1b60e38042ded4b447d5ed5c6cbe0dcf.ppt
- Количество слайдов: 43
 Is radiology replacing the scalpel: Advances in minimally invasive techniques Dr Steven Allen Consultant Breast Radiologist Breast Imaging Lead, Royal Marsden Hospital, Sutton Specialist Advisor to NICE on breast interventional procedures
Is radiology replacing the scalpel: Advances in minimally invasive techniques Dr Steven Allen Consultant Breast Radiologist Breast Imaging Lead, Royal Marsden Hospital, Sutton Specialist Advisor to NICE on breast interventional procedures
 Radiological Breast Intervention n n Diagnosis (biopsies) Therapy
Radiological Breast Intervention n n Diagnosis (biopsies) Therapy
 Fine Needle Aspiration n Insufficient material retrieved for definitive diagnosis n Interpretation is highly dependent on skill of cytopathologist n Cannot distinguish in situ versus invasive carcinomas n Difficult to distinguish atypical ductal hyperplasia from low-grade DCIS or low-grade invasive ductal carcinoma n New “Best practice diagnostic guidelines for patients presenting with breast symptoms”* *Willett et al. Best practice diagnostic guidelines for patients presenting with breast symptoms. Nov 2010. www. rcrbreast group. com/Documents/BBCDiagnostic. Guidelines. pdf
Fine Needle Aspiration n Insufficient material retrieved for definitive diagnosis n Interpretation is highly dependent on skill of cytopathologist n Cannot distinguish in situ versus invasive carcinomas n Difficult to distinguish atypical ductal hyperplasia from low-grade DCIS or low-grade invasive ductal carcinoma n New “Best practice diagnostic guidelines for patients presenting with breast symptoms”* *Willett et al. Best practice diagnostic guidelines for patients presenting with breast symptoms. Nov 2010. www. rcrbreast group. com/Documents/BBCDiagnostic. Guidelines. pdf
 Fine Needle Aspiration-Uses n n n Where core biopsy not technically possible Lymph nodes Complex cysts Radiologically benign, young women Clotting issues Local anaesthetic allergy
Fine Needle Aspiration-Uses n n n Where core biopsy not technically possible Lymph nodes Complex cysts Radiologically benign, young women Clotting issues Local anaesthetic allergy
 Why do we need breast needle biopsy? n n Definitive benign diagnosis avoids unnecessary surgery Knowledge of the type and extent of malignancy influences choice of treatment n ADH or Ductal carcinoma in situ? n Ductal carcinoma in situ or invasive disease? n Invasive tumour type - eg lobular n Invasive tumour grade n Oestrogen receptor status n Other tumour markers n Tumour genetics
Why do we need breast needle biopsy? n n Definitive benign diagnosis avoids unnecessary surgery Knowledge of the type and extent of malignancy influences choice of treatment n ADH or Ductal carcinoma in situ? n Ductal carcinoma in situ or invasive disease? n Invasive tumour type - eg lobular n Invasive tumour grade n Oestrogen receptor status n Other tumour markers n Tumour genetics
 Problems with core biopsy n n n False negatives on core (2 -10%, mainly calcifications) Trend to increasing size of biopsy sample to minimize this BUT cheap ( approx £ 15 per needle, £ 50 per case versus £ 150 per needle, £ 500 per case)
Problems with core biopsy n n n False negatives on core (2 -10%, mainly calcifications) Trend to increasing size of biopsy sample to minimize this BUT cheap ( approx £ 15 per needle, £ 50 per case versus £ 150 per needle, £ 500 per case)
 Automated 14 g core biopsy deals with more than 90% of cases Very large core biopsy techniques have been developed to deal with the rest and also to help solve diagnostic problems
Automated 14 g core biopsy deals with more than 90% of cases Very large core biopsy techniques have been developed to deal with the rest and also to help solve diagnostic problems
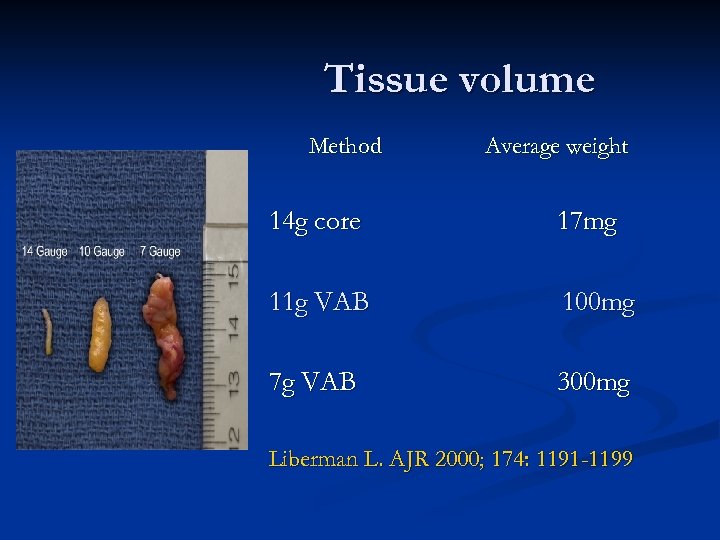 Tissue volume Method Average weight 14 g core 17 mg 11 g VAB 100 mg 7 g VAB 300 mg Liberman L. AJR 2000; 174: 1191 -1199
Tissue volume Method Average weight 14 g core 17 mg 11 g VAB 100 mg 7 g VAB 300 mg Liberman L. AJR 2000; 174: 1191 -1199
 Vacuum Assisted Biopsy n n n In USA probably overperformed Increasing in Europe where probably still underperformed The role is extending (MRI, therapy? )
Vacuum Assisted Biopsy n n n In USA probably overperformed Increasing in Europe where probably still underperformed The role is extending (MRI, therapy? )
 When should vacuum assisted biopsy be used? Indications : n Very small mass lesions n Equivocal or failed core biopsy n Architectural distortions n Microcalcifications n Papillary and mucocele like lesions n Diffuse non-specific abnormality n Complex cysts and abscesses n Excision of benign lesions n Malignant disease ? ?
When should vacuum assisted biopsy be used? Indications : n Very small mass lesions n Equivocal or failed core biopsy n Architectural distortions n Microcalcifications n Papillary and mucocele like lesions n Diffuse non-specific abnormality n Complex cysts and abscesses n Excision of benign lesions n Malignant disease ? ?
 VAB effects n n Will detect more ADH *, LCIS Will detect more DCIS, Invasive cancer* * cancer Reduced surgical biopsy rate Better preoperative surgical and medical treatment planning * Winchester * *Kettritz et al. Arch Surg 2003: 138(6); 619 -22 et al. Cancer 2004: 100(2); 245 -51
VAB effects n n Will detect more ADH *, LCIS Will detect more DCIS, Invasive cancer* * cancer Reduced surgical biopsy rate Better preoperative surgical and medical treatment planning * Winchester * *Kettritz et al. Arch Surg 2003: 138(6); 619 -22 et al. Cancer 2004: 100(2); 245 -51
 VAB - risks n Haematoma rates are actually low*, and not significantly different to core biopsy n Pain? ** n Clip migration *Lai, et al. Vacuum-assisted large-core breast biopsy: complications and their incidence. Can Assoc Radiol J. 2000 Aug; 51(4): 232 -6. **Szynglarewicz, et al. Pain experienced by patients during minimal-invasive ultrasound-guided breast biopsy: Vacuum-assisted vs core-needle procedure. EJSO, . 2011 Feb 28, Epub
VAB - risks n Haematoma rates are actually low*, and not significantly different to core biopsy n Pain? ** n Clip migration *Lai, et al. Vacuum-assisted large-core breast biopsy: complications and their incidence. Can Assoc Radiol J. 2000 Aug; 51(4): 232 -6. **Szynglarewicz, et al. Pain experienced by patients during minimal-invasive ultrasound-guided breast biopsy: Vacuum-assisted vs core-needle procedure. EJSO, . 2011 Feb 28, Epub
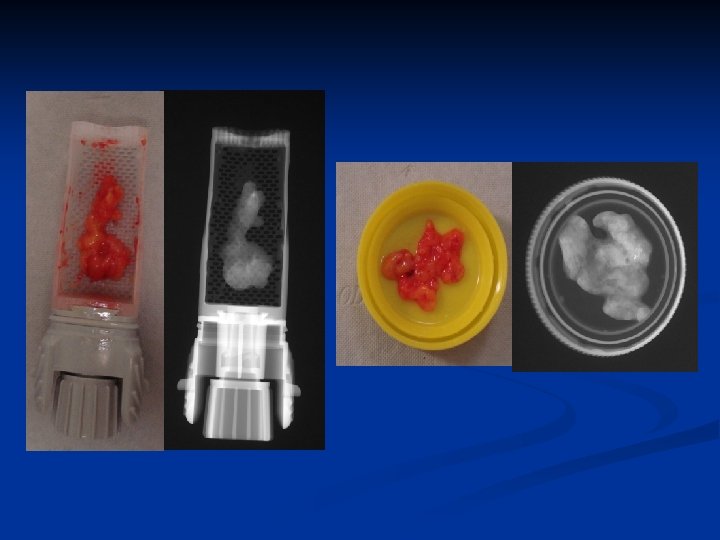
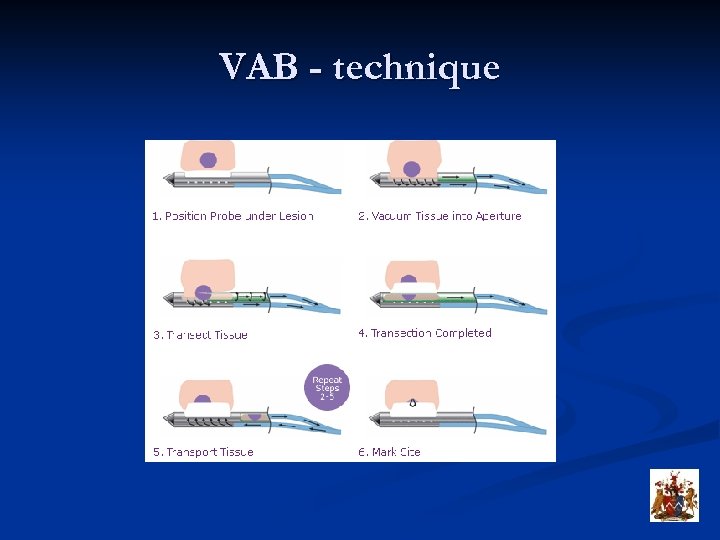 VAB - technique
VAB - technique

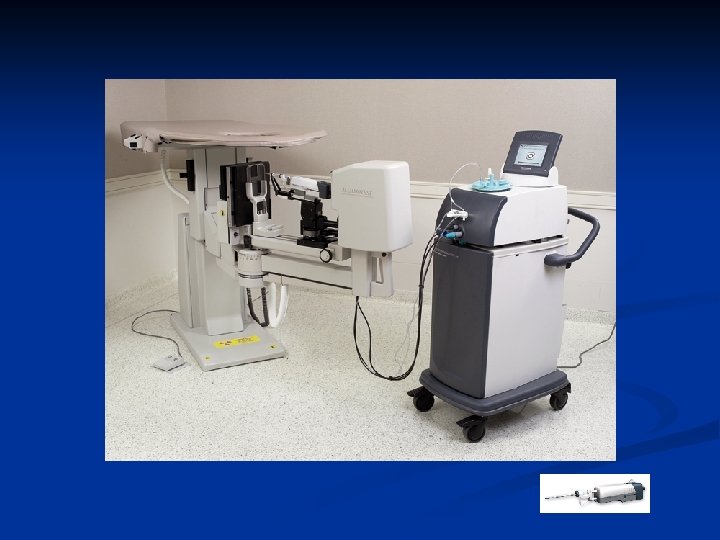
 ™) En. Cor (Seno. Rx
™) En. Cor (Seno. Rx

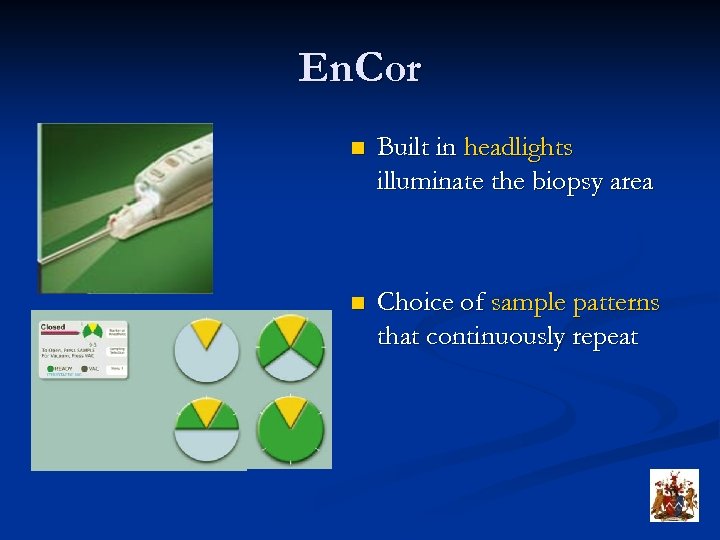 En. Cor n Built in headlights illuminate the biopsy area n Choice of sample patterns that continuously repeat
En. Cor n Built in headlights illuminate the biopsy area n Choice of sample patterns that continuously repeat
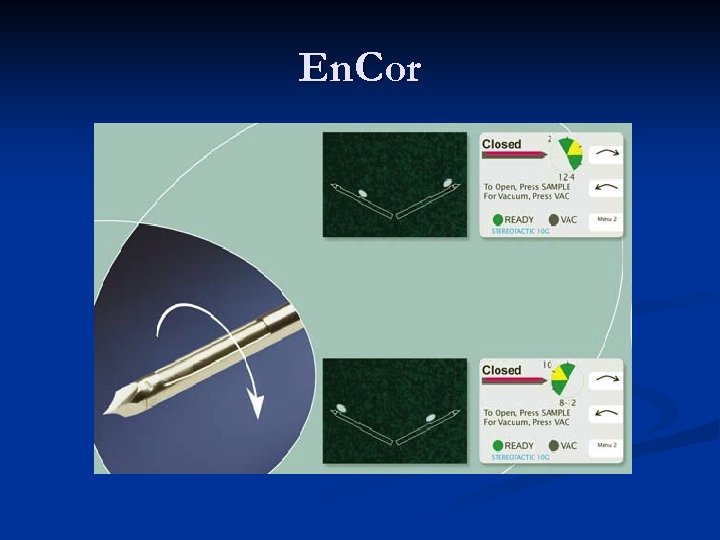 En. Cor
En. Cor
 ATEC (Suros surgical)
ATEC (Suros surgical)
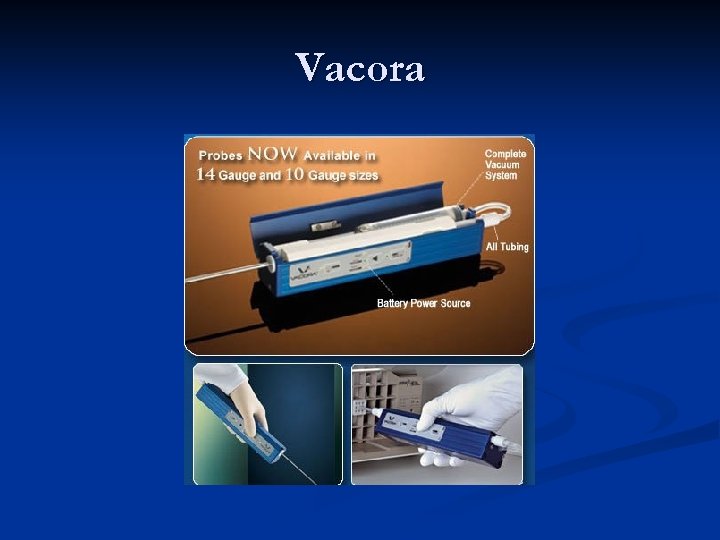 Vacora
Vacora
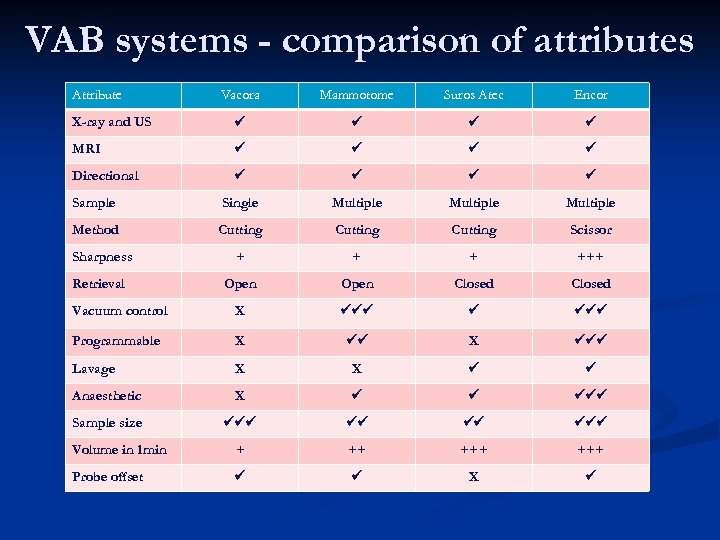 VAB systems - comparison of attributes Attribute Vacora Mammotome Suros Atec Encor X-ray and US MRI Directional Sample Single Multiple Method Cutting Scissor Sharpness + +++ Retrieval Open Closed Vacuum control X Programmable X X Lavage X X Anaesthetic X Sample size Volume in 1 min + ++ +++ Probe offset X
VAB systems - comparison of attributes Attribute Vacora Mammotome Suros Atec Encor X-ray and US MRI Directional Sample Single Multiple Method Cutting Scissor Sharpness + +++ Retrieval Open Closed Vacuum control X Programmable X X Lavage X X Anaesthetic X Sample size Volume in 1 min + ++ +++ Probe offset X
 Vacuum assisted excision n n Increasing use to excise benign lesions in a “piecemeal” fashion as an alternative to surgery Cannot give margin status on excision Newer devices are very automated allowing most procedures to be performed in <30 minutes Significant time, cost, morbidity benefits
Vacuum assisted excision n n Increasing use to excise benign lesions in a “piecemeal” fashion as an alternative to surgery Cannot give margin status on excision Newer devices are very automated allowing most procedures to be performed in <30 minutes Significant time, cost, morbidity benefits
 Vacuum assisted excision § § § Benign lesions such as fibroadenomas * Recurrence rate may be higher for lesions >2 cm Papillary lesions All B 3 lesions without atypia* * Lymph nodes? Cancers? * Grady et al, Breast J 2008, 14(3): 275 -8 * * Tennant et al, Breast 2008, 17(6): 546 -9
Vacuum assisted excision § § § Benign lesions such as fibroadenomas * Recurrence rate may be higher for lesions >2 cm Papillary lesions All B 3 lesions without atypia* * Lymph nodes? Cancers? * Grady et al, Breast J 2008, 14(3): 275 -8 * * Tennant et al, Breast 2008, 17(6): 546 -9
 ™ Breast Lesion Excision The Intact System (BLES) Handle & Disposable Wand Controller & Vacuum Source
™ Breast Lesion Excision The Intact System (BLES) Handle & Disposable Wand Controller & Vacuum Source
 The Intact BLES n Developed in USA in 2001, the INTACT breast lesion excision system (BLES) has a unique capability of obtaining a single large biopsy sample using radiofrequency cauterisation n It has been used extensively in the USA as an equivalent large biopsy device to current vacuum assisted systems (>40, 000 cases!). n At least equivalent diagnostically to VAB devices* *Sie et al, 2006. Multicenter Evaluation of the Breast Lesion Excision System, a Percutaneous, Vacuum-Assisted, Intact-Specimen Breast Biopsy Device. Cancer 107: 5
The Intact BLES n Developed in USA in 2001, the INTACT breast lesion excision system (BLES) has a unique capability of obtaining a single large biopsy sample using radiofrequency cauterisation n It has been used extensively in the USA as an equivalent large biopsy device to current vacuum assisted systems (>40, 000 cases!). n At least equivalent diagnostically to VAB devices* *Sie et al, 2006. Multicenter Evaluation of the Breast Lesion Excision System, a Percutaneous, Vacuum-Assisted, Intact-Specimen Breast Biopsy Device. Cancer 107: 5
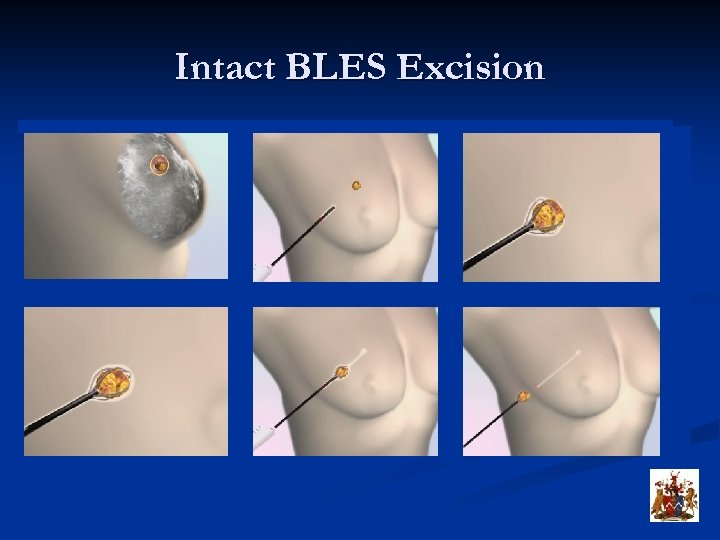 Intact BLES Excision
Intact BLES Excision
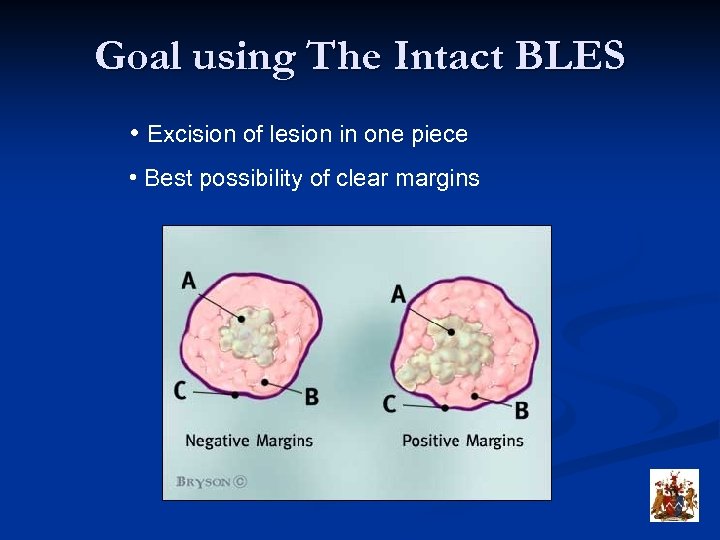 Goal using The Intact BLES • Excision of lesion in one piece • Best possibility of clear margins
Goal using The Intact BLES • Excision of lesion in one piece • Best possibility of clear margins
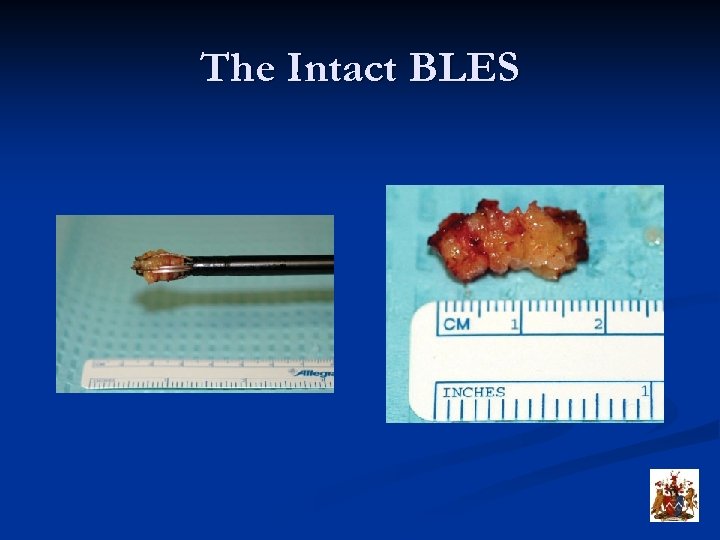 The Intact BLES
The Intact BLES
 Specimen radiograph
Specimen radiograph
 The Intact BLES n RMH have had this since 2007 and are the second centre outside the USA n Approved as a biopsy device by appropriate committees n However due to its of obtaining a single large sample, we have almost exclusively used this in an attempt at whole lesion excision n Most of our patient group have been referred from the NHSBSP, and we have attempted to perform complete excision biopsy in removing small breast lesions with a margin * *Allen SD, Nerurkar A, Della Rovere GU. The breast lesion excision system (BLES): a novel technique in the diagnostic and therapeutic management of small indeterminate breast lesions? Eur Radiol. 2011 Jan 15.
The Intact BLES n RMH have had this since 2007 and are the second centre outside the USA n Approved as a biopsy device by appropriate committees n However due to its of obtaining a single large sample, we have almost exclusively used this in an attempt at whole lesion excision n Most of our patient group have been referred from the NHSBSP, and we have attempted to perform complete excision biopsy in removing small breast lesions with a margin * *Allen SD, Nerurkar A, Della Rovere GU. The breast lesion excision system (BLES): a novel technique in the diagnostic and therapeutic management of small indeterminate breast lesions? Eur Radiol. 2011 Jan 15.
 The Intact BLES n Many borderline (high risk) lesions can be completely excised without surgery in a short well tolerated outpatient procedure * n The results very much represent what can be achieved during the early stages of using this new technique n Complementary to VAB as an alternative therapy to surgery for small breast lesions *Whitworth PW. Intact Percutaneous Excision (IPEX) for Definitive Diagnosis of High-Risk Breast Lesions. Ann Surg Oncol. 2011 Oct; 18(11): 3095. Epub 2011 Sep 9
The Intact BLES n Many borderline (high risk) lesions can be completely excised without surgery in a short well tolerated outpatient procedure * n The results very much represent what can be achieved during the early stages of using this new technique n Complementary to VAB as an alternative therapy to surgery for small breast lesions *Whitworth PW. Intact Percutaneous Excision (IPEX) for Definitive Diagnosis of High-Risk Breast Lesions. Ann Surg Oncol. 2011 Oct; 18(11): 3095. Epub 2011 Sep 9
 The Intact BLES n NICE have now approved this as a large biopsy device n The potential of this technique may grow further as wand technology/unit experience improves n Current wand sizes/yield limit excision of many lesions n A 30 mm wand has been in use in selected centres >6/12 n ? whole cancer excision
The Intact BLES n NICE have now approved this as a large biopsy device n The potential of this technique may grow further as wand technology/unit experience improves n Current wand sizes/yield limit excision of many lesions n A 30 mm wand has been in use in selected centres >6/12 n ? whole cancer excision
 30 mm wand
30 mm wand
 Thermal Ablation n n n Radiofrequency ablation Cryoablation Laser therapy High Intensity focused ultrasound (HIFU) All require a probe to be inserted into the tumour under image guidance (usually ultrasound) Margins, margins
Thermal Ablation n n n Radiofrequency ablation Cryoablation Laser therapy High Intensity focused ultrasound (HIFU) All require a probe to be inserted into the tumour under image guidance (usually ultrasound) Margins, margins
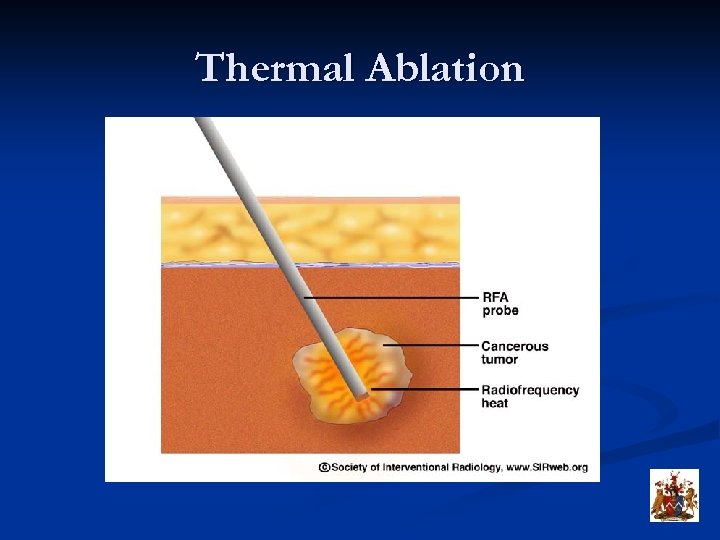 Thermal Ablation
Thermal Ablation
 RF Ablation n n RF ablation most fashionable Small, centrally sited, low grade tumours, elderly patients Low level of evidence Almost invariably combined with surgery* *Imoto S, et al. Breast. 2009 Apr; 18(2): 130 -4
RF Ablation n n RF ablation most fashionable Small, centrally sited, low grade tumours, elderly patients Low level of evidence Almost invariably combined with surgery* *Imoto S, et al. Breast. 2009 Apr; 18(2): 130 -4
 RF Ablation ? neoadjuvant n n RFA combined with immunologically active cytokines (IL-7 and IL-15) in mice induced immune responses to tumors, inhibited tumor development and lung metastasis * RFA combined with other treatment deliveries? *Habibi M, et al. Breast Cancer Res Treat. 2009 Apr; 114(3): 423 -31.
RF Ablation ? neoadjuvant n n RFA combined with immunologically active cytokines (IL-7 and IL-15) in mice induced immune responses to tumors, inhibited tumor development and lung metastasis * RFA combined with other treatment deliveries? *Habibi M, et al. Breast Cancer Res Treat. 2009 Apr; 114(3): 423 -31.
 Conclusions n Biopsies are getting larger! n Core biopsy and even FNA still maintain a role n As with other fields of interventional radiology, the breast interventionalist is finding a role extension in therapy of benign and now malignant breast disease
Conclusions n Biopsies are getting larger! n Core biopsy and even FNA still maintain a role n As with other fields of interventional radiology, the breast interventionalist is finding a role extension in therapy of benign and now malignant breast disease