4b702ae81584c2ac661fea98c2084d0b.ppt
- Количество слайдов: 54
 Interventions to reduce coercion: with a particular focus on JCPs George Szmukler Oslo May 23 rd 2013 Institute of Psychiatry at The Maudsley
Interventions to reduce coercion: with a particular focus on JCPs George Szmukler Oslo May 23 rd 2013 Institute of Psychiatry at The Maudsley
 Outline • Inpatient coercion (briefly) • ‘Advance Statements’ – JCPs (before ‘Crimson’ study) – PADs • Results of ‘Crimson’ study • Results of ‘Joshua’ study
Outline • Inpatient coercion (briefly) • ‘Advance Statements’ – JCPs (before ‘Crimson’ study) – PADs • Results of ‘Crimson’ study • Results of ‘Joshua’ study
 Reducing inpatient ‘coercion’ 1 Seclusion and restraint 2 ‘Perceived coercion’ 3
Reducing inpatient ‘coercion’ 1 Seclusion and restraint 2 ‘Perceived coercion’ 3
 Reducing restraint and seclusion on inpatient units • No RCTs • Range of ‘systems’ interventions - unique to each organisation Leadership, monitoring of seclusion episodes, staff education, treatment plan improvements, emergency response teams, behavioural consultation, increased staff: patient ratios, treating patients as active participants, ‘Early Recognition Method’ • All are pre- post- comparisons • 15 studies reporting significant reductions in use of seclusion Mistral et al (2002), Schreiner et al (2004), Sullivan et al (2004; 2005), Smith et al (2005), Fowler (2006) or restraint/seclusion Kalogjera et al (1989), Taxis (2002), Donat (2003), Donovan et al (2003), Fisher (2003), D’Orio et al (2004), Le. Bel et al (2004), Green et al (2006), Regan et al (2006), Hellerstein et al (2007) • Risk of ‘publication bias’ 4
Reducing restraint and seclusion on inpatient units • No RCTs • Range of ‘systems’ interventions - unique to each organisation Leadership, monitoring of seclusion episodes, staff education, treatment plan improvements, emergency response teams, behavioural consultation, increased staff: patient ratios, treating patients as active participants, ‘Early Recognition Method’ • All are pre- post- comparisons • 15 studies reporting significant reductions in use of seclusion Mistral et al (2002), Schreiner et al (2004), Sullivan et al (2004; 2005), Smith et al (2005), Fowler (2006) or restraint/seclusion Kalogjera et al (1989), Taxis (2002), Donat (2003), Donovan et al (2003), Fisher (2003), D’Orio et al (2004), Le. Bel et al (2004), Green et al (2006), Regan et al (2006), Hellerstein et al (2007) • Risk of ‘publication bias’ 4
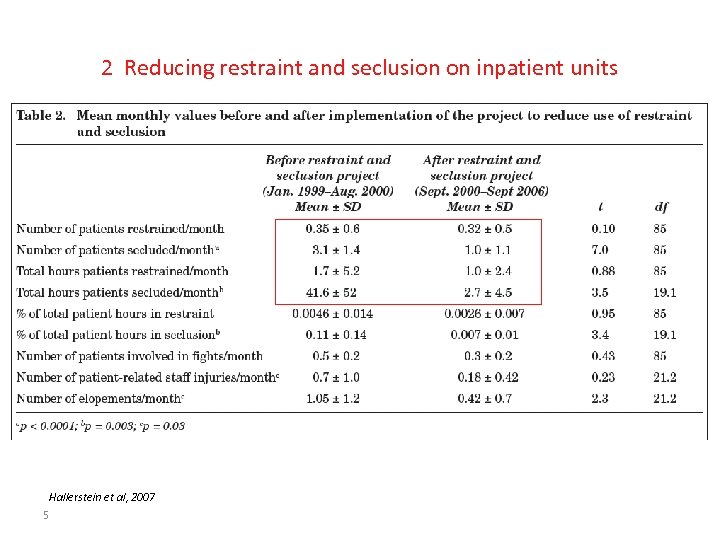 2 Reducing restraint and seclusion on inpatient units Hallerstein et al, 2007 5
2 Reducing restraint and seclusion on inpatient units Hallerstein et al, 2007 5
 1 Intervention to reduce ‘perceived coercion’ on acute psychiatric wards (Sorgaard 2004) • • • Two acute wards: 12 week intervention phase 190 patients (~ 28% psychosis, ~50% mood disorders; ~50% involuntary admission) Intervention: – – • engage patient in formulating treatment plan regular joint evaluations of progress renegotiate treatment plans if necessary regular meetings at least once per week; jointly written daily case notes Outcome measures: – Patient satisfaction (SPRI) (+ patronizing communication and physical harassment) – Perceived coercion’ (Coercion ladder) – Obtained shortly before discharge 6
1 Intervention to reduce ‘perceived coercion’ on acute psychiatric wards (Sorgaard 2004) • • • Two acute wards: 12 week intervention phase 190 patients (~ 28% psychosis, ~50% mood disorders; ~50% involuntary admission) Intervention: – – • engage patient in formulating treatment plan regular joint evaluations of progress renegotiate treatment plans if necessary regular meetings at least once per week; jointly written daily case notes Outcome measures: – Patient satisfaction (SPRI) (+ patronizing communication and physical harassment) – Perceived coercion’ (Coercion ladder) – Obtained shortly before discharge 6
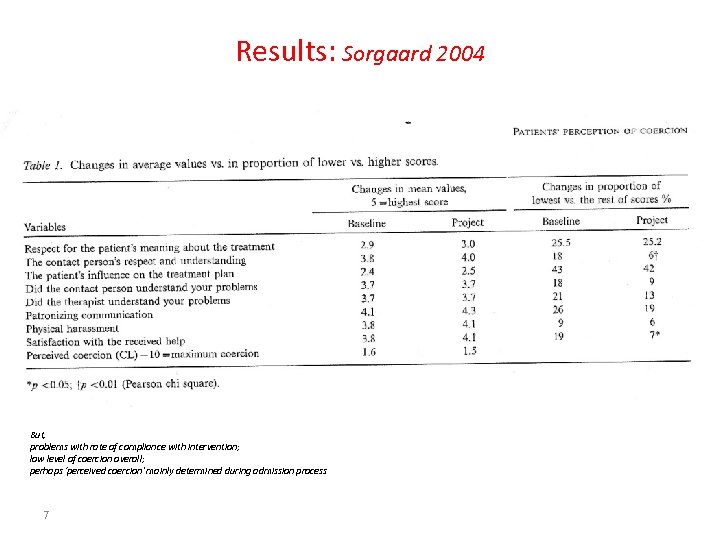 Results: Sorgaard 2004 But, problems with rate of compliance with intervention; low level of coercion overall; perhaps ‘perceived coercion’ mainly determined during admission process 7
Results: Sorgaard 2004 But, problems with rate of compliance with intervention; low level of coercion overall; perhaps ‘perceived coercion’ mainly determined during admission process 7
 Use of ‘advance statements’ to reduce coercion • What is an ‘advance statement’? • Types of ‘advance statement’ • Research evidence 8
Use of ‘advance statements’ to reduce coercion • What is an ‘advance statement’? • Types of ‘advance statement’ • Research evidence 8
 ‘Advance Statements’ • ‘Advance Statements’ express treatment preferences, anticipating a time in the future when the patient will not be capable of stating them. • Purpose - to prevent adverse consequences of relapse, and thus to reduce the need for coercion, by giving patient more control over treatment decisions. 9
‘Advance Statements’ • ‘Advance Statements’ express treatment preferences, anticipating a time in the future when the patient will not be capable of stating them. • Purpose - to prevent adverse consequences of relapse, and thus to reduce the need for coercion, by giving patient more control over treatment decisions. 9
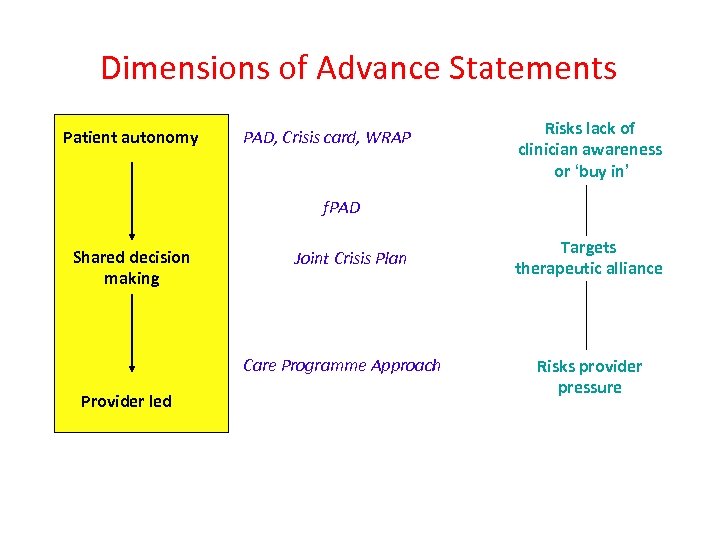 Dimensions of Advance Statements Patient autonomy PAD, Crisis card, WRAP Risks lack of clinician awareness or ‘buy in’ f. PAD Shared decision making Joint Crisis Plan Care Programme Approach Provider led Targets therapeutic alliance Risks provider pressure
Dimensions of Advance Statements Patient autonomy PAD, Crisis card, WRAP Risks lack of clinician awareness or ‘buy in’ f. PAD Shared decision making Joint Crisis Plan Care Programme Approach Provider led Targets therapeutic alliance Risks provider pressure
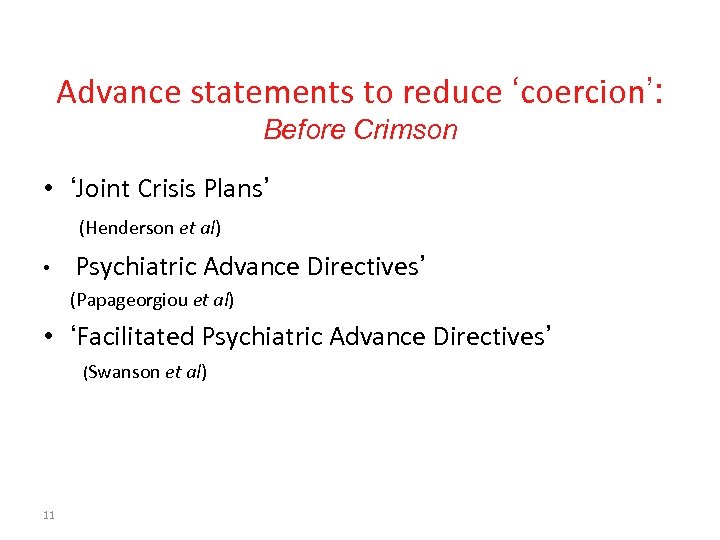 Advance statements to reduce ‘coercion’: Before Crimson • ‘Joint Crisis Plans’ (Henderson et al) • Psychiatric Advance Directives’ (Papageorgiou et al) • ‘Facilitated Psychiatric Advance Directives’ (Swanson et al) 11
Advance statements to reduce ‘coercion’: Before Crimson • ‘Joint Crisis Plans’ (Henderson et al) • Psychiatric Advance Directives’ (Papageorgiou et al) • ‘Facilitated Psychiatric Advance Directives’ (Swanson et al) 11
 A randomised controlled trial of Joint Crisis Plans Claire Henderson, Kim Sutherby, Chris Flood, Morven Leese, Graham Thornicroft, George Szmukler, Institute of Psychiatry, King’s College London & South London and Maudsley NHS Trust Institute of Psychiatry at The Maudsley
A randomised controlled trial of Joint Crisis Plans Claire Henderson, Kim Sutherby, Chris Flood, Morven Leese, Graham Thornicroft, George Szmukler, Institute of Psychiatry, King’s College London & South London and Maudsley NHS Trust Institute of Psychiatry at The Maudsley
 An RCT of Joint Crisis Plans Aim to evaluate the effectiveness of JCPs on inpatient service use and objective coercion (use of the Mental Health Act 1983) during admission.
An RCT of Joint Crisis Plans Aim to evaluate the effectiveness of JCPs on inpatient service use and objective coercion (use of the Mental Health Act 1983) during admission.
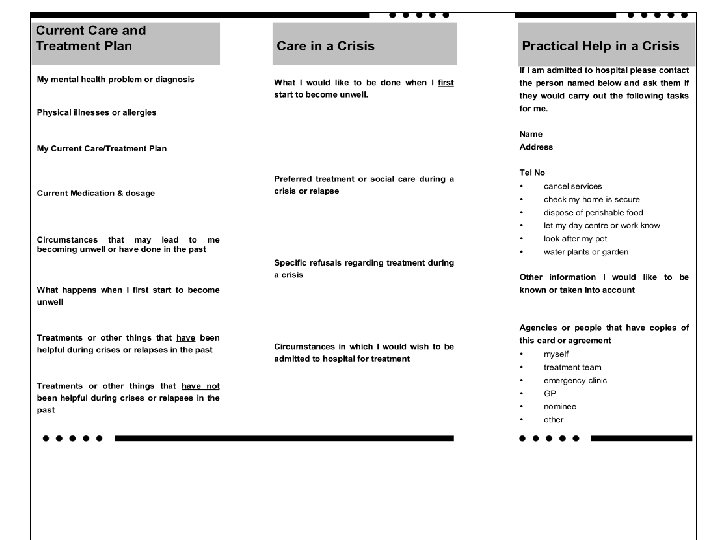
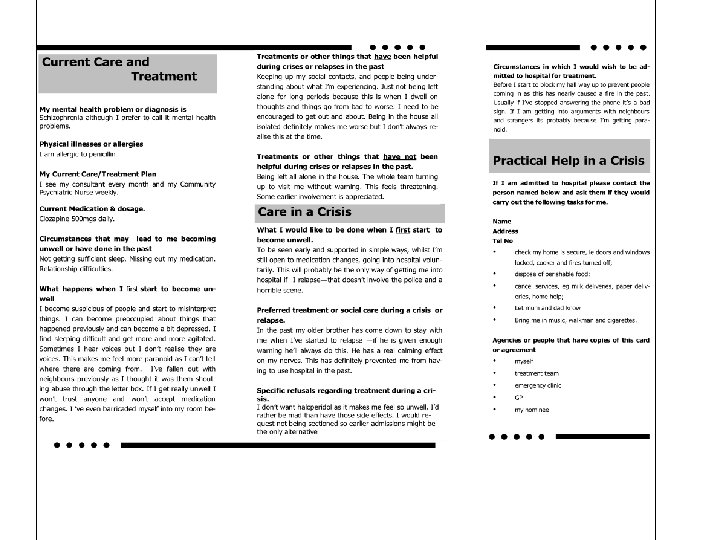
 Joint Crisis Plan • Experimental intervention – Project worker explains to patient – ‘Menu’ of subheadings – JCP meeting: facilitator; attendees, negotiation; patient decides – Controls: detailed information leaflets; written care plan (CPA) 14
Joint Crisis Plan • Experimental intervention – Project worker explains to patient – ‘Menu’ of subheadings – JCP meeting: facilitator; attendees, negotiation; patient decides – Controls: detailed information leaflets; written care plan (CPA) 14

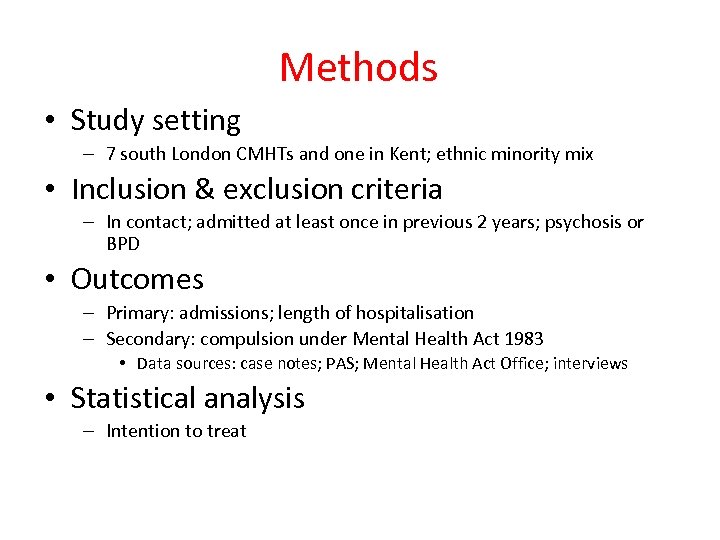 Methods • Study setting – 7 south London CMHTs and one in Kent; ethnic minority mix • Inclusion & exclusion criteria – In contact; admitted at least once in previous 2 years; psychosis or BPD • Outcomes – Primary: admissions; length of hospitalisation – Secondary: compulsion under Mental Health Act 1983 • Data sources: case notes; PAS; Mental Health Act Office; interviews • Statistical analysis – Intention to treat
Methods • Study setting – 7 south London CMHTs and one in Kent; ethnic minority mix • Inclusion & exclusion criteria – In contact; admitted at least once in previous 2 years; psychosis or BPD • Outcomes – Primary: admissions; length of hospitalisation – Secondary: compulsion under Mental Health Act 1983 • Data sources: case notes; PAS; Mental Health Act Office; interviews • Statistical analysis – Intention to treat
 Baseline demographic and clinical characteristics of participant groups (1) Intervention group (n=80) Control group (n=80) 39. 5 (12. 1) 38. 6 (10. 6) Gender: male, n (%) 47 (59) Ethnicity, n (%) White Black Other 29 (36) 44 (55) 7 (9) 34 (42) 40 (50) 6 (7) 5 5 Age in years (mean [s. d]) Number of previous psychiatric admissions (median)
Baseline demographic and clinical characteristics of participant groups (1) Intervention group (n=80) Control group (n=80) 39. 5 (12. 1) 38. 6 (10. 6) Gender: male, n (%) 47 (59) Ethnicity, n (%) White Black Other 29 (36) 44 (55) 7 (9) 34 (42) 40 (50) 6 (7) 5 5 Age in years (mean [s. d]) Number of previous psychiatric admissions (median)
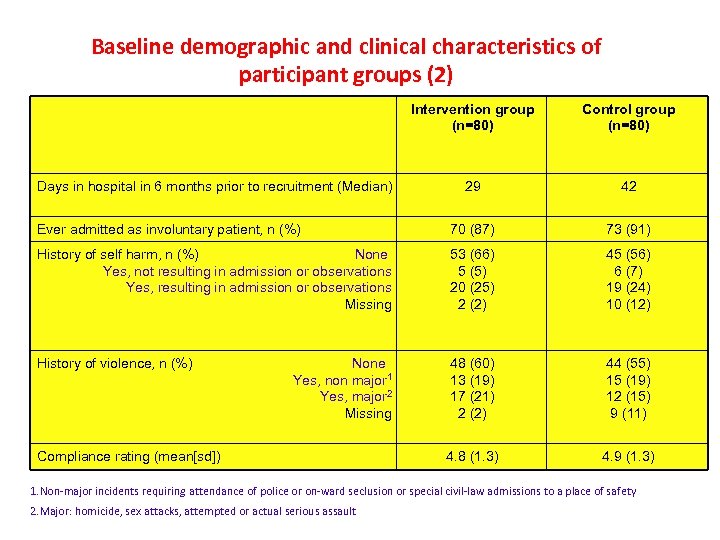 Baseline demographic and clinical characteristics of participant groups (2) Intervention group (n=80) Control group (n=80) 29 42 Ever admitted as involuntary patient, n (%) 70 (87) 73 (91) History of self harm, n (%) None Yes, not resulting in admission or observations Yes, resulting in admission or observations Missing 53 (66) 5 (5) 20 (25) 2 (2) 45 (56) 6 (7) 19 (24) 10 (12) History of violence, n (%) 48 (60) 13 (19) 17 (21) 2 (2) 44 (55) 15 (19) 12 (15) 9 (11) 4. 8 (1. 3) 4. 9 (1. 3) Days in hospital in 6 months prior to recruitment (Median) None Yes, non major 1 Yes, major 2 Missing Compliance rating (mean[sd]) 1. Non-major incidents requiring attendance of police or on-ward seclusion or special civil-law admissions to a place of safety 2. Major: homicide, sex attacks, attempted or actual serious assault
Baseline demographic and clinical characteristics of participant groups (2) Intervention group (n=80) Control group (n=80) 29 42 Ever admitted as involuntary patient, n (%) 70 (87) 73 (91) History of self harm, n (%) None Yes, not resulting in admission or observations Yes, resulting in admission or observations Missing 53 (66) 5 (5) 20 (25) 2 (2) 45 (56) 6 (7) 19 (24) 10 (12) History of violence, n (%) 48 (60) 13 (19) 17 (21) 2 (2) 44 (55) 15 (19) 12 (15) 9 (11) 4. 8 (1. 3) 4. 9 (1. 3) Days in hospital in 6 months prior to recruitment (Median) None Yes, non major 1 Yes, major 2 Missing Compliance rating (mean[sd]) 1. Non-major incidents requiring attendance of police or on-ward seclusion or special civil-law admissions to a place of safety 2. Major: homicide, sex attacks, attempted or actual serious assault
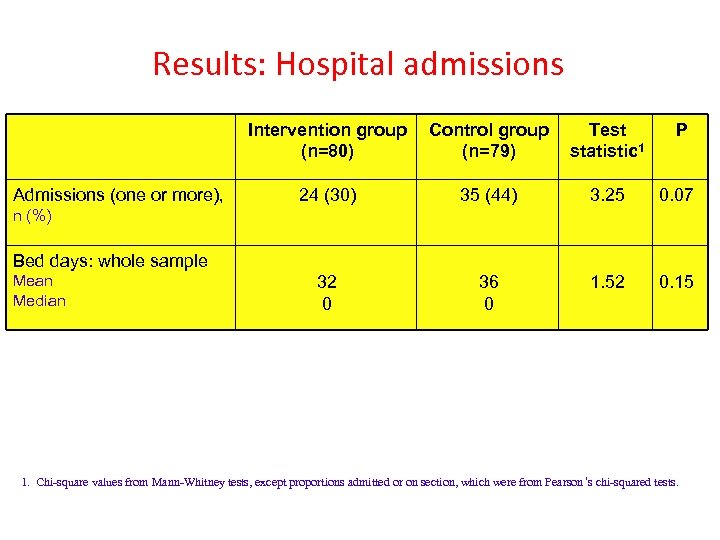 Results: Hospital admissions Intervention group (n=80) Admissions (one or more), Control group (n=79) Test statistic 1 P 24 (30) 35 (44) 3. 25 0. 07 32 0 36 0 1. 52 0. 15 n (%) Bed days: whole sample Mean Median 1. Chi-square values from Mann-Whitney tests, except proportions admitted or on section, which were from Pearson ’s chi-squared tests.
Results: Hospital admissions Intervention group (n=80) Admissions (one or more), Control group (n=79) Test statistic 1 P 24 (30) 35 (44) 3. 25 0. 07 32 0 36 0 1. 52 0. 15 n (%) Bed days: whole sample Mean Median 1. Chi-square values from Mann-Whitney tests, except proportions admitted or on section, which were from Pearson ’s chi-squared tests.
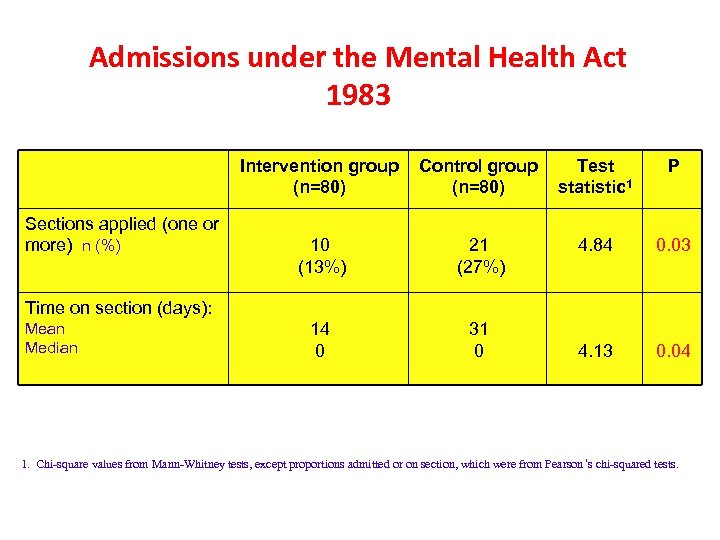 Admissions under the Mental Health Act 1983 Intervention group (n=80) Sections applied (one or more) n (%) Control group (n=80) Test statistic 1 P 10 (13%) 21 (27%) 4. 84 0. 03 14 0 31 0 4. 13 0. 04 Time on section (days): Mean Median 1. Chi-square values from Mann-Whitney tests, except proportions admitted or on section, which were from Pearson ’s chi-squared tests.
Admissions under the Mental Health Act 1983 Intervention group (n=80) Sections applied (one or more) n (%) Control group (n=80) Test statistic 1 P 10 (13%) 21 (27%) 4. 84 0. 03 14 0 31 0 4. 13 0. 04 Time on section (days): Mean Median 1. Chi-square values from Mann-Whitney tests, except proportions admitted or on section, which were from Pearson ’s chi-squared tests.
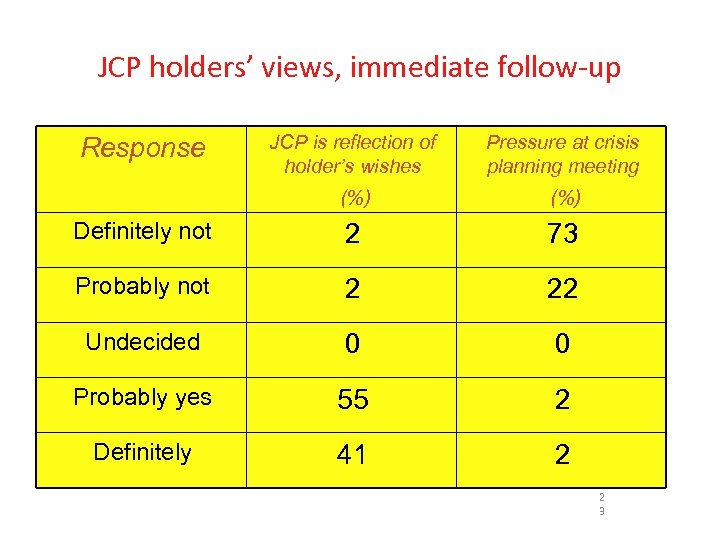 JCP holders’ views, immediate follow-up JCP is reflection of holder’s wishes Pressure at crisis planning meeting (%) Definitely not 2 73 Probably not 2 22 Undecided 0 0 Probably yes 55 2 Definitely 41 2 Response 2 3
JCP holders’ views, immediate follow-up JCP is reflection of holder’s wishes Pressure at crisis planning meeting (%) Definitely not 2 73 Probably not 2 22 Undecided 0 0 Probably yes 55 2 Definitely 41 2 Response 2 3
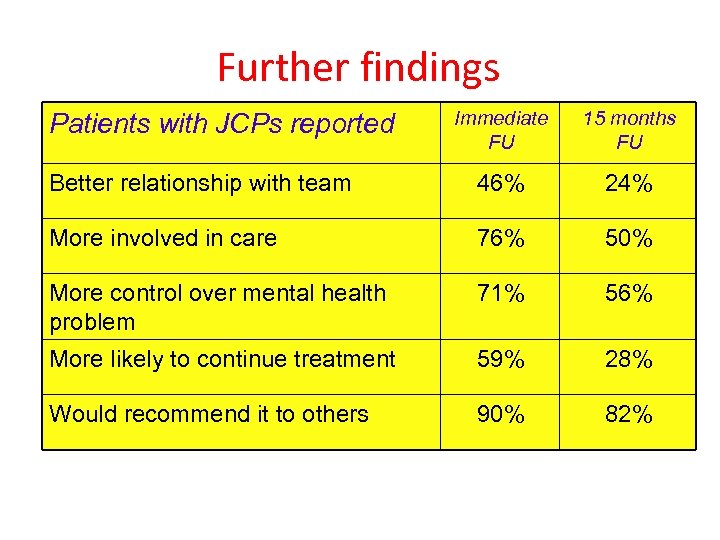 Further findings Immediate FU 15 months FU Better relationship with team 46% 24% More involved in care 76% 50% More control over mental health problem 71% 56% More likely to continue treatment 59% 28% Would recommend it to others 90% 82% Patients with JCPs reported
Further findings Immediate FU 15 months FU Better relationship with team 46% 24% More involved in care 76% 50% More control over mental health problem 71% 56% More likely to continue treatment 59% 28% Would recommend it to others 90% 82% Patients with JCPs reported
 Advance directives for patients compulsorily admitted to hospital with serious mental illness: Randomised controlled trial (A Papageorgiou et al, 2002) Aims To evaluate whether use of ‘advance directives’ by patients with mental illness leads to lower rates of compulsory readmission to hospital. Subjects 156 patients admitted involuntarily Intervention ‘Advance directive’ completed with research worker, but clinical team not significantly involved. RCT. Outcome measures Compulsory readmissions, days in hospital, satisfaction. Results None significant Conclusions Users' advance instruction had little observable impact on the outcome of care at 12 months. But, providers of care not significantly involved in advance directive
Advance directives for patients compulsorily admitted to hospital with serious mental illness: Randomised controlled trial (A Papageorgiou et al, 2002) Aims To evaluate whether use of ‘advance directives’ by patients with mental illness leads to lower rates of compulsory readmission to hospital. Subjects 156 patients admitted involuntarily Intervention ‘Advance directive’ completed with research worker, but clinical team not significantly involved. RCT. Outcome measures Compulsory readmissions, days in hospital, satisfaction. Results None significant Conclusions Users' advance instruction had little observable impact on the outcome of care at 12 months. But, providers of care not significantly involved in advance directive
 RCT of facilitated PADS (Swanson et al, 2006) • Method: 469 patients with severe mental illness in two county-based mental health systems (North Carolina) randomly assigned to a facilitated advance directive (FPAD) session or control group. • Results: 61% of the 239 patients allocated to the F-PAD group completed legal advance instructions or authorized a proxy decisionmaker, compared with 3% of control group. • At 1 month follow-up, F-PAD participants had significantly greater working alliance and were significantly more likely to report receiving the mental health services they believed they needed.
RCT of facilitated PADS (Swanson et al, 2006) • Method: 469 patients with severe mental illness in two county-based mental health systems (North Carolina) randomly assigned to a facilitated advance directive (FPAD) session or control group. • Results: 61% of the 239 patients allocated to the F-PAD group completed legal advance instructions or authorized a proxy decisionmaker, compared with 3% of control group. • At 1 month follow-up, F-PAD participants had significantly greater working alliance and were significantly more likely to report receiving the mental health services they believed they needed.
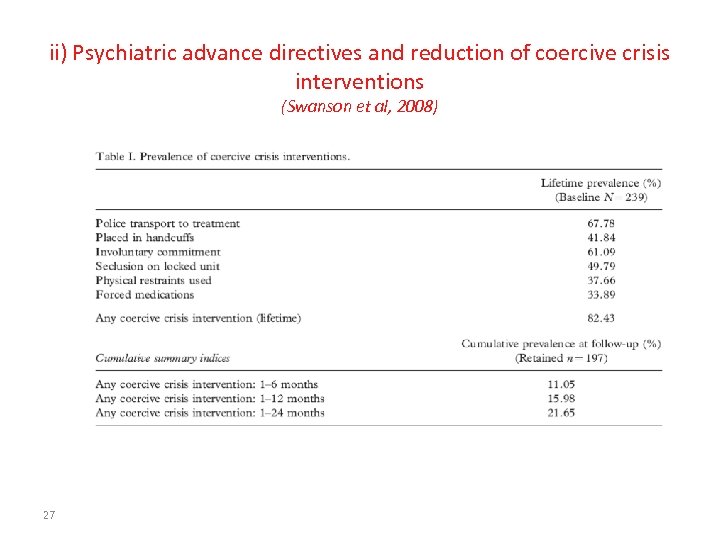 ii) Psychiatric advance directives and reduction of coercive crisis interventions (Swanson et al, 2008) 27
ii) Psychiatric advance directives and reduction of coercive crisis interventions (Swanson et al, 2008) 27
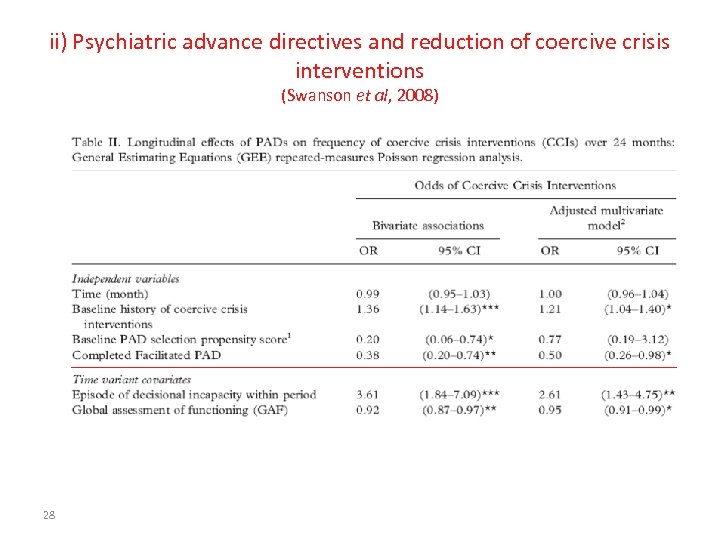 ii) Psychiatric advance directives and reduction of coercive crisis interventions (Swanson et al, 2008) 28
ii) Psychiatric advance directives and reduction of coercive crisis interventions (Swanson et al, 2008) 28
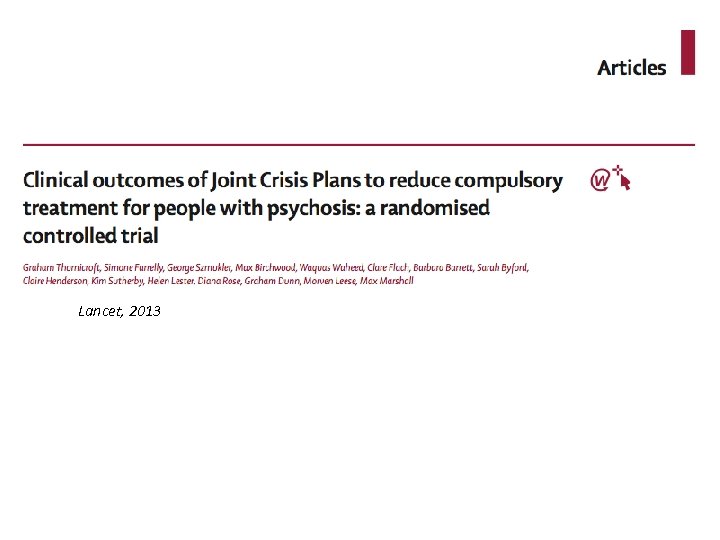 Lancet, 2013
Lancet, 2013
 Crimson Study: methods • Single-blind, ‘intention to treat’ RCT • JCP v TAU • Experimental intervention – Project worker explains to patient – ‘Menu’ of subheadings – JCP meeting: facilitator; attendees, negotiation; patient decides – Copy to those psychiatric team, electronic record, anyone else nominated by patient – After 9 months participant asked if JCP needed update – Fidelity ratings of random selection at 3 phases of study 30
Crimson Study: methods • Single-blind, ‘intention to treat’ RCT • JCP v TAU • Experimental intervention – Project worker explains to patient – ‘Menu’ of subheadings – JCP meeting: facilitator; attendees, negotiation; patient decides – Copy to those psychiatric team, electronic record, anyone else nominated by patient – After 9 months participant asked if JCP needed update – Fidelity ratings of random selection at 3 phases of study 30
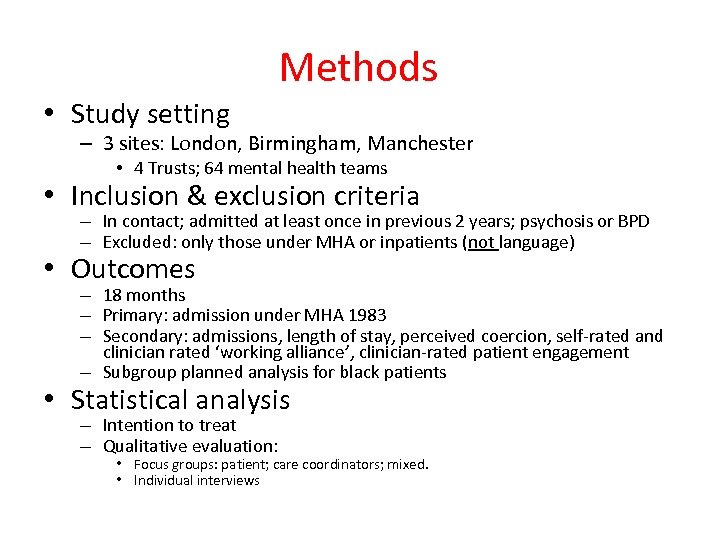 Methods • Study setting – 3 sites: London, Birmingham, Manchester • 4 Trusts; 64 mental health teams • Inclusion & exclusion criteria – In contact; admitted at least once in previous 2 years; psychosis or BPD – Excluded: only those under MHA or inpatients (not language) • Outcomes – 18 months – Primary: admission under MHA 1983 – Secondary: admissions, length of stay, perceived coercion, self-rated and clinician rated ‘working alliance’, clinician-rated patient engagement – Subgroup planned analysis for black patients • Statistical analysis – Intention to treat – Qualitative evaluation: • Focus groups: patient; care coordinators; mixed. • Individual interviews
Methods • Study setting – 3 sites: London, Birmingham, Manchester • 4 Trusts; 64 mental health teams • Inclusion & exclusion criteria – In contact; admitted at least once in previous 2 years; psychosis or BPD – Excluded: only those under MHA or inpatients (not language) • Outcomes – 18 months – Primary: admission under MHA 1983 – Secondary: admissions, length of stay, perceived coercion, self-rated and clinician rated ‘working alliance’, clinician-rated patient engagement – Subgroup planned analysis for black patients • Statistical analysis – Intention to treat – Qualitative evaluation: • Focus groups: patient; care coordinators; mixed. • Individual interviews
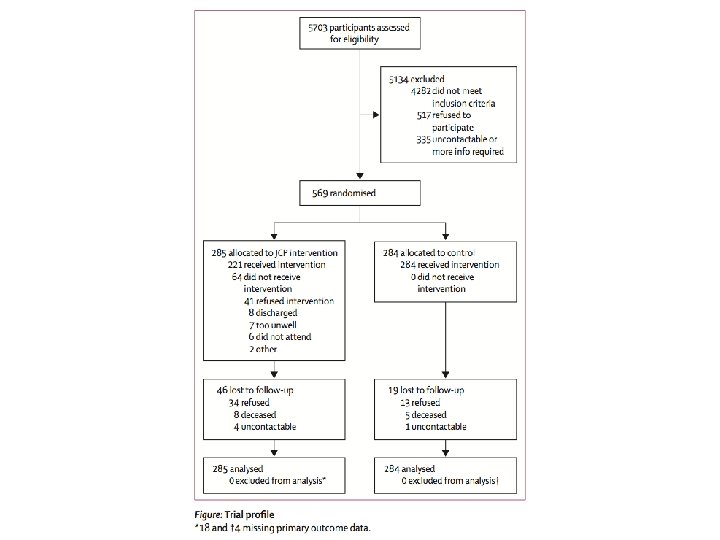
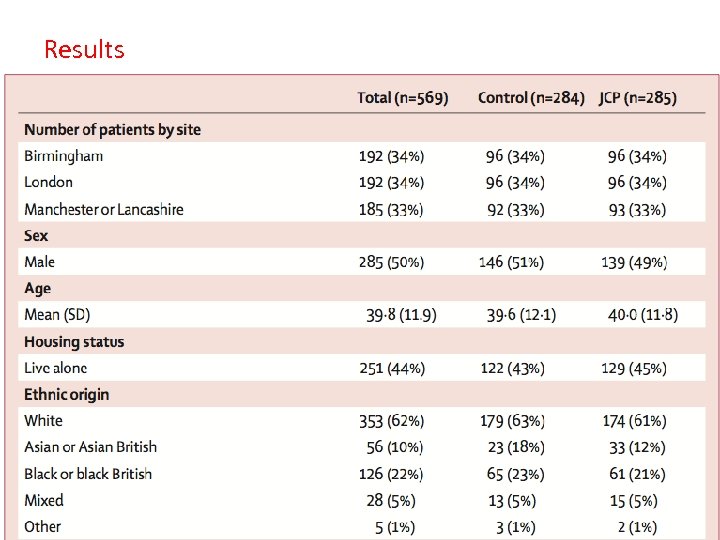 Results
Results

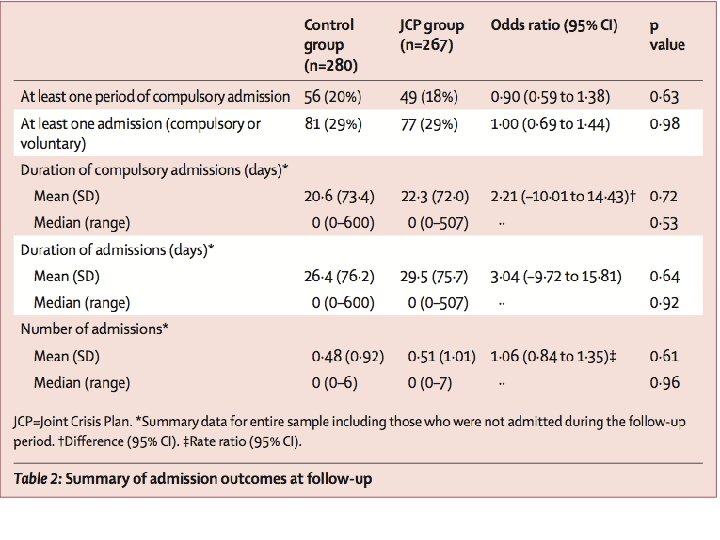
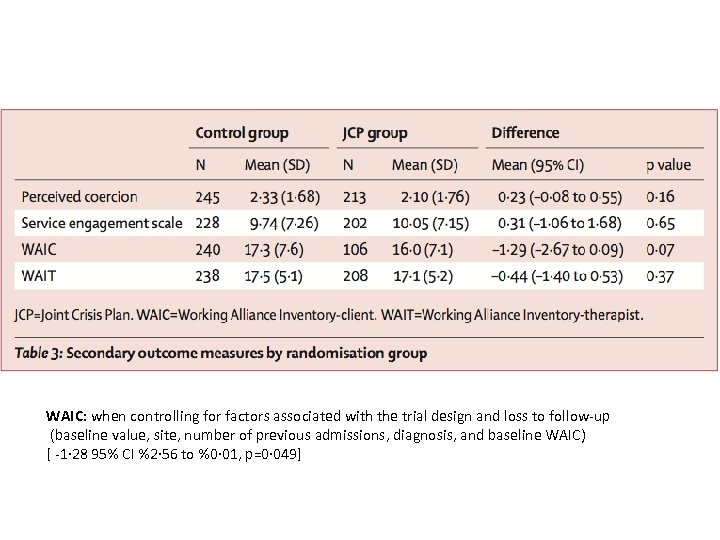 WAIC: when controlling for factors associated with the trial design and loss to follow-up (baseline value, site, number of previous admissions, diagnosis, and baseline WAIC) [ -1· 28 95% CI %2· 56 to %0· 01, p=0· 049]
WAIC: when controlling for factors associated with the trial design and loss to follow-up (baseline value, site, number of previous admissions, diagnosis, and baseline WAIC) [ -1· 28 95% CI %2· 56 to %0· 01, p=0· 049]

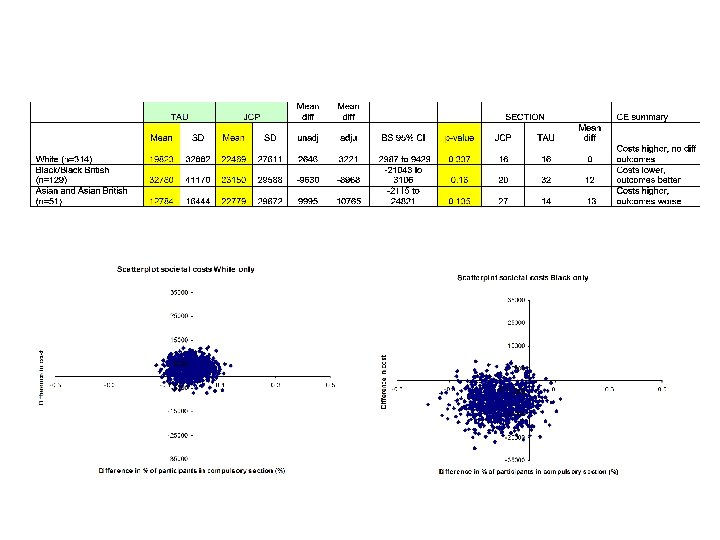
 Economic analysis The addition of JCPs to TAU had no significant effect on total societal cost per participant over 18 -months follow-up. From the service cost perspective, however, a higher probability (80%) of JCPs being the more cost-effective option. Exploration by ethnic group highlights distinct patterns of costs and effects. Whilst the evidence does not support the cost-effectiveness of JCPs for White or Asian ethnic groups, there is at least a 90% probability of the JCP intervention being the more cost-effective option in the Black ethnic group.
Economic analysis The addition of JCPs to TAU had no significant effect on total societal cost per participant over 18 -months follow-up. From the service cost perspective, however, a higher probability (80%) of JCPs being the more cost-effective option. Exploration by ethnic group highlights distinct patterns of costs and effects. Whilst the evidence does not support the cost-effectiveness of JCPs for White or Asian ethnic groups, there is at least a 90% probability of the JCP intervention being the more cost-effective option in the Black ethnic group.
 Qualitative Study • 12 focus groups – Types of groups: 5 patient, 5 care coordinators, 2 combined – 58 people: 35 patients, 22 care coordinators, 1 psychiatrist • 37 individual interviews – 16 psychiatrist, 6 care coordinators, 15 patients
Qualitative Study • 12 focus groups – Types of groups: 5 patient, 5 care coordinators, 2 combined – 58 people: 35 patients, 22 care coordinators, 1 psychiatrist • 37 individual interviews – 16 psychiatrist, 6 care coordinators, 15 patients
 Qualitative Study • PATIENTS – Patients with JCPs felt more respected and more understood by clinicians, particularly with regard to treatment preferences – Benefits when JCP meeting acted as a vehicle for clinicians to demonstrate respect for patients’ experiences and views – However, more common was poor clinician engagement with the process (48% in association with CPA meeting) • CLINICIANS – “Already carry out ‘joint’ planning” – Ambivalence about ‘care planning’; a bureaucratic exercise with limited clinical benefit – Did not recognise that JCP required a change in clinician-patient relationship – JCPs not honoured in practice; 5/28 care coordinators referred to the JCP
Qualitative Study • PATIENTS – Patients with JCPs felt more respected and more understood by clinicians, particularly with regard to treatment preferences – Benefits when JCP meeting acted as a vehicle for clinicians to demonstrate respect for patients’ experiences and views – However, more common was poor clinician engagement with the process (48% in association with CPA meeting) • CLINICIANS – “Already carry out ‘joint’ planning” – Ambivalence about ‘care planning’; a bureaucratic exercise with limited clinical benefit – Did not recognise that JCP required a change in clinician-patient relationship – JCPs not honoured in practice; 5/28 care coordinators referred to the JCP
 Why did the JCP intervention fail? • Lack of clinician ‘buy-in’ – 48% associated with CPA review • Negativity about CPA reviews: patient’s voice not heard; clinicians see it as imposed bureaucratic exercise – Delays in arranging meetings – Inadequate formative meeting – Fidelity scale insensitive
Why did the JCP intervention fail? • Lack of clinician ‘buy-in’ – 48% associated with CPA review • Negativity about CPA reviews: patient’s voice not heard; clinicians see it as imposed bureaucratic exercise – Delays in arranging meetings – Inadequate formative meeting – Fidelity scale insensitive
 Methods • aged 18 years or older • meeting diagnostic criteria for BPD [according to DSM-IV-TR criteria] • had self-harmed in the previous 12 months [defined as at least one act with a non-fatal outcome in which the individual had deliberately initiated a behaviour (such as self-cutting), or ingested a toxic substance or object, with the intention of causing harm to themselves] • under the ongoing care of a CMHT
Methods • aged 18 years or older • meeting diagnostic criteria for BPD [according to DSM-IV-TR criteria] • had self-harmed in the previous 12 months [defined as at least one act with a non-fatal outcome in which the individual had deliberately initiated a behaviour (such as self-cutting), or ingested a toxic substance or object, with the intention of causing harm to themselves] • under the ongoing care of a CMHT
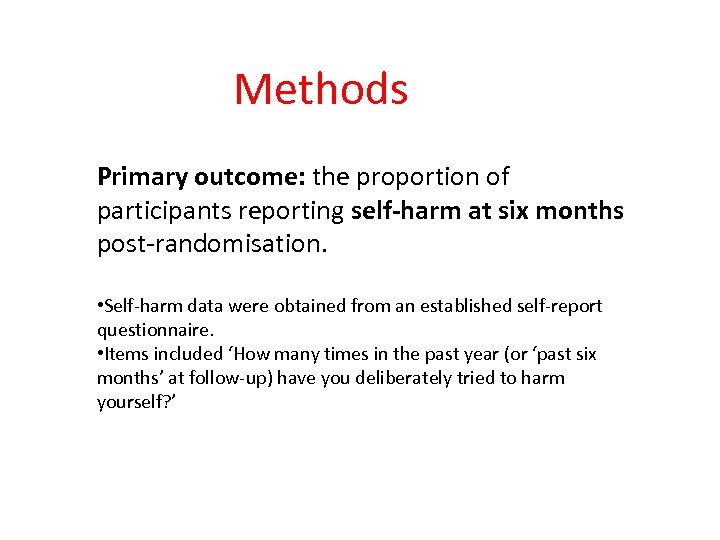 Methods Primary outcome: the proportion of participants reporting self-harm at six months post-randomisation. • Self-harm data were obtained from an established self-report questionnaire. • Items included ‘How many times in the past year (or ‘past six months’ at follow-up) have you deliberately tried to harm yourself? ’
Methods Primary outcome: the proportion of participants reporting self-harm at six months post-randomisation. • Self-harm data were obtained from an established self-report questionnaire. • Items included ‘How many times in the past year (or ‘past six months’ at follow-up) have you deliberately tried to harm yourself? ’
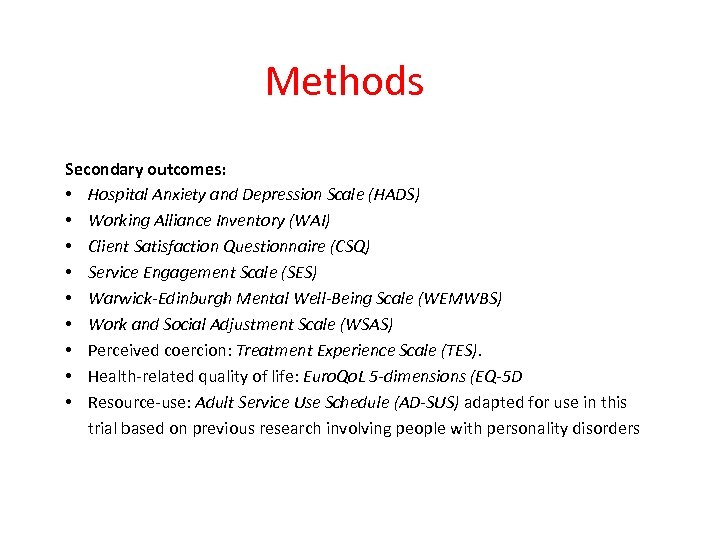 Methods Secondary outcomes: • Hospital Anxiety and Depression Scale (HADS) • Working Alliance Inventory (WAI) • Client Satisfaction Questionnaire (CSQ) • Service Engagement Scale (SES) • Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) • Work and Social Adjustment Scale (WSAS) • Perceived coercion: Treatment Experience Scale (TES). • Health-related quality of life: Euro. Qo. L 5 -dimensions (EQ-5 D • Resource-use: Adult Service Use Schedule (AD-SUS) adapted for use in this trial based on previous research involving people with personality disorders
Methods Secondary outcomes: • Hospital Anxiety and Depression Scale (HADS) • Working Alliance Inventory (WAI) • Client Satisfaction Questionnaire (CSQ) • Service Engagement Scale (SES) • Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) • Work and Social Adjustment Scale (WSAS) • Perceived coercion: Treatment Experience Scale (TES). • Health-related quality of life: Euro. Qo. L 5 -dimensions (EQ-5 D • Resource-use: Adult Service Use Schedule (AD-SUS) adapted for use in this trial based on previous research involving people with personality disorders
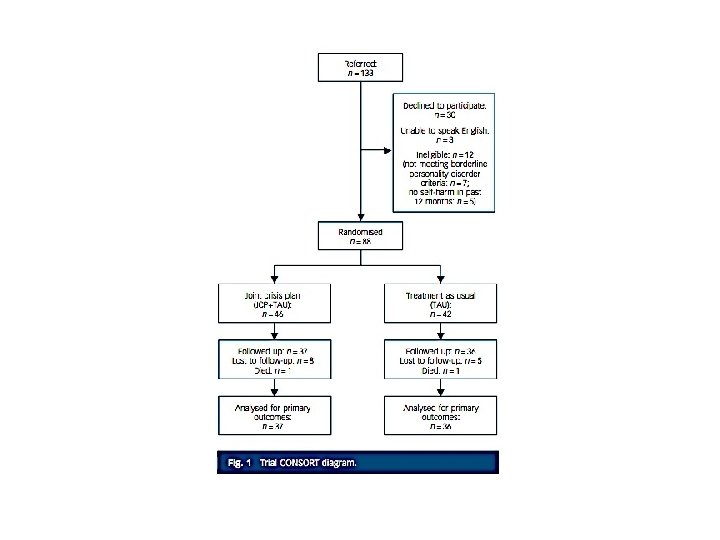
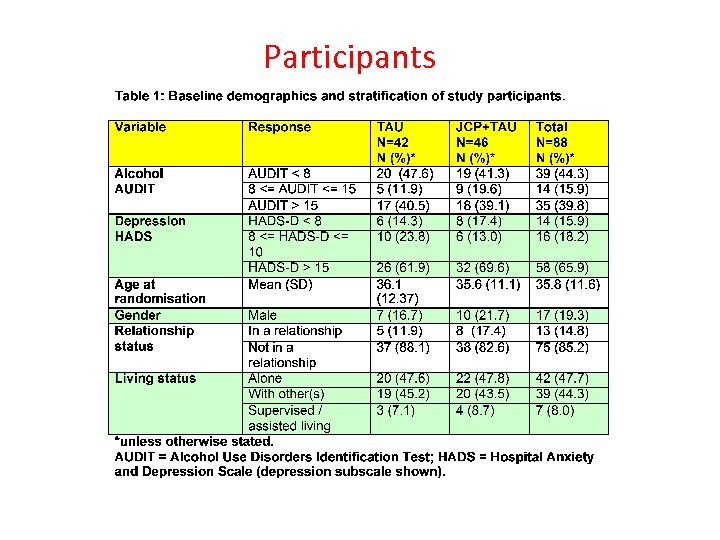 Participants
Participants
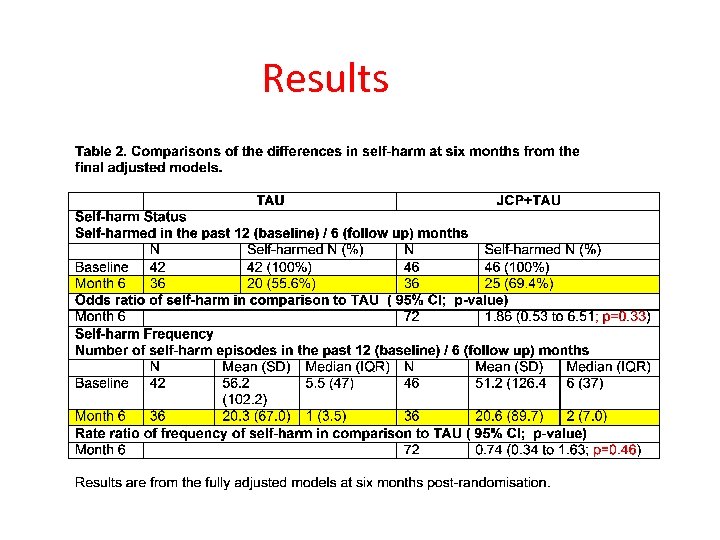 Results
Results
 Results
Results
 Results
Results
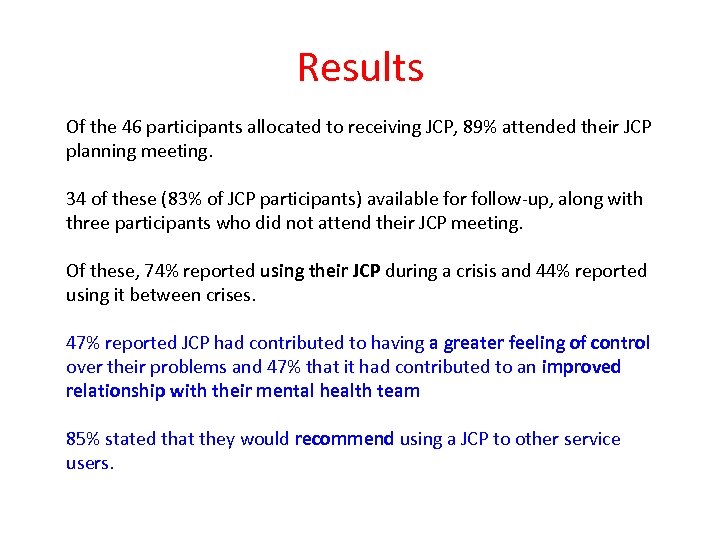 Results Of the 46 participants allocated to receiving JCP, 89% attended their JCP planning meeting. 34 of these (83% of JCP participants) available for follow-up, along with three participants who did not attend their JCP meeting. Of these, 74% reported using their JCP during a crisis and 44% reported using it between crises. 47% reported JCP had contributed to having a greater feeling of control over their problems and 47% that it had contributed to an improved relationship with their mental health team 85% stated that they would recommend using a JCP to other service users.
Results Of the 46 participants allocated to receiving JCP, 89% attended their JCP planning meeting. 34 of these (83% of JCP participants) available for follow-up, along with three participants who did not attend their JCP meeting. Of these, 74% reported using their JCP during a crisis and 44% reported using it between crises. 47% reported JCP had contributed to having a greater feeling of control over their problems and 47% that it had contributed to an improved relationship with their mental health team 85% stated that they would recommend using a JCP to other service users.
 Implications • No difference in terms of measured outcomes • Yet, the patients valued the intervention • What does this mean? – Is the intervention worthwhile? – Does it merit further investigation? • If so, what sort of investigation?
Implications • No difference in terms of measured outcomes • Yet, the patients valued the intervention • What does this mean? – Is the intervention worthwhile? – Does it merit further investigation? • If so, what sort of investigation?
 Lessons for coercion research To be considered in next session
Lessons for coercion research To be considered in next session


