0fef09b44b04586f05e339bd67d9a2da.ppt
- Количество слайдов: 31
Keys to Communicating with Patients about Obesity
Overview • Sociocultural context • Anti-fat attitudes • Starting the conversation • Managing unrealistic expectations
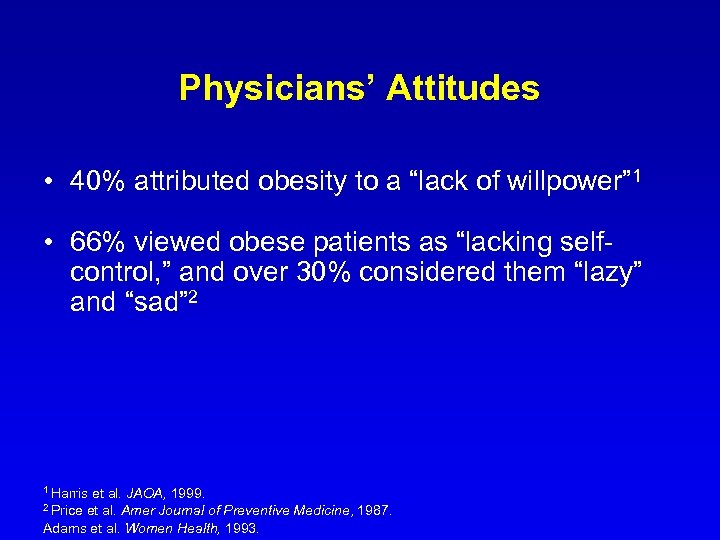
Physicians’ Attitudes • 40% attributed obesity to a “lack of willpower” 1 • 66% viewed obese patients as “lacking selfcontrol, ” and over 30% considered them “lazy” and “sad” 2 1 Harris et al. JAOA, 1999. et al. Amer Journal of Preventive Medicine, 1987. Adams et al. Women Health, 1993. 2 Price
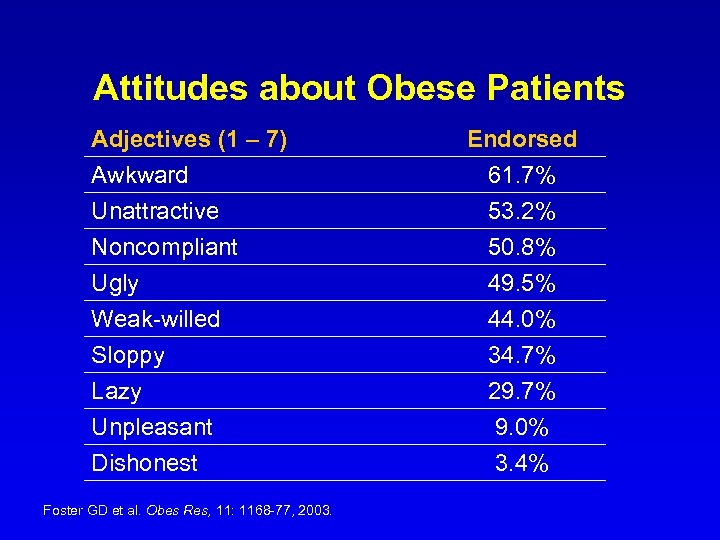
Attitudes about Obese Patients Adjectives (1 – 7) Awkward Unattractive Noncompliant Ugly Weak-willed Sloppy Lazy Unpleasant Dishonest Foster GD et al. Obes Res, 11: 1168 -77, 2003. Endorsed 61. 7% 53. 2% 50. 8% 49. 5% 44. 0% 34. 7% 29. 7% 9. 0% 3. 4%
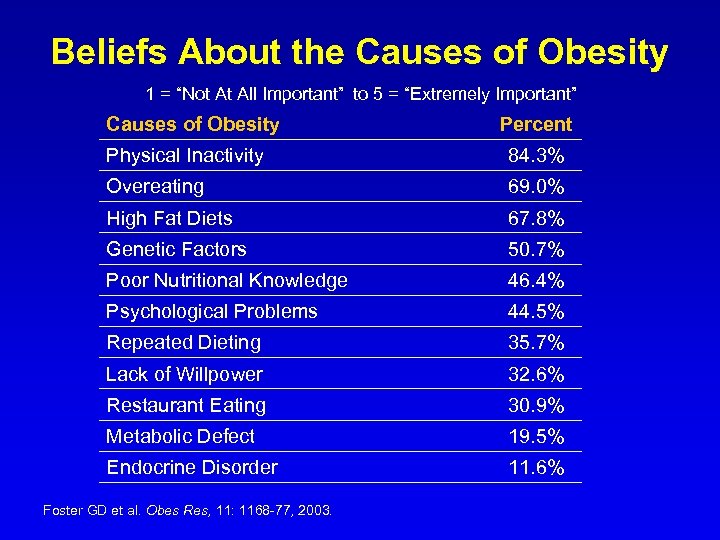
Beliefs About the Causes of Obesity 1 = “Not At All Important” to 5 = “Extremely Important” Causes of Obesity Percent Physical Inactivity 84. 3% Overeating 69. 0% High Fat Diets 67. 8% Genetic Factors 50. 7% Poor Nutritional Knowledge 46. 4% Psychological Problems 44. 5% Repeated Dieting 35. 7% Lack of Willpower 32. 6% Restaurant Eating 30. 9% Metabolic Defect 19. 5% Endocrine Disorder 11. 6% Foster GD et al. Obes Res, 11: 1168 -77, 2003.
Patient Attitudes Toward Physician Treatment of Obesity • 88% of obese patients seeking bariatric surgery reported always or usually being treated disrespectfully by the medical profession Rand & Mac. Gregor. Southern Medical Journal, 1990.
Patient Attitudes Toward Physician Treatment of Obesity • Physicians’ negative attitudes toward obesity contribute to obese patients’ avoidance of seeking routine, preventive medical care • Reasons given by obese patients for such avoidance include: insensitive comments about weight, physician disapproval of patient size and being made to feel that weight is their most important characteristic Robinson et al. JABFP, 1995.
Managing Your Own Attitudes • Acknowledge them • Be aware of likely triggers • Discuss feelings with your colleagues
Likely Triggers • Behaviors/attitudes that approximate the stereotype • Factors leading to decreased tolerance • Unwanted clinical outcomes
Making the Office Environment Receptive • Have gowns available that fit larger patients • Buy a scale that can weigh all of your patients • Use larger blood pressure cuffs when appropriate • Provide some armless chairs in the waiting room • Include the whole office team
Talking about Obesity • Few physicians talk about obesity • Futility and avoidance (Frank, JAMA 1993) • Limitations of the busy practice environment
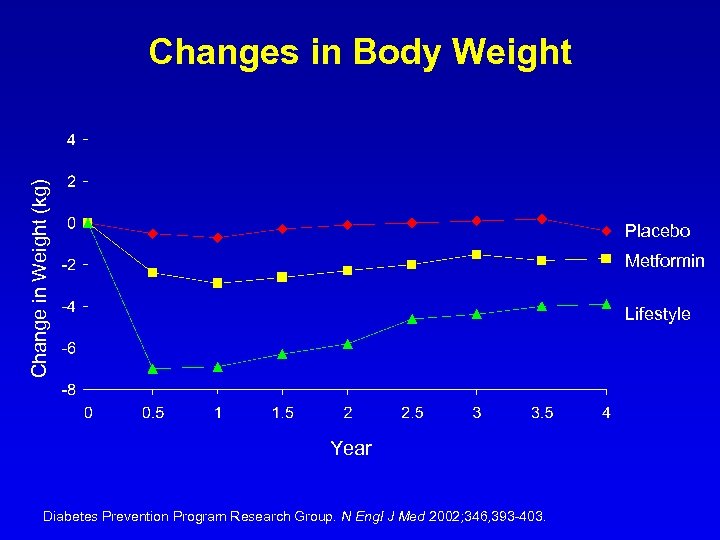
Change in Weight (kg) Changes in Body Weight Placebo Metformin Lifestyle Year Diabetes Prevention Program Research Group. N Engl J Med 2002; 346, 393 -403.
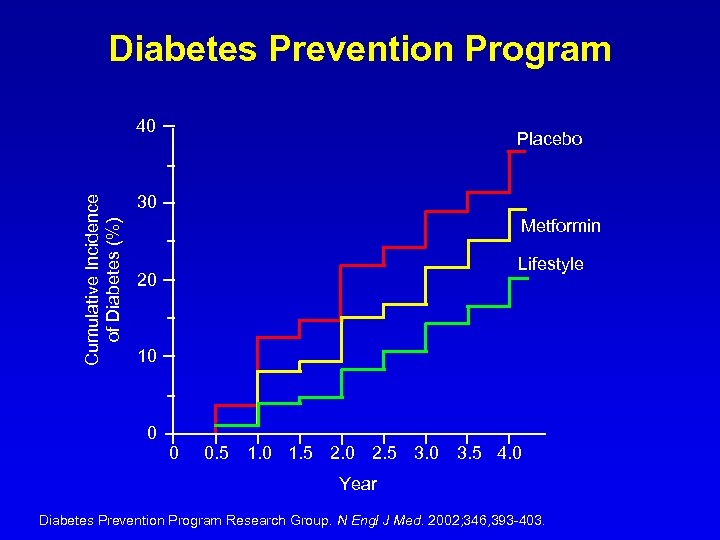
Diabetes Prevention Program Cumulative Incidence of Diabetes (%) 40 Placebo 30 Metformin Lifestyle 20 10 0 0 0. 5 1. 0 1. 5 2. 0 2. 5 3. 0 3. 5 4. 0 Year Diabetes Prevention Program Research Group. N Engl J Med. 2002; 346, 393 -403.
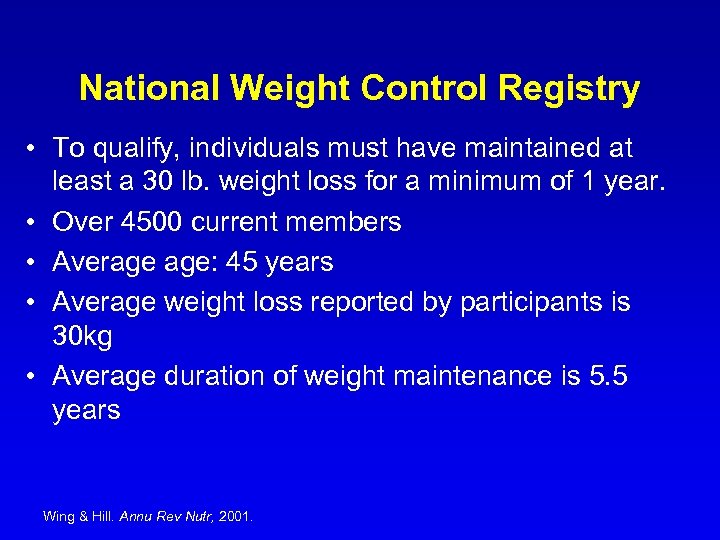
National Weight Control Registry • To qualify, individuals must have maintained at least a 30 lb. weight loss for a minimum of 1 year. • Over 4500 current members • Average age: 45 years • Average weight loss reported by participants is 30 kg • Average duration of weight maintenance is 5. 5 years Wing & Hill. Annu Rev Nutr, 2001.
Thin for Life by Anne M. Fletcher, M. S. , R. D. • Shares techniques of people who have succeeded in keeping weight off for good • Refutes the popular notion that losing weight permanently is hopeless
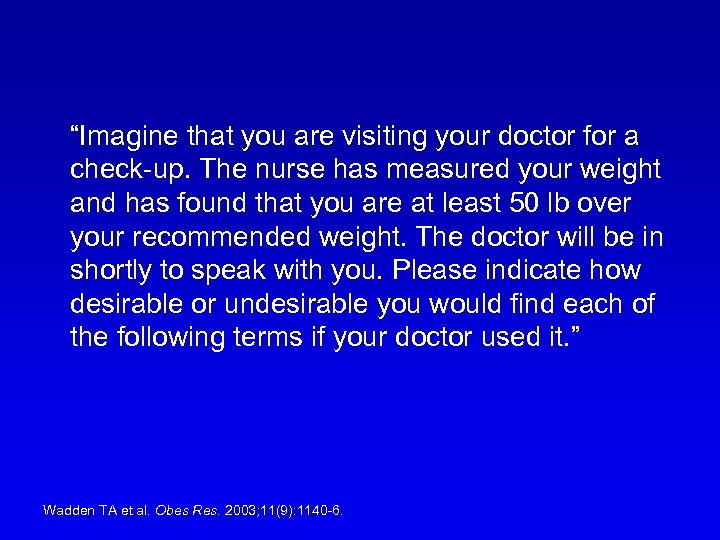
“Imagine that you are visiting your doctor for a check-up. The nurse has measured your weight and has found that you are at least 50 lb over your recommended weight. The doctor will be in shortly to speak with you. Please indicate how desirable or undesirable you would find each of the following terms if your doctor used it. ” Wadden TA et al. Obes Res. 2003; 11(9): 1140 -6.
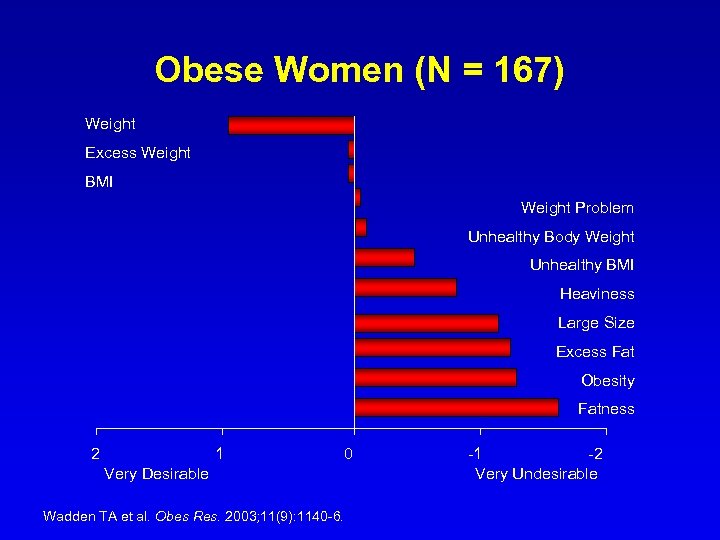
Obese Women (N = 167) Weight Excess Weight BMI Weight Problem Unhealthy Body Weight Unhealthy BMI Heaviness Large Size Excess Fat Obesity Fatness 2 1 0 Very Desirable Wadden TA et al. Obes Res. 2003; 11(9): 1140 -6. -1 -2 Very Undesirable
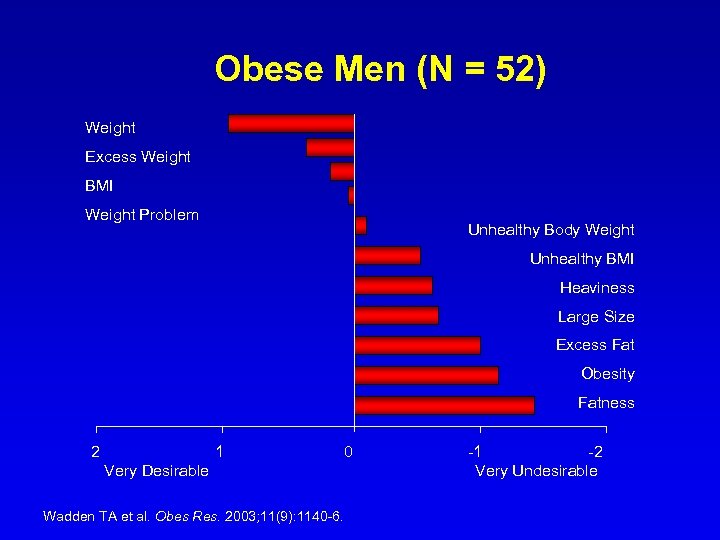
Obese Men (N = 52) Weight Excess Weight BMI Weight Problem Unhealthy Body Weight Unhealthy BMI Heaviness Large Size Excess Fat Obesity Fatness 2 1 0 Very Desirable Wadden TA et al. Obes Res. 2003; 11(9): 1140 -6. -1 -2 Very Undesirable
Assessing Readiness • • • Why now? What changes will you have to make? What will change if you lose weight? What do others think about your weight? What else is going on in your life?
Assessing Readiness • We are not good at predicting outcomes. • Patients ultimately make the decision. • Providers assess costs/benefits in a variety of contexts.
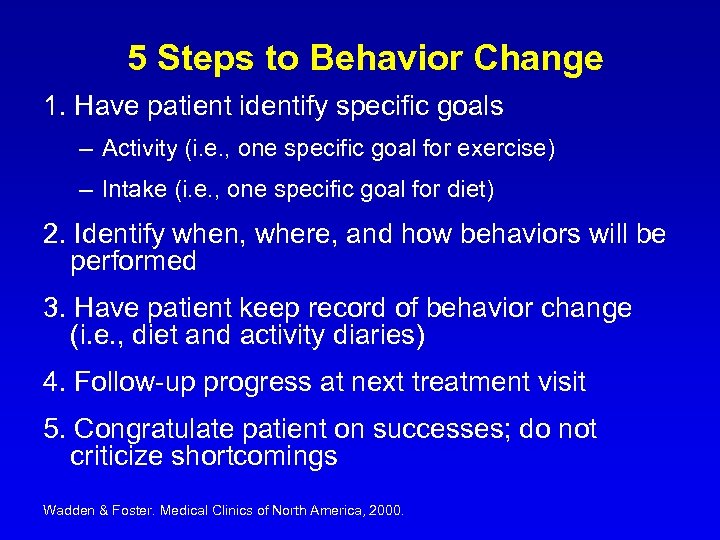
5 Steps to Behavior Change 1. Have patient identify specific goals – Activity (i. e. , one specific goal for exercise) – Intake (i. e. , one specific goal for diet) 2. Identify when, where, and how behaviors will be performed 3. Have patient keep record of behavior change (i. e. , diet and activity diaries) 4. Follow-up progress at next treatment visit 5. Congratulate patient on successes; do not criticize shortcomings Wadden & Foster. Medical Clinics of North America, 2000.
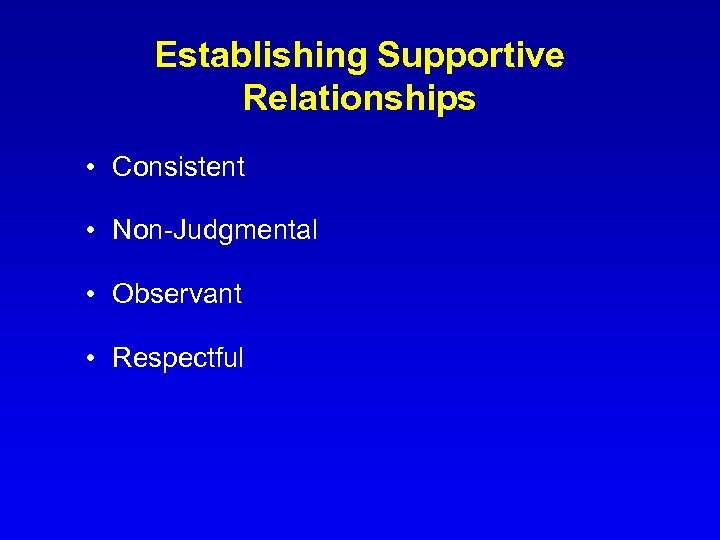
Establishing Supportive Relationships • Consistent • Non-Judgmental • Observant • Respectful
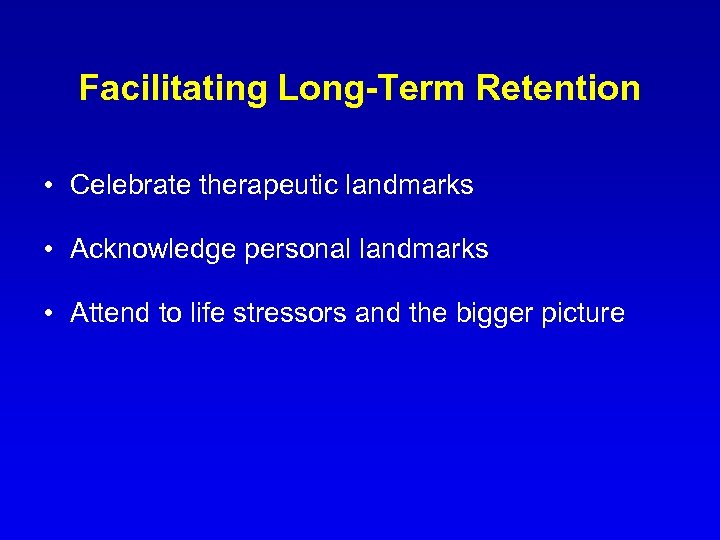
Facilitating Long-Term Retention • Celebrate therapeutic landmarks • Acknowledge personal landmarks • Attend to life stressors and the bigger picture
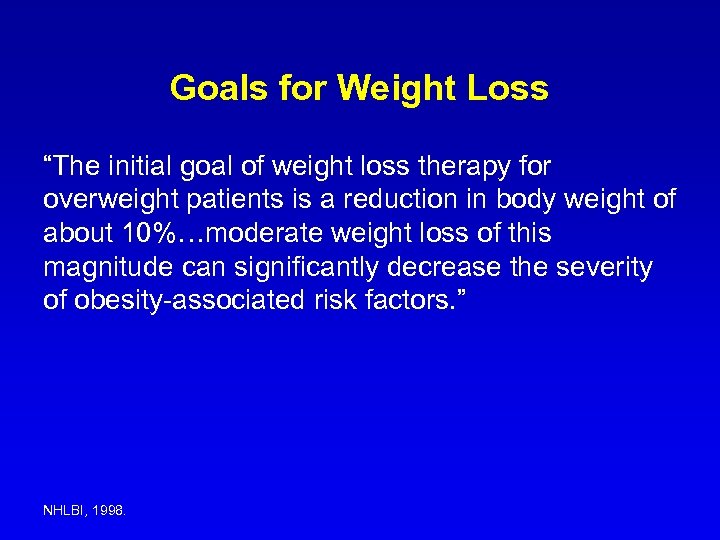
Goals for Weight Loss “The initial goal of weight loss therapy for overweight patients is a reduction in body weight of about 10%…moderate weight loss of this magnitude can significantly decrease the severity of obesity-associated risk factors. ” NHLBI, 1998.
Study Design Subjects: 60 obese women 40. 0 ± 8. 7 years 99. 1 ± 12. 3 kg BMI = 36. 3 ± 4. 3 kg/m 2
Goal Weights • Averaged 32% reduction in body weight • Three times greater than the goals recommended by the National Academy of Science and Department of Agriculture • Greatly exceeds weight losses of nonsurgical treatments
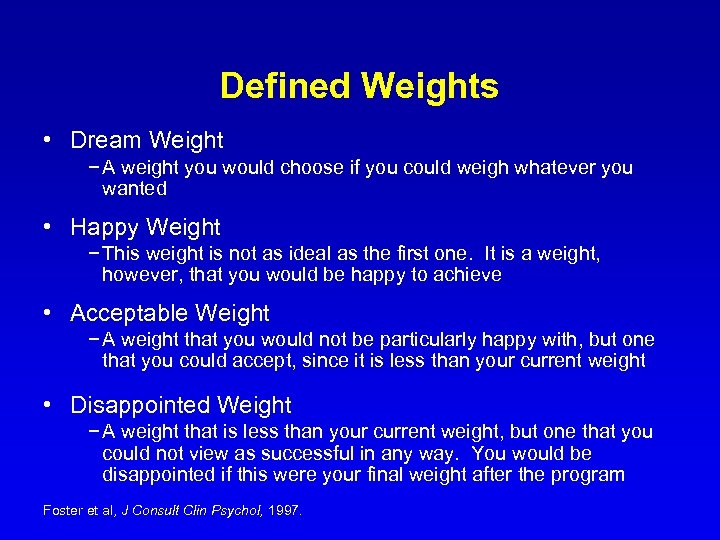
Defined Weights • Dream Weight − A weight you would choose if you could weigh whatever you wanted • Happy Weight − This weight is not as ideal as the first one. It is a weight, however, that you would be happy to achieve • Acceptable Weight − A weight that you would not be particularly happy with, but one that you could accept, since it is less than your current weight • Disappointed Weight − A weight that is less than your current weight, but one that you could not view as successful in any way. You would be disappointed if this were your final weight after the program Foster et al, J Consult Clin Psychol, 1997.
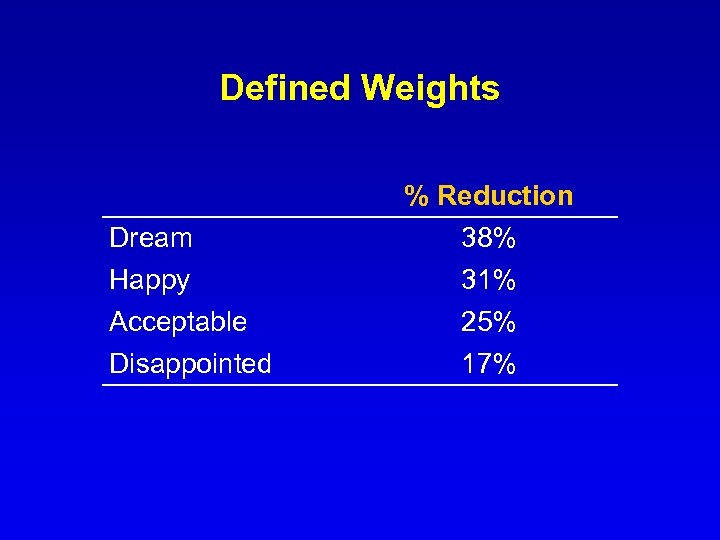
Defined Weights Dream Happy Acceptable Disappointed % Reduction 38% 31% 25% 17%
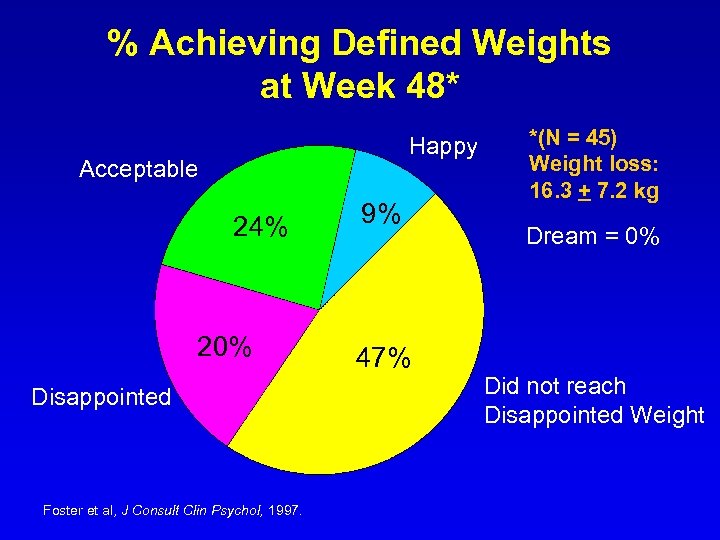
% Achieving Defined Weights at Week 48* Happy Acceptable 24% 20% Disappointed Foster et al, J Consult Clin Psychol, 1997. 9% 47% *(N = 45) Weight loss: 16. 3 + 7. 2 kg Dream = 0% Did not reach Disappointed Weight
Helping Patients Accept More Modest Weight Losses • Be clear about what treatment can do and what it cannot do • Discuss biological limits • Focus on non-weight outcomes
“As with any chronic illness, we rarely have an opportunity to cure. But we do have an opportunity to treat the patient with respect. Such an experience may be the greatest gift that a doctor can give an obese patient; it compares favorably with the modest benefits of our program of weight reduction. ” Albert J. Stunkard, MD Obesity: Theory and Therapy, 1993; Lippincott-Raven.
0fef09b44b04586f05e339bd67d9a2da.ppt