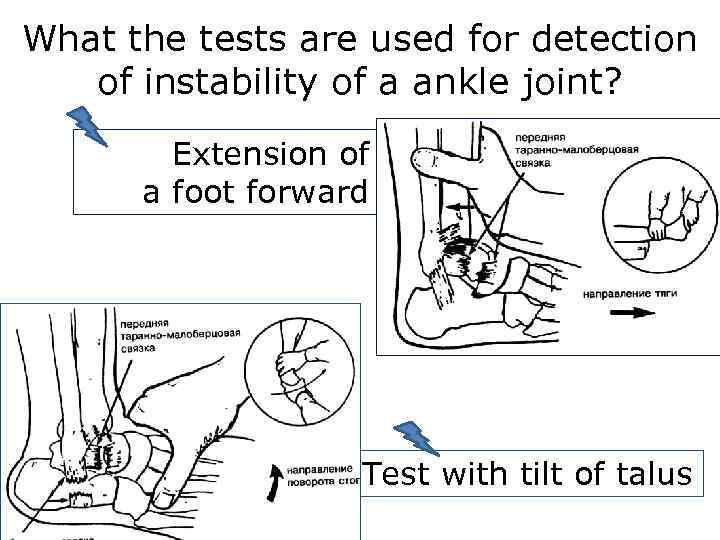 What the tests are used for detection of instability of a ankle joint? Extension of a foot forward Test with tilt of talus
What the tests are used for detection of instability of a ankle joint? Extension of a foot forward Test with tilt of talus
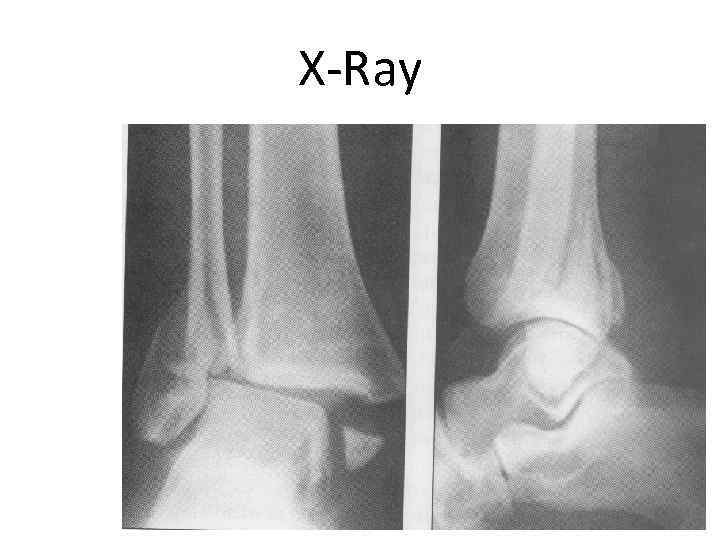 X-Ray
X-Ray
 Xray result • Fracture of lateral and medial malleolus Posterior and lateral subluxation of talus Rupture of tibia and fibula syndesmosis
Xray result • Fracture of lateral and medial malleolus Posterior and lateral subluxation of talus Rupture of tibia and fibula syndesmosis
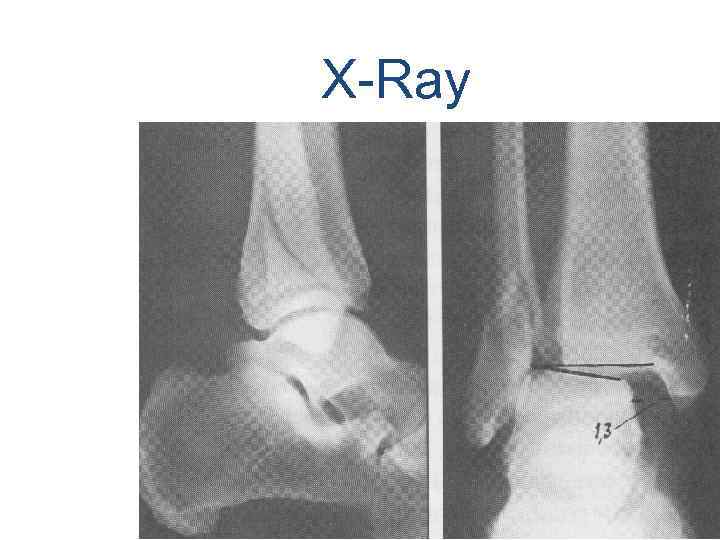 X-Ray
X-Ray
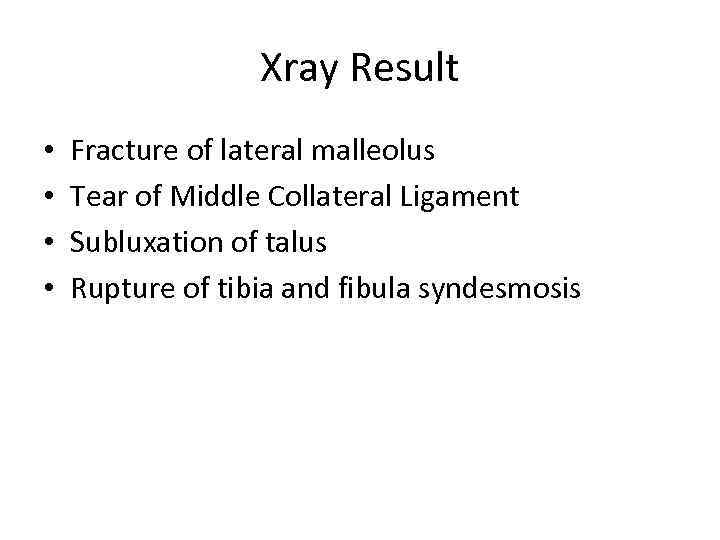 Xray Result • • Fracture of lateral malleolus Tear of Middle Collateral Ligament Subluxation of talus Rupture of tibia and fibula syndesmosis
Xray Result • • Fracture of lateral malleolus Tear of Middle Collateral Ligament Subluxation of talus Rupture of tibia and fibula syndesmosis
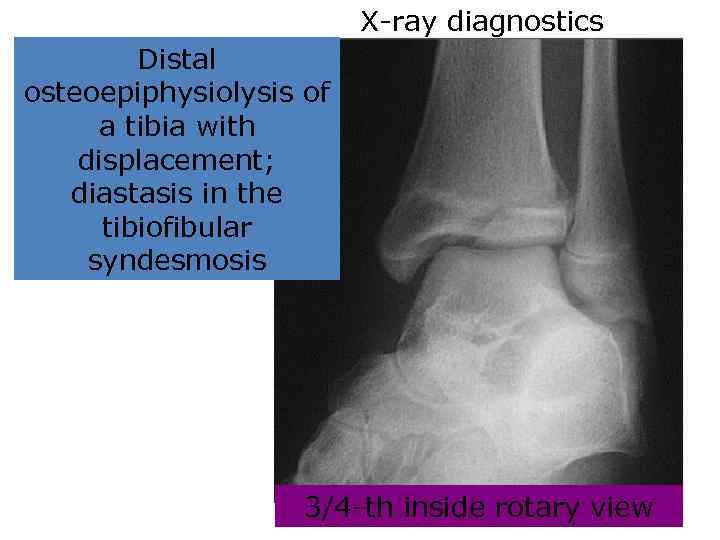 X-ray diagnostics Distal osteoepiphysiolysis of a tibia with displacement; diastasis in the tibiofibular syndesmosis 3/4 -th inside rotary view
X-ray diagnostics Distal osteoepiphysiolysis of a tibia with displacement; diastasis in the tibiofibular syndesmosis 3/4 -th inside rotary view
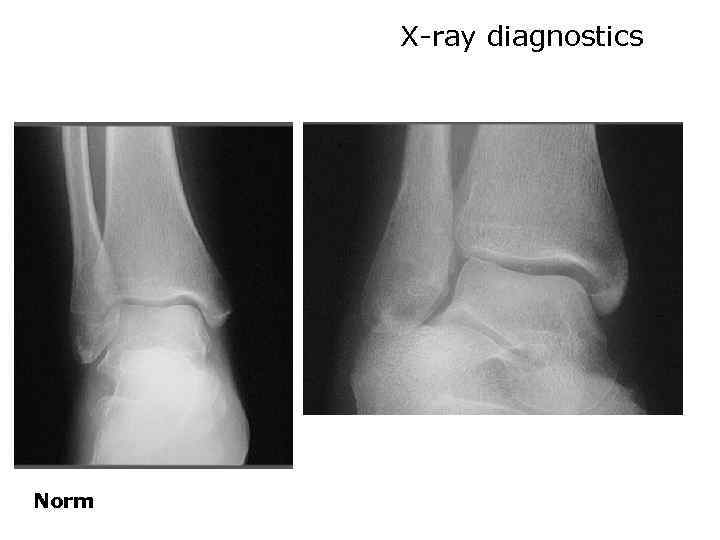 X-ray diagnostics Norm
X-ray diagnostics Norm
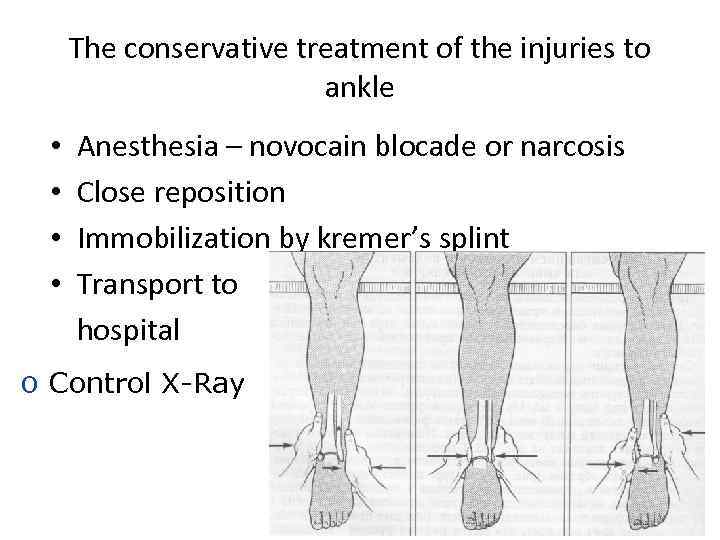 The conservative treatment of the injuries to ankle • • Anesthesia – novocain blocade or narcosis Close reposition Immobilization by kremer’s splint Transport to hospital o Control X-Ray
The conservative treatment of the injuries to ankle • • Anesthesia – novocain blocade or narcosis Close reposition Immobilization by kremer’s splint Transport to hospital o Control X-Ray
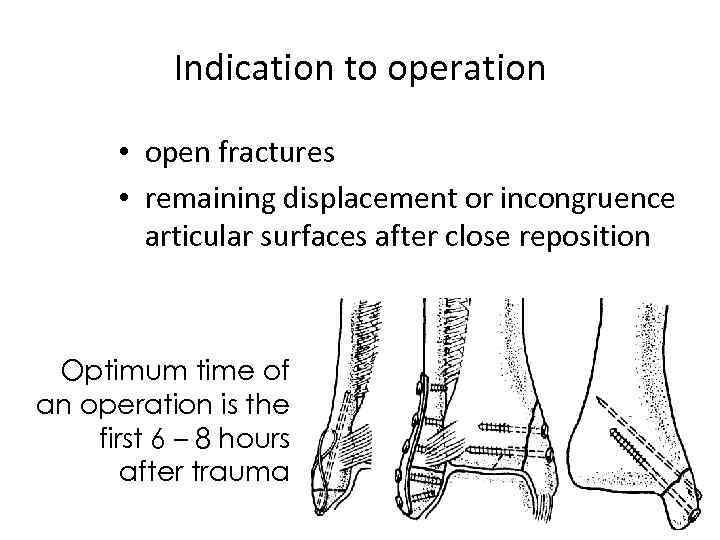 Indication to operation • open fractures • remaining displacement or incongruence articular surfaces after close reposition Optimum time of an operation is the first 6 – 8 hours after trauma
Indication to operation • open fractures • remaining displacement or incongruence articular surfaces after close reposition Optimum time of an operation is the first 6 – 8 hours after trauma
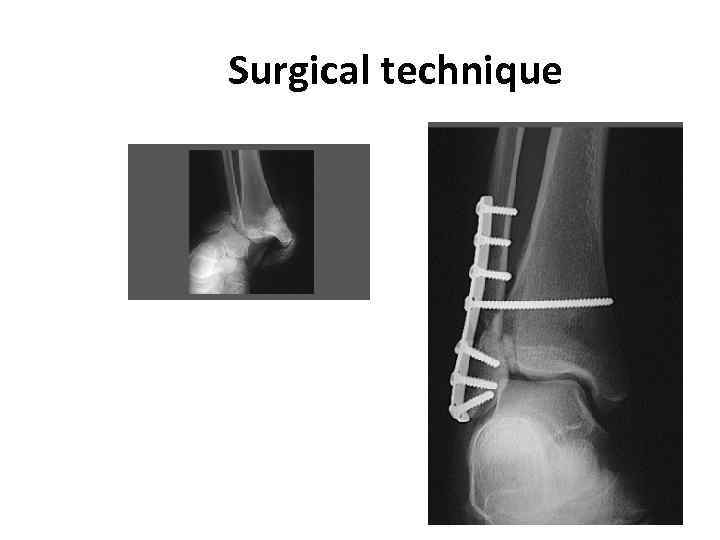 Surgical technique
Surgical technique
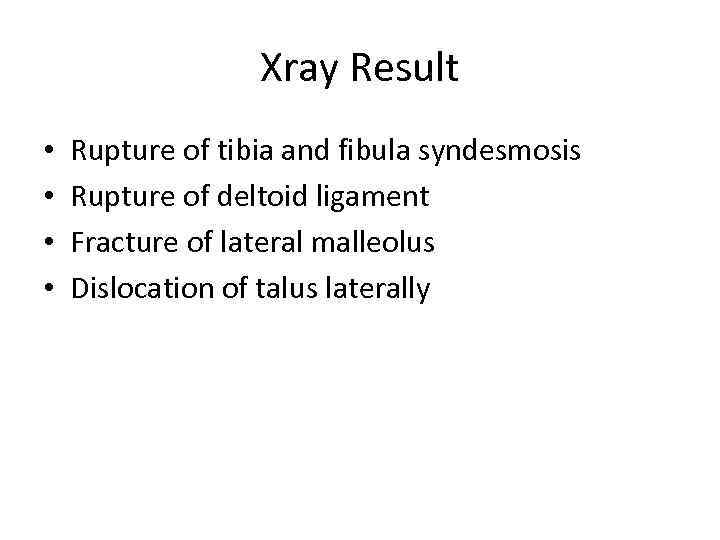 Xray Result • • Rupture of tibia and fibula syndesmosis Rupture of deltoid ligament Fracture of lateral malleolus Dislocation of talus laterally
Xray Result • • Rupture of tibia and fibula syndesmosis Rupture of deltoid ligament Fracture of lateral malleolus Dislocation of talus laterally
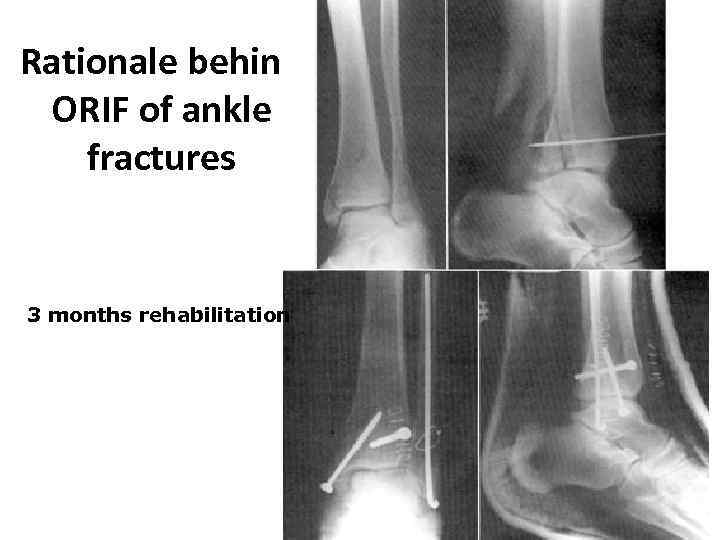 Rationale behind ORIF of ankle fractures 3 months rehabilitation
Rationale behind ORIF of ankle fractures 3 months rehabilitation
 Modern method of osteosynthesis Minimally Invasive Plate Osteosynthesis (MIPO)
Modern method of osteosynthesis Minimally Invasive Plate Osteosynthesis (MIPO)
 Case presentation
Case presentation
 Xray Result • Fracture of lateral malleolus • Fracture of tibia and fibula syndesmosis
Xray Result • Fracture of lateral malleolus • Fracture of tibia and fibula syndesmosis
 Minimally Invasive Plate Osteosynthesis (MIPO)
Minimally Invasive Plate Osteosynthesis (MIPO)
 View after the operation
View after the operation
 Rehabilitation • • • middle period of consolidation is 6 – 8 weeks medical exercises massage physiotherapy insole-supinator
Rehabilitation • • • middle period of consolidation is 6 – 8 weeks medical exercises massage physiotherapy insole-supinator
 References • http: //www. orthobullets. com/trauma/1047/a nkle-fractures • https: //www 2. aofoundation. org/wps/portal/s urgery? show. Page=diagnosis&bone=Tibia&seg ment=Malleoli
References • http: //www. orthobullets. com/trauma/1047/a nkle-fractures • https: //www 2. aofoundation. org/wps/portal/s urgery? show. Page=diagnosis&bone=Tibia&seg ment=Malleoli
 Department of Traumatology and Orthopaedic Surgery Injury of foot
Department of Traumatology and Orthopaedic Surgery Injury of foot
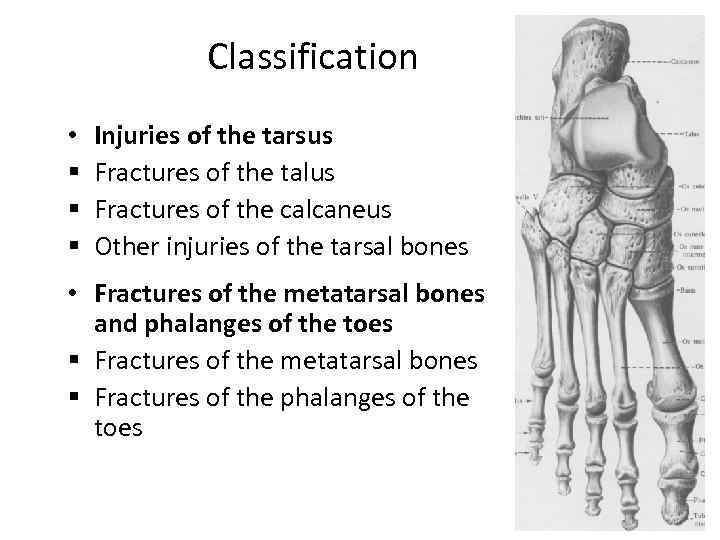 Classification • § § § Injuries of the tarsus Fractures of the talus Fractures of the calcaneus Other injuries of the tarsal bones • Fractures of the metatarsal bones and phalanges of the toes § Fractures of the metatarsal bones § Fractures of the phalanges of the toes
Classification • § § § Injuries of the tarsus Fractures of the talus Fractures of the calcaneus Other injuries of the tarsal bones • Fractures of the metatarsal bones and phalanges of the toes § Fractures of the metatarsal bones § Fractures of the phalanges of the toes
 Fracture of the talus
Fracture of the talus
 EPIDEMIOLOGY • These are second in frequency among all tarsal fractures. • The incidence of fractures of the talus ranges from 0. 1% to 0. 85% all fractures and 5% to 7% of foot injuries. • Approximately 14% to 26% of talar neck fractures had associate fracture of the medial malleolus. • Lateral process of the talus fractures accounted for 2. 3% of a snowboarding injuries and 15% of all ankle injuries. • Fractures of the talar head are rare with an incidence of 3% to 5% c all fractures of the talus.
EPIDEMIOLOGY • These are second in frequency among all tarsal fractures. • The incidence of fractures of the talus ranges from 0. 1% to 0. 85% all fractures and 5% to 7% of foot injuries. • Approximately 14% to 26% of talar neck fractures had associate fracture of the medial malleolus. • Lateral process of the talus fractures accounted for 2. 3% of a snowboarding injuries and 15% of all ankle injuries. • Fractures of the talar head are rare with an incidence of 3% to 5% c all fractures of the talus.
 Mechanism of injury • Most commonly with a motor vehicle accident or a fall from a height with a component of hyperdorsifiexion of the ankle. The talar neck fractures as it impacts the anterior margin of the tibia. • crashing airplane impacting the plantar aspect of the foot, resulting in a talar neck fracture
Mechanism of injury • Most commonly with a motor vehicle accident or a fall from a height with a component of hyperdorsifiexion of the ankle. The talar neck fractures as it impacts the anterior margin of the tibia. • crashing airplane impacting the plantar aspect of the foot, resulting in a talar neck fracture
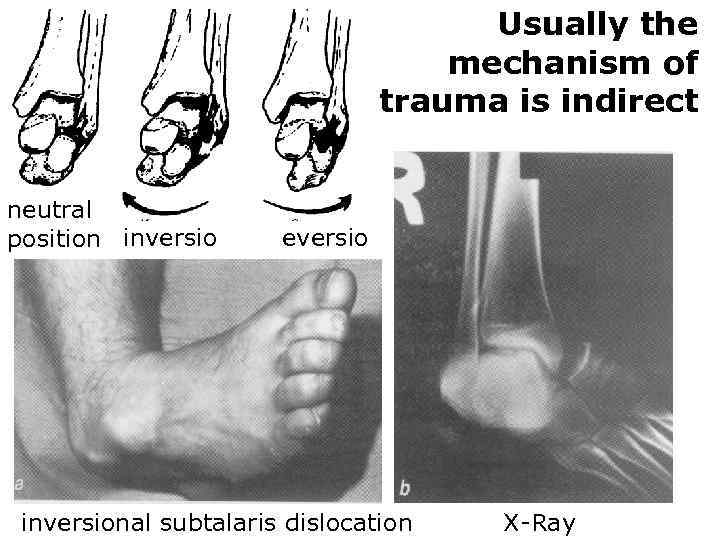 Usually the mechanism of trauma is indirect neutral position inversio eversio inversional subtalaris dislocation X-Ray
Usually the mechanism of trauma is indirect neutral position inversio eversio inversional subtalaris dislocation X-Ray
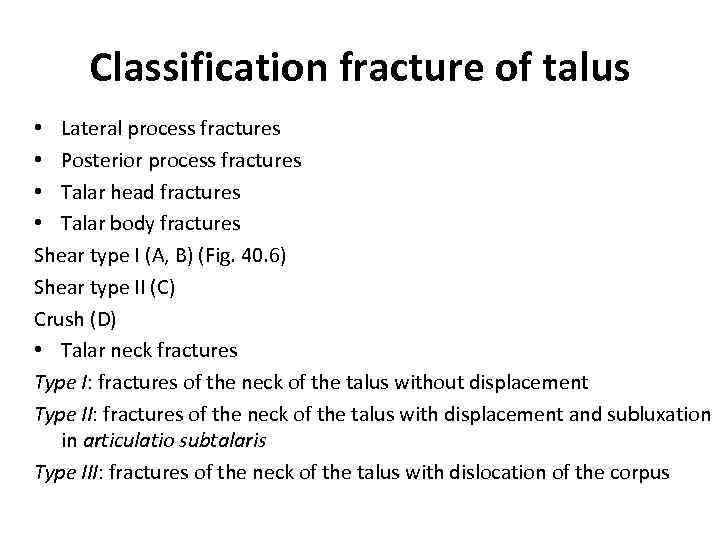 Classification fracture of talus • Lateral process fractures • Posterior process fractures • Talar head fractures • Talar body fractures Shear type I (A, B) (Fig. 40. 6) Shear type II (C) Crush (D) • Talar neck fractures Type I: fractures of the neck of the talus without displacement Type II: fractures of the neck of the talus with displacement and subluxation in articulatio subtalaris Type III: fractures of the neck of the talus with dislocation of the corpus
Classification fracture of talus • Lateral process fractures • Posterior process fractures • Talar head fractures • Talar body fractures Shear type I (A, B) (Fig. 40. 6) Shear type II (C) Crush (D) • Talar neck fractures Type I: fractures of the neck of the talus without displacement Type II: fractures of the neck of the talus with displacement and subluxation in articulatio subtalaris Type III: fractures of the neck of the talus with dislocation of the corpus
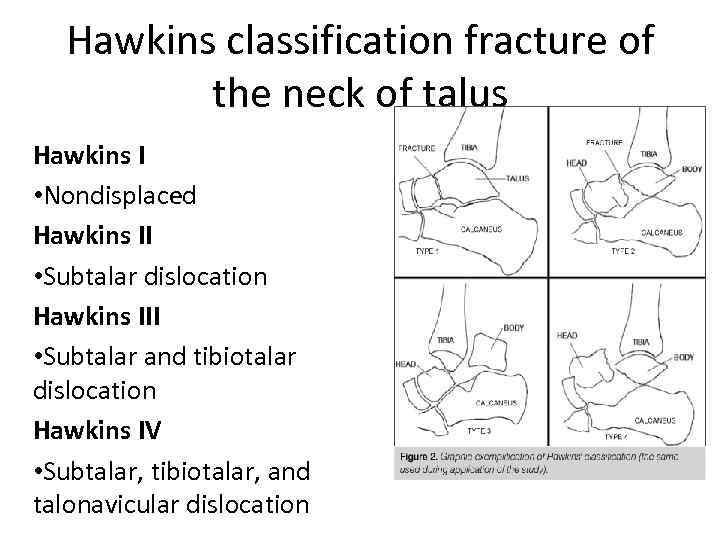 Hawkins classification fracture of the neck of talus Hawkins I • Nondisplaced Hawkins II • Subtalar dislocation Hawkins III • Subtalar and tibiotalar dislocation Hawkins IV • Subtalar, tibiotalar, and talonavicular dislocation
Hawkins classification fracture of the neck of talus Hawkins I • Nondisplaced Hawkins II • Subtalar dislocation Hawkins III • Subtalar and tibiotalar dislocation Hawkins IV • Subtalar, tibiotalar, and talonavicular dislocation
 Clinical presentation • pain • Range of foot and ankle motion is typically painful and may elicit crepitus. • Diffuse swelling of the hindfoot with tenderness • Associated fractures of the foot and ankle are commonly seen with fractures of the talar neck and body.
Clinical presentation • pain • Range of foot and ankle motion is typically painful and may elicit crepitus. • Diffuse swelling of the hindfoot with tenderness • Associated fractures of the foot and ankle are commonly seen with fractures of the talar neck and body.
 Conservative treatment Indication: Nondisplaced Fractures (Hawkins Type I), talar body fracture, nondisplaced fracture of the head of talus • short leg cast or boot for 8 to 12 weeks • patient should remain non-weight bearing for 6 weeks until radiographic evidence of fracture healing
Conservative treatment Indication: Nondisplaced Fractures (Hawkins Type I), talar body fracture, nondisplaced fracture of the head of talus • short leg cast or boot for 8 to 12 weeks • patient should remain non-weight bearing for 6 weeks until radiographic evidence of fracture healing
 Operative treatment Indication: all Displaced fractures • Open reposition internal fixation osteosynthesis by plate and screw
Operative treatment Indication: all Displaced fractures • Open reposition internal fixation osteosynthesis by plate and screw
 Fracture of the calcaneous
Fracture of the calcaneous
 Epidemiology • Calcaneus fractures account for approximately 2% of all fractures. The calcaneus, or os calcis, is the most frequently fractured tarsal bone. • Displaced intra-articular fractures comprise 60% to 75% of calcaneus fractures. • 90 percent of calcaneus fractures occur in men between 21 and 45 years of age, with the majority being in industrial workers. • Approximately 10% of calcaneus fractures are open injuries
Epidemiology • Calcaneus fractures account for approximately 2% of all fractures. The calcaneus, or os calcis, is the most frequently fractured tarsal bone. • Displaced intra-articular fractures comprise 60% to 75% of calcaneus fractures. • 90 percent of calcaneus fractures occur in men between 21 and 45 years of age, with the majority being in industrial workers. • Approximately 10% of calcaneus fractures are open injuries
 MECHANISM OF INJURY • Axial loading: Falls from a height are responsible for most intra-articular fractures • Twisting forces may be associated with extraarticular calcanein fractures
MECHANISM OF INJURY • Axial loading: Falls from a height are responsible for most intra-articular fractures • Twisting forces may be associated with extraarticular calcanein fractures
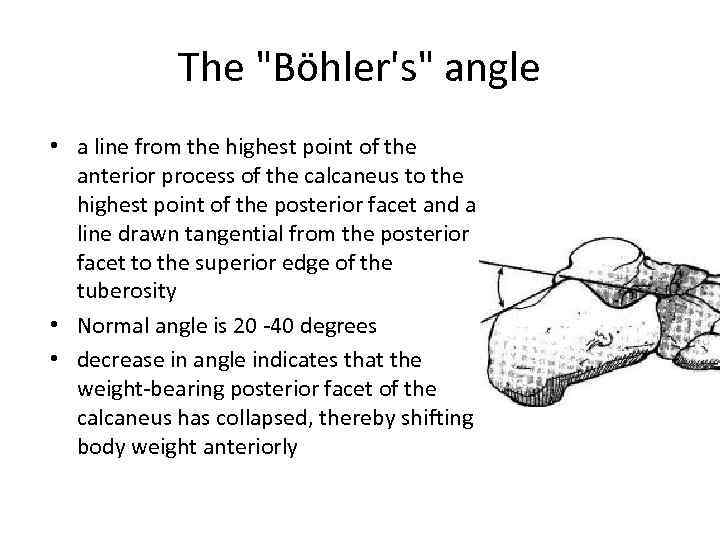 The "Böhler's" angle • a line from the highest point of the anterior process of the calcaneus to the highest point of the posterior facet and a line drawn tangential from the posterior facet to the superior edge of the tuberosity • Normal angle is 20 -40 degrees • decrease in angle indicates that the weight-bearing posterior facet of the calcaneus has collapsed, thereby shifting body weight anteriorly
The "Böhler's" angle • a line from the highest point of the anterior process of the calcaneus to the highest point of the posterior facet and a line drawn tangential from the posterior facet to the superior edge of the tuberosity • Normal angle is 20 -40 degrees • decrease in angle indicates that the weight-bearing posterior facet of the calcaneus has collapsed, thereby shifting body weight anteriorly
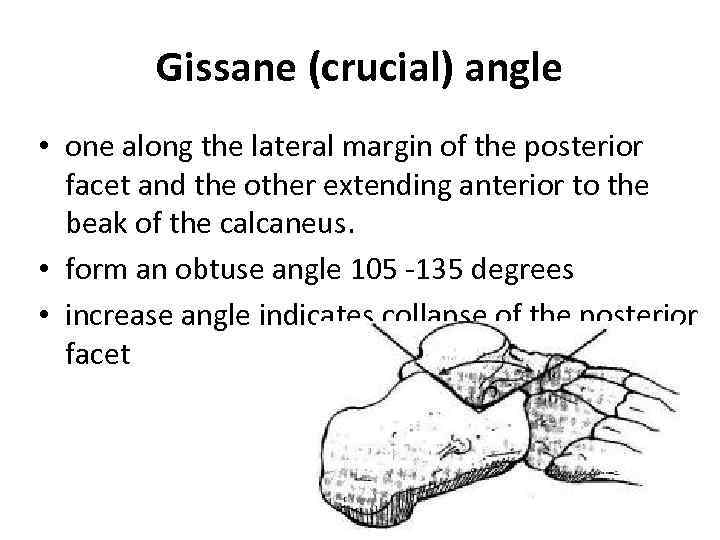 Gissane (crucial) angle • one along the lateral margin of the posterior facet and the other extending anterior to the beak of the calcaneus. • form an obtuse angle 105 -135 degrees • increase angle indicates collapse of the posterior facet
Gissane (crucial) angle • one along the lateral margin of the posterior facet and the other extending anterior to the beak of the calcaneus. • form an obtuse angle 105 -135 degrees • increase angle indicates collapse of the posterior facet
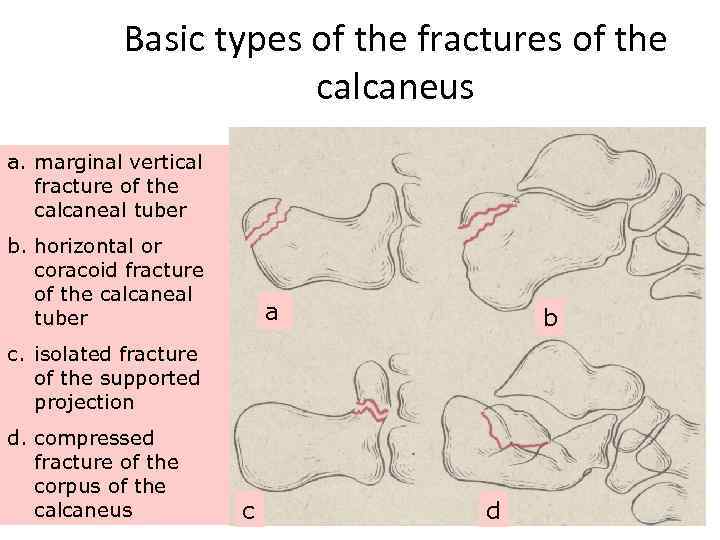 Basic types of the fractures of the calcaneus a. marginal vertical fracture of the calcaneal tuber b. horizontal or coracoid fracture of the calcaneal tuber a b c. isolated fracture of the supported projection d. compressed fracture of the corpus of the calcaneus c d
Basic types of the fractures of the calcaneus a. marginal vertical fracture of the calcaneal tuber b. horizontal or coracoid fracture of the calcaneal tuber a b c. isolated fracture of the supported projection d. compressed fracture of the corpus of the calcaneus c d
 Classification fracture of calcaneus Extra-articular Fractures lntra-articular Fractures (do not involve the posterior • Essex-Lopresti facet) Classification • Anterior process fractures • Sanders Classification • • Tuberosity fractures Medial process fractures Sustentacular fractures Body fractures not involving the subtalar articulation
Classification fracture of calcaneus Extra-articular Fractures lntra-articular Fractures (do not involve the posterior • Essex-Lopresti facet) Classification • Anterior process fractures • Sanders Classification • • Tuberosity fractures Medial process fractures Sustentacular fractures Body fractures not involving the subtalar articulation
 Essex-Lopresti classification Primary Fracture Line • Fracture line exits anterolaterally at the crucial angle or as far distally as the calcaneocuboid joint. Posteriorly, the fracture moves from plantar medial to dorsal lateral, producing two main fragments: • Anteromedial fragment: rarely comminuted, remains attached to talus by deltoid and interosseous talocalcaneal ligaments. • Posterolateral fragment: usually displaces superolaterally, variable comminution, resulting in incongruity of posterior facet with heel shortening and widening.
Essex-Lopresti classification Primary Fracture Line • Fracture line exits anterolaterally at the crucial angle or as far distally as the calcaneocuboid joint. Posteriorly, the fracture moves from plantar medial to dorsal lateral, producing two main fragments: • Anteromedial fragment: rarely comminuted, remains attached to talus by deltoid and interosseous talocalcaneal ligaments. • Posterolateral fragment: usually displaces superolaterally, variable comminution, resulting in incongruity of posterior facet with heel shortening and widening.
 Secondary Fracture Line • Tongue fracture: A secondary fracture line appears beneath the facet and exits posteriorly through the tuberosity. • Joint Depression fracture: A secondary fracture line exits just behind the posterior facet. • Heel shortening and widening occurs leading to rotation of tuberosity fragment into varus. This causes lateral wall blowout, which may extend as far anteriorly as the calcaneocuboid joint. As the lateral edge of the talus collapses further, there will be additional comminution of the articular surface.
Secondary Fracture Line • Tongue fracture: A secondary fracture line appears beneath the facet and exits posteriorly through the tuberosity. • Joint Depression fracture: A secondary fracture line exits just behind the posterior facet. • Heel shortening and widening occurs leading to rotation of tuberosity fragment into varus. This causes lateral wall blowout, which may extend as far anteriorly as the calcaneocuboid joint. As the lateral edge of the talus collapses further, there will be additional comminution of the articular surface.
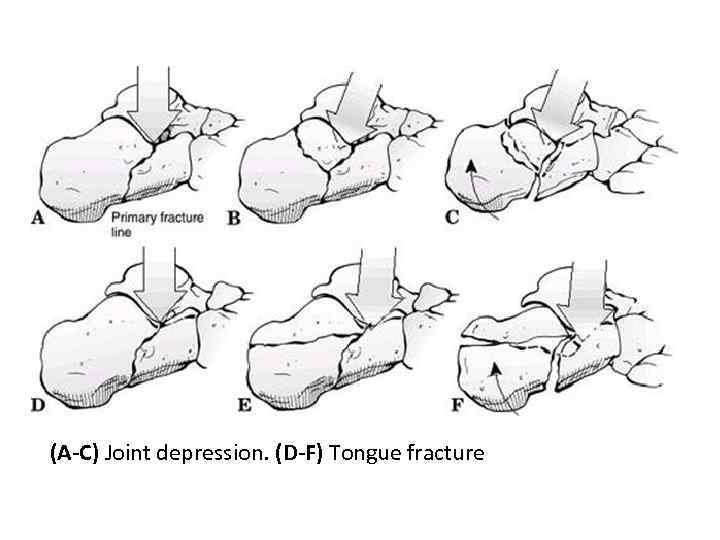 (A-C) Joint depression. (D-F) Tongue fracture
(A-C) Joint depression. (D-F) Tongue fracture
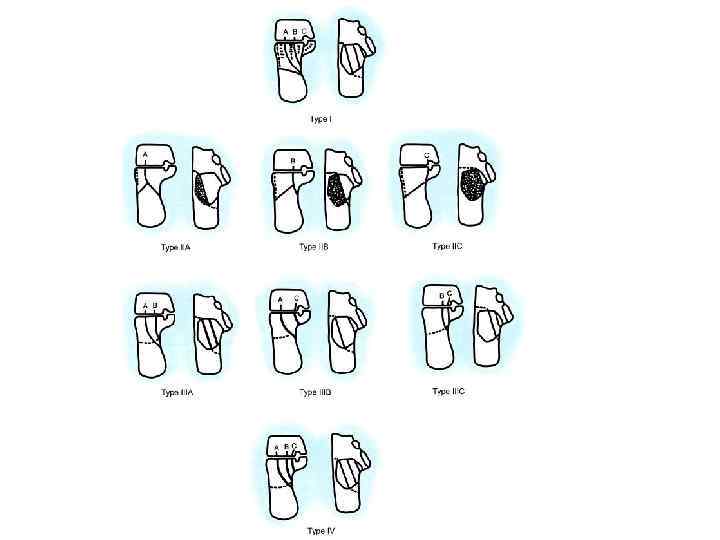
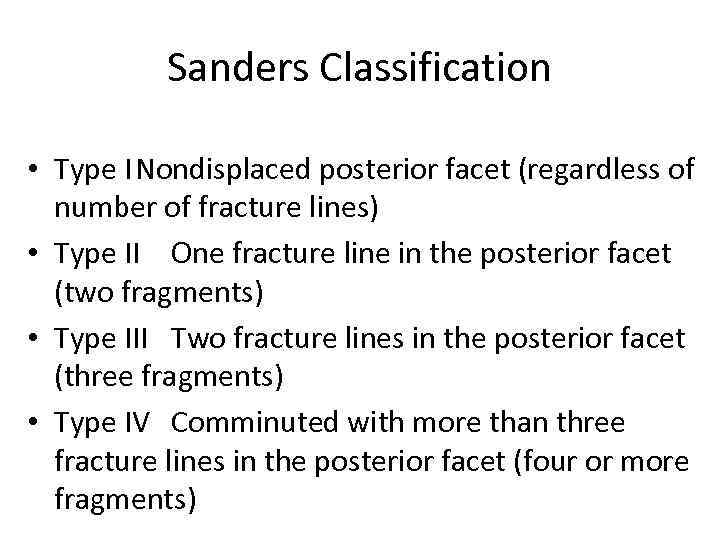 Sanders Classification • Type INondisplaced posterior facet (regardless of number of fracture lines) • Type II One fracture line in the posterior facet (two fragments) • Type III Two fracture lines in the posterior facet (three fragments) • Type IV Comminuted with more than three fracture lines in the posterior facet (four or more fragments)
Sanders Classification • Type INondisplaced posterior facet (regardless of number of fracture lines) • Type II One fracture line in the posterior facet (two fragments) • Type III Two fracture lines in the posterior facet (three fragments) • Type IV Comminuted with more than three fracture lines in the posterior facet (four or more fragments)
 Basic symptoms of the fractures of the calcaneus • The general symptoms of damage: a pain, a swelling, a bruise, increase of local temperature, lesion of function, flat-footed. • Authentic symptoms of fractures: crepitus, deformation. Possible appearance of bone’s fragments in a wound for open penetrating fractures
Basic symptoms of the fractures of the calcaneus • The general symptoms of damage: a pain, a swelling, a bruise, increase of local temperature, lesion of function, flat-footed. • Authentic symptoms of fractures: crepitus, deformation. Possible appearance of bone’s fragments in a wound for open penetrating fractures
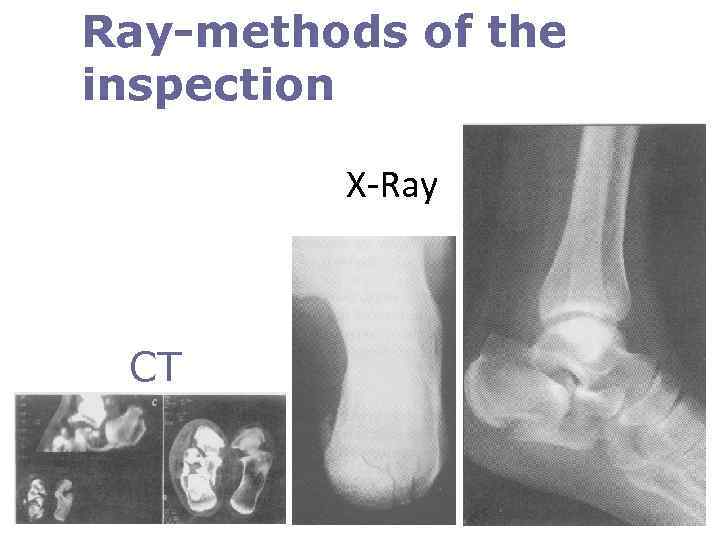 Ray-methods of the inspection X-Ray CT
Ray-methods of the inspection X-Ray CT
 Conservative treatment • consists of a supportive splint to allow dissipation of the initial fracture hematoma, followed by conversion to a prefabricated fracture boot • non-weight-bearing restrictions are maintained for approximately 10 to 12 weeks, until radiographic union Indication: • Nondisplaced fractures. • Anterior process fractures with less than 25% involvement of the calcaneal-cuboid articulation. • Fractures in patients with severe peripheral vascular disease or insulin-dependent diabetes.
Conservative treatment • consists of a supportive splint to allow dissipation of the initial fracture hematoma, followed by conversion to a prefabricated fracture boot • non-weight-bearing restrictions are maintained for approximately 10 to 12 weeks, until radiographic union Indication: • Nondisplaced fractures. • Anterior process fractures with less than 25% involvement of the calcaneal-cuboid articulation. • Fractures in patients with severe peripheral vascular disease or insulin-dependent diabetes.
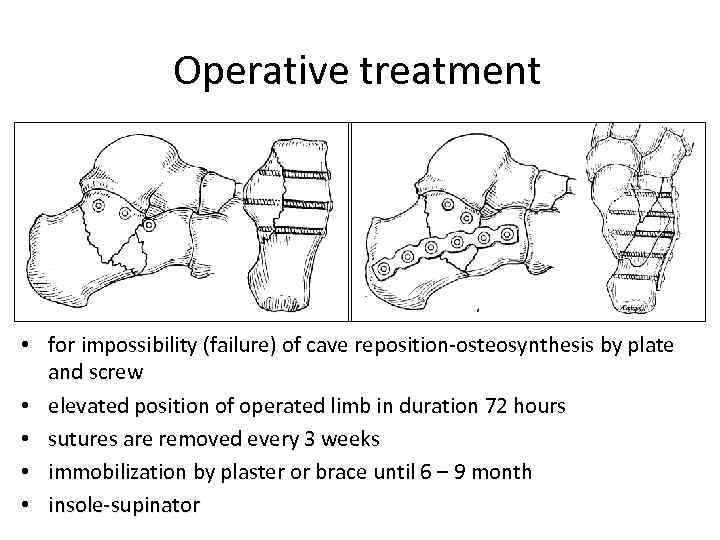 Operative treatment • for impossibility (failure) of cave reposition-osteosynthesis by plate and screw • elevated position of operated limb in duration 72 hours • sutures are removed every 3 weeks • immobilization by plaster or brace until 6 – 9 month • insole-supinator
Operative treatment • for impossibility (failure) of cave reposition-osteosynthesis by plate and screw • elevated position of operated limb in duration 72 hours • sutures are removed every 3 weeks • immobilization by plaster or brace until 6 – 9 month • insole-supinator
 Fracture of the midfoot
Fracture of the midfoot
 Epidemiology • Injuries to the midfoot are rare. • The most commonly fractured bone was the cuboid followed by navicular and cuneiform (6%). • The male-to-female ratio is 1: 1. 2
Epidemiology • Injuries to the midfoot are rare. • The most commonly fractured bone was the cuboid followed by navicular and cuneiform (6%). • The male-to-female ratio is 1: 1. 2
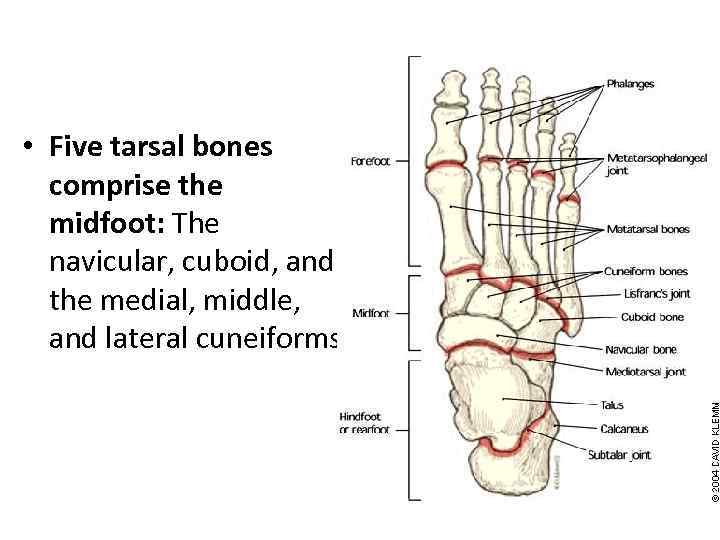 • Five tarsal bones comprise the midfoot: The navicular, cuboid, and the medial, middle, and lateral cuneiforms.
• Five tarsal bones comprise the midfoot: The navicular, cuboid, and the medial, middle, and lateral cuneiforms.
 Mechanism of Injury • High-energy trauma: This is most common and may result from direct impact from a motor vehicle accident or a combination of axial loading and torsion, such as during impact from a fall or jump from a height. • Low-energy injuries: This may result in a sprain during athletic or dance activities.
Mechanism of Injury • High-energy trauma: This is most common and may result from direct impact from a motor vehicle accident or a combination of axial loading and torsion, such as during impact from a fall or jump from a height. • Low-energy injuries: This may result in a sprain during athletic or dance activities.
 Classification • Modial Stress Injury • longitudinal Stress Injury • Lateral Stress Injury "Nutcracker fracture": This is the characteristic fracture of the cuboid as the forefoot driven laterally, crushing the cuboid be-tween the calcaneus and the fourth and fifth metatarsal bases. • Plantar Stress Injury
Classification • Modial Stress Injury • longitudinal Stress Injury • Lateral Stress Injury "Nutcracker fracture": This is the characteristic fracture of the cuboid as the forefoot driven laterally, crushing the cuboid be-tween the calcaneus and the fourth and fifth metatarsal bases. • Plantar Stress Injury
 Clinical presentation swelling and tenderness Pain ecchymosis deformity Stress maneuvers consist of forefoot abduction, adduction, flex-ion, and extension, and may result in reproduction of pain and instability. • serial examinations to evaluate the possibility of foot compartment syndrome. • • •
Clinical presentation swelling and tenderness Pain ecchymosis deformity Stress maneuvers consist of forefoot abduction, adduction, flex-ion, and extension, and may result in reproduction of pain and instability. • serial examinations to evaluate the possibility of foot compartment syndrome. • • •
 Treatment Conservative • For Nondisplaced fractures • a short leg cw fracture brace with initial non— weight bearing for 6 weeks. Operative • For displaced fracture • open reduction and internal fixation
Treatment Conservative • For Nondisplaced fractures • a short leg cw fracture brace with initial non— weight bearing for 6 weeks. Operative • For displaced fracture • open reduction and internal fixation
 Fracture of the metatarsal bones
Fracture of the metatarsal bones
 Mechanism of Injury • Direct: This most commonly occurs when a heavy object is dropped on the forefoot. • Twisting: This occurs with body torque when the toes are fixed, such as when a person catches the toes in a narrow opening with continued ambulation. • Avulsion: This occurs particularly at the base of the fifth metatarsal. • Stress fractures: These occur especially at the necks of the second and third metatarsals and the proximal fifth metatarsal
Mechanism of Injury • Direct: This most commonly occurs when a heavy object is dropped on the forefoot. • Twisting: This occurs with body torque when the toes are fixed, such as when a person catches the toes in a narrow opening with continued ambulation. • Avulsion: This occurs particularly at the base of the fifth metatarsal. • Stress fractures: These occur especially at the necks of the second and third metatarsals and the proximal fifth metatarsal
 OTA Classification fracture of metatarsal bone Types: 1. Metatarsal proximal and distal nonarticular and diaphysis 2. Metatarsal proximal and distalpartial articular diaphysis wedge comminution 3. Metatarsal proximal and distal complete articular diaphysis comminuted
OTA Classification fracture of metatarsal bone Types: 1. Metatarsal proximal and distal nonarticular and diaphysis 2. Metatarsal proximal and distalpartial articular diaphysis wedge comminution 3. Metatarsal proximal and distal complete articular diaphysis comminuted
 Treatment Conservative • For Nondisplaced fractures • hard-soled shoe Operative • For displaced fracture • open reduction and internal fixation osteosynthesis by plate and screws
Treatment Conservative • For Nondisplaced fractures • hard-soled shoe Operative • For displaced fracture • open reduction and internal fixation osteosynthesis by plate and screws

 Injury to Metatarsopharangeal Joints
Injury to Metatarsopharangeal Joints
 Epidemiology • Injuries to the first MTP joint are relatively common, especially in athletic activities or ballet. • The incidence in US football and soccer has risen because of the • use of artificial playing surfaces as well as lighter, more flexible shoes that permit enhanced motion at the MTP joint
Epidemiology • Injuries to the first MTP joint are relatively common, especially in athletic activities or ballet. • The incidence in US football and soccer has risen because of the • use of artificial playing surfaces as well as lighter, more flexible shoes that permit enhanced motion at the MTP joint
 Classification Bowers and Martin • Grade I: Strain at the proximal attachment of the volar plate from • the first metatarsal head • Grade II: Avulsion of the volar plate from the metatarsal head • Grade III: Impaction injury to the dorsal surface of the metatarsal • head with or without an avulsion or chip fracture
Classification Bowers and Martin • Grade I: Strain at the proximal attachment of the volar plate from • the first metatarsal head • Grade II: Avulsion of the volar plate from the metatarsal head • Grade III: Impaction injury to the dorsal surface of the metatarsal • head with or without an avulsion or chip fracture
 Alms Classification of First Metatarsophalangeal Dislocations This is based on the integrity of the sesamoid complex. • Type I: Volar plate avulsed off the first metatarsal head, proximal phalanx displaced dorsally; intersesamoid ligament remaining intact and lying over the dorsum of the metatarsalhead • Type HA: Rupture of the intersesamoid ligament • Type IIB: Longitudinal fracture of either sesamoid
Alms Classification of First Metatarsophalangeal Dislocations This is based on the integrity of the sesamoid complex. • Type I: Volar plate avulsed off the first metatarsal head, proximal phalanx displaced dorsally; intersesamoid ligament remaining intact and lying over the dorsum of the metatarsalhead • Type HA: Rupture of the intersesamoid ligament • Type IIB: Longitudinal fracture of either sesamoid
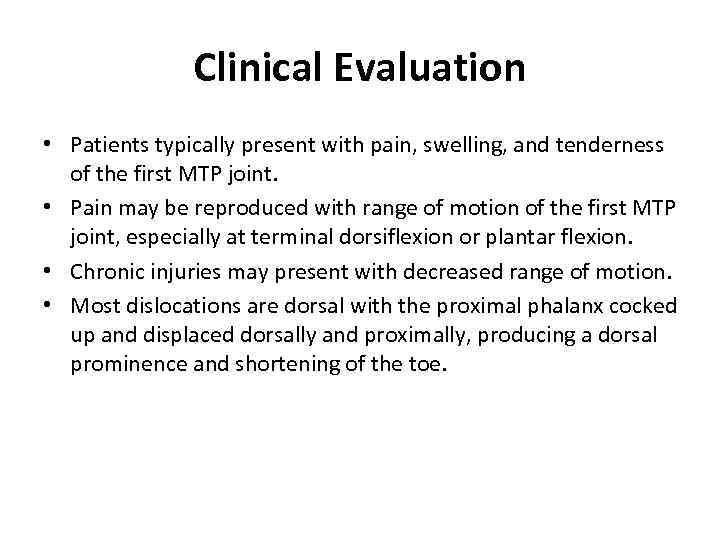 Clinical Evaluation • Patients typically present with pain, swelling, and tenderness of the first MTP joint. • Pain may be reproduced with range of motion of the first MTP joint, especially at terminal dorsiflexion or plantar flexion. • Chronic injuries may present with decreased range of motion. • Most dislocations are dorsal with the proximal phalanx cocked up and displaced dorsally and proximally, producing a dorsal prominence and shortening of the toe.
Clinical Evaluation • Patients typically present with pain, swelling, and tenderness of the first MTP joint. • Pain may be reproduced with range of motion of the first MTP joint, especially at terminal dorsiflexion or plantar flexion. • Chronic injuries may present with decreased range of motion. • Most dislocations are dorsal with the proximal phalanx cocked up and displaced dorsally and proximally, producing a dorsal prominence and shortening of the toe.
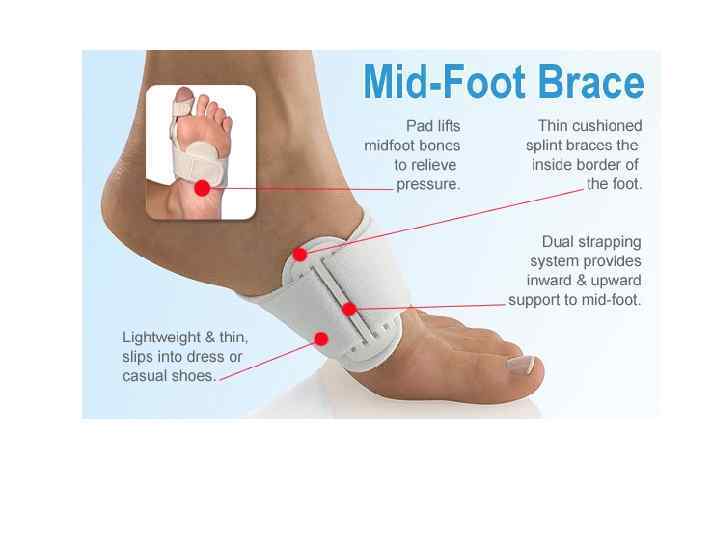
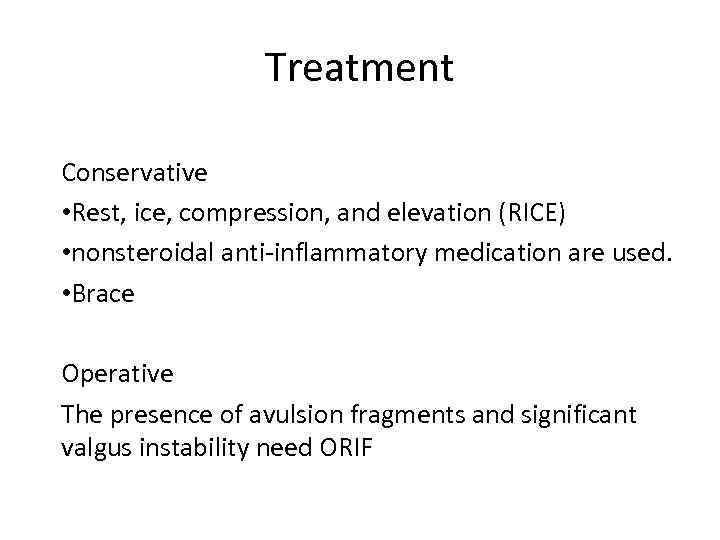 Treatment Conservative • Rest, ice, compression, and elevation (RICE) • nonsteroidal anti-inflammatory medication are used. • Brace Operative The presence of avulsion fragments and significant valgus instability need ORIF
Treatment Conservative • Rest, ice, compression, and elevation (RICE) • nonsteroidal anti-inflammatory medication are used. • Brace Operative The presence of avulsion fragments and significant valgus instability need ORIF
 Fracture of the phalanges of the toe
Fracture of the phalanges of the toe
 Classification • Location: Proximal, middle, distal phalanx • • • Angulation Displacement Comminution Intra-articular involvement Presence of fracture-dislocation
Classification • Location: Proximal, middle, distal phalanx • • • Angulation Displacement Comminution Intra-articular involvement Presence of fracture-dislocation
 Conservative Treatment • Nondisplaced fractures irrespective of articular involvement can be treated with a stiff-soled shoe and protected weight bearing with advancement as tolerated. • Use of buddy taping between adjacent toes may provide pain relief and help to stabilize potentially unstable fracture patterns.
Conservative Treatment • Nondisplaced fractures irrespective of articular involvement can be treated with a stiff-soled shoe and protected weight bearing with advancement as tolerated. • Use of buddy taping between adjacent toes may provide pain relief and help to stabilize potentially unstable fracture patterns.
 Operative treatment • Operative reduction is reserved for those rare fractures with gross instability or persistent intra-articular discontinuity
Operative treatment • Operative reduction is reserved for those rare fractures with gross instability or persistent intra-articular discontinuity


