a364d380cd560939949868998b5e18d9.ppt
- Количество слайдов: 19
 KENYA Nutrition Deep Dive 11 th MAY, 2016 USAID PREG Meeting
KENYA Nutrition Deep Dive 11 th MAY, 2016 USAID PREG Meeting
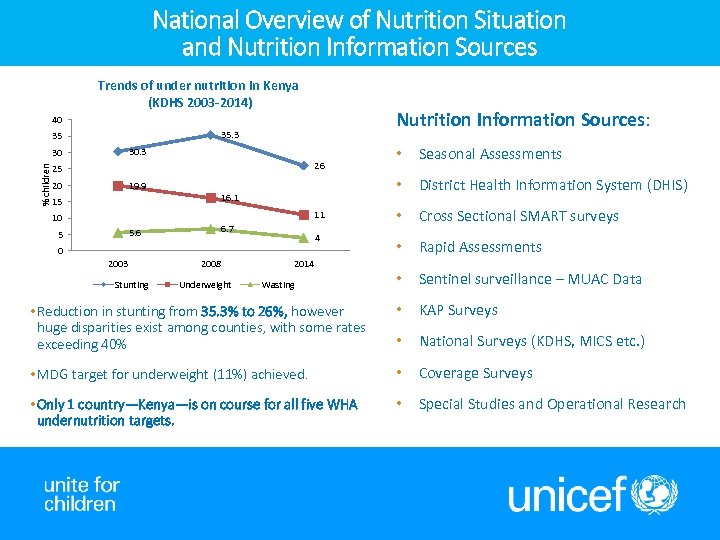 National Overview of Nutrition Situation and Nutrition Information Sources Trends of under nutrition in Kenya (KDHS 2003 -2014) Nutrition Information Sources: 40 35. 3 35 • Seasonal Assessments • District Health Information System (DHIS) • Cross Sectional SMART surveys • Rapid Assessments • Sentinel surveillance – MUAC Data • Reduction in stunting from 35. 3% to 26%, however huge disparities exist among counties, with some rates exceeding 40% • KAP Surveys • National Surveys (KDHS, MICS etc. ) • MDG target for underweight (11%) achieved. • Coverage Surveys • Only 1 country—Kenya—is on course for all five WHA undernutrition targets. • Special Studies and Operational Research 30. 3 % children 30 26 25 20 19. 9 16. 1 15 11 10 6. 7 5. 6 5 4 0 2003 Stunting 2008 Underweight 2014 Wasting
National Overview of Nutrition Situation and Nutrition Information Sources Trends of under nutrition in Kenya (KDHS 2003 -2014) Nutrition Information Sources: 40 35. 3 35 • Seasonal Assessments • District Health Information System (DHIS) • Cross Sectional SMART surveys • Rapid Assessments • Sentinel surveillance – MUAC Data • Reduction in stunting from 35. 3% to 26%, however huge disparities exist among counties, with some rates exceeding 40% • KAP Surveys • National Surveys (KDHS, MICS etc. ) • MDG target for underweight (11%) achieved. • Coverage Surveys • Only 1 country—Kenya—is on course for all five WHA undernutrition targets. • Special Studies and Operational Research 30. 3 % children 30 26 25 20 19. 9 16. 1 15 11 10 6. 7 5. 6 5 4 0 2003 Stunting 2008 Underweight 2014 Wasting
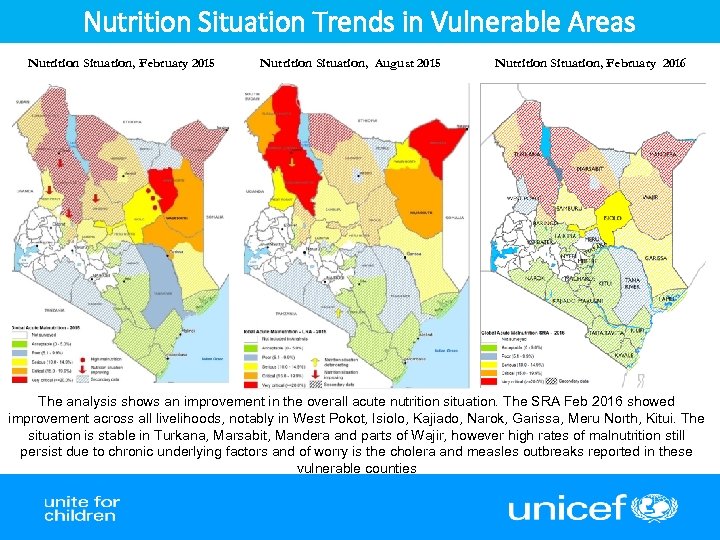 Nutrition Situation Trends in Vulnerable Areas Nutrition Situation, February 2015 Nutrition Situation, August 2015 Nutrition Situation, February 2016 The analysis shows an improvement in the overall acute nutrition situation. The SRA Feb 2016 showed improvement across all livelihoods, notably in West Pokot, Isiolo, Kajiado, Narok, Garissa, Meru North, Kitui. The situation is stable in Turkana, Marsabit, Mandera and parts of Wajir, however high rates of malnutrition still persist due to chronic underlying factors and of worry is the cholera and measles outbreaks reported in these vulnerable counties
Nutrition Situation Trends in Vulnerable Areas Nutrition Situation, February 2015 Nutrition Situation, August 2015 Nutrition Situation, February 2016 The analysis shows an improvement in the overall acute nutrition situation. The SRA Feb 2016 showed improvement across all livelihoods, notably in West Pokot, Isiolo, Kajiado, Narok, Garissa, Meru North, Kitui. The situation is stable in Turkana, Marsabit, Mandera and parts of Wajir, however high rates of malnutrition still persist due to chronic underlying factors and of worry is the cholera and measles outbreaks reported in these vulnerable counties
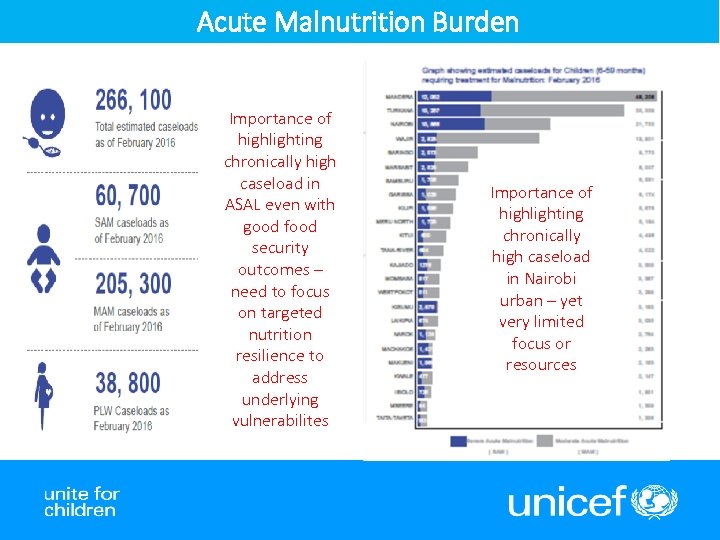 Acute Malnutrition Burden Importance of highlighting chronically high caseload in ASAL even with good food security outcomes – need to focus on targeted nutrition resilience to address underlying vulnerabilites Importance of highlighting chronically high caseload in Nairobi urban – yet very limited focus or resources
Acute Malnutrition Burden Importance of highlighting chronically high caseload in ASAL even with good food security outcomes – need to focus on targeted nutrition resilience to address underlying vulnerabilites Importance of highlighting chronically high caseload in Nairobi urban – yet very limited focus or resources
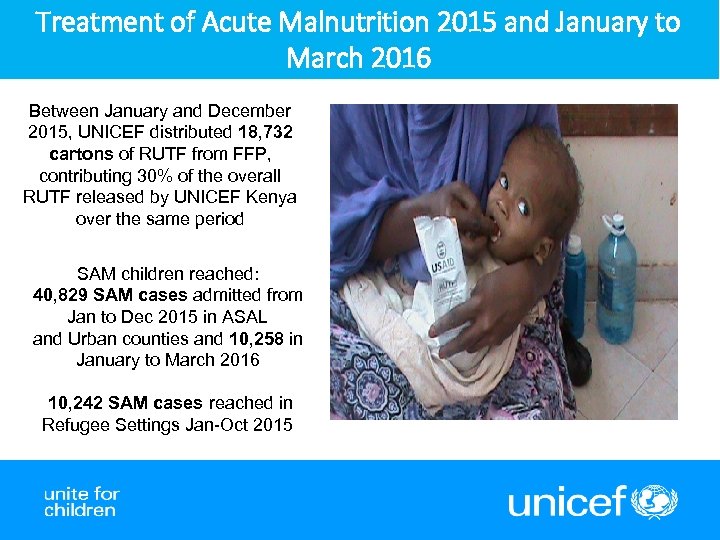 Treatment of Acute Malnutrition 2015 and January to March 2016 Between January and December 2015, UNICEF distributed 18, 732 cartons of RUTF from FFP, contributing 30% of the overall RUTF released by UNICEF Kenya over the same period SAM children reached: 40, 829 SAM cases admitted from Jan to Dec 2015 in ASAL and Urban counties and 10, 258 in January to March 2016 10, 242 SAM cases reached in Refugee Settings Jan-Oct 2015
Treatment of Acute Malnutrition 2015 and January to March 2016 Between January and December 2015, UNICEF distributed 18, 732 cartons of RUTF from FFP, contributing 30% of the overall RUTF released by UNICEF Kenya over the same period SAM children reached: 40, 829 SAM cases admitted from Jan to Dec 2015 in ASAL and Urban counties and 10, 258 in January to March 2016 10, 242 SAM cases reached in Refugee Settings Jan-Oct 2015
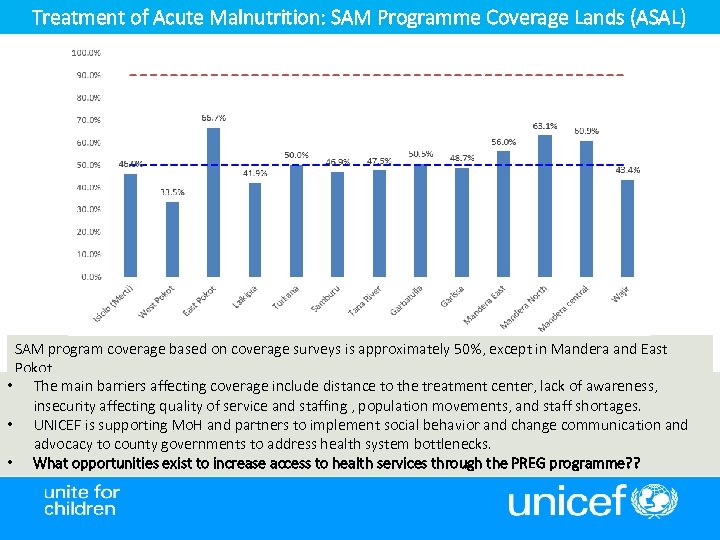 Treatment of Acute Malnutrition: SAM Programme Coverage Lands (ASAL) SAM program coverage based on coverage surveys is approximately 50%, except in Mandera and East Pokot • The main barriers affecting coverage include distance to the treatment center, lack of awareness, insecurity affecting quality of service and staffing , population movements, and staff shortages. • UNICEF is supporting Mo. H and partners to implement social behavior and change communication and advocacy to county governments to address health system bottlenecks. • What opportunities exist to increase access to health services through the PREG programme? ?
Treatment of Acute Malnutrition: SAM Programme Coverage Lands (ASAL) SAM program coverage based on coverage surveys is approximately 50%, except in Mandera and East Pokot • The main barriers affecting coverage include distance to the treatment center, lack of awareness, insecurity affecting quality of service and staffing , population movements, and staff shortages. • UNICEF is supporting Mo. H and partners to implement social behavior and change communication and advocacy to county governments to address health system bottlenecks. • What opportunities exist to increase access to health services through the PREG programme? ?
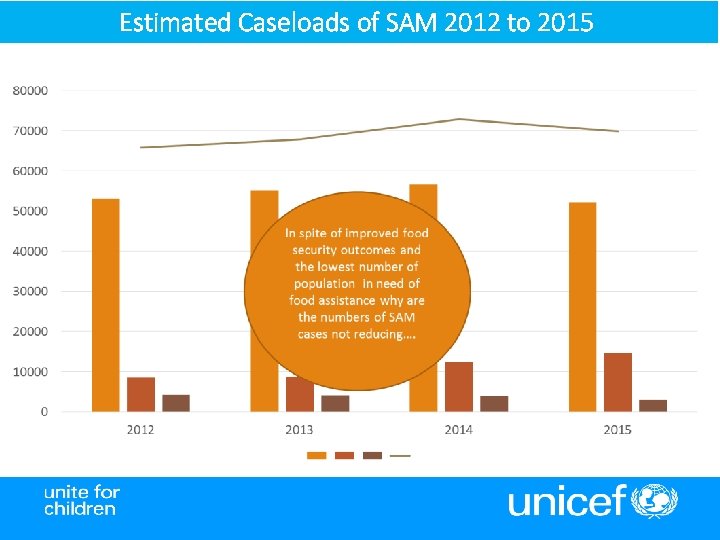 Estimated Caseloads of SAM 2012 to 2015
Estimated Caseloads of SAM 2012 to 2015
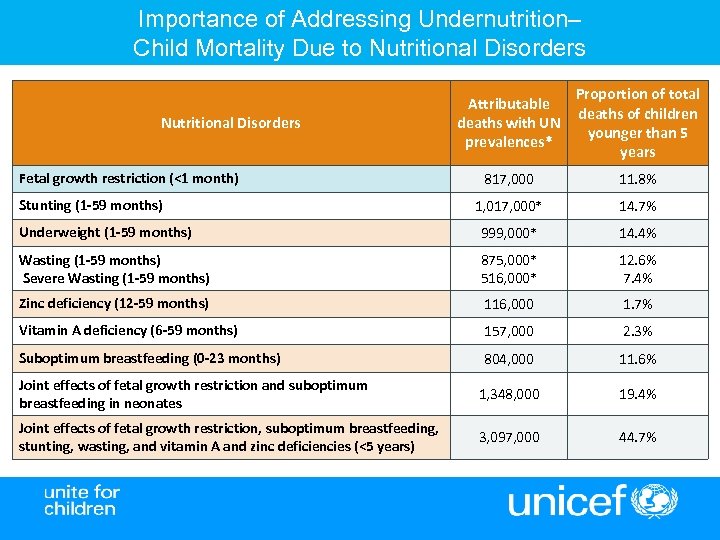 Importance of Addressing Undernutrition– Child Mortality Due to Nutritional Disorders Attributable deaths with UN prevalences* Proportion of total deaths of children younger than 5 years 817, 000 11. 8% 1, 017, 000* 14. 7% Underweight (1 -59 months) 999, 000* 14. 4% Wasting (1 -59 months) Severe Wasting (1 -59 months) 875, 000* 516, 000* 12. 6% 7. 4% Zinc deficiency (12 -59 months) 116, 000 1. 7% Vitamin A deficiency (6 -59 months) 157, 000 2. 3% Suboptimum breastfeeding (0 -23 months) 804, 000 11. 6% Joint effects of fetal growth restriction and suboptimum breastfeeding in neonates 1, 348, 000 19. 4% Joint effects of fetal growth restriction, suboptimum breastfeeding, stunting, wasting, and vitamin A and zinc deficiencies (<5 years) 3, 097, 000 44. 7% Nutritional Disorders Fetal growth restriction (<1 month) Stunting (1 -59 months)
Importance of Addressing Undernutrition– Child Mortality Due to Nutritional Disorders Attributable deaths with UN prevalences* Proportion of total deaths of children younger than 5 years 817, 000 11. 8% 1, 017, 000* 14. 7% Underweight (1 -59 months) 999, 000* 14. 4% Wasting (1 -59 months) Severe Wasting (1 -59 months) 875, 000* 516, 000* 12. 6% 7. 4% Zinc deficiency (12 -59 months) 116, 000 1. 7% Vitamin A deficiency (6 -59 months) 157, 000 2. 3% Suboptimum breastfeeding (0 -23 months) 804, 000 11. 6% Joint effects of fetal growth restriction and suboptimum breastfeeding in neonates 1, 348, 000 19. 4% Joint effects of fetal growth restriction, suboptimum breastfeeding, stunting, wasting, and vitamin A and zinc deficiencies (<5 years) 3, 097, 000 44. 7% Nutritional Disorders Fetal growth restriction (<1 month) Stunting (1 -59 months)
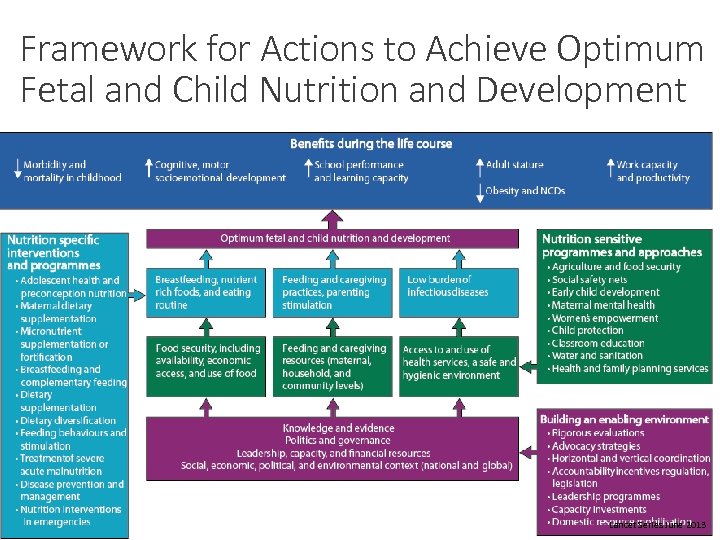 Framework for Actions to Achieve Optimum Fetal and Child Nutrition and Development 9 Lancet Series June 2013
Framework for Actions to Achieve Optimum Fetal and Child Nutrition and Development 9 Lancet Series June 2013
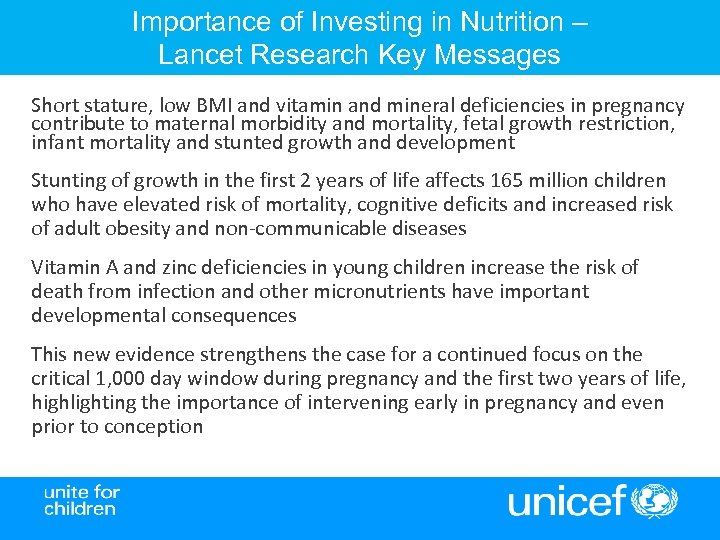 Importance of Investing in Nutrition – Lancet Research Key Messages Short stature, low BMI and vitamin and mineral deficiencies in pregnancy contribute to maternal morbidity and mortality, fetal growth restriction, infant mortality and stunted growth and development Stunting of growth in the first 2 years of life affects 165 million children who have elevated risk of mortality, cognitive deficits and increased risk of adult obesity and non-communicable diseases Vitamin A and zinc deficiencies in young children increase the risk of death from infection and other micronutrients have important developmental consequences This new evidence strengthens the case for a continued focus on the critical 1, 000 day window during pregnancy and the first two years of life, highlighting the importance of intervening early in pregnancy and even prior to conception
Importance of Investing in Nutrition – Lancet Research Key Messages Short stature, low BMI and vitamin and mineral deficiencies in pregnancy contribute to maternal morbidity and mortality, fetal growth restriction, infant mortality and stunted growth and development Stunting of growth in the first 2 years of life affects 165 million children who have elevated risk of mortality, cognitive deficits and increased risk of adult obesity and non-communicable diseases Vitamin A and zinc deficiencies in young children increase the risk of death from infection and other micronutrients have important developmental consequences This new evidence strengthens the case for a continued focus on the critical 1, 000 day window during pregnancy and the first two years of life, highlighting the importance of intervening early in pregnancy and even prior to conception
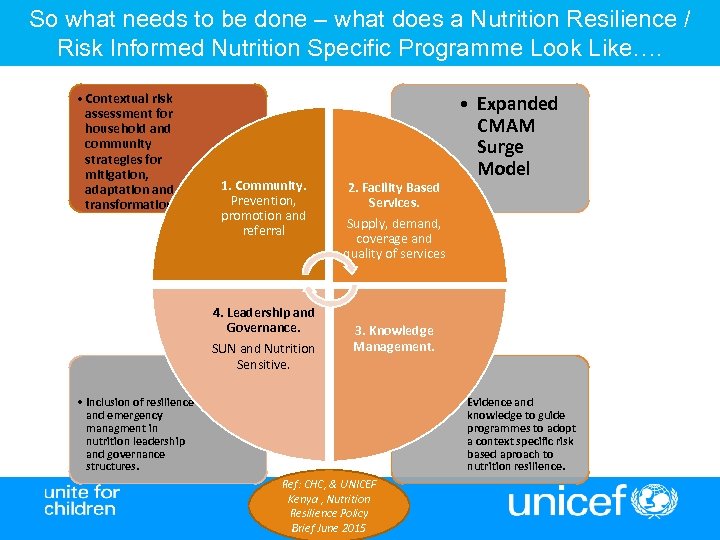 So what needs to be done – what does a Nutrition Resilience / Risk Informed Nutrition Specific Programme Look Like…. • Contextual risk assessment for household and community strategies for mitigation, adaptation and transformation. 1. Community. Prevention, promotion and referral 4. Leadership and Governance. SUN and Nutrition Sensitive. 2. Facility Based Services. • Expanded CMAM Surge Model Supply, demand, coverage and quality of services 3. Knowledge Management. • Inclusion of resilience and emergency managment in nutrition leadership and governance structures. • Evidence and knowledge to guide programmes to adopt a context specific risk based aproach to nutrition resilience. Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
So what needs to be done – what does a Nutrition Resilience / Risk Informed Nutrition Specific Programme Look Like…. • Contextual risk assessment for household and community strategies for mitigation, adaptation and transformation. 1. Community. Prevention, promotion and referral 4. Leadership and Governance. SUN and Nutrition Sensitive. 2. Facility Based Services. • Expanded CMAM Surge Model Supply, demand, coverage and quality of services 3. Knowledge Management. • Inclusion of resilience and emergency managment in nutrition leadership and governance structures. • Evidence and knowledge to guide programmes to adopt a context specific risk based aproach to nutrition resilience. Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
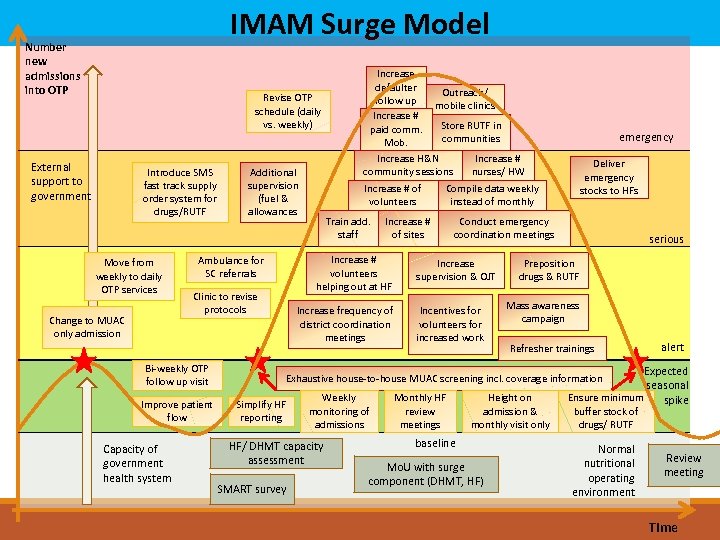 IMAM Surge Model Number new admissions into OTP Revise OTP schedule (daily vs. weekly) External support to government Introduce SMS fast track supply order system for drugs/RUTF Move from weekly to daily OTP services Change to MUAC only admission Additional supervision (fuel & allowances Clinic to revise protocols Improve patient flow Capacity of government health system Increase # of volunteers Train add. staff Increase frequency of district coordination meetings emergency Deliver emergency stocks to HFs Compile data weekly instead of monthly Increase # of sites Increase # volunteers helping out at HF Ambulance for SC referrals Bi-weekly OTP follow up visit Increase defaulter Outreach/ follow up mobile clinics Increase # Store RUTF in paid communities Mob. Increase H&N Increase # community sessions nurses/ HW Conduct emergency coordination meetings Increase supervision & OJT Incentives for volunteers for increased work serious Preposition drugs & RUTF Mass awareness campaign Refresher trainings alert Expected seasonal Ensure minimum spike Exhaustive house-to-house MUAC screening incl. coverage information Simplify HF reporting Weekly monitoring of admissions HF/ DHMT capacity assessment SMART survey Monthly HF review meetings Height on admission & monthly visit only baseline Mo. U with surge component (DHMT, HF) buffer stock of drugs/ RUTF Normal nutritional operating environment Review meeting Time
IMAM Surge Model Number new admissions into OTP Revise OTP schedule (daily vs. weekly) External support to government Introduce SMS fast track supply order system for drugs/RUTF Move from weekly to daily OTP services Change to MUAC only admission Additional supervision (fuel & allowances Clinic to revise protocols Improve patient flow Capacity of government health system Increase # of volunteers Train add. staff Increase frequency of district coordination meetings emergency Deliver emergency stocks to HFs Compile data weekly instead of monthly Increase # of sites Increase # volunteers helping out at HF Ambulance for SC referrals Bi-weekly OTP follow up visit Increase defaulter Outreach/ follow up mobile clinics Increase # Store RUTF in paid communities Mob. Increase H&N Increase # community sessions nurses/ HW Conduct emergency coordination meetings Increase supervision & OJT Incentives for volunteers for increased work serious Preposition drugs & RUTF Mass awareness campaign Refresher trainings alert Expected seasonal Ensure minimum spike Exhaustive house-to-house MUAC screening incl. coverage information Simplify HF reporting Weekly monitoring of admissions HF/ DHMT capacity assessment SMART survey Monthly HF review meetings Height on admission & monthly visit only baseline Mo. U with surge component (DHMT, HF) buffer stock of drugs/ RUTF Normal nutritional operating environment Review meeting Time
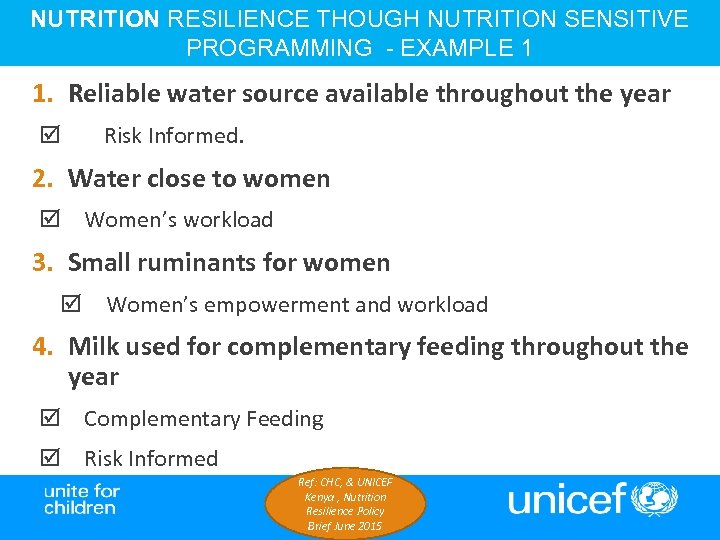 NUTRITION RESILIENCE THOUGH NUTRITION SENSITIVE PROGRAMMING - EXAMPLE 1 1. Reliable water source available throughout the year Risk Informed. 2. Water close to women Women’s workload 3. Small ruminants for women Women’s empowerment and workload 4. Milk used for complementary feeding throughout the year Complementary Feeding Risk Informed Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
NUTRITION RESILIENCE THOUGH NUTRITION SENSITIVE PROGRAMMING - EXAMPLE 1 1. Reliable water source available throughout the year Risk Informed. 2. Water close to women Women’s workload 3. Small ruminants for women Women’s empowerment and workload 4. Milk used for complementary feeding throughout the year Complementary Feeding Risk Informed Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
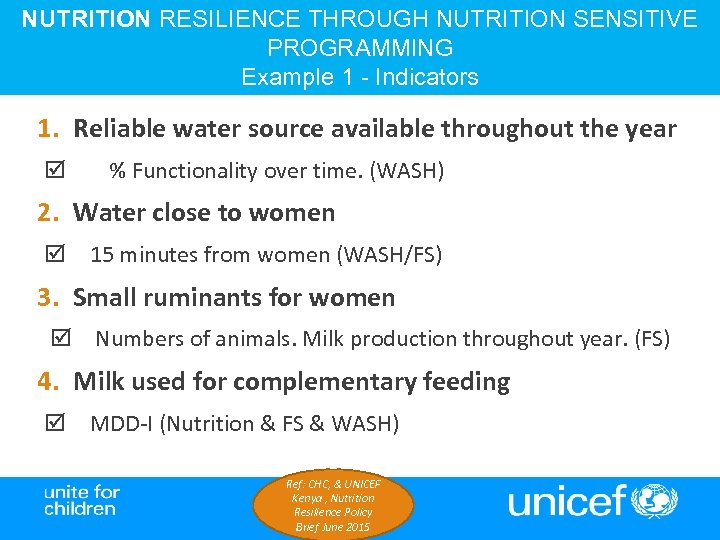 NUTRITION RESILIENCE THROUGH NUTRITION SENSITIVE PROGRAMMING Example 1 - Indicators 1. Reliable water source available throughout the year % Functionality over time. (WASH) 2. Water close to women 15 minutes from women (WASH/FS) 3. Small ruminants for women Numbers of animals. Milk production throughout year. (FS) 4. Milk used for complementary feeding MDD-I (Nutrition & FS & WASH) Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
NUTRITION RESILIENCE THROUGH NUTRITION SENSITIVE PROGRAMMING Example 1 - Indicators 1. Reliable water source available throughout the year % Functionality over time. (WASH) 2. Water close to women 15 minutes from women (WASH/FS) 3. Small ruminants for women Numbers of animals. Milk production throughout year. (FS) 4. Milk used for complementary feeding MDD-I (Nutrition & FS & WASH) Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
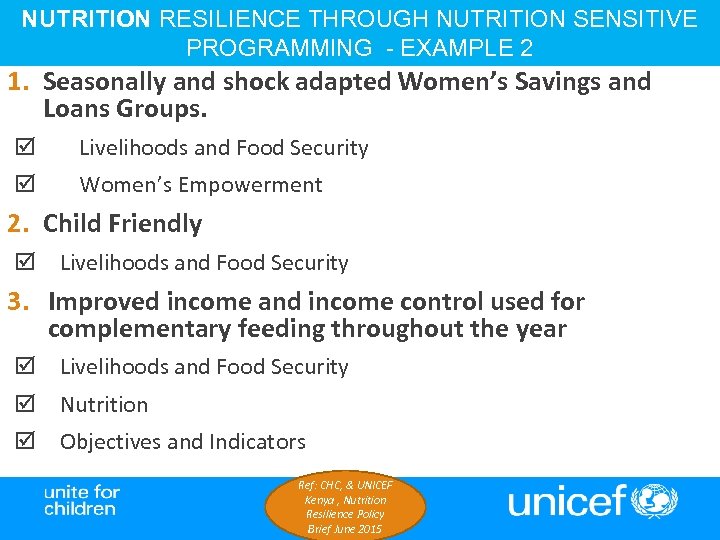 NUTRITION RESILIENCE THROUGH NUTRITION SENSITIVE PROGRAMMING - EXAMPLE 2 1. Seasonally and shock adapted Women’s Savings and Loans Groups. Livelihoods and Food Security Women’s Empowerment 2. Child Friendly Livelihoods and Food Security 3. Improved income and income control used for complementary feeding throughout the year Livelihoods and Food Security Nutrition Objectives and Indicators Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
NUTRITION RESILIENCE THROUGH NUTRITION SENSITIVE PROGRAMMING - EXAMPLE 2 1. Seasonally and shock adapted Women’s Savings and Loans Groups. Livelihoods and Food Security Women’s Empowerment 2. Child Friendly Livelihoods and Food Security 3. Improved income and income control used for complementary feeding throughout the year Livelihoods and Food Security Nutrition Objectives and Indicators Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
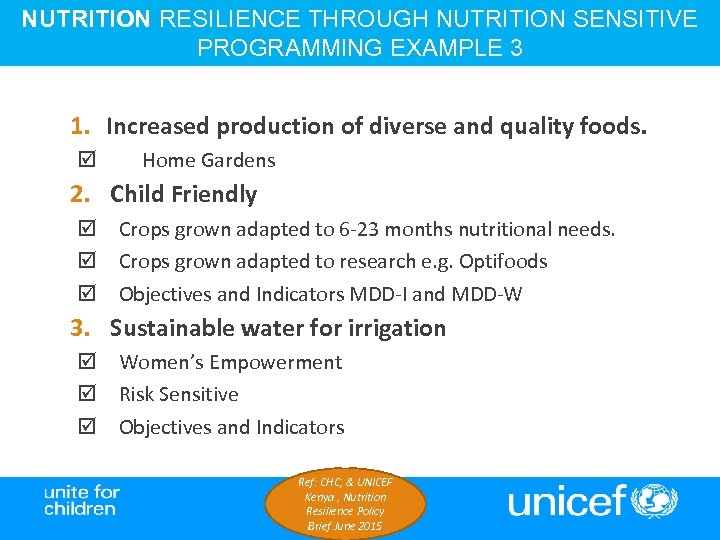 NUTRITION RESILIENCE THROUGH NUTRITION SENSITIVE PROGRAMMING EXAMPLE 3 1. Increased production of diverse and quality foods. Home Gardens 2. Child Friendly Crops grown adapted to 6 -23 months nutritional needs. Crops grown adapted to research e. g. Optifoods Objectives and Indicators MDD-I and MDD-W 3. Sustainable water for irrigation Women’s Empowerment Risk Sensitive Objectives and Indicators Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
NUTRITION RESILIENCE THROUGH NUTRITION SENSITIVE PROGRAMMING EXAMPLE 3 1. Increased production of diverse and quality foods. Home Gardens 2. Child Friendly Crops grown adapted to 6 -23 months nutritional needs. Crops grown adapted to research e. g. Optifoods Objectives and Indicators MDD-I and MDD-W 3. Sustainable water for irrigation Women’s Empowerment Risk Sensitive Objectives and Indicators Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
 Nutrition Resilience programming ØDoes not need to be a fully integrated programme. ØCan be intrasectoral implementation. ØNeeds integrated planning for joint objectives and shared M+E plan. ØCan address Chronic AND Acute Nutrition Deprivation. ØNutrition Sensitive. ØNot only integration of behaviour change Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
Nutrition Resilience programming ØDoes not need to be a fully integrated programme. ØCan be intrasectoral implementation. ØNeeds integrated planning for joint objectives and shared M+E plan. ØCan address Chronic AND Acute Nutrition Deprivation. ØNutrition Sensitive. ØNot only integration of behaviour change Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
 NUTRITION RESILIENCE AND RESILIENCE FOR NUTRITION Bottom Line…. We need BOTH Nutrition specific and sensitive Programming to be designed, planned, implemented and monitored together targeting those most nutritionally vulnerable!! Well nourished people are more resilient = Nutrition Resilience. More resilient people are better nourished = Resilience for Nutrition The measure of success of a resilience programme are reduced caseloads of acute and chronic malnutrition Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015
NUTRITION RESILIENCE AND RESILIENCE FOR NUTRITION Bottom Line…. We need BOTH Nutrition specific and sensitive Programming to be designed, planned, implemented and monitored together targeting those most nutritionally vulnerable!! Well nourished people are more resilient = Nutrition Resilience. More resilient people are better nourished = Resilience for Nutrition The measure of success of a resilience programme are reduced caseloads of acute and chronic malnutrition Ref: CHC, & UNICEF Kenya , Nutrition Resilience Policy Brief June 2015