e4ea634f539fc1083a57dab3326a2c15.ppt
- Количество слайдов: 11
Intestinal Behçet Disease From the Literature to the Clinic Doreen Benary December 10 th, 2009 Doreen Benary 3 rd year Medical Student NY-State American Program Tel Aviv University
What is Behçet Disease? Behçet disease is a chronic, relapsing inflammatory disorder of unknown etiology with multi-system involvement due to a vasculitis of large and small vessels. It’s marked by eye inflammation, oral and genital ulcers, and skin lesions, as well as a varying multisystem involvement including joints, blood vessels, CNS and the GI tract. The etiology is unknown, but like other inflammatory diseases, it is thought result from a combination of autoimmune, genetic and infectious causes
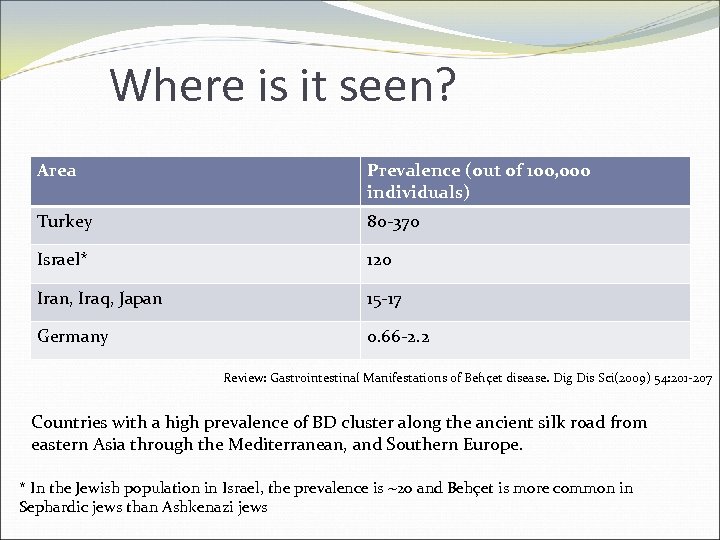
Where is it seen? Area Prevalence (out of 100, 000 individuals) Turkey 80 -370 Israel* 120 Iran, Iraq, Japan 15 -17 Germany 0. 66 -2. 2 Review: Gastrointestinal Manifestations of Behçet disease. Dig Dis Sci(2009) 54: 201 -207 Countries with a high prevalence of BD cluster along the ancient silk road from eastern Asia through the Mediterranean, and Southern Europe. * In the Jewish population in Israel, the prevalence is ~20 and Behçet is more common in Sephardic jews than Ashkenazi jews
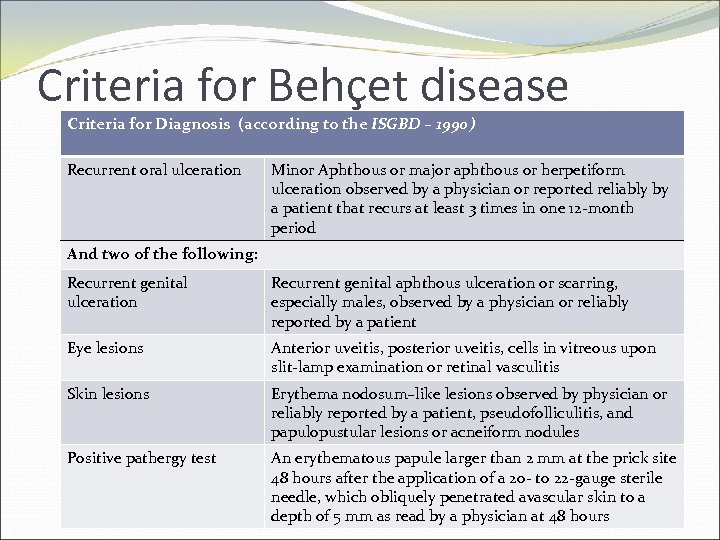
Criteria for Behçet disease Criteria for Diagnosis (according to the ISGBD – 1990) Recurrent oral ulceration Minor Aphthous or major aphthous or herpetiform ulceration observed by a physician or reported reliably by a patient that recurs at least 3 times in one 12 -month period And two of the following: Recurrent genital ulceration Recurrent genital aphthous ulceration or scarring, especially males, observed by a physician or reliably reported by a patient Eye lesions Anterior uveitis, posterior uveitis, cells in vitreous upon slit-lamp examination or retinal vasculitis Skin lesions Erythema nodosum–like lesions observed by physician or reliably reported by a patient, pseudofolliculitis, and papulopustular lesions or acneiform nodules Positive pathergy test An erythematous papule larger than 2 mm at the prick site 48 hours after the application of a 20 - to 22 -gauge sterile needle, which obliquely penetrated avascular skin to a depth of 5 mm as read by a physician at 48 hours
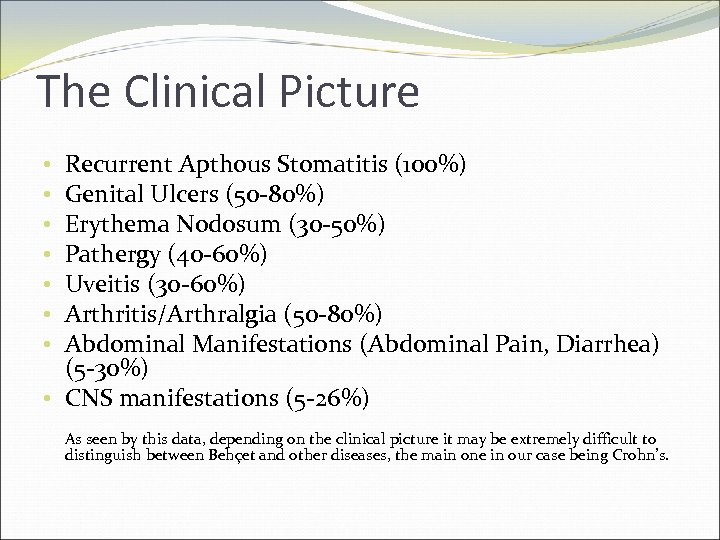
The Clinical Picture Recurrent Apthous Stomatitis (100%) Genital Ulcers (50 -80%) Erythema Nodosum (30 -50%) Pathergy (40 -60%) Uveitis (30 -60%) Arthritis/Arthralgia (50 -80%) Abdominal Manifestations (Abdominal Pain, Diarrhea) (5 -30%) • CNS manifestations (5 -26%) • • As seen by this data, depending on the clinical picture it may be extremely difficult to distinguish between Behçet and other diseases, the main one in our case being Crohn’s.
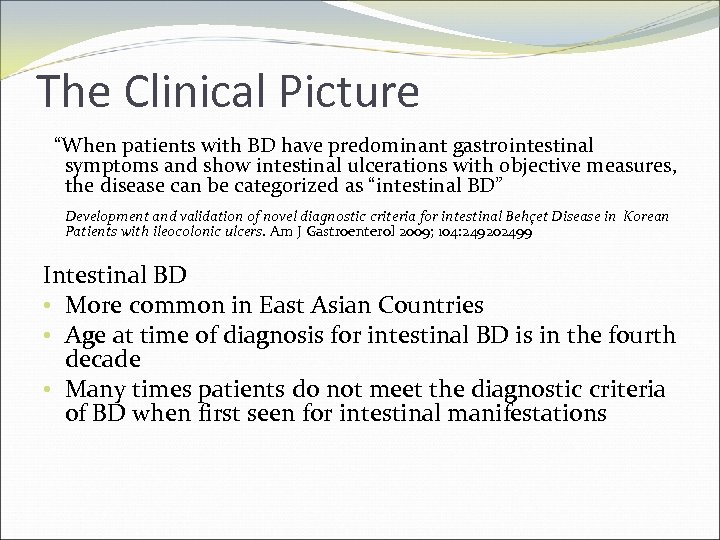
The Clinical Picture “When patients with BD have predominant gastrointestinal symptoms and show intestinal ulcerations with objective measures, the disease can be categorized as “intestinal BD” Development and validation of novel diagnostic criteria for intestinal Behçet Disease in Korean Patients with ileocolonic ulcers. Am J Gastroenterol 2009; 104: 249202499 Intestinal BD • More common in East Asian Countries • Age at time of diagnosis for intestinal BD is in the fourth decade • Many times patients do not meet the diagnostic criteria of BD when first seen for intestinal manifestations
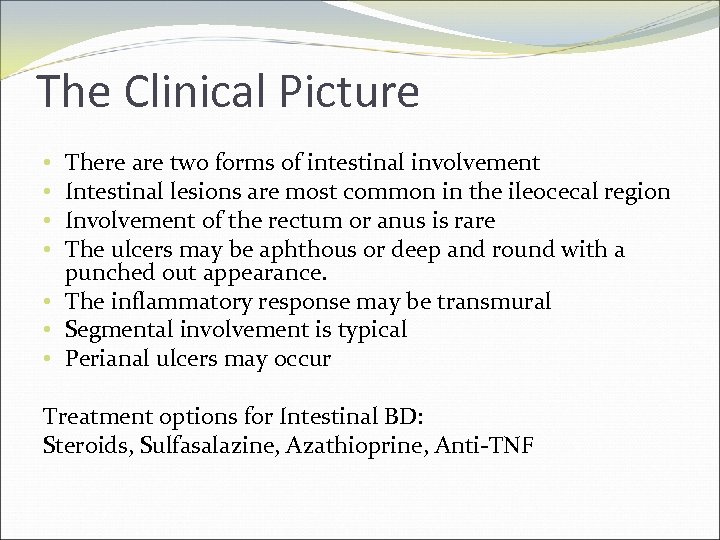
The Clinical Picture There are two forms of intestinal involvement Intestinal lesions are most common in the ileocecal region Involvement of the rectum or anus is rare The ulcers may be aphthous or deep and round with a punched out appearance. • The inflammatory response may be transmural • Segmental involvement is typical • Perianal ulcers may occur • • Treatment options for Intestinal BD: Steroids, Sulfasalazine, Azathioprine, Anti-TNF
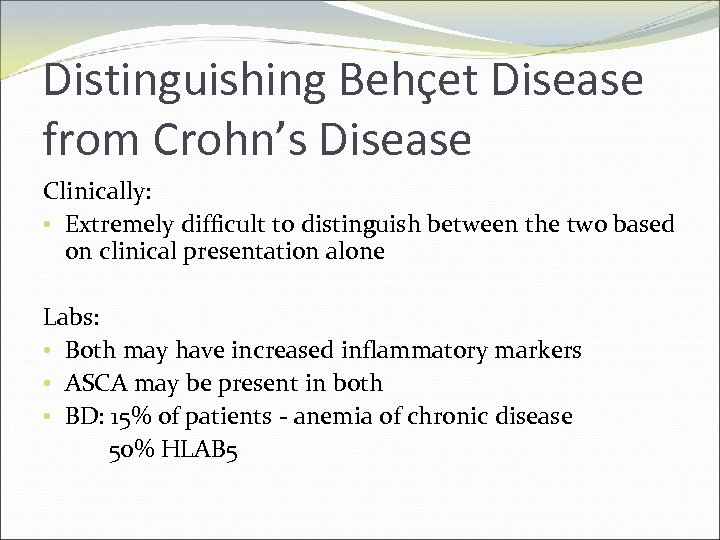
Distinguishing Behçet Disease from Crohn’s Disease Clinically: • Extremely difficult to distinguish between the two based on clinical presentation alone Labs: • Both may have increased inflammatory markers • ASCA may be present in both • BD: 15% of patients - anemia of chronic disease 50% HLAB 5
Distinguishing Behçet Disease from Crohn’s Disease Endoscopically: • Round ulcers are suggestive of Behçet's disease and longitudinal ulcers are suggestive of Crohn's disease. • Irregular/geographic-shaped ulcers and focal distributions are suggestive of Behçet's disease, while segmental/diffuse lesions suggest Crohn's. Differential diagnosis of intestinal Behçet's disease and Crohn's disease by colonoscopic findings. Endoscopy. 2009 Jan; 41(1): 9 -16 • Intestinal lesions found in Crohns disease tend to have a cobblestone appearance whereas those in Behçet are round and oval punched out ulcers. • Granulomas are only rarely found in lesions of BD
So is that it? From all the data and literature two main things stand out: 1. Long Term Follow-Up is Essential – due to the natural course of the disease, symptoms may occur at different times, and have varying time intervals between them. 2. Even with clear definitions, things aren’t always so clear cut. Although there are many definitions and distinctions that can be made, most patients do not necessarily present with the ‘classical’ signs.
So is that it? “A case of Intestinal Behçet Disease Similar to Crohn’s Colitis” J Korean Med Sci 2007; 22: 918 -22 “ 39 -yr-old female was diagnosed as having Behcet’s disease. She was admitted to our hospital because of oral and genital ulcer, lower abdominal pain, and frequent diarrhea. Colonosopy showed diffuse involvement of multiple longitudinal ulcers with inflammatory pseudopolyps with a cobblestone appearance and ano-rectal fistula was suspected. These findings are extremely rare in Behcet’s disease. However, there were no granulomas, the hallmark of Crohn’s colitis. Microscopically, perivasculitis and multiple lymph follicles compatible with Behcet’s disease were seen. “ “In the present case, we made the diagnosis of Behcet’s disease as described above. However, the gastrointestinal manifestation of this case is quite atypical for Behcet’s colitis and more similar to Crohn’s colitis. ” “Clinical and pathological findings are characteristic of intestinal Behcet’s disease. Bowel symptoms, endoscopic appearance, and the response to medical treatment were compatible with Crohn’s colitis. These findings suggest that Behcet’s disease may be a part of the spectrum of chronic inflammatory bowel disease. "
e4ea634f539fc1083a57dab3326a2c15.ppt