Urology-1.ppt
- Количество слайдов: 44
 Ivano-Frankivsk National Medical University Chair of Pediatric Surgery and Pediatrics Propaedeutic Lecture for students of the 5 th year on the topic: "Urolithiasis. Edematous scrotum syndrome. Traumatic injuries of the urinary system"
Ivano-Frankivsk National Medical University Chair of Pediatric Surgery and Pediatrics Propaedeutic Lecture for students of the 5 th year on the topic: "Urolithiasis. Edematous scrotum syndrome. Traumatic injuries of the urinary system"
 Plan of the lecture: l Etiology and pathogenesis of urolithiasis. l Clinic and diagnosis of urolithiasis. l Treatment of urolithiasis in children. l Syndrome of swollen scrotum in boys: clinic and diagnostics, tactics of treatment. l Injuries of the testicles and scrotum. l Injuries of the kidney in children. l Injuries of the urinary tract organs in children.
Plan of the lecture: l Etiology and pathogenesis of urolithiasis. l Clinic and diagnosis of urolithiasis. l Treatment of urolithiasis in children. l Syndrome of swollen scrotum in boys: clinic and diagnostics, tactics of treatment. l Injuries of the testicles and scrotum. l Injuries of the kidney in children. l Injuries of the urinary tract organs in children.
 Urolithiasis l Found in many countries. There are countries where it is very common, but there are regions in which are very rare. l In Ukraine endemic in urolithiasis areas of Donbass, Dnipropetrovsk and Kharkiv regions. l Carpathians although not endemic region in this pathology, but its incidence in children is increasing every year.
Urolithiasis l Found in many countries. There are countries where it is very common, but there are regions in which are very rare. l In Ukraine endemic in urolithiasis areas of Donbass, Dnipropetrovsk and Kharkiv regions. l Carpathians although not endemic region in this pathology, but its incidence in children is increasing every year.
 Etiology and pathogenesis of Urolithiasis Crystallization theory: Violation of colloidal status crystallization of urine salts. Normally urine is an ultrafiltrate of blood plasma, which contains large amount of mineral and organic products metabolism, residual products of metabolism that are in suspended form or dissolved due to the presence of stabilizing colloids in urine. Its system may be disrupted by changing the reaction and surface tension of urine, difficulties outflow of urine, the presence of bacteria in urine, leukocytes, fibrin. Thus there is deposition of salts, crystalline particles, which then serve as cores for future stones are formed.
Etiology and pathogenesis of Urolithiasis Crystallization theory: Violation of colloidal status crystallization of urine salts. Normally urine is an ultrafiltrate of blood plasma, which contains large amount of mineral and organic products metabolism, residual products of metabolism that are in suspended form or dissolved due to the presence of stabilizing colloids in urine. Its system may be disrupted by changing the reaction and surface tension of urine, difficulties outflow of urine, the presence of bacteria in urine, leukocytes, fibrin. Thus there is deposition of salts, crystalline particles, which then serve as cores for future stones are formed.
 Matrix theory l Basis of stone is organic core (matrix), on which are superimposed the salt crystals. This is confirmed by the fact, that each urinary stone consists of two components: an organic matrix (2 -3% of stone) and the mineral, which is intimately associated with the matrix. l Significant role in the etiology of urolithiasis play: vitamin deficiencies, hyperparathyroidism, urinary tract infection, violation of the urine outflow, damage of the brain and spinal cord, damage of skeleton, hyperthermia, a way of life.
Matrix theory l Basis of stone is organic core (matrix), on which are superimposed the salt crystals. This is confirmed by the fact, that each urinary stone consists of two components: an organic matrix (2 -3% of stone) and the mineral, which is intimately associated with the matrix. l Significant role in the etiology of urolithiasis play: vitamin deficiencies, hyperparathyroidism, urinary tract infection, violation of the urine outflow, damage of the brain and spinal cord, damage of skeleton, hyperthermia, a way of life.
 Etiology and pathogenesis of Urolithiasis l Very important are: metabolic disorders, diseases of the digestive tract, especially the food, social and living conditions. l The child's body contains more extracellular fluid, which is easily lost during diarrhea, vomiting, fever. Dehydration leads to oliguria and increased concentration of urine, which promotes stone formation. l Thus, an important factor, contributing to the formation of stones, is urine stasis. In turn, urinary tract stones lead to urine stasis.
Etiology and pathogenesis of Urolithiasis l Very important are: metabolic disorders, diseases of the digestive tract, especially the food, social and living conditions. l The child's body contains more extracellular fluid, which is easily lost during diarrhea, vomiting, fever. Dehydration leads to oliguria and increased concentration of urine, which promotes stone formation. l Thus, an important factor, contributing to the formation of stones, is urine stasis. In turn, urinary tract stones lead to urine stasis.
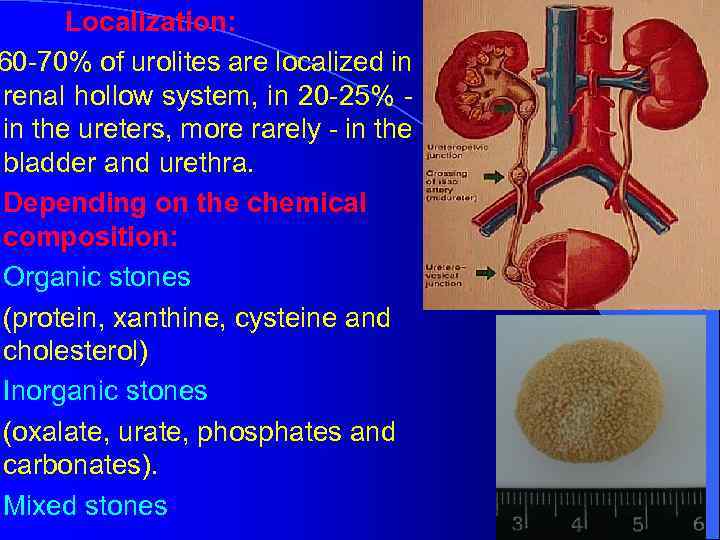 Localization: 60 -70% of urolites are localized in renal hollow system, in 20 -25% - in the ureters, more rarely - in the bladder and urethra. Depending on the chemical composition: Organic stones (protein, xanthine, cysteine and cholesterol) Inorganic stones (oxalate, urate, phosphates and carbonates). Mixed stones
Localization: 60 -70% of urolites are localized in renal hollow system, in 20 -25% - in the ureters, more rarely - in the bladder and urethra. Depending on the chemical composition: Organic stones (protein, xanthine, cysteine and cholesterol) Inorganic stones (oxalate, urate, phosphates and carbonates). Mixed stones
 Clinical picture of Urolithiasis l Depends on the child's age, size and location of stones. In children older, than 7 years, often the first manifestation of urolithiasis is renal colic. l In renal colic arises anxiety child, sharp abdominal pain accompanied by nausea and vomiting. When pain patients twists, taking forced position. In children under 7 years renal colic is rare due to the fact, that they have relatively wide ureter. l Uncomplicated urolithiasis appears aching pain in the abdomen and lumbar region. There hematuria, especially after physical activity.
Clinical picture of Urolithiasis l Depends on the child's age, size and location of stones. In children older, than 7 years, often the first manifestation of urolithiasis is renal colic. l In renal colic arises anxiety child, sharp abdominal pain accompanied by nausea and vomiting. When pain patients twists, taking forced position. In children under 7 years renal colic is rare due to the fact, that they have relatively wide ureter. l Uncomplicated urolithiasis appears aching pain in the abdomen and lumbar region. There hematuria, especially after physical activity.
 Clinical picture of Urolithiasis l The cause of hematuria is mucosal injury by concrements, joining infections. Reliable sign of urolithiasis is the stone in urine. l Very quickly urolithiasis is complicated by infection and the development of pyelonephritis: the pain does not go out, there is a fever, frequent painful urination, thus leaving turbid urine. The patient worsens sleep and appetite, nausea worried, pale skin. l Another complication is hydronephrosis, that occurs after occlusion of ureter by stone. When occlusion two ureters or urethra occurs anuria.
Clinical picture of Urolithiasis l The cause of hematuria is mucosal injury by concrements, joining infections. Reliable sign of urolithiasis is the stone in urine. l Very quickly urolithiasis is complicated by infection and the development of pyelonephritis: the pain does not go out, there is a fever, frequent painful urination, thus leaving turbid urine. The patient worsens sleep and appetite, nausea worried, pale skin. l Another complication is hydronephrosis, that occurs after occlusion of ureter by stone. When occlusion two ureters or urethra occurs anuria.
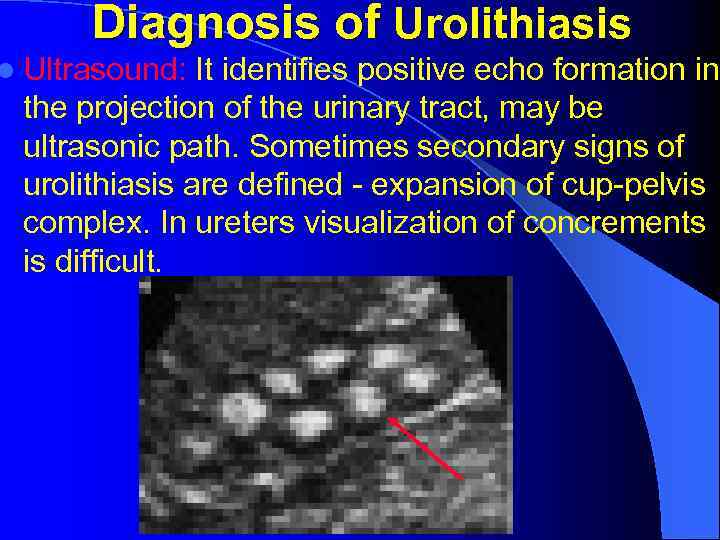 Diagnosis of Urolithiasis l Ultrasound: It identifies positive echo formation in the projection of the urinary tract, may be ultrasonic path. Sometimes secondary signs of urolithiasis are defined - expansion of cup-pelvis complex. In ureters visualization of concrements is difficult.
Diagnosis of Urolithiasis l Ultrasound: It identifies positive echo formation in the projection of the urinary tract, may be ultrasonic path. Sometimes secondary signs of urolithiasis are defined - expansion of cup-pelvis complex. In ureters visualization of concrements is difficult.
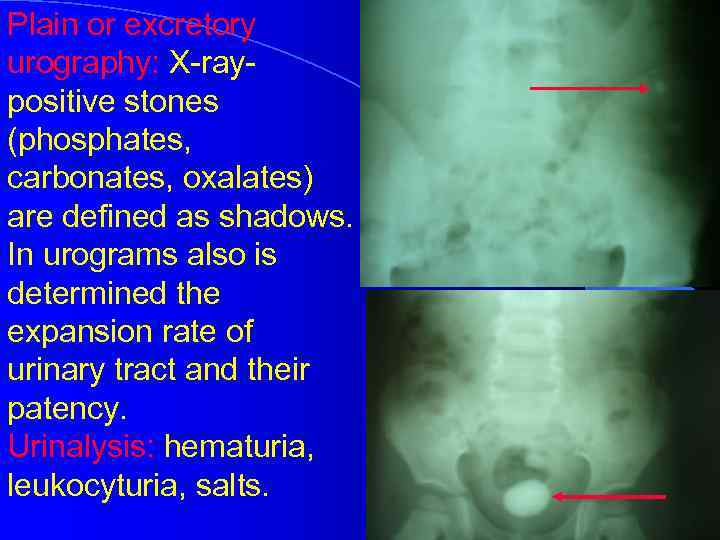 Plain or excretory urography: X-raypositive stones (phosphates, carbonates, oxalates) are defined as shadows. In urograms also is determined the expansion rate of urinary tract and their patency. Urinalysis: hematuria, leukocyturia, salts.
Plain or excretory urography: X-raypositive stones (phosphates, carbonates, oxalates) are defined as shadows. In urograms also is determined the expansion rate of urinary tract and their patency. Urinalysis: hematuria, leukocyturia, salts.
 Treatment of Urolithiasis l Conservative: the introduction of analgesics and antispasmodics, non-steroidal anti-inflammatory drugs. Assign thermal treatments (bath, hot water bottle), novocaine blockade of the spermatic cord or the round ligament of the uterus. During prolonged colic catheterization of the ureter is indicated. It is recommended to drink plenty of fluids. Physiotherapy treatment (Diathermy, Vibrotherapy) is applied. l If you can not obtain a discharge of stones with conservative methods, the method of extracorporeal lithotripsy is used.
Treatment of Urolithiasis l Conservative: the introduction of analgesics and antispasmodics, non-steroidal anti-inflammatory drugs. Assign thermal treatments (bath, hot water bottle), novocaine blockade of the spermatic cord or the round ligament of the uterus. During prolonged colic catheterization of the ureter is indicated. It is recommended to drink plenty of fluids. Physiotherapy treatment (Diathermy, Vibrotherapy) is applied. l If you can not obtain a discharge of stones with conservative methods, the method of extracorporeal lithotripsy is used.
 Treatment of Urolithiasis l With the ineffectiveness of all these methods is carried out surgical treatment, whose purpose is not only to remove the stones, but also eliminating the causes of urostasis. l After removal of urolites treatment should be aimed at preventing stone formation: diet, vitamins, mineral water, spa treatment. l Equally important in the prevention of urolithiasis is treatment of pyelonephritis.
Treatment of Urolithiasis l With the ineffectiveness of all these methods is carried out surgical treatment, whose purpose is not only to remove the stones, but also eliminating the causes of urostasis. l After removal of urolites treatment should be aimed at preventing stone formation: diet, vitamins, mineral water, spa treatment. l Equally important in the prevention of urolithiasis is treatment of pyelonephritis.
 Syndrome of swollen scrotum l is a group of acute illnesses of the testicles and appendages, requiring urgent surgery. l For a long time, various acute diseases of the scrotum was united in diagnosis of "acute orchitis" and treated conservatively. This tactic resulted in a high frequency of hypoplasia or atrophy of the testes and in the future - to violations of reproductive function. 1) Torsion of the spermatic cord. 2) Torsion of hydatis testicles. 3) Acute orchiepididymitis. 4) Injuries of the testicles.
Syndrome of swollen scrotum l is a group of acute illnesses of the testicles and appendages, requiring urgent surgery. l For a long time, various acute diseases of the scrotum was united in diagnosis of "acute orchitis" and treated conservatively. This tactic resulted in a high frequency of hypoplasia or atrophy of the testes and in the future - to violations of reproductive function. 1) Torsion of the spermatic cord. 2) Torsion of hydatis testicles. 3) Acute orchiepididymitis. 4) Injuries of the testicles.
 Torsion of the spermatic cord l Most commonly occurs in children under 1 year and in the pubertal age (90%). l The cause of spermatic cord torsion (SCT) is a sharp reduction of muscle, that raises the testicle, the fibers of which have a spiraling motion. l Preferably there intravaginal torsion (inside the vaginal membrane testes), but in children under 1 year is more common testicular torsion with shells (extravaginal form). l Crucial importance in the etiopathogenesis of torsion has morphological immaturity of the spermatic cord.
Torsion of the spermatic cord l Most commonly occurs in children under 1 year and in the pubertal age (90%). l The cause of spermatic cord torsion (SCT) is a sharp reduction of muscle, that raises the testicle, the fibers of which have a spiraling motion. l Preferably there intravaginal torsion (inside the vaginal membrane testes), but in children under 1 year is more common testicular torsion with shells (extravaginal form). l Crucial importance in the etiopathogenesis of torsion has morphological immaturity of the spermatic cord.
 Complications of SCT l Acute impairment of blood and lymph circulation and development of the hemorrhagic infarct of testis. l Irreversible pathological changes in the testis occurs very quickly, and after 6 -10 hours after torsion occurs necrosis. l Immune reactions, resulting SCT, can lead to dysfunction also healthy (contralateral) testis.
Complications of SCT l Acute impairment of blood and lymph circulation and development of the hemorrhagic infarct of testis. l Irreversible pathological changes in the testis occurs very quickly, and after 6 -10 hours after torsion occurs necrosis. l Immune reactions, resulting SCT, can lead to dysfunction also healthy (contralateral) testis.
 Clinic of SCT l In patient occurs acute pain in the affected part of the scrotum, sometimes align also general complaints - fainting, pale skin, cold sweat, nausea. l Pain can irradiate in the inguinal area. l On examination, swelling and redness of skin scrotum are marked, in palpation is defined enlarged, dense, sharply painful testicle. Spermatic cord is thickened and compacted. l Location of testicle is changed - toned to the top of scrotum.
Clinic of SCT l In patient occurs acute pain in the affected part of the scrotum, sometimes align also general complaints - fainting, pale skin, cold sweat, nausea. l Pain can irradiate in the inguinal area. l On examination, swelling and redness of skin scrotum are marked, in palpation is defined enlarged, dense, sharply painful testicle. Spermatic cord is thickened and compacted. l Location of testicle is changed - toned to the top of scrotum.
 Diagnosis of SCT l Diafanoskopy (ray bright light)- testicle not enlightened l Ultrasound, Doppler of testicle and spermatic cord vessels - venous stasis, depleted blood circulation, induration of testicles are defined. l The differential diagnosis must spend with tumors also other acute diseases of the testes.
Diagnosis of SCT l Diafanoskopy (ray bright light)- testicle not enlightened l Ultrasound, Doppler of testicle and spermatic cord vessels - venous stasis, depleted blood circulation, induration of testicles are defined. l The differential diagnosis must spend with tumors also other acute diseases of the testes.
 Treatment of SCT l l l Surgery, should be performed immediately upon diagnosis or even with suspected it. Access is scrotal or inguinal. After untwisting the spermatic cord (detorsion), novocaine blockade of it and warming of testicle by damp cloth with warm solution are conducted. The viability of testicle (color, luster membranes) is evaluated, testis is fixed by sutures to separate membranes of scrotum, scrotum is drained by a rubber drainage. If necrotic testicle, orchidektomy is performed, then fixation the opposite testicle is carried out. Anti-inflammatory drugs, vitamins A, E, C, Heparin,
Treatment of SCT l l l Surgery, should be performed immediately upon diagnosis or even with suspected it. Access is scrotal or inguinal. After untwisting the spermatic cord (detorsion), novocaine blockade of it and warming of testicle by damp cloth with warm solution are conducted. The viability of testicle (color, luster membranes) is evaluated, testis is fixed by sutures to separate membranes of scrotum, scrotum is drained by a rubber drainage. If necrotic testicle, orchidektomy is performed, then fixation the opposite testicle is carried out. Anti-inflammatory drugs, vitamins A, E, C, Heparin,
 Testicular hydatis torsion l More common occurs in boys aged 4 to 15 years. l Morhanyi’s hydatis are derivatives of primary genital ducts (Volf’s and Muller’s). There are 5 kinds of hydatis. Its sizes may be from 2 to 10 mm in diameter. l Hydatis can subverted around the leg, which leads to ischemia, infection and necrosis. Inflammation from hydatis goes on testicle and its shells. Without surgery occurs atrophy of testicle. Rarely cystic degeneration and malignancy of hydatis are observed.
Testicular hydatis torsion l More common occurs in boys aged 4 to 15 years. l Morhanyi’s hydatis are derivatives of primary genital ducts (Volf’s and Muller’s). There are 5 kinds of hydatis. Its sizes may be from 2 to 10 mm in diameter. l Hydatis can subverted around the leg, which leads to ischemia, infection and necrosis. Inflammation from hydatis goes on testicle and its shells. Without surgery occurs atrophy of testicle. Rarely cystic degeneration and malignancy of hydatis are observed.
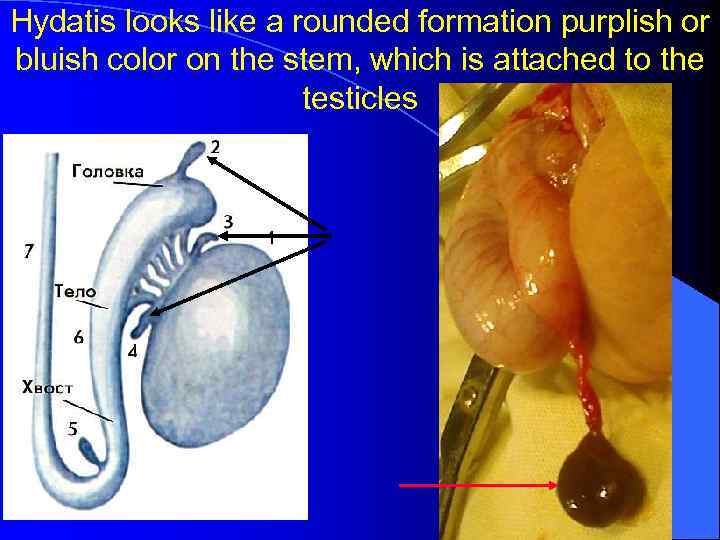 Hydatis looks like a rounded formation purplish or bluish color on the stem, which is attached to the testicles
Hydatis looks like a rounded formation purplish or bluish color on the stem, which is attached to the testicles
 Clinic of testicular hydatis torsion l Complaints of pain in the affected part of the scrotum. Locally reveal edema and hyperemia of the corresponding half of the scrotum. In palpation is determined the increased testicle, near the upper pole of it palpable dense, sharply painful knot. Sometimes it shows through the scrotum, dark color. Diagnosis l based on the data of ultrasound and diafanoskopy. Sometimes is performed testicular membranes puncture, thus getting turbid liquid.
Clinic of testicular hydatis torsion l Complaints of pain in the affected part of the scrotum. Locally reveal edema and hyperemia of the corresponding half of the scrotum. In palpation is determined the increased testicle, near the upper pole of it palpable dense, sharply painful knot. Sometimes it shows through the scrotum, dark color. Diagnosis l based on the data of ultrasound and diafanoskopy. Sometimes is performed testicular membranes puncture, thus getting turbid liquid.
 Treatment of testicular hydatis torsion l Surgical. Involves the removal hydatis, drainage of testicle membranes. Novocaine blockade of the spermatic cord is performed. l After surgery anti-inflammatory and metabolic drugs (Aevit, Nicotinic acid, 5% Aminocapronic acid, Nimesulide, Kvartsetin) are prescribed.
Treatment of testicular hydatis torsion l Surgical. Involves the removal hydatis, drainage of testicle membranes. Novocaine blockade of the spermatic cord is performed. l After surgery anti-inflammatory and metabolic drugs (Aevit, Nicotinic acid, 5% Aminocapronic acid, Nimesulide, Kvartsetin) are prescribed.
 Orchitis l This is an acute inflammation of the testicle, which is caused by infection, trauma, and other factors. There are specific and nonspecific orchitis. l Specific orchitis develops under the influence of pathogen, tropic to testicular tissue (mumps, tuberculosis, hepatitis, etc. ). l Etiologic factor is infection. In the pathogenesis are important also autoimmune reactions. Pathogen effect on spermatogenic epithelium. Affects parenchymal and interstitial cells.
Orchitis l This is an acute inflammation of the testicle, which is caused by infection, trauma, and other factors. There are specific and nonspecific orchitis. l Specific orchitis develops under the influence of pathogen, tropic to testicular tissue (mumps, tuberculosis, hepatitis, etc. ). l Etiologic factor is infection. In the pathogenesis are important also autoimmune reactions. Pathogen effect on spermatogenic epithelium. Affects parenchymal and interstitial cells.
 Orchitis Swelling of the testicle tissue leads to ischemia it and at the future - to atrophy. Clinic. It starts acutely, there is pain that gives back to perineum, lower abdomen. Testicle becomes dense, enlarged, painful. Later there is swelling and redness of the scrotum. Conservative treatment: antibiotics, compresses, glucocorticoids, Aspirin. Suspensory is imposed. In the presence of fluid under the testicular shells is performed surgery - decompression of testicles. The operation is carried out in the urgent manner. More often orchitis is a complication of hydatis torsion, testicular torsion.
Orchitis Swelling of the testicle tissue leads to ischemia it and at the future - to atrophy. Clinic. It starts acutely, there is pain that gives back to perineum, lower abdomen. Testicle becomes dense, enlarged, painful. Later there is swelling and redness of the scrotum. Conservative treatment: antibiotics, compresses, glucocorticoids, Aspirin. Suspensory is imposed. In the presence of fluid under the testicular shells is performed surgery - decompression of testicles. The operation is carried out in the urgent manner. More often orchitis is a complication of hydatis torsion, testicular torsion.
 Algorithm of urgent actions in syndrome of swollen scrotum: Preoperative preparation: administration of analgesics. Surgical intervention: access (often - scrotal), detorsion of testis, removing of hydatis, drainage of testicular membranes, spermatic cord blockade with 0. 25% Sol. Novocaine + Hydrocortisone administration. Postoperative treatment: antibiotics, metabolic drugs - Trental, vitamins A, E, antioxidants, Kvartsetin. Untimely and inadequate treatment, refusal of emergency operations may lead to ischemia and atrophy of testes, chronic dropsy, obstruction of vas deferens. Later it leads to male infertility.
Algorithm of urgent actions in syndrome of swollen scrotum: Preoperative preparation: administration of analgesics. Surgical intervention: access (often - scrotal), detorsion of testis, removing of hydatis, drainage of testicular membranes, spermatic cord blockade with 0. 25% Sol. Novocaine + Hydrocortisone administration. Postoperative treatment: antibiotics, metabolic drugs - Trental, vitamins A, E, antioxidants, Kvartsetin. Untimely and inadequate treatment, refusal of emergency operations may lead to ischemia and atrophy of testes, chronic dropsy, obstruction of vas deferens. Later it leads to male infertility.
 Injury of the scrotum and testicles l There are open and closed injuries. By type: contusion, rupture, dislocation and compression of the testicle. Upon impact the scrotum and testicles there is swelling of tissues, in severe cases - hemorrhage or hematoma. l The extreme degree of testicular rupture is crushing or separation of it from the spermatic cord. l One of the rare variants injury is testicular dislocation (one or two) that can be found in the inguinal canal, under the skin of the abdomen, thighs, perineum. l Open injuries: torn, chopped, sliced and bitten wounds.
Injury of the scrotum and testicles l There are open and closed injuries. By type: contusion, rupture, dislocation and compression of the testicle. Upon impact the scrotum and testicles there is swelling of tissues, in severe cases - hemorrhage or hematoma. l The extreme degree of testicular rupture is crushing or separation of it from the spermatic cord. l One of the rare variants injury is testicular dislocation (one or two) that can be found in the inguinal canal, under the skin of the abdomen, thighs, perineum. l Open injuries: torn, chopped, sliced and bitten wounds.
 Clinic l Depends on the nature of the damage. In closed injuries there are swelling and hemorrhage of soft tissues, increasing and tenderness of testis and epididimus, thickening and tenderness of spermatic cord. When bleeding into the tissues of scrotum or testicles is determined hematocele or scrotal hematoma, sometimes is defined fluctuation. Scrotum may be increased in size by 3 -5 times. In open injuries is visible wound of scrotum and testicles. Gaps of testicles and applications is usually accompanied by varying degrees of traumatic shock. When testicular dislocation is empty scrotum, the testicles are determined abroad.
Clinic l Depends on the nature of the damage. In closed injuries there are swelling and hemorrhage of soft tissues, increasing and tenderness of testis and epididimus, thickening and tenderness of spermatic cord. When bleeding into the tissues of scrotum or testicles is determined hematocele or scrotal hematoma, sometimes is defined fluctuation. Scrotum may be increased in size by 3 -5 times. In open injuries is visible wound of scrotum and testicles. Gaps of testicles and applications is usually accompanied by varying degrees of traumatic shock. When testicular dislocation is empty scrotum, the testicles are determined abroad.
 Treatment l In closed injuries - bed rest, cold on the scrotum, imposing of suspensory. Later is prescribed thermal and physiotherapy. In the presence of hematoma is revealed draining, transmitting hemostasis. At slaughter - novocaine blockade of the spermatic cord is performed. When break of testis - emergency operation - suturing of tunica albuginea and drainage. In open injuries - revision of wound, primary surgical treatment, necrectomy, suturing the testicle and scrotum with the drainage When crushing or separation of testis orchidektomy is indicated. To all children with
Treatment l In closed injuries - bed rest, cold on the scrotum, imposing of suspensory. Later is prescribed thermal and physiotherapy. In the presence of hematoma is revealed draining, transmitting hemostasis. At slaughter - novocaine blockade of the spermatic cord is performed. When break of testis - emergency operation - suturing of tunica albuginea and drainage. In open injuries - revision of wound, primary surgical treatment, necrectomy, suturing the testicle and scrotum with the drainage When crushing or separation of testis orchidektomy is indicated. To all children with
 Injury of kidney l Arises as a result of closed injury of the lumbar region (face, falling from height, compression). l The kidneys in children are more prone to injury because the musculoskeletal system provides enough protection function and kidney fairly mobile. l About 20% of injuries occur when renal pathology (tumors, hydronephrosis, etc. ). l There are open and closed injuries of kidneys.
Injury of kidney l Arises as a result of closed injury of the lumbar region (face, falling from height, compression). l The kidneys in children are more prone to injury because the musculoskeletal system provides enough protection function and kidney fairly mobile. l About 20% of injuries occur when renal pathology (tumors, hydronephrosis, etc. ). l There are open and closed injuries of kidneys.
 Classification of renal injuries l I deg. - Damage of parenchyma without evidence of accumulation of fluid (blood, urine) in capsule or around it. l II deg. - Partial damage with little accumulation of fluid under the capsule or around it (urohematoma). l III deg. - Rupture of the kidney with significant accumulation of fluid around the kidney. l IV deg. - Crushing of kidney while maintaining a connection with parts of it and maintaining circulation. l V deg. - Damage of the vascular pedicle, ureter separation.
Classification of renal injuries l I deg. - Damage of parenchyma without evidence of accumulation of fluid (blood, urine) in capsule or around it. l II deg. - Partial damage with little accumulation of fluid under the capsule or around it (urohematoma). l III deg. - Rupture of the kidney with significant accumulation of fluid around the kidney. l IV deg. - Crushing of kidney while maintaining a connection with parts of it and maintaining circulation. l V deg. - Damage of the vascular pedicle, ureter separation.
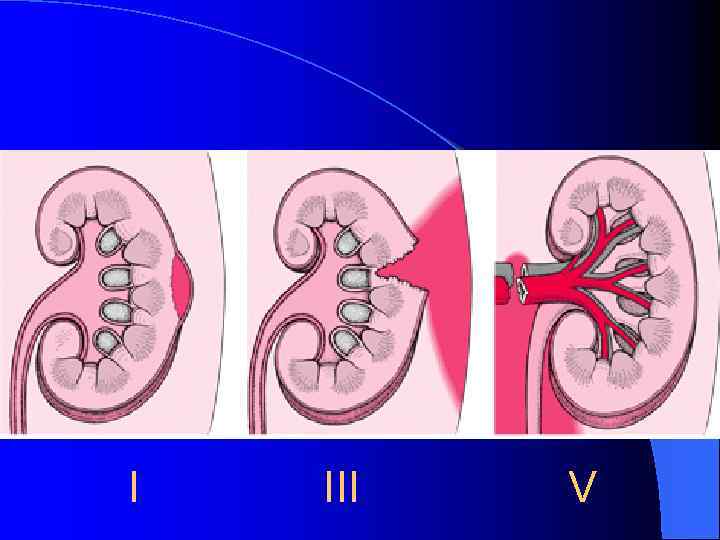 І ІІІ V
І ІІІ V
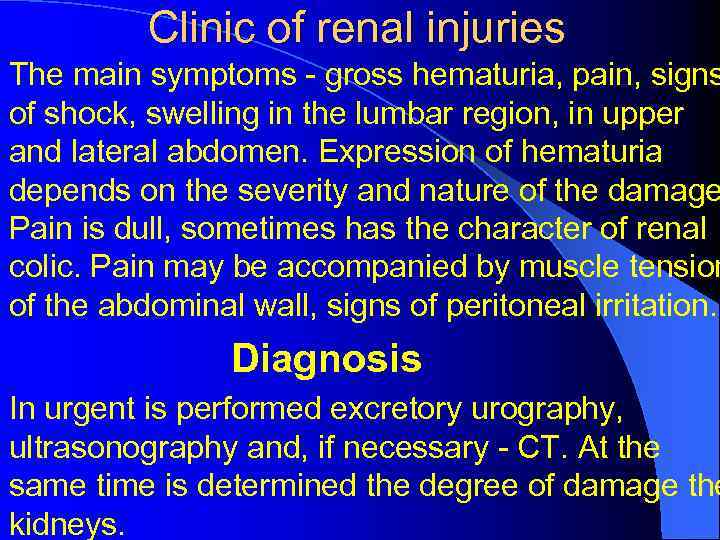 Clinic of renal injuries l The main symptoms - gross hematuria, pain, signs of shock, swelling in the lumbar region, in upper and lateral abdomen. Expression of hematuria depends on the severity and nature of the damage Pain is dull, sometimes has the character of renal colic. Pain may be accompanied by muscle tension of the abdominal wall, signs of peritoneal irritation. l Diagnosis l In urgent is performed excretory urography, ultrasonography and, if necessary - CT. At the same time is determined the degree of damage the kidneys.
Clinic of renal injuries l The main symptoms - gross hematuria, pain, signs of shock, swelling in the lumbar region, in upper and lateral abdomen. Expression of hematuria depends on the severity and nature of the damage Pain is dull, sometimes has the character of renal colic. Pain may be accompanied by muscle tension of the abdominal wall, signs of peritoneal irritation. l Diagnosis l In urgent is performed excretory urography, ultrasonography and, if necessary - CT. At the same time is determined the degree of damage the kidneys.
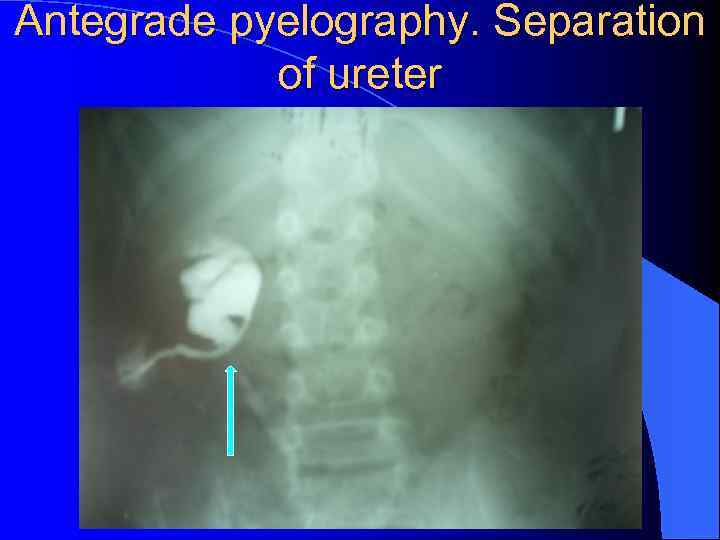 Antegrade pyelography. Separation of ureter
Antegrade pyelography. Separation of ureter
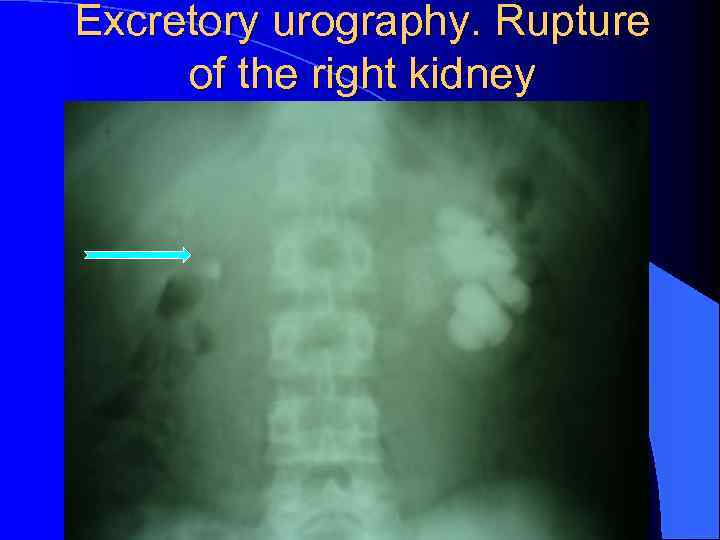 Excretory urography. Rupture of the right kidney
Excretory urography. Rupture of the right kidney
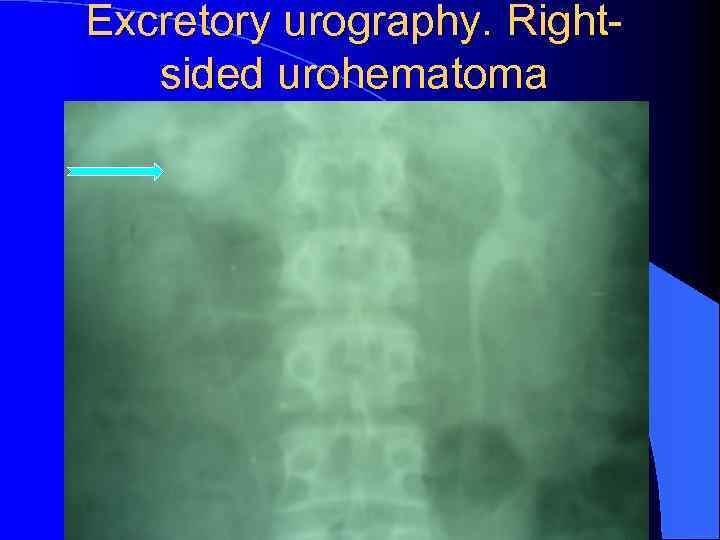 Excretory urography. Rightsided urohematoma
Excretory urography. Rightsided urohematoma
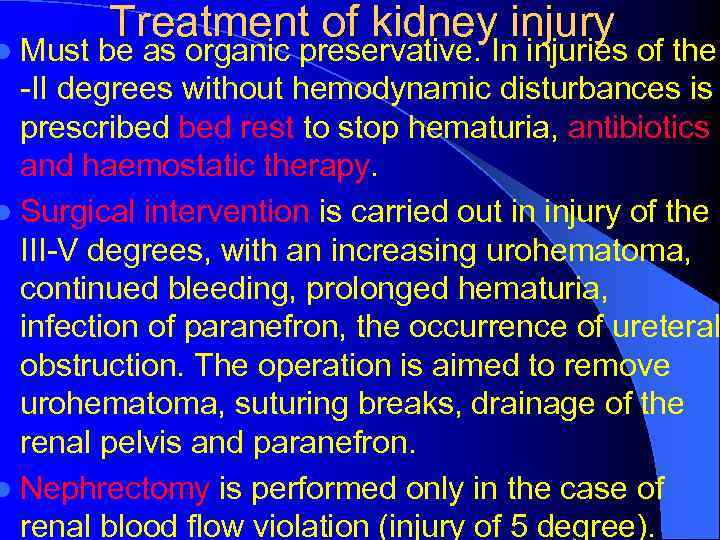 Treatment of kidney injury l Must be as organic preservative. In injuries of the -II degrees without hemodynamic disturbances is prescribed rest to stop hematuria, antibiotics and haemostatic therapy. l Surgical intervention is carried out in injury of the III-V degrees, with an increasing urohematoma, continued bleeding, prolonged hematuria, infection of paranefron, the occurrence of ureteral obstruction. The operation is aimed to remove urohematoma, suturing breaks, drainage of the renal pelvis and paranefron. l Nephrectomy is performed only in the case of renal blood flow violation (injury of 5 degree).
Treatment of kidney injury l Must be as organic preservative. In injuries of the -II degrees without hemodynamic disturbances is prescribed rest to stop hematuria, antibiotics and haemostatic therapy. l Surgical intervention is carried out in injury of the III-V degrees, with an increasing urohematoma, continued bleeding, prolonged hematuria, infection of paranefron, the occurrence of ureteral obstruction. The operation is aimed to remove urohematoma, suturing breaks, drainage of the renal pelvis and paranefron. l Nephrectomy is performed only in the case of renal blood flow violation (injury of 5 degree).
 Damage of ureters l Belong to a very rare injury. Detected by excretory urography. Treatment exclusively surgical and depends on the type of injury. Damage of the bladder intraperitoneal extraperitoneal Resulting from compression of the lower body, kick or fall from a height in a crowded bladder. Damage arising from fractures of the pelvis by displaced fragments or with penetrating wounds of the perineum.
Damage of ureters l Belong to a very rare injury. Detected by excretory urography. Treatment exclusively surgical and depends on the type of injury. Damage of the bladder intraperitoneal extraperitoneal Resulting from compression of the lower body, kick or fall from a height in a crowded bladder. Damage arising from fractures of the pelvis by displaced fragments or with penetrating wounds of the perineum.
 Bladder Injuries Clinic Intra-abdominal injury: are present peritoneal symptoms - abdominal pain, vomiting, muscle tension o anterior abdominal wall, peritoneal irritation symptoms, blunting in cape places of abdomen with percussion. Urination disorders - frequent urge release drops of bloody urine, patient can not urinate self. When bladder catheterization is observed gross hematuria. Extraperitoneal damage: signs of peritonitis are not pronounced, disturbing pain under pubis by palpation and muscle tension. Painful urination, stands a small amount of urine, colored with blood. To confirm the diagnosis is used cystography.
Bladder Injuries Clinic Intra-abdominal injury: are present peritoneal symptoms - abdominal pain, vomiting, muscle tension o anterior abdominal wall, peritoneal irritation symptoms, blunting in cape places of abdomen with percussion. Urination disorders - frequent urge release drops of bloody urine, patient can not urinate self. When bladder catheterization is observed gross hematuria. Extraperitoneal damage: signs of peritonitis are not pronounced, disturbing pain under pubis by palpation and muscle tension. Painful urination, stands a small amount of urine, colored with blood. To confirm the diagnosis is used cystography.
 Treatment of bladder injuries Surgical l When intraabdominal - laparotomy, is examined the upper and posterior wall of the bladder. Gaps are stitched of two rows ketgut seams. Must carry out sanitation of the abdominal cavity and epiсystostomy. l When extraperitoneal injuries also is imposed epicystostoma.
Treatment of bladder injuries Surgical l When intraabdominal - laparotomy, is examined the upper and posterior wall of the bladder. Gaps are stitched of two rows ketgut seams. Must carry out sanitation of the abdominal cavity and epiсystostomy. l When extraperitoneal injuries also is imposed epicystostoma.
 Injury of urethra l Arises in impact perineum to a solid object or bone fractures of the pelvis. Preferably is damaged posterior urethra. There are penetrating and nonpenetrating gaps. l Clinic is characterized by bleeding from urethra, perineal hematoma, urinary retention, where there is a feeling of fullness. Urine penetrates soft tissues, urinary abscess may occur. With the spread it to the pelvis condition of child much worse. For diagnosis is used retrograde urography, with visible contrast penetration beyond the urethra.
Injury of urethra l Arises in impact perineum to a solid object or bone fractures of the pelvis. Preferably is damaged posterior urethra. There are penetrating and nonpenetrating gaps. l Clinic is characterized by bleeding from urethra, perineal hematoma, urinary retention, where there is a feeling of fullness. Urine penetrates soft tissues, urinary abscess may occur. With the spread it to the pelvis condition of child much worse. For diagnosis is used retrograde urography, with visible contrast penetration beyond the urethra.
 Treatment of the urethra injuries l Begins with antishock measures. Bladder catheterization is contraindicated. l Emergency operation is conducted: imposing epicystostoma, drainage of paraurethral hematoma. Later - suturing of breaks urethra. l Often after such injuries occur stricture of urethra channel that require bouginage. In the ineffectiveness of the treatment is carried out complex plastic surgery to restore patency of the urethra.
Treatment of the urethra injuries l Begins with antishock measures. Bladder catheterization is contraindicated. l Emergency operation is conducted: imposing epicystostoma, drainage of paraurethral hematoma. Later - suturing of breaks urethra. l Often after such injuries occur stricture of urethra channel that require bouginage. In the ineffectiveness of the treatment is carried out complex plastic surgery to restore patency of the urethra.
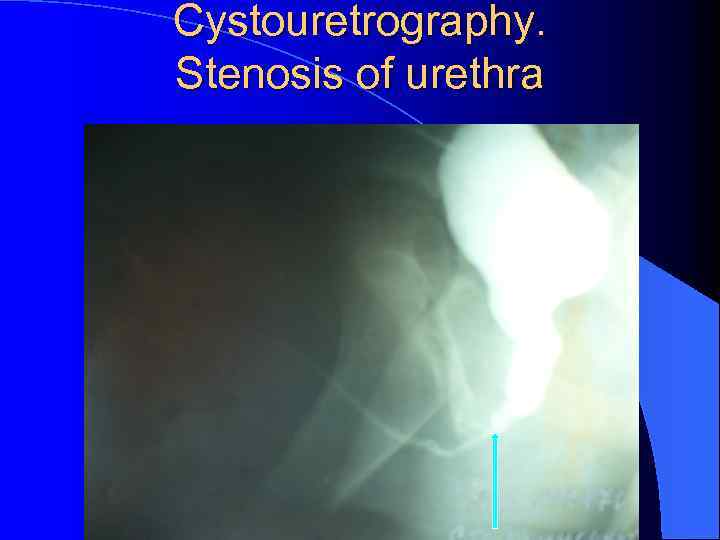 Cystouretrography. Stenosis of urethra
Cystouretrography. Stenosis of urethra



