51f52338339912e8003b849f19e70dff.ppt
- Количество слайдов: 63
 KEY CONCEPTS IN ACUTE PAIN MANAGEMENT - 2 SURGERY RESIDENTS John Penning MD FRCPC Director Acute Pain Service The Ottawa Hospital Nov. 15, 2011
KEY CONCEPTS IN ACUTE PAIN MANAGEMENT - 2 SURGERY RESIDENTS John Penning MD FRCPC Director Acute Pain Service The Ottawa Hospital Nov. 15, 2011
 Objectives n n Review the “new” acute pain ladder When step # 3 on the ladder isn’t working? – Pronociception, glial activation? ? – Role of anti-hyperalgesic drugs n n Fundamentals of IV PCA What is an epidural anyway? Epidural pitfalls for the surgeon Review principles discussed by case presentation – Opioid tolerance, conversion from IV to PO – When, how to use naloxone – Assessing the hypotensive epidural patient
Objectives n n Review the “new” acute pain ladder When step # 3 on the ladder isn’t working? – Pronociception, glial activation? ? – Role of anti-hyperalgesic drugs n n Fundamentals of IV PCA What is an epidural anyway? Epidural pitfalls for the surgeon Review principles discussed by case presentation – Opioid tolerance, conversion from IV to PO – When, how to use naloxone – Assessing the hypotensive epidural patient
 Multi-modal Analgesia Orders n Celecoxib 100 – 200 mg PO Q 12 H or n Naproxen 250 – 375 mg PO Q 8 H Available OTC as “Aleve” 220 mg n n n Acetaminophen 650 mg PO Q 4 H Tramadol 25 – 50 – 75 mg PO Q 4 H prn Hydromorphone 1 – 2 mg PO Q 4 H prn To supplement Tramadol if required
Multi-modal Analgesia Orders n Celecoxib 100 – 200 mg PO Q 12 H or n Naproxen 250 – 375 mg PO Q 8 H Available OTC as “Aleve” 220 mg n n n Acetaminophen 650 mg PO Q 4 H Tramadol 25 – 50 – 75 mg PO Q 4 H prn Hydromorphone 1 – 2 mg PO Q 4 H prn To supplement Tramadol if required
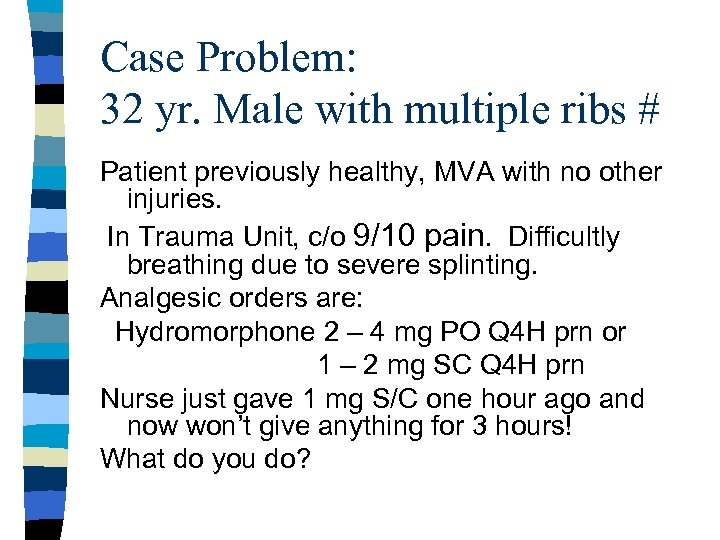 Case Problem: 32 yr. Male with multiple ribs # Patient previously healthy, MVA with no other injuries. In Trauma Unit, c/o 9/10 pain. Difficultly breathing due to severe splinting. Analgesic orders are: Hydromorphone 2 – 4 mg PO Q 4 H prn or 1 – 2 mg SC Q 4 H prn Nurse just gave 1 mg S/C one hour ago and now won’t give anything for 3 hours! What do you do?
Case Problem: 32 yr. Male with multiple ribs # Patient previously healthy, MVA with no other injuries. In Trauma Unit, c/o 9/10 pain. Difficultly breathing due to severe splinting. Analgesic orders are: Hydromorphone 2 – 4 mg PO Q 4 H prn or 1 – 2 mg SC Q 4 H prn Nurse just gave 1 mg S/C one hour ago and now won’t give anything for 3 hours! What do you do?
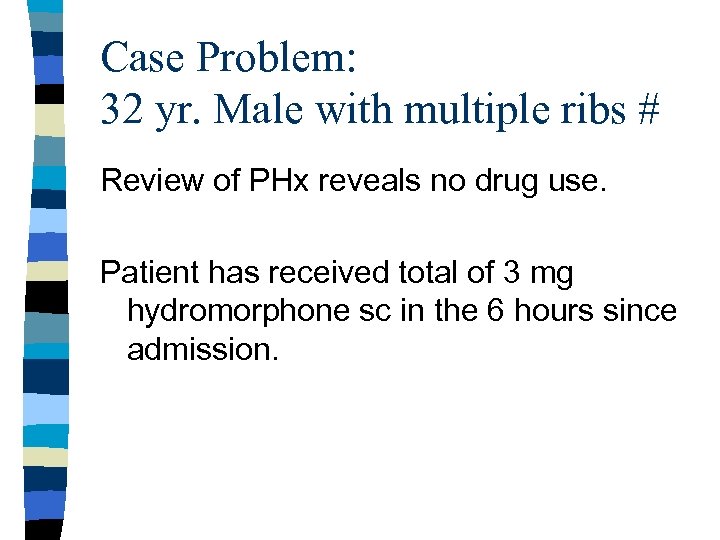 Case Problem: 32 yr. Male with multiple ribs # Review of PHx reveals no drug use. Patient has received total of 3 mg hydromorphone sc in the 6 hours since admission.
Case Problem: 32 yr. Male with multiple ribs # Review of PHx reveals no drug use. Patient has received total of 3 mg hydromorphone sc in the 6 hours since admission.
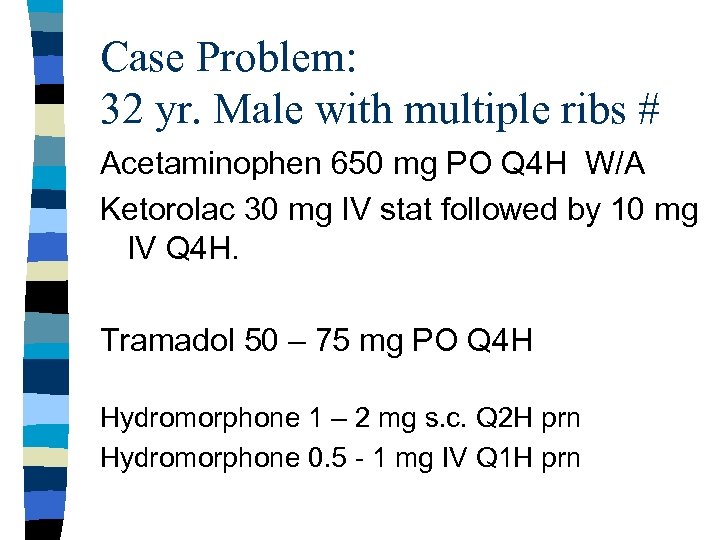 Case Problem: 32 yr. Male with multiple ribs # Acetaminophen 650 mg PO Q 4 H W/A Ketorolac 30 mg IV stat followed by 10 mg IV Q 4 H. Tramadol 50 – 75 mg PO Q 4 H Hydromorphone 1 – 2 mg s. c. Q 2 H prn Hydromorphone 0. 5 - 1 mg IV Q 1 H prn
Case Problem: 32 yr. Male with multiple ribs # Acetaminophen 650 mg PO Q 4 H W/A Ketorolac 30 mg IV stat followed by 10 mg IV Q 4 H. Tramadol 50 – 75 mg PO Q 4 H Hydromorphone 1 – 2 mg s. c. Q 2 H prn Hydromorphone 0. 5 - 1 mg IV Q 1 H prn
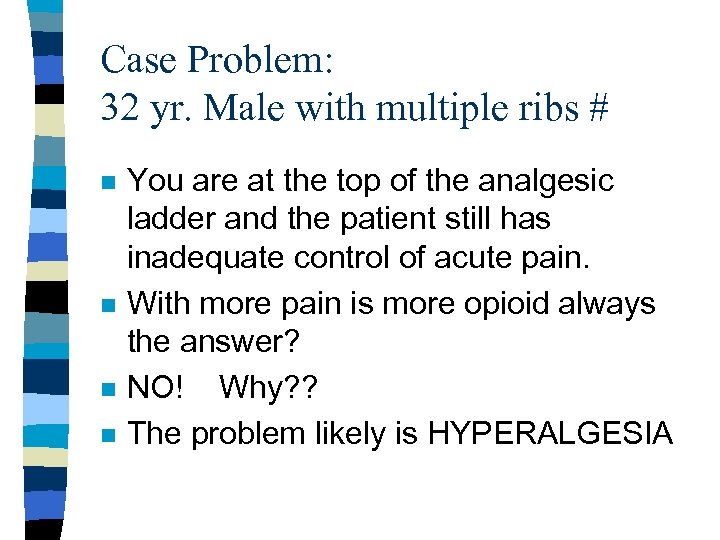 Case Problem: 32 yr. Male with multiple ribs # n n You are at the top of the analgesic ladder and the patient still has inadequate control of acute pain. With more pain is more opioid always the answer? NO! Why? ? The problem likely is HYPERALGESIA
Case Problem: 32 yr. Male with multiple ribs # n n You are at the top of the analgesic ladder and the patient still has inadequate control of acute pain. With more pain is more opioid always the answer? NO! Why? ? The problem likely is HYPERALGESIA
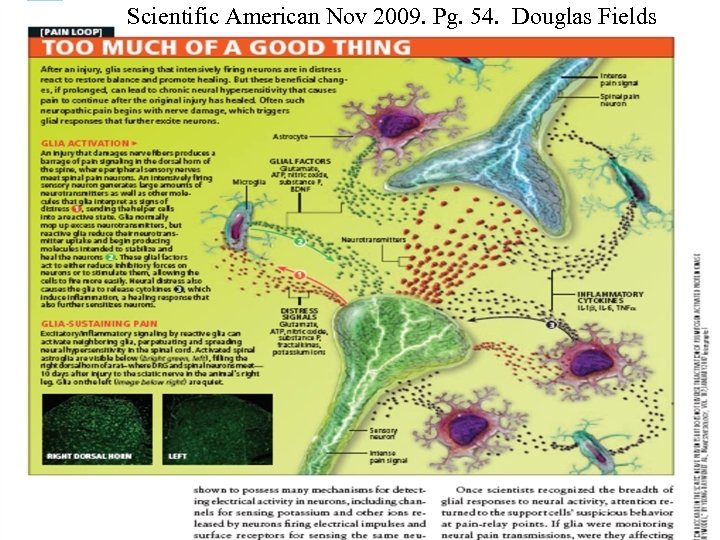 Scientific American Nov 2009. Pg. 54. Douglas Fields
Scientific American Nov 2009. Pg. 54. Douglas Fields
 E = MC 2
E = MC 2
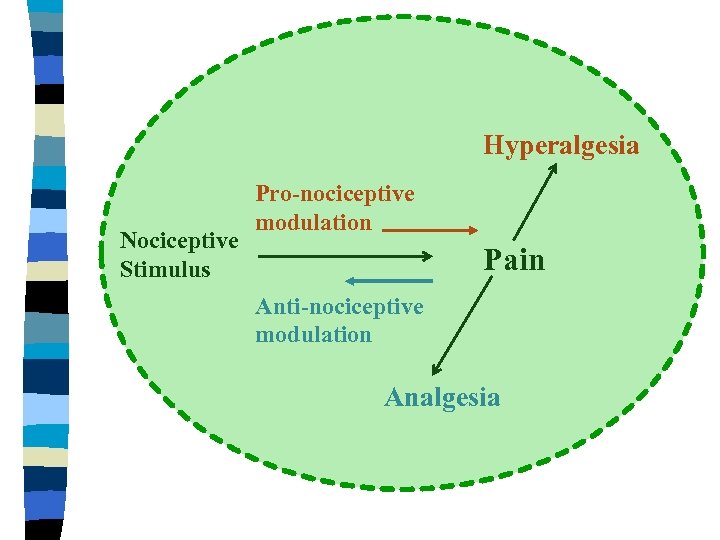 Hyperalgesia Nociceptive Stimulus Pro-nociceptive modulation Pain Anti-nociceptive modulation Analgesia
Hyperalgesia Nociceptive Stimulus Pro-nociceptive modulation Pain Anti-nociceptive modulation Analgesia
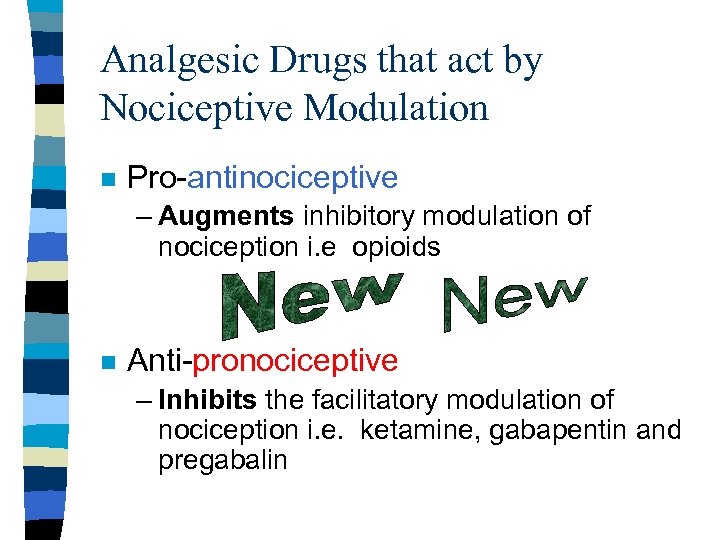 Analgesic Drugs that act by Nociceptive Modulation n Pro-antinociceptive – Augments inhibitory modulation of nociception i. e opioids n Anti-pronociceptive – Inhibits the facilitatory modulation of nociception i. e. ketamine, gabapentin and pregabalin
Analgesic Drugs that act by Nociceptive Modulation n Pro-antinociceptive – Augments inhibitory modulation of nociception i. e opioids n Anti-pronociceptive – Inhibits the facilitatory modulation of nociception i. e. ketamine, gabapentin and pregabalin
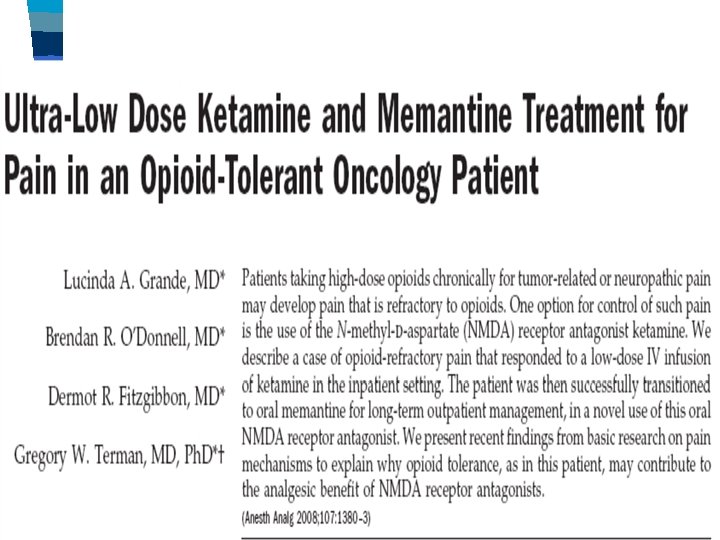
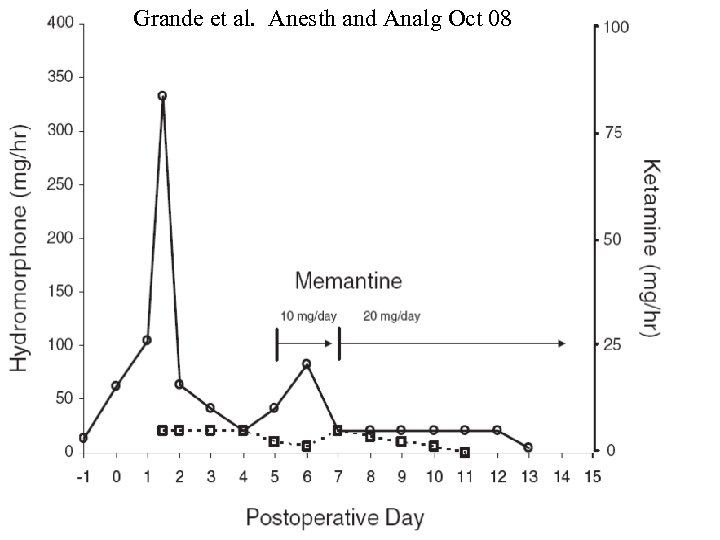 Grande et al. Anesth and Analg Oct 08
Grande et al. Anesth and Analg Oct 08
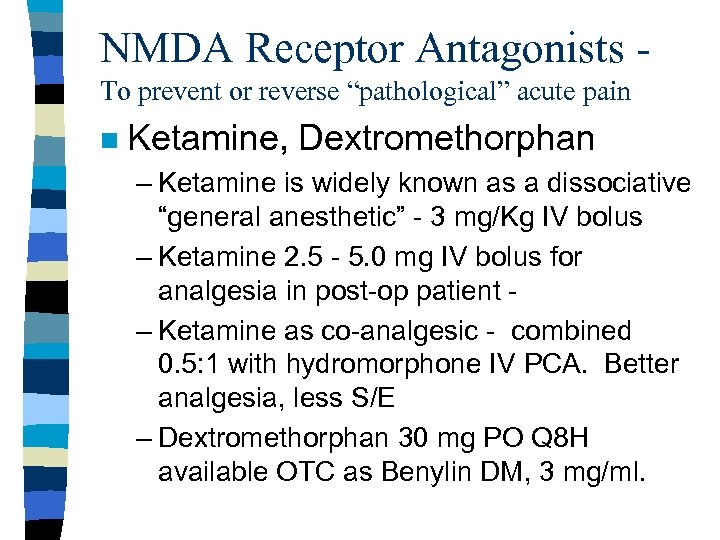 NMDA Receptor Antagonists To prevent or reverse “pathological” acute pain n Ketamine, Dextromethorphan – Ketamine is widely known as a dissociative “general anesthetic” - 3 mg/Kg IV bolus – Ketamine 2. 5 - 5. 0 mg IV bolus for analgesia in post-op patient – Ketamine as co-analgesic - combined 0. 5: 1 with hydromorphone IV PCA. Better analgesia, less S/E – Dextromethorphan 30 mg PO Q 8 H available OTC as Benylin DM, 3 mg/ml.
NMDA Receptor Antagonists To prevent or reverse “pathological” acute pain n Ketamine, Dextromethorphan – Ketamine is widely known as a dissociative “general anesthetic” - 3 mg/Kg IV bolus – Ketamine 2. 5 - 5. 0 mg IV bolus for analgesia in post-op patient – Ketamine as co-analgesic - combined 0. 5: 1 with hydromorphone IV PCA. Better analgesia, less S/E – Dextromethorphan 30 mg PO Q 8 H available OTC as Benylin DM, 3 mg/ml.
 Case Problem: 32 yr. Male with multiple ribs # IV PCA with hydromorphone / ketamine Ketorolac changed to naproxen when eating. 250 mg PO Q 8 H Or Celecoxib 200 mg PO Q 12 H for 5 days then 100 mg Q 12 H until no longer needed.
Case Problem: 32 yr. Male with multiple ribs # IV PCA with hydromorphone / ketamine Ketorolac changed to naproxen when eating. 250 mg PO Q 8 H Or Celecoxib 200 mg PO Q 12 H for 5 days then 100 mg Q 12 H until no longer needed.
 Case Problem: 32 yr. Male with multiple ribs # On day three patient is doing well and planning for D/C tomorrow. Convert to PO hydromorphone. Daily IV PCA use is 20 mg per day. Equals about 40 mg per day orally. Order about 50% as long acting. 9 mg HM Contin Q 12 H and 2 – 4 mg PO Q 4 H prn.
Case Problem: 32 yr. Male with multiple ribs # On day three patient is doing well and planning for D/C tomorrow. Convert to PO hydromorphone. Daily IV PCA use is 20 mg per day. Equals about 40 mg per day orally. Order about 50% as long acting. 9 mg HM Contin Q 12 H and 2 – 4 mg PO Q 4 H prn.
 Case Problem: 32 yr. Male with multiple ribs # Weaning instructions: As daily “breakthough” hydromorphone requirements decrease, reduce the Contin dose by 25% increments. HM The NSAID or coxib is D/C after the opioids D/C Acetaminophen is last to be D/C
Case Problem: 32 yr. Male with multiple ribs # Weaning instructions: As daily “breakthough” hydromorphone requirements decrease, reduce the Contin dose by 25% increments. HM The NSAID or coxib is D/C after the opioids D/C Acetaminophen is last to be D/C
 Analgesic Drugs that act by Nociceptive Modulation n Anti-pronociceptive – Inhibits the facilitatory modulation of nociception i. e. ketamine, gabapentin and pregabalin, lidocaine
Analgesic Drugs that act by Nociceptive Modulation n Anti-pronociceptive – Inhibits the facilitatory modulation of nociception i. e. ketamine, gabapentin and pregabalin, lidocaine
 Pregabalin for acute pain? n n Acute pain is “off-label” use Be cautious of Over-sedation – Sleep deprivation – Elderly – Patient already has significant opioids
Pregabalin for acute pain? n n Acute pain is “off-label” use Be cautious of Over-sedation – Sleep deprivation – Elderly – Patient already has significant opioids
 Pregabalin: The Good, The Bad and the Ugly n The Good – Chronic pain in region of surgery, when pronociceptive mechanisms play a role such as joint arthroplasty, bowel surgery in IBD patients, chronic limb ischemic pain, opioid tolerant patients n The Bad – Mild pain when simple analgesics like acetaminophen, NSAIDs or low dose opioid or tramadol suffice. n The Ugly – Too large a dose in sleep deprived patient already in state of “morphine-failure”
Pregabalin: The Good, The Bad and the Ugly n The Good – Chronic pain in region of surgery, when pronociceptive mechanisms play a role such as joint arthroplasty, bowel surgery in IBD patients, chronic limb ischemic pain, opioid tolerant patients n The Bad – Mild pain when simple analgesics like acetaminophen, NSAIDs or low dose opioid or tramadol suffice. n The Ugly – Too large a dose in sleep deprived patient already in state of “morphine-failure”
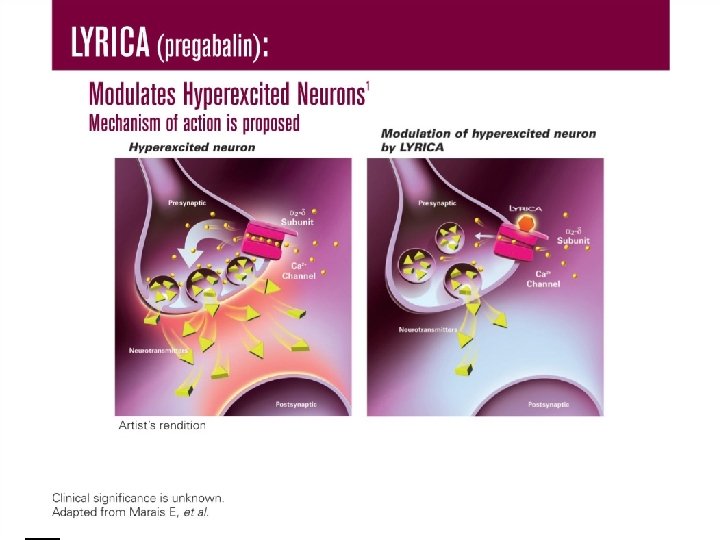
 Pregabalin dosage n This is NOT a one size fits all. – Drugs binding to receptors have considerable patient to patient variability in dose: response n n n Alpha-2 delta sub-unit of Voltage-Gated Calcium Channel 75 mg PO 2 hours pre-op (50 – 150) 50 mg PO Q 8 H for 3 to 5 days (25 – 75)
Pregabalin dosage n This is NOT a one size fits all. – Drugs binding to receptors have considerable patient to patient variability in dose: response n n n Alpha-2 delta sub-unit of Voltage-Gated Calcium Channel 75 mg PO 2 hours pre-op (50 – 150) 50 mg PO Q 8 H for 3 to 5 days (25 – 75)
 The New Challenges in Managing Acute Pain after Surgery and Trauma n The Opioid Tolerant Patient – The greatest change in practice/attitudes in the last 10 years is the now wide spread acceptance of the use of opioids for CHRONIC NON-MALIGNANT PAIN – Renders the “usual” standard “box” orders totally inadequate in these patients n Get a pre-op Anesthesia/APS consult – The Brief Pain Inventory – “BPI”
The New Challenges in Managing Acute Pain after Surgery and Trauma n The Opioid Tolerant Patient – The greatest change in practice/attitudes in the last 10 years is the now wide spread acceptance of the use of opioids for CHRONIC NON-MALIGNANT PAIN – Renders the “usual” standard “box” orders totally inadequate in these patients n Get a pre-op Anesthesia/APS consult – The Brief Pain Inventory – “BPI”
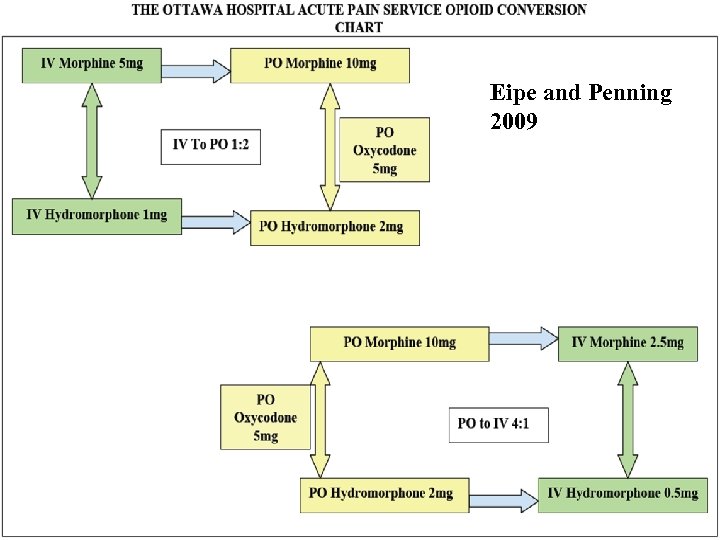 Eipe and Penning 2009
Eipe and Penning 2009
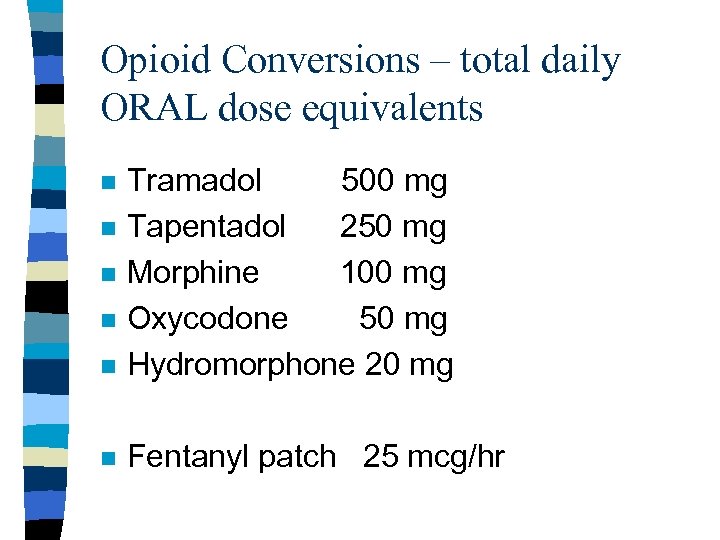 Opioid Conversions – total daily ORAL dose equivalents n Tramadol 500 mg Tapentadol 250 mg Morphine 100 mg Oxycodone 50 mg Hydromorphone 20 mg n Fentanyl patch 25 mcg/hr n n
Opioid Conversions – total daily ORAL dose equivalents n Tramadol 500 mg Tapentadol 250 mg Morphine 100 mg Oxycodone 50 mg Hydromorphone 20 mg n Fentanyl patch 25 mcg/hr n n
 The surgeon and IV PCA? n Hydromorphone opioid of choice – (0. 5 mg/ml) – Less active metabolites than morphine – Better tolerated in renal insufficiency/elderly – Safety? In setting of having both available it is better to be more familiar with HM (substitution errors) i. e. want to avoid giving HM at the morphine dose!
The surgeon and IV PCA? n Hydromorphone opioid of choice – (0. 5 mg/ml) – Less active metabolites than morphine – Better tolerated in renal insufficiency/elderly – Safety? In setting of having both available it is better to be more familiar with HM (substitution errors) i. e. want to avoid giving HM at the morphine dose!
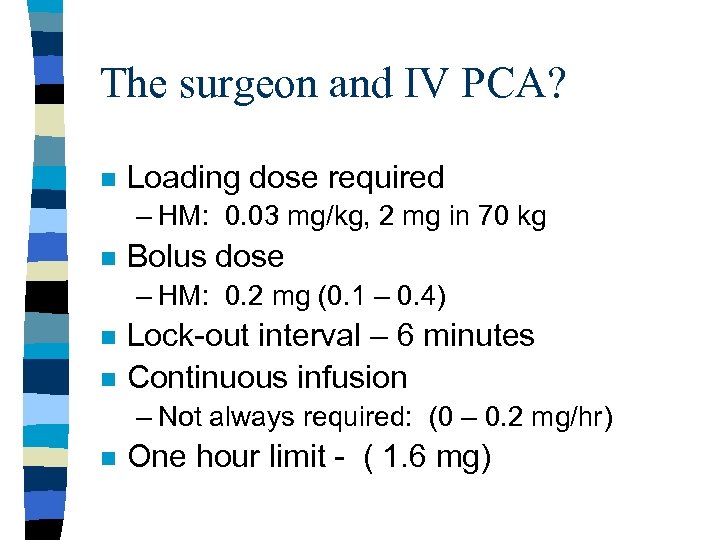 The surgeon and IV PCA? n Loading dose required – HM: 0. 03 mg/kg, 2 mg in 70 kg n Bolus dose – HM: 0. 2 mg (0. 1 – 0. 4) n n Lock-out interval – 6 minutes Continuous infusion – Not always required: (0 – 0. 2 mg/hr) n One hour limit - ( 1. 6 mg)
The surgeon and IV PCA? n Loading dose required – HM: 0. 03 mg/kg, 2 mg in 70 kg n Bolus dose – HM: 0. 2 mg (0. 1 – 0. 4) n n Lock-out interval – 6 minutes Continuous infusion – Not always required: (0 – 0. 2 mg/hr) n One hour limit - ( 1. 6 mg)
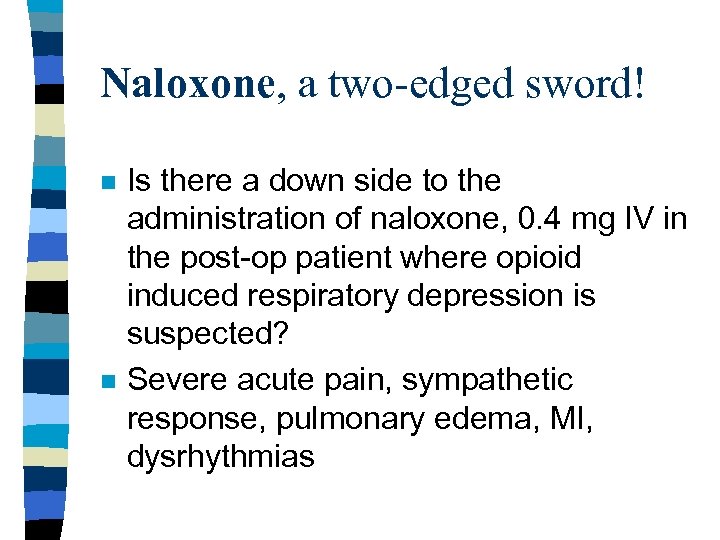 Naloxone, a two-edged sword! n n Is there a down side to the administration of naloxone, 0. 4 mg IV in the post-op patient where opioid induced respiratory depression is suspected? Severe acute pain, sympathetic response, pulmonary edema, MI, dysrhythmias
Naloxone, a two-edged sword! n n Is there a down side to the administration of naloxone, 0. 4 mg IV in the post-op patient where opioid induced respiratory depression is suspected? Severe acute pain, sympathetic response, pulmonary edema, MI, dysrhythmias
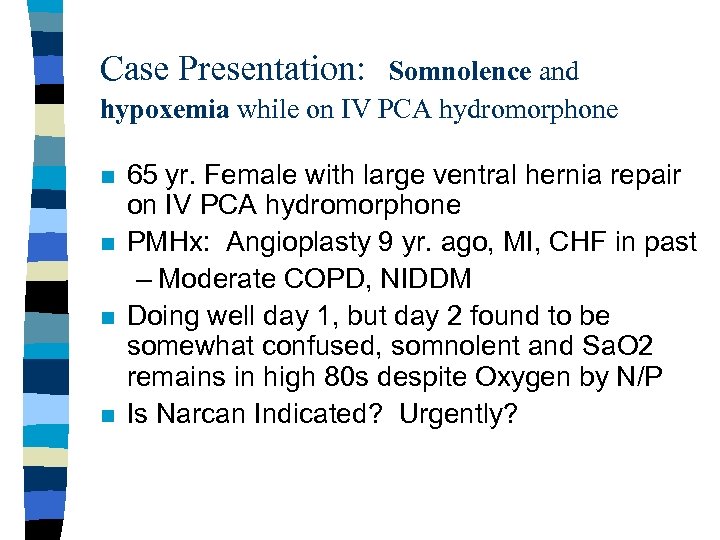 Case Presentation: Somnolence and hypoxemia while on IV PCA hydromorphone n n 65 yr. Female with large ventral hernia repair on IV PCA hydromorphone PMHx: Angioplasty 9 yr. ago, MI, CHF in past – Moderate COPD, NIDDM Doing well day 1, but day 2 found to be somewhat confused, somnolent and Sa. O 2 remains in high 80 s despite Oxygen by N/P Is Narcan Indicated? Urgently?
Case Presentation: Somnolence and hypoxemia while on IV PCA hydromorphone n n 65 yr. Female with large ventral hernia repair on IV PCA hydromorphone PMHx: Angioplasty 9 yr. ago, MI, CHF in past – Moderate COPD, NIDDM Doing well day 1, but day 2 found to be somewhat confused, somnolent and Sa. O 2 remains in high 80 s despite Oxygen by N/P Is Narcan Indicated? Urgently?
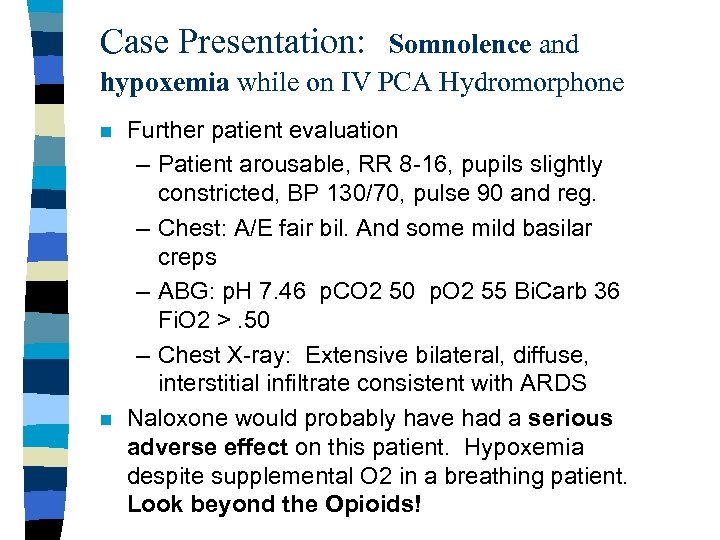 Case Presentation: Somnolence and hypoxemia while on IV PCA Hydromorphone n n Further patient evaluation – Patient arousable, RR 8 -16, pupils slightly constricted, BP 130/70, pulse 90 and reg. – Chest: A/E fair bil. And some mild basilar creps – ABG: p. H 7. 46 p. CO 2 50 p. O 2 55 Bi. Carb 36 Fi. O 2 >. 50 – Chest X-ray: Extensive bilateral, diffuse, interstitial infiltrate consistent with ARDS Naloxone would probably have had a serious adverse effect on this patient. Hypoxemia despite supplemental O 2 in a breathing patient. Look beyond the Opioids!
Case Presentation: Somnolence and hypoxemia while on IV PCA Hydromorphone n n Further patient evaluation – Patient arousable, RR 8 -16, pupils slightly constricted, BP 130/70, pulse 90 and reg. – Chest: A/E fair bil. And some mild basilar creps – ABG: p. H 7. 46 p. CO 2 50 p. O 2 55 Bi. Carb 36 Fi. O 2 >. 50 – Chest X-ray: Extensive bilateral, diffuse, interstitial infiltrate consistent with ARDS Naloxone would probably have had a serious adverse effect on this patient. Hypoxemia despite supplemental O 2 in a breathing patient. Look beyond the Opioids!
 Case Presentation: Somnolence and hypoxemia while on IV PCA Hydromorphone n Management of suspected opioid induced respiratory depression – – – Support A/W Simulate breathing Supply supplemental oxygen Assess Sa. O 2, BP, Pulse Naloxone titration, IF INDICATED • 0. 04 mg Q 5 min. X 3 as needed n n Hypoxemia is a medical emergency Hypercarbia is NOT
Case Presentation: Somnolence and hypoxemia while on IV PCA Hydromorphone n Management of suspected opioid induced respiratory depression – – – Support A/W Simulate breathing Supply supplemental oxygen Assess Sa. O 2, BP, Pulse Naloxone titration, IF INDICATED • 0. 04 mg Q 5 min. X 3 as needed n n Hypoxemia is a medical emergency Hypercarbia is NOT
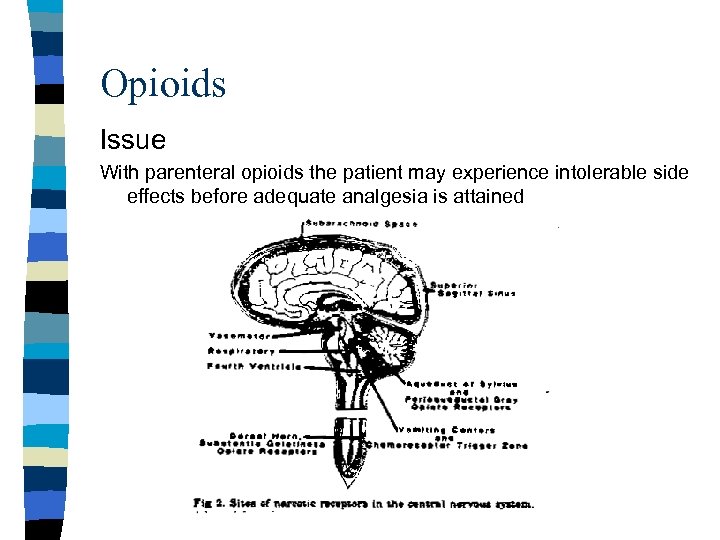 Opioids Issue With parenteral opioids the patient may experience intolerable side effects before adequate analgesia is attained
Opioids Issue With parenteral opioids the patient may experience intolerable side effects before adequate analgesia is attained
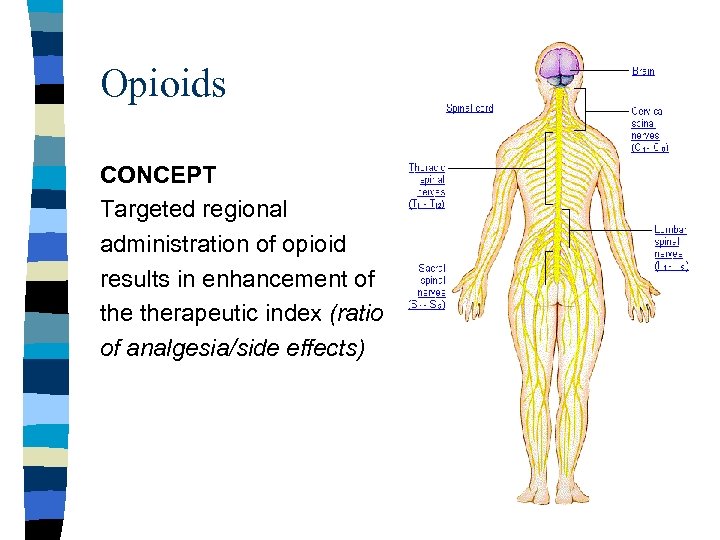 Opioids CONCEPT Targeted regional administration of opioid results in enhancement of therapeutic index (ratio of analgesia/side effects)
Opioids CONCEPT Targeted regional administration of opioid results in enhancement of therapeutic index (ratio of analgesia/side effects)
 Neuraxial Opioids – the good n Intrathecal morphine – simple technique – potent analgesia for 12 -16 hrs. – highly effective for pain in lower abdomen and lower limbs
Neuraxial Opioids – the good n Intrathecal morphine – simple technique – potent analgesia for 12 -16 hrs. – highly effective for pain in lower abdomen and lower limbs
 Neuraxial Opioids – adverse effects n n n Risk of delayed onset of respiratory depression, peaks at 6 hours Urinary retention >50% for 16 hours Pruritus, is not an allergy
Neuraxial Opioids – adverse effects n n n Risk of delayed onset of respiratory depression, peaks at 6 hours Urinary retention >50% for 16 hours Pruritus, is not an allergy
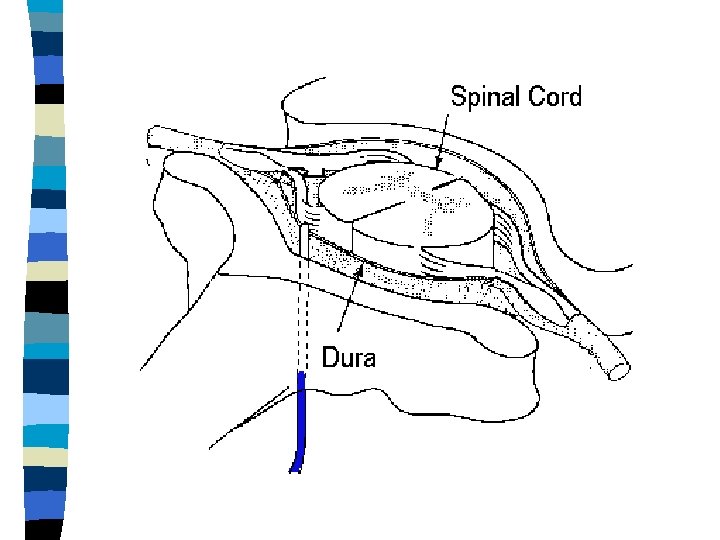
 What is an “EPIDURAL”? n Anatomical – Location of the catheter, C 7 – L 5 • Cervical, thoracic and lumbar epidurals • Segmental Blockade n Drugs – Opioids (hydrophillic vs. lipophillic) • morphine, hydromorphone, demerol, fentanyl • Hydrophillic drugs migrate rostrally and also yield greater spinal selectivity
What is an “EPIDURAL”? n Anatomical – Location of the catheter, C 7 – L 5 • Cervical, thoracic and lumbar epidurals • Segmental Blockade n Drugs – Opioids (hydrophillic vs. lipophillic) • morphine, hydromorphone, demerol, fentanyl • Hydrophillic drugs migrate rostrally and also yield greater spinal selectivity
 What is an “EPIDURAL”? n Drugs – Local Anesthetics : • Lidocaine, bupivacaine, ropivacaine Varying concentrations/drug mass produces “Differential Blockade” sympathetics > somatosensory > motor – Adjuncts: epinephrine – Mode of Drug Delivery – Intermittent bolus vs. continuous infusions
What is an “EPIDURAL”? n Drugs – Local Anesthetics : • Lidocaine, bupivacaine, ropivacaine Varying concentrations/drug mass produces “Differential Blockade” sympathetics > somatosensory > motor – Adjuncts: epinephrine – Mode of Drug Delivery – Intermittent bolus vs. continuous infusions
 True or False? n Epidural analgesia impairs the resolution of post-operative ileus i. e. it “slows down the gut” delaying return of normal bowel function.
True or False? n Epidural analgesia impairs the resolution of post-operative ileus i. e. it “slows down the gut” delaying return of normal bowel function.
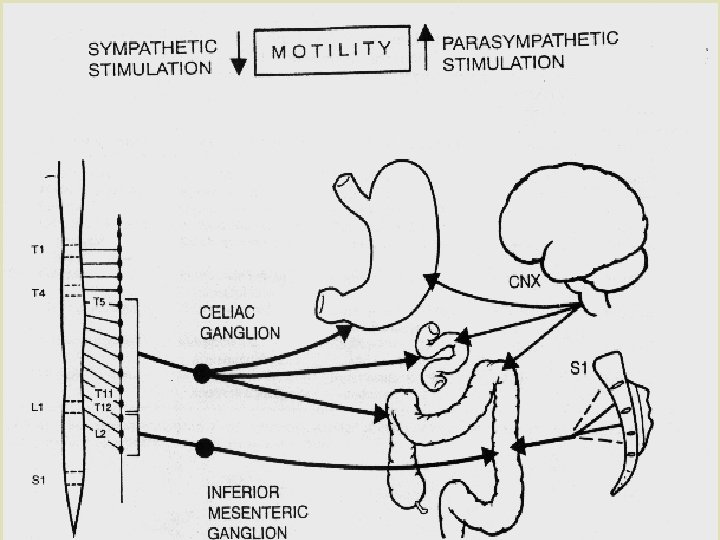
 Epidural analgesia and recovery of bowel motililty? ? n n Thoracic placement of epidural with the administration of local anesthesic and minimal opioid will promote bowel recovery via sympathetic blockade If the primary mode of epidural analgesia is via potent opioid, recovery of motility may be delayed.
Epidural analgesia and recovery of bowel motililty? ? n n Thoracic placement of epidural with the administration of local anesthesic and minimal opioid will promote bowel recovery via sympathetic blockade If the primary mode of epidural analgesia is via potent opioid, recovery of motility may be delayed.
 True or False? n Epidural analgesia necessitates a foley catheter until the epidural is removed.
True or False? n Epidural analgesia necessitates a foley catheter until the epidural is removed.
 What about epidurals and the foley catheter? ? n Less Urinary Tract Infection by Earlier Removal of Bladder Catheter in Surgical Patients Receiving Thoracic Epidural Analgesia. Zaouter C, Kaneva P, Carli F (Mc. Gill) Regional Anesthesia and Pain Medicine Nov-Dec 2009 pp. 542 -552.
What about epidurals and the foley catheter? ? n Less Urinary Tract Infection by Earlier Removal of Bladder Catheter in Surgical Patients Receiving Thoracic Epidural Analgesia. Zaouter C, Kaneva P, Carli F (Mc. Gill) Regional Anesthesia and Pain Medicine Nov-Dec 2009 pp. 542 -552.
 Epidural Pit-falls for the Surgeon n n Epidural hematoma – > 50 reported cases in USA in patients treated with LMWH – Epidural insertion and removal of the catheter – Risk factors: Elderly, low body weight, twice daily dosing, anti-coagulation vs. prophylactic dose range The decision to fully anti-coagulate a patient with an epidural in-situ should be made in consultation with anesthesia and thrombosis medicine
Epidural Pit-falls for the Surgeon n n Epidural hematoma – > 50 reported cases in USA in patients treated with LMWH – Epidural insertion and removal of the catheter – Risk factors: Elderly, low body weight, twice daily dosing, anti-coagulation vs. prophylactic dose range The decision to fully anti-coagulate a patient with an epidural in-situ should be made in consultation with anesthesia and thrombosis medicine
 Epidural Pit-falls for the Surgeon n More epidural hematoma risks!! – Heparin 5000 units s. c. Q 8 H for thromboprophyllaxis? ? This is full clinical anti-coagulation for some patients! n Once daily LMWH at thromboprophyllactic dose is safer.
Epidural Pit-falls for the Surgeon n More epidural hematoma risks!! – Heparin 5000 units s. c. Q 8 H for thromboprophyllaxis? ? This is full clinical anti-coagulation for some patients! n Once daily LMWH at thromboprophyllactic dose is safer.
 What about anti-platelet agents? n Plavix – ASRA guidelines state no neuraxial anesthesia or epidural catheters implemented until D/C for 7 days – – Plavix may be started 12 – 24 hour after neuraxial block or catheter removal – concensus only, speculative – Obviously risk is much lower than with heparin/coumadin since reports are extremely rare – New agents on horizon? ?
What about anti-platelet agents? n Plavix – ASRA guidelines state no neuraxial anesthesia or epidural catheters implemented until D/C for 7 days – – Plavix may be started 12 – 24 hour after neuraxial block or catheter removal – concensus only, speculative – Obviously risk is much lower than with heparin/coumadin since reports are extremely rare – New agents on horizon? ?
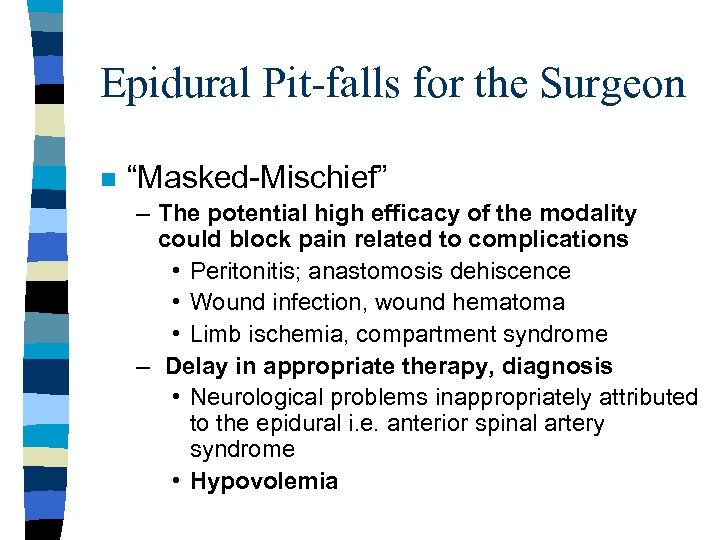 Epidural Pit-falls for the Surgeon n “Masked-Mischief” – The potential high efficacy of the modality could block pain related to complications • Peritonitis; anastomosis dehiscence • Wound infection, wound hematoma • Limb ischemia, compartment syndrome – Delay in appropriate therapy, diagnosis • Neurological problems inappropriately attributed to the epidural i. e. anterior spinal artery syndrome • Hypovolemia
Epidural Pit-falls for the Surgeon n “Masked-Mischief” – The potential high efficacy of the modality could block pain related to complications • Peritonitis; anastomosis dehiscence • Wound infection, wound hematoma • Limb ischemia, compartment syndrome – Delay in appropriate therapy, diagnosis • Neurological problems inappropriately attributed to the epidural i. e. anterior spinal artery syndrome • Hypovolemia
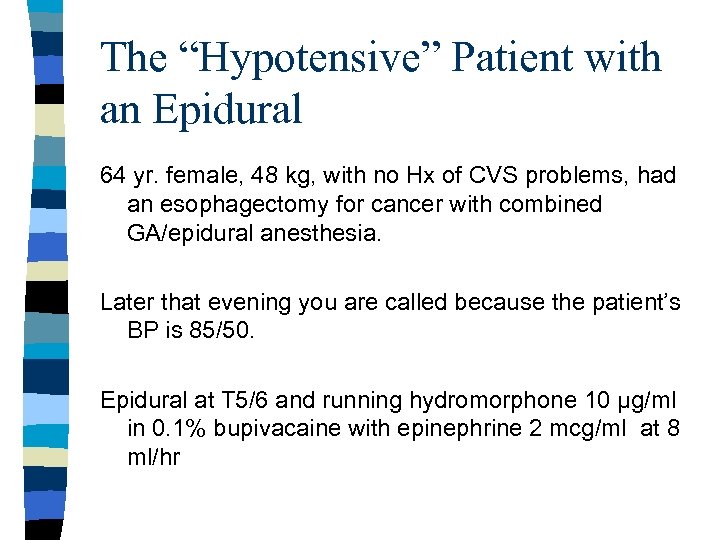 The “Hypotensive” Patient with an Epidural 64 yr. female, 48 kg, with no Hx of CVS problems, had an esophagectomy for cancer with combined GA/epidural anesthesia. Later that evening you are called because the patient’s BP is 85/50. Epidural at T 5/6 and running hydromorphone 10 µg/ml in 0. 1% bupivacaine with epinephrine 2 mcg/ml at 8 ml/hr
The “Hypotensive” Patient with an Epidural 64 yr. female, 48 kg, with no Hx of CVS problems, had an esophagectomy for cancer with combined GA/epidural anesthesia. Later that evening you are called because the patient’s BP is 85/50. Epidural at T 5/6 and running hydromorphone 10 µg/ml in 0. 1% bupivacaine with epinephrine 2 mcg/ml at 8 ml/hr
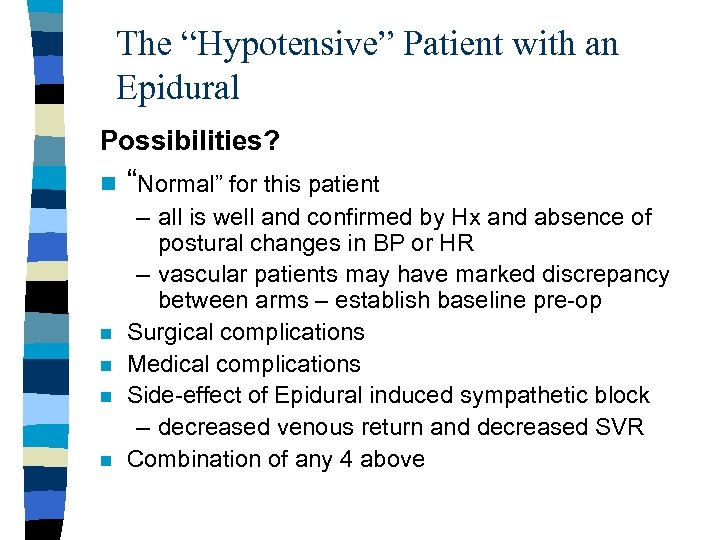 The “Hypotensive” Patient with an Epidural Possibilities? n “Normal” for this patient – all is well and confirmed by Hx and absence of postural changes in BP or HR – vascular patients may have marked discrepancy between arms – establish baseline pre-op n Surgical complications n Medical complications n Side-effect of Epidural induced sympathetic block – decreased venous return and decreased SVR n Combination of any 4 above
The “Hypotensive” Patient with an Epidural Possibilities? n “Normal” for this patient – all is well and confirmed by Hx and absence of postural changes in BP or HR – vascular patients may have marked discrepancy between arms – establish baseline pre-op n Surgical complications n Medical complications n Side-effect of Epidural induced sympathetic block – decreased venous return and decreased SVR n Combination of any 4 above
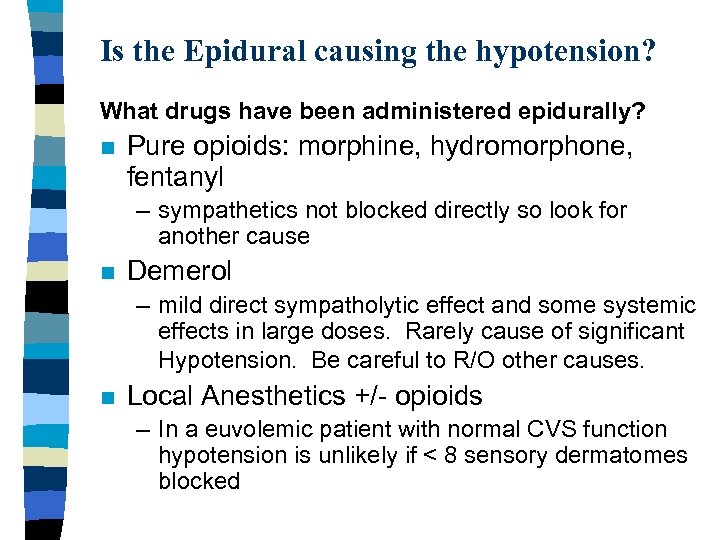 Is the Epidural causing the hypotension? What drugs have been administered epidurally? n Pure opioids: morphine, hydromorphone, fentanyl – sympathetics not blocked directly so look for another cause n Demerol – mild direct sympatholytic effect and some systemic effects in large doses. Rarely cause of significant Hypotension. Be careful to R/O other causes. n Local Anesthetics +/- opioids – In a euvolemic patient with normal CVS function hypotension is unlikely if < 8 sensory dermatomes blocked
Is the Epidural causing the hypotension? What drugs have been administered epidurally? n Pure opioids: morphine, hydromorphone, fentanyl – sympathetics not blocked directly so look for another cause n Demerol – mild direct sympatholytic effect and some systemic effects in large doses. Rarely cause of significant Hypotension. Be careful to R/O other causes. n Local Anesthetics +/- opioids – In a euvolemic patient with normal CVS function hypotension is unlikely if < 8 sensory dermatomes blocked
 Is the Epidural Local Anesthetic causing the hypotension? n Intrathecal catheter migration n Inadvertent overdose n “Un-masking” of problem with the patient. n “Sensitive” patient
Is the Epidural Local Anesthetic causing the hypotension? n Intrathecal catheter migration n Inadvertent overdose n “Un-masking” of problem with the patient. n “Sensitive” patient
 Is the Epidural Local Anesthetic causing the hypotension? Management n ABCs – supplemental O 2, fluid bolus, elevate legs – ephedrine 5 mg or phenylephrine 50 µg IV bolus – Hold the epidural infusion n Quantify the extent of block – motor block? Thoracic epidural? , that’s a problem! – Sensory block (cold, sharp) • In a euvolemic patient with normal CVS function hypotension is unlikely if < 8 sensory dermatomes blocked
Is the Epidural Local Anesthetic causing the hypotension? Management n ABCs – supplemental O 2, fluid bolus, elevate legs – ephedrine 5 mg or phenylephrine 50 µg IV bolus – Hold the epidural infusion n Quantify the extent of block – motor block? Thoracic epidural? , that’s a problem! – Sensory block (cold, sharp) • In a euvolemic patient with normal CVS function hypotension is unlikely if < 8 sensory dermatomes blocked
 Management of Hypotension Cont’d n High thoracic epidural blockade may block the compensatory tachycardia response to hypovolemia. – Cardio-accelerator sympathetic nerve fibres arise from T 1 - T 4 – sympathetic block may extend several dermatomes above the sensory blockade n n Correct the underlying cause Remove bupicacaine and change to epidural hydromorphone if patient remains hemodynamically unstable
Management of Hypotension Cont’d n High thoracic epidural blockade may block the compensatory tachycardia response to hypovolemia. – Cardio-accelerator sympathetic nerve fibres arise from T 1 - T 4 – sympathetic block may extend several dermatomes above the sensory blockade n n Correct the underlying cause Remove bupicacaine and change to epidural hydromorphone if patient remains hemodynamically unstable
 36 yr. Open Cholecystectomy patient experiencing difficulty weaning from IV PCA n Endometriosis, fibromyalgia and chronic low back pain- has been on Tylenol #3 for several years- functions well and stable usage of 810/day n Day 3 post-op Tylenol #3, 2 tabs Q 4 h started and IV PCA D/C n Patient c/o severe pain, not able to go home
36 yr. Open Cholecystectomy patient experiencing difficulty weaning from IV PCA n Endometriosis, fibromyalgia and chronic low back pain- has been on Tylenol #3 for several years- functions well and stable usage of 810/day n Day 3 post-op Tylenol #3, 2 tabs Q 4 h started and IV PCA D/C n Patient c/o severe pain, not able to go home
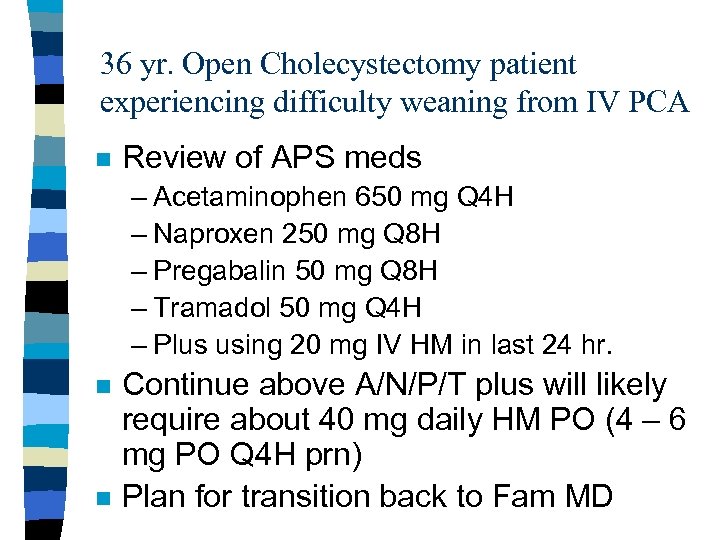 36 yr. Open Cholecystectomy patient experiencing difficulty weaning from IV PCA n Review of APS meds – Acetaminophen 650 mg Q 4 H – Naproxen 250 mg Q 8 H – Pregabalin 50 mg Q 8 H – Tramadol 50 mg Q 4 H – Plus using 20 mg IV HM in last 24 hr. n n Continue above A/N/P/T plus will likely require about 40 mg daily HM PO (4 – 6 mg PO Q 4 H prn) Plan for transition back to Fam MD
36 yr. Open Cholecystectomy patient experiencing difficulty weaning from IV PCA n Review of APS meds – Acetaminophen 650 mg Q 4 H – Naproxen 250 mg Q 8 H – Pregabalin 50 mg Q 8 H – Tramadol 50 mg Q 4 H – Plus using 20 mg IV HM in last 24 hr. n n Continue above A/N/P/T plus will likely require about 40 mg daily HM PO (4 – 6 mg PO Q 4 H prn) Plan for transition back to Fam MD
 Conclusion: Key Concepts n n The foundation of all acute pain Rx protocols is NSAIDS and acetaminophen. Codeine is a “pro-drug”. Problems may occur with under or over conversion to morphine Tramadol to be considered as second step in the acute pain ladder Naloxone can be a dangerous drug, careful titration is almost always possible
Conclusion: Key Concepts n n The foundation of all acute pain Rx protocols is NSAIDS and acetaminophen. Codeine is a “pro-drug”. Problems may occur with under or over conversion to morphine Tramadol to be considered as second step in the acute pain ladder Naloxone can be a dangerous drug, careful titration is almost always possible
 Conclusions n Inadequate analgesia despite cyclooxygenase inhibitors and opioids? – Think “Hyperalgesia” – Consider an anti-hyperalgesic like ketamine, pregabalin n n All epidurals are not equivalent Epidural pitfalls
Conclusions n Inadequate analgesia despite cyclooxygenase inhibitors and opioids? – Think “Hyperalgesia” – Consider an anti-hyperalgesic like ketamine, pregabalin n n All epidurals are not equivalent Epidural pitfalls
 Useful texts n Free!! From Canadian Pain Society Managing Pain: The Canadian Healthcare Professional’s Reference. Edited by Roman Jovey. 2008.
Useful texts n Free!! From Canadian Pain Society Managing Pain: The Canadian Healthcare Professional’s Reference. Edited by Roman Jovey. 2008.
 ACUTE PAIN MANAGEMENT: SCIENTIFIC EVIDENCE 3 nd Edition Feb ‘ 10 Australian and New Zealand College of Anaesthetists And Faculty of Pain Medicine. http: //www. anzca. edu. au/publications/acutepain. pdf The above web site has the entire document and is freely Available to download.
ACUTE PAIN MANAGEMENT: SCIENTIFIC EVIDENCE 3 nd Edition Feb ‘ 10 Australian and New Zealand College of Anaesthetists And Faculty of Pain Medicine. http: //www. anzca. edu. au/publications/acutepain. pdf The above web site has the entire document and is freely Available to download.
 Useful websites on Pain Prospect: Procedure Specific Post-op Pain Management http: //www. postoppain. org/frameset. htm n Pain Explained http: //www. painexplained. ca/content. asp? node=4 n The Canadian Pain Society http: //www. canadianpainsociety. ca/indexenglish. h tml n
Useful websites on Pain Prospect: Procedure Specific Post-op Pain Management http: //www. postoppain. org/frameset. htm n Pain Explained http: //www. painexplained. ca/content. asp? node=4 n The Canadian Pain Society http: //www. canadianpainsociety. ca/indexenglish. h tml n
 Useful websites on Pain Institute http: //www. medscape. com/infosite/paininstitute/article 5? src=0_0_ad_ldr Internation Association for the Study of Pain http: //www. iasppain. org//AM/Template. cfm? Section=Home n
Useful websites on Pain Institute http: //www. medscape. com/infosite/paininstitute/article 5? src=0_0_ad_ldr Internation Association for the Study of Pain http: //www. iasppain. org//AM/Template. cfm? Section=Home n


