0f168cd2bf5429a5dc4a4d7dae576462.ppt
- Количество слайдов: 174
Interventions for Tuberculosis Control and Elimination Slides from the web site http: //www. tbrieder. org Compiled by: Hans L Rieder
Brick kindly provided by Reuben Granich
Pot kindly provided by Liisa Parkkali
The Area of the “Magic Mountain”
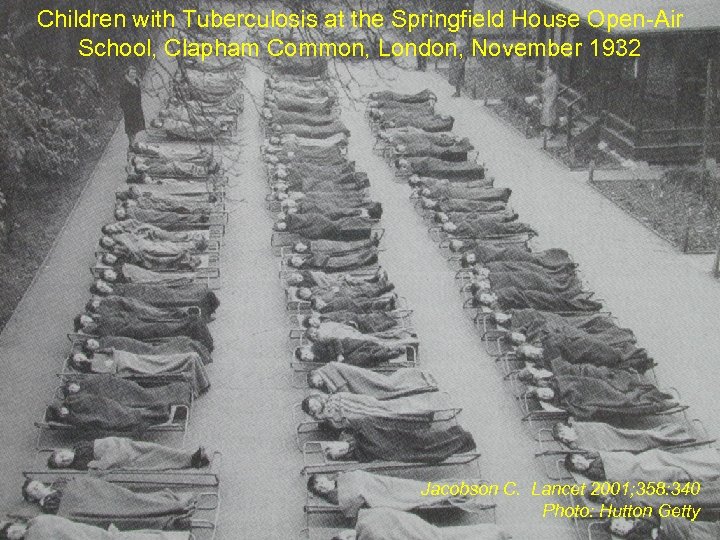
Children with Tuberculosis at the Springfield House Open-Air School, Clapham Common, London, November 1932 Jacobson C. Lancet 2001; 358: 340 Photo: Hutton Getty
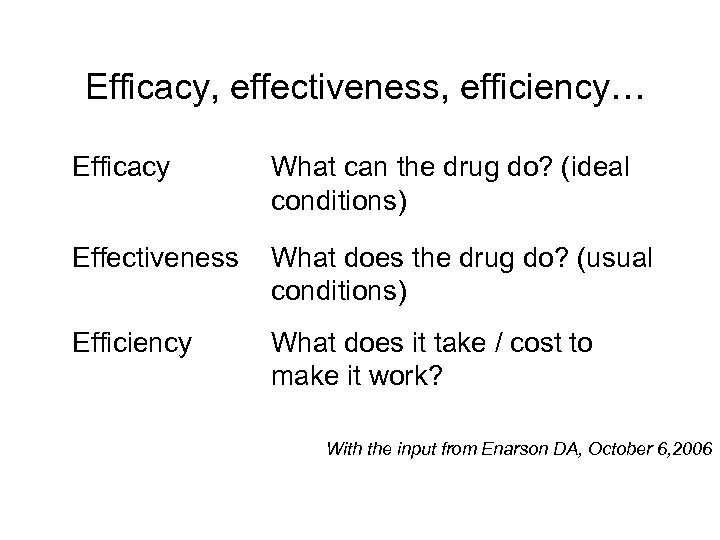
Efficacy, effectiveness, efficiency… Efficacy What can the drug do? (ideal conditions) Effectiveness What does the drug do? (usual conditions) Efficiency What does it take / cost to make it work? With the input from Enarson DA, October 6, 2006
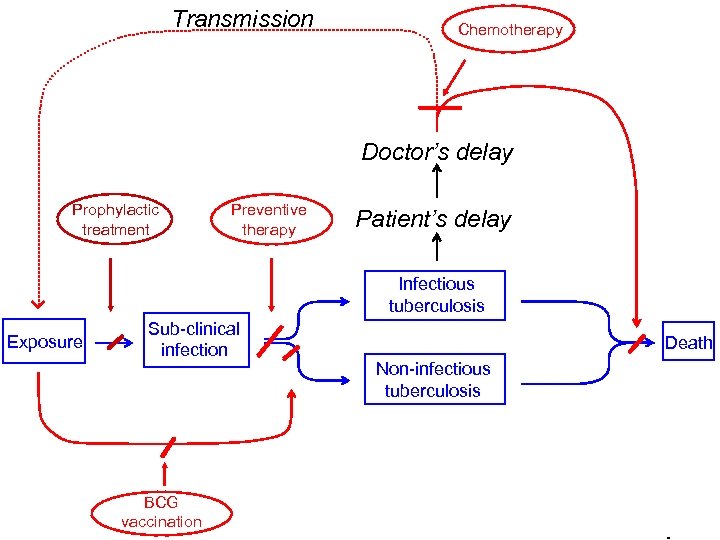
Transmission Chemotherapy Doctor’s delay Prophylactic treatment Preventive therapy Patient’s delay Infectious tuberculosis Exposure Sub-clinical infection BCG vaccination Death Non-infectious tuberculosis
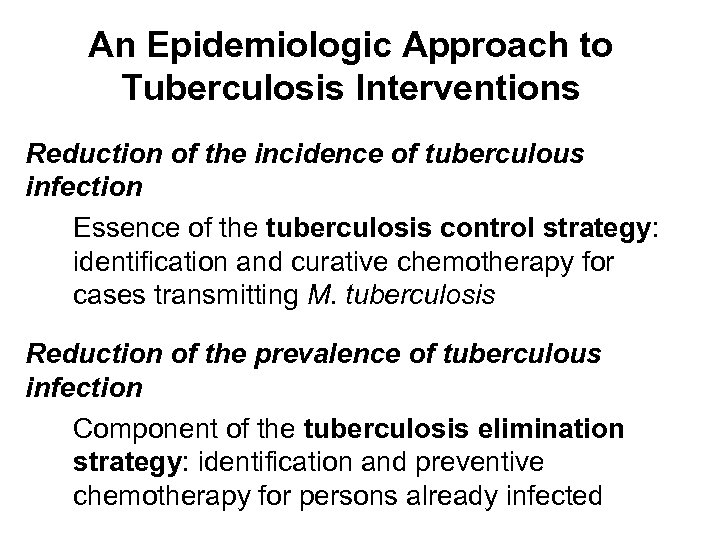
An Epidemiologic Approach to Tuberculosis Interventions Reduction of the incidence of tuberculous infection Essence of the tuberculosis control strategy: identification and curative chemotherapy for cases transmitting M. tuberculosis Reduction of the prevalence of tuberculous infection Component of the tuberculosis elimination strategy: identification and preventive chemotherapy for persons already infected
Chemotherapy
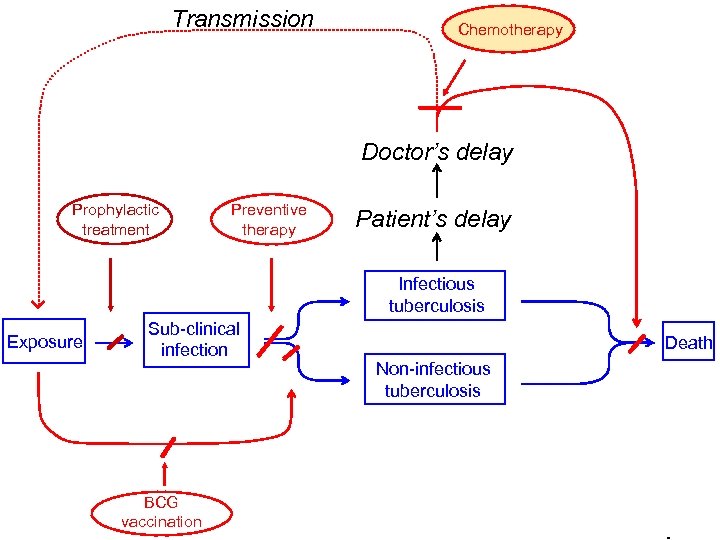
Transmission Chemotherapy Doctor’s delay Prophylactic treatment Preventive therapy Patient’s delay Infectious tuberculosis Exposure Sub-clinical infection BCG vaccination Death Non-infectious tuberculosis
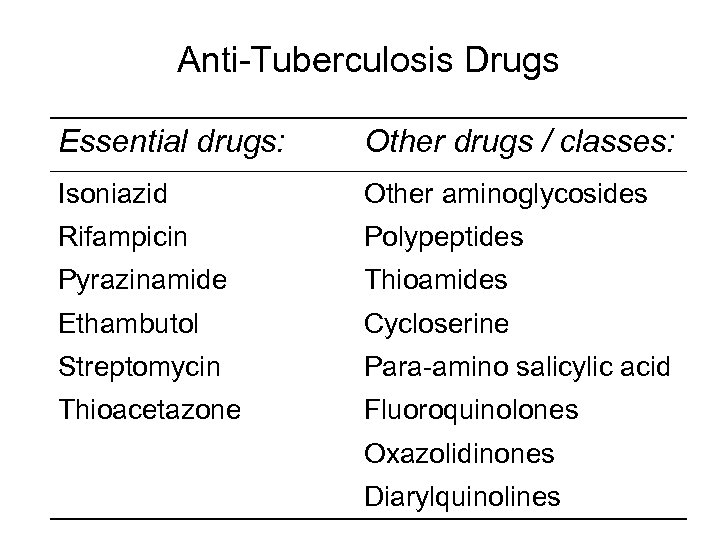
Anti-Tuberculosis Drugs Essential drugs: Other drugs / classes: Isoniazid Other aminoglycosides Rifampicin Polypeptides Pyrazinamide Thioamides Ethambutol Cycloserine Streptomycin Para-amino salicylic acid Thioacetazone Fluoroquinolones Oxazolidinones Diarylquinolines

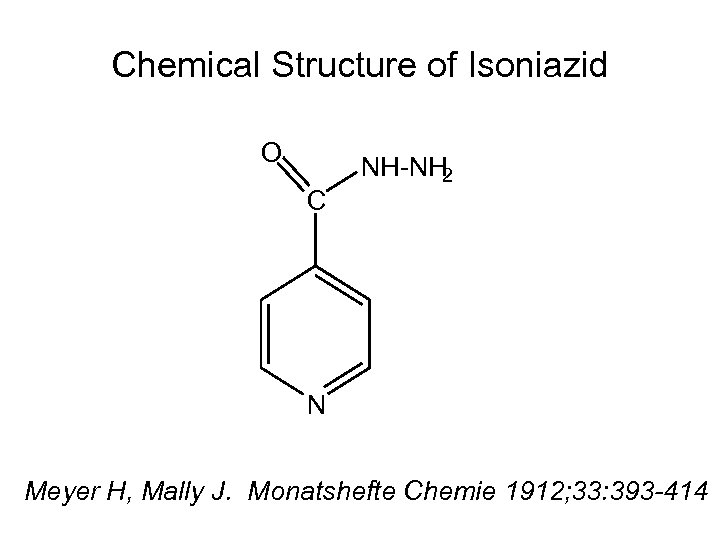
Chemical Structure of Isoniazid O C NH-NH 2 N Meyer H, Mally J. Monatshefte Chemie 1912; 33: 393 -414
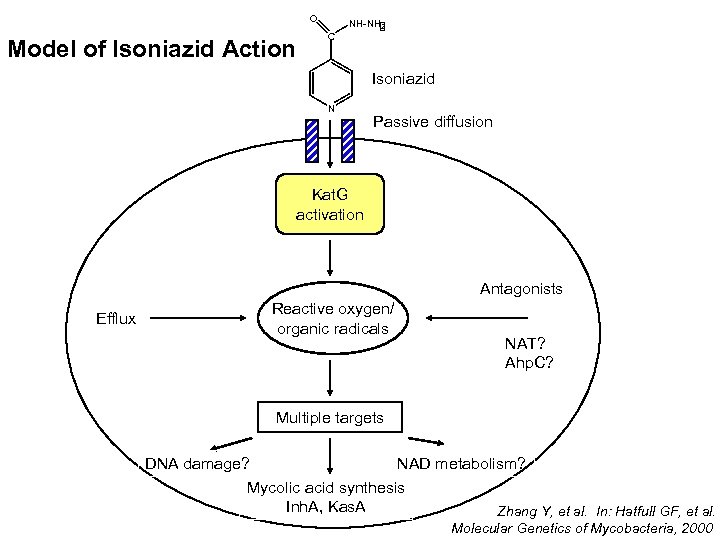
O Model of Isoniazid Action NH-NH 2 C Isoniazid N Passive diffusion Kat. G activation Antagonists Efflux Reactive oxygen/ organic radicals NAT? Ahp. C? Multiple targets DNA damage? NAD metabolism? Mycolic acid synthesis Inh. A, Kas. A Zhang Y, et al. In: Hatfull GF, et al. Molecular Genetics of Mycobacteria, 2000



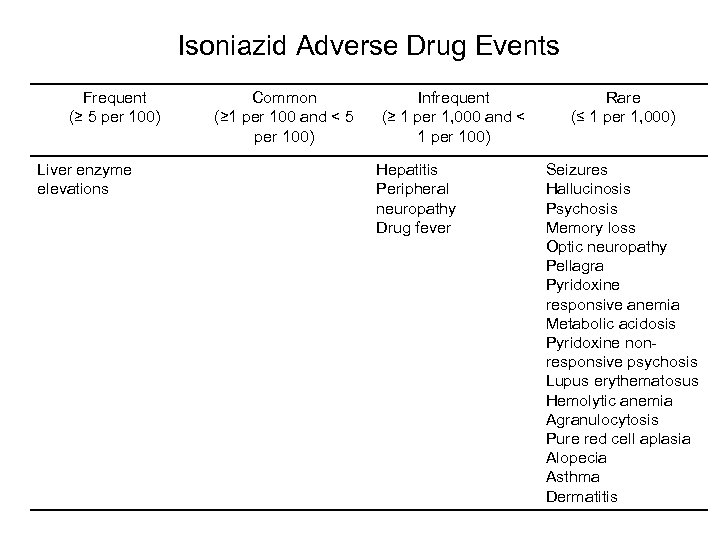
Isoniazid Adverse Drug Events Frequent (≥ 5 per 100) Liver enzyme elevations Common (≥ 1 per 100 and < 5 per 100) Infrequent (≥ 1 per 1, 000 and < 1 per 100) Hepatitis Peripheral neuropathy Drug fever Rare (≤ 1 per 1, 000) Seizures Hallucinosis Psychosis Memory loss Optic neuropathy Pellagra Pyridoxine responsive anemia Metabolic acidosis Pyridoxine nonresponsive psychosis Lupus erythematosus Hemolytic anemia Agranulocytosis Pure red cell aplasia Alopecia Asthma Dermatitis


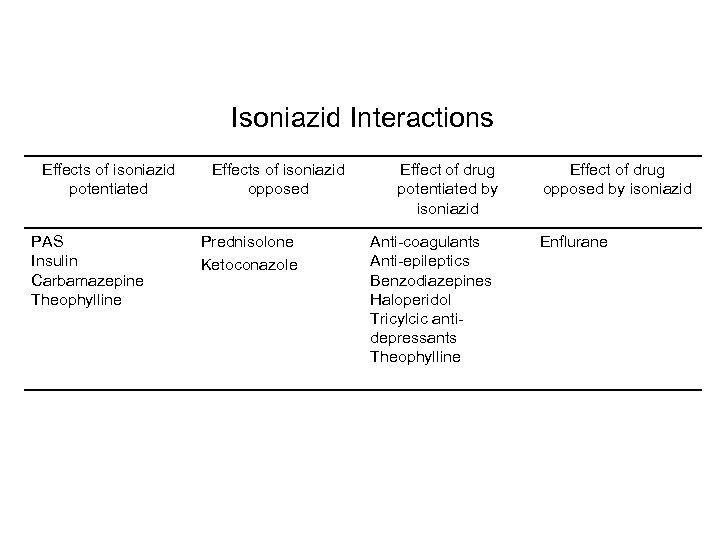
Isoniazid Interactions Effects of isoniazid potentiated PAS Insulin Carbamazepine Theophylline Effects of isoniazid opposed Prednisolone Ketoconazole Effect of drug potentiated by isoniazid Anti-coagulants Anti-epileptics Benzodiazepines Haloperidol Tricylcic antidepressants Theophylline Effect of drug opposed by isoniazid Enflurane
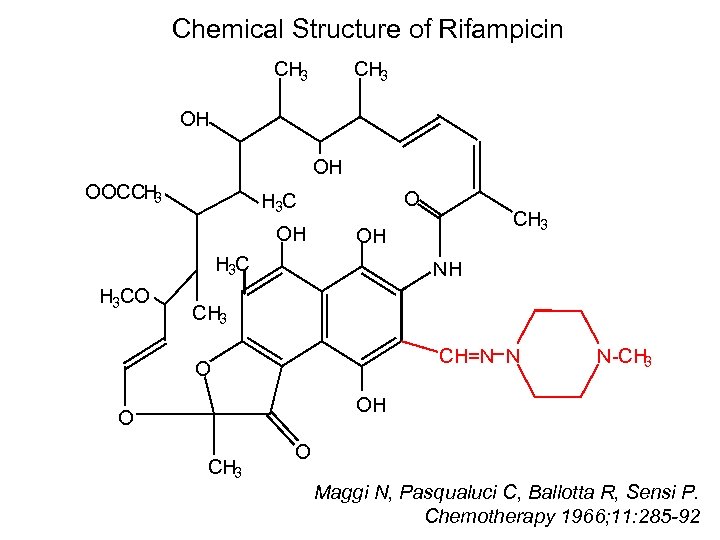
Chemical Structure of Rifampicin CH 3 OH OH OOCCH 3 O H 3 C OH OH H 3 CO CH 3 NH CH 3 CH=N N O N-CH 3 OH O CH 3 O Maggi N, Pasqualuci C, Ballotta R, Sensi P. Chemotherapy 1966; 11: 285 -92
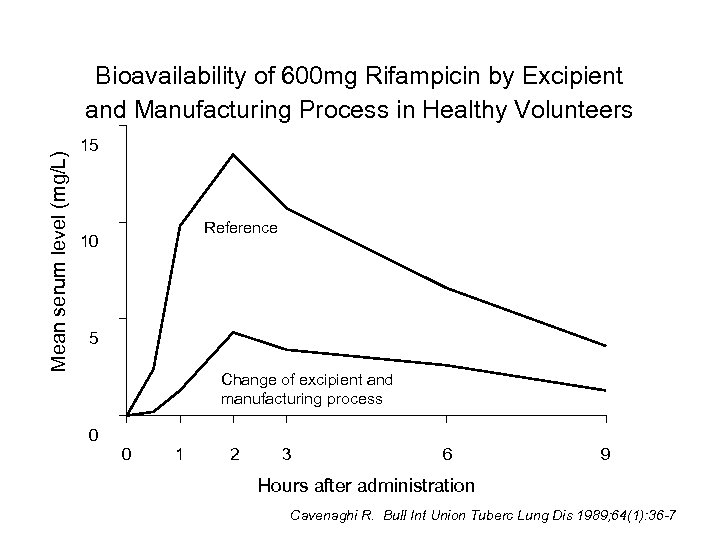
Mean serum level (mg/L) Bioavailability of 600 mg Rifampicin by Excipient and Manufacturing Process in Healthy Volunteers 15 Reference 10 5 Change of excipient and manufacturing process 0 0 1 2 3 6 9 Hours after administration Cavenaghi R. Bull Int Union Tuberc Lung Dis 1989; 64(1): 36 -7





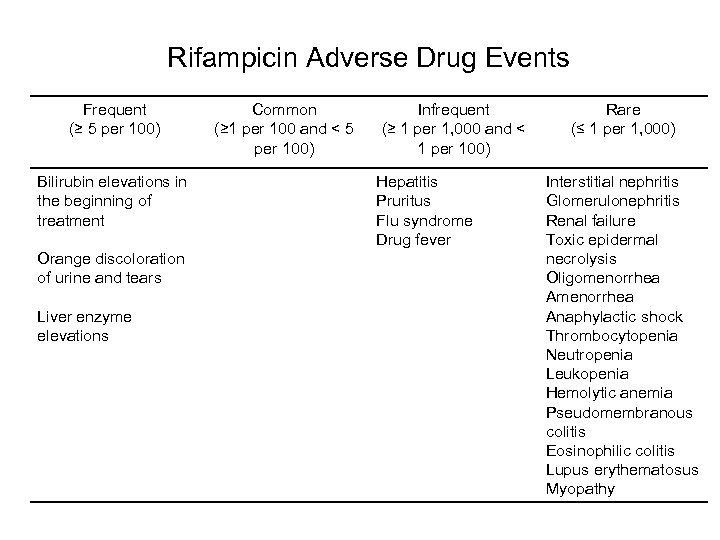
Rifampicin Adverse Drug Events Frequent (≥ 5 per 100) Bilirubin elevations in the beginning of treatment Orange discoloration of urine and tears Liver enzyme elevations Common (≥ 1 per 100 and < 5 per 100) Infrequent (≥ 1 per 1, 000 and < 1 per 100) Hepatitis Pruritus Flu syndrome Drug fever Rare (≤ 1 per 1, 000) Interstitial nephritis Glomerulonephritis Renal failure Toxic epidermal necrolysis Oligomenorrhea Anaphylactic shock Thrombocytopenia Neutropenia Leukopenia Hemolytic anemia Pseudomembranous colitis Eosinophilic colitis Lupus erythematosus Myopathy
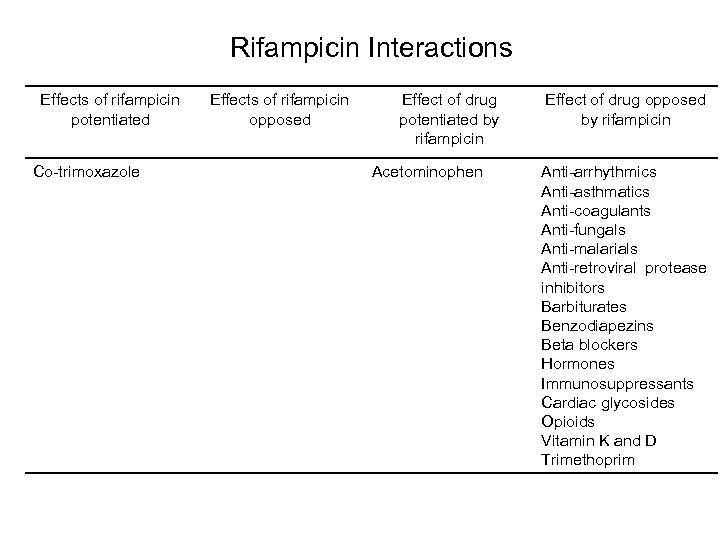
Rifampicin Interactions Effects of rifampicin potentiated Co-trimoxazole Effects of rifampicin opposed Effect of drug potentiated by rifampicin Acetominophen Effect of drug opposed by rifampicin Anti-arrhythmics Anti-asthmatics Anti-coagulants Anti-fungals Anti-malarials Anti-retroviral protease inhibitors Barbiturates Benzodiapezins Beta blockers Hormones Immunosuppressants Cardiac glycosides Opioids Vitamin K and D Trimethoprim
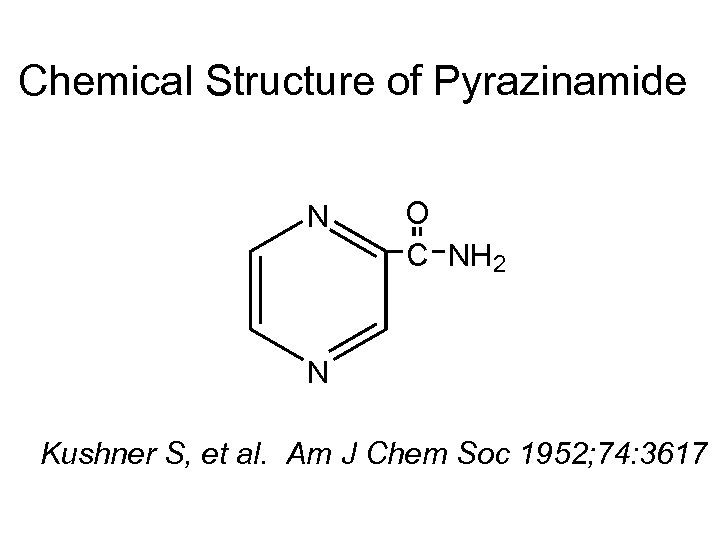
Chemical Structure of Pyrazinamide N O C NH 2 N Kushner S, et al. Am J Chem Soc 1952; 74: 3617

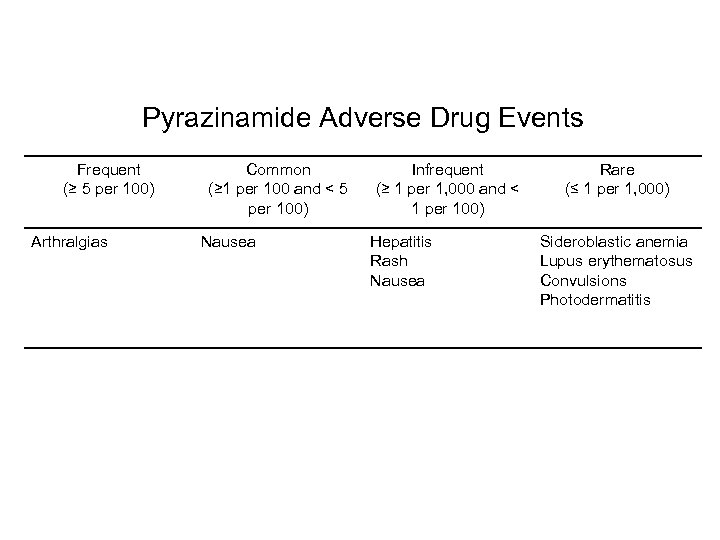
Pyrazinamide Adverse Drug Events Frequent (≥ 5 per 100) Arthralgias Common (≥ 1 per 100 and < 5 per 100) Nausea Infrequent (≥ 1 per 1, 000 and < 1 per 100) Hepatitis Rash Nausea Rare (≤ 1 per 1, 000) Sideroblastic anemia Lupus erythematosus Convulsions Photodermatitis
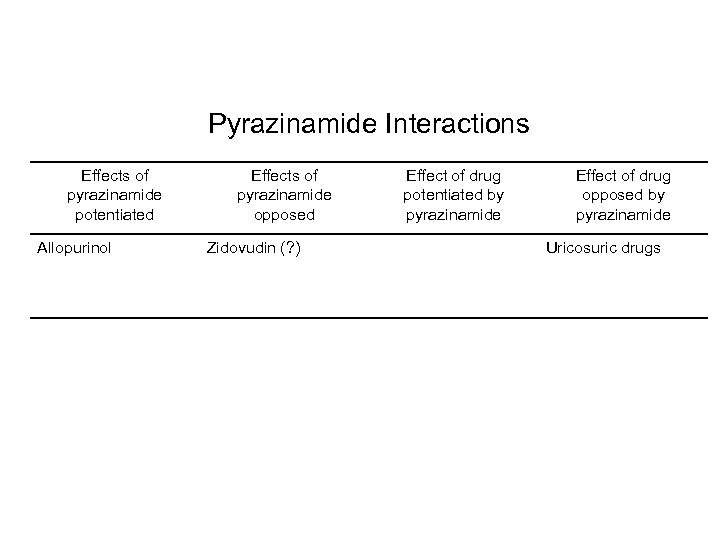
Pyrazinamide Interactions Effects of pyrazinamide potentiated Allopurinol Effects of pyrazinamide opposed Zidovudin (? ) Effect of drug potentiated by pyrazinamide Effect of drug opposed by pyrazinamide Uricosuric drugs
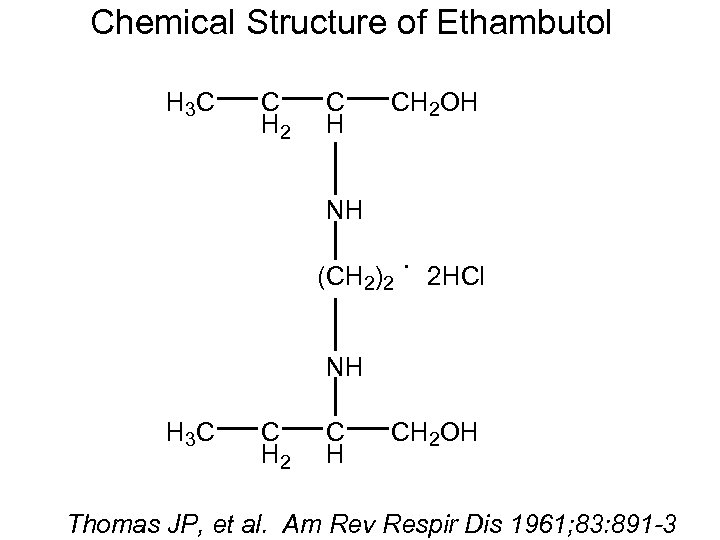
Chemical Structure of Ethambutol H 3 C C H 2 C H CH 2 OH NH (CH 2)2 . 2 HCl NH H 3 C C H 2 C H CH 2 OH Thomas JP, et al. Am Rev Respir Dis 1961; 83: 891 -3

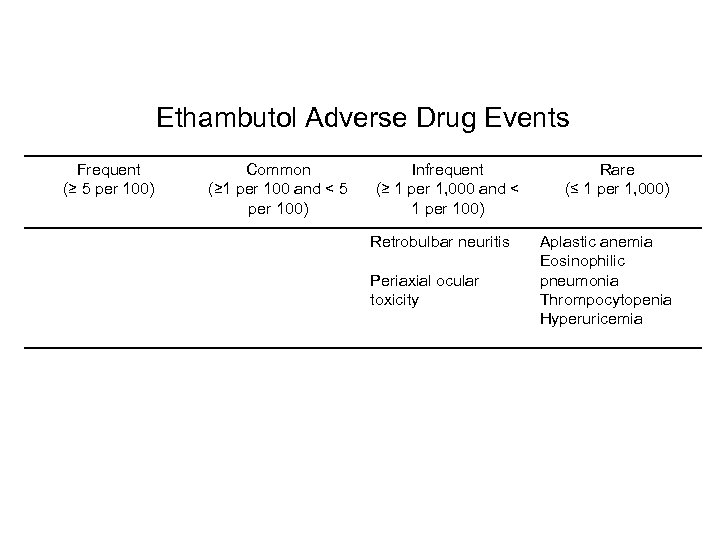
Ethambutol Adverse Drug Events Frequent (≥ 5 per 100) Common (≥ 1 per 100 and < 5 per 100) Infrequent (≥ 1 per 1, 000 and < 1 per 100) Retrobulbar neuritis Periaxial ocular toxicity Rare (≤ 1 per 1, 000) Aplastic anemia Eosinophilic pneumonia Thrompocytopenia Hyperuricemia
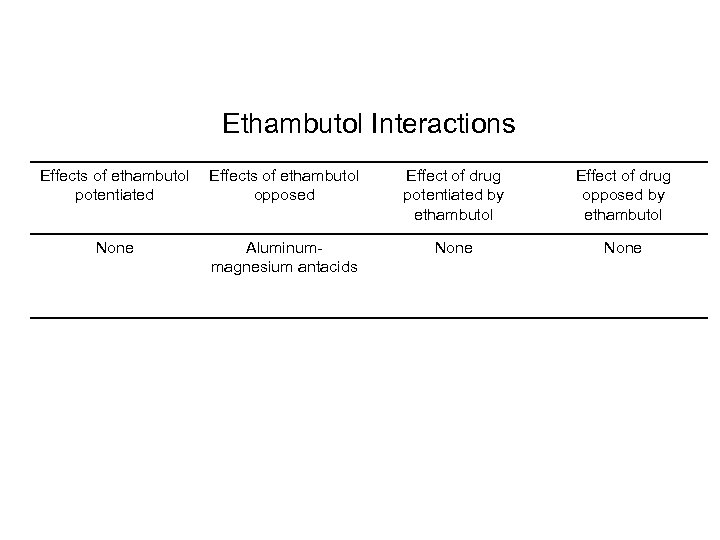
Ethambutol Interactions Effects of ethambutol potentiated Effects of ethambutol opposed Effect of drug potentiated by ethambutol Effect of drug opposed by ethambutol None Aluminummagnesium antacids None
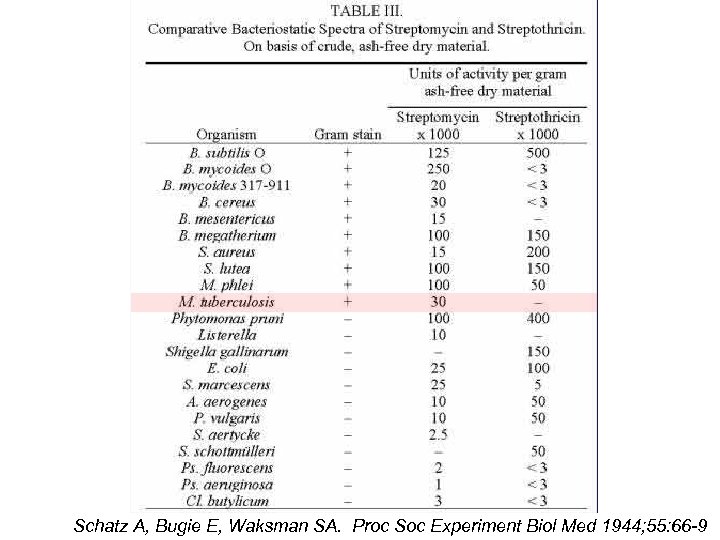
Schatz A, Bugie E, Waksman SA. Proc Soc Experiment Biol Med 1944; 55: 66 -9
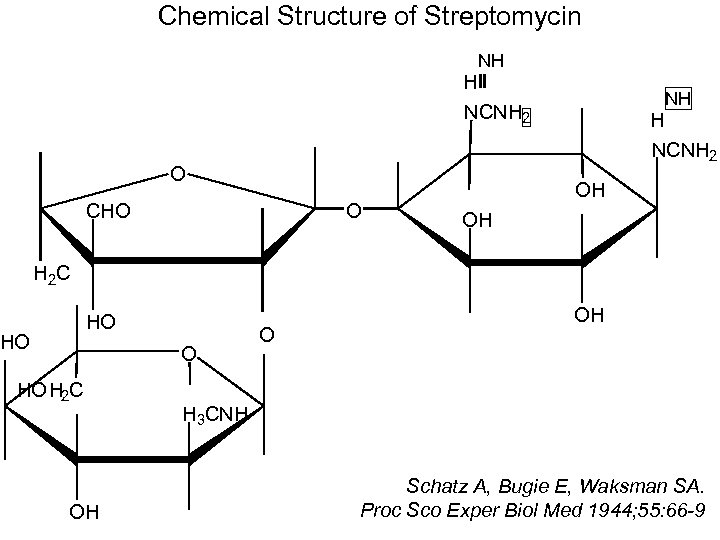
Chemical Structure of Streptomycin NH H NCNH 2 O CHO O NH H NCNH 2 OH OH H 2 C HO HO H 2 C OH O OH H 3 CNH Schatz A, Bugie E, Waksman SA. Proc Sco Exper Biol Med 1944; 55: 66 -9
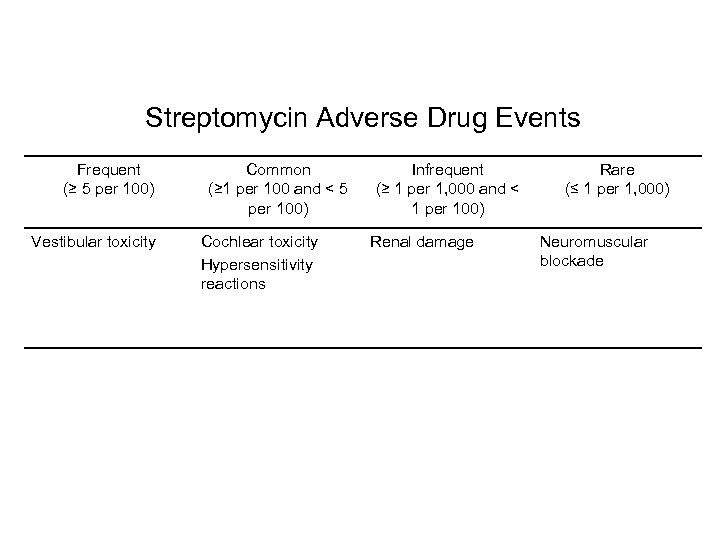
Streptomycin Adverse Drug Events Frequent (≥ 5 per 100) Vestibular toxicity Common (≥ 1 per 100 and < 5 per 100) Cochlear toxicity Hypersensitivity reactions Infrequent (≥ 1 per 1, 000 and < 1 per 100) Renal damage Rare (≤ 1 per 1, 000) Neuromuscular blockade
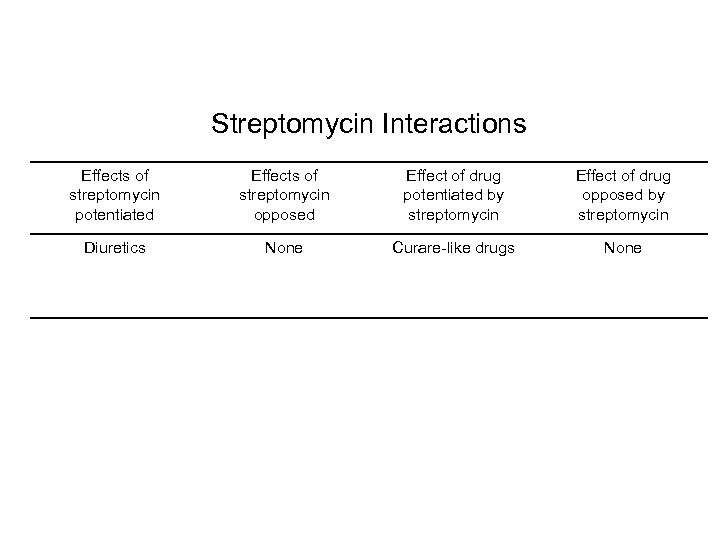
Streptomycin Interactions Effects of streptomycin potentiated Effects of streptomycin opposed Effect of drug potentiated by streptomycin Effect of drug opposed by streptomycin Diuretics None Curare-like drugs None
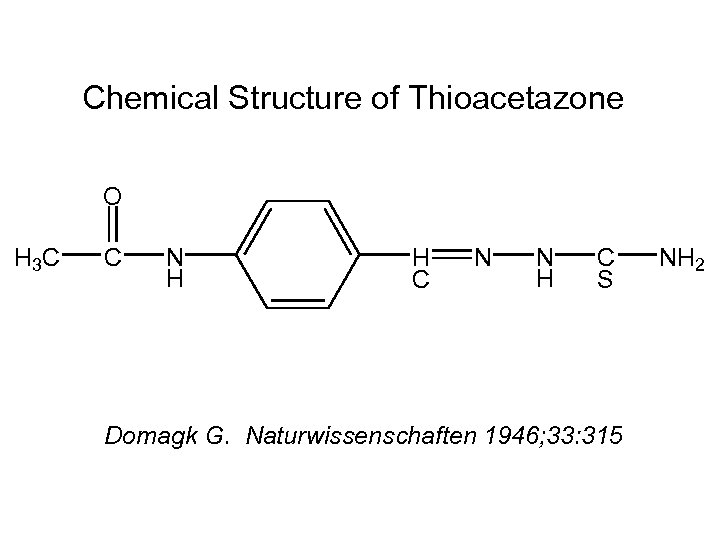
Chemical Structure of Thioacetazone O H 3 C C N H H C N N H C S Domagk G. Naturwissenschaften 1946; 33: 315 NH 2
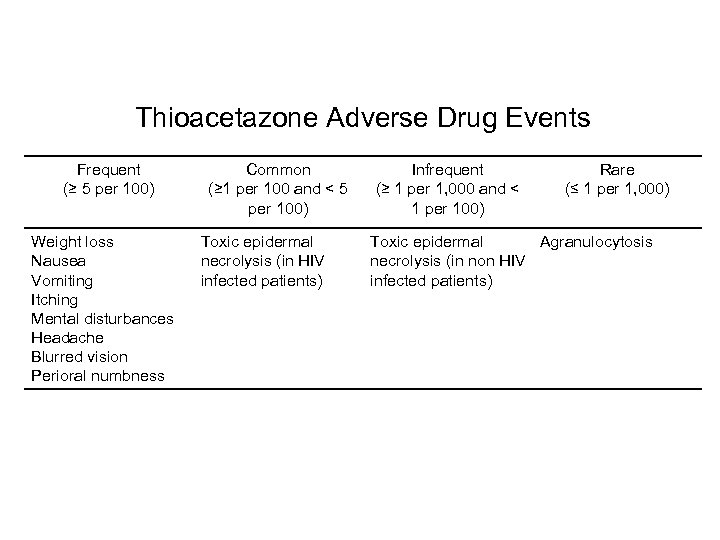
Thioacetazone Adverse Drug Events Frequent (≥ 5 per 100) Weight loss Nausea Vomiting Itching Mental disturbances Headache Blurred vision Perioral numbness Common (≥ 1 per 100 and < 5 per 100) Toxic epidermal necrolysis (in HIV infected patients) Infrequent (≥ 1 per 1, 000 and < 1 per 100) Rare (≤ 1 per 1, 000) Toxic epidermal Agranulocytosis necrolysis (in non HIV infected patients)

Tuberculosis Patient in Malawi with Thioazetazone-Associated Toxic Epidermal Necrolysis Photo courtesy: Tone Ringdal

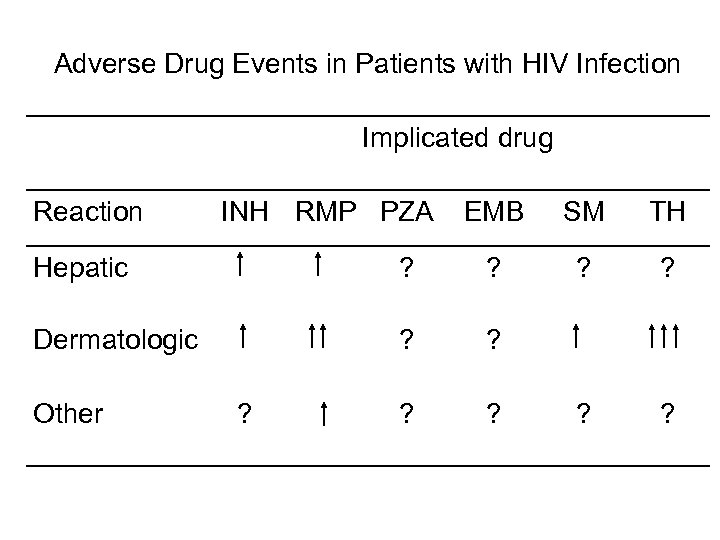
Adverse Drug Events in Patients with HIV Infection Implicated drug Reaction INH RMP PZA EMB SM TH ? ? Hepatic ? ? Dermatologic ? ? Other ?
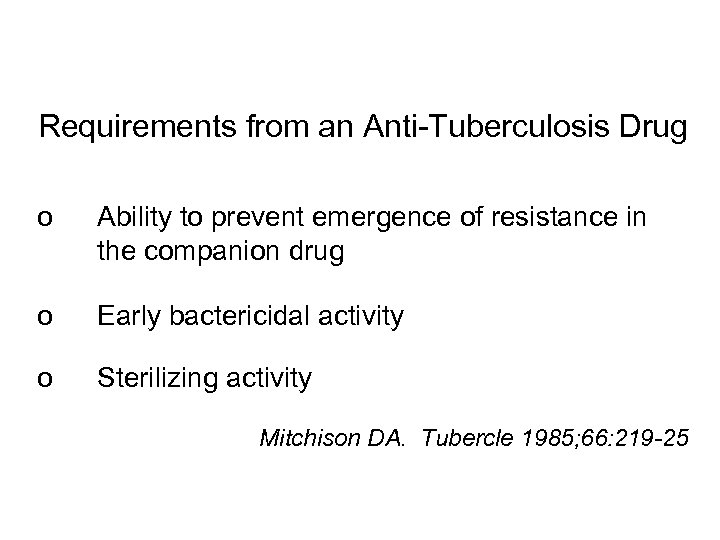
Requirements from an Anti-Tuberculosis Drug o Ability to prevent emergence of resistance in the companion drug o Early bactericidal activity o Sterilizing activity Mitchison DA. Tubercle 1985; 66: 219 -25
Hypotheses About Emergence of Anti. Tuberculosis Drug Resistance o Crude probability of selection o Differential bactericidal activity o Sub-inhibitory concentrations o Differential lag phases of drugs




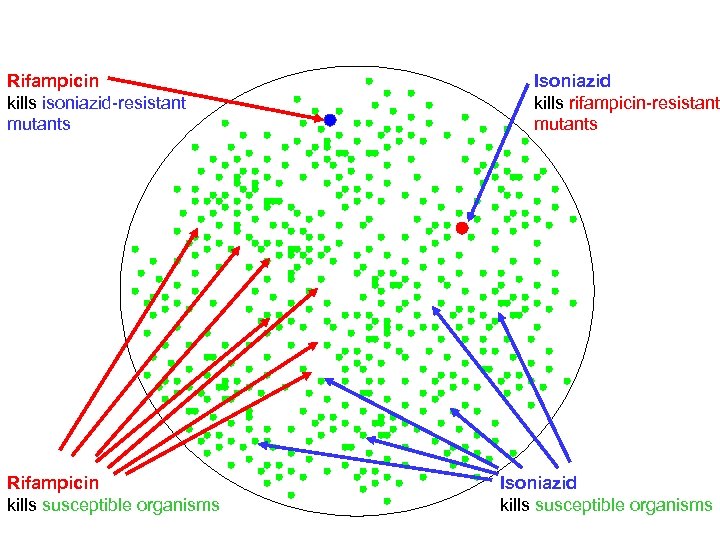
Rifampicin kills isoniazid-resistant mutants Rifampicin kills susceptible organisms Isoniazid kills rifampicin-resistant mutants Isoniazid kills susceptible organisms

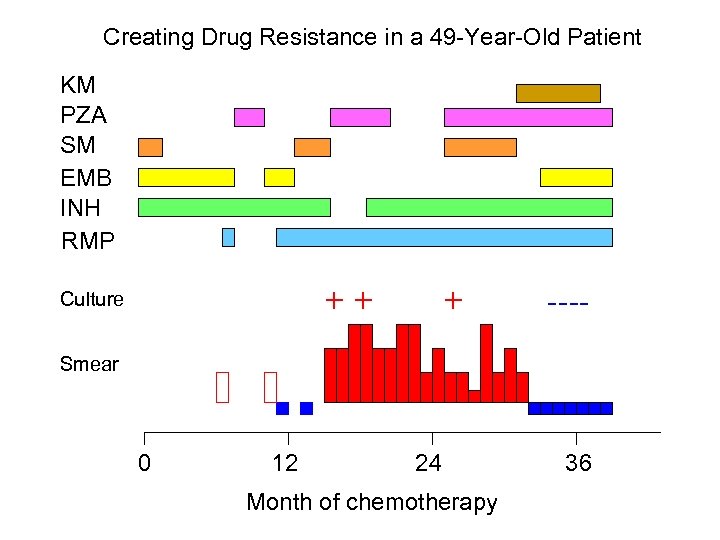
Creating Drug Resistance in a 49 -Year-Old Patient KM PZA SM EMB INH RMP ++ Culture + ---- Smear 0 12 24 Month of chemotherapy 36
Errors in Management Leading to MDR in the USA Findings Among 28 of 35 Patients with MDR o Adding a single drug to a failing regimen o Inadequate primary regimen o Failure to recognize primary or acquired resistance o Failure to recognize and deal with non-adherence o Inappropriate preventive therapy Mahmoudi A, et al. JAMA 1993; 270: 65 -8





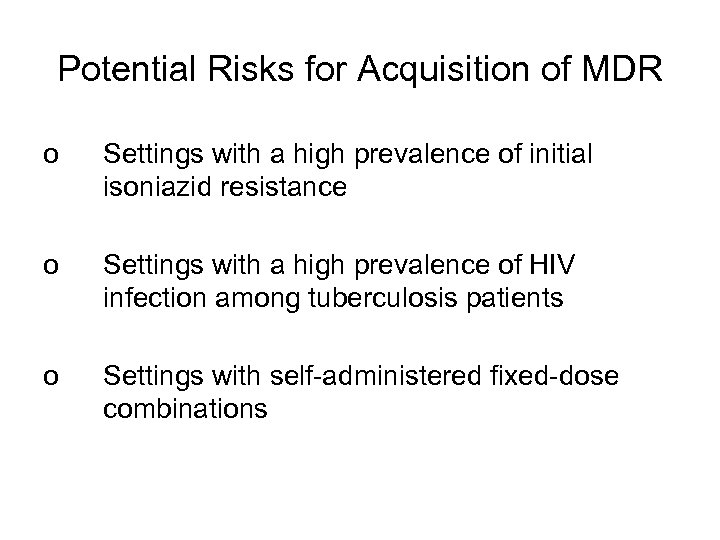
Potential Risks for Acquisition of MDR o Settings with a high prevalence of initial isoniazid resistance o Settings with a high prevalence of HIV infection among tuberculosis patients o Settings with self-administered fixed-dose combinations




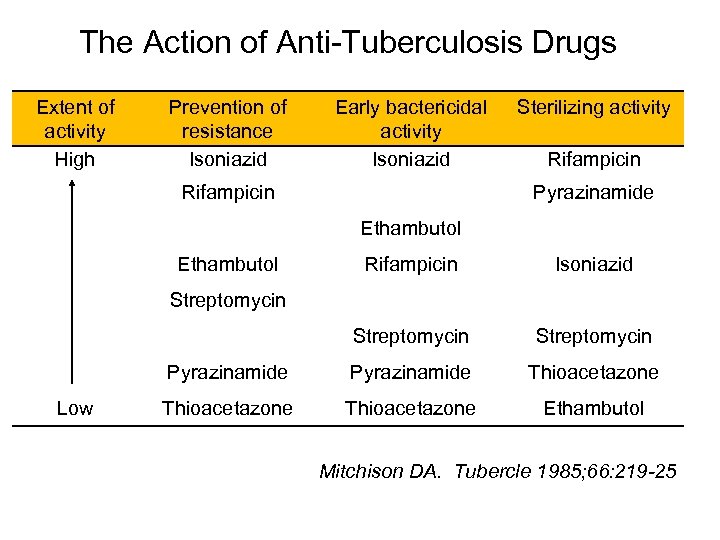
The Action of Anti-Tuberculosis Drugs Extent of activity High Prevention of resistance Isoniazid Early bactericidal activity Isoniazid Rifampicin Sterilizing activity Rifampicin Pyrazinamide Ethambutol Rifampicin Isoniazid Streptomycin Pyrazinamide Thioacetazone Ethambutol Streptomycin Low Mitchison DA. Tubercle 1985; 66: 219 -25


1954 2004

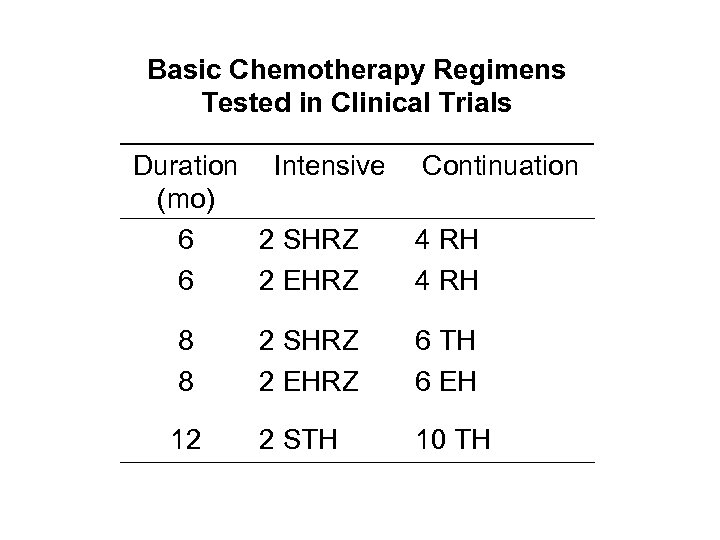
Basic Chemotherapy Regimens Tested in Clinical Trials Duration Intensive (mo) 6 2 SHRZ 6 2 EHRZ Continuation 4 RH 8 8 2 SHRZ 2 EHRZ 6 TH 6 EH 12 2 STH 10 TH
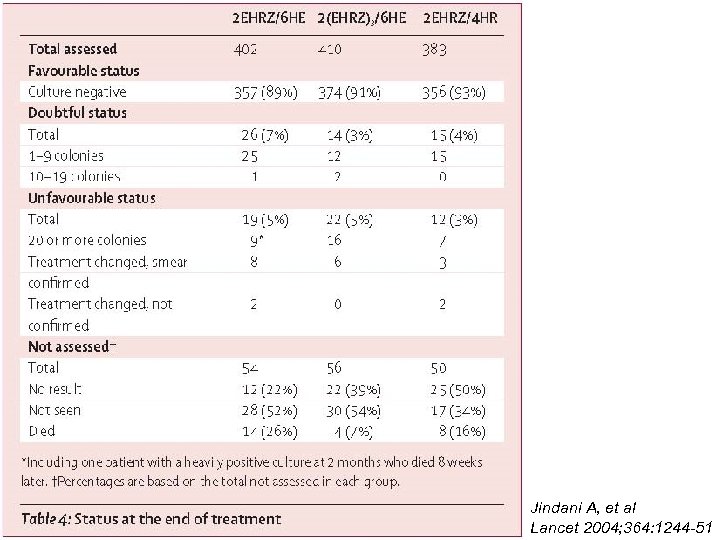
Jindani A, et al Lancet 2004; 364: 1244 -51
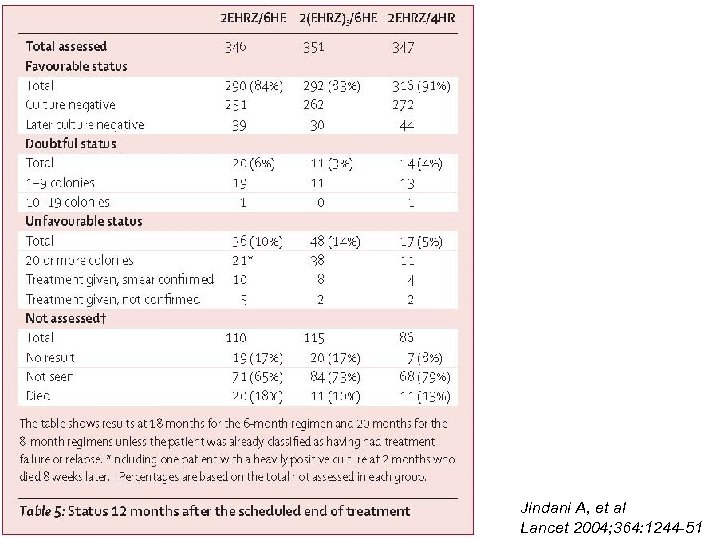
Jindani A, et al Lancet 2004; 364: 1244 -51


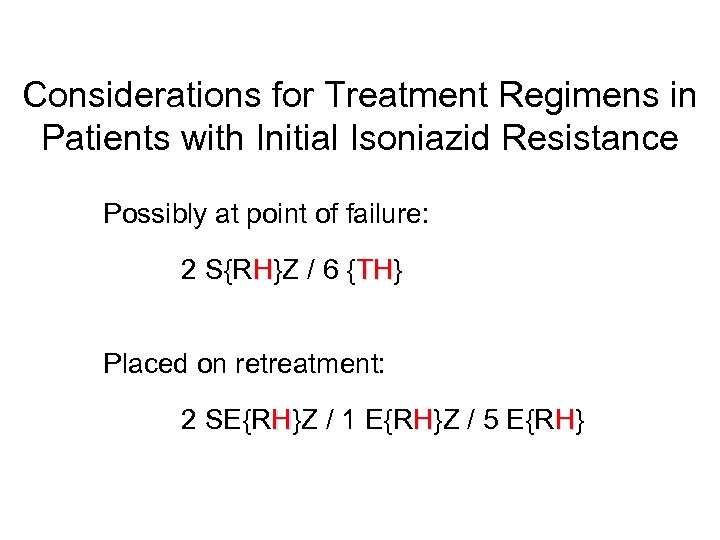
Considerations for Treatment Regimens in Patients with Initial Isoniazid Resistance Possibly at point of failure: 2 S{RH}Z / 6 {TH} TH Placed on retreatment: 2 SE{RH}Z / 1 E{RH}Z / 5 E{RH}
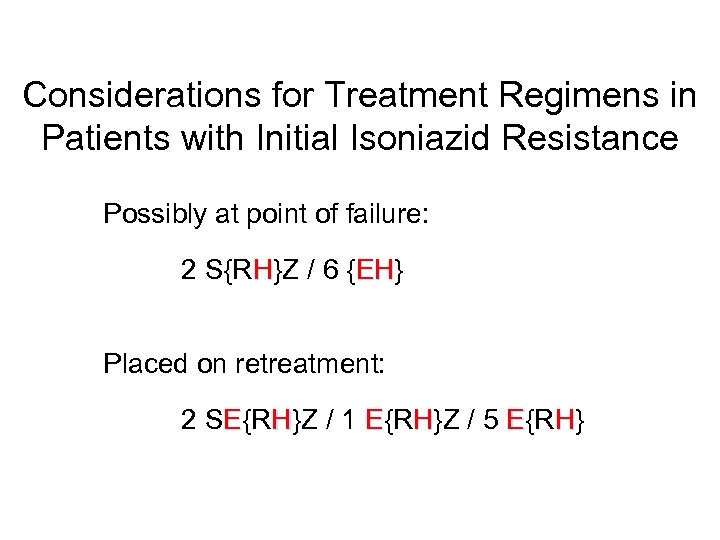
Considerations for Treatment Regimens in Patients with Initial Isoniazid Resistance Possibly at point of failure: 2 S{RH}Z / 6 {EH} EH Placed on retreatment: 2 SE{RH}Z / 1 E{RH}Z / 5 E{RH}
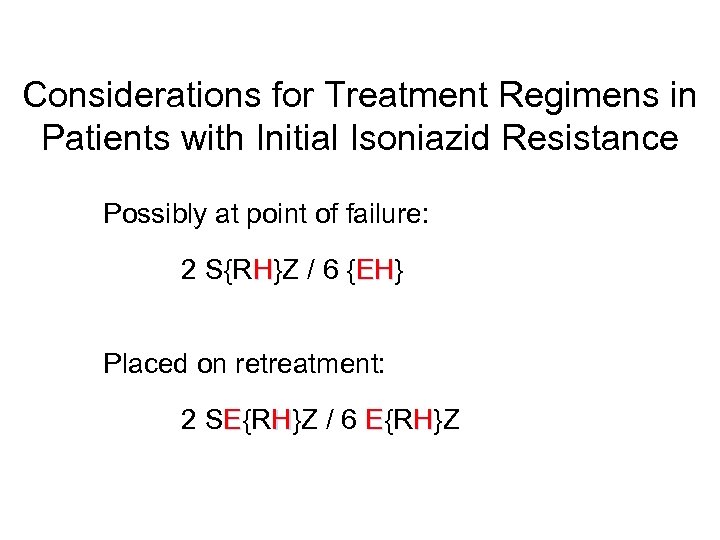
Considerations for Treatment Regimens in Patients with Initial Isoniazid Resistance Possibly at point of failure: 2 S{RH}Z / 6 {EH} EH Placed on retreatment: 2 SE{RH}Z / 6 E{RH}Z
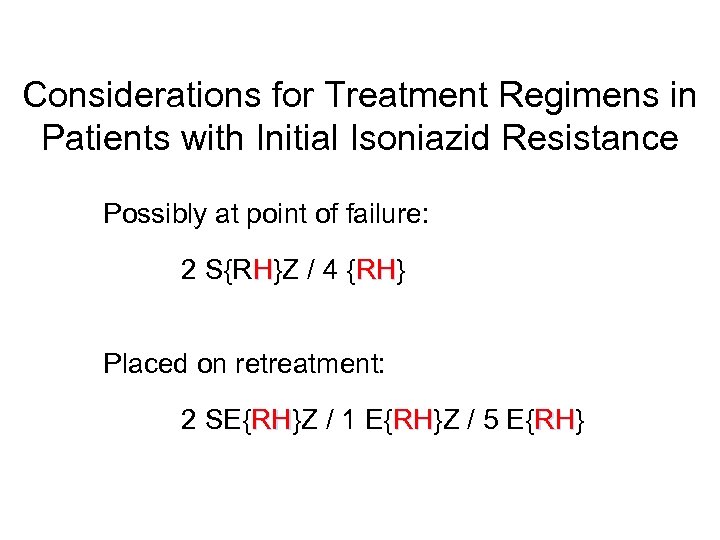
Considerations for Treatment Regimens in Patients with Initial Isoniazid Resistance Possibly at point of failure: 2 S{RH}Z / 4 {RH} RH Placed on retreatment: 2 SE{RH}Z / 1 E{RH}Z / 5 E{RH} RH RH RH

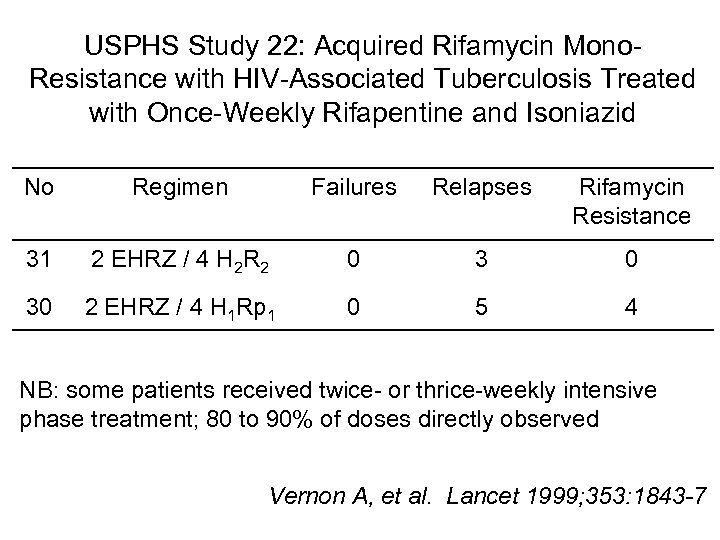
USPHS Study 22: Acquired Rifamycin Mono. Resistance with HIV-Associated Tuberculosis Treated with Once-Weekly Rifapentine and Isoniazid No Regimen Failures Relapses Rifamycin Resistance 31 2 EHRZ / 4 H 2 R 2 0 30 2 EHRZ / 4 H 1 Rp 1 0 5 4 NB: some patients received twice- or thrice-weekly intensive phase treatment; 80 to 90% of doses directly observed Vernon A, et al. Lancet 1999; 353: 1843 -7

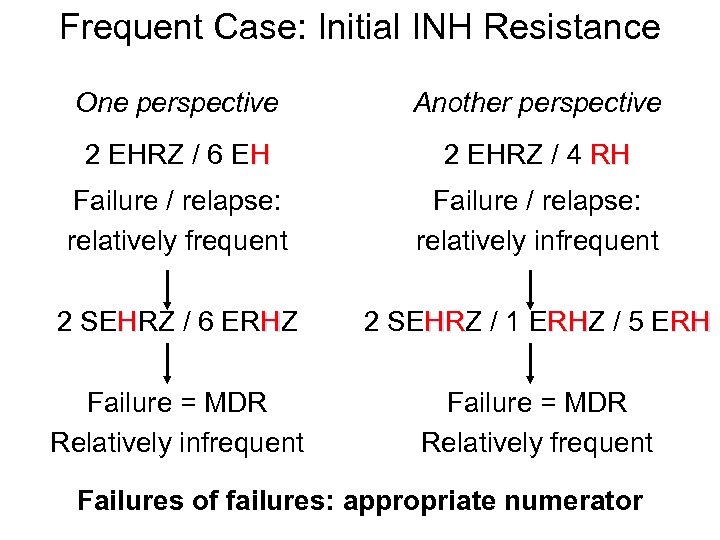
Frequent Case: Initial INH Resistance One perspective Another perspective 2 EHRZ / 6 EH 2 EHRZ / 4 RH Failure / relapse: relatively frequent Failure / relapse: relatively infrequent 2 SEHRZ / 6 ERHZ 2 SEHRZ / 1 ERHZ / 5 ERH HR RH Failure = MDR Relatively infrequent Failure = MDR Relatively frequent Failures of failures: appropriate numerator
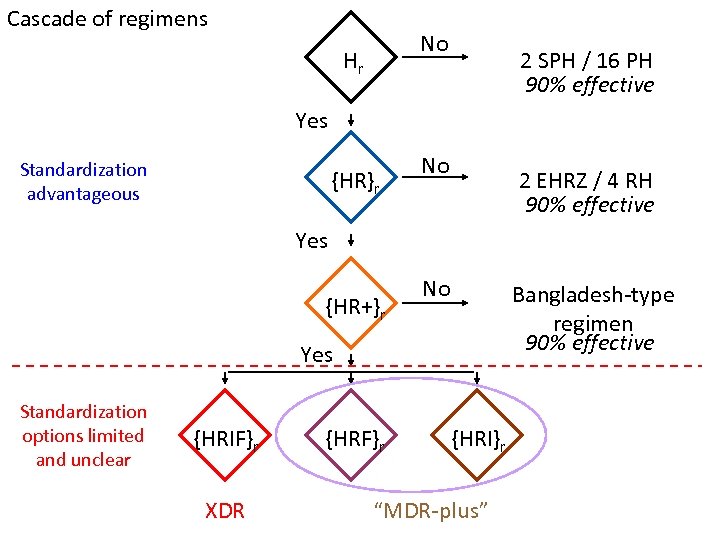
Cascade of regimens No Hr 2 SPH / 16 PH 90% effective Yes Standardization advantageous {HR}r No 2 EHRZ / 4 RH 90% effective Yes {HR+}r No Bangladesh-type regimen 90% effective Yes Standardization options limited and unclear {HRIF}r XDR {HRF}r {HRI}r “MDR-plus”
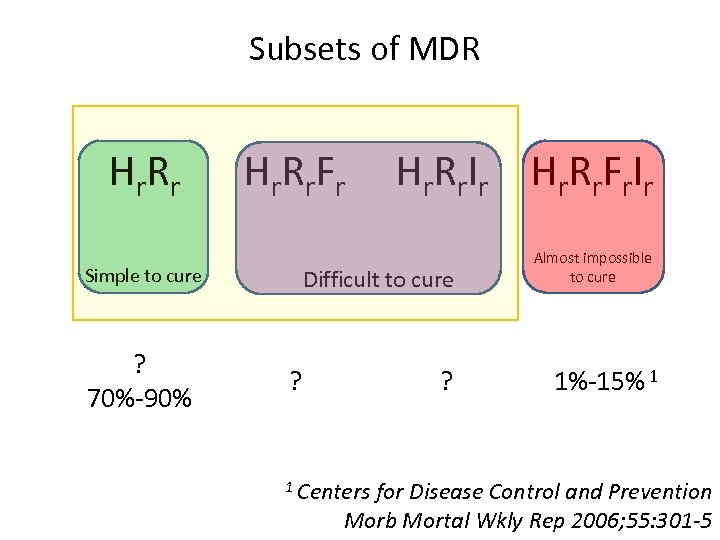
Subsets of MDR Hr R r F r Simple to cure ? 70%-90% Hr R r I r Hr R r F r I r Difficult to cure ? ? 1 Centers Almost impossible to cure 1%-15% 1 for Disease Control and Prevention Morb Mortal Wkly Rep 2006; 55: 301 -5

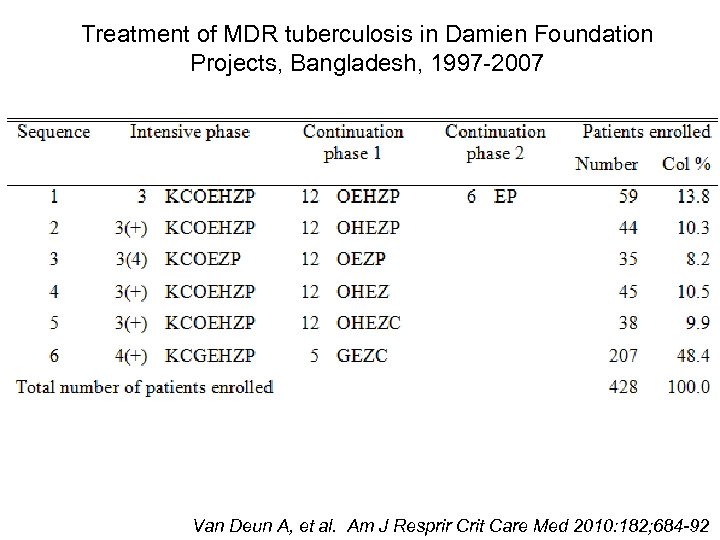
Treatment of MDR tuberculosis in Damien Foundation Projects, Bangladesh, 1997 -2007 Van Deun A, et al. Am J Resprir Crit Care Med 2010: 182; 684 -92
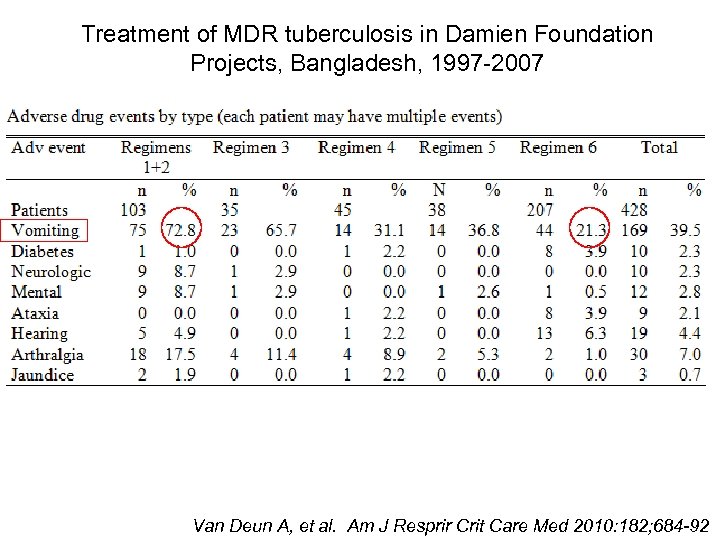
Treatment of MDR tuberculosis in Damien Foundation Projects, Bangladesh, 1997 -2007 Van Deun A, et al. Am J Resprir Crit Care Med 2010: 182; 684 -92
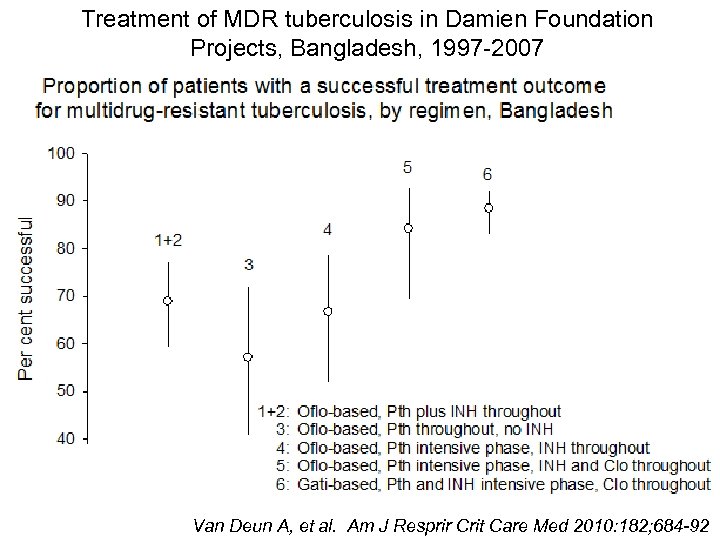
Treatment of MDR tuberculosis in Damien Foundation Projects, Bangladesh, 1997 -2007 Van Deun A, et al. Am J Resprir Crit Care Med 2010: 182; 684 -92
Van Deun A, et al. Am J Resprir Crit Care Med 2010: 182; 684 -92
Van Deun A, et al. Am J Resprir Crit Care Med 2010: 182; 684 -92
Van Deun A, et al. Am J Resprir Crit Care Med 2010: 182; 684 -92
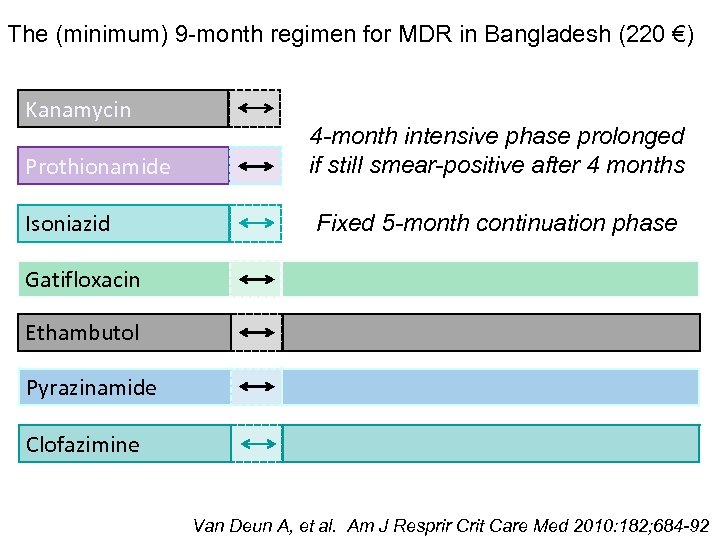
The (minimum) 9 -month regimen for MDR in Bangladesh (220 €) Kanamycin Prothionamide Isoniazid 4 -month intensive phase prolonged if still smear-positive after 4 months Fixed 5 -month continuation phase Gatifloxacin Ethambutol Pyrazinamide Clofazimine Van Deun A, et al. Am J Resprir Crit Care Med 2010: 182; 684 -92

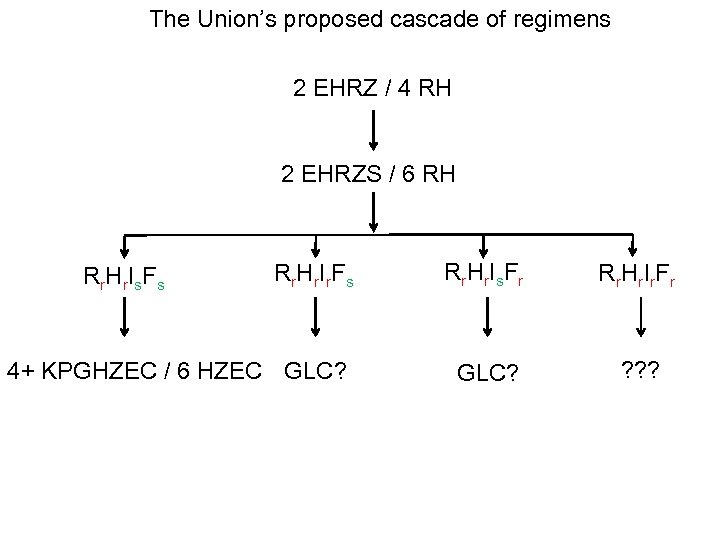
The Union’s proposed cascade of regimens 2 EHRZ / 4 RH 2 EHRZS / 6 RH R r. H r. I r. F s Rr. Hr. Is. Fr R r. H r. I r. F r 4+ KPGHZEC / 6 HZEC GLC? ? ? ? Rr. Hr. Is. Fs
Prophylactic Treatment (Or perhaps better: primary prophylaxis)
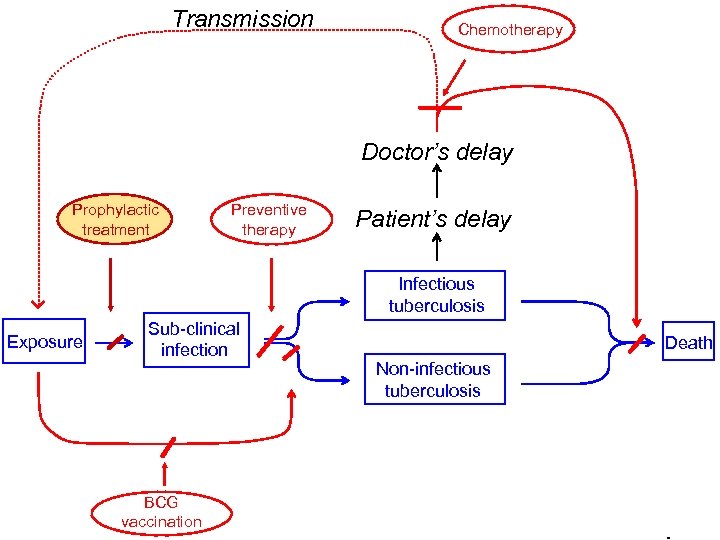
Transmission Chemotherapy Doctor’s delay Prophylactic treatment Preventive therapy Patient’s delay Infectious tuberculosis Exposure Sub-clinical infection BCG vaccination Death Non-infectious tuberculosis

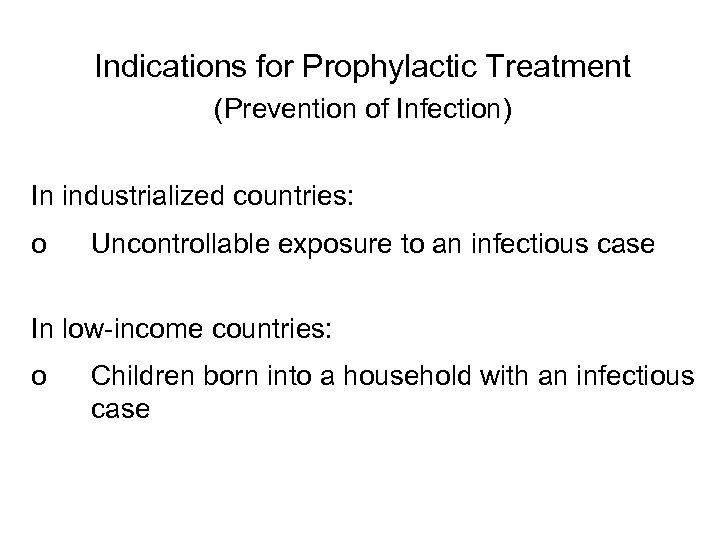
Indications for Prophylactic Treatment (Prevention of Infection) In industrialized countries: o Uncontrollable exposure to an infectious case In low-income countries: o Children born into a household with an infectious case
Vaccination
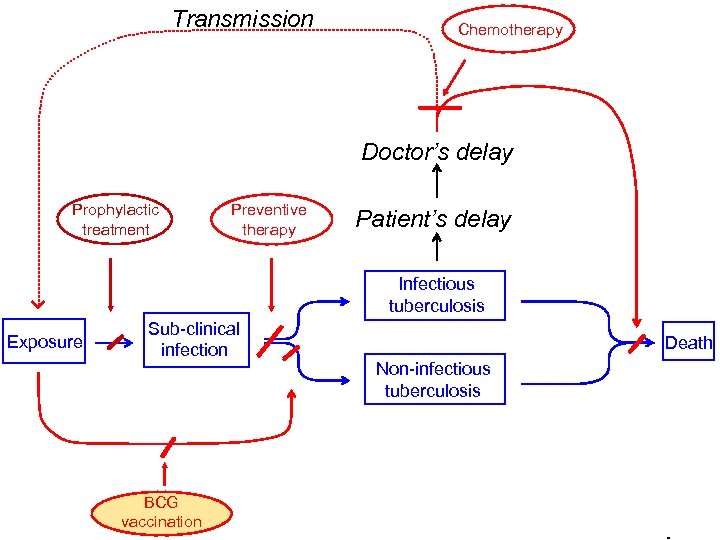
Transmission Chemotherapy Doctor’s delay Prophylactic treatment Preventive therapy Patient’s delay Infectious tuberculosis Exposure Sub-clinical infection BCG vaccination Death Non-infectious tuberculosis
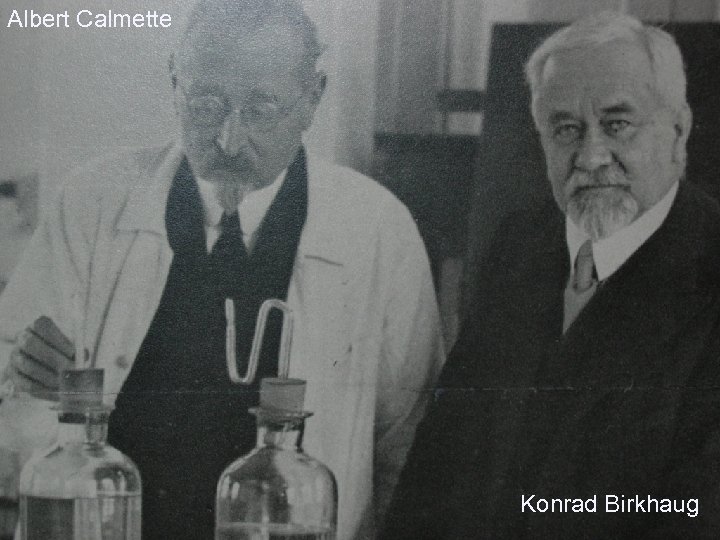
Albert Calmette Konrad Birkhaug
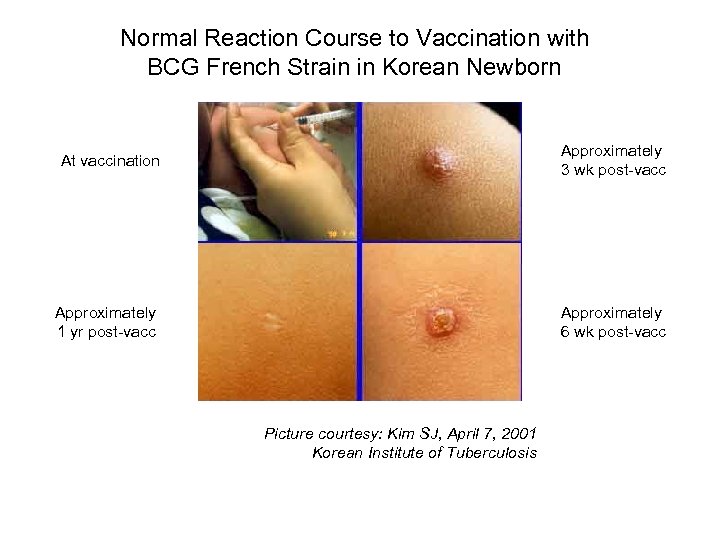
Normal Reaction Course to Vaccination with BCG French Strain in Korean Newborn At vaccination Approximately 3 wk post-vacc Approximately 1 yr post-vacc Approximately 6 wk post-vacc Picture courtesy: Kim SJ, April 7, 2001 Korean Institute of Tuberculosis
Protection from BCG Vaccination o Protection against dissemination, meningitis, and death o Protection of infants against any form o Protection of children other than infants o Protection of adults
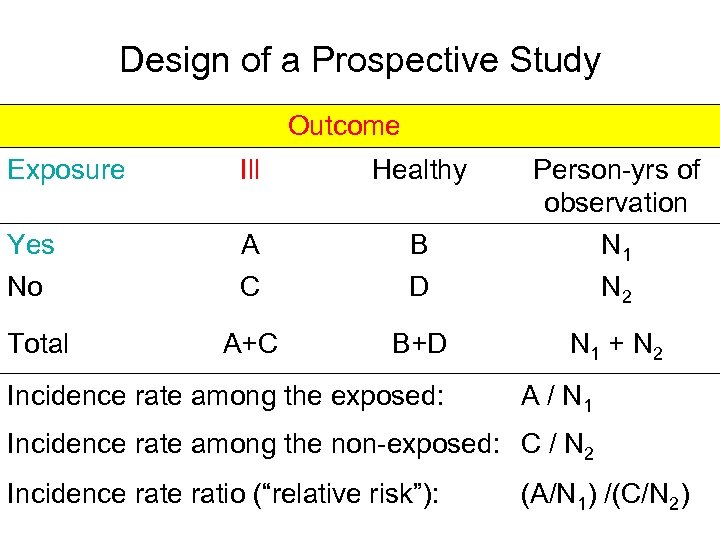
Design of a Prospective Study Outcome Exposure Ill Healthy Yes No A C B D Person-yrs of observation N 1 N 2 Total A+C B+D N 1 + N 2 Incidence rate among the exposed: A / N 1 Incidence rate among the non-exposed: C / N 2 Incidence ratio (“relative risk”): (A/N 1) /(C/N 2)
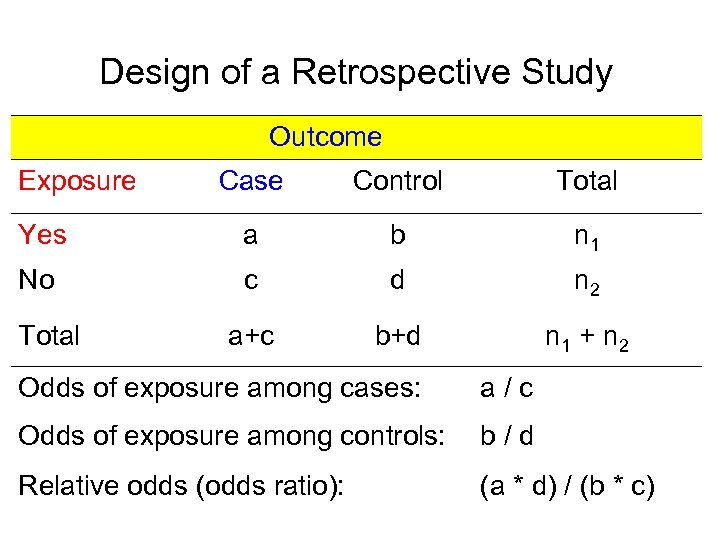
Design of a Retrospective Study Outcome Exposure Case Control Total Yes a b n 1 No c d n 2 a+c b+d n 1 + n 2 Total Odds of exposure among cases: a/c Odds of exposure among controls: b/d Relative odds (odds ratio): (a * d) / (b * c)













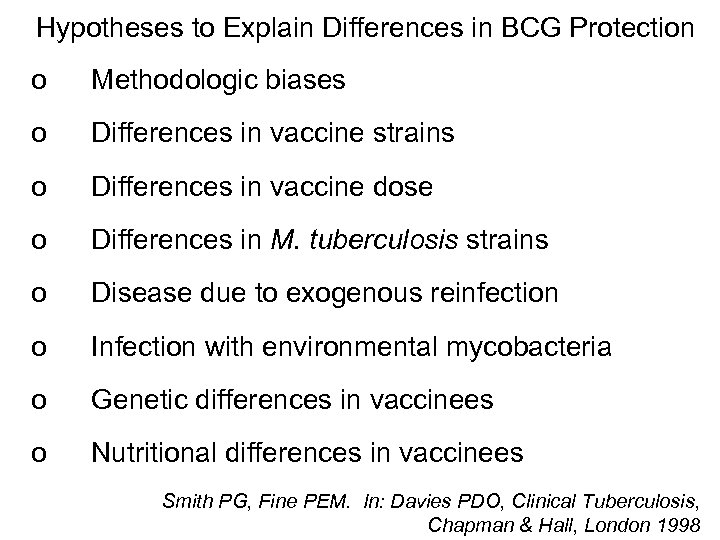
Hypotheses to Explain Differences in BCG Protection o Methodologic biases o Differences in vaccine strains o Differences in vaccine dose o Differences in M. tuberculosis strains o Disease due to exogenous reinfection o Infection with environmental mycobacteria o Genetic differences in vaccinees o Nutritional differences in vaccinees Smith PG, Fine PEM. In: Davies PDO, Clinical Tuberculosis, Chapman & Hall, London 1998

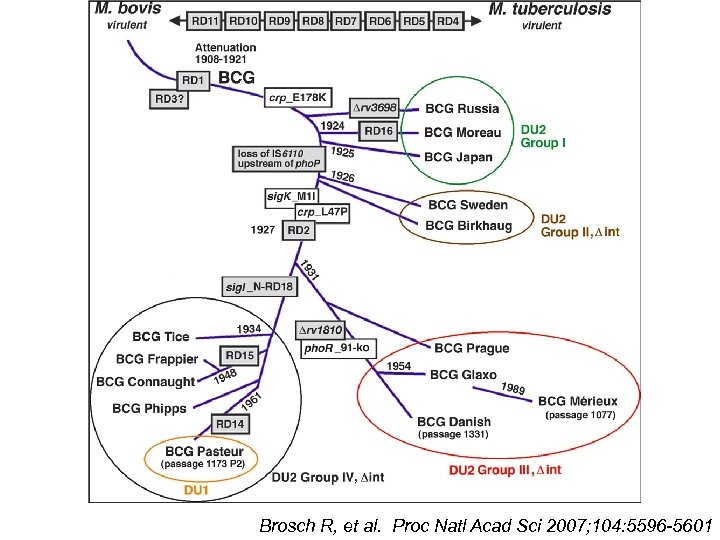
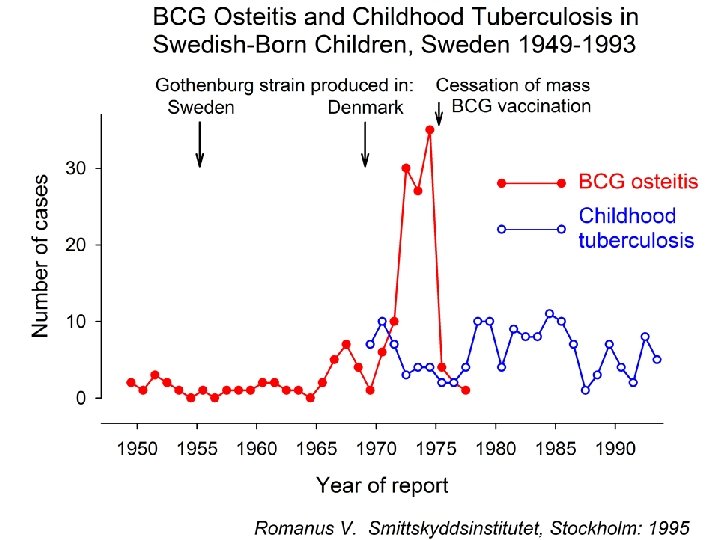
Brosch R, et al. Proc Natl Acad Sci 2007; 104: 5596 -5601





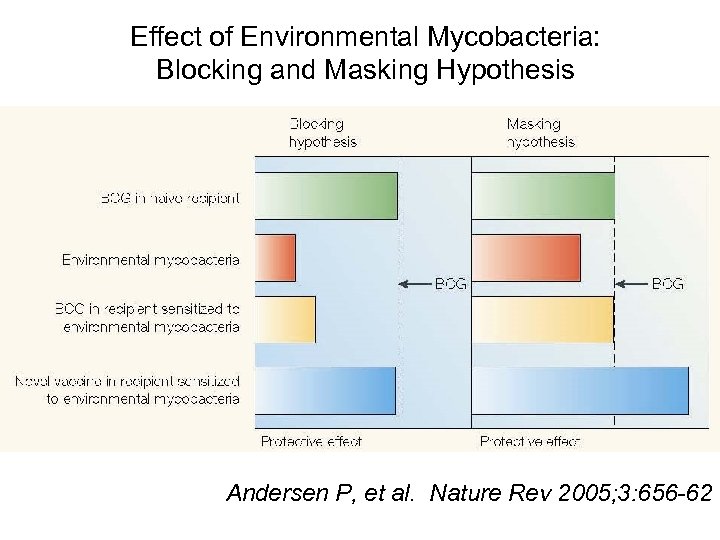
Effect of Environmental Mycobacteria: Blocking and Masking Hypothesis Andersen P, et al. Nature Rev 2005; 3: 656 -62

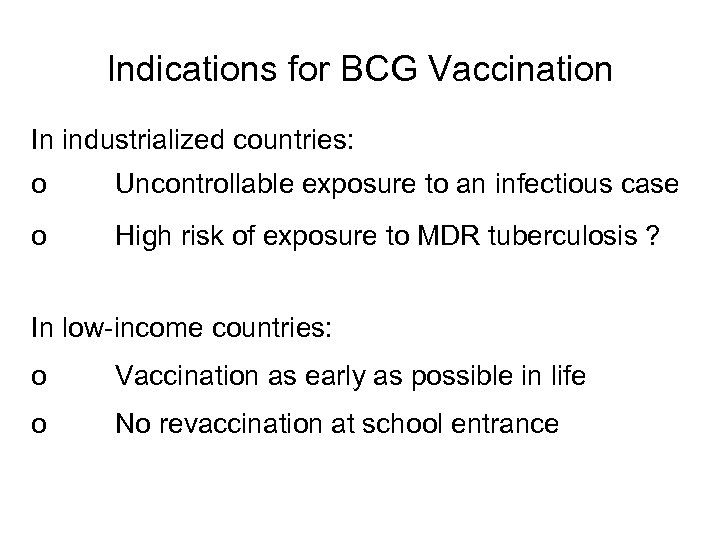
Indications for BCG Vaccination In industrialized countries: o Uncontrollable exposure to an infectious case o High risk of exposure to MDR tuberculosis ? In low-income countries: o Vaccination as early as possible in life o No revaccination at school entrance
Preventive Therapy (Or perhaps better: secondary prophylaxis)
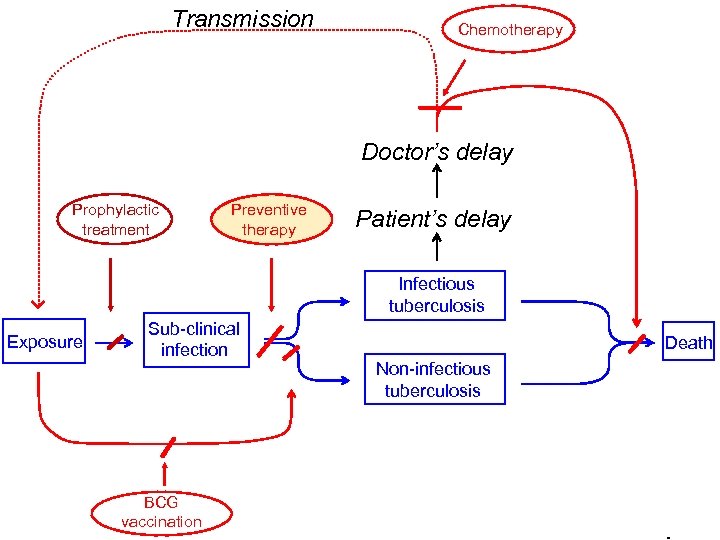
Transmission Chemotherapy Doctor’s delay Prophylactic treatment Preventive therapy Patient’s delay Infectious tuberculosis Exposure Sub-clinical infection BCG vaccination Death Non-infectious tuberculosis


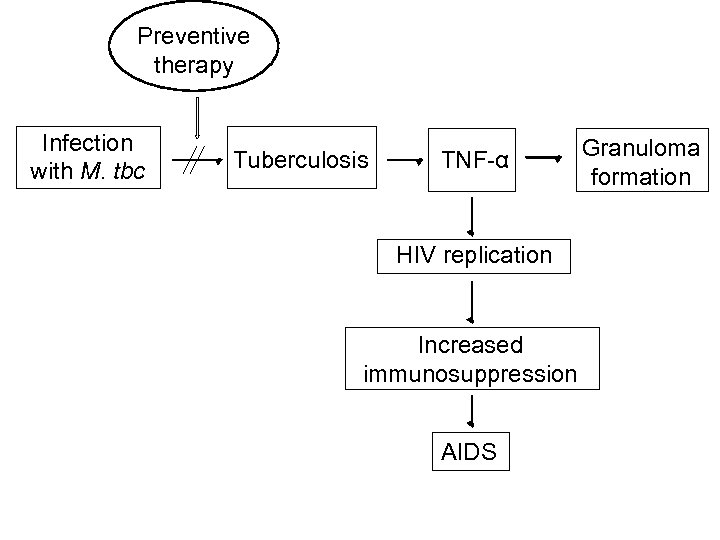
Preventive therapy Infection with M. tbc Tuberculosis TNF-α HIV replication Increased immunosuppression AIDS Granuloma formation




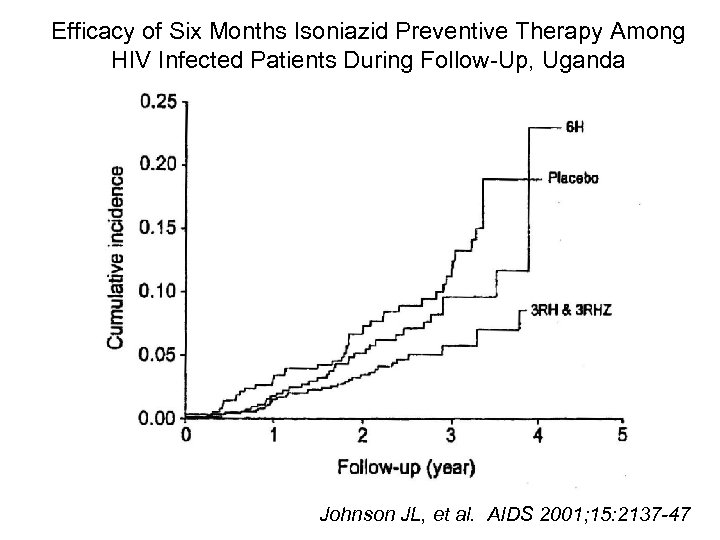
Efficacy of Six Months Isoniazid Preventive Therapy Among HIV Infected Patients During Follow-Up, Uganda Johnson JL, et al. AIDS 2001; 15: 2137 -47


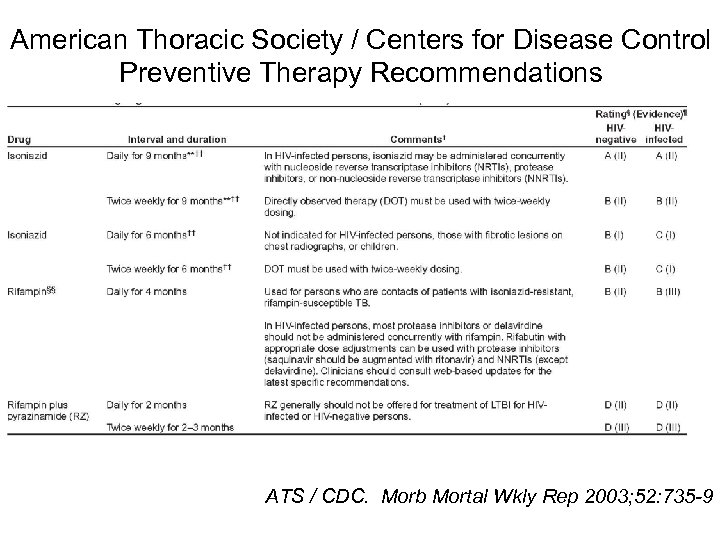
American Thoracic Society / Centers for Disease Control Preventive Therapy Recommendations ATS / CDC. Morb Mortal Wkly Rep 2003; 52: 735 -9
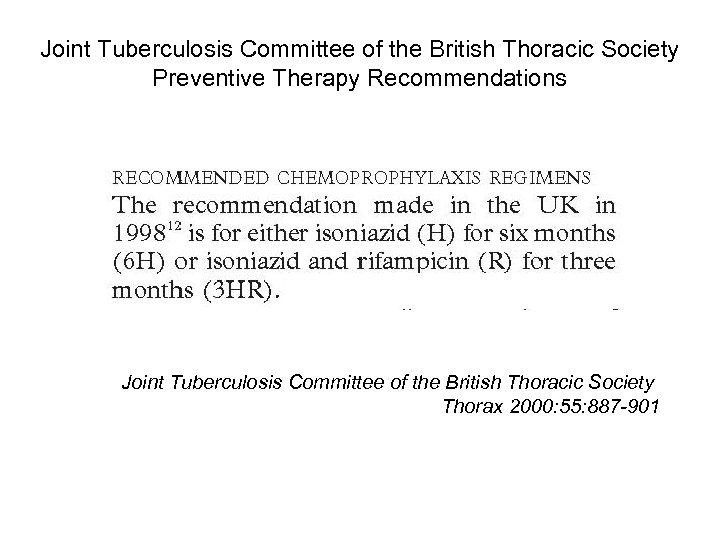
Joint Tuberculosis Committee of the British Thoracic Society Preventive Therapy Recommendations Joint Tuberculosis Committee of the British Thoracic Society Thorax 2000: 55: 887 -901
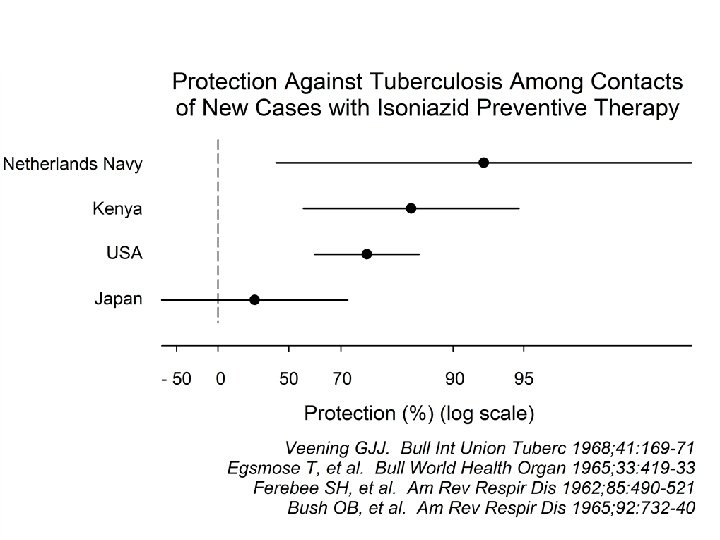
Factors Determining Effectiveness of Preventive Chemotherapy o Probability of tuberculous infection o Risk of tuberculosis given infection o Efficacy of regimen o Adherence to treatment
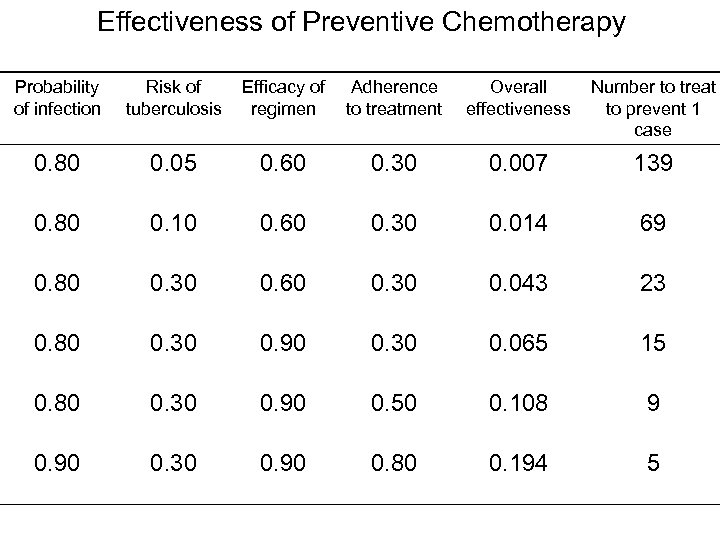
Effectiveness of Preventive Chemotherapy Probability of infection Risk of tuberculosis Efficacy of regimen Adherence to treatment Overall effectiveness Number to treat to prevent 1 case 0. 80 0. 05 0. 60 0. 30 0. 007 139 0. 80 0. 10 0. 60 0. 30 0. 014 69 0. 80 0. 30 0. 60 0. 30 0. 043 23 0. 80 0. 30 0. 90 0. 30 0. 065 15 0. 80 0. 30 0. 90 0. 50 0. 108 9 0. 90 0. 30 0. 90 0. 80 0. 194 5



Problems with Preventive Chemotherapy o Difficulties in ensuring adherence o Efficacious but inefficient o Rare adverse drug events o Ensuring certainty to exclude active tuberculosis
Considerations in the Use of Preventive Therapy Logistic and material feasibility and ease: o Household contacts > persons with risk factors > risk groups > general population o Drug costs: isoniazid << rifampicin, pyrazinamide o Risk perception adherence
Indications for Preventive Therapy In industrialized countries: o Young persons with tuberculous infection o Persons with risk factors In low-income countries: o Children < 5 -yr-old, free of disease living with a sputum smear-positive case
To conclude: Some food for thought
All too cherished working hypotheses Once infected with Mycobacterium tuberculosis, infection persists for the remaining life time and may reactivate at any time. The immunologic response we measure informs us about persisters
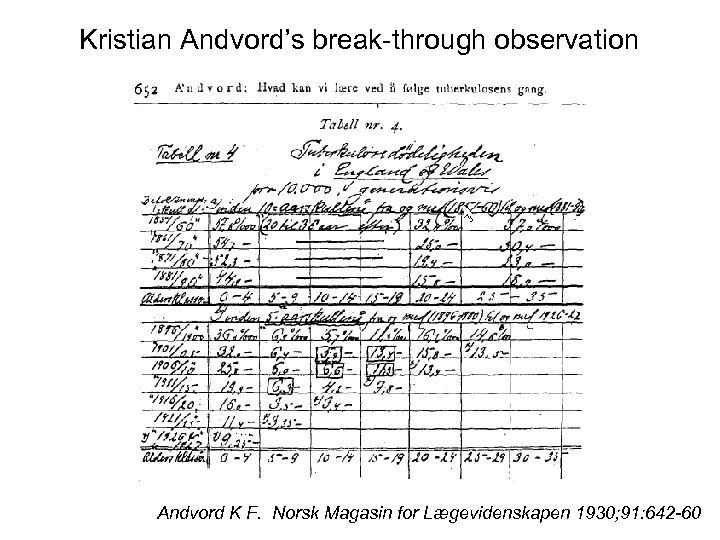
Kristian Andvord’s break-through observation Andvord K F. Norsk Magasin for Lægevidenskapen 1930; 91: 642 -60

Andvord’s conclusion Childhood experience with Mycobacterium tuberculosis predicts adult experience
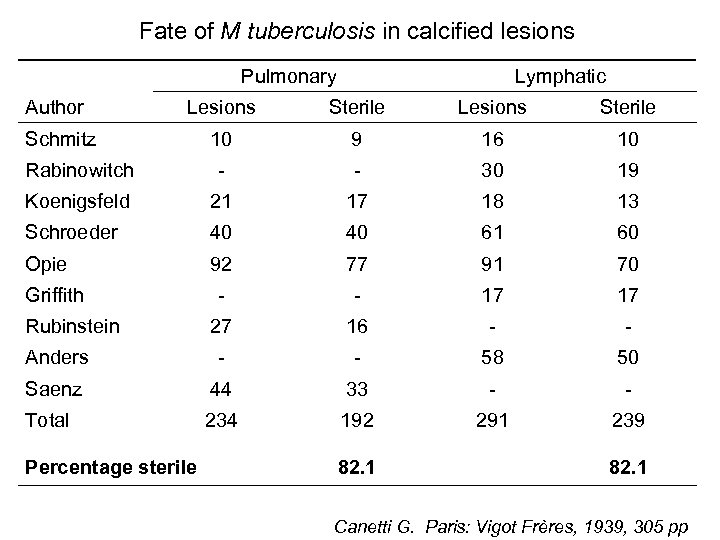
Fate of M tuberculosis in calcified lesions Pulmonary Author Lymphatic Lesions Sterile 10 9 16 10 Rabinowitch - - 30 19 Koenigsfeld 21 17 18 13 Schroeder 40 40 61 60 Opie 92 77 91 70 - - 17 17 27 16 - - Anders - - 58 50 Saenz 44 33 - - Total 234 192 291 239 Schmitz Griffith Rubinstein Percentage sterile 82. 1 Canetti G. Paris: Vigot Frères, 1939, 305 pp

Observation and dilemma Observation Bacilli are killed in the majority of cases following primary infection A large proportion of disease in adults is the result of reinfection Dilemma Reconciling Andvord and Canetti
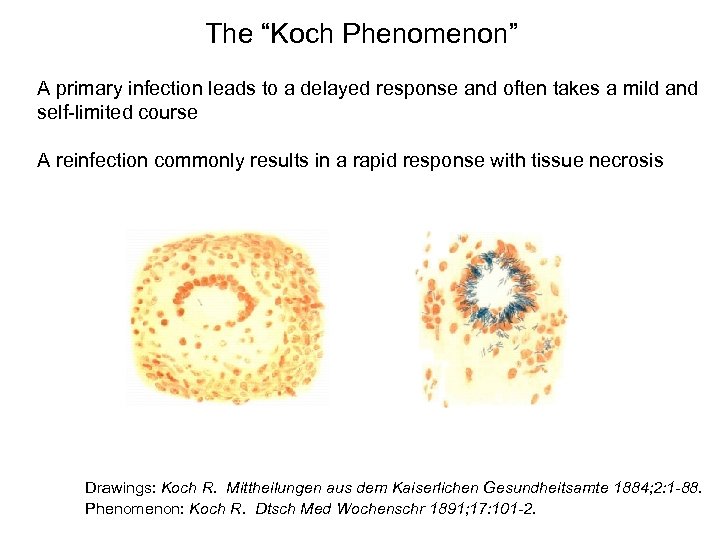
The “Koch Phenomenon” A primary infection leads to a delayed response and often takes a mild and self-limited course A reinfection commonly results in a rapid response with tissue necrosis Drawings: Koch R. Mittheilungen aus dem Kaiserlichen Gesundheitsamte 1884; 2: 1 -88. Phenomenon: Koch R. Dtsch Med Wochenschr 1891; 17: 101 -2.

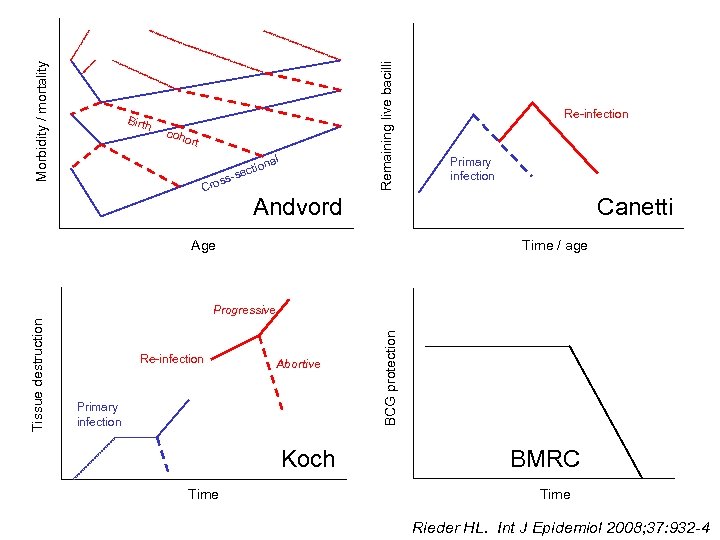
Remaining live bacilli Morbidity / mortality Birth coho rt nal ctio s-se s Cro Re-infection Primary infection Andvord Canetti Age Time / age Re-infection Abortive Primary infection Koch Time BCG protection Tissue destruction Progressive BMRC Time Rieder HL. Int J Epidemiol 2008; 37: 932 -4
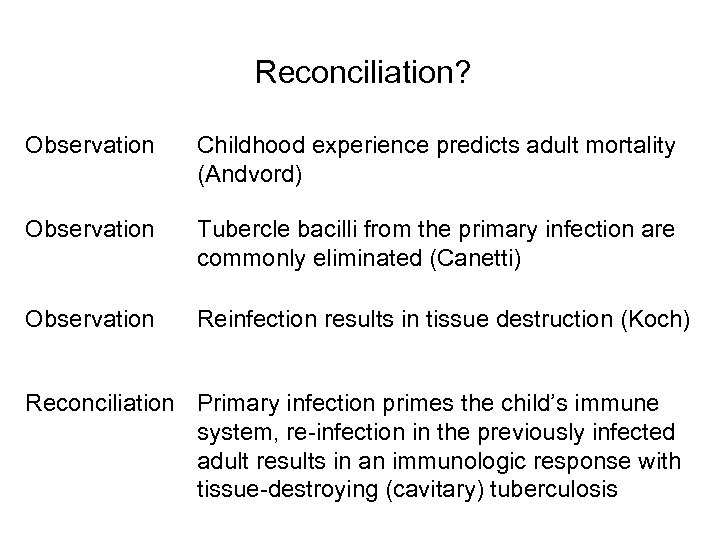
Reconciliation? Observation Childhood experience predicts adult mortality (Andvord) Observation Tubercle bacilli from the primary infection are commonly eliminated (Canetti) Observation Reinfection results in tissue destruction (Koch) Reconciliation Primary infection primes the child’s immune system, re-infection in the previously infected adult results in an immunologic response with tissue-destroying (cavitary) tuberculosis
Trying to fit observations …. o A first infection is commonly overcome and frequently ends in the elimination of bacilli but primes the immune system for a decade or more o A primed immune system may protect against subsequent re-infection or, alternatively, results in a severe tissue damaging response o A positive tuberculin skin test is neither expression of live bacilli nor of protective immunity, it only reflects the immune response following prior infection
Conclusions o Chemotherapy of infectious tuberculosis has both individual and epidemiologic impact o BCG vaccination impacts on individual health, but little on the epidemiologic situation o Treatment of other than infectious cases benefits individuals but impacts little on the epidemiologic situation o Preventive therapy may benefit the individual but is unlikely to impact importantly on the epidemiologic situation
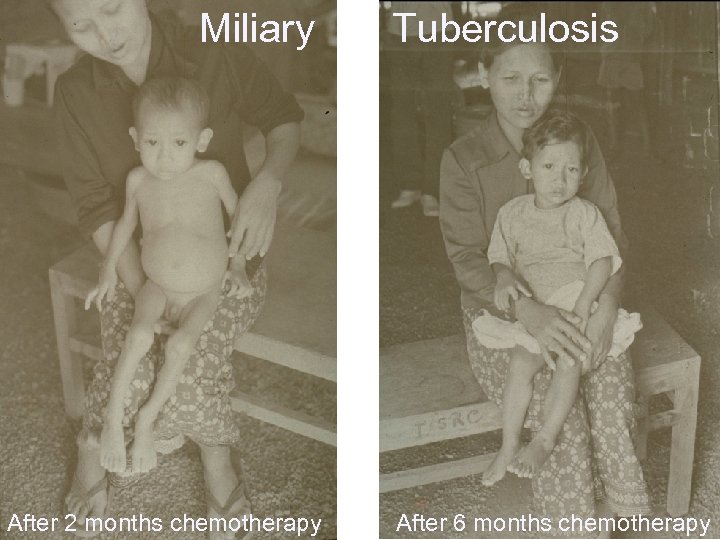
Miliary After 2 months chemotherapy Tuberculosis After 6 months chemotherapy
0f168cd2bf5429a5dc4a4d7dae576462.ppt