766b57a4dff216190476d0273735fcaf.ppt
- Количество слайдов: 66
Joint Mobilization • • • Superior and inferior tibiofibular joints Talocrural joint Subtalar joint Intertarsal joints Intermetatarsal joints TMT, MTP, IP joints
Resting Positions • Talocrural joint: 10° plantar flexion • Subtalar and midtarsal joints: midrange inversion- eversion • MTP joints – #1: 20° dorsiflexion – #2 -5: 20° plantar flexion • IP joints: 20 plantar flexion
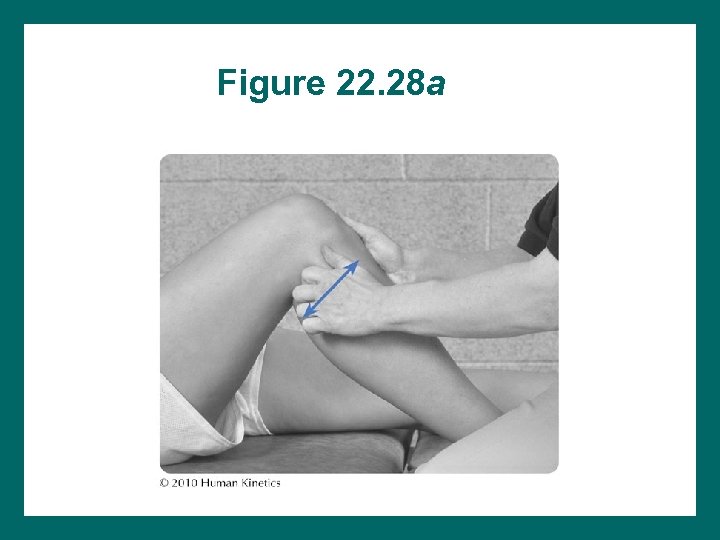
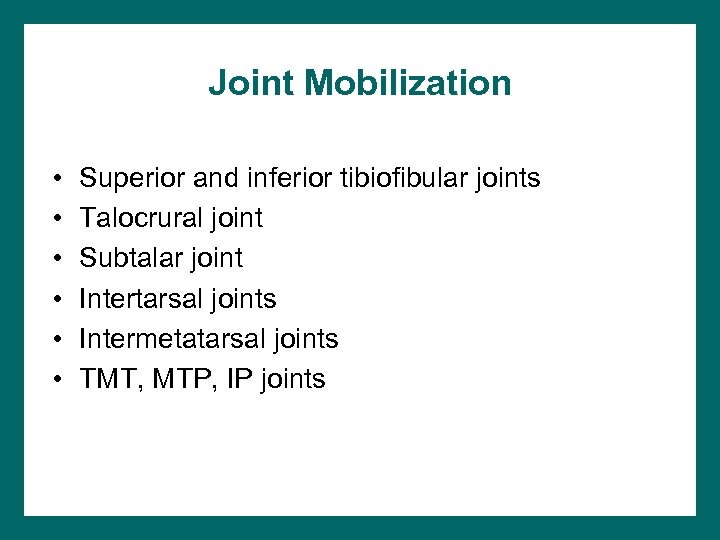
Figure 22. 28 a
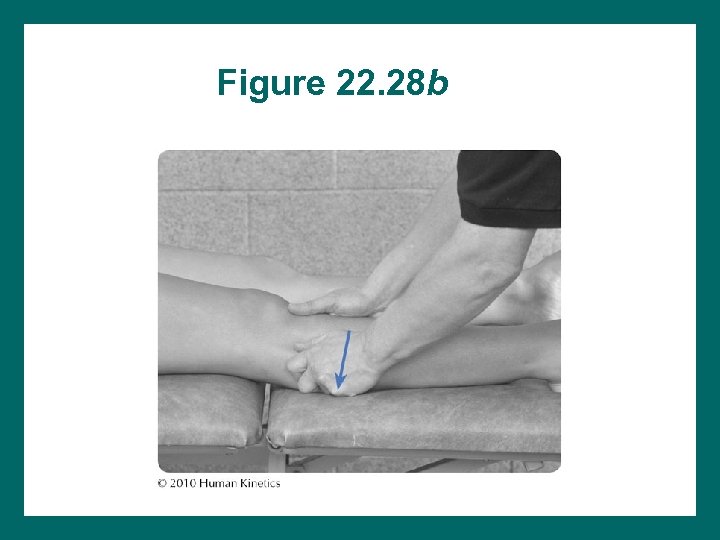
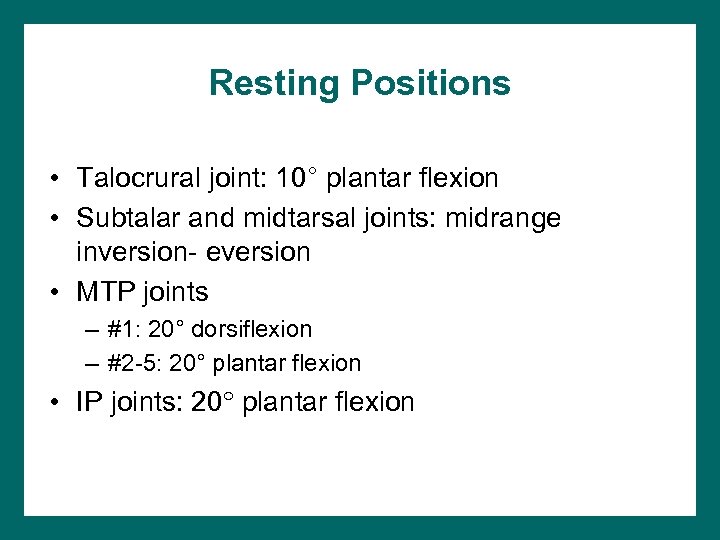
Figure 22. 28 b
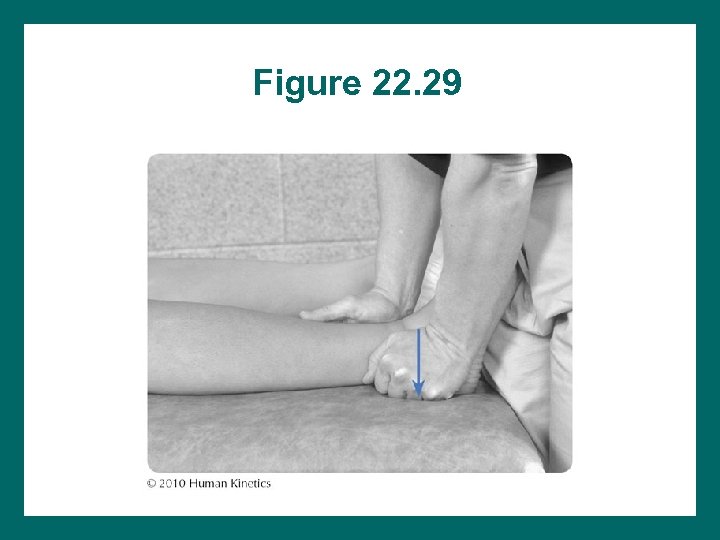
Figure 22. 29
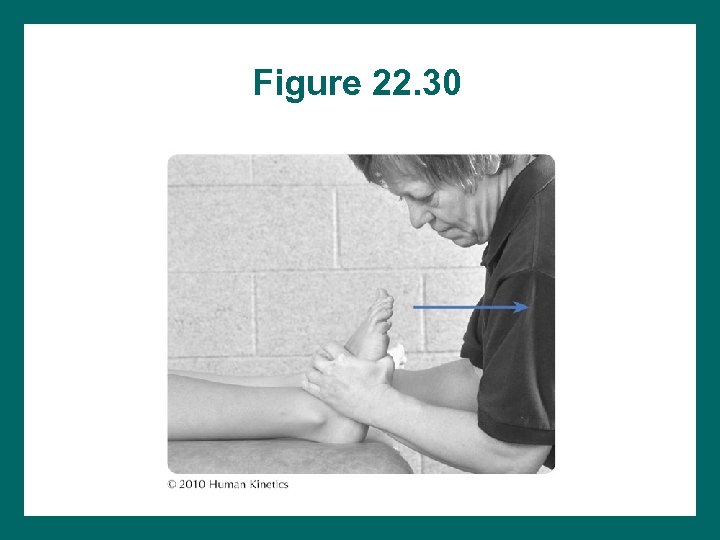
Figure 22. 30
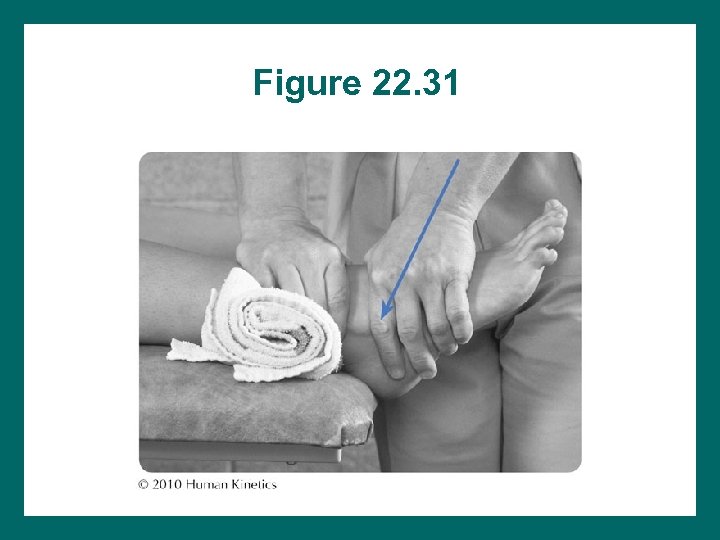
Figure 22. 31
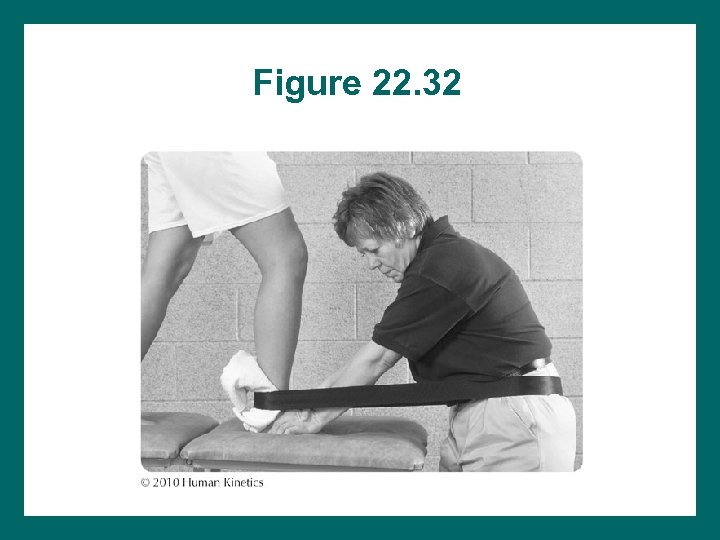
Figure 22. 32
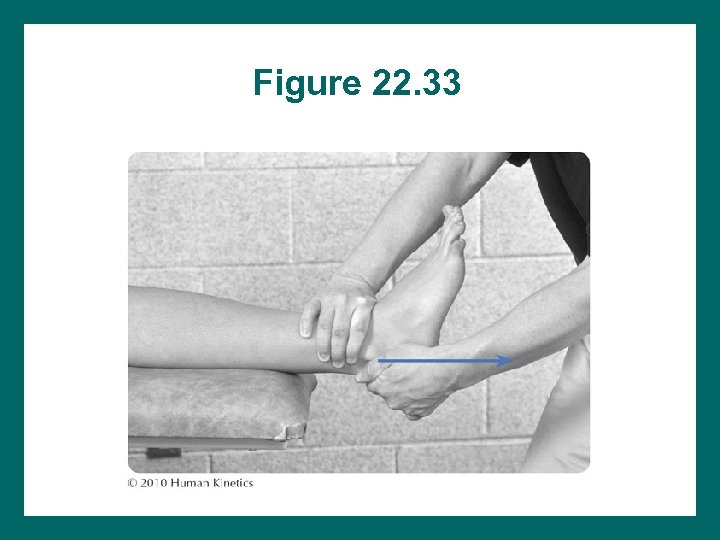
Figure 22. 33
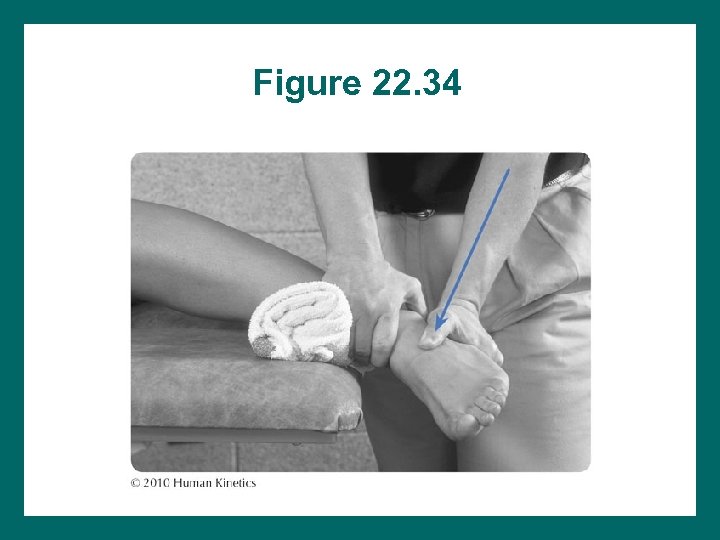
Figure 22. 34
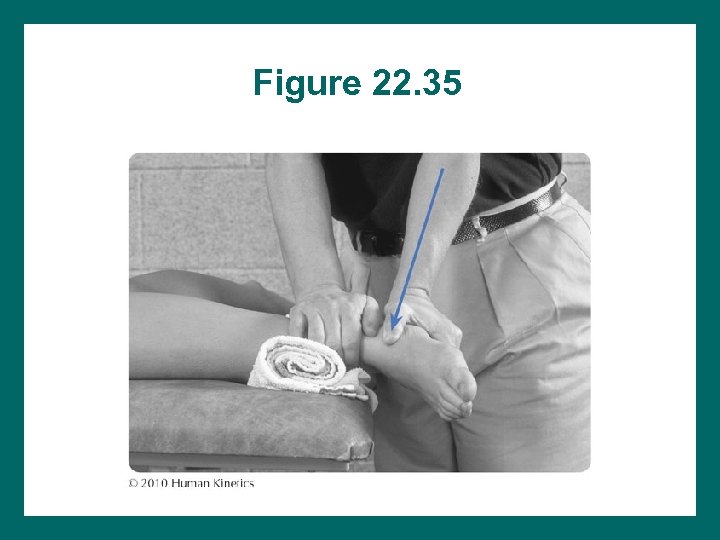
Figure 22. 35
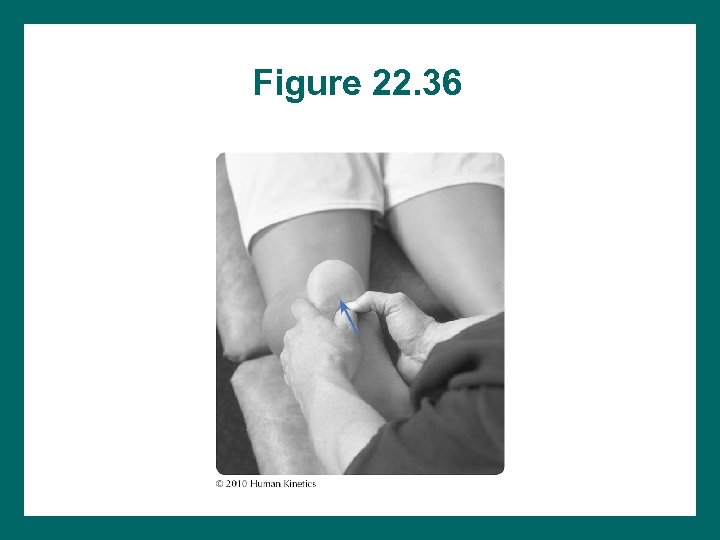
Figure 22. 36
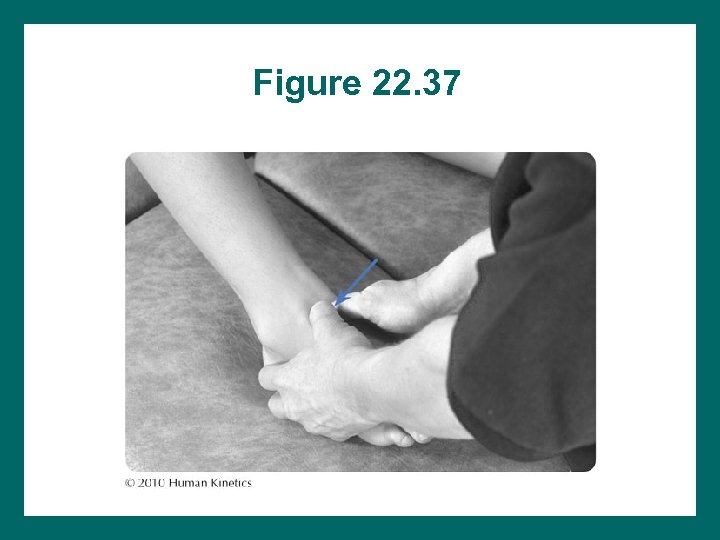
Figure 22. 37
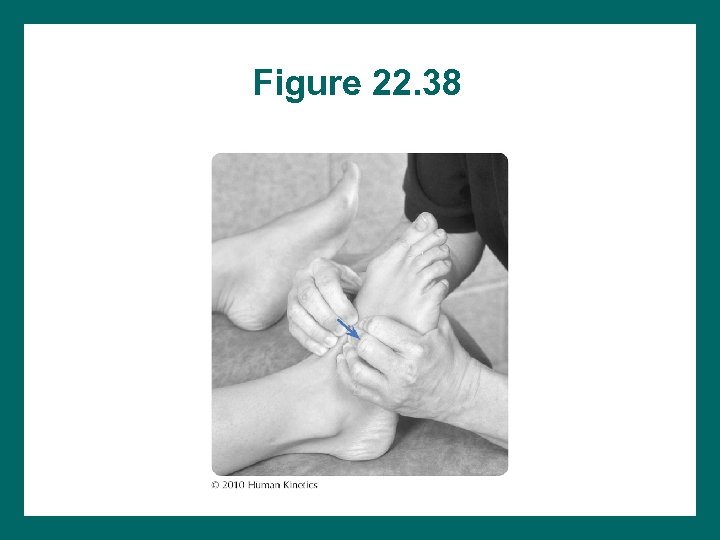
Figure 22. 38
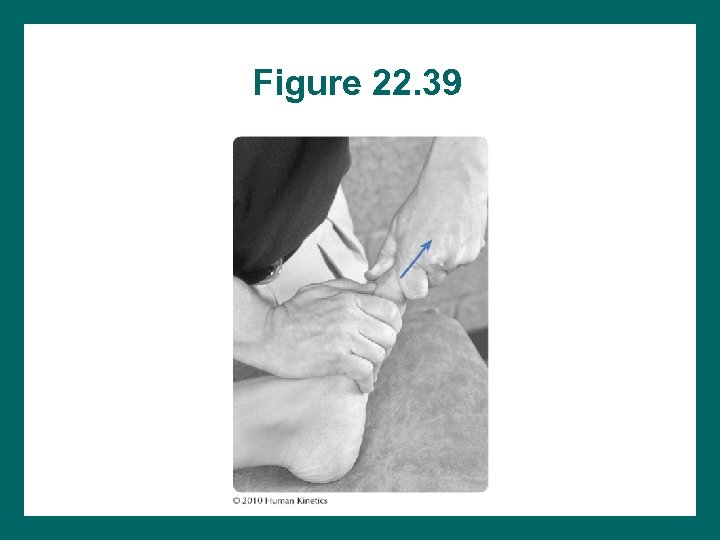
Figure 22. 39
Flexibility Exercises • • Active flexibility: 15 -20 s hold 4 -5 reps Perform throughout the day (min = 3 -4 times) May require prolonged stretch
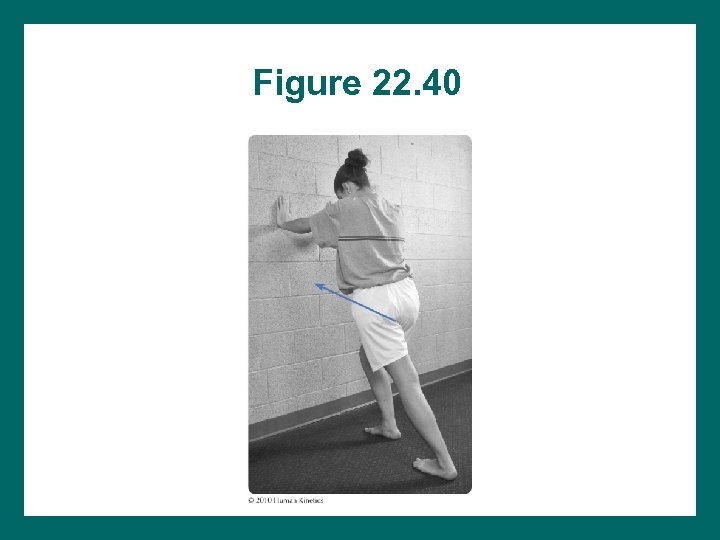
Figure 22. 40
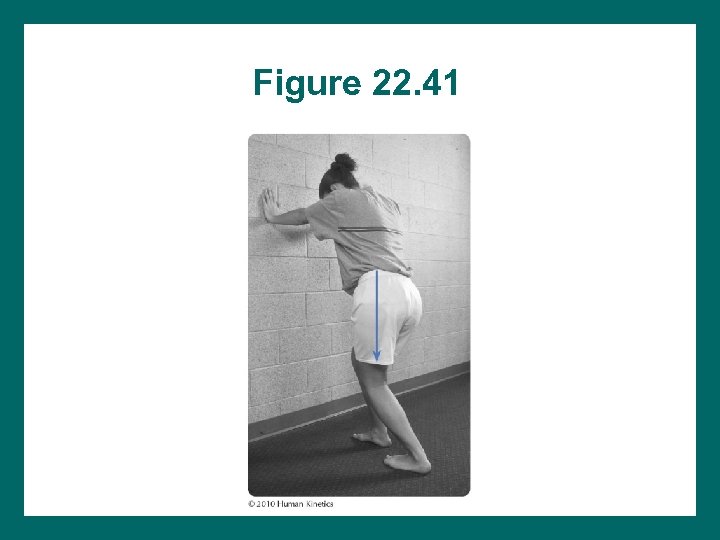
Figure 22. 41
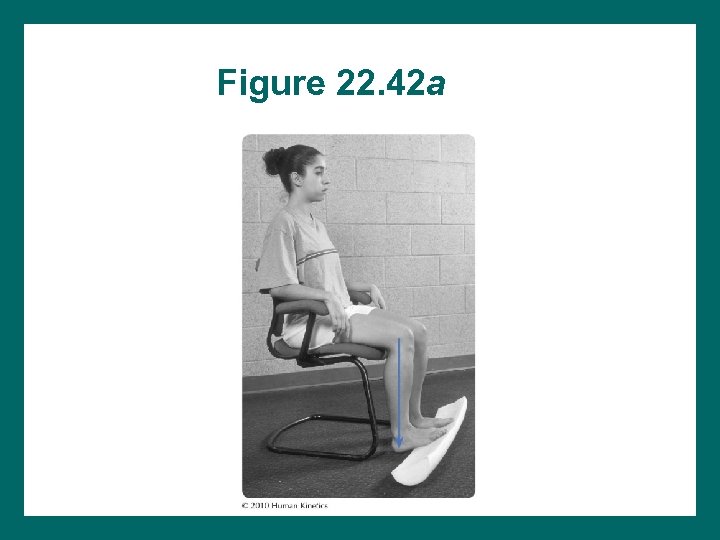
Figure 22. 42 a
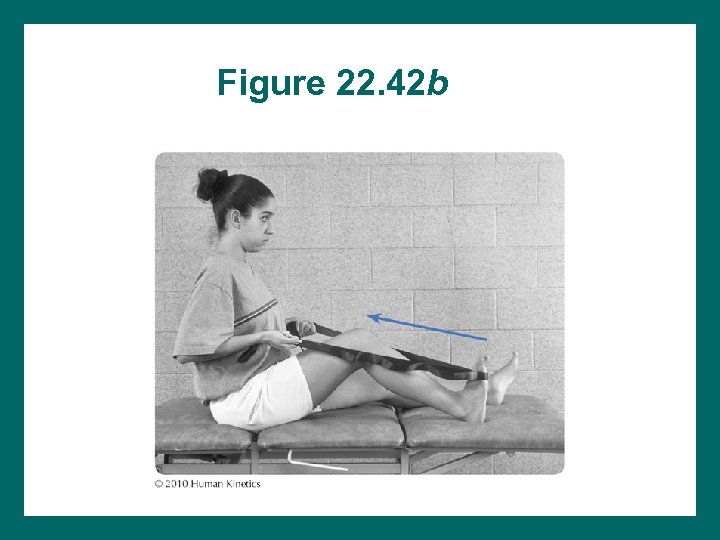
Figure 22. 42 b
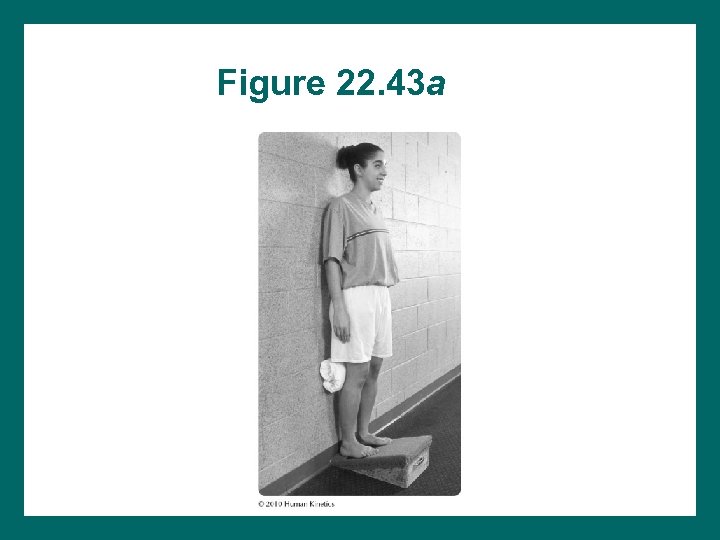
Figure 22. 43 a
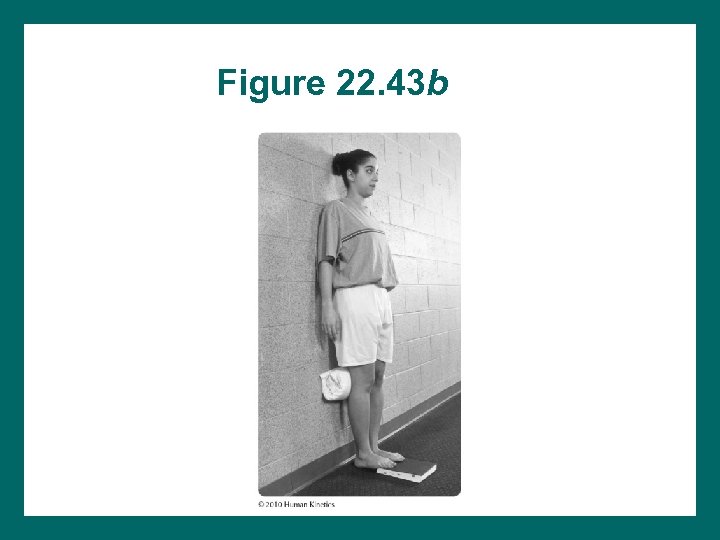
Figure 22. 43 b
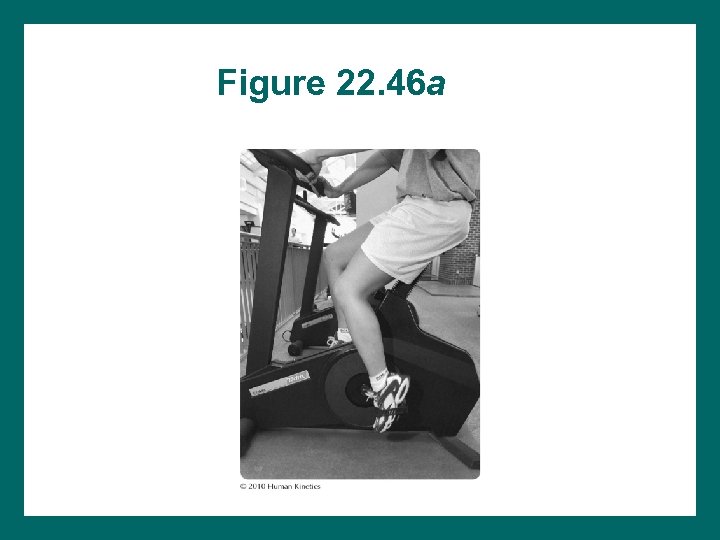
Figure 22. 46 a
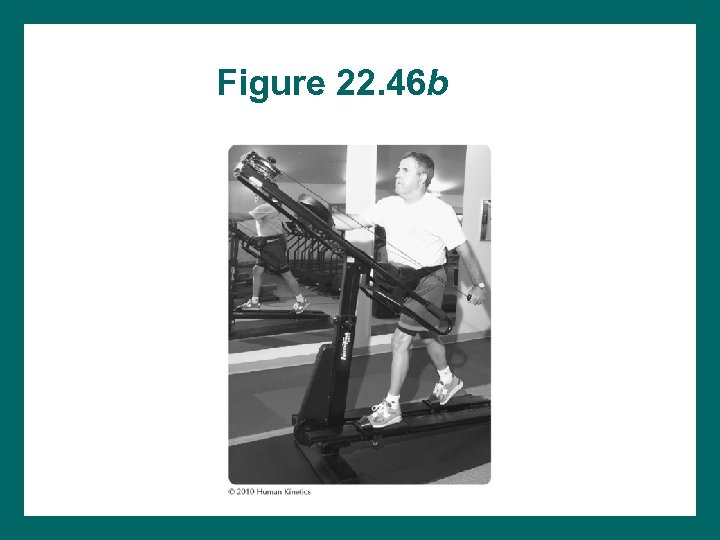
Figure 22. 46 b
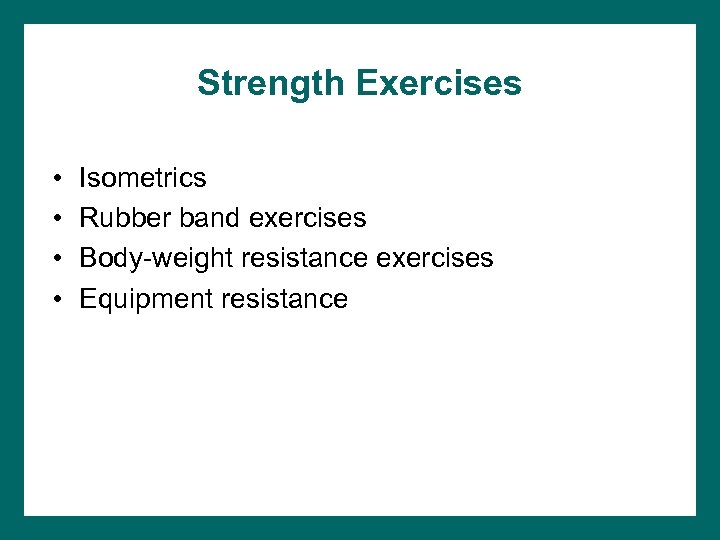
Strength Exercises • • Isometrics Rubber band exercises Body-weight resistance exercises Equipment resistance
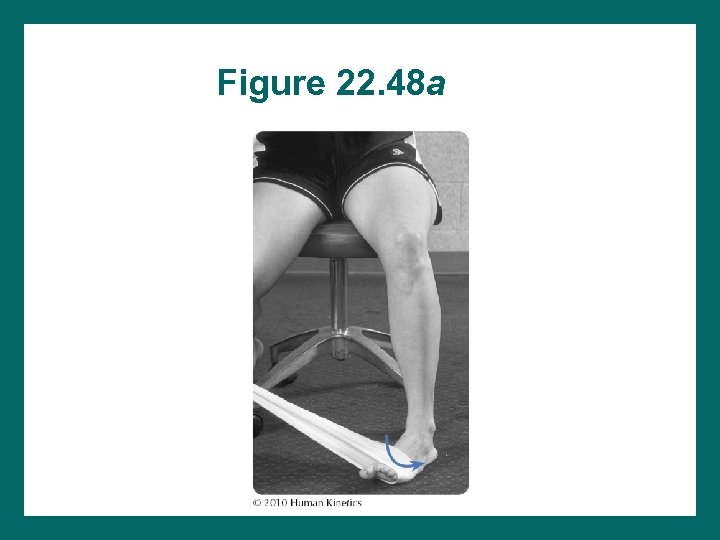
Figure 22. 48 a
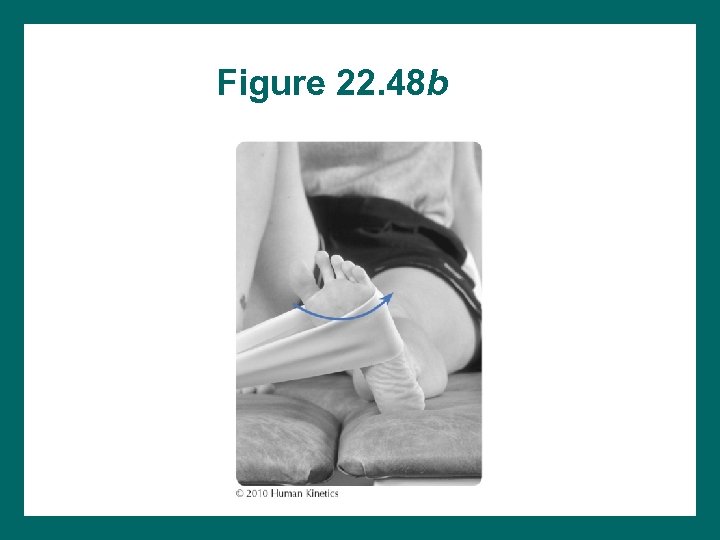
Figure 22. 48 b
Figure 22. 48 c
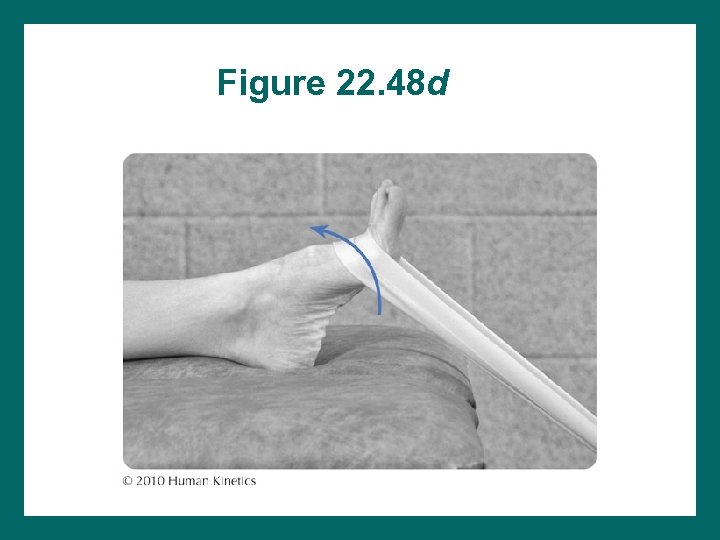
Figure 22. 48 d

Figure 22. 48 e
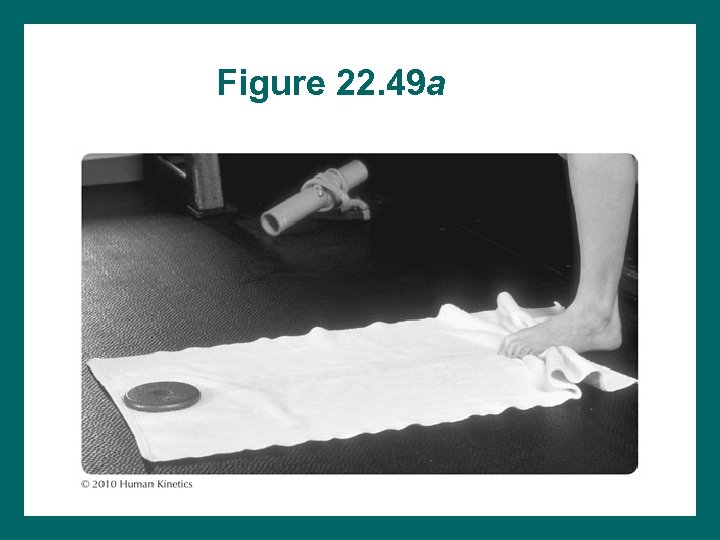
Figure 22. 49 a
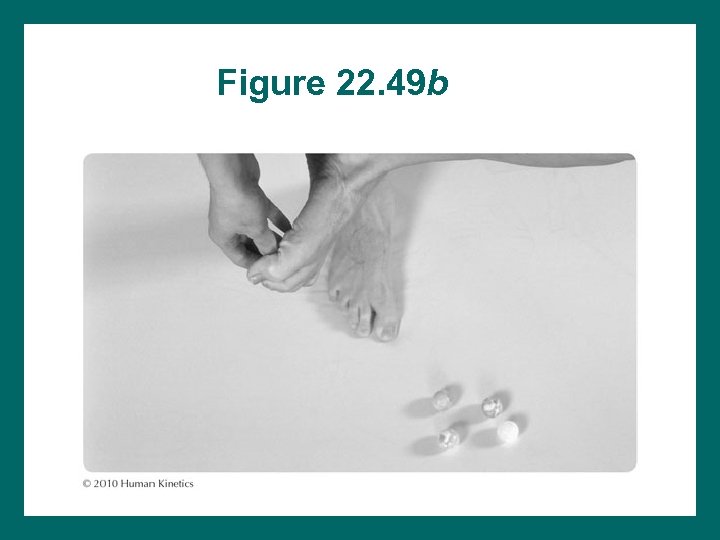
Figure 22. 49 b
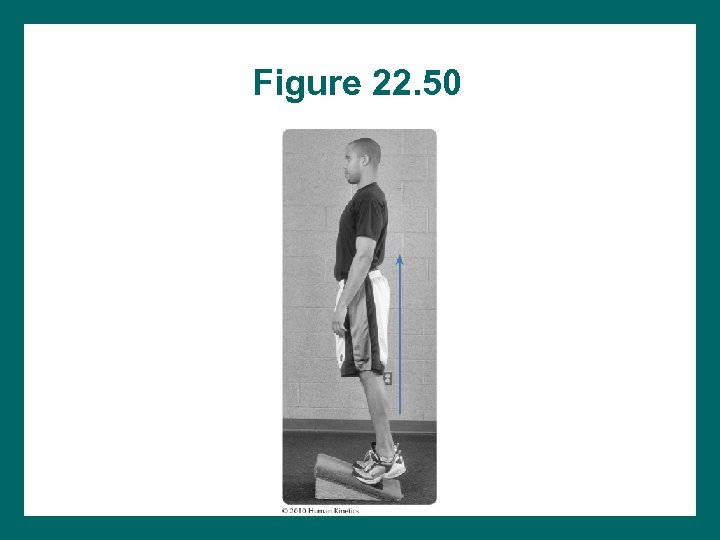
Figure 22. 50
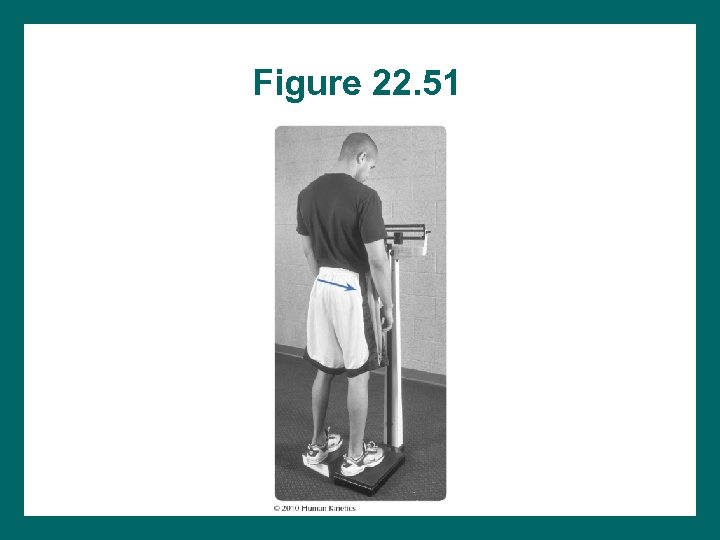
Figure 22. 51
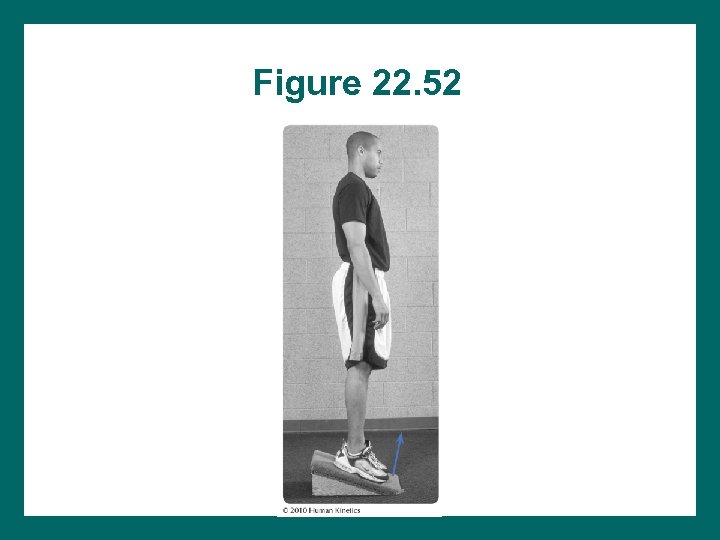
Figure 22. 52
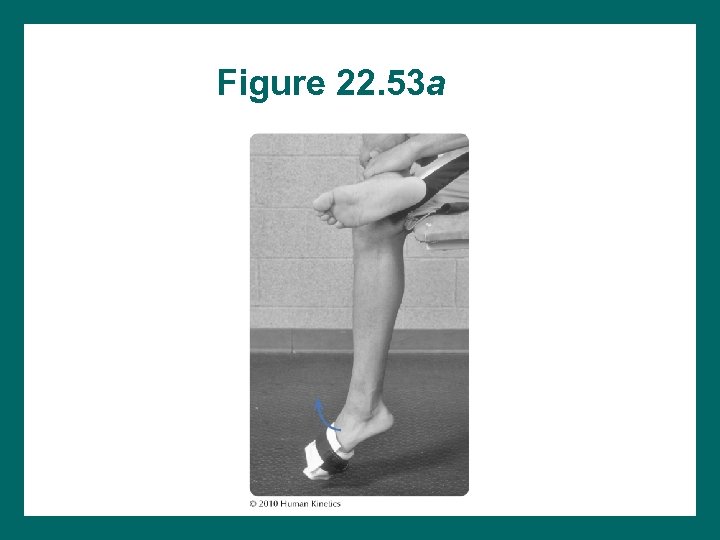
Figure 22. 53 a
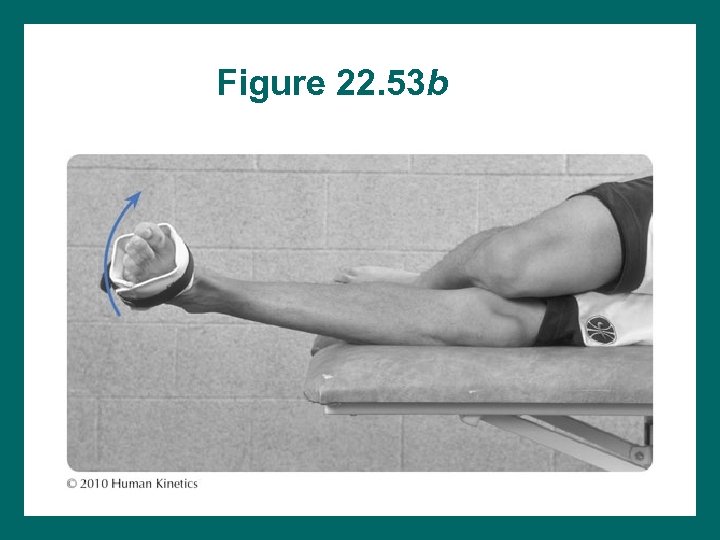
Figure 22. 53 b
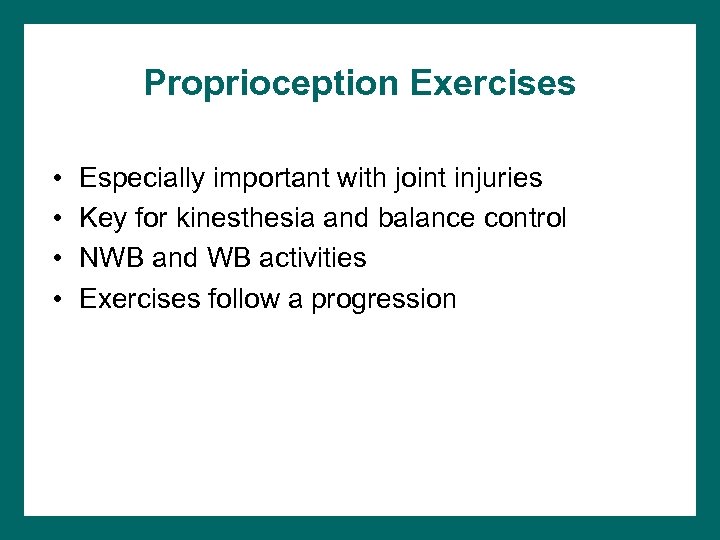
Proprioception Exercises • • Especially important with joint injuries Key for kinesthesia and balance control NWB and WB activities Exercises follow a progression
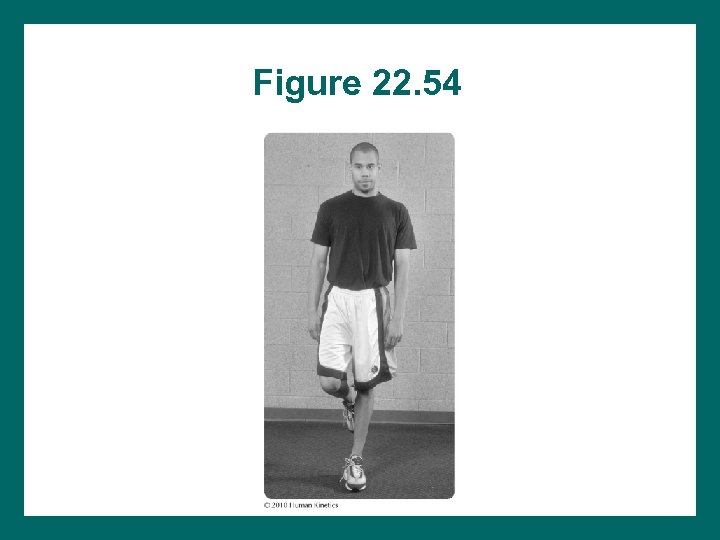
Figure 22. 54
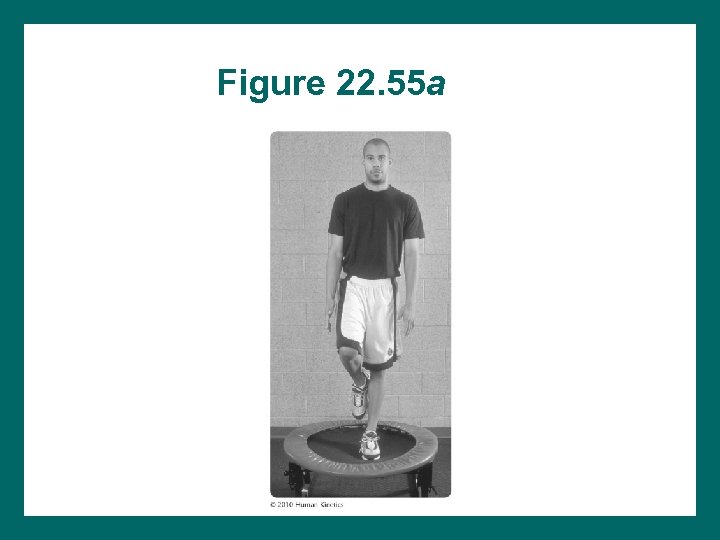
Figure 22. 55 a
Figure 22. 55 b
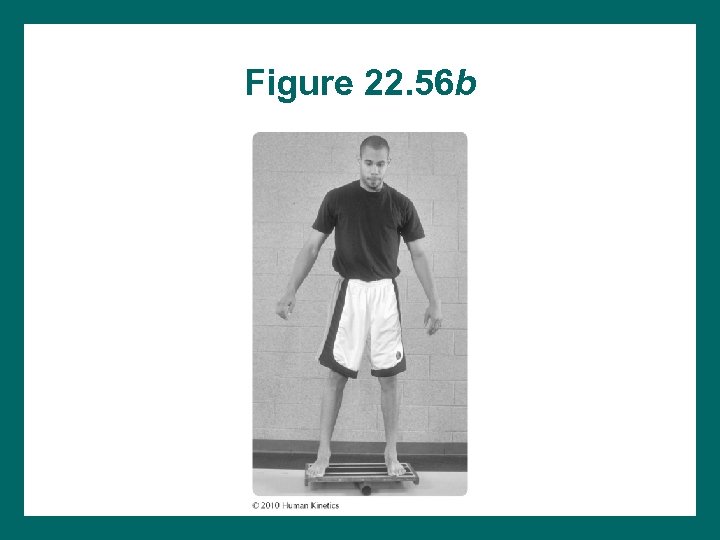
Figure 22. 56 b
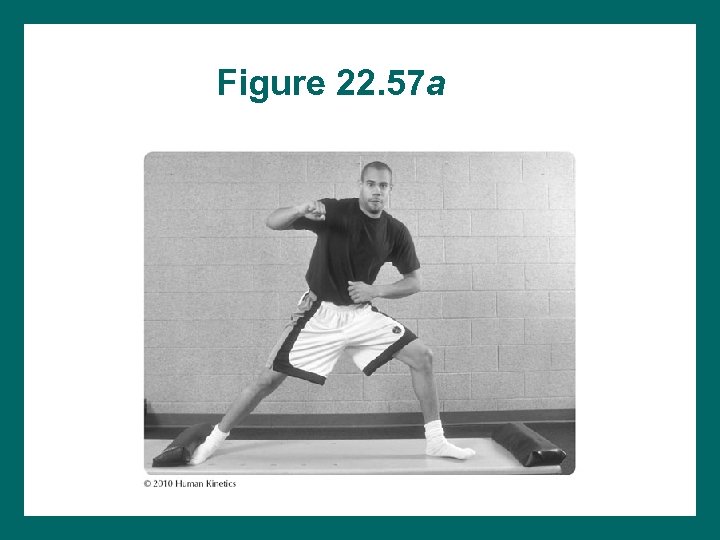
Figure 22. 57 a
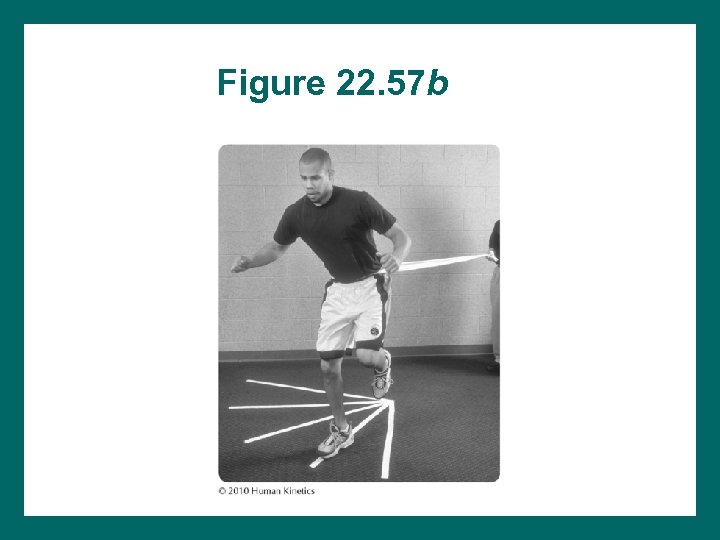
Figure 22. 57 b
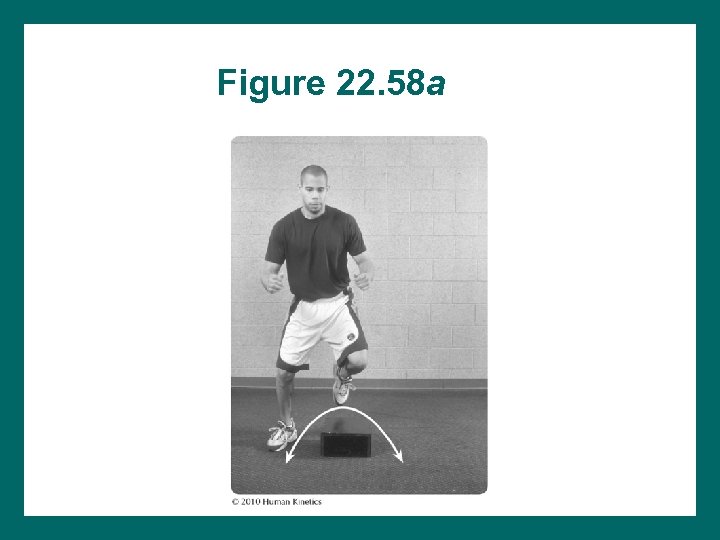
Figure 22. 58 a
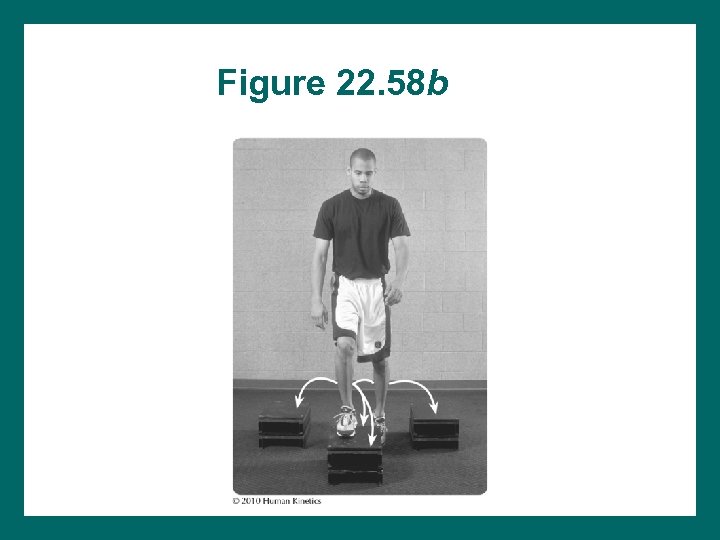
Figure 22. 58 b
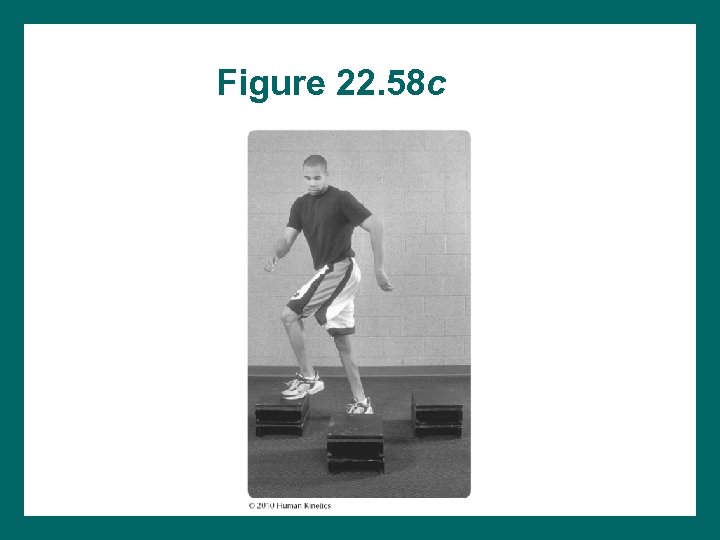
Figure 22. 58 c
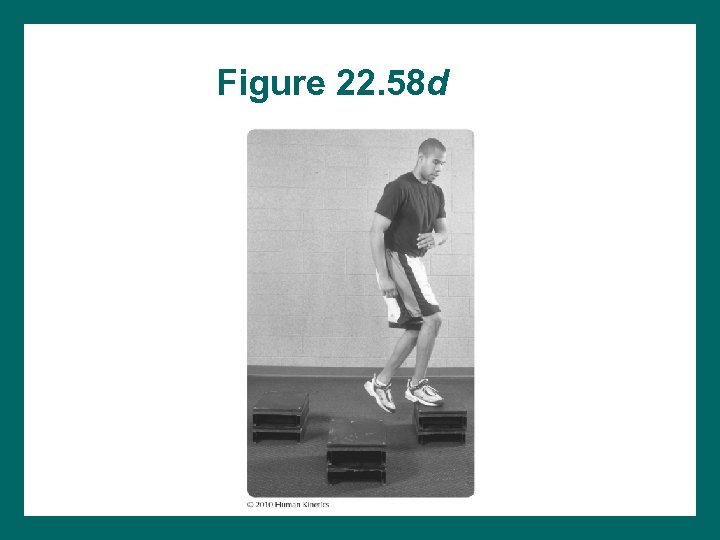
Figure 22. 58 d
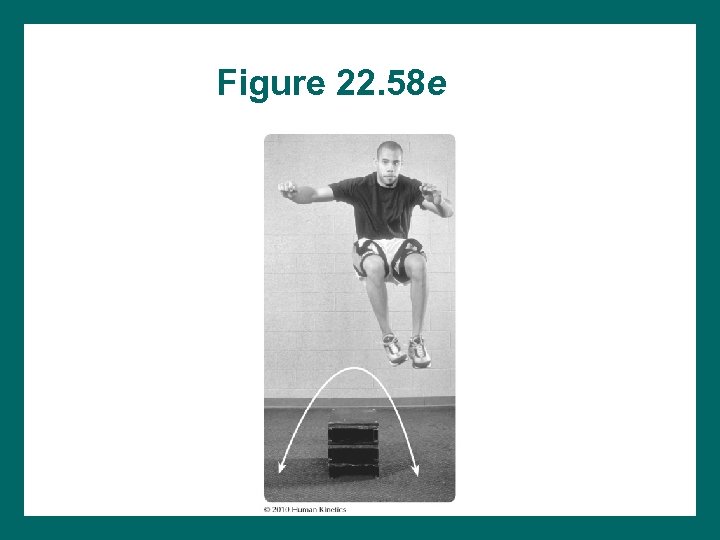
Figure 22. 58 e
Functional Activities • • • Zigzag runs Side shuffles Figure-8 runs 90° cuts to L and R Jumps, hops, leaps All performed without hesitation or favoring of involved leg
Figure 22. 59 a
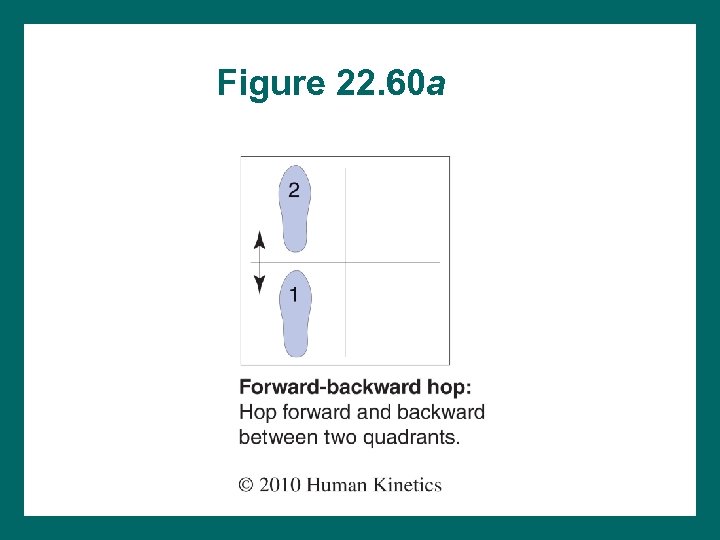
Figure 22. 60 a
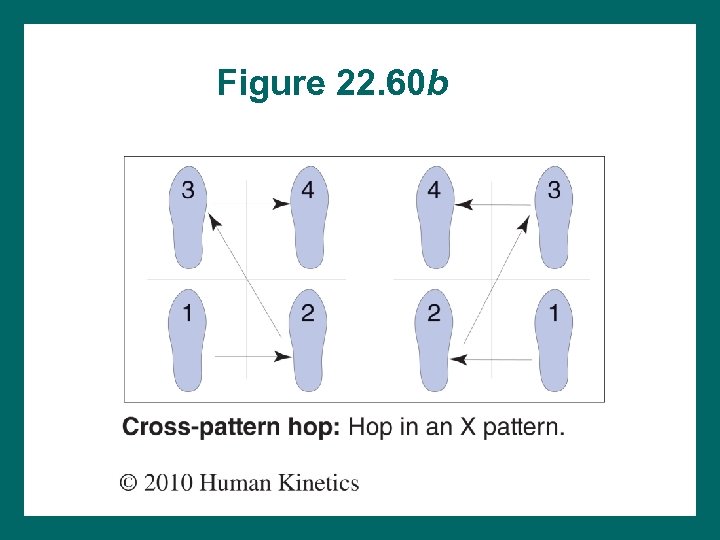
Figure 22. 60 b
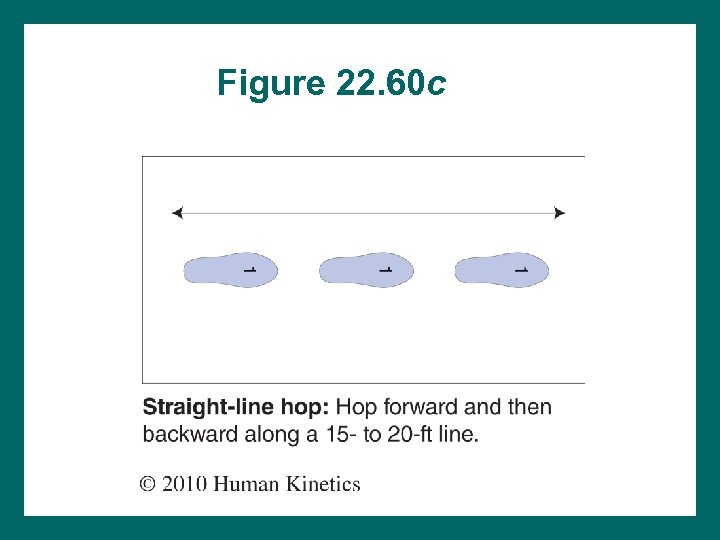
Figure 22. 60 c
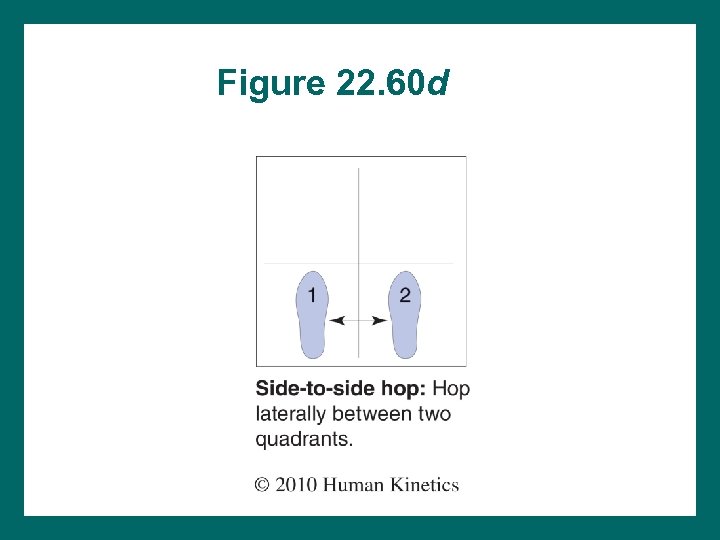
Figure 22. 60 d
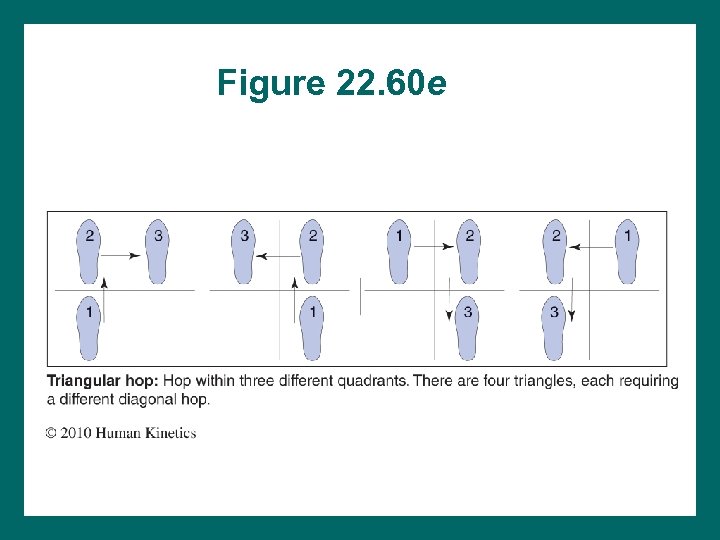
Figure 22. 60 e
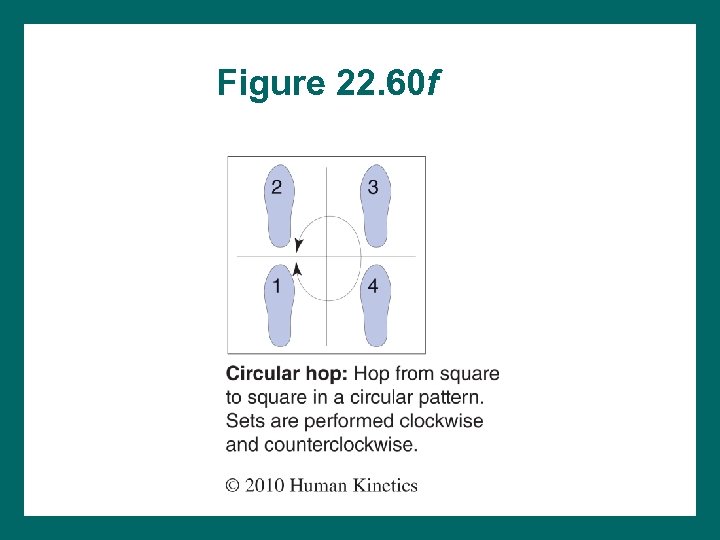
Figure 22. 60 f
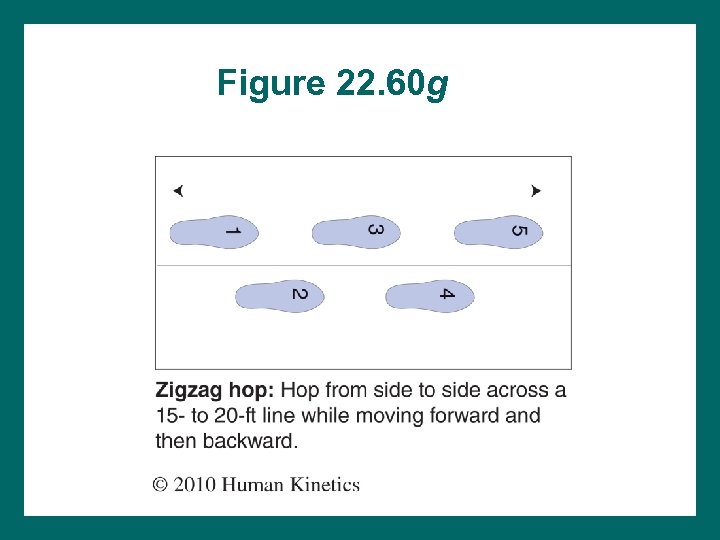
Figure 22. 60 g
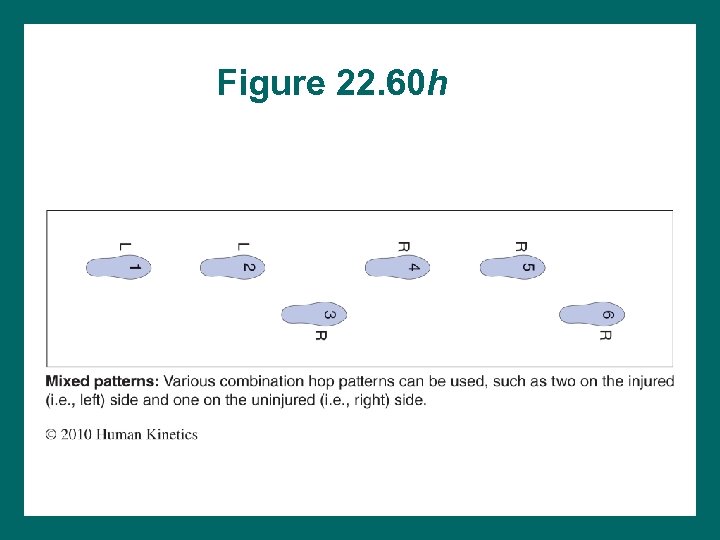
Figure 22. 60 h
Acute Ankle Sprains • Sprains of anterior tibiofibular ligament require extra WB precautions. • Control of pain and edema is the first priority. • Active range of motion (AROM) begins early. • Include strength exercises for inversion and eversion. • Peroneal strains can accompany sprains.
Chronic Ankle Sprains • • • Scar tissue can limit joint or soft-tissue mobility. Chronic muscle weakness may be present. Kinesthesia can recurrence risk Compensatory gait can reinjury risk May need additional time for rehab
Peroneal Tendon Dislocation • Often overlooked • Mechanism: ankle dorsiflexion with active peroneal contraction; inversion sprain • Inversion: most susceptible to dislocation in 15° -25° plantar flexion • Usually self-reduced • If conservative management is unsuccessful, surgery may be required
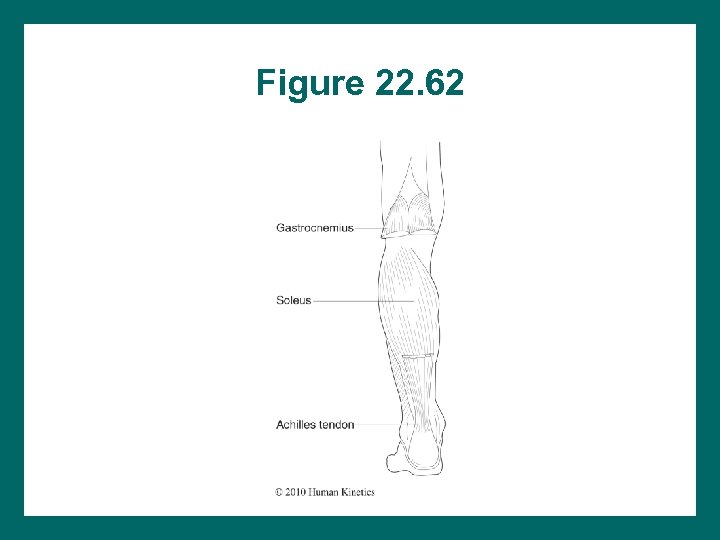
Figure 22. 62
Achilles Tendon Injuries • Prolonged pronation Achilles stress • Poorest circulation on Achilles is 2 -5 cm above insertion; susceptible site • Scar tissue palpated more medially than laterally • Must correct cause to reduce risk of tendinopathy recurrence • Surgical repair of Achilles rupture usually more successful than conservative management
Other Injuries • Chronic – – Tendinopathy: peroneals, trigger points Shin splints Compartment syndromes Foot: plantar fasciitis, tarsal tunnel syndrome, sesamoiditis • Acute – Fractures: epiphyseal, stress, acute – Turf toe – Compartment syndromes
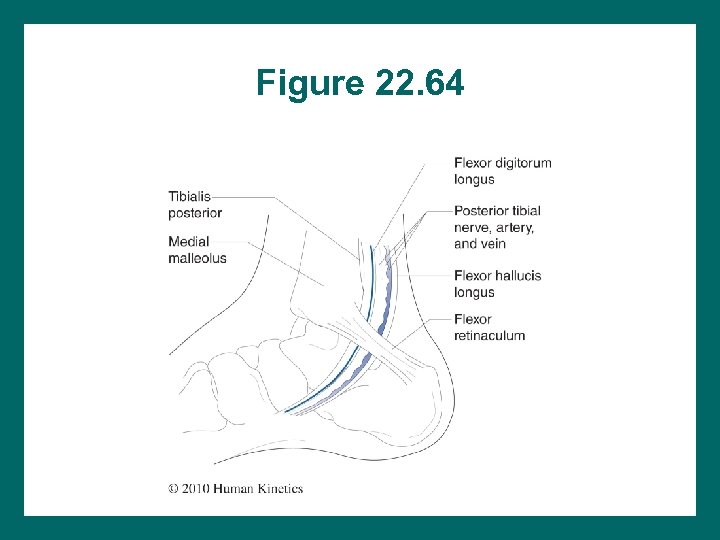
Figure 22. 64
766b57a4dff216190476d0273735fcaf.ppt