lection3-neonatology.ppt
- Количество слайдов: 95
 INTRAUTERINE AND PERINATAL INFECTIONS
INTRAUTERINE AND PERINATAL INFECTIONS
 INFECTIONS OF NEONATAL INFANT 2% of fetus infected in utero 10% infected in first month of life
INFECTIONS OF NEONATAL INFANT 2% of fetus infected in utero 10% infected in first month of life
 A variety of maternal infections may be transmitted to the fetus during pregnancy Viral infections. Cytomegalovirus, herpes simplex, hepatitis, coxsackie, rubella, mumps Protozoal infection. Toxoplasma gondii and malaria, Spirochetal infection. Treponema pallidum. Bacterial infections. Listeria monocytogenes, group B streptococci, E. coli. Candidosis. Candida albicans, tropicalis, cruzei.
A variety of maternal infections may be transmitted to the fetus during pregnancy Viral infections. Cytomegalovirus, herpes simplex, hepatitis, coxsackie, rubella, mumps Protozoal infection. Toxoplasma gondii and malaria, Spirochetal infection. Treponema pallidum. Bacterial infections. Listeria monocytogenes, group B streptococci, E. coli. Candidosis. Candida albicans, tropicalis, cruzei.
 EPIDEMIOLOGY Transplacental hematogenous spread Vertical transmission of infection Exposed to infectious diseases in the nursery or in the community
EPIDEMIOLOGY Transplacental hematogenous spread Vertical transmission of infection Exposed to infectious diseases in the nursery or in the community
 Mode of infection of the fetus Hematogenous through the placenta. Direct infection of the placenta. Ascending infection from the vagina resulting in amnionitis. During passage through the birth canal.
Mode of infection of the fetus Hematogenous through the placenta. Direct infection of the placenta. Ascending infection from the vagina resulting in amnionitis. During passage through the birth canal.
 The fetus responds to infection There is low immunoglobulin production Poor macrophage mobilization. The immature fetal blood brain barrier offers little protection against organisms (and therefore, the central nervous system is often involved in intrauterine infections)
The fetus responds to infection There is low immunoglobulin production Poor macrophage mobilization. The immature fetal blood brain barrier offers little protection against organisms (and therefore, the central nervous system is often involved in intrauterine infections)
 The fetus responds to infection The first trimester is a phase of active differentiation of the organs of embryogenesis. Many viral infections during the first trimester of pregnancy are teratogenic (lead to birth of malformed babies).
The fetus responds to infection The first trimester is a phase of active differentiation of the organs of embryogenesis. Many viral infections during the first trimester of pregnancy are teratogenic (lead to birth of malformed babies).
 The fetus responds to infection The infection of the fetus from the mother during the latter part of pregnancy does not cause birth defects but may retard the intrauterine development.
The fetus responds to infection The infection of the fetus from the mother during the latter part of pregnancy does not cause birth defects but may retard the intrauterine development.
 Presenting Sings and Symptoms of Infections in Newborn Infants General Fever, temperature, instability Poor feeding Edema Perinatal asphyxia Congenital malformations
Presenting Sings and Symptoms of Infections in Newborn Infants General Fever, temperature, instability Poor feeding Edema Perinatal asphyxia Congenital malformations
 Presenting Sings and Symptoms of Infections in Newborn Infants Cardiovascular System Pallor, mottling, cold, clammy skin Tachycardia Hypotension Bradycardia
Presenting Sings and Symptoms of Infections in Newborn Infants Cardiovascular System Pallor, mottling, cold, clammy skin Tachycardia Hypotension Bradycardia
 Presenting Sings and Symptoms of Infections in Newborn Infants Central Nervous System Irritability, lethargy, tremors Hyporeflexia, hypotonia Abnormal Moro reflex Irregular respirations Full fontanel High-pitched cry
Presenting Sings and Symptoms of Infections in Newborn Infants Central Nervous System Irritability, lethargy, tremors Hyporeflexia, hypotonia Abnormal Moro reflex Irregular respirations Full fontanel High-pitched cry
 Presenting Sings and Symptoms of Infections in Newborn Infants Gastrointestinal System - Abdominal distention, vomiting, diarrhea, hepatomegaly Respiratory System Apnea, dyspnea, tachypnea, retraction flaring, grunting, cyanosis
Presenting Sings and Symptoms of Infections in Newborn Infants Gastrointestinal System - Abdominal distention, vomiting, diarrhea, hepatomegaly Respiratory System Apnea, dyspnea, tachypnea, retraction flaring, grunting, cyanosis
 Presenting Sings and Symptoms of Infections in Newborn Infants Hematologic System Jaundice, Splenomegaly, Petechiae purpura, Bleeding, Anemia Renal System Oliguria
Presenting Sings and Symptoms of Infections in Newborn Infants Hematologic System Jaundice, Splenomegaly, Petechiae purpura, Bleeding, Anemia Renal System Oliguria
 ETIOLOGY Transplacentally transmitted – Syphilis, Borrelia burgdorferi, Rubella, CMV, Parvovirus B 19, HIV, Varicellazoster, Listeria mocytogenes, Toxoplasmosis, Tuberculosis, HBV, HSV
ETIOLOGY Transplacentally transmitted – Syphilis, Borrelia burgdorferi, Rubella, CMV, Parvovirus B 19, HIV, Varicellazoster, Listeria mocytogenes, Toxoplasmosis, Tuberculosis, HBV, HSV
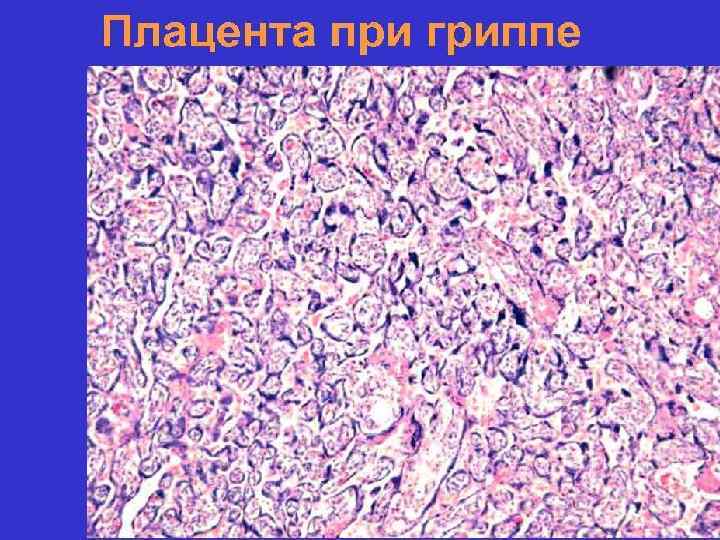
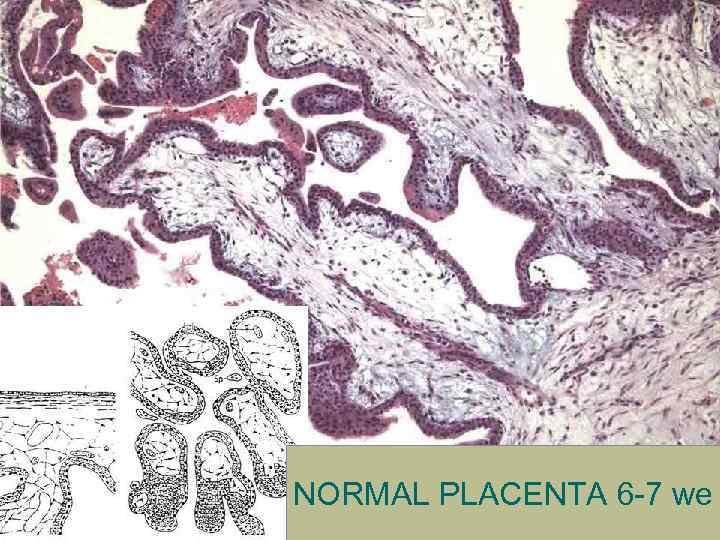 NORMAL PLACENTA 6 -7 we
NORMAL PLACENTA 6 -7 we



 ETIOLOGY Intrapartum & Postpartum infections – Enteric organisms, Gonococci, Chlamydia, Enteroviruses, Streptococcus pneumoniae, HSV
ETIOLOGY Intrapartum & Postpartum infections – Enteric organisms, Gonococci, Chlamydia, Enteroviruses, Streptococcus pneumoniae, HSV
 ETIOLOGY Nosocomial infections Klebsiella pneumoniae, E. Coli, Salmonella, Citrobacter , S. aureus, Campilobacter, Pseudomonas, aeruginosa, Serratia, Candida, Adenoviruses, influenza CMV, HAV, HSV , Rotaviruses, Rhinoviruses
ETIOLOGY Nosocomial infections Klebsiella pneumoniae, E. Coli, Salmonella, Citrobacter , S. aureus, Campilobacter, Pseudomonas, aeruginosa, Serratia, Candida, Adenoviruses, influenza CMV, HAV, HSV , Rotaviruses, Rhinoviruses
 Nosocomial infections а
Nosocomial infections а








 TORCH-syndrome (A. Namias. 1971) Infection T-toxoplasmosis O-Other diseases R-Rubella C-Cytomegalovirus H-Herpes simplex virus Symptoms Intrauterine growth retardation Hepatomegaly Jaundice Purpura Cardiovascular disorders Neurological disorders
TORCH-syndrome (A. Namias. 1971) Infection T-toxoplasmosis O-Other diseases R-Rubella C-Cytomegalovirus H-Herpes simplex virus Symptoms Intrauterine growth retardation Hepatomegaly Jaundice Purpura Cardiovascular disorders Neurological disorders

 Nosocomial infections
Nosocomial infections
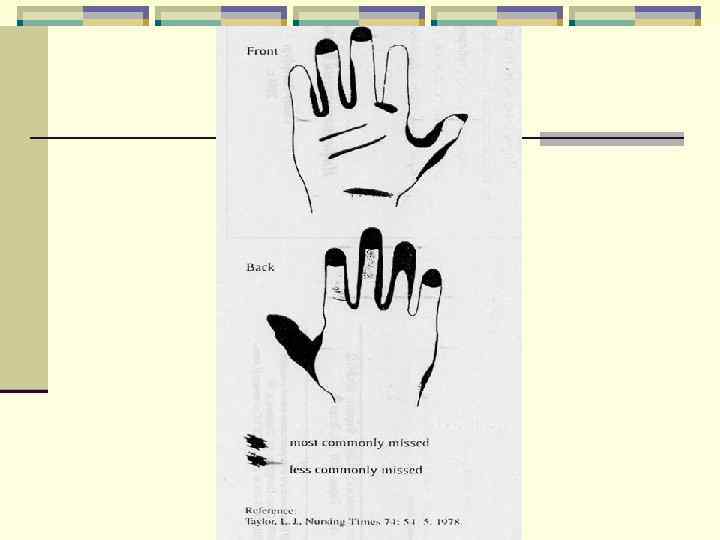
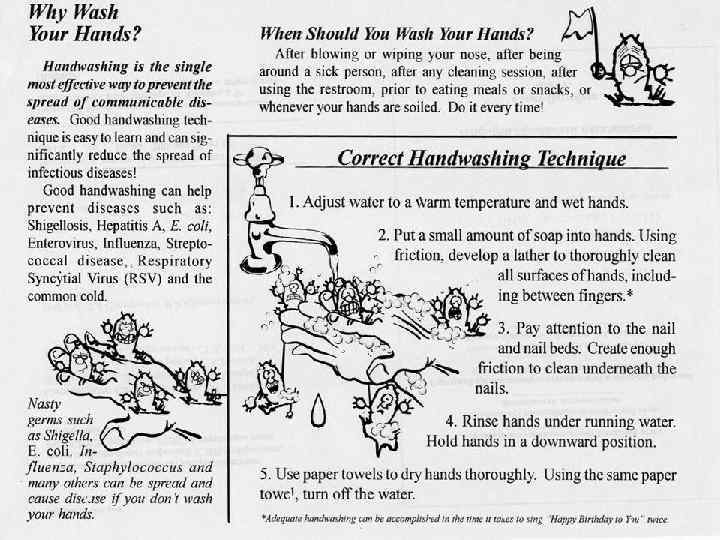
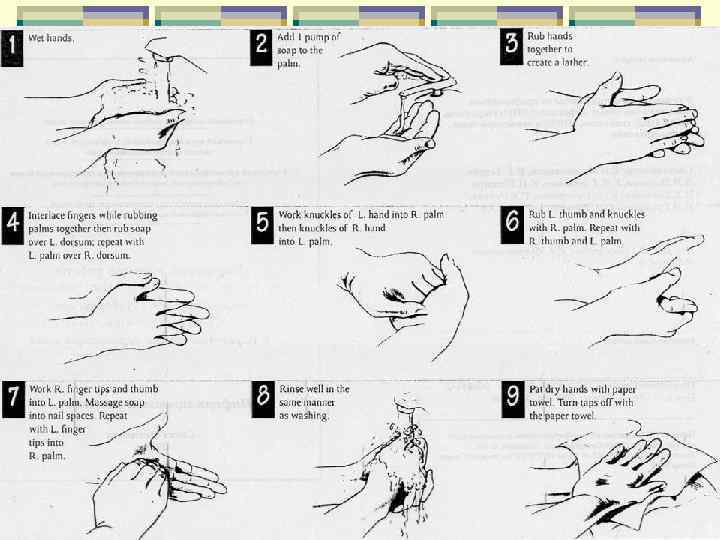

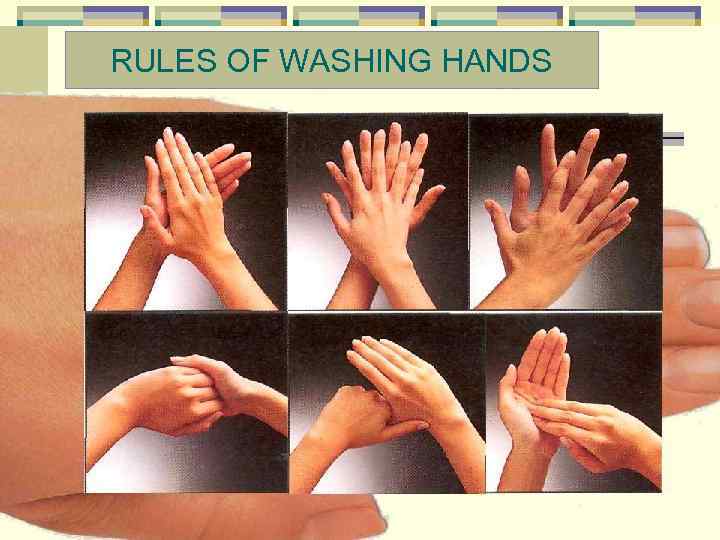 RULES OF WASHING HANDS
RULES OF WASHING HANDS
 PERINATAL FACTORS PREDISPOSING TO INFECTION Abortions, stillbirth, congenital malformation as a result of previous pregnancies Maternal genital tract infections Maternal somatic diseases (diabetes mellitus, urinary tract infections, myocarditis) Maternal chorioamnionitis
PERINATAL FACTORS PREDISPOSING TO INFECTION Abortions, stillbirth, congenital malformation as a result of previous pregnancies Maternal genital tract infections Maternal somatic diseases (diabetes mellitus, urinary tract infections, myocarditis) Maternal chorioamnionitis
 PERINATAL FACTORS PREDISPOSING TO INFECTION Acute infectious diseases during pregnancy Premature discharge of amniotic fluid Prematurity or low birth weight Frequent use of invasive procedures in newborns
PERINATAL FACTORS PREDISPOSING TO INFECTION Acute infectious diseases during pregnancy Premature discharge of amniotic fluid Prematurity or low birth weight Frequent use of invasive procedures in newborns
 LABORATORY FINDINGS Invasive methods : amniocentesis – bacteriological test of amniotic fluid, cordocentesis – bacteriological & serological tests of navel (umdilical) blood.
LABORATORY FINDINGS Invasive methods : amniocentesis – bacteriological test of amniotic fluid, cordocentesis – bacteriological & serological tests of navel (umdilical) blood.
 LABORATORY FINDINGS Indirect methods : Bacteriological tests of excreta from woman’s urogenital tract & another biological fluids Serological tests – indirect fluorescent antibody test (IFA), neonatal Ig. M, Ig. G antibodies titers.
LABORATORY FINDINGS Indirect methods : Bacteriological tests of excreta from woman’s urogenital tract & another biological fluids Serological tests – indirect fluorescent antibody test (IFA), neonatal Ig. M, Ig. G antibodies titers.
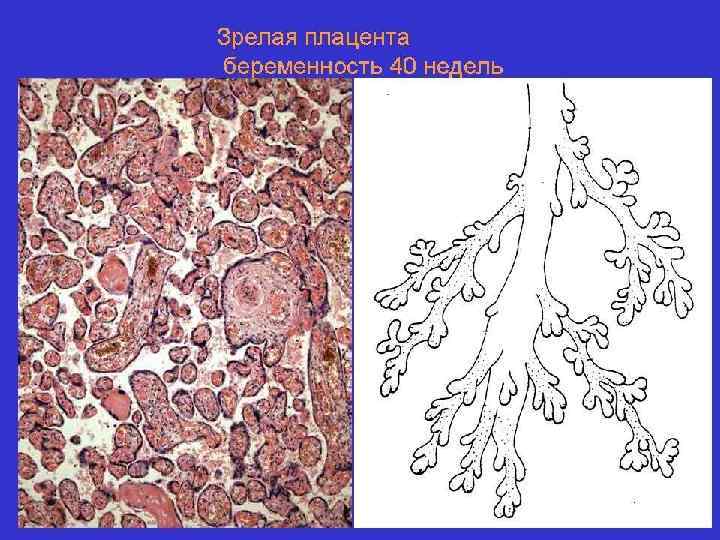
 LABORATORY FINDINGS Indirect methods : Fetus USG – growth retardation, polyhydramnios, ultrasound features of placental disorders. Placental histological examination.
LABORATORY FINDINGS Indirect methods : Fetus USG – growth retardation, polyhydramnios, ultrasound features of placental disorders. Placental histological examination.
 CONGENITAL RUBELLA INFECTION The risk of fetal infection is 50% or higher if the mother acquires infection during the first four weeks of gestation. It declines to about 25% between 23 -26 weeks and then rises again to 70% or more in maternal rubella infection during the latter part of gestation. Most fatal illness is manifested in the first 8 -10 weeks of gestation.
CONGENITAL RUBELLA INFECTION The risk of fetal infection is 50% or higher if the mother acquires infection during the first four weeks of gestation. It declines to about 25% between 23 -26 weeks and then rises again to 70% or more in maternal rubella infection during the latter part of gestation. Most fatal illness is manifested in the first 8 -10 weeks of gestation.

 CONGENITAL RUBELLA INFECTION Clinical manifestations 1. Intrauterine hazards. Abortions. Congenital defects, 2. Late sequelae, 3. Active infection at birth
CONGENITAL RUBELLA INFECTION Clinical manifestations 1. Intrauterine hazards. Abortions. Congenital defects, 2. Late sequelae, 3. Active infection at birth
 CONGENITAL RUBELLA INFECTION Congenital defects, sensorineural hearing defects, cardiovascular malformations respiratory disorders hemopoietic abnormalities skeletal defects ocular disorders (cataract, glaucoma, microphthalmia)
CONGENITAL RUBELLA INFECTION Congenital defects, sensorineural hearing defects, cardiovascular malformations respiratory disorders hemopoietic abnormalities skeletal defects ocular disorders (cataract, glaucoma, microphthalmia)

 CONGENITAL RUBELLA INFECTION Congenital defects, genitourinary diseases (polycystic kidneys) esophageal, jejunal atresia central nervous system problems of microcephaly and mental retardation intrauterine growth retardation
CONGENITAL RUBELLA INFECTION Congenital defects, genitourinary diseases (polycystic kidneys) esophageal, jejunal atresia central nervous system problems of microcephaly and mental retardation intrauterine growth retardation
 CONGENITAL RUBELLA INFECTION Late sequelae, diabetes, thyroid dysfunction, progressive rubella encephalitis, psychomotor defects, dental abnormalities, language disorders.
CONGENITAL RUBELLA INFECTION Late sequelae, diabetes, thyroid dysfunction, progressive rubella encephalitis, psychomotor defects, dental abnormalities, language disorders.
 CONGENITAL RUBELLA INFECTION Active infection at birth • • hemolytic anemia, thrombocytopenic purpura, hepatitis, encephalitis, petechial blue-berry muffin lesions myocarditis pneumonitis, seizures.
CONGENITAL RUBELLA INFECTION Active infection at birth • • hemolytic anemia, thrombocytopenic purpura, hepatitis, encephalitis, petechial blue-berry muffin lesions myocarditis pneumonitis, seizures.
 CONGENITAL RUBELLA INFECTION Active infection at birth Baby may shed virus up to the age of 18 months. The prognosis is generally poor.
CONGENITAL RUBELLA INFECTION Active infection at birth Baby may shed virus up to the age of 18 months. The prognosis is generally poor.
 CONGENITAL RUBELLA INFECTION Prevention No effective therapeutic modality for the treatment of either postnatal or congenital rubella is currently available. The disease can be effectively prevented through immunization of all boys and girls before puberty. After puberty, immunization should be advised only after estimation of Hemagglutination Inhibition (HI) antibody.
CONGENITAL RUBELLA INFECTION Prevention No effective therapeutic modality for the treatment of either postnatal or congenital rubella is currently available. The disease can be effectively prevented through immunization of all boys and girls before puberty. After puberty, immunization should be advised only after estimation of Hemagglutination Inhibition (HI) antibody.
 CONGENITAL RUBELLA INFECTION If a pregnant mother is suspected to be exposed to possible rubella during early pregnancy less than 16 weeks of gestation, HI antibody titer in the blood should be obtained immediately and after three to six weeks' interval, irrespective of the occurrence of any rash.
CONGENITAL RUBELLA INFECTION If a pregnant mother is suspected to be exposed to possible rubella during early pregnancy less than 16 weeks of gestation, HI antibody titer in the blood should be obtained immediately and after three to six weeks' interval, irrespective of the occurrence of any rash.
 CONGENITAL RUBELLA INFECTION A fourfold or greater increase in HI antibody titer indicates rubella infection. If the infection is confirmed, medical termination of pregnancy should be advised.
CONGENITAL RUBELLA INFECTION A fourfold or greater increase in HI antibody titer indicates rubella infection. If the infection is confirmed, medical termination of pregnancy should be advised.
 CYTOMEGALIC INCLUSION VIRUS DISEASE The infection is transmitted through oropharyngeal secretions, urine, cervical and vaginal secretions, spermatic fluid, breast milk and blood. Cytomegalovirus is transmitted mostly from primary or rarely from recurrent maternal infection.
CYTOMEGALIC INCLUSION VIRUS DISEASE The infection is transmitted through oropharyngeal secretions, urine, cervical and vaginal secretions, spermatic fluid, breast milk and blood. Cytomegalovirus is transmitted mostly from primary or rarely from recurrent maternal infection.

 CYTOMEGALIC INCLUSION VIRUS DISEASE Neonatal cytomegalic inclusion disease becomes symptomatic in about ten percent of infected babies following primary maternal infection.
CYTOMEGALIC INCLUSION VIRUS DISEASE Neonatal cytomegalic inclusion disease becomes symptomatic in about ten percent of infected babies following primary maternal infection.
 CYTOMEGALIC INCLUSION VIRUS DISEASE There may be a fatal infection of fetus involving viscera; a baby may be born with residual neurological damage; there is a mild disease with only serological and virological evidence of disease.
CYTOMEGALIC INCLUSION VIRUS DISEASE There may be a fatal infection of fetus involving viscera; a baby may be born with residual neurological damage; there is a mild disease with only serological and virological evidence of disease.
 CYTOMEGALIC INCLUSION VIRUS DISEASE Clinical manifestation anemia, thrombocytopenic purpura; hepatosplenomegaly, neonatal hepatitis, jaundice; respiratory distress due to pneumonia; petechial rash.
CYTOMEGALIC INCLUSION VIRUS DISEASE Clinical manifestation anemia, thrombocytopenic purpura; hepatosplenomegaly, neonatal hepatitis, jaundice; respiratory distress due to pneumonia; petechial rash.
 CYTOMEGALIC INCLUSION VIRUS DISEASE Clinical manifestation meningoencephalitis, microcephaly, intracerebral calcification (usually periventricular) and chorioretinitis;
CYTOMEGALIC INCLUSION VIRUS DISEASE Clinical manifestation meningoencephalitis, microcephaly, intracerebral calcification (usually periventricular) and chorioretinitis;
 CYTOMEGALIC INCLUSION VIRUS DISEASE Late sequelae mental retardation, deafness, convulsions, paralysis, spasticity and motor disability.
CYTOMEGALIC INCLUSION VIRUS DISEASE Late sequelae mental retardation, deafness, convulsions, paralysis, spasticity and motor disability.
 CYTOMEGALIC INCLUSION VIRUS DISEASE Diagnosis Laboratory investigations show: raised cord serum Ig. M, atypical lymphocytosis and thrombocytopenia. isolation of CMV from white blood cells, urine and throat, conjunctival and rectal swabs.
CYTOMEGALIC INCLUSION VIRUS DISEASE Diagnosis Laboratory investigations show: raised cord serum Ig. M, atypical lymphocytosis and thrombocytopenia. isolation of CMV from white blood cells, urine and throat, conjunctival and rectal swabs.
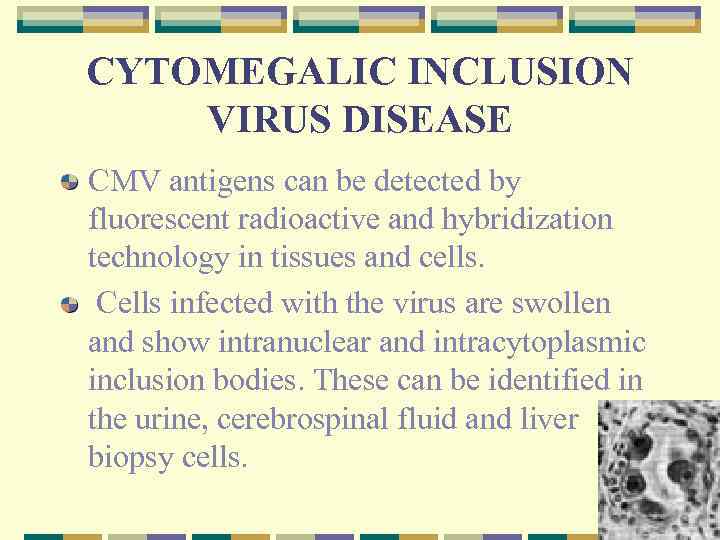 CYTOMEGALIC INCLUSION VIRUS DISEASE CMV antigens can be detected by fluorescent radioactive and hybridization technology in tissues and cells. Cells infected with the virus are swollen and show intranuclear and intracytoplasmic inclusion bodies. These can be identified in the urine, cerebrospinal fluid and liver biopsy cells.
CYTOMEGALIC INCLUSION VIRUS DISEASE CMV antigens can be detected by fluorescent radioactive and hybridization technology in tissues and cells. Cells infected with the virus are swollen and show intranuclear and intracytoplasmic inclusion bodies. These can be identified in the urine, cerebrospinal fluid and liver biopsy cells.
 CYTOMEGALIC INCLUSION VIRUS DISEASE Prognosis The prognosis is poor and death rate is high. The babies born in subsequent pregnancies are generally not affected.
CYTOMEGALIC INCLUSION VIRUS DISEASE Prognosis The prognosis is poor and death rate is high. The babies born in subsequent pregnancies are generally not affected.
 CYTOMEGALIC INCLUSION VIRUS DISEASE Treatment No satisfactory treatment is available. A new antiviral drug gancyclovir appears promising and is currently under investigation.
CYTOMEGALIC INCLUSION VIRUS DISEASE Treatment No satisfactory treatment is available. A new antiviral drug gancyclovir appears promising and is currently under investigation.
 HERPES SIMPLEX virus (HSV) Type I: HSV infection spreads by close personal contacts and primarily infects the oropharynx. Type II: HSV has a predilection for genitalia and is therefore transmitted as a venereal infection
HERPES SIMPLEX virus (HSV) Type I: HSV infection spreads by close personal contacts and primarily infects the oropharynx. Type II: HSV has a predilection for genitalia and is therefore transmitted as a venereal infection

 HERPES SIMPLEX However, neonatal HSV is almost always acquired during vaginal delivery or by ascending infection following early rupture of membranes. The illness usually starts from the fourth to tenth day after birth and simulates septicemia.
HERPES SIMPLEX However, neonatal HSV is almost always acquired during vaginal delivery or by ascending infection following early rupture of membranes. The illness usually starts from the fourth to tenth day after birth and simulates septicemia.
 HERPES SIMPLEX Vesicular skin lesions may appear as the initial sign. The infant develops fever or hypothermia, dyspnea, myocarditis and circulatory collapse. The liver is enlarged due to hepatitis. The baby appears lethargic and may present with vomiting and convulsions.
HERPES SIMPLEX Vesicular skin lesions may appear as the initial sign. The infant develops fever or hypothermia, dyspnea, myocarditis and circulatory collapse. The liver is enlarged due to hepatitis. The baby appears lethargic and may present with vomiting and convulsions.
 HERPES SIMPLEX Either hepatic or central nervous system symptoms may predominate. Hematologic, reticuloendothelial and pulmonary systems may also be involved
HERPES SIMPLEX Either hepatic or central nervous system symptoms may predominate. Hematologic, reticuloendothelial and pulmonary systems may also be involved
 HERPES SIMPLEX Diagnosis CSF shows moderate pleocytosis (50 -200 cells/mm 3) and disproportionate elevation of proteins (500 -1000 mg/d. L). Characteristic cells or histological changes in the scrapings of tissue help in establishing the diagnosis.
HERPES SIMPLEX Diagnosis CSF shows moderate pleocytosis (50 -200 cells/mm 3) and disproportionate elevation of proteins (500 -1000 mg/d. L). Characteristic cells or histological changes in the scrapings of tissue help in establishing the diagnosis.
 HERPES SIMPLEX Diagnosis Herpes simplex virus can be identified from clinical and necropsy material either by culture or by immunofluorescent techniques.
HERPES SIMPLEX Diagnosis Herpes simplex virus can be identified from clinical and necropsy material either by culture or by immunofluorescent techniques.
 HERPES SIMPLEX Acyclovir is the current treatment of neonatal HSV infection. Infants with eye, mouth and skin disease should be administered acyclovir 30 -45 mg per kg per day for 10 -14 days. If the disease involves CVS, the recommended duration of therapy is 21 days.
HERPES SIMPLEX Acyclovir is the current treatment of neonatal HSV infection. Infants with eye, mouth and skin disease should be administered acyclovir 30 -45 mg per kg per day for 10 -14 days. If the disease involves CVS, the recommended duration of therapy is 21 days.
 HERPES SIMPLEX Prognosis The mortality rate is very high. A women with cervical HSV should be delivered by caeserean section to prevent transmission of infection to the baby.
HERPES SIMPLEX Prognosis The mortality rate is very high. A women with cervical HSV should be delivered by caeserean section to prevent transmission of infection to the baby.
 TOXOPLASMOSIS Infection with an intracellular, protozoan parasite called Toxoplasma gondii causes toxoplasmosis. The final host of this peculiar parasite are members of the cat family. The illness is transmitted to the fetus in about 40 percent of cases during acute primary disease of the mother.
TOXOPLASMOSIS Infection with an intracellular, protozoan parasite called Toxoplasma gondii causes toxoplasmosis. The final host of this peculiar parasite are members of the cat family. The illness is transmitted to the fetus in about 40 percent of cases during acute primary disease of the mother.
 TOXOPLASMOSIS The clinical features Cerebroocular lesions are the most common, the diagnosis must be considered even in their absence. Based on the predominant lesions, the disease may be classified as cerebro-ocular visceral cerebral subclinical
TOXOPLASMOSIS The clinical features Cerebroocular lesions are the most common, the diagnosis must be considered even in their absence. Based on the predominant lesions, the disease may be classified as cerebro-ocular visceral cerebral subclinical
 TOXOPLASMOSIS The symptoms and signs may include: Fever, refusal to feed and maculopapular rash, Hepatosplenomegaly and jaundice, Meningoencephalitis, chorioretinitis, convulsions, hydrocephalus or microcephaly and cerebral calcification usually diffuse. Thrombocytopenia and bleeding manifestations, Intrauterine growth retardation.
TOXOPLASMOSIS The symptoms and signs may include: Fever, refusal to feed and maculopapular rash, Hepatosplenomegaly and jaundice, Meningoencephalitis, chorioretinitis, convulsions, hydrocephalus or microcephaly and cerebral calcification usually diffuse. Thrombocytopenia and bleeding manifestations, Intrauterine growth retardation.
 TOXOPLASMOSIS The diagnosis is confirmed by demonstration of the parasite in the cerebrospinal fluid or in the tissues. The indirect fluorescent antibody test (IFA) has recently been used for early diagnosis. Ig. M IFA antibodies are present in the serum of infected neonates.
TOXOPLASMOSIS The diagnosis is confirmed by demonstration of the parasite in the cerebrospinal fluid or in the tissues. The indirect fluorescent antibody test (IFA) has recently been used for early diagnosis. Ig. M IFA antibodies are present in the serum of infected neonates.
 TOXOPLASMOSIS Treatment. Pyrimethamine (1 mg/kg/day) in two divided doses orally for one week and then half the dose for six months to one year plus sulfadiazine or sulfisoxazole (100 mg/ kg/day) are useful in the treatment. Folinic acid should be given along with to prevent hematologic toxicity. Corticosteroids are used if inflammatory lesions are also present
TOXOPLASMOSIS Treatment. Pyrimethamine (1 mg/kg/day) in two divided doses orally for one week and then half the dose for six months to one year plus sulfadiazine or sulfisoxazole (100 mg/ kg/day) are useful in the treatment. Folinic acid should be given along with to prevent hematologic toxicity. Corticosteroids are used if inflammatory lesions are also present
 TOXOPLASMOSIS Prevention. Avoid consumption of raw and under cooked meat products by the pregnant mothers. Avoid handling of the soil potentially contaminated with cat feces. Spiramycin has been used for treatment of maternal infection to prevent fetal toxoplasma infection. Treatment by sulfadiazine and pyrimethamine should be avoided because of their possible teratogenic effects.
TOXOPLASMOSIS Prevention. Avoid consumption of raw and under cooked meat products by the pregnant mothers. Avoid handling of the soil potentially contaminated with cat feces. Spiramycin has been used for treatment of maternal infection to prevent fetal toxoplasma infection. Treatment by sulfadiazine and pyrimethamine should be avoided because of their possible teratogenic effects.
 CONGENITAL SYPHILIS Congenital syphilis results from transplacental transfer of Treponema pallidum from the infected mother to the fetus. Rarely the infection may be contracted during passage through the birth canal.
CONGENITAL SYPHILIS Congenital syphilis results from transplacental transfer of Treponema pallidum from the infected mother to the fetus. Rarely the infection may be contracted during passage through the birth canal.
 CONGENITAL SYPHILIS Early manifestations Mucocutaneous manifestations. A bullous rash, reddish maculopapular rash. Flat, wart like moist condylomata are also seen. Most infants with congenital syphilis present with rhinitis or snuffles. Hepatosplenomegaly is a frequent presenting feature.
CONGENITAL SYPHILIS Early manifestations Mucocutaneous manifestations. A bullous rash, reddish maculopapular rash. Flat, wart like moist condylomata are also seen. Most infants with congenital syphilis present with rhinitis or snuffles. Hepatosplenomegaly is a frequent presenting feature.
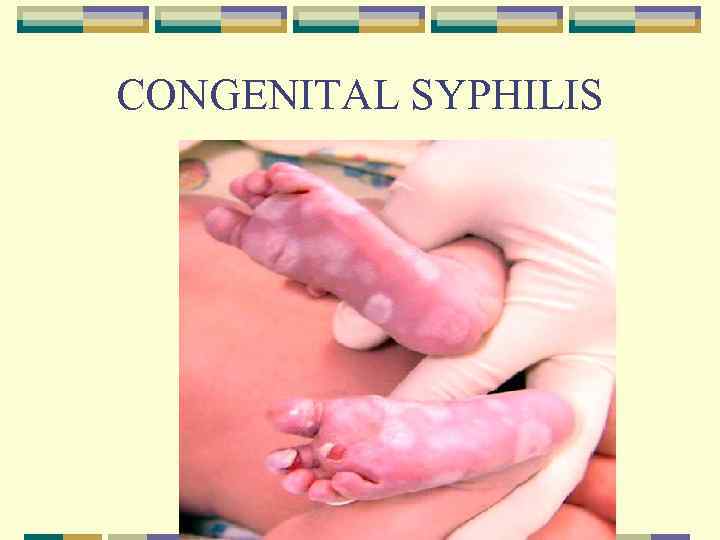 CONGENITAL SYPHILIS
CONGENITAL SYPHILIS
 CONGENITAL SYPHILIS Early manifestations Generalized lymphadenopathy is seen in 50% of patients. Hematologic manifestations - Coomb's negative hemolytic anemia, bleeding diathesis, thrombocytopenia and erythroblastemia. Renal lesions (Nephrosis or nephritis).
CONGENITAL SYPHILIS Early manifestations Generalized lymphadenopathy is seen in 50% of patients. Hematologic manifestations - Coomb's negative hemolytic anemia, bleeding diathesis, thrombocytopenia and erythroblastemia. Renal lesions (Nephrosis or nephritis).
 CONGENITAL SYPHILIS Early manifestations Skeletal lesions - osteochondritis and syphilitic metaphysitis. Upper limbs are more often affected than the lower limbs. The long bones are painful and the infant may be unable to move the limb (pseudoparalysis).
CONGENITAL SYPHILIS Early manifestations Skeletal lesions - osteochondritis and syphilitic metaphysitis. Upper limbs are more often affected than the lower limbs. The long bones are painful and the infant may be unable to move the limb (pseudoparalysis).
 CONGENITAL SYPHILIS Early manifestations Central nervous system - leptomeningitis, hydrocephalus and cranial nerve palsies. Patients may be brought with congenital glaucoma and chorioretinitis. Failure to thrive and intrauterine growth retardation are constant features. The birth weight is low and the infant presents a wizened appearance.
CONGENITAL SYPHILIS Early manifestations Central nervous system - leptomeningitis, hydrocephalus and cranial nerve palsies. Patients may be brought with congenital glaucoma and chorioretinitis. Failure to thrive and intrauterine growth retardation are constant features. The birth weight is low and the infant presents a wizened appearance.
 CONGENITAL SYPHILIS Late manifestations. Stigmata or residua of initial lesions of congenital syphilis (Hutchinson's teeth, frontal bossing, short maxilla, saddle nose, high-arched palate, enlargement of sternoclavicular portion of clavicle, protuberant mandible, radiating perioral scars (rhagades), saber tibia and mulberry molars).
CONGENITAL SYPHILIS Late manifestations. Stigmata or residua of initial lesions of congenital syphilis (Hutchinson's teeth, frontal bossing, short maxilla, saddle nose, high-arched palate, enlargement of sternoclavicular portion of clavicle, protuberant mandible, radiating perioral scars (rhagades), saber tibia and mulberry molars).
 CONGENITAL SYPHILIS Late hypersensitivity reactions. These include interstitial keratitis, nerve deafness and Glutton's joints. The latter manifest around the age of puberty. Painless synovitis of the knee joint is the most common lesion.
CONGENITAL SYPHILIS Late hypersensitivity reactions. These include interstitial keratitis, nerve deafness and Glutton's joints. The latter manifest around the age of puberty. Painless synovitis of the knee joint is the most common lesion.
 CONGENITAL SYPHILIS Diagnosis clinical evaluation, epidemiologic considerations examination of placenta serological tests in the mother and the infants. The most useful test is Fluorescent Treponemal Antibody Absorption (FIA-ABS-lg. M) test. Specific Treponema pallidum Ig. M antibodies isuseful for diagnosis of congenital syphilis.
CONGENITAL SYPHILIS Diagnosis clinical evaluation, epidemiologic considerations examination of placenta serological tests in the mother and the infants. The most useful test is Fluorescent Treponemal Antibody Absorption (FIA-ABS-lg. M) test. Specific Treponema pallidum Ig. M antibodies isuseful for diagnosis of congenital syphilis.
 CONGENITAL SYPHILIS Treatment If the CSF is abnormal, the infant must be treated with 150, 000 units of penicillin per kg of body weight per day in two or three divided doses, given IM or IV for a minimum of 21 days.
CONGENITAL SYPHILIS Treatment If the CSF is abnormal, the infant must be treated with 150, 000 units of penicillin per kg of body weight per day in two or three divided doses, given IM or IV for a minimum of 21 days.
 CONGENITAL SYPHILIS If the cerebrospinal fluid is normal, 100, 000150, 000 units of penicillin/kg/ day is given in divided doses for 10 -14 days. Interstitial keratitis is treated with corticosteroids locally and a mydriatic, agent, e. g. , atropine. The nerve deafness is treated with oral steroids and penicillin.
CONGENITAL SYPHILIS If the cerebrospinal fluid is normal, 100, 000150, 000 units of penicillin/kg/ day is given in divided doses for 10 -14 days. Interstitial keratitis is treated with corticosteroids locally and a mydriatic, agent, e. g. , atropine. The nerve deafness is treated with oral steroids and penicillin.
 CONGENITAL SYPHILIS Follow-up. These children should be kept under surveillance for a year. Serological tests for syphilis are repeated 46 weeks after therapy and the cerebrospinal fluid is reviewed.
CONGENITAL SYPHILIS Follow-up. These children should be kept under surveillance for a year. Serological tests for syphilis are repeated 46 weeks after therapy and the cerebrospinal fluid is reviewed.
 THANK YOU FOR YOUR ATTENTION
THANK YOU FOR YOUR ATTENTION


