b6fff4cb91a3ac97323328edb517a829.ppt
- Количество слайдов: 66
INTERVENTIONAL PAIN MANAGEMENT FOR LBP Dr. dr. Yusak M. T. Siahaan, Sp. S, FIPP Siloam Hospital Lippo Village/ Medical Faculty Pelita Harapan University
What is Pain? Pain is an unpleasant sensory and/or emotional experience associated with actual or potential tissue damage, or described in terms of such damage. (International Association for the Study of Pain)
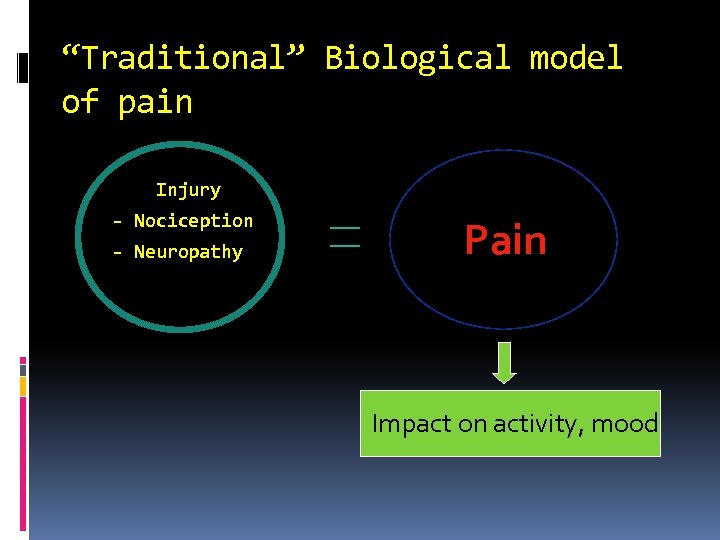
“Traditional” Biological model of pain Injury - Nociception - Neuropathy Pain Impact on activity, mood
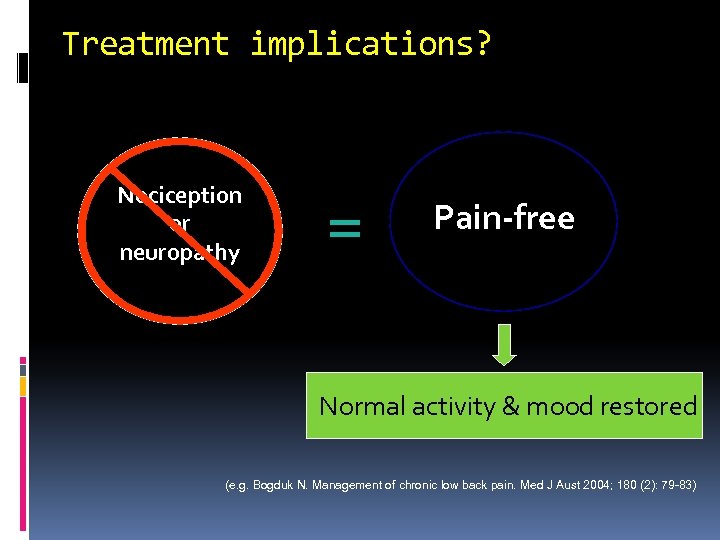
Treatment implications? Nociception or neuropathy Pain-free Normal activity & mood restored (e. g. Bogduk N. Management of chronic low back pain. Med J Aust 2004; 180 (2): 79 -83)
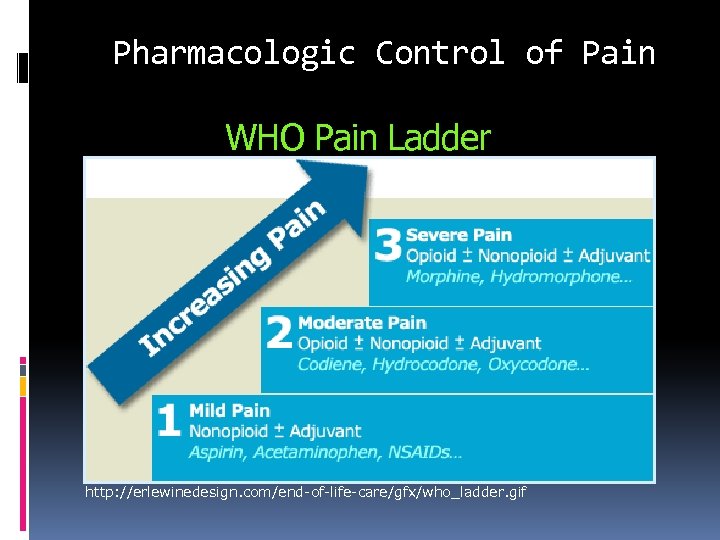
Pharmacologic Control of Pain WHO Pain Ladder http: //erlewinedesign. com/end-of-life-care/gfx/who_ladder. gif
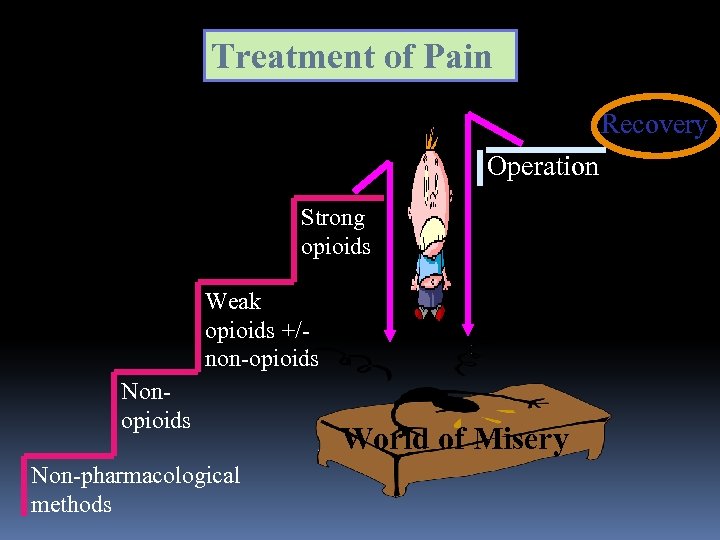
Treatment of Pain Recovery Operation Strong opioids Weak opioids +/non-opioids Non-pharmacological methods World of Misery
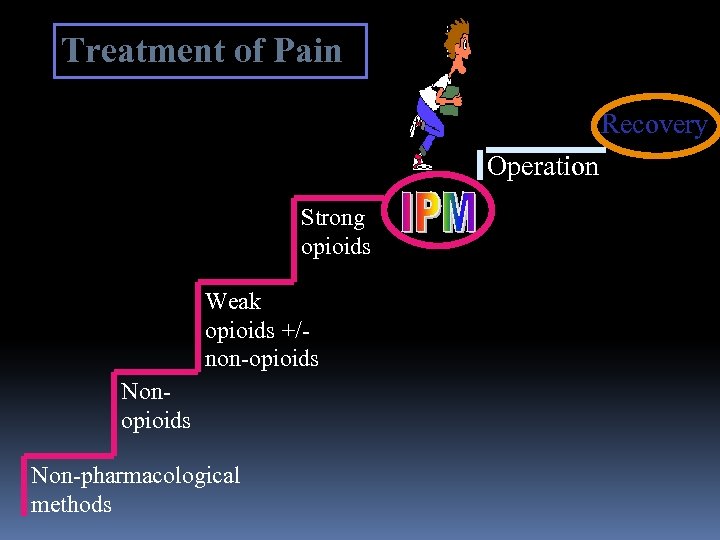
Treatment of Pain Recovery Operation Strong opioids Weak opioids +/non-opioids Non-pharmacological methods
Interventional Pain Management w The discipline of medicine devoted to the diagnosis and treatment of pain and related disorders by the application of interventional techniques in managing sub-acute, chronic, persistent, and intractable pain, independently or in conjunction with other modalities of treatments.
Interventional Pain Management w Minimally invasive procedures including percutaneous precision needle placement, with placement of drugs in targeted areas or ablation of targeted nerves.
IPM are group of procedures with different mechanism of actions 1. Targeted delivery of drugs 2. Blocking of nerve signals corrects neuropathy.
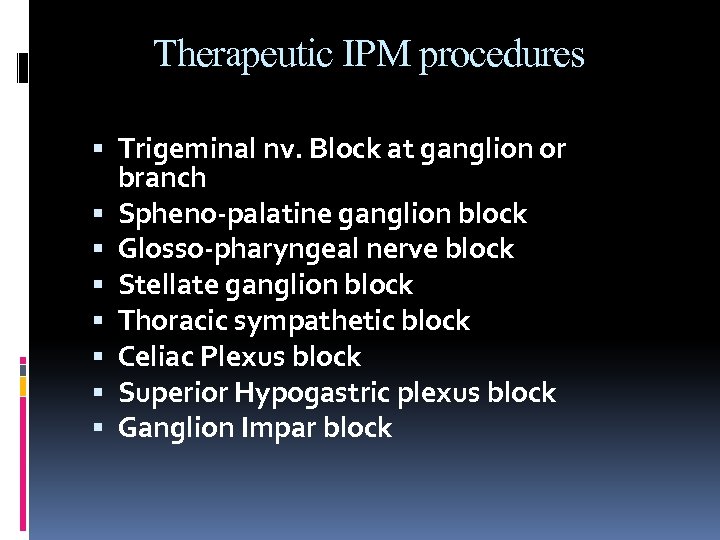
Therapeutic IPM procedures Trigeminal nv. Block at ganglion or branch Spheno-palatine ganglion block Glosso-pharyngeal nerve block Stellate ganglion block Thoracic sympathetic block Celiac Plexus block Superior Hypogastric plexus block Ganglion Impar block
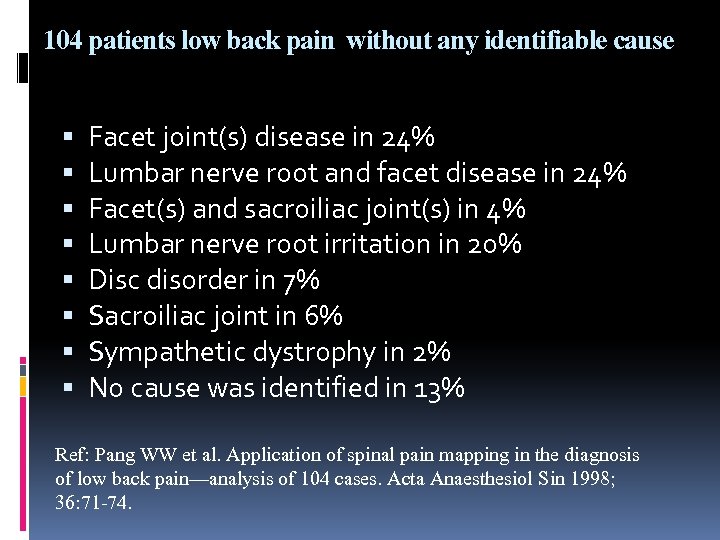
104 patients low back pain without any identifiable cause Facet joint(s) disease in 24% Lumbar nerve root and facet disease in 24% Facet(s) and sacroiliac joint(s) in 4% Lumbar nerve root irritation in 20% Disc disorder in 7% Sacroiliac joint in 6% Sympathetic dystrophy in 2% No cause was identified in 13% Ref: Pang WW et al. Application of spinal pain mapping in the diagnosis of low back pain—analysis of 104 cases. Acta Anaesthesiol Sin 1998; 36: 71 -74.
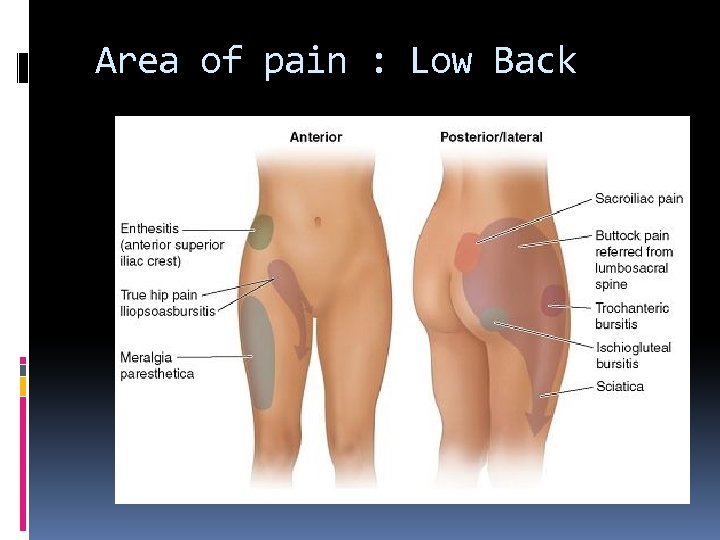
Area of pain : Low Back
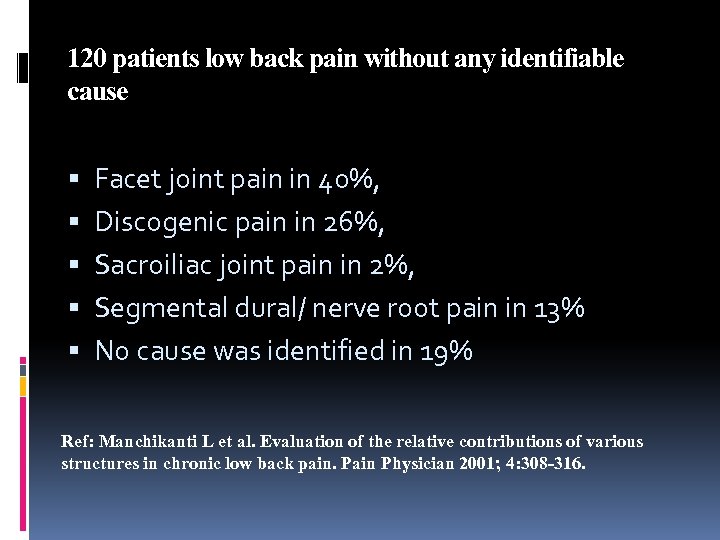
120 patients low back pain without any identifiable cause Facet joint pain in 40%, Discogenic pain in 26%, Sacroiliac joint pain in 2%, Segmental dural/ nerve root pain in 13% No cause was identified in 19% Ref: Manchikanti L et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician 2001; 4: 308 -316.
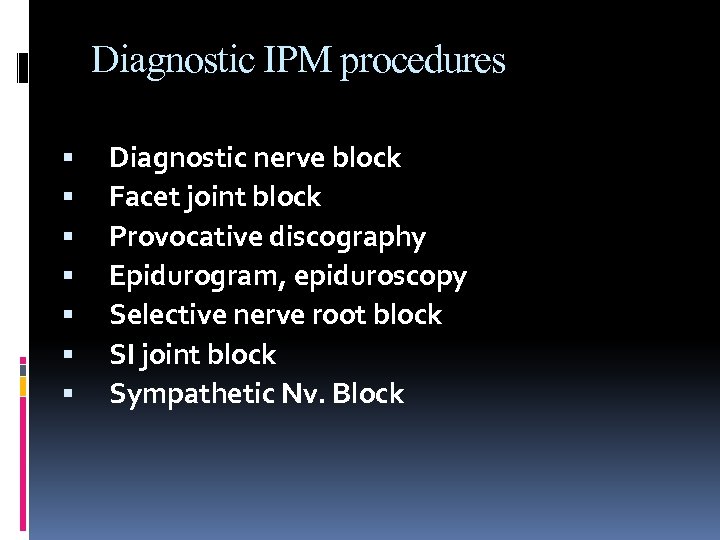
Diagnostic IPM procedures Diagnostic nerve block Facet joint block Provocative discography Epidurogram, epiduroscopy Selective nerve root block SI joint block Sympathetic Nv. Block
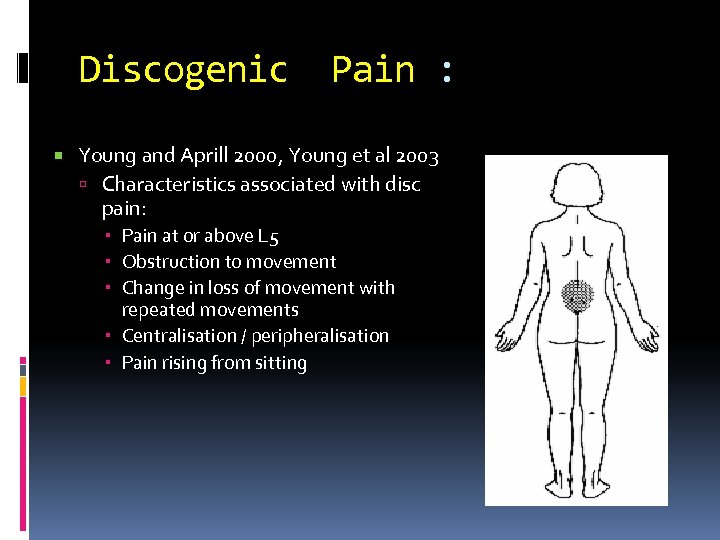
Discogenic Pain : Young and Aprill 2000, Young et al 2003 Characteristics associated with disc pain: Pain at or above L 5 Obstruction to movement Change in loss of movement with repeated movements Centralisation / peripheralisation Pain rising from sitting
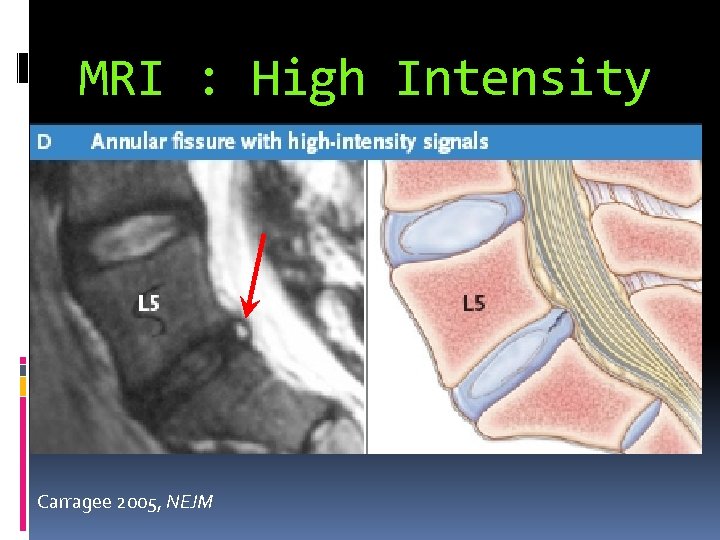
MRI : High Intensity Zone Carragee 2005, NEJM
Discogenic pain : management Treatment Medication Functional restoration Intradiscal Electrothermal Therapy (IDET) Lumbar fusion
Management : Medication Analgesics NSAIDS (mechanism of pain relief unclear) Tylenol, Tramadol Opioids (time contingent use most effective) Anti-inflammatories NSAID’s (consider side effects) Corticosteroids (consider side effects) Muscle relaxants
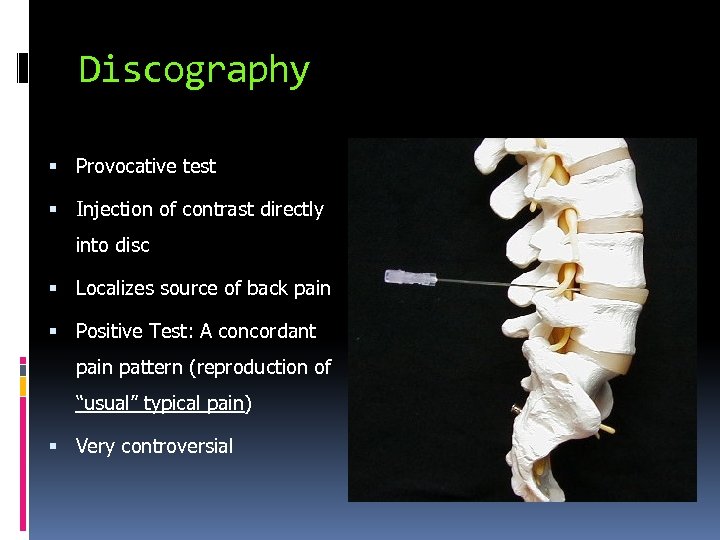
Discography Provocative test Injection of contrast directly into disc Localizes source of back pain Positive Test: A concordant pain pattern (reproduction of “usual” typical pain) Very controversial
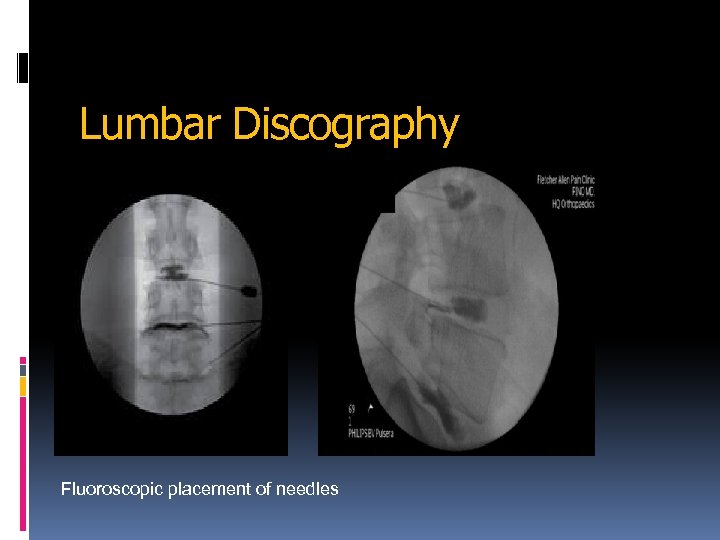
Lumbar Discography Fluoroscopic placement of needles
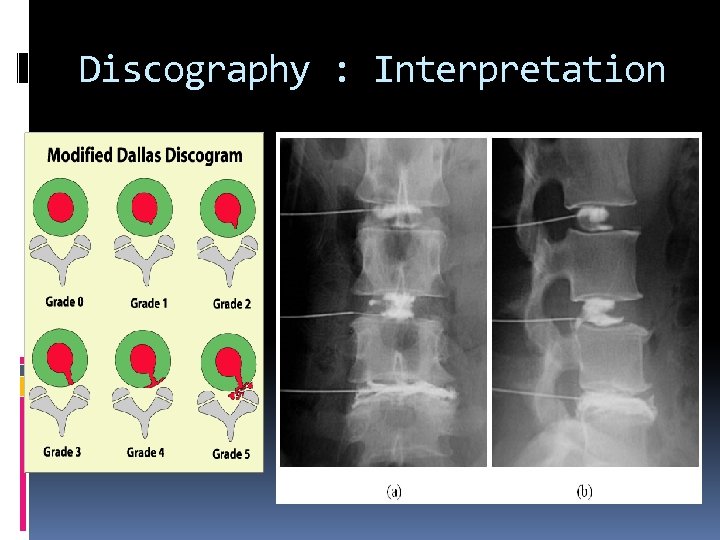
Discography : Interpretation
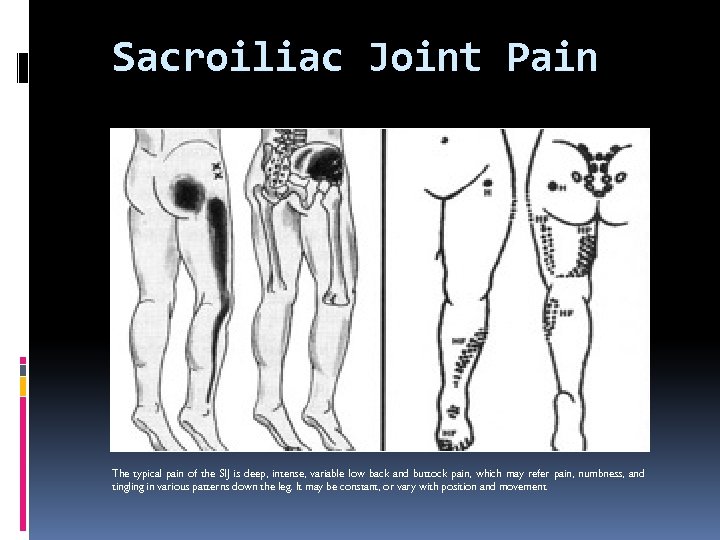
Sacroiliac Joint Pain The typical pain of the SIJ is deep, intense, variable low back and buttock pain, which may refer pain, numbness, and tingling in various patterns down the leg. It may be constant, or vary with position and movement
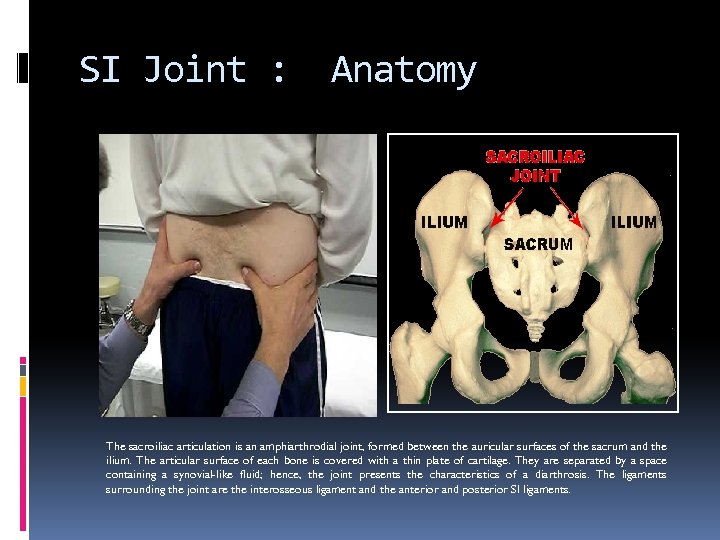
SI Joint : Anatomy The sacroiliac articulation is an amphiarthrodial joint, formed between the auricular surfaces of the sacrum and the ilium. The articular surface of each bone is covered with a thin plate of cartilage. They are separated by a space containing a synovial-like fluid; hence, the joint presents the characteristics of a diarthrosis. The ligaments surrounding the joint are the interosseous ligament and the anterior and posterior SI ligaments.
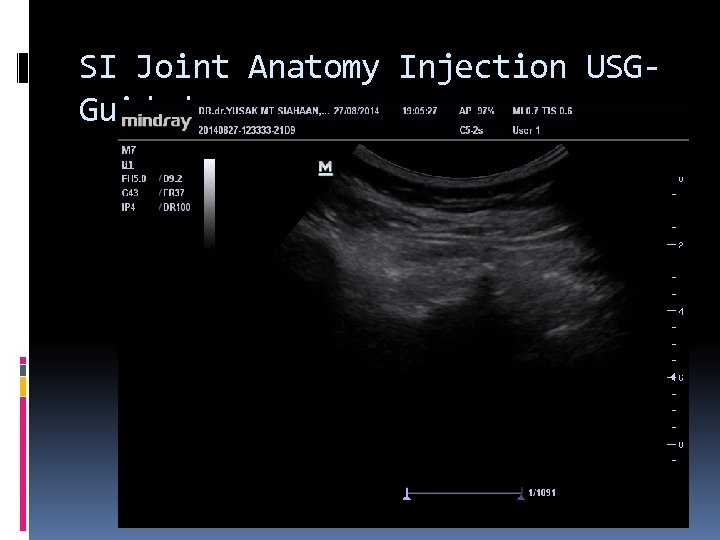
SI Joint Anatomy Injection USGGuided
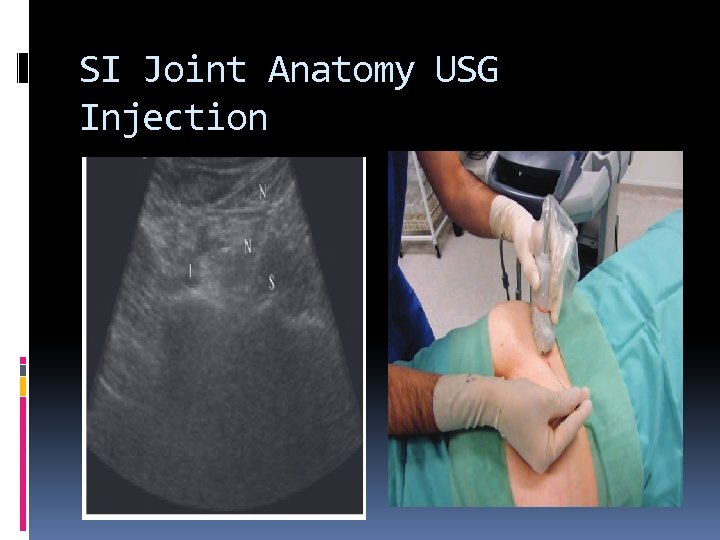
SI Joint Anatomy USG Injection
Sacroiliac Joint Injection Carm Guided
Sacroiliac Joint Injection Carm Guided
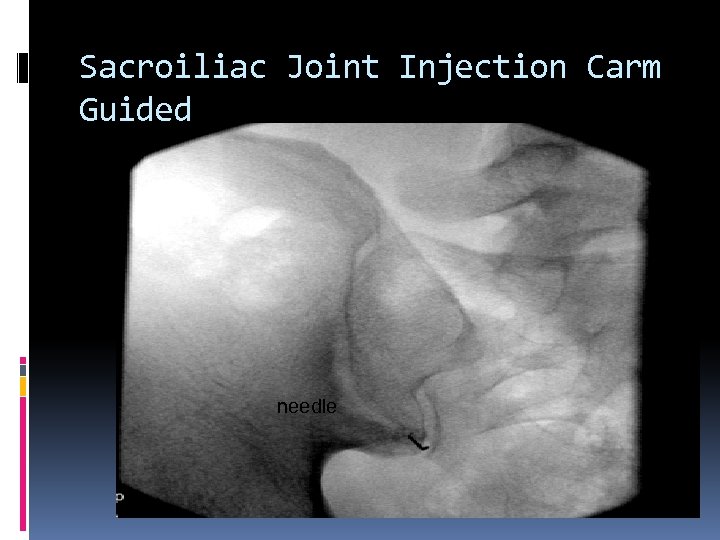
Sacroiliac Joint Injection Carm Guided needle
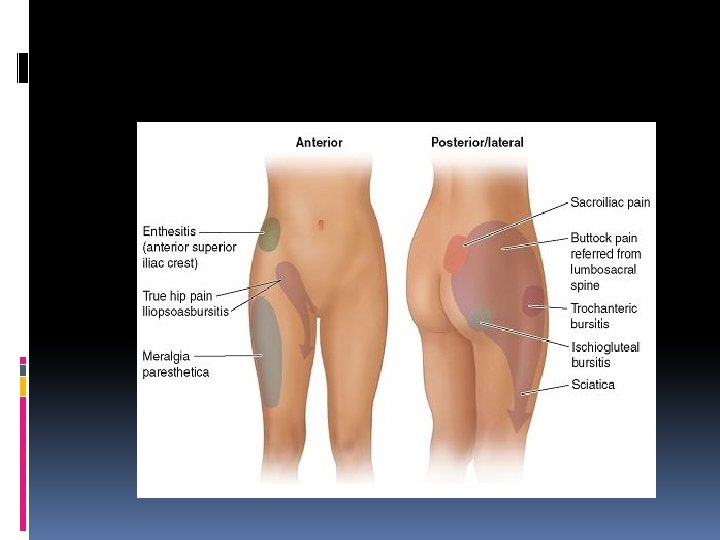
Piriformis Syndrome Pain
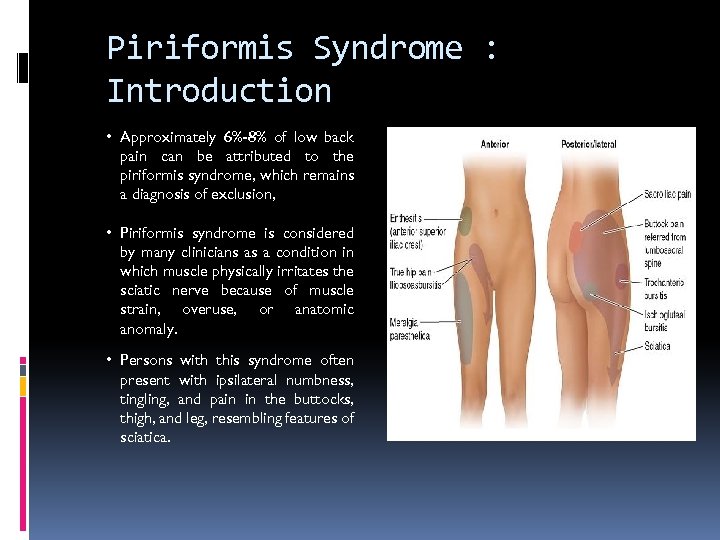
Piriformis Syndrome : Introduction • Approximately 6%-8% of low back pain can be attributed to the piriformis syndrome, which remains a diagnosis of exclusion, • Piriformis syndrome is considered by many clinicians as a condition in which muscle physically irritates the sciatic nerve because of muscle strain, overuse, or anatomic anomaly. • Persons with this syndrome often present with ipsilateral numbness, tingling, and pain in the buttocks, thigh, and leg, resembling features of sciatica.
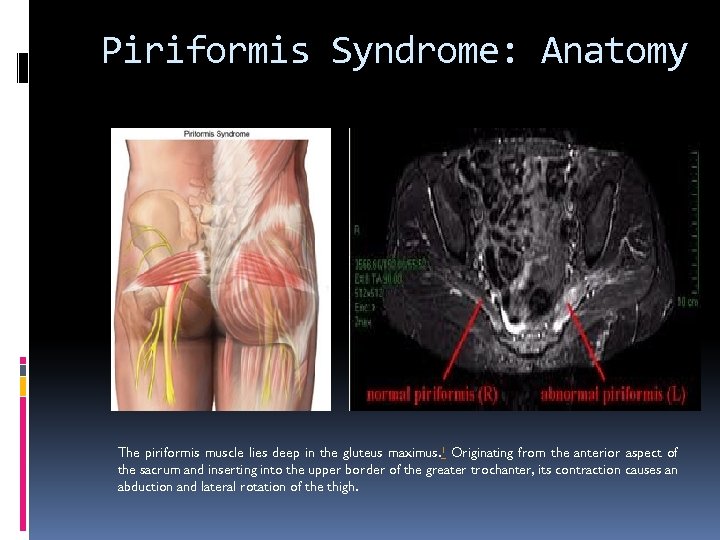
Piriformis Syndrome: Anatomy The piriformis muscle lies deep in the gluteus maximus. 1 Originating from the anterior aspect of the sacrum and inserting into the upper border of the greater trochanter, its contraction causes an abduction and lateral rotation of the thigh.
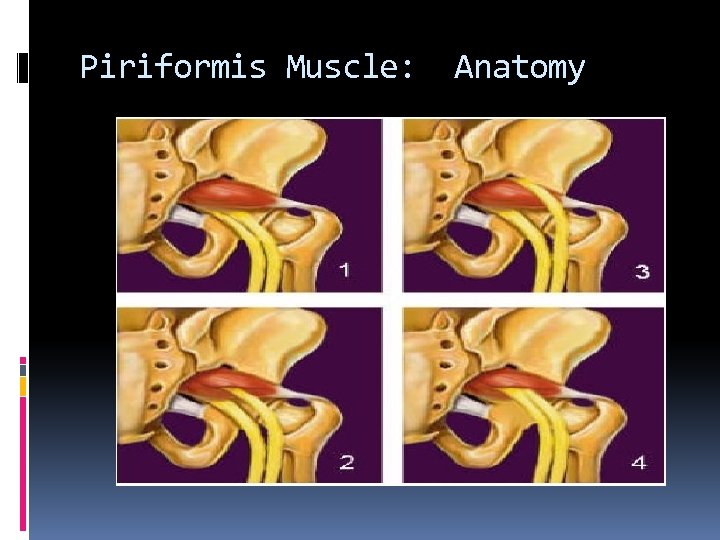
Piriformis Muscle: Anatomy
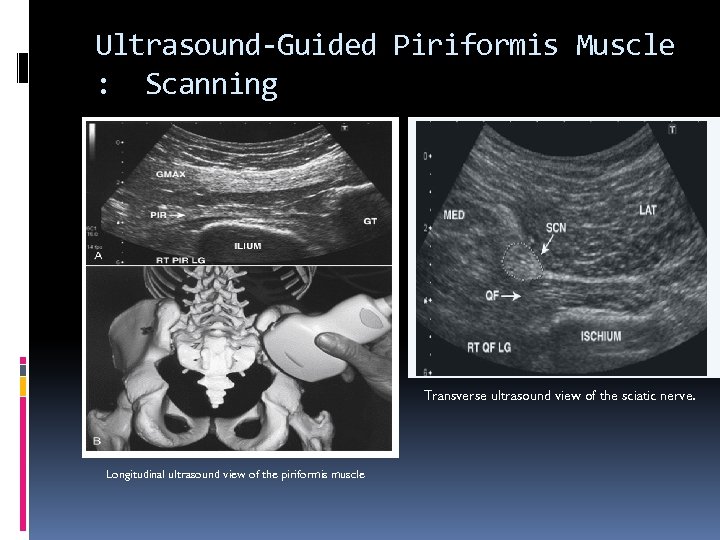
Ultrasound-Guided Piriformis Muscle : Scanning Transverse ultrasound view of the sciatic nerve. Longitudinal ultrasound view of the piriformis muscle
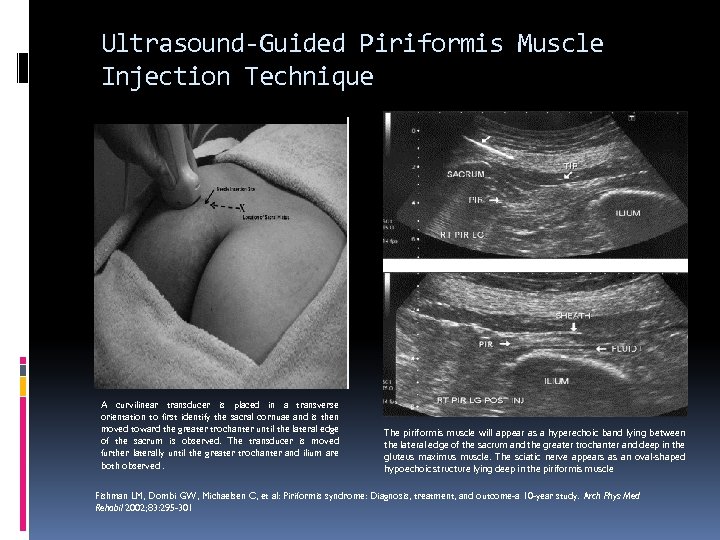
Ultrasound-Guided Piriformis Muscle Injection Technique A curvilinear transducer is placed in a transverse orientation to first identify the sacral cornuae and is then moved toward the greater trochanter until the lateral edge of the sacrum is observed. The transducer is moved further laterally until the greater trochanter and ilium are both observed. The piriformis muscle will appear as a hyperechoic band lying between the lateral edge of the sacrum and the greater trochanter and deep in the gluteus maximus muscle. The sciatic nerve appears as an oval-shaped hypoechoic structure lying deep in the piriformis muscle Fishman LM, Dombi GW, Michaelsen C, et al: Piriformis syndrome: Diagnosis, treatment, and outcome-a 10 -year study. Arch Phys Med Rehabil 2002; 83: 295 -301
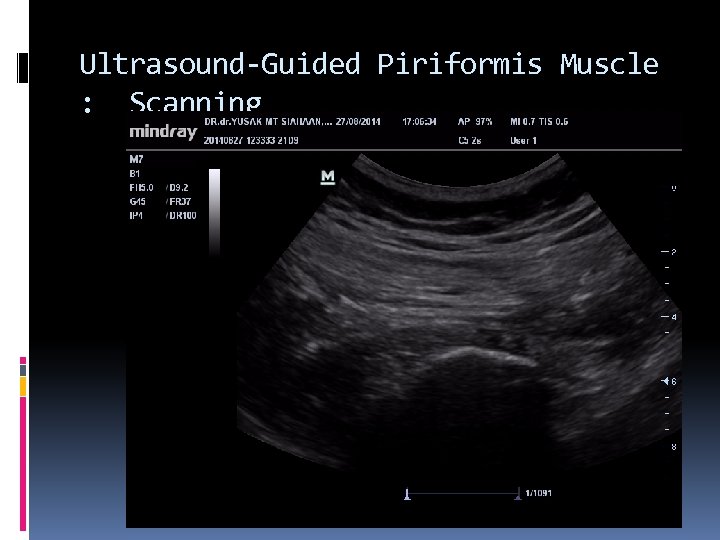
Ultrasound-Guided Piriformis Muscle : Scanning
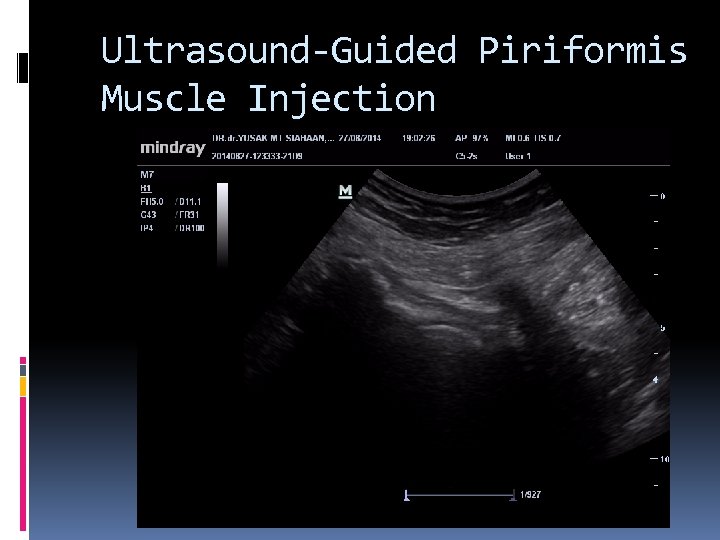
Ultrasound-Guided Piriformis Muscle Injection
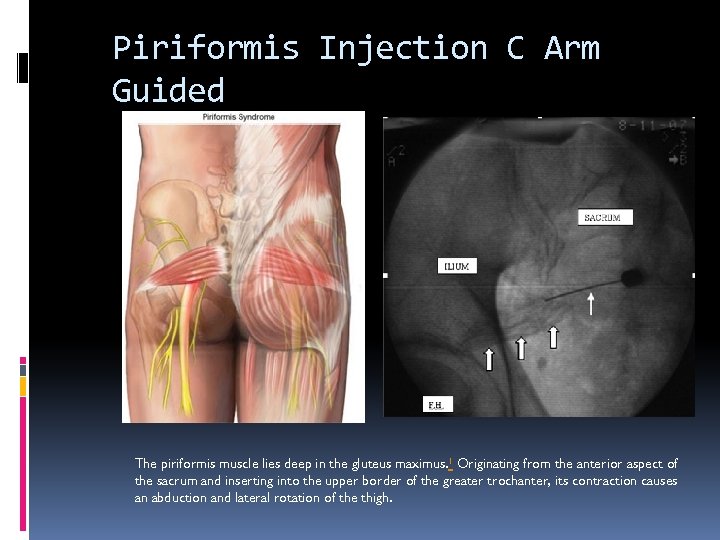
Piriformis Injection C Arm Guided The piriformis muscle lies deep in the gluteus maximus. 1 Originating from the anterior aspect of the sacrum and inserting into the upper border of the greater trochanter, its contraction causes an abduction and lateral rotation of the thigh.
Herniated Disc pain A herniated lumbar disc can press on the nerves in the spine and may cause pain, numbness, tingling or weakness of the leg called "sciatica. " Sciatica affects about 1 -2% of all people, usually between the ages of 30 and 50. A herniated lumbar disc may also cause back pain, although back pain alone (without leg pain) can have many causes other than a herniated disc.
Herniated Disc pain : symptoms Low Back to lower leg Sharp, shooting or burning pain Decreased with standing : increased with bending or sitting Positive straight leg raise test
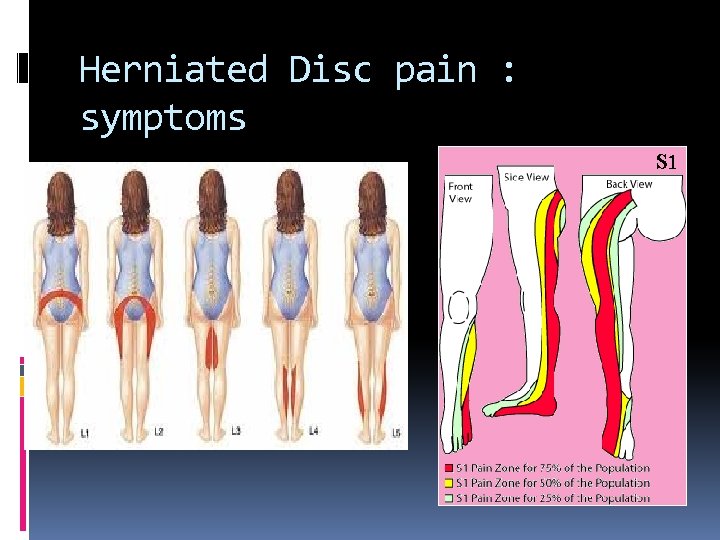
Herniated Disc pain : symptoms
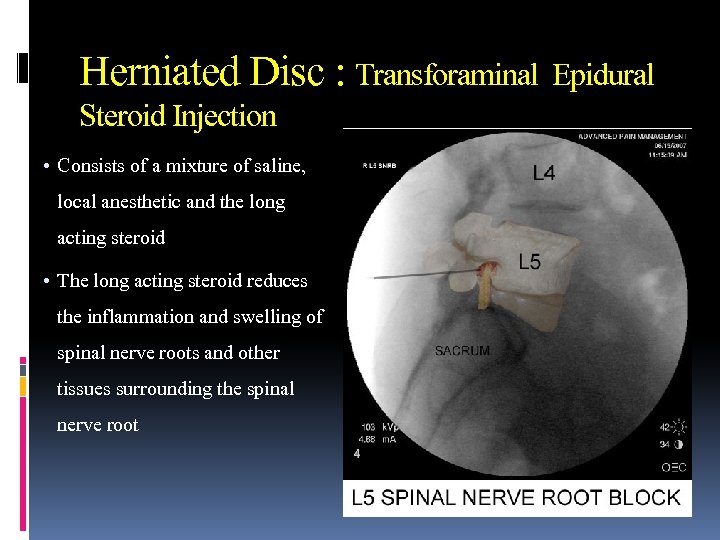
Herniated Disc : Transforaminal Steroid Injection • Consists of a mixture of saline, local anesthetic and the long acting steroid • The long acting steroid reduces the inflammation and swelling of spinal nerve roots and other tissues surrounding the spinal nerve root Epidural
Transforaminal Epidural Steroid
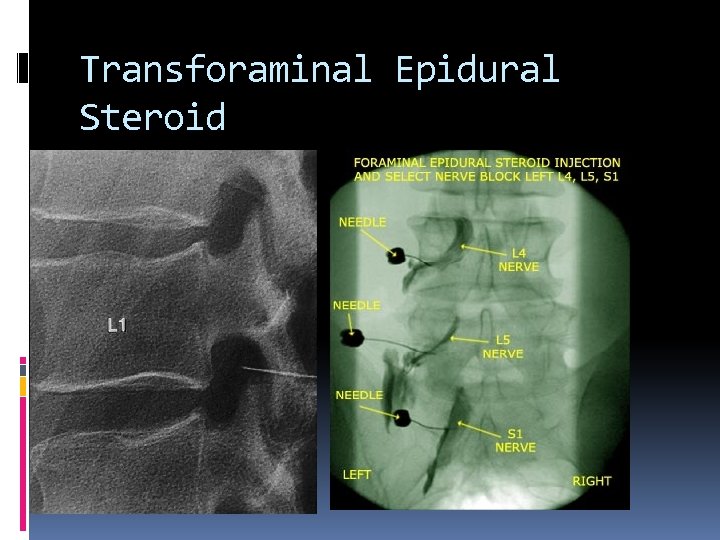
Transforaminal Epidural Steroid
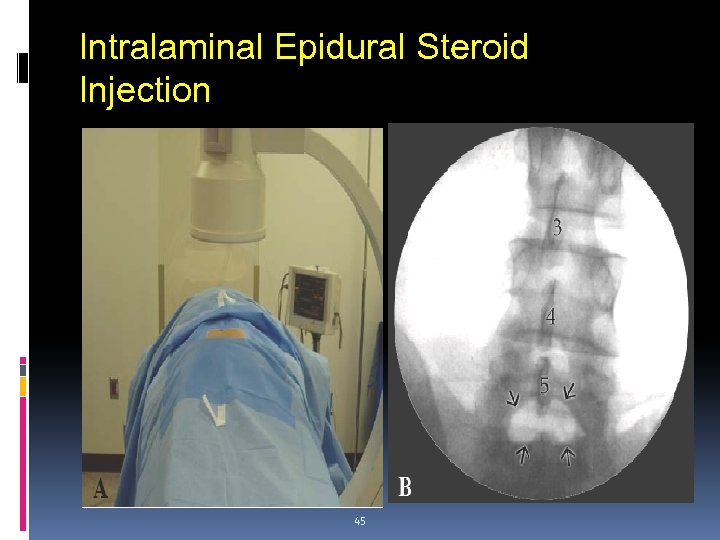
Intralaminal Epidural Steroid Injection 45
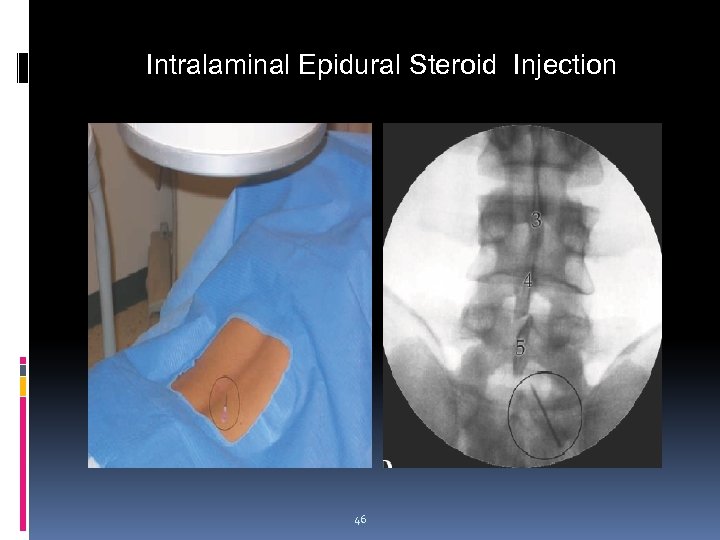
Intralaminal Epidural Steroid Injection 46
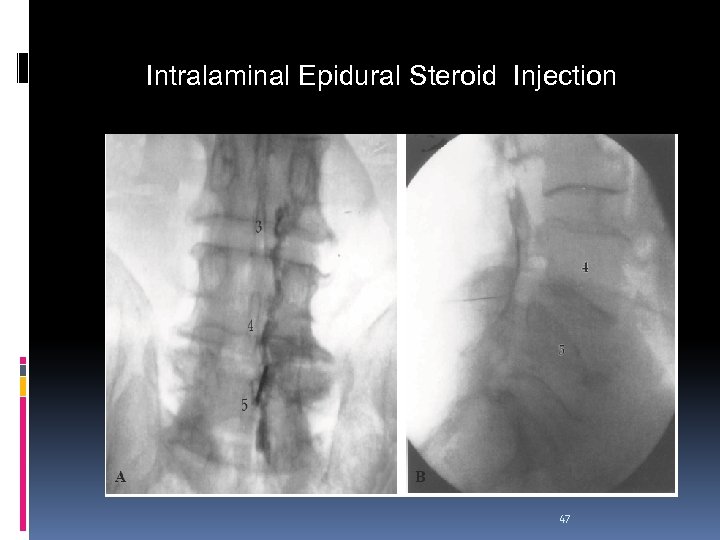
Intralaminal Epidural Steroid Injection 47
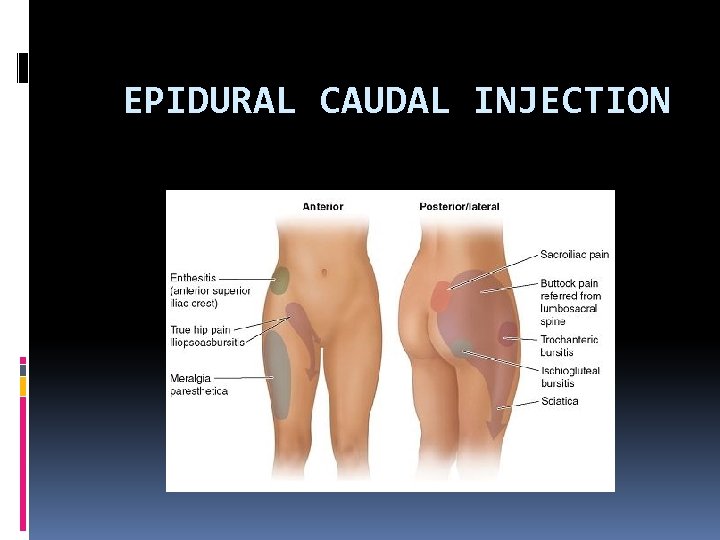
EPIDURAL CAUDAL INJECTION
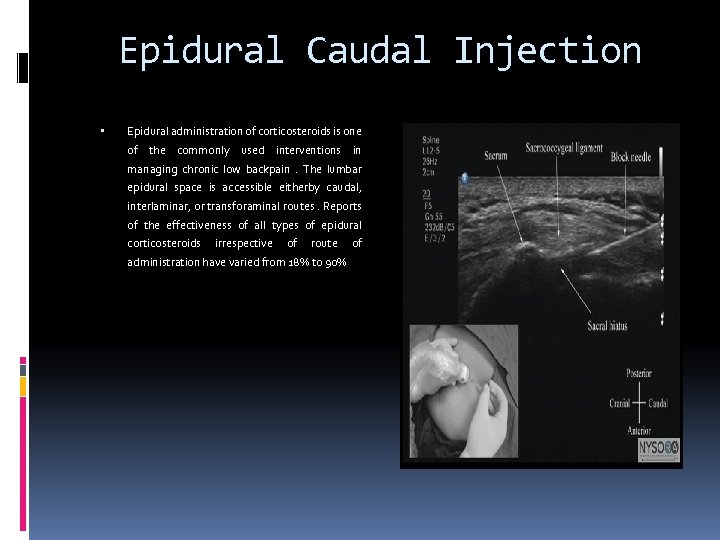
Epidural Caudal Injection Epidural administration of corticosteroids is one of the commonly used interventions in managing chronic low backpain. The lumbar epidural space is accessible eitherby caudal, interlaminar, or transforaminal routes. Reports of the effectiveness of all types of epidural corticosteroids irrespective of route administration have varied from 18% to 90% of
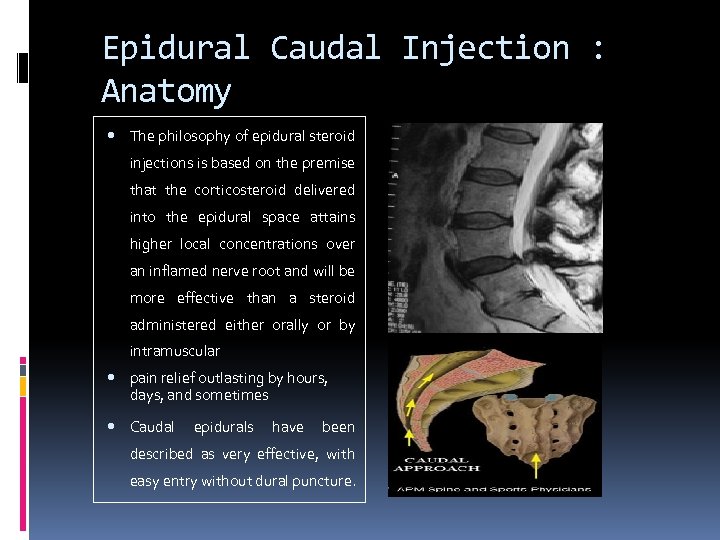
Epidural Caudal Injection : Anatomy The philosophy of epidural steroid injections is based on the premise that the corticosteroid delivered into the epidural space attains higher local concentrations over an inflamed nerve root and will be more effective than a steroid administered either orally or by intramuscular pain relief outlasting by hours, days, and sometimes Caudal epidurals have been described as very effective, with easy entry without dural puncture.
Epidural Caudal Injection USGGuided
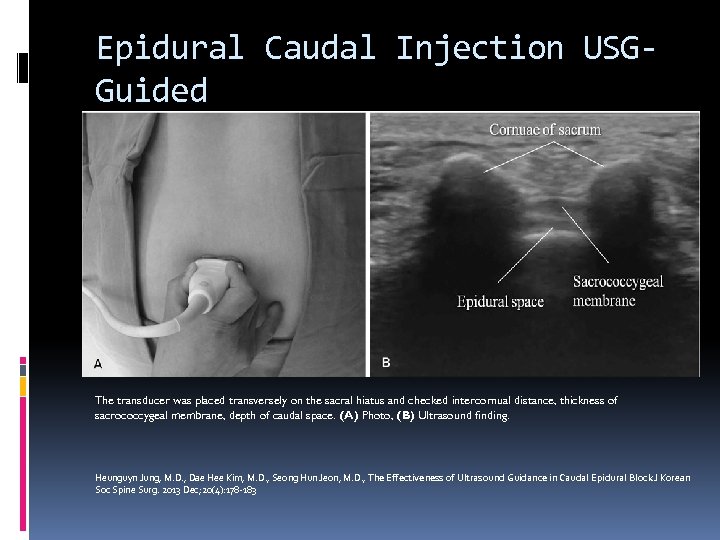
Epidural Caudal Injection USGGuided The transducer was placed transversely on the sacral hiatus and checked intercornual distance, thickness of sacrococcygeal membrane, depth of caudal space. (A) Photo, (B) Ultrasound finding. Heunguyn Jung, M. D. , Dae Hee Kim, M. D. , Seong Hun Jeon, M. D. , The Effectiveness of Ultrasound Guidance in Caudal Epidural Block J Korean Soc Spine Surg. 2013 Dec; 20(4): 178 -183
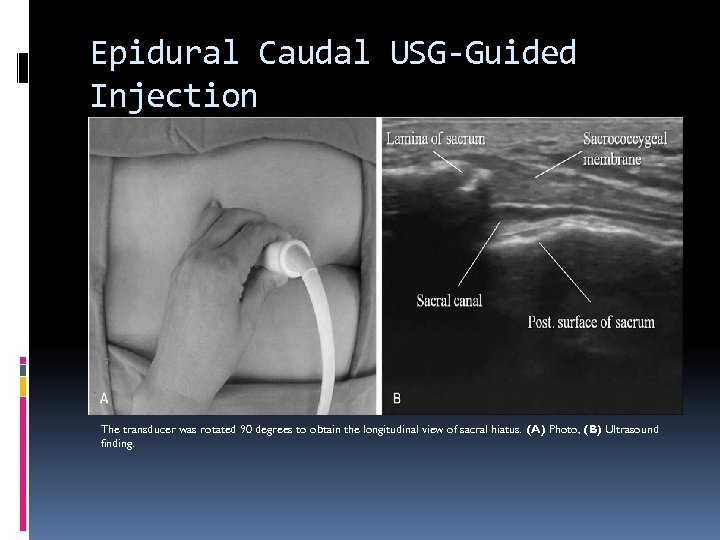
Epidural Caudal USG-Guided Injection The transducer was rotated 90 degrees to obtain the longitudinal view of sacral hiatus. (A) Photo, (B) Ultrasound finding.
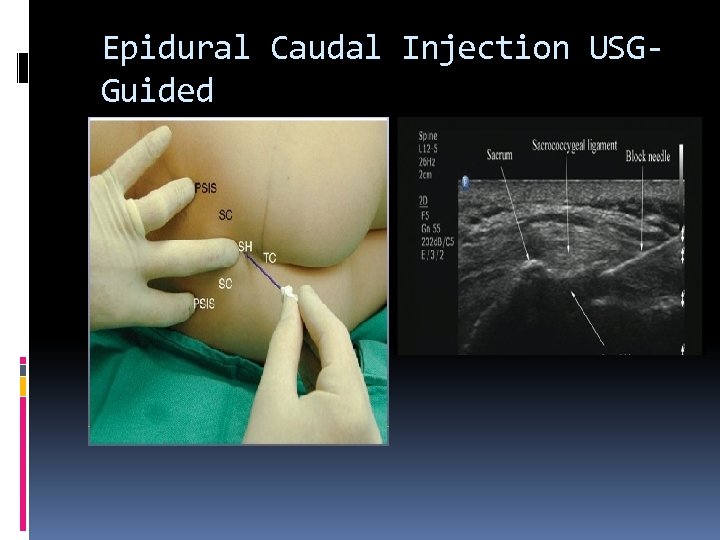
Epidural Caudal Injection USGGuided
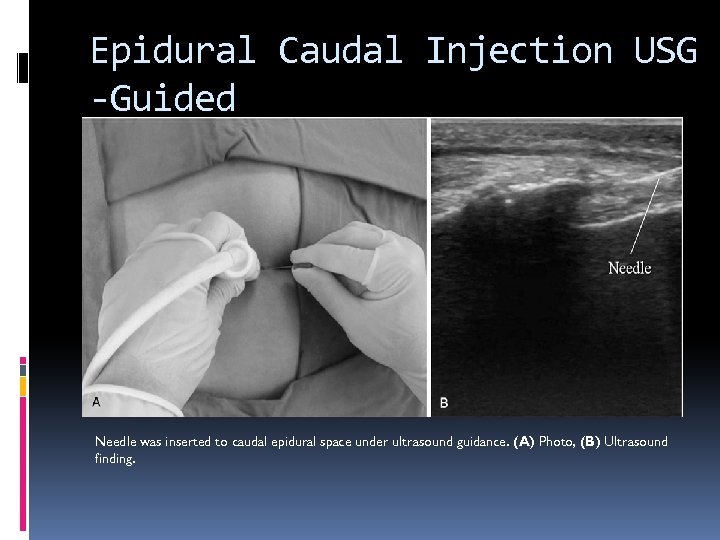
Epidural Caudal Injection USG -Guided Needle was inserted to caudal epidural space under ultrasound guidance. (A) Photo, (B) Ultrasound finding.
Epidural Caudal Injection USGGuided
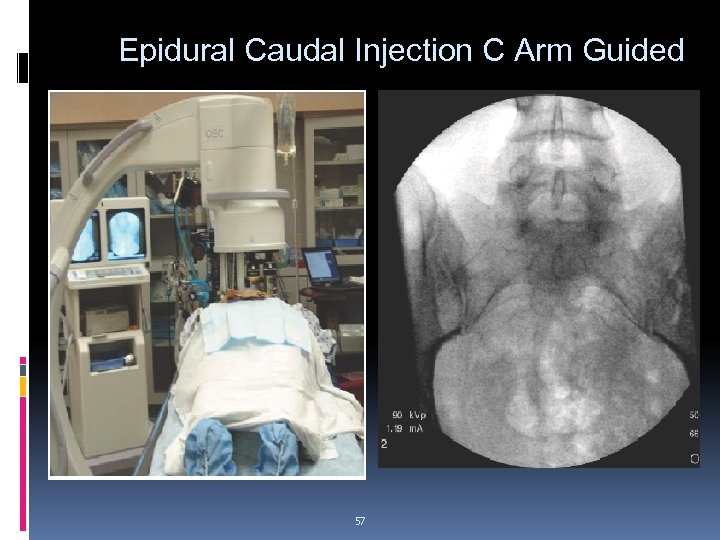
Epidural Caudal Injection C Arm Guided 57
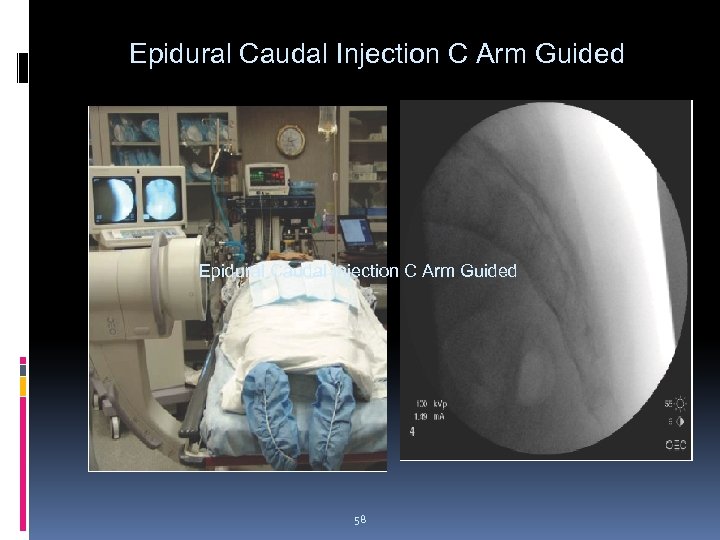
Epidural Caudal Injection C Arm Guided 58
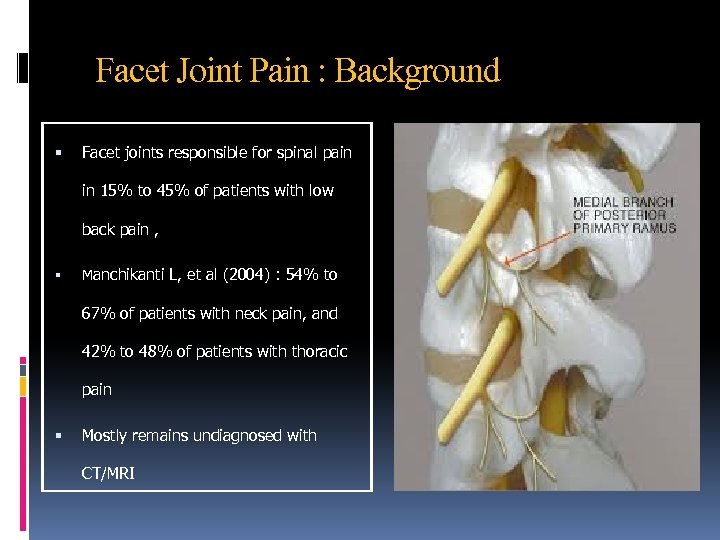
Facet Joint Pain : Background Facet joints responsible for spinal pain in 15% to 45% of patients with low back pain , Manchikanti L, et al (2004) : 54% to 67% of patients with neck pain, and 42% to 48% of patients with thoracic pain Mostly remains undiagnosed with CT/MRI
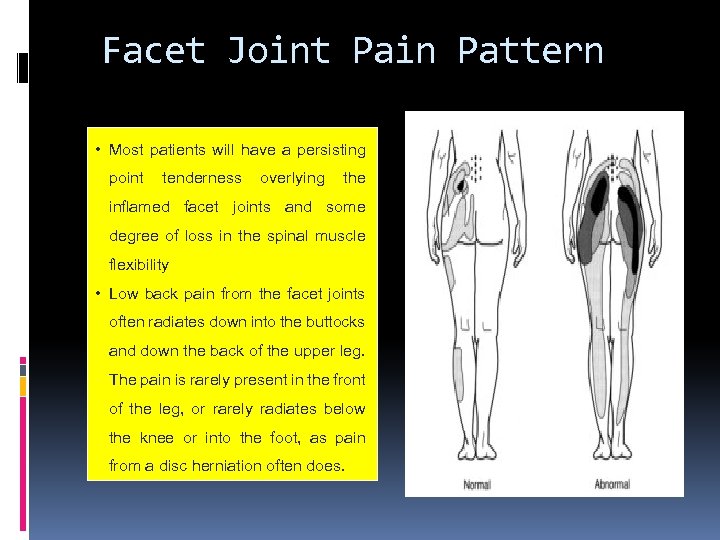
Facet Joint Pain Pattern • Most patients will have a persisting point tenderness overlying the inflamed facet joints and some degree of loss in the spinal muscle flexibility • Low back pain from the facet joints often radiates down into the buttocks and down the back of the upper leg. The pain is rarely present in the front of the leg, or rarely radiates below the knee or into the foot, as pain from a disc herniation often does.

Facet Joint pain : treatment Postural Rehabilitation Anti-inflamatory drugs Intervetebral Differential Dynamics (IDD) Therapeutic injections Facet joint injection Medial Branch block
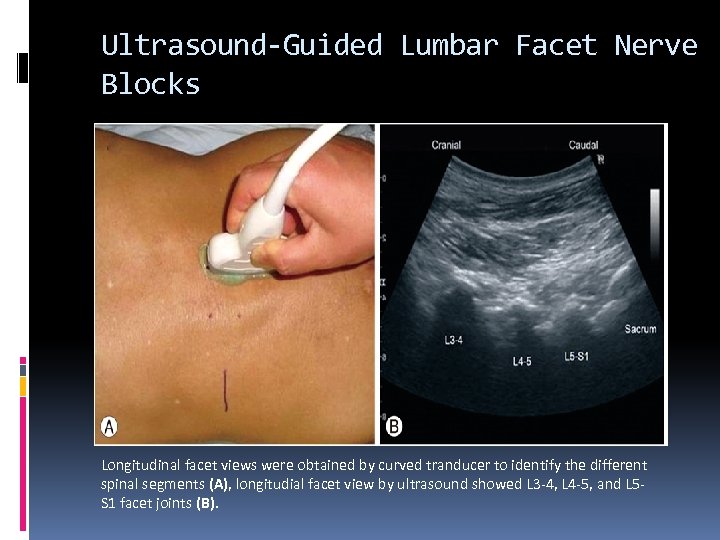
Ultrasound-Guided Lumbar Facet Nerve Blocks Longitudinal facet views were obtained by curved tranducer to identify the different spinal segments (A), longitudial facet view by ultrasound showed L 3 -4, L 4 -5, and L 5 S 1 facet joints (B).
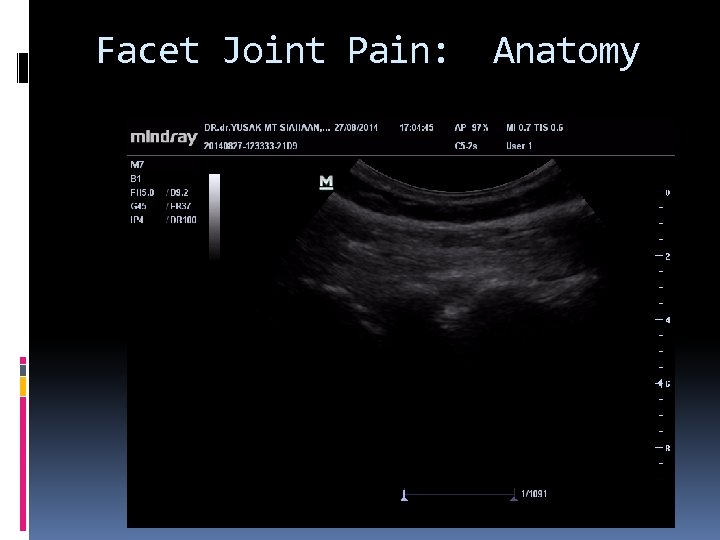
Facet Joint Pain: Anatomy
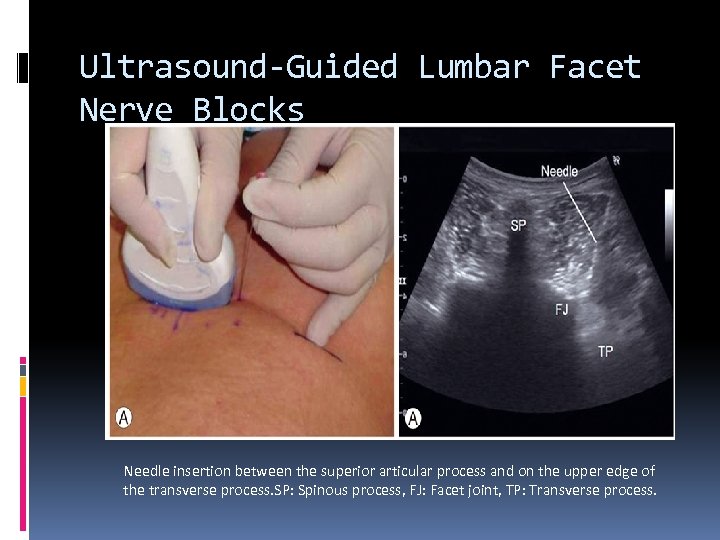
Ultrasound-Guided Lumbar Facet Nerve Blocks Needle insertion between the superior articular process and on the upper edge of the transverse process. SP: Spinous process, FJ: Facet joint, TP: Transverse process.
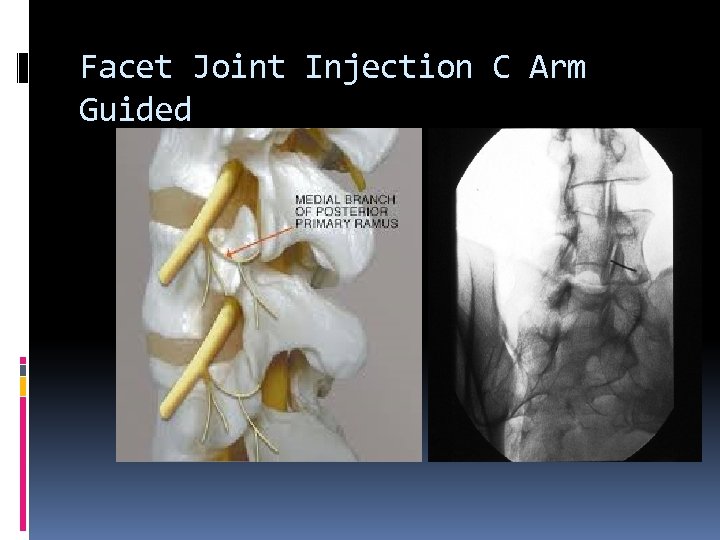
Facet Joint Injection C Arm Guided

Radiofrequency Ablation
b6fff4cb91a3ac97323328edb517a829.ppt