6c4a8e97e49dae87868cbd546d2bb8f3.ppt
- Количество слайдов: 16

Introducing telecare. Global challenges, local strategies Computer-Based Technology and Caregiving for Older Adults Moving from Ideas to Implementation: A Caregiver’s Perspective 2 -3 October 2003 NIH Campus / Natcher Conference Center Bethesda, Maryland James Barlow Innovation Studies Centre

Changing demands on care provision § Demographic and social change, especially ageing in most industrialised countries § Rising cost of care delivery § Demand for better quality services and improved access § Care staffing shortages in some countries
Moves towards ICT enabled care § Governments are turning to ICT to help address emerging care needs § Technology innovation: sensors, information processing, telecoms costs/availability, better interfaces § Care service providers and technology / infrastructure suppliers can see new market opportunities
Telecare v. telemedicine § ICT enabled care delivery: – Telecare is essentially a ‘B 2 C’ service: between the patient / client and the care system – Telemedicine is essentially a ‘B 2 B’ service: between health professionals § Long experience of telemedicine in developed countries (and many developing ones) but telecare is new and complex to implement
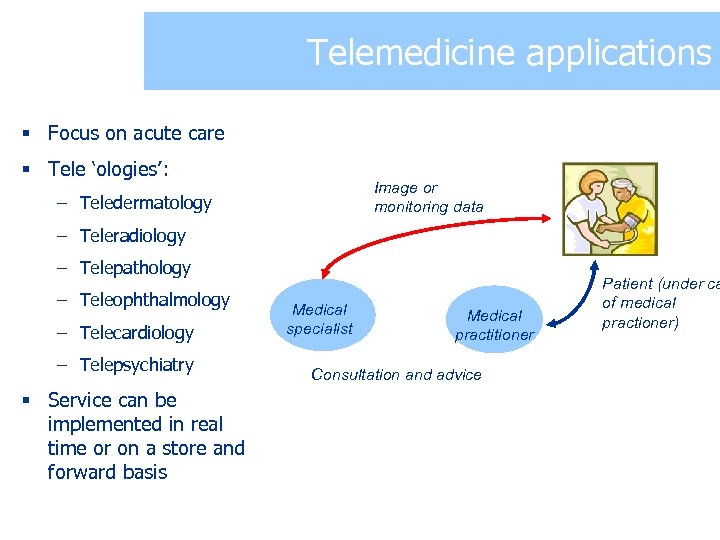
Telemedicine applications § Focus on acute care § Tele ‘ologies’: Image or monitoring data – Teledermatology – Teleradiology – Telepathology – Teleophthalmology – Telecardiology – Telepsychiatry § Service can be implemented in real time or on a store and forward basis Medical specialist Medical practitioner Consultation and advice Patient (under ca of medical practioner)
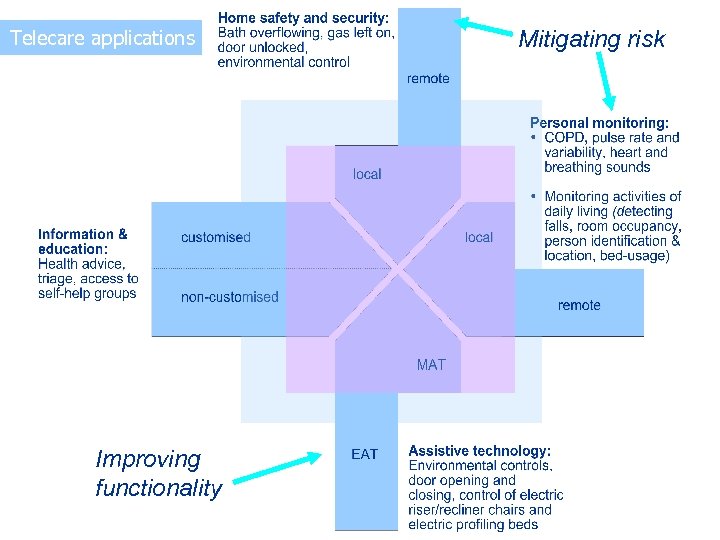
Telecare applications Improving functionality Mitigating risk
‘Thanks to the smarter home, a home help is required only once a year, to adjust the clock’
Broad demand categories for telecare § Focus so far has been on older people: – Those who are becoming generally more dependent – Those with chronic illness – The ‘recovering well’, i. e. those moving from hospital to home § Demand may also emerge from the ‘informed individual’, i. e. those concerned with maintaining a healthy lifestyle or caring for minor conditions themselves
Implementing telecare – the experience so far § Different approaches: – single condition disease management, e. g. SHL Tele. Medicine (Israel): 24 -hour ECG monitoring and feedback to patients, 50, 000 subscribers – focus on local problems, e. g. Sweden and Norway remote consultation / monitoring initiatives tackling care needs in sparsely populated areas – UK model: use existing community alarm system to move from 1 st generation systems (no embedded intelligence) to 2 nd generation systems (more intelligence and automatic response) § However, despite many pilots few become mainstream and few build on past lessons
Typical problems § Australia’s experience is replicated elsewhere: – arrangements for financing and delivery of health care – focus on healthcare delivery within the hospital setting rather than community – the hospital based training and working practices and preferences of clinicians to deliver health care in a personal rather than a remote manner – lack of understanding of the role of ICT in care processes
Key influences on implementation § Structural and operational complexity: generally much higher for telecare than telemedicine § Large number of stakeholders and generally incomplete understanding of care processes § Need to accommodate differing perceptions of risk and different value systems in different parts of the care system § Distribution of costs and benefits within the system § Policy tension between modernisation (telecare) and evidence-based innovation (RCT as the ‘gold standard’)

Developing countries: basic problems § $2000 bn spent globally each year on healthcare but: – $170 bn in developing countries (per capita expenditure is 1/30 of developed countries) – acute shortage of doctors, particularly specialists: Sub-Saharan Africa has fewer than 10 doctors per 100, 000 people, 14 countries do not have a single radiologist § Basic challenge is to ensure effective coverage / effectiveness of existing resources
Telemedicine or telecare? § Different demands on care system in most developing countries: – Disease prevention and treatment is the priority – Ageing population less of an issue – Different family structures: extended families provide support – But there is a role for telemedicine: specialists and services are concentrated in cities; workers in rural health care isolated from support and up to date information – ITU has 50+ projects in developing countries, WHO assessing impact

Developing countries and telemedicine: potential problems? § Quality of telecoms infrastructure § Capital expenditure decisions fail to consider resource implications – hidden technology acquisition & deployment costs, need to manage assets across lifecycle § Bad experiences in medical technology – dumping of poor equipment § Need to develop associated training, management programmes § Scaling up § Cross border payment and legal issues
Conclusions 1 § There is considerable potential to use ICT to help meet elderly care needs in developed countries, but there are big differences in needs between developed and developing countries: – Developing countries need to solve basic healthcare provision before introducing hi-tech solutions (although telemedicine has a role) – Developed countries’ needs revolve around improved service delivery in a context of rapid demographic and economic change
Conclusions 2 § Evidence from existing telecare / telemedicine projects points to importance of understanding the local context, as well as generic lessons: – future evolution of care delivery must start from existing situation and recognition of what telecare / telemedicine can achieve – the purpose and fit of telecare / telemedicine in the wider care system should drive its introduction – not the technology – this will require a better understanding of telecare / telemedicine’s impact at the system-wide level and new approaches to evaluation
6c4a8e97e49dae87868cbd546d2bb8f3.ppt