d40587dbe54e6c72fb450e0b5448fe1a.ppt
- Количество слайдов: 54


KT Trials Must Overcome Both Poor Practitioner and Patient Performance . . . many unanswered questions and a plea for collaboration, innovation and research Brian Haynes
Objectives • To review some problems of practitioner and patient adherence • To assess the “state of the science” in overcoming these problems • To invite transdisciplinary researchers to “gang up” on these problems
For every complex problem. . . there is a simple solution. . . and it is wrong. C. S. Snow
How many of you are doing/have done… …research in which both practitioner and patient adherence are targeted?
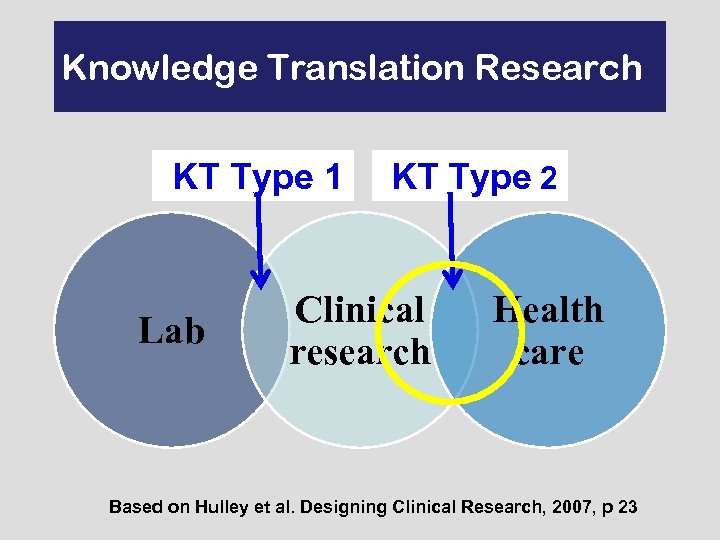
Knowledge Translation Research KT Type 1 Lab KT Type 2 Clinical research Health care Based on Hulley et al. Designing Clinical Research, 2007, p 23
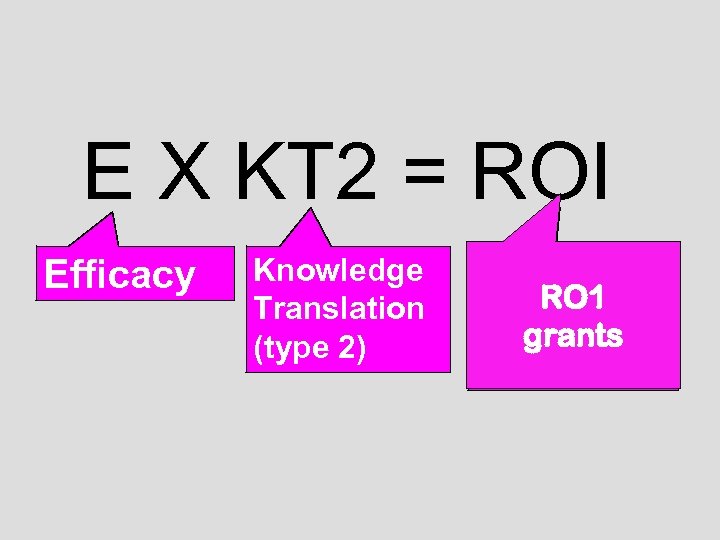
E X KT 2 = ROI Efficacy Knowledge Translation (type 2) Return on Real RO 1 Investmentof Outcomes grants Importance
E = Efficacy. . . …effects of health care interventions under relatively optimal circumstances. (Can this work? )
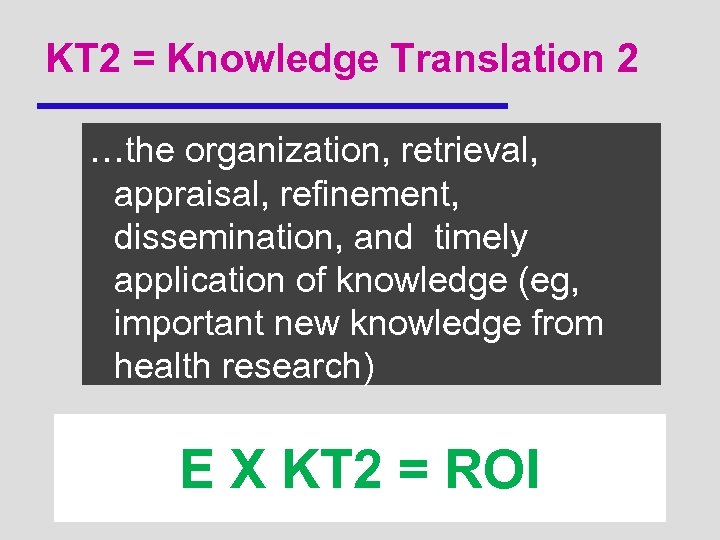
KT 2 = Knowledge Translation 2 …the organization, retrieval, appraisal, refinement, dissemination, and timely application of knowledge (eg, important new knowledge from health research) E X KT 2 = ROI
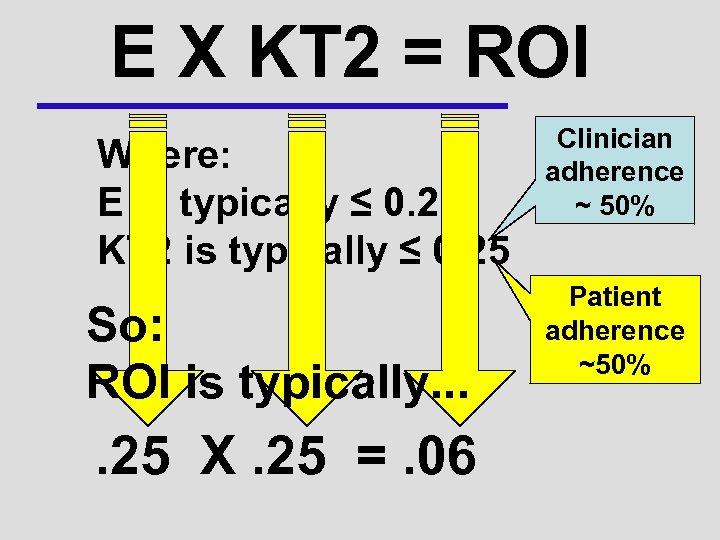
E X KT 2 = ROI Where: E is typically ≤ 0. 25 KT 2 is typically ≤ 0. 25 So: ROI is typically. . 25 X. 25 =. 06 Clinician adherence ~ 50% Patient adherence ~50%
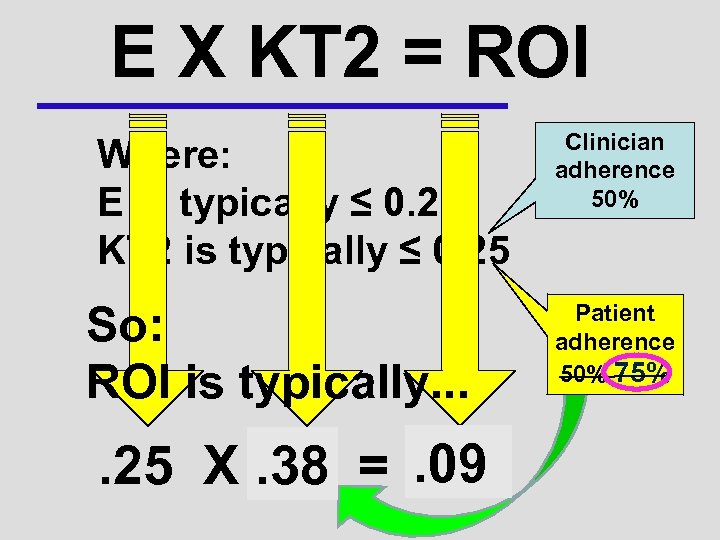
E X KT 2 = ROI Where: E is typically ≤ 0. 25 KT 2 is typically ≤ 0. 25 So: ROI is typically. . 09. 38. 25 X. 25 =. 06 Clinician adherence 50% Patient adherence 50% 75%
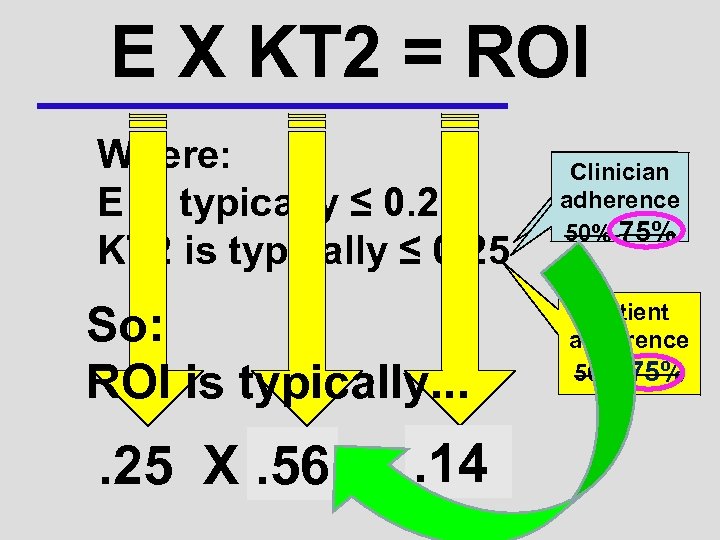
E X KT 2 = ROI Where: E is typically ≤ 0. 25 KT 2 is typically ≤ 0. 25 So: ROI is typically. . 14. 56. 25 X. 25 =. 06 Clinician adherence 50% 75% Patient adherence 50% 75%
Clinician Adherence
When I was a graduate student… In trials of antihypertensive therapy, some of the physicians didn’t know what they were doing… …only 49% of patients in the community were treated …among the prescriptions for ‘treated’ patients were Valium and Phenobarbital
• In all, 73% of microalbuminuric patients were not on ACE-I/ARB. • Hypertensive type II diabetic patients were often left untreated and only a minority of those treated were optimally controlled.
Typical implementation rates for stroke care < 50%
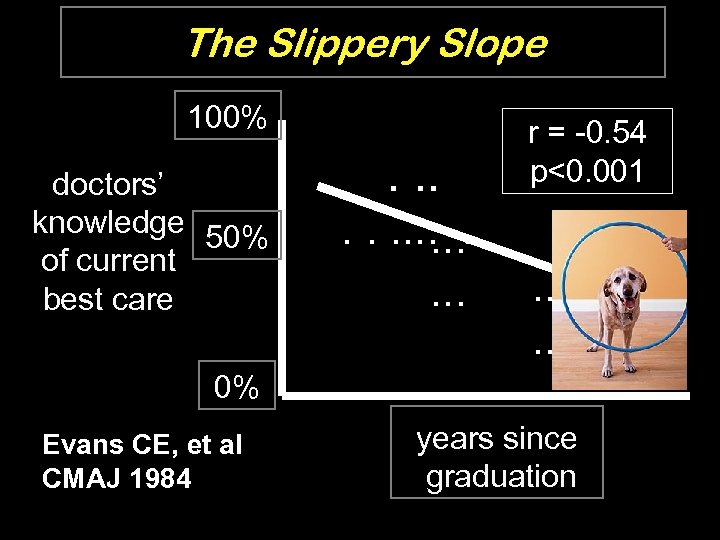
The Slippery Slope 100% doctors’ knowledge 50% of current best care . . . . r = -0. 54 p<0. 001 . . . . 0% Evans CE, et al CMAJ 1984 years since graduation
Typical time to regular implementation of innovations 17 to 20 years
Corticosteroids for threatened preterm delivery* California increased use of antenatal corticosteroids from 76% to 86% over a 3 year period with a statewide QI cycle. *Wirtschafter et al. 2006
EPOC: Cochrane Review Group on Effective Practice and Organization of Care Reviews of interventions to assist professionals to improve the quality of care they provide.
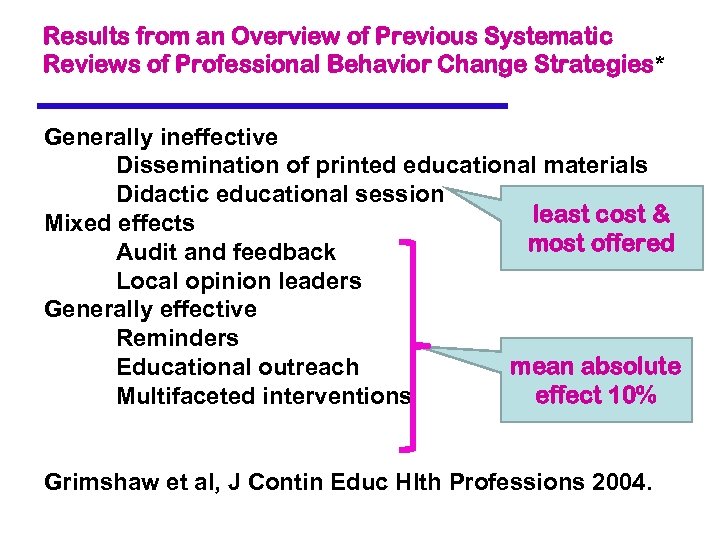
Results from an Overview of Previous Systematic Reviews of Professional Behavior Change Strategies* Generally ineffective Dissemination of printed educational materials Didactic educational session least cost & Mixed effects most offered Audit and feedback Local opinion leaders Generally effective Reminders mean absolute Educational outreach effect 10% Multifaceted interventions Grimshaw et al, J Contin Educ Hlth Professions 2004.
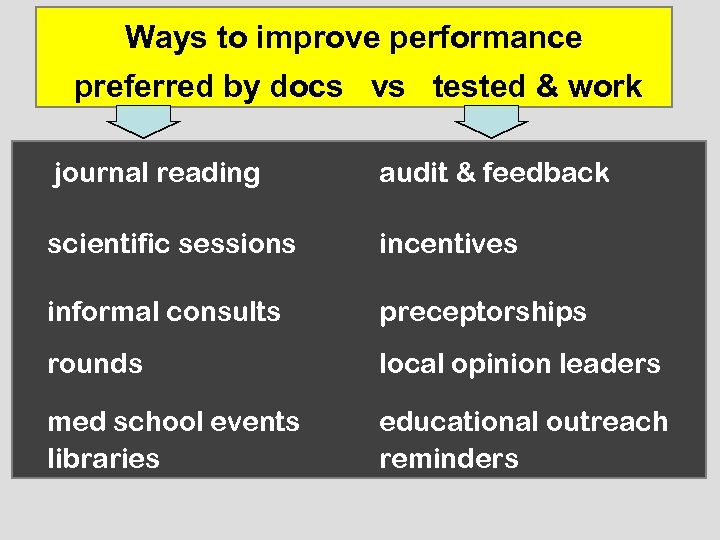
Ways to improve performance preferred by docs vs tested & work journal reading audit & feedback scientific sessions incentives informal consults preceptorships rounds local opinion leaders med school events libraries educational outreach reminders
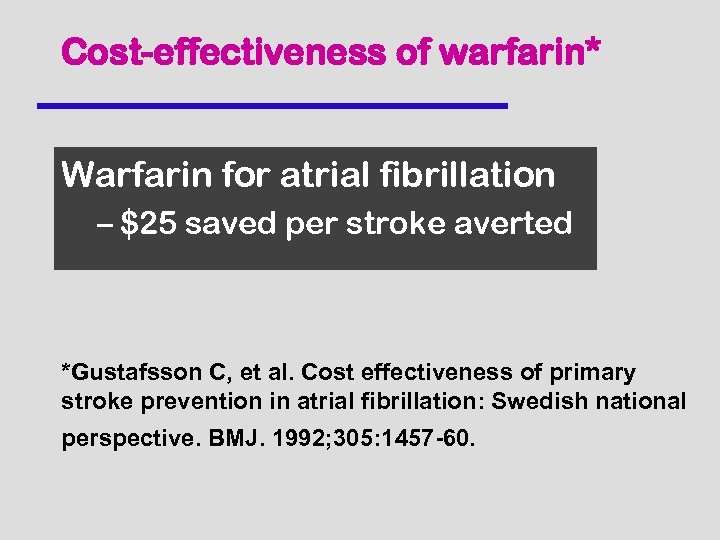
Cost-effectiveness of warfarin* Warfarin for atrial fibrillation – $25 saved per stroke averted *Gustafsson C, et al. Cost effectiveness of primary stroke prevention in atrial fibrillation: Swedish national perspective. BMJ. 1992; 305: 1457 -60.
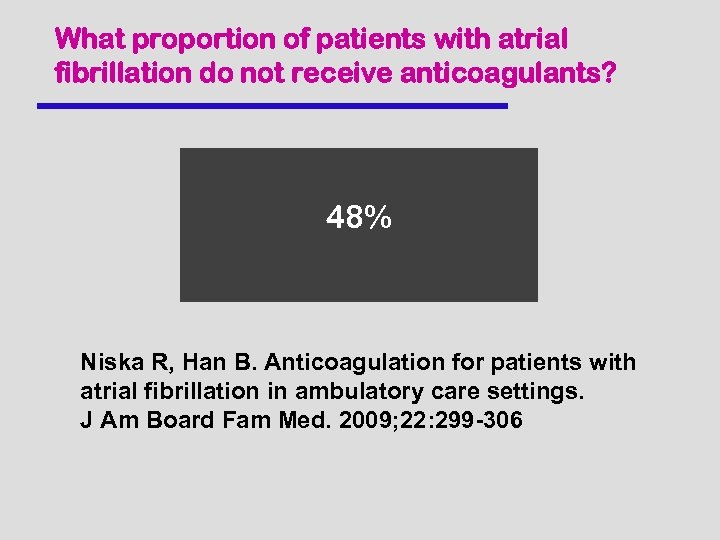
What proportion of patients with atrial fibrillation do not receive anticoagulants? 48% Niska R, Han B. Anticoagulation for patients with atrial fibrillation in ambulatory care settings. J Am Board Fam Med. 2009; 22: 299 -306
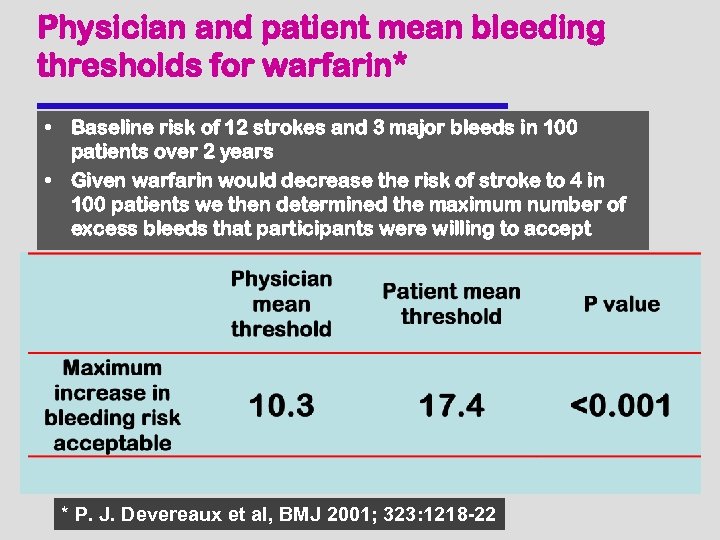
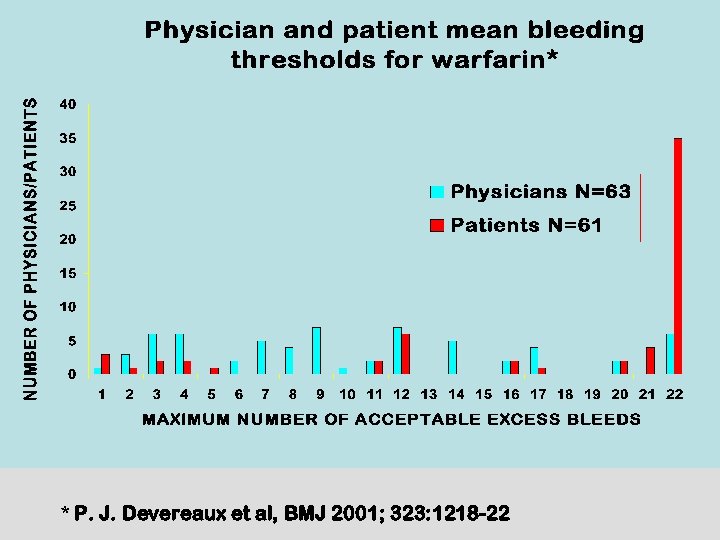
Physician and patient mean bleeding thresholds for warfarin* • Baseline risk of 12 strokes and 3 major bleeds in 100 patients over 2 years • Given warfarin would decrease the risk of stroke to 4 in 100 patients we then determined the maximum number of excess bleeds that participants were willing to accept * P. J. Devereaux et al, BMJ 2001; 323: 1218 -22
* P. J. Devereaux et al, BMJ 2001; 323: 1218 -22
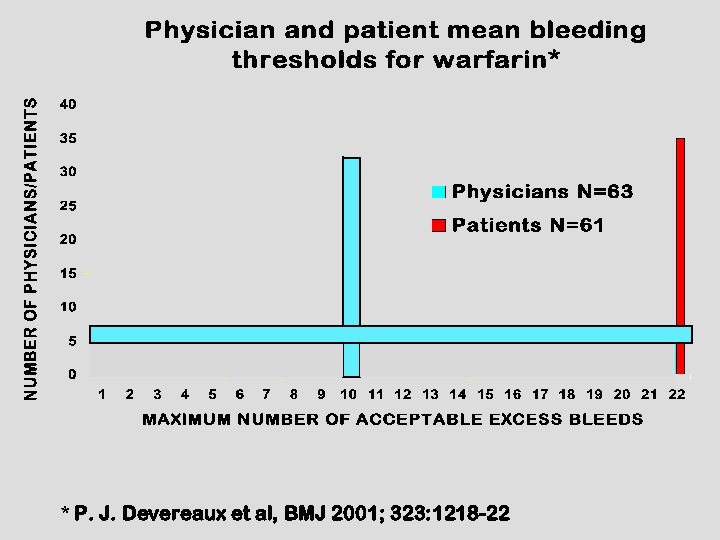
* P. J. Devereaux et al, BMJ 2001; 323: 1218 -22
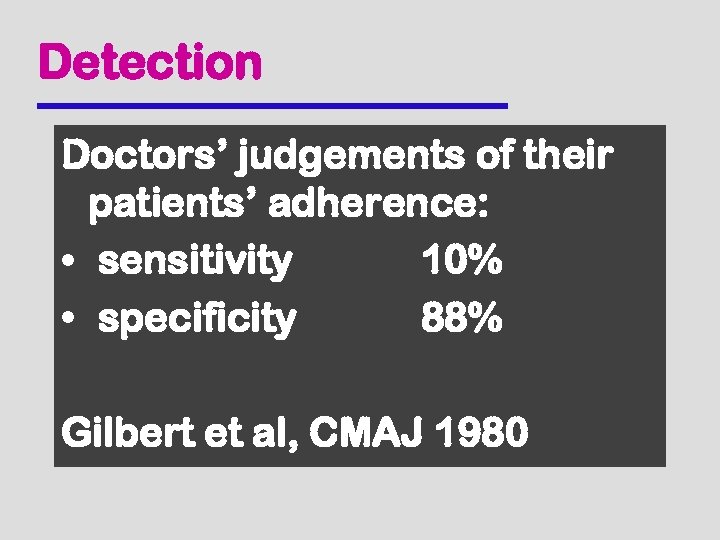
Detection Doctors’ judgements of their patients’ adherence: • sensitivity 10% • specificity 88% Gilbert et al, CMAJ 1980
Patient Adherence
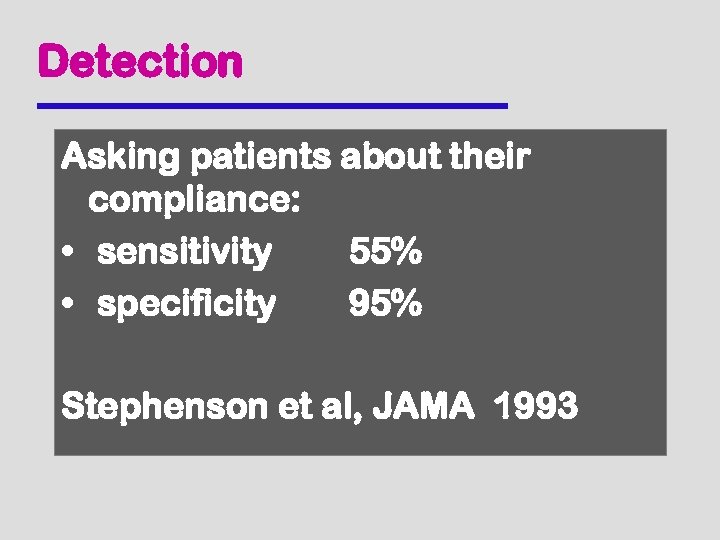
Detection Asking patients about their compliance: • sensitivity 55% • specificity 95% Stephenson et al, JAMA 1993
Patient adherence - definition. . . extent to which a person's behavior (in terms of taking medication, following a diet, modifying habits or attending clinics) coincides with medical or health advice = patient compliance ≠ concordance (…with agreed recommendations, WHO)
The age-old adherence dilemma. . . “There’s many a slip twixt the cup and the lip. ”
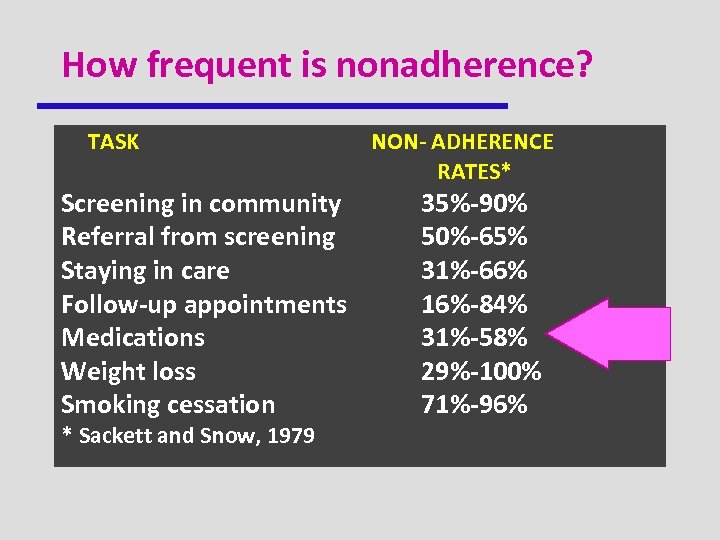
How frequent is nonadherence? TASK Screening in community Referral from screening Staying in care Follow-up appointments Medications Weight loss Smoking cessation * Sackett and Snow, 1979 NON- ADHERENCE RATES* 35%-90% 50%-65% 31%-66% 16%-84% 31%-58% 29%-100% 71%-96%
The new adherence dilemma. . . l There are many more efficacious, self-administered treatments now l Our ability to help patients follow their treatments has not kept pace l Thus, the gap between how healthy people could be and how healthy they are has widened a lot
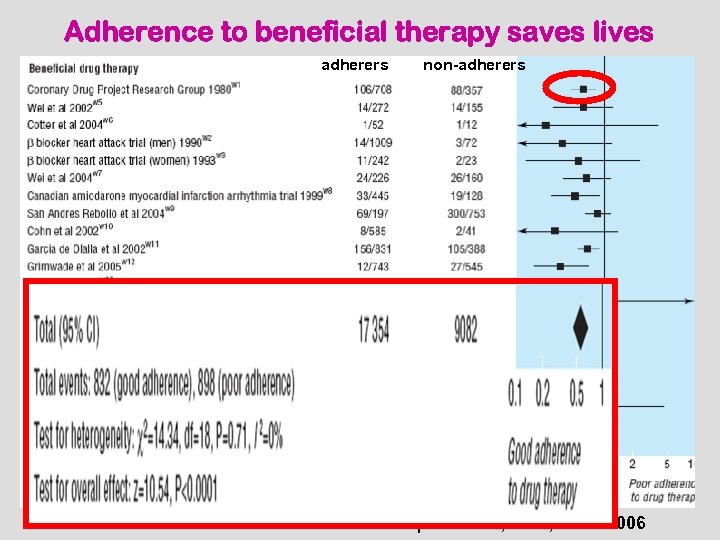
Adherence to beneficial therapy saves lives adherers non-adherers Simpson et al, BMJ, June 2006
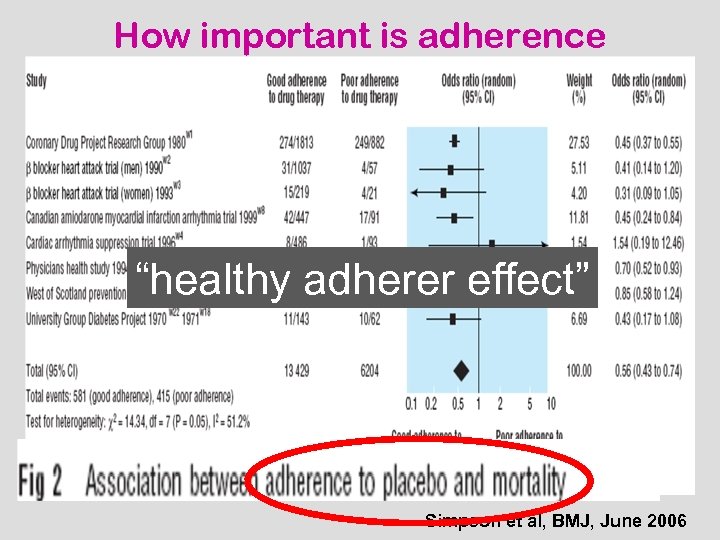
How important is adherence “healthy adherer effect” Simpson et al, BMJ, June 2006
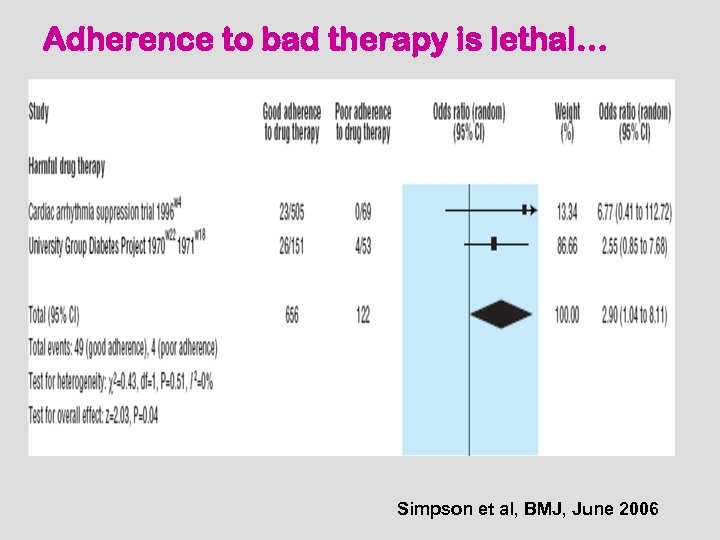
Adherence to bad therapy is lethal… Simpson et al, BMJ, June 2006
Interventions to Improve Compliance with Prescribed Medications: A Systematic Review Brian Haynes Elizabeth Ackloo Navdeep Sahota Aqeel Degani Cochrane Database of Systematic Reviews , April 2008
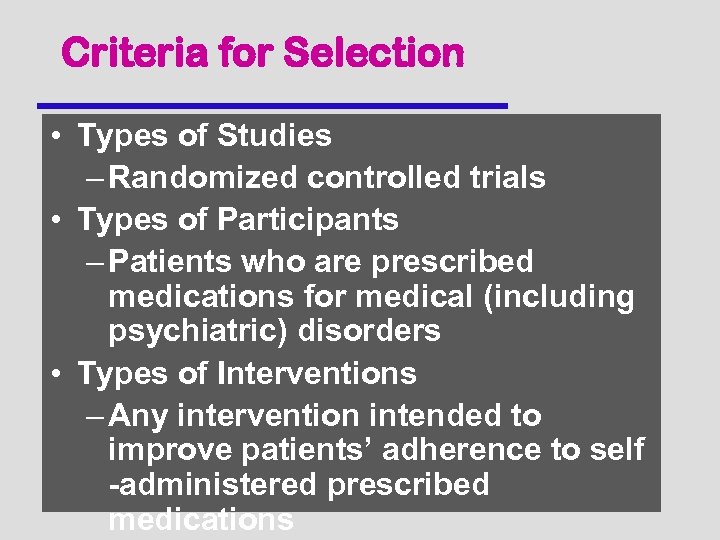
Criteria for Selection • Types of Studies – Randomized controlled trials • Types of Participants – Patients who are prescribed medications for medical (including psychiatric) disorders • Types of Interventions – Any intervention intended to improve patients’ adherence to self -administered prescribed medications
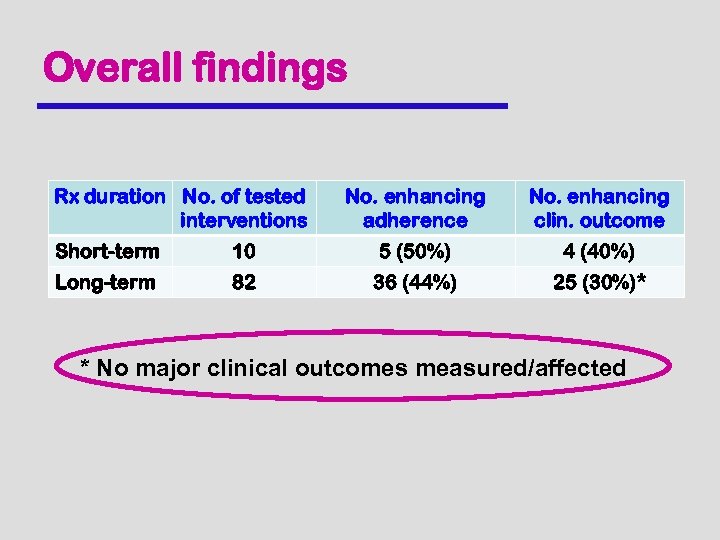
Overall findings Rx duration No. of tested interventions No. enhancing adherence No. enhancing clin. outcome Short-term 10 5 (50%) 4 (40%) Long-term 82 36 (44%) 25 (30%)* * No major clinical outcomes measured/affected
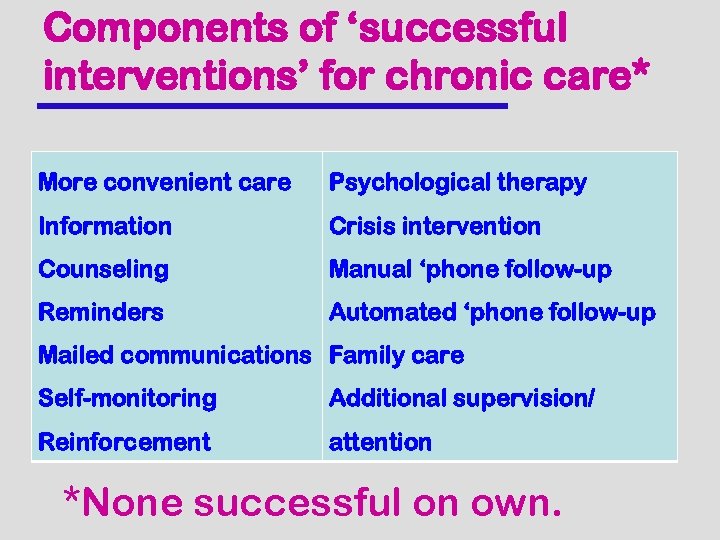
Components of ‘successful interventions’ for chronic care* More convenient care Psychological therapy Information Crisis intervention Counseling Manual ‘phone follow-up Reminders Automated ‘phone follow-up Mailed communications Family care Self-monitoring Additional supervision/ Reinforcement attention *None successful on own.
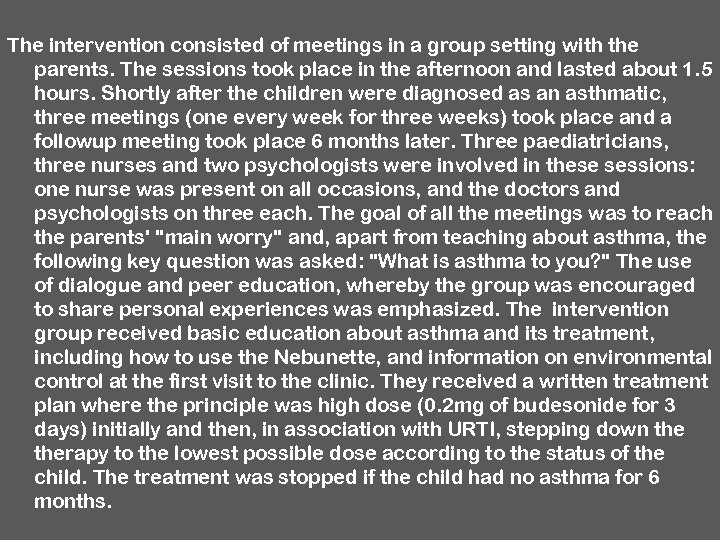
The intervention consisted of meetings in a group setting with the parents. The sessions took place in the afternoon and lasted about 1. 5 hours. Shortly after the children were diagnosed as an asthmatic, three meetings (one every week for three weeks) took place and a followup meeting took place 6 months later. Three paediatricians, three nurses and two psychologists were involved in these sessions: one nurse was present on all occasions, and the doctors and psychologists on three each. The goal of all the meetings was to reach the parents' "main worry" and, apart from teaching about asthma, the following key question was asked: "What is asthma to you? " The use of dialogue and peer education, whereby the group was encouraged to share personal experiences was emphasized. The intervention group received basic education about asthma and its treatment, including how to use the Nebunette, and information on environmental control at the first visit to the clinic. They received a written treatment plan where the principle was high dose (0. 2 mg of budesonide for 3 days) initially and then, in association with URTI, stepping down therapy to the lowest possible dose according to the status of the child. The treatment was stopped if the child had no asthma for 6 months.
Problems with the research… • Many studies too small to detect a benefit (need about 50 per group to detect a 25% absolute difference in adherence with 80% power)
Problems with the research. . . The research is l fragmented l weak l noncumulative l unimaginative l impractical l often atheoretical or hypotheoretical Most research is done by “amateurs”
Knowledge of hypertension bore no relationship to compliance either at the beginning of the study (r = -0. 03) or at 6 months (r=0. 08) Those who mastered the knowledge fared no better than those who did not. …socially unacceptable! (but highly reproducible…)
Problems with the research… • Measures of adherence are imprecise • Measures of outcomes are intermediate at best (eg blood pressure; viral load) • Follow-up too short/not repeated postintervention
Conclusions • Low adherence is a major health problem (and can be fatal) • Research documents the limited effects of interventions to date • Interventions that have some effect are typically complex and “labour intensive” (= expensive) • More and better research is needed!
What to do: Priorities for advancing adherence (international panel)* • Simple, feasible interventions (for *both* clinicians and patients) • Improved theory/development through conjoint efforts of medical, pharma, social and ‘technical’ scientists * Van Dulmen et al. BMC Health Services Research 2008, 8: 47
What to do: Priorities for advancing adherence (international panel)* • Involve patient groups • Focus efforts on non-adherent patients • Focus theory development on improving adherence (rather than explaining it) * Van Dulmen et al. BMC Health Services Research 2008, 8: 47
We need to innovate… • across disciplines • along the path of care • across diseases
We need better treatments…the “polypill bar”
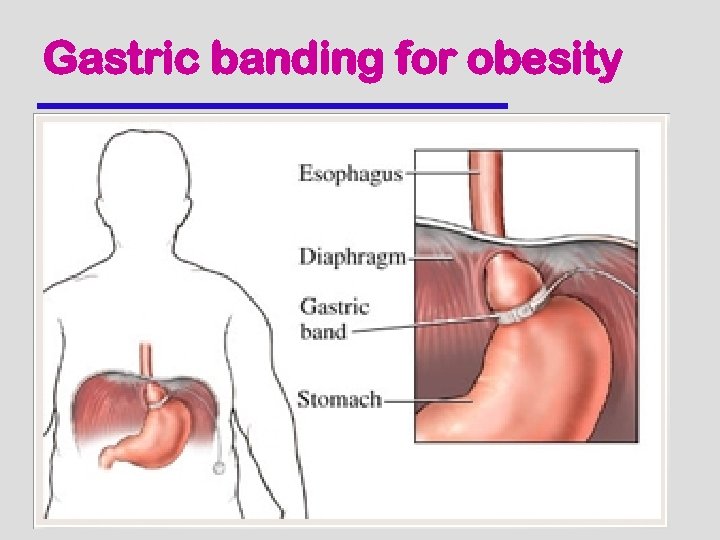
Gastric banding for obesity
Combined practitioner-patient interventions eg Diabetes In-CHARGE (with H Gerstein and D Hunt) • People with type 2 diabetes complete a brief questionnaire • They receive a set of the current diabetes care recommendations that match their condition • With patient consent, a copy goes to their family physician

d40587dbe54e6c72fb450e0b5448fe1a.ppt