90d1ebd6f429868ceb3e419a179f09ea.ppt
- Количество слайдов: 77
 Is it MG Crisis? Dr Chan Yan Fat Alfred Caritas Medical Center 20/01/2009
Is it MG Crisis? Dr Chan Yan Fat Alfred Caritas Medical Center 20/01/2009
 Background history • • 82 -year-old woman, ex-smoker Mother of 6 children Resident in Canada and being FU at there Post-radioactive-iodine hypothyroidism Asthma with nil attack for years Essential hypertension Ocular myasthenia gravis (MG) since 2002
Background history • • 82 -year-old woman, ex-smoker Mother of 6 children Resident in Canada and being FU at there Post-radioactive-iodine hypothyroidism Asthma with nil attack for years Essential hypertension Ocular myasthenia gravis (MG) since 2002
 Long term medication • • • L-thyroxine 75 microgram daily Candesartan 8 mg daily Ventolin 2 puffs Qid PRN Becotide 2 puffs BD Pyridostigmine (Mestinon) 60 mg BD
Long term medication • • • L-thyroxine 75 microgram daily Candesartan 8 mg daily Ventolin 2 puffs Qid PRN Becotide 2 puffs BD Pyridostigmine (Mestinon) 60 mg BD
 History of present illness • Visit Hong Kong since one week ago • Upper respiratory infection since arrival • Fever and sputum for 3 days, and put on oral Levofloxacin 100 mg BD + Romilar • Subjective double vision for one day, with bilateral upper limb weakness + numbness, but still able to walk • While at Precious blood Hospital, developed choking and SOB
History of present illness • Visit Hong Kong since one week ago • Upper respiratory infection since arrival • Fever and sputum for 3 days, and put on oral Levofloxacin 100 mg BD + Romilar • Subjective double vision for one day, with bilateral upper limb weakness + numbness, but still able to walk • While at Precious blood Hospital, developed choking and SOB
 To CMC AED 9/3/08 at 1900 • • BP 202/89, pulse 72, Sa. O 2 88% room air GCS 15/15, Fever 38. 0 degree Speak full sentence, Sa. O 2 96% at 2 L O 2 “muscle weakness” at 4/5 Chest clear; PFR 170 150 Impression: mild MG Decision: consult ICU
To CMC AED 9/3/08 at 1900 • • BP 202/89, pulse 72, Sa. O 2 88% room air GCS 15/15, Fever 38. 0 degree Speak full sentence, Sa. O 2 96% at 2 L O 2 “muscle weakness” at 4/5 Chest clear; PFR 170 150 Impression: mild MG Decision: consult ICU

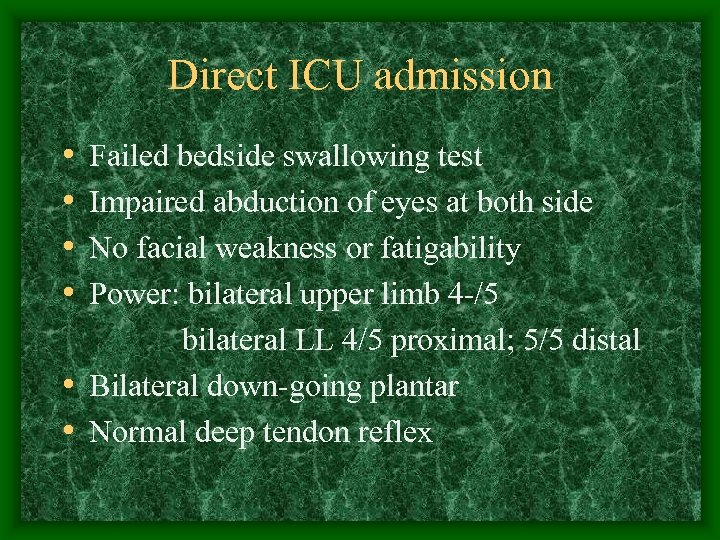 Direct ICU admission • • Failed bedside swallowing test Impaired abduction of eyes at both side No facial weakness or fatigability Power: bilateral upper limb 4 -/5 bilateral LL 4/5 proximal; 5/5 distal • Bilateral down-going plantar • Normal deep tendon reflex
Direct ICU admission • • Failed bedside swallowing test Impaired abduction of eyes at both side No facial weakness or fatigability Power: bilateral upper limb 4 -/5 bilateral LL 4/5 proximal; 5/5 distal • Bilateral down-going plantar • Normal deep tendon reflex
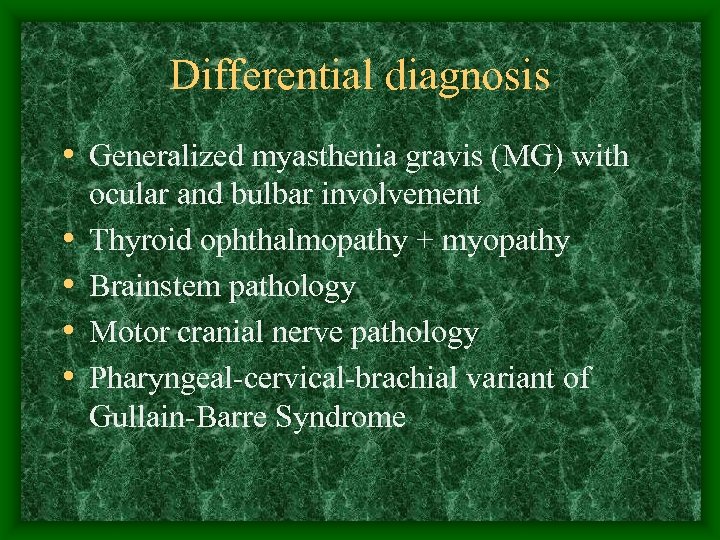 Differential diagnosis • Generalized myasthenia gravis (MG) with • • ocular and bulbar involvement Thyroid ophthalmopathy + myopathy Brainstem pathology Motor cranial nerve pathology Pharyngeal-cervical-brachial variant of Gullain-Barre Syndrome
Differential diagnosis • Generalized myasthenia gravis (MG) with • • ocular and bulbar involvement Thyroid ophthalmopathy + myopathy Brainstem pathology Motor cranial nerve pathology Pharyngeal-cervical-brachial variant of Gullain-Barre Syndrome
 Impression at ICU Generalized MG with bulbar involvement Precipitated by……
Impression at ICU Generalized MG with bulbar involvement Precipitated by……
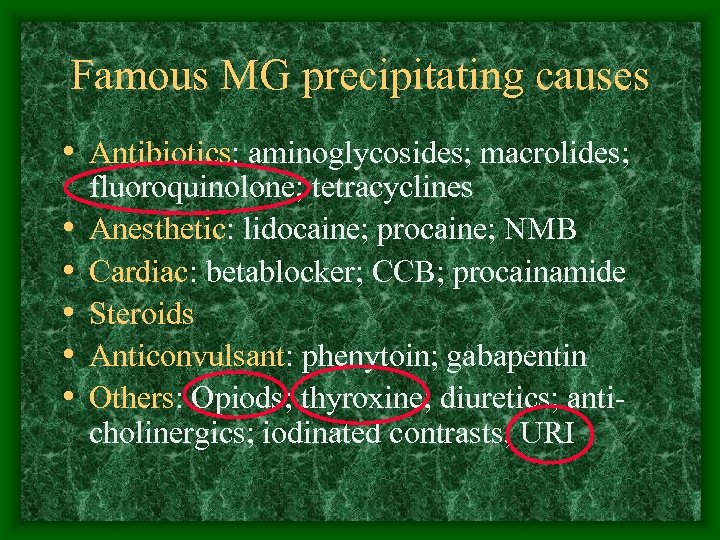 Famous MG precipitating causes • Antibiotics: aminoglycosides; macrolides; • • • fluoroquinolone; tetracyclines Anesthetic: lidocaine; procaine; NMB Cardiac: betablocker; CCB; procainamide Steroids Anticonvulsant: phenytoin; gabapentin Others: Opiods; thyroxine; diuretics; anticholinergics; iodinated contrasts; URI
Famous MG precipitating causes • Antibiotics: aminoglycosides; macrolides; • • • fluoroquinolone; tetracyclines Anesthetic: lidocaine; procaine; NMB Cardiac: betablocker; CCB; procainamide Steroids Anticonvulsant: phenytoin; gabapentin Others: Opiods; thyroxine; diuretics; anticholinergics; iodinated contrasts; URI
 Management by on-call MO • • Keep NPO for possible intubation later Increase Mestinon 60 mg tds Insert RT for medication Check CBP/RFT/LFT/INR/ABG/ESR Blood, sputum and urine for culture Serum viral titre Urgent plain CT brain
Management by on-call MO • • Keep NPO for possible intubation later Increase Mestinon 60 mg tds Insert RT for medication Check CBP/RFT/LFT/INR/ABG/ESR Blood, sputum and urine for culture Serum viral titre Urgent plain CT brain
 Blood test • • WCC 15. 4 (Neutrophil 85. 4%) Hemoglobin 13. 5 with MCV 89. 9 ESR 87 CK 145; albumin 37, globulin 42 RFT and LFT normal TSH 1. 79 (0. 50 -4. 70) p. H 7. 41, CO 2 42. 6, O 2 176, HCO 3 26
Blood test • • WCC 15. 4 (Neutrophil 85. 4%) Hemoglobin 13. 5 with MCV 89. 9 ESR 87 CK 145; albumin 37, globulin 42 RFT and LFT normal TSH 1. 79 (0. 50 -4. 70) p. H 7. 41, CO 2 42. 6, O 2 176, HCO 3 26
 Progress on 10/3/08 at ICU D 2 • Subjective deterioration and require frequent suction of oral secretion/ sputum • Examination in AM around: ØHoarseness and weak cough ØDrooling of saliva ØPoor AE over both chest • Impression: MG crisis
Progress on 10/3/08 at ICU D 2 • Subjective deterioration and require frequent suction of oral secretion/ sputum • Examination in AM around: ØHoarseness and weak cough ØDrooling of saliva ØPoor AE over both chest • Impression: MG crisis
 Bronchoscopy • Very poor cough effort • Continuous aspiration of saliva and upper airway secretion into lower tract • BAL done at right lower lobe for virus study and bacterial culture
Bronchoscopy • Very poor cough effort • Continuous aspiration of saliva and upper airway secretion into lower tract • BAL done at right lower lobe for virus study and bacterial culture
 Management at ICU day 2 • Endotracheal intubation • Start IV Augmentin for chest infection • Start iv Intragram (IVIG) 21 g (BW 53 kg), plan daily dose for 5 days • Trace old record from Canada family doctor about the diagnosis and previous workup of myasthenia gravis
Management at ICU day 2 • Endotracheal intubation • Start IV Augmentin for chest infection • Start iv Intragram (IVIG) 21 g (BW 53 kg), plan daily dose for 5 days • Trace old record from Canada family doctor about the diagnosis and previous workup of myasthenia gravis
 Progress at ICU day 4 • All ocular movement is full, no ptosis • Hand-grip 3/5; right wrist flexion 2/5; rest • • of upper limb power 0/5 ! Both thigh 3/5, both ankle 4/5 Absent deep tendon reflex of lower limb, markedly decreased at upper limb Paraesthesia over 4 limb, nil sensory level BP 100/55, fever down
Progress at ICU day 4 • All ocular movement is full, no ptosis • Hand-grip 3/5; right wrist flexion 2/5; rest • • of upper limb power 0/5 ! Both thigh 3/5, both ankle 4/5 Absent deep tendon reflex of lower limb, markedly decreased at upper limb Paraesthesia over 4 limb, nil sensory level BP 100/55, fever down
 Atypical presentation of MG! Deterioration with iv Ig Other pathology?
Atypical presentation of MG! Deterioration with iv Ig Other pathology?
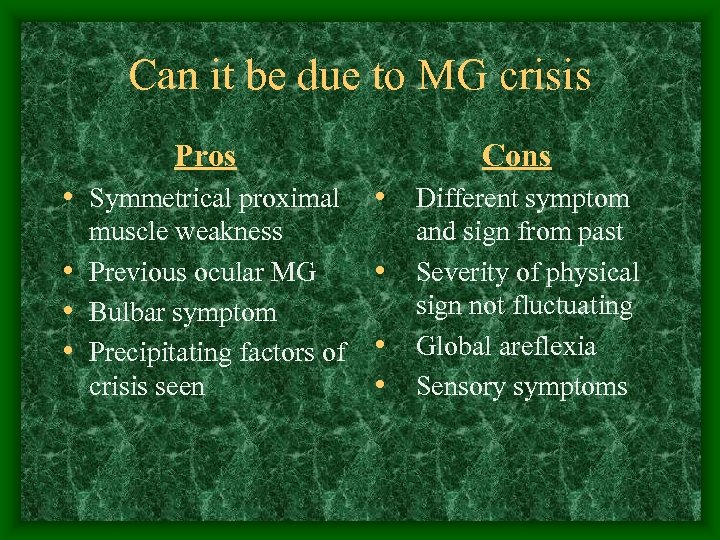 Can it be due to MG crisis Pros • Symmetrical proximal muscle weakness • Previous ocular MG • Bulbar symptom • Precipitating factors of crisis seen Cons • Different symptom • • • and sign from past Severity of physical sign not fluctuating Global areflexia Sensory symptoms
Can it be due to MG crisis Pros • Symmetrical proximal muscle weakness • Previous ocular MG • Bulbar symptom • Precipitating factors of crisis seen Cons • Different symptom • • • and sign from past Severity of physical sign not fluctuating Global areflexia Sensory symptoms
 Management at ICU day 4 • Stop Intragram • Off Mestinon plan to have more MG workup first e. g. electrophysiology • Urgent MRI cervical spine to upper thoracic spine to look for cord lesion • Trace again past medical record from Canada doctor by relative
Management at ICU day 4 • Stop Intragram • Off Mestinon plan to have more MG workup first e. g. electrophysiology • Urgent MRI cervical spine to upper thoracic spine to look for cord lesion • Trace again past medical record from Canada doctor by relative
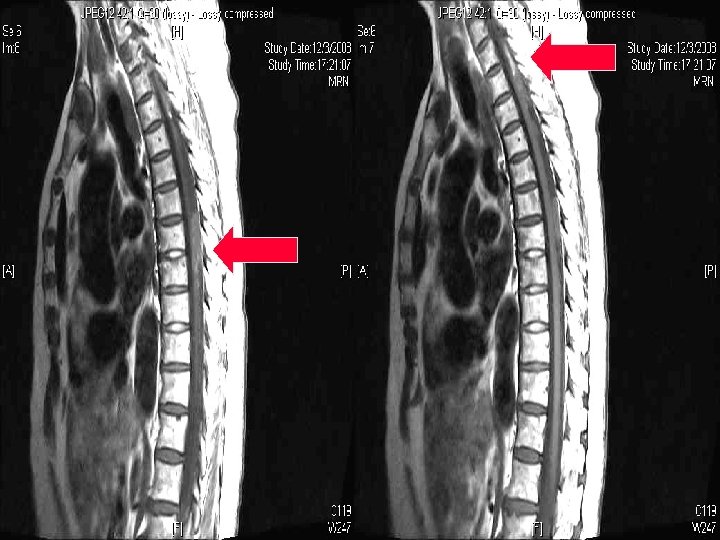
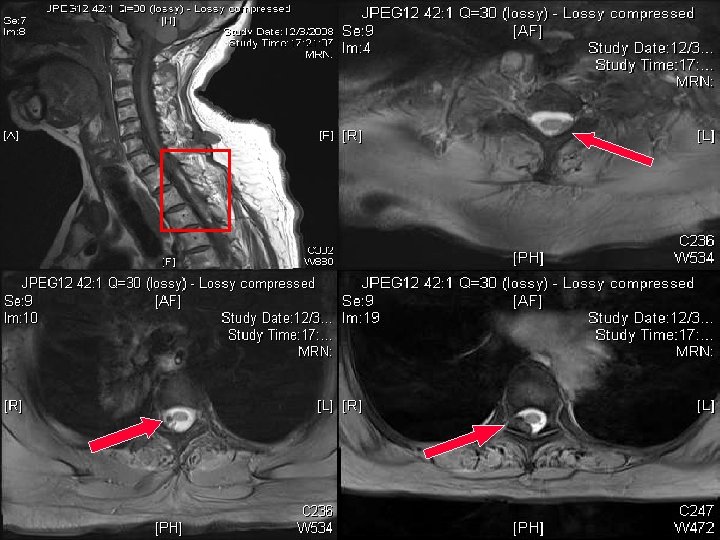
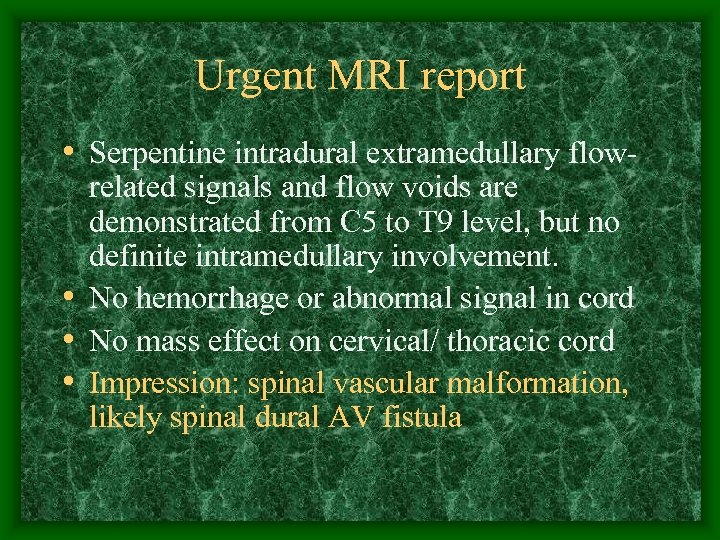 Urgent MRI report • Serpentine intradural extramedullary flowrelated signals and flow voids are demonstrated from C 5 to T 9 level, but no definite intramedullary involvement. • No hemorrhage or abnormal signal in cord • No mass effect on cervical/ thoracic cord • Impression: spinal vascular malformation, likely spinal dural AV fistula
Urgent MRI report • Serpentine intradural extramedullary flowrelated signals and flow voids are demonstrated from C 5 to T 9 level, but no definite intramedullary involvement. • No hemorrhage or abnormal signal in cord • No mass effect on cervical/ thoracic cord • Impression: spinal vascular malformation, likely spinal dural AV fistula
 Can it be spinal cord insult? ! Pros • • Tetraparesis Areflexia Hypotension Normal cognitive function all along • MRI showed vascular lesion around cord Cons • Proximal affected • • preferentially No sensory level Bulbar symptoms Ophthalmoplegia, though improved Normal cord signal
Can it be spinal cord insult? ! Pros • • Tetraparesis Areflexia Hypotension Normal cognitive function all along • MRI showed vascular lesion around cord Cons • Proximal affected • • preferentially No sensory level Bulbar symptoms Ophthalmoplegia, though improved Normal cord signal
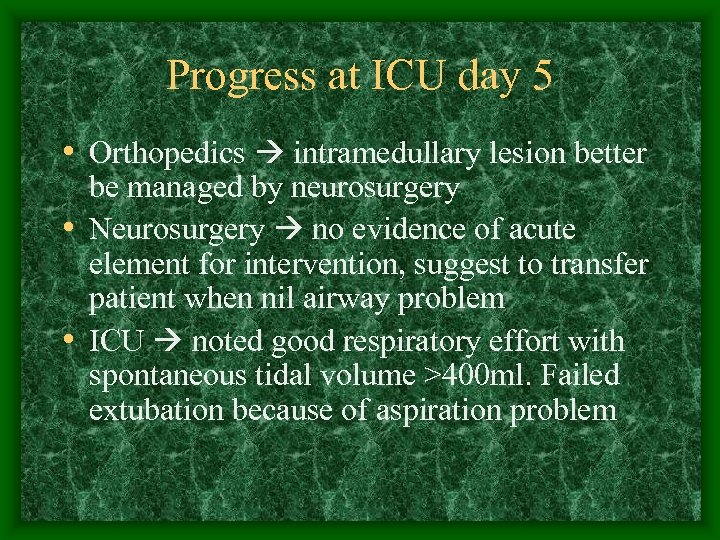 Progress at ICU day 5 • Orthopedics intramedullary lesion better be managed by neurosurgery • Neurosurgery no evidence of acute element for intervention, suggest to transfer patient when nil airway problem • ICU noted good respiratory effort with spontaneous tidal volume >400 ml. Failed extubation because of aspiration problem
Progress at ICU day 5 • Orthopedics intramedullary lesion better be managed by neurosurgery • Neurosurgery no evidence of acute element for intervention, suggest to transfer patient when nil airway problem • ICU noted good respiratory effort with spontaneous tidal volume >400 ml. Failed extubation because of aspiration problem
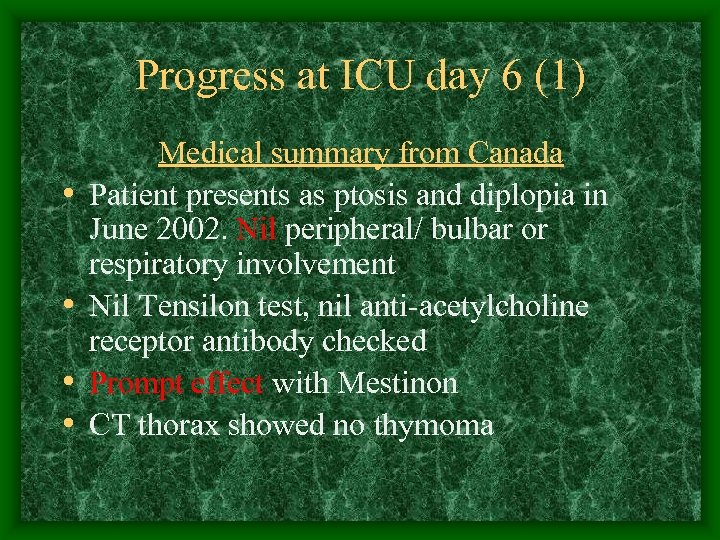 Progress at ICU day 6 (1) • • Medical summary from Canada Patient presents as ptosis and diplopia in June 2002. Nil peripheral/ bulbar or respiratory involvement Nil Tensilon test, nil anti-acetylcholine receptor antibody checked Prompt effect with Mestinon CT thorax showed no thymoma
Progress at ICU day 6 (1) • • Medical summary from Canada Patient presents as ptosis and diplopia in June 2002. Nil peripheral/ bulbar or respiratory involvement Nil Tensilon test, nil anti-acetylcholine receptor antibody checked Prompt effect with Mestinon CT thorax showed no thymoma
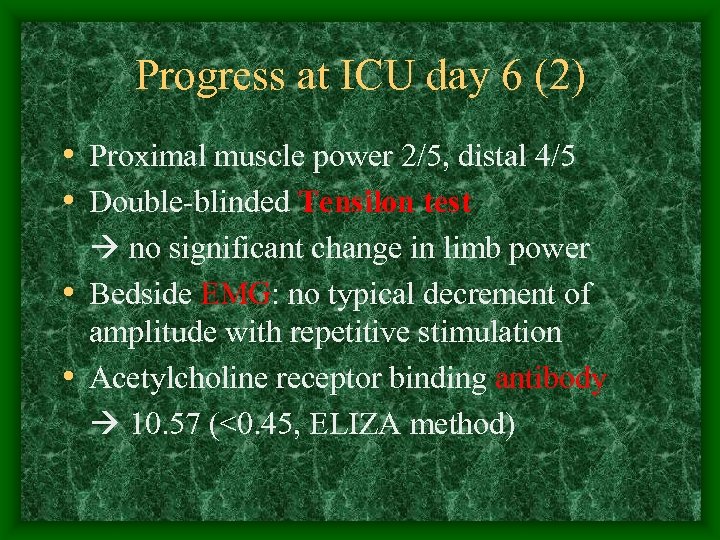 Progress at ICU day 6 (2) • Proximal muscle power 2/5, distal 4/5 • Double-blinded Tensilon test no significant change in limb power • Bedside EMG: no typical decrement of amplitude with repetitive stimulation • Acetylcholine receptor binding antibody 10. 57 (<0. 45, ELIZA method)
Progress at ICU day 6 (2) • Proximal muscle power 2/5, distal 4/5 • Double-blinded Tensilon test no significant change in limb power • Bedside EMG: no typical decrement of amplitude with repetitive stimulation • Acetylcholine receptor binding antibody 10. 57 (<0. 45, ELIZA method)
 Every sign must have explanation
Every sign must have explanation
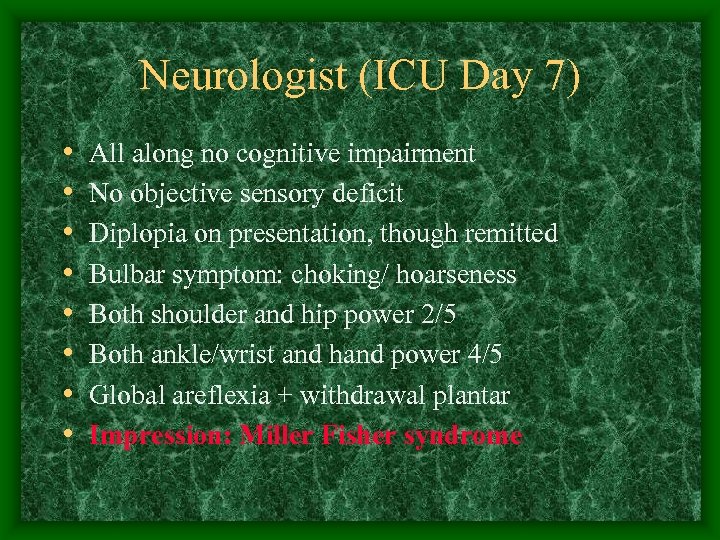 Neurologist (ICU Day 7) • • All along no cognitive impairment No objective sensory deficit Diplopia on presentation, though remitted Bulbar symptom: choking/ hoarseness Both shoulder and hip power 2/5 Both ankle/wrist and hand power 4/5 Global areflexia + withdrawal plantar Impression: Miller Fisher syndrome
Neurologist (ICU Day 7) • • All along no cognitive impairment No objective sensory deficit Diplopia on presentation, though remitted Bulbar symptom: choking/ hoarseness Both shoulder and hip power 2/5 Both ankle/wrist and hand power 4/5 Global areflexia + withdrawal plantar Impression: Miller Fisher syndrome
 Retrospectively, look at the graph of vital signs…….
Retrospectively, look at the graph of vital signs…….
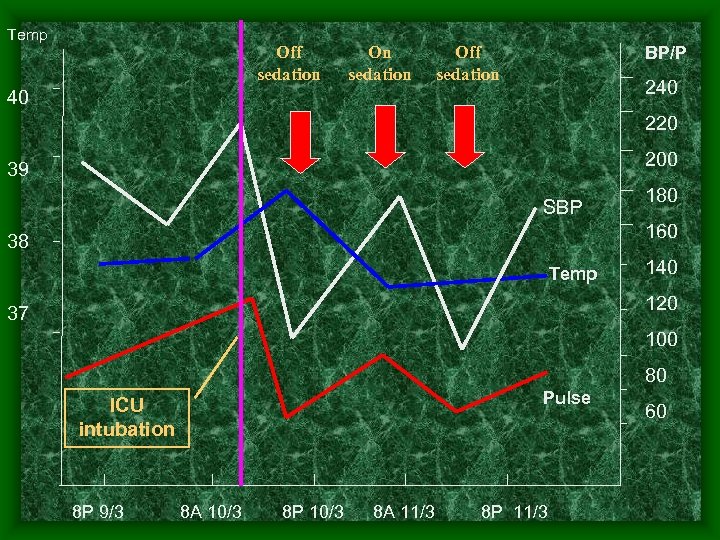 Temp Off sedation On sedation BP/P Off sedation 240 40 220 200 39 SBP 180 160 38 Temp 140 120 37 100 80 Pulse ICU intubation 8 P 9/3 8 A 10/3 8 P 10/3 8 A 11/3 8 P 11/3 60
Temp Off sedation On sedation BP/P Off sedation 240 40 220 200 39 SBP 180 160 38 Temp 140 120 37 100 80 Pulse ICU intubation 8 P 9/3 8 A 10/3 8 P 10/3 8 A 11/3 8 P 11/3 60
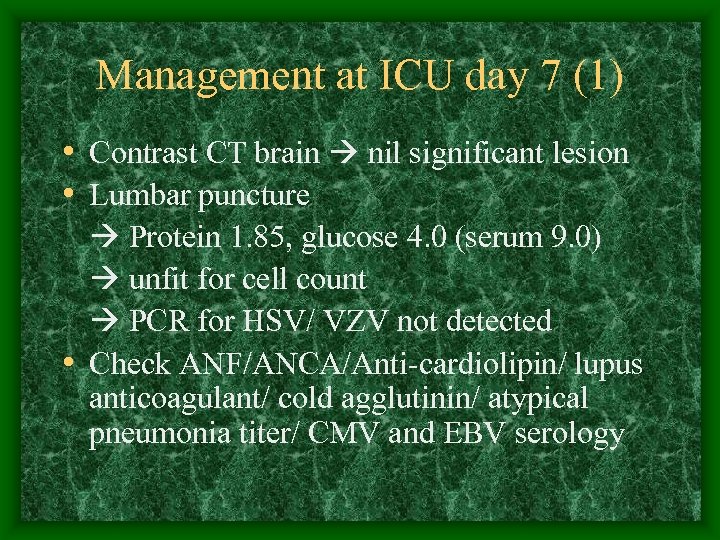 Management at ICU day 7 (1) • Contrast CT brain nil significant lesion • Lumbar puncture Protein 1. 85, glucose 4. 0 (serum 9. 0) unfit for cell count PCR for HSV/ VZV not detected • Check ANF/ANCA/Anti-cardiolipin/ lupus anticoagulant/ cold agglutinin/ atypical pneumonia titer/ CMV and EBV serology
Management at ICU day 7 (1) • Contrast CT brain nil significant lesion • Lumbar puncture Protein 1. 85, glucose 4. 0 (serum 9. 0) unfit for cell count PCR for HSV/ VZV not detected • Check ANF/ANCA/Anti-cardiolipin/ lupus anticoagulant/ cold agglutinin/ atypical pneumonia titer/ CMV and EBV serology
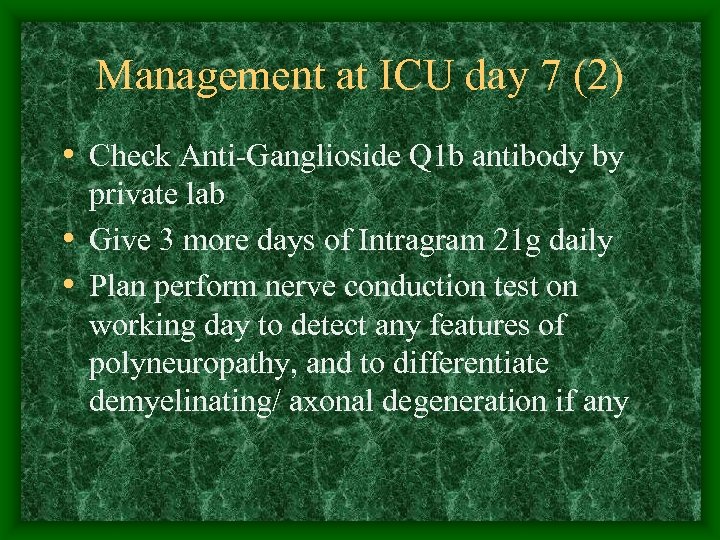 Management at ICU day 7 (2) • Check Anti-Ganglioside Q 1 b antibody by private lab • Give 3 more days of Intragram 21 g daily • Plan perform nerve conduction test on working day to detect any features of polyneuropathy, and to differentiate demyelinating/ axonal degeneration if any
Management at ICU day 7 (2) • Check Anti-Ganglioside Q 1 b antibody by private lab • Give 3 more days of Intragram 21 g daily • Plan perform nerve conduction test on working day to detect any features of polyneuropathy, and to differentiate demyelinating/ axonal degeneration if any
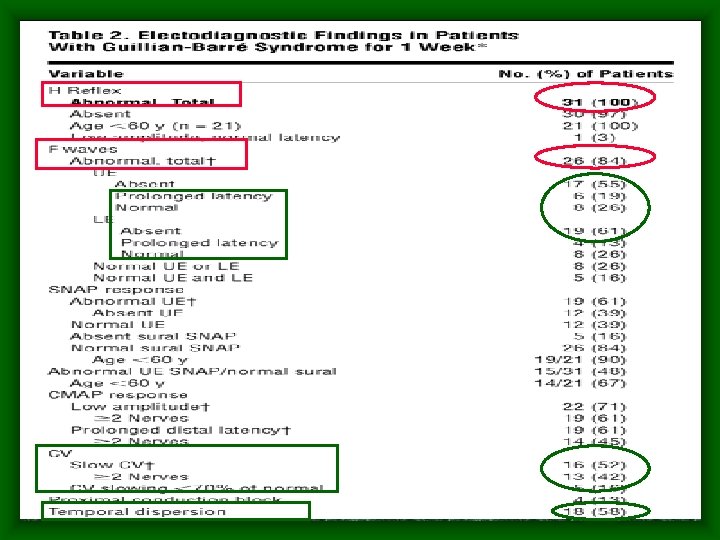
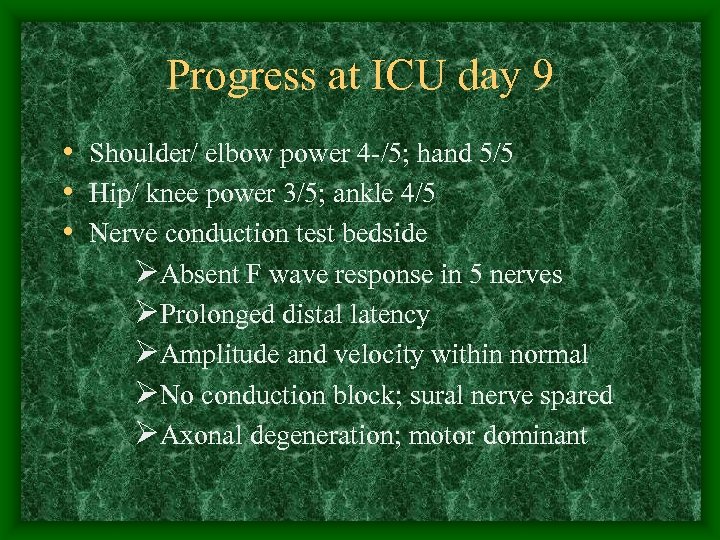 Progress at ICU day 9 • Shoulder/ elbow power 4 -/5; hand 5/5 • Hip/ knee power 3/5; ankle 4/5 • Nerve conduction test bedside ØAbsent F wave response in 5 nerves ØProlonged distal latency ØAmplitude and velocity within normal ØNo conduction block; sural nerve spared ØAxonal degeneration; motor dominant
Progress at ICU day 9 • Shoulder/ elbow power 4 -/5; hand 5/5 • Hip/ knee power 3/5; ankle 4/5 • Nerve conduction test bedside ØAbsent F wave response in 5 nerves ØProlonged distal latency ØAmplitude and velocity within normal ØNo conduction block; sural nerve spared ØAxonal degeneration; motor dominant
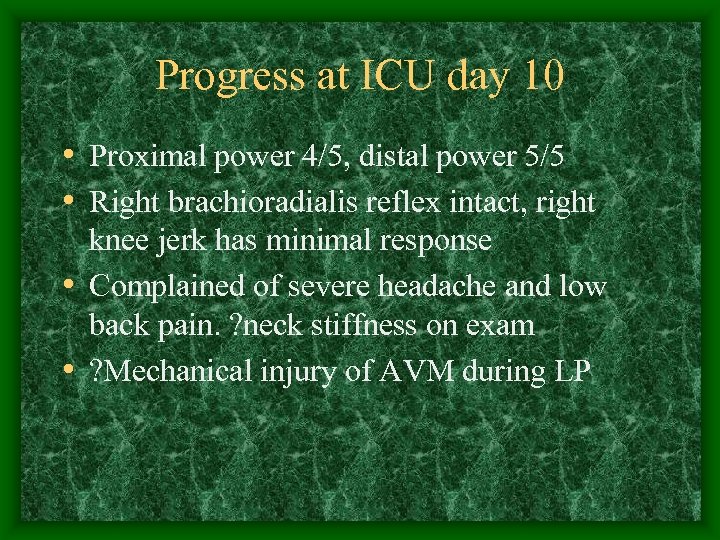 Progress at ICU day 10 • Proximal power 4/5, distal power 5/5 • Right brachioradialis reflex intact, right knee jerk has minimal response • Complained of severe headache and low back pain. ? neck stiffness on exam • ? Mechanical injury of AVM during LP
Progress at ICU day 10 • Proximal power 4/5, distal power 5/5 • Right brachioradialis reflex intact, right knee jerk has minimal response • Complained of severe headache and low back pain. ? neck stiffness on exam • ? Mechanical injury of AVM during LP
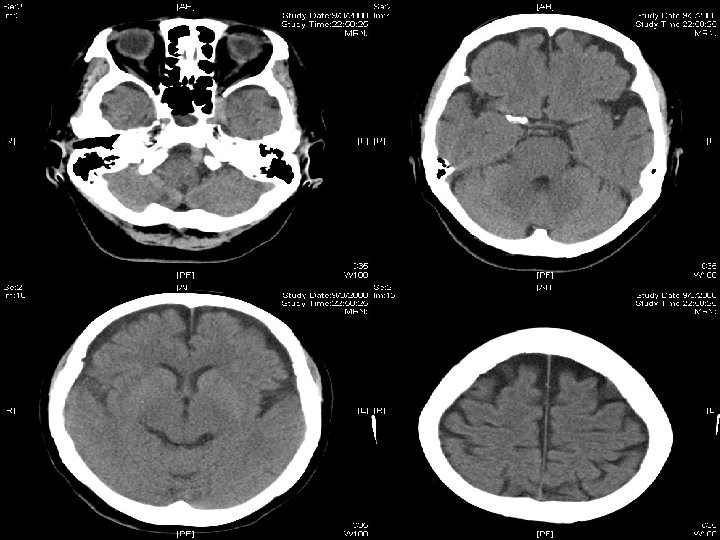
 CT brain + C-spine + L-spine • Brain showed nil significant abnormality • No abnormal vasculature in cervical cord • Small enhancing vessels along surface of thecal sac at level down to L 2 • No evidence of bleeding from vessel
CT brain + C-spine + L-spine • Brain showed nil significant abnormality • No abnormal vasculature in cervical cord • Small enhancing vessels along surface of thecal sac at level down to L 2 • No evidence of bleeding from vessel
 Our decision
Our decision
 Further progress • • Off RT and oral diet tolerated since day 11 Discharge to general ward on day 15 Anti-Ganglioside Q 1 b 105 (<20) ANF 1: 80; Anti-ds DNA 13 (<35) C-ANCA weak +ve; PR 3 -ANCA 6 (<20) Cold agglutinin 8 (<32) Lupus anticoagulant not detected Anti-cardiolipin Ig. G 9. 5 (weak +ve)
Further progress • • Off RT and oral diet tolerated since day 11 Discharge to general ward on day 15 Anti-Ganglioside Q 1 b 105 (<20) ANF 1: 80; Anti-ds DNA 13 (<35) C-ANCA weak +ve; PR 3 -ANCA 6 (<20) Cold agglutinin 8 (<32) Lupus anticoagulant not detected Anti-cardiolipin Ig. G 9. 5 (weak +ve)
 At rehabilitation • Repeated NCT on day 19 showed improving polyneuropathy. Yet EMG showed equivocal MG features • Repeated Tensilon test on day 25 Still NEGATIVE result • Neurology opinion not to resume Mestinon since MG not the dominant illness • Home on day 48
At rehabilitation • Repeated NCT on day 19 showed improving polyneuropathy. Yet EMG showed equivocal MG features • Repeated Tensilon test on day 25 Still NEGATIVE result • Neurology opinion not to resume Mestinon since MG not the dominant illness • Home on day 48
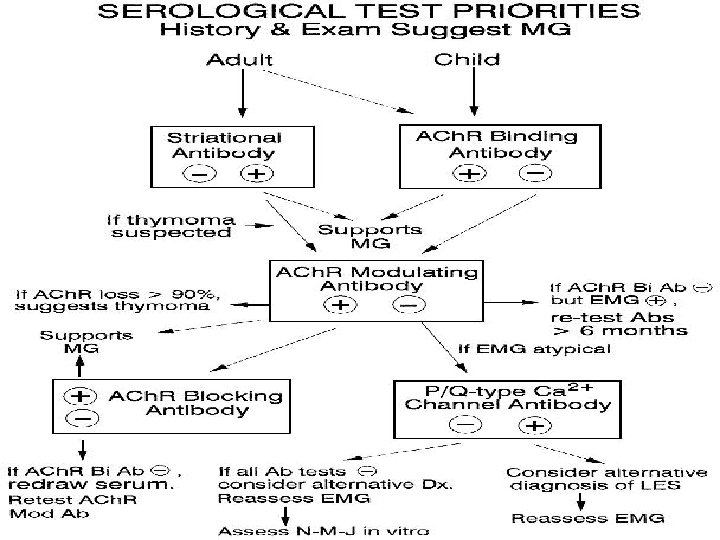
 Neurology FU • No ocular/ bulbar or peripheral symptom • Private MRI brain and brain stem bilateral frontal lobe atrophy only • Imp: assay for ACh. R binding antibody in HA is ELIZA, may not be specific enough • Decision: check ACh. R binding antibody (RIA) + ACh. R modulating antibody + ACh. R blocking antibody
Neurology FU • No ocular/ bulbar or peripheral symptom • Private MRI brain and brain stem bilateral frontal lobe atrophy only • Imp: assay for ACh. R binding antibody in HA is ELIZA, may not be specific enough • Decision: check ACh. R binding antibody (RIA) + ACh. R modulating antibody + ACh. R blocking antibody
 Myasthenia Gravis overview • Autoimmune disease • Antibodies against post-synaptic acetylcholine receptor (ACh. R), or receptor associated protein (muscle-specific TK) • Fluctuating weakness of muscles in various combination of ocular; bulbar; limb; resp • Two clinical form: Ocular vs. Generalized
Myasthenia Gravis overview • Autoimmune disease • Antibodies against post-synaptic acetylcholine receptor (ACh. R), or receptor associated protein (muscle-specific TK) • Fluctuating weakness of muscles in various combination of ocular; bulbar; limb; resp • Two clinical form: Ocular vs. Generalized
 Presenting symptoms • Ocular: >50%. Among ocular presentation, >50% progress to generalized in 2 years • Bulbar: 15%. Dysarthria/ dysphagia and fatigable chewing • Proximal limb: <5% as presenting symptom • Rare: isolated neck; isolated resp; isolated distal limb weakness
Presenting symptoms • Ocular: >50%. Among ocular presentation, >50% progress to generalized in 2 years • Bulbar: 15%. Dysarthria/ dysphagia and fatigable chewing • Proximal limb: <5% as presenting symptom • Rare: isolated neck; isolated resp; isolated distal limb weakness
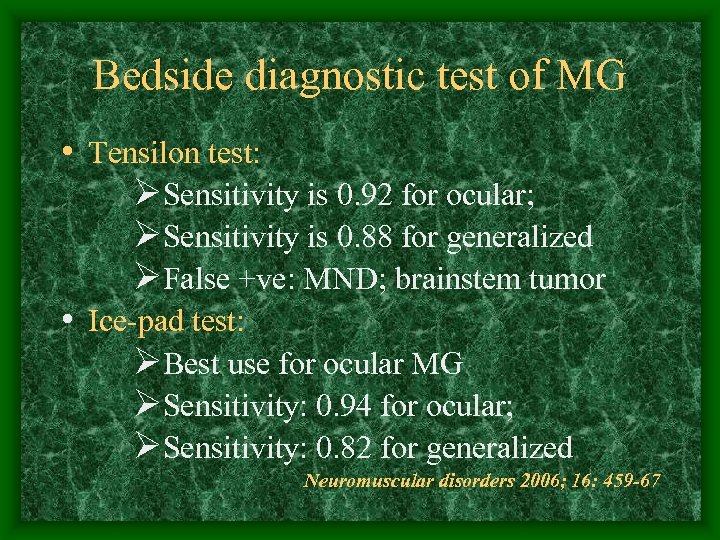 Bedside diagnostic test of MG • Tensilon test: ØSensitivity is 0. 92 for ocular; ØSensitivity is 0. 88 for generalized ØFalse +ve: MND; brainstem tumor • Ice-pad test: ØBest use for ocular MG ØSensitivity: 0. 94 for ocular; ØSensitivity: 0. 82 for generalized Neuromuscular disorders 2006; 16: 459 -67
Bedside diagnostic test of MG • Tensilon test: ØSensitivity is 0. 92 for ocular; ØSensitivity is 0. 88 for generalized ØFalse +ve: MND; brainstem tumor • Ice-pad test: ØBest use for ocular MG ØSensitivity: 0. 94 for ocular; ØSensitivity: 0. 82 for generalized Neuromuscular disorders 2006; 16: 459 -67
 Ice test 2 min ice Ophthalmology 1999: 106: 1282
Ice test 2 min ice Ophthalmology 1999: 106: 1282
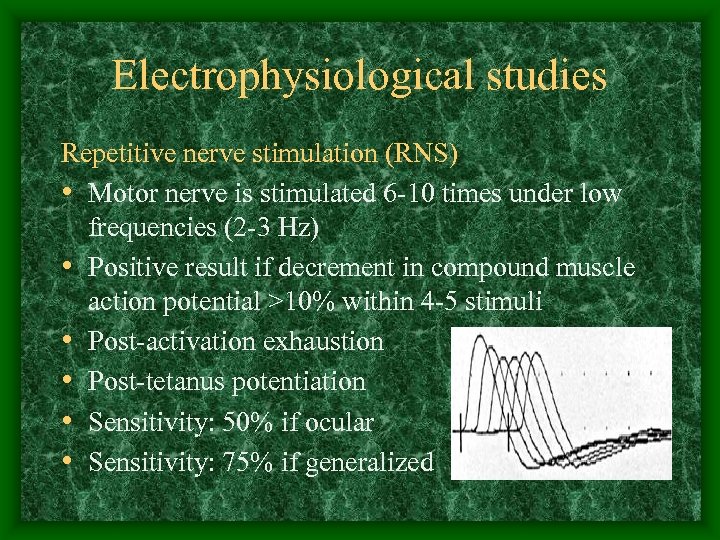 Electrophysiological studies Repetitive nerve stimulation (RNS) • Motor nerve is stimulated 6 -10 times under low frequencies (2 -3 Hz) • Positive result if decrement in compound muscle action potential >10% within 4 -5 stimuli • Post-activation exhaustion • Post-tetanus potentiation • Sensitivity: 50% if ocular • Sensitivity: 75% if generalized
Electrophysiological studies Repetitive nerve stimulation (RNS) • Motor nerve is stimulated 6 -10 times under low frequencies (2 -3 Hz) • Positive result if decrement in compound muscle action potential >10% within 4 -5 stimuli • Post-activation exhaustion • Post-tetanus potentiation • Sensitivity: 50% if ocular • Sensitivity: 75% if generalized
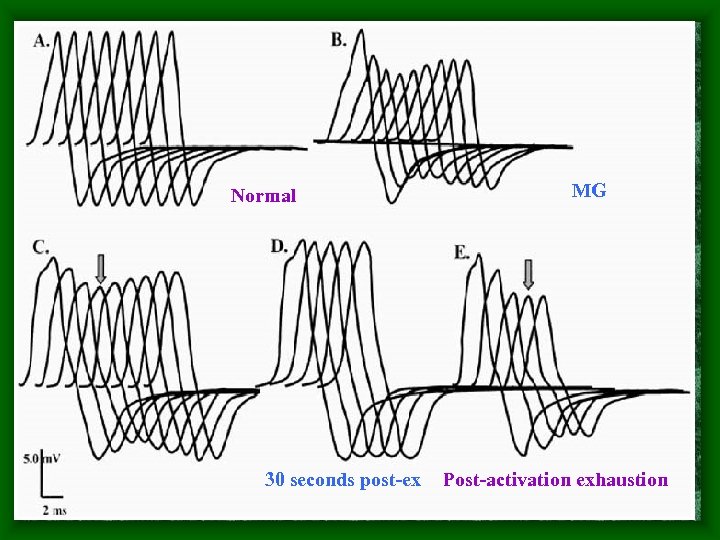 Normal 30 seconds post-ex MG Post-activation exhaustion
Normal 30 seconds post-ex MG Post-activation exhaustion
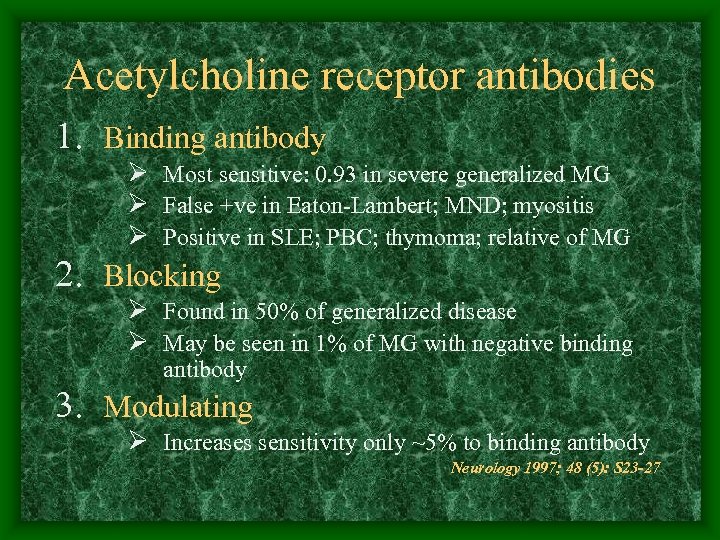 Acetylcholine receptor antibodies 1. Binding antibody Ø Most sensitive: 0. 93 in severe generalized MG Ø False +ve in Eaton-Lambert; MND; myositis Ø Positive in SLE; PBC; thymoma; relative of MG 2. Blocking Ø Found in 50% of generalized disease Ø May be seen in 1% of MG with negative binding antibody 3. Modulating Ø Increases sensitivity only ~5% to binding antibody Neurology 1997; 48 (5): S 23 -27
Acetylcholine receptor antibodies 1. Binding antibody Ø Most sensitive: 0. 93 in severe generalized MG Ø False +ve in Eaton-Lambert; MND; myositis Ø Positive in SLE; PBC; thymoma; relative of MG 2. Blocking Ø Found in 50% of generalized disease Ø May be seen in 1% of MG with negative binding antibody 3. Modulating Ø Increases sensitivity only ~5% to binding antibody Neurology 1997; 48 (5): S 23 -27
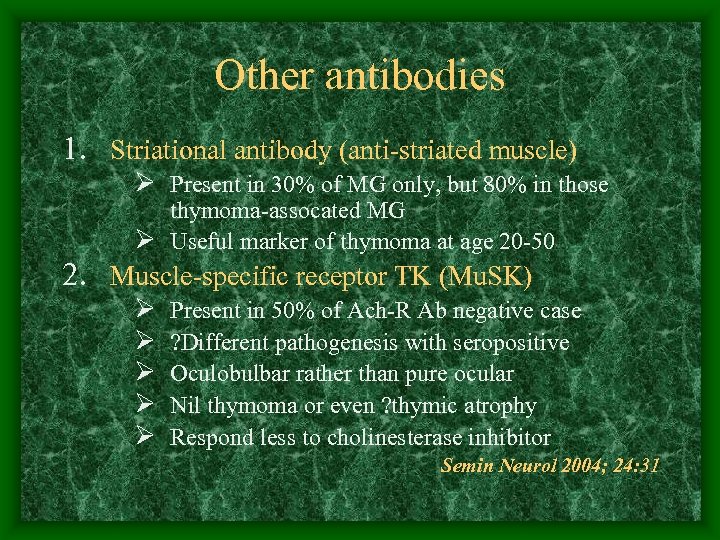 Other antibodies 1. Striational antibody (anti-striated muscle) Ø Present in 30% of MG only, but 80% in those thymoma-assocated MG Ø Useful marker of thymoma at age 20 -50 2. Muscle-specific receptor TK (Mu. SK) Ø Ø Ø Present in 50% of Ach-R Ab negative case ? Different pathogenesis with seropositive Oculobulbar rather than pure ocular Nil thymoma or even ? thymic atrophy Respond less to cholinesterase inhibitor Semin Neurol 2004; 24: 31
Other antibodies 1. Striational antibody (anti-striated muscle) Ø Present in 30% of MG only, but 80% in those thymoma-assocated MG Ø Useful marker of thymoma at age 20 -50 2. Muscle-specific receptor TK (Mu. SK) Ø Ø Ø Present in 50% of Ach-R Ab negative case ? Different pathogenesis with seropositive Oculobulbar rather than pure ocular Nil thymoma or even ? thymic atrophy Respond less to cholinesterase inhibitor Semin Neurol 2004; 24: 31
 Our patients had all three Ach. R antibodies positive, with titre high or very high at OPD
Our patients had all three Ach. R antibodies positive, with titre high or very high at OPD
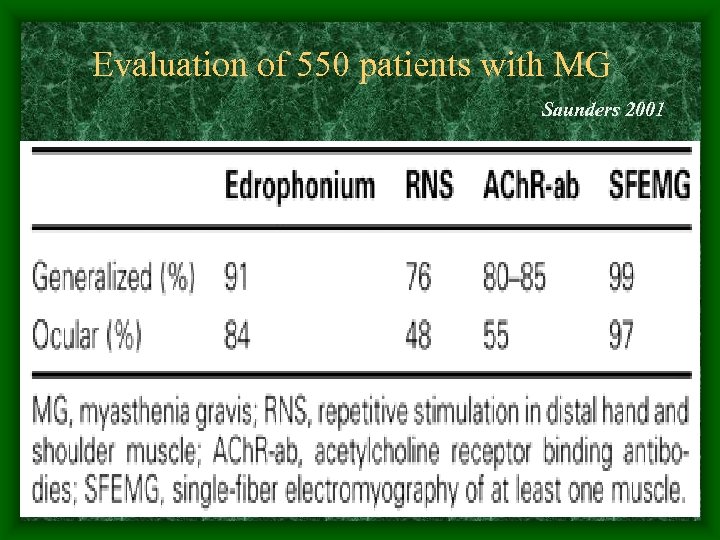 Evaluation of 550 patients with MG Saunders 2001
Evaluation of 550 patients with MG Saunders 2001
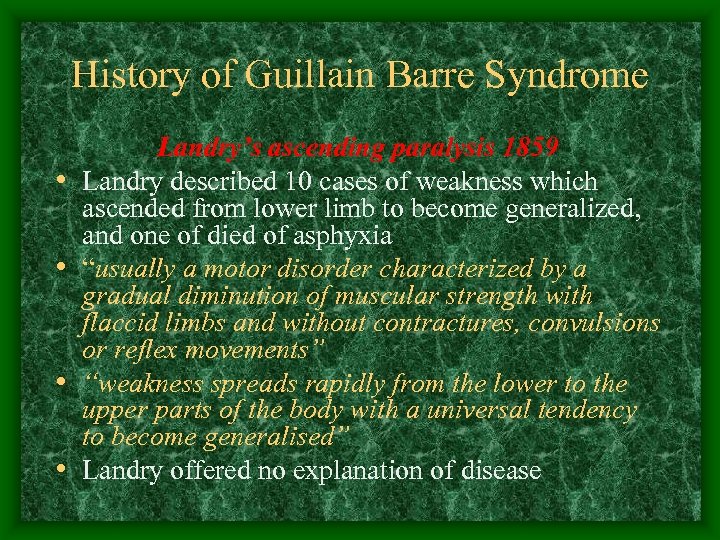 History of Guillain Barre Syndrome • • Landry’s ascending paralysis 1859 Landry described 10 cases of weakness which ascended from lower limb to become generalized, and one of died of asphyxia “usually a motor disorder characterized by a gradual diminution of muscular strength with flaccid limbs and without contractures, convulsions or reflex movements” “weakness spreads rapidly from the lower to the upper parts of the body with a universal tendency to become generalised” Landry offered no explanation of disease
History of Guillain Barre Syndrome • • Landry’s ascending paralysis 1859 Landry described 10 cases of weakness which ascended from lower limb to become generalized, and one of died of asphyxia “usually a motor disorder characterized by a gradual diminution of muscular strength with flaccid limbs and without contractures, convulsions or reflex movements” “weakness spreads rapidly from the lower to the upper parts of the body with a universal tendency to become generalised” Landry offered no explanation of disease
 • Guillain and Barre spotted two soldiers in WWI becoming partially paralyzed, but then recovered spontaneously • With Strohl, a paper was published in 1916, reporting educed reflexes and CSF finding of raised protein without high WCC • In 1927, Guillain Barre syndrome was introduced, but Strohl…. . .
• Guillain and Barre spotted two soldiers in WWI becoming partially paralyzed, but then recovered spontaneously • With Strohl, a paper was published in 1916, reporting educed reflexes and CSF finding of raised protein without high WCC • In 1927, Guillain Barre syndrome was introduced, but Strohl…. . .
 Guillain Strohl Barre
Guillain Strohl Barre
 Essential features of GBS • Progressive symmetrical muscle weakness associated with depressed deep tendon reflexes, usually begins at proximal legs • Severity varies a lot from mild difficulty in walking to complete paralysis and respiratory failure • Extremities, facial, bulbar and respiratory muscles are affected in combination
Essential features of GBS • Progressive symmetrical muscle weakness associated with depressed deep tendon reflexes, usually begins at proximal legs • Severity varies a lot from mild difficulty in walking to complete paralysis and respiratory failure • Extremities, facial, bulbar and respiratory muscles are affected in combination
 Other features of GBS • • Facial weakness >50% Oropharyngeal weakness 50% Oculomotor weakness 15% Respiratory failure ventilation 30% Begins from face and UL 10% Paresthesias in hand/feet 80% (Yet nil sign) Prominent severe back pain Dysautonomia 70% (e. g. HT alt with shock) NEJM 1992; 326: 1130
Other features of GBS • • Facial weakness >50% Oropharyngeal weakness 50% Oculomotor weakness 15% Respiratory failure ventilation 30% Begins from face and UL 10% Paresthesias in hand/feet 80% (Yet nil sign) Prominent severe back pain Dysautonomia 70% (e. g. HT alt with shock) NEJM 1992; 326: 1130
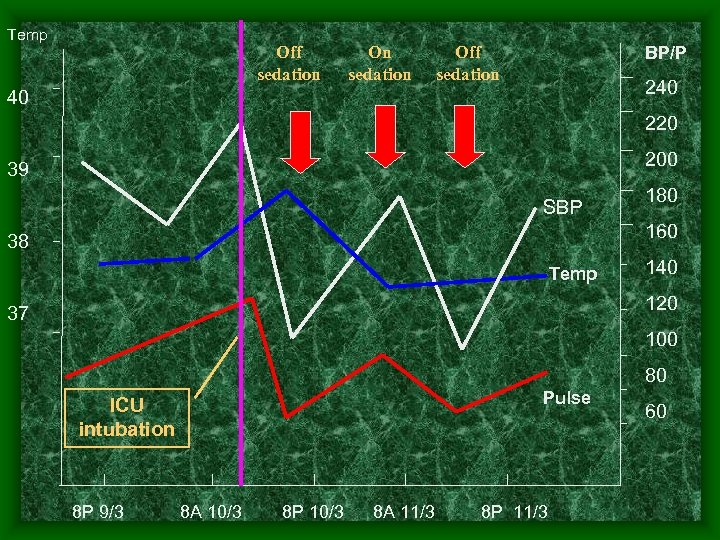 Temp Off sedation On sedation BP/P Off sedation 240 40 220 200 39 SBP 180 160 38 Temp 140 120 37 100 80 Pulse ICU intubation 8 P 9/3 8 A 10/3 8 P 10/3 8 A 11/3 8 P 11/3 60
Temp Off sedation On sedation BP/P Off sedation 240 40 220 200 39 SBP 180 160 38 Temp 140 120 37 100 80 Pulse ICU intubation 8 P 9/3 8 A 10/3 8 P 10/3 8 A 11/3 8 P 11/3 60
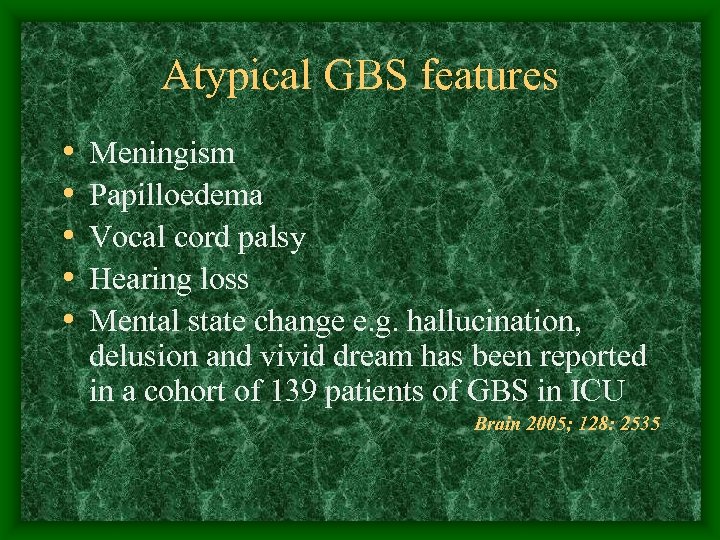 Atypical GBS features • • • Meningism Papilloedema Vocal cord palsy Hearing loss Mental state change e. g. hallucination, delusion and vivid dream has been reported in a cohort of 139 patients of GBS in ICU Brain 2005; 128: 2535
Atypical GBS features • • • Meningism Papilloedema Vocal cord palsy Hearing loss Mental state change e. g. hallucination, delusion and vivid dream has been reported in a cohort of 139 patients of GBS in ICU Brain 2005; 128: 2535
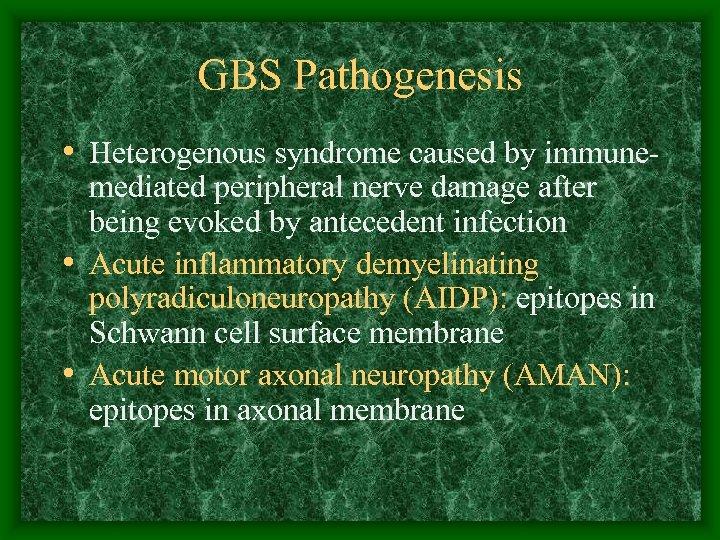 GBS Pathogenesis • Heterogenous syndrome caused by immunemediated peripheral nerve damage after being evoked by antecedent infection • Acute inflammatory demyelinating polyradiculoneuropathy (AIDP): epitopes in Schwann cell surface membrane • Acute motor axonal neuropathy (AMAN): epitopes in axonal membrane
GBS Pathogenesis • Heterogenous syndrome caused by immunemediated peripheral nerve damage after being evoked by antecedent infection • Acute inflammatory demyelinating polyradiculoneuropathy (AIDP): epitopes in Schwann cell surface membrane • Acute motor axonal neuropathy (AMAN): epitopes in axonal membrane
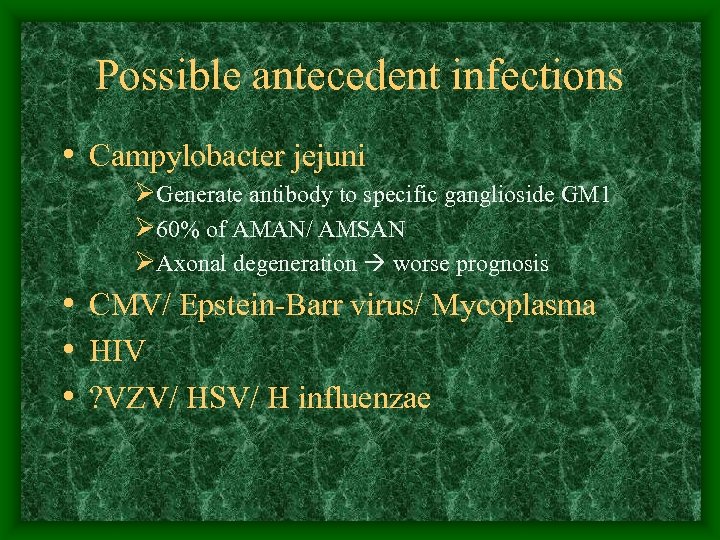 Possible antecedent infections • Campylobacter jejuni ØGenerate antibody to specific ganglioside GM 1 Ø 60% of AMAN/ AMSAN ØAxonal degeneration worse prognosis • CMV/ Epstein-Barr virus/ Mycoplasma • HIV • ? VZV/ HSV/ H influenzae
Possible antecedent infections • Campylobacter jejuni ØGenerate antibody to specific ganglioside GM 1 Ø 60% of AMAN/ AMSAN ØAxonal degeneration worse prognosis • CMV/ Epstein-Barr virus/ Mycoplasma • HIV • ? VZV/ HSV/ H influenzae
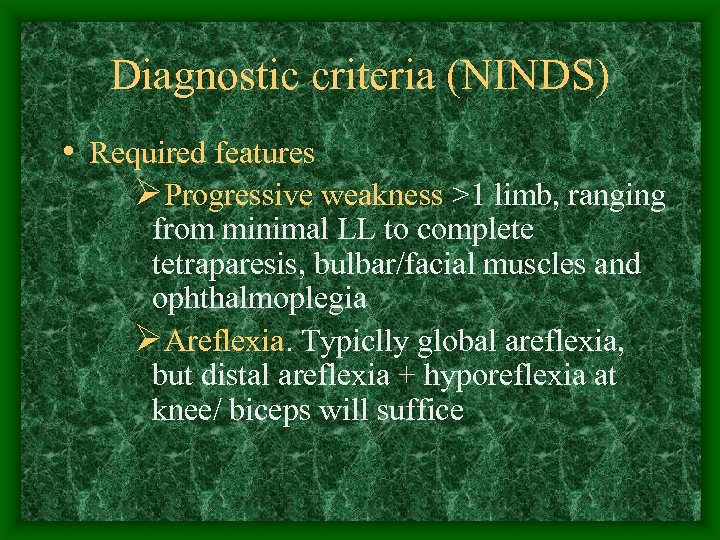 Diagnostic criteria (NINDS) • Required features ØProgressive weakness >1 limb, ranging from minimal LL to complete tetraparesis, bulbar/facial muscles and ophthalmoplegia ØAreflexia. Typiclly global areflexia, but distal areflexia + hyporeflexia at knee/ biceps will suffice
Diagnostic criteria (NINDS) • Required features ØProgressive weakness >1 limb, ranging from minimal LL to complete tetraparesis, bulbar/facial muscles and ophthalmoplegia ØAreflexia. Typiclly global areflexia, but distal areflexia + hyporeflexia at knee/ biceps will suffice
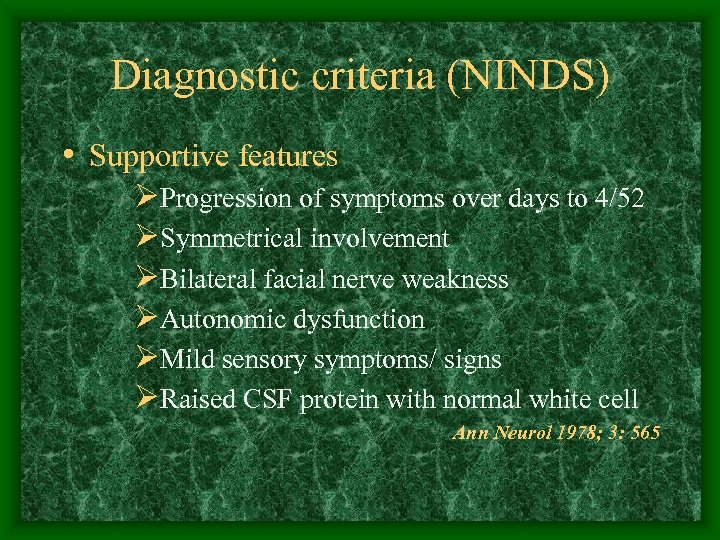 Diagnostic criteria (NINDS) • Supportive features ØProgression of symptoms over days to 4/52 ØSymmetrical involvement ØBilateral facial nerve weakness ØAutonomic dysfunction ØMild sensory symptoms/ signs ØRaised CSF protein with normal white cell Ann Neurol 1978; 3: 565
Diagnostic criteria (NINDS) • Supportive features ØProgression of symptoms over days to 4/52 ØSymmetrical involvement ØBilateral facial nerve weakness ØAutonomic dysfunction ØMild sensory symptoms/ signs ØRaised CSF protein with normal white cell Ann Neurol 1978; 3: 565
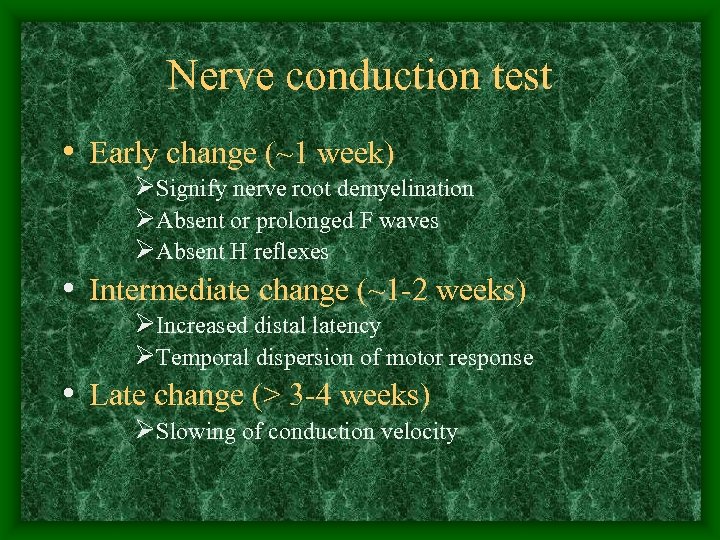 Nerve conduction test • Early change (~1 week) ØSignify nerve root demyelination ØAbsent or prolonged F waves ØAbsent H reflexes • Intermediate change (~1 -2 weeks) ØIncreased distal latency ØTemporal dispersion of motor response • Late change (> 3 -4 weeks) ØSlowing of conduction velocity
Nerve conduction test • Early change (~1 week) ØSignify nerve root demyelination ØAbsent or prolonged F waves ØAbsent H reflexes • Intermediate change (~1 -2 weeks) ØIncreased distal latency ØTemporal dispersion of motor response • Late change (> 3 -4 weeks) ØSlowing of conduction velocity
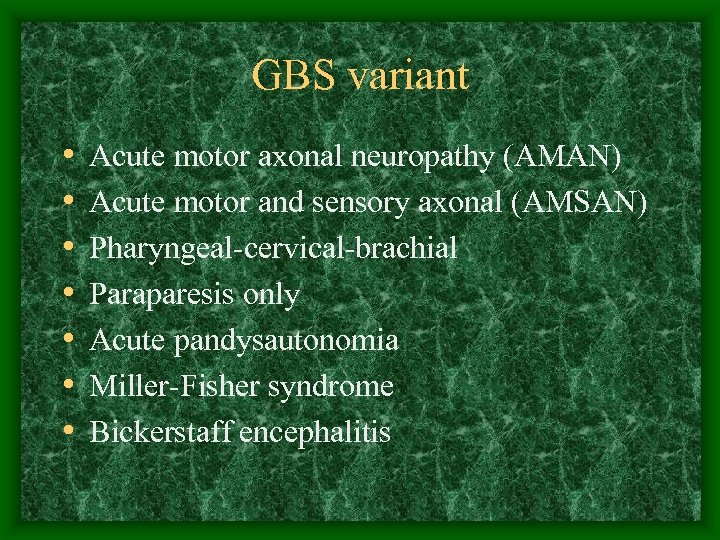 GBS variant • • Acute motor axonal neuropathy (AMAN) Acute motor and sensory axonal (AMSAN) Pharyngeal-cervical-brachial Paraparesis only Acute pandysautonomia Miller-Fisher syndrome Bickerstaff encephalitis
GBS variant • • Acute motor axonal neuropathy (AMAN) Acute motor and sensory axonal (AMSAN) Pharyngeal-cervical-brachial Paraparesis only Acute pandysautonomia Miller-Fisher syndrome Bickerstaff encephalitis
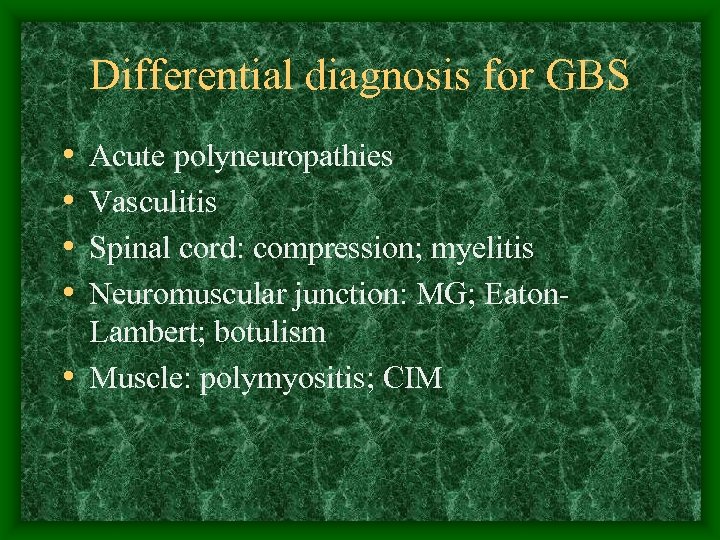 Differential diagnosis for GBS • • Acute polyneuropathies Vasculitis Spinal cord: compression; myelitis Neuromuscular junction: MG; Eaton. Lambert; botulism • Muscle: polymyositis; CIM
Differential diagnosis for GBS • • Acute polyneuropathies Vasculitis Spinal cord: compression; myelitis Neuromuscular junction: MG; Eaton. Lambert; botulism • Muscle: polymyositis; CIM
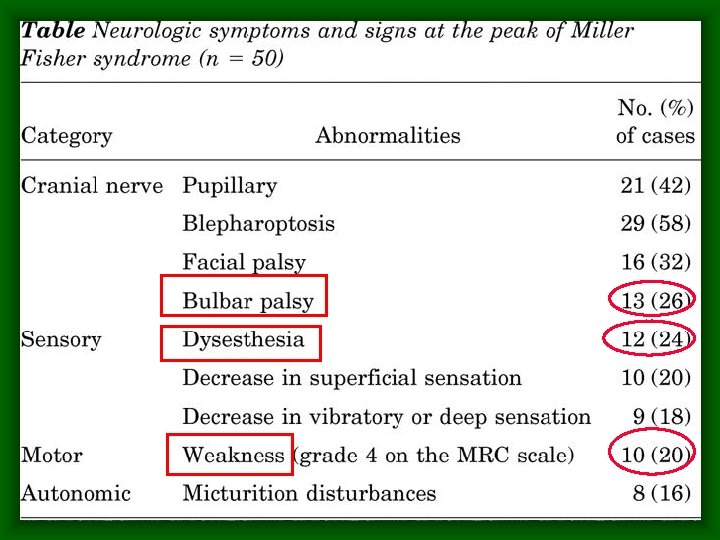
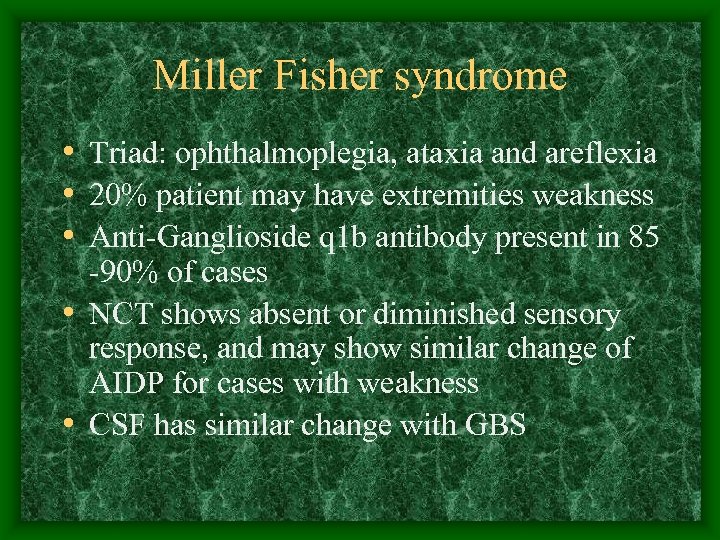 Miller Fisher syndrome • Triad: ophthalmoplegia, ataxia and areflexia • 20% patient may have extremities weakness • Anti-Ganglioside q 1 b antibody present in 85 -90% of cases • NCT shows absent or diminished sensory response, and may show similar change of AIDP for cases with weakness • CSF has similar change with GBS
Miller Fisher syndrome • Triad: ophthalmoplegia, ataxia and areflexia • 20% patient may have extremities weakness • Anti-Ganglioside q 1 b antibody present in 85 -90% of cases • NCT shows absent or diminished sensory response, and may show similar change of AIDP for cases with weakness • CSF has similar change with GBS
 Differential diagnosis for MFS • • Brainstem stroke Myasthenia gravis Wernicke encephalopathy Other neuromusclar junction disease e. g. Eaton-Lambert, botulism • Bickerstaff encephalitis: ophthalmoplegia + ataxia + hyper-reflexia + anti-G Q 1 b +ve
Differential diagnosis for MFS • • Brainstem stroke Myasthenia gravis Wernicke encephalopathy Other neuromusclar junction disease e. g. Eaton-Lambert, botulism • Bickerstaff encephalitis: ophthalmoplegia + ataxia + hyper-reflexia + anti-G Q 1 b +ve
 Treatment of MFS • Supportive care including ventilatory • • support, DVT prophylaxis, pain control Cardiovascualar monitoring and control Cholinesterase inhibitor not useful Immunomodulating therapy: IVIG; plasmapheresis Steroid has not been shown beneficial
Treatment of MFS • Supportive care including ventilatory • • support, DVT prophylaxis, pain control Cardiovascualar monitoring and control Cholinesterase inhibitor not useful Immunomodulating therapy: IVIG; plasmapheresis Steroid has not been shown beneficial
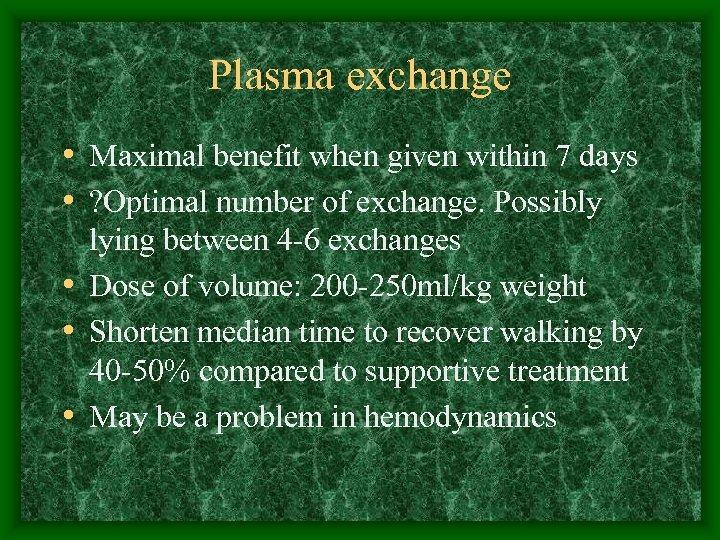 Plasma exchange • Maximal benefit when given within 7 days • ? Optimal number of exchange. Possibly lying between 4 -6 exchanges • Dose of volume: 200 -250 ml/kg weight • Shorten median time to recover walking by 40 -50% compared to supportive treatment • May be a problem in hemodynamics
Plasma exchange • Maximal benefit when given within 7 days • ? Optimal number of exchange. Possibly lying between 4 -6 exchanges • Dose of volume: 200 -250 ml/kg weight • Shorten median time to recover walking by 40 -50% compared to supportive treatment • May be a problem in hemodynamics
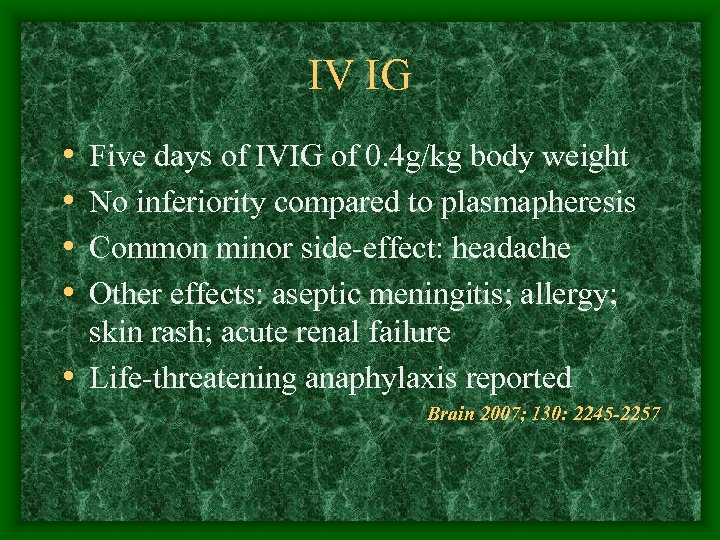 IV IG • • Five days of IVIG of 0. 4 g/kg body weight No inferiority compared to plasmapheresis Common minor side-effect: headache Other effects: aseptic meningitis; allergy; skin rash; acute renal failure • Life-threatening anaphylaxis reported Brain 2007; 130: 2245 -2257
IV IG • • Five days of IVIG of 0. 4 g/kg body weight No inferiority compared to plasmapheresis Common minor side-effect: headache Other effects: aseptic meningitis; allergy; skin rash; acute renal failure • Life-threatening anaphylaxis reported Brain 2007; 130: 2245 -2257
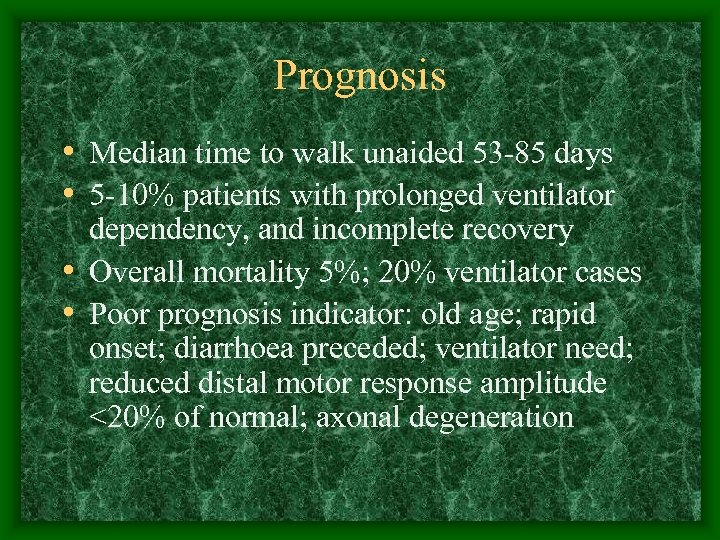 Prognosis • Median time to walk unaided 53 -85 days • 5 -10% patients with prolonged ventilator dependency, and incomplete recovery • Overall mortality 5%; 20% ventilator cases • Poor prognosis indicator: old age; rapid onset; diarrhoea preceded; ventilator need; reduced distal motor response amplitude <20% of normal; axonal degeneration
Prognosis • Median time to walk unaided 53 -85 days • 5 -10% patients with prolonged ventilator dependency, and incomplete recovery • Overall mortality 5%; 20% ventilator cases • Poor prognosis indicator: old age; rapid onset; diarrhoea preceded; ventilator need; reduced distal motor response amplitude <20% of normal; axonal degeneration
 In summary, our patient • Past history of ocular MG • Symptom and sign suggest MFS • MRI shows bystander vascular malformation • • around spinal cord NCT showed axonal degeneration Improved rapidly Presence of anti-gangliose Q 1 b antibody Anti-Ach. R antibodies signify underlying MG
In summary, our patient • Past history of ocular MG • Symptom and sign suggest MFS • MRI shows bystander vascular malformation • • around spinal cord NCT showed axonal degeneration Improved rapidly Presence of anti-gangliose Q 1 b antibody Anti-Ach. R antibodies signify underlying MG
 Wish you happy lunar new year
Wish you happy lunar new year


