729beb825675f466c5cd1f91b92cdbb5.ppt
- Количество слайдов: 34
International Comparisons in CVD Morbidity and Mortality • CVD accounts for 25 -45% of deaths among different countries • CVD death rates (per 100, 000) range from 1310 in Russia to 201 in Japan (6. 5 fold difference) in men and from 581 in Russia to 84 in France (7 -fold difference) • USA ranks 16 th for both men (413) and women (201)
Secular Trends in CHD and Stroke Mortality • From 1985 -1992, greatest annual decline (6 -7%) in CHD seen in Israel among men and France among women, USA intermediate (4%), increases in Poland Romania. • Stroke death rates declined most in Australia, Italy, and France (8 -9%), USA about 3%.
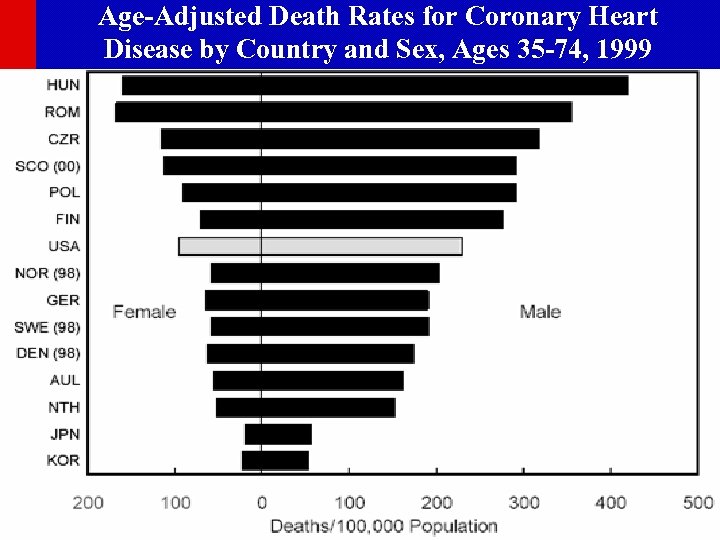
Age-Adjusted Death Rates for Coronary Heart Disease by Country and Sex, Ages 35 -74, 1999
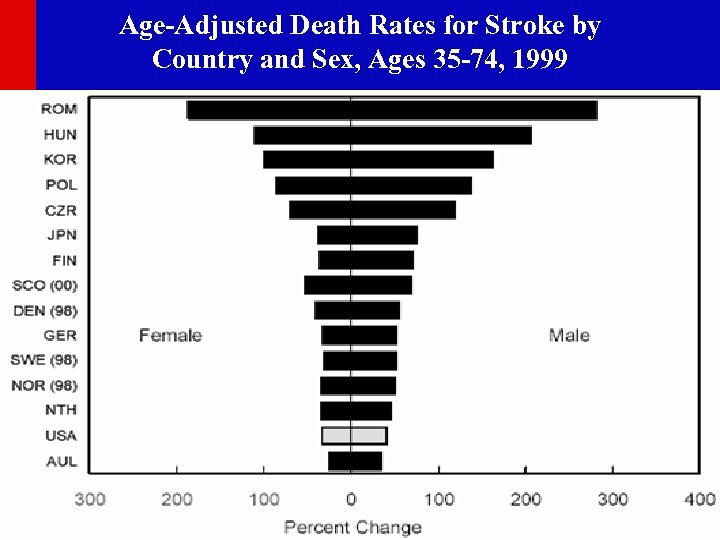
Age-Adjusted Death Rates for Stroke by Country and Sex, Ages 35 -74, 1999
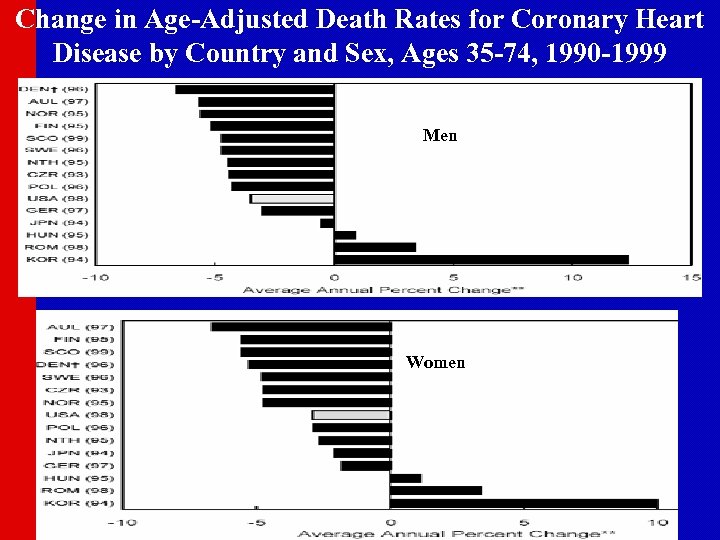
Change in Age-Adjusted Death Rates for Coronary Heart Disease by Country and Sex, Ages 35 -74, 1990 -1999 Men Women
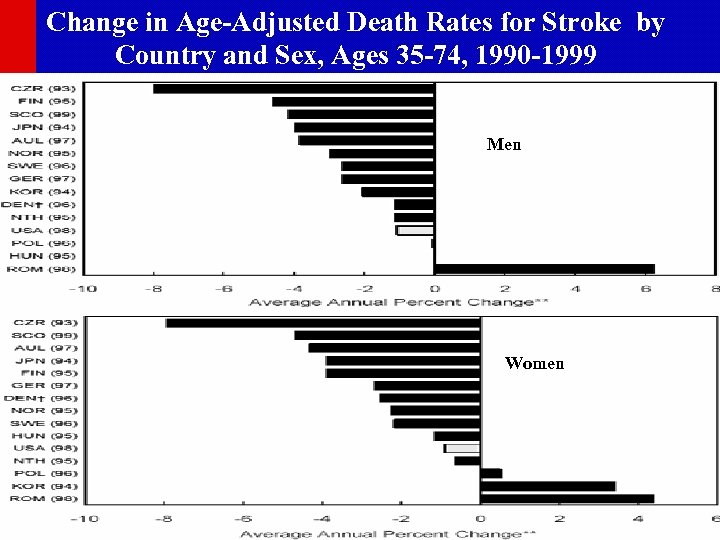
Change in Age-Adjusted Death Rates for Stroke by Country and Sex, Ages 35 -74, 1990 -1999 Men Women
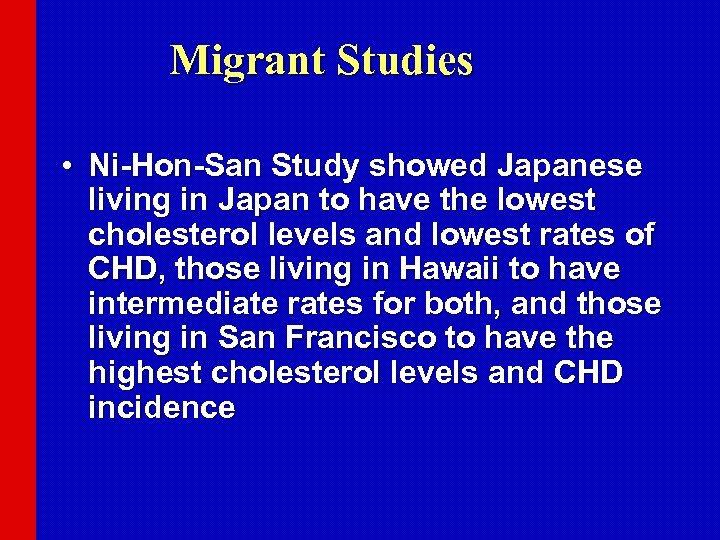
Migrant Studies • Ni-Hon-San Study showed Japanese living in Japan to have the lowest cholesterol levels and lowest rates of CHD, those living in Hawaii to have intermediate rates for both, and those living in San Francisco to have the highest cholesterol levels and CHD incidence
Approaches to Primary and Secondary Prevention of CVD • Primary prevention involves prevention of onset of disease in persons without symptoms. • Primordial prevention involves the prevention of risk factors causative o the disease, thereby reducing the likelihood of development of the disease. • Secondary prevention refers to the prevention of death or recurrence of disease in those who are already symptomatic
Risk Factor Concepts in Primary Prevention • Nonmodifiable risk factors include age, sexc, race, and family history of CVD, which can identify high-risk populations • Behavioral risk factors include sedentary lifestyle, unhealthful diet, heavy alcohol or cigarette consumption. • Physiological risk factors include hypertension, obesity, lipid problems, and diabetes, which may be a consequence of behavioral risk factors.
Population vs. High-Risk Approach • Risk factors, such as cholesterol or blood pressure, have a wide bell-shaped distribution, often with a “tail” of high values. • The “high-risk approach” involves identification and intensive treatment of those at the high end of the “tail”, often at greatest risk of CVD, reducing levels to “normal”. • But most cases of CVD do not occur among the highest levels of a given risk factor, and in fact, occur among those in the “average” risk group. • Significant reduction in the population burden of CVD can occur only from a “population approach” shifting the entire population distribution to lower levels.
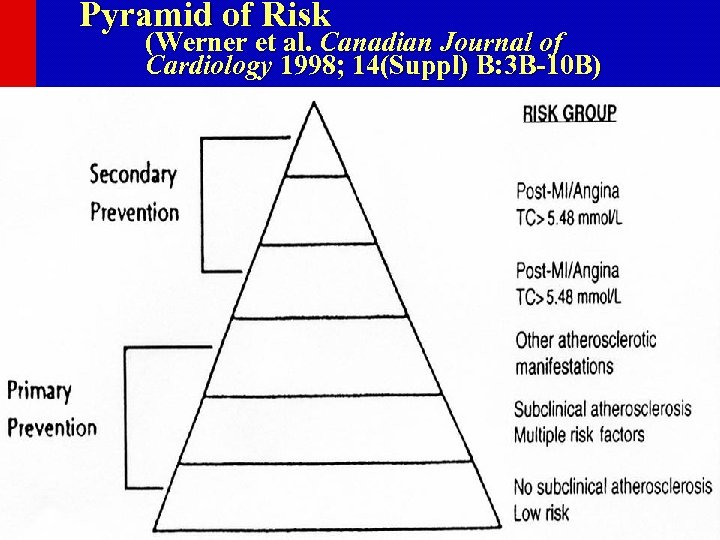
Pyramid of Risk (Werner et al. Canadian Journal of Cardiology 1998; 14(Suppl) B: 3 B-10 B)
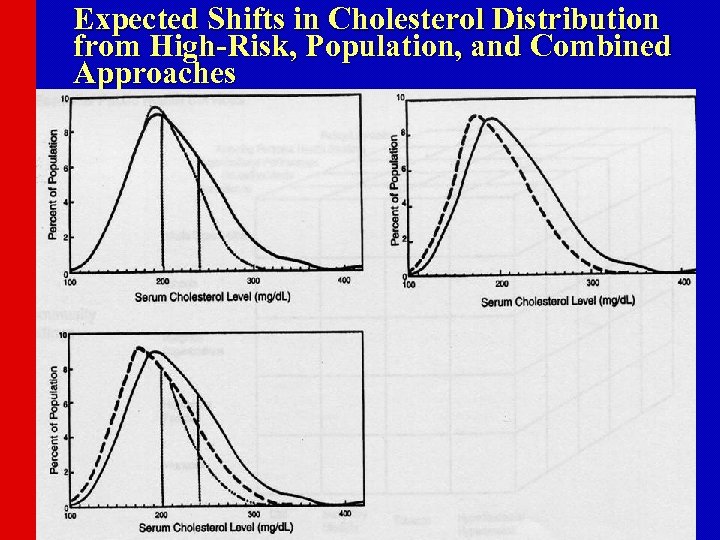
Expected Shifts in Cholesterol Distribution from High-Risk, Population, and Combined Approaches
Population and Community-Wide CVD Risk Reduction Approaches • Populations with high rates of CVD are those with Western lifestyles of high-fat diets, physical inactivity, and tobacco use. • Targets of a population-wide approach must be these behaviors causative of the physiologic risk factors or directly causative of CVD. • Requires public health services such as surveillance (e. g. , BFRSS), education (AHA, NCEP), organizational partnerships (Singapore Declaration), and legislation/policy (Anti-Tobacco policies) • Activities in a variety of community settings: schools, worksites, churches, healthcare facilities, entire communities
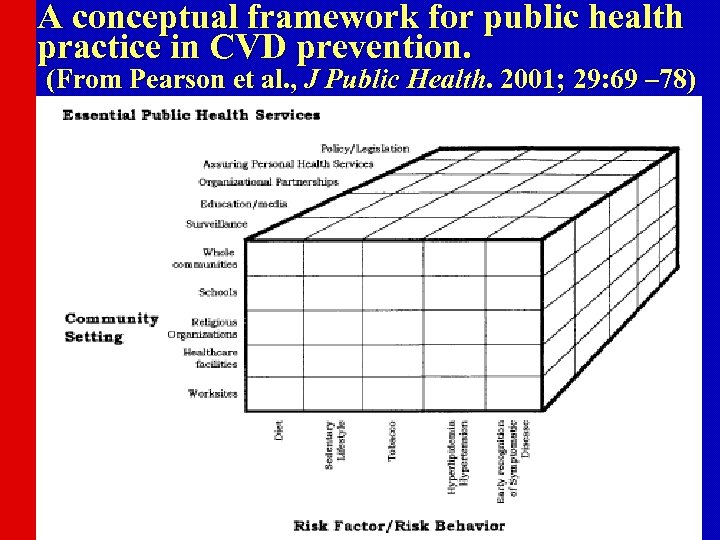
A conceptual framework for public health practice in CVD prevention. (From Pearson et al. , J Public Health. 2001; 29: 69 – 78)
Communitywide CVD Prevention Programs • Stanford 3 -Community Study (1972 -75) showed mass media vs. no intervention in high-risk residents to result in 23% reduction in CHD risk score • North Karelia (1972 -) showed public education campaign to reduce smoking, fat consumption, blood pressure, and cholesterol • Stanford 5 -City Project (1980 -86) showed reductions in smoking, cholesterol, BP, and CHD risk • Minnesota Heart Health Program (1980 -88) showed some increases in physical activity and in women reductions in smoking

Materials Developed for US Community Intervention Trials • • • Mass media, brochures and direct mail Events and contests Screenings Group and direct education School programs and worksite interventions Physician and medical setting programs Grocery store and restaurant projects Church interventions Policies
Individual and High-Risk Approaches • Primary Prevention Guidelines (1995) and Secondary Prevention Guidelines (Revised 2001) released by the American Heart Association provide advice regarding risk factor assessment, lifestyle modification, and pharmacologic interventions for specific risk factors • Barriers exist in the community and healthcare setting that prevent efficient risk reduction • Surveys of CVD prevention-related services show disappointing results regarding cholesterol-lowering therapy, smoking cessation, and other measures of risk reduction
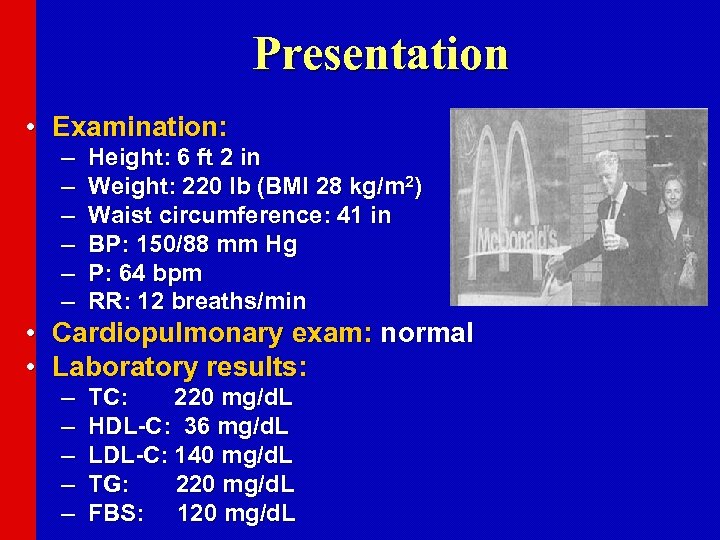
Presentation • Examination: – – – Height: 6 ft 2 in Weight: 220 lb (BMI 28 kg/m 2) Waist circumference: 41 in BP: 150/88 mm Hg P: 64 bpm RR: 12 breaths/min • Cardiopulmonary exam: normal • Laboratory results: – – – TC: 220 mg/d. L HDL-C: 36 mg/d. L LDL-C: 140 mg/d. L TG: 220 mg/d. L FBS: 120 mg/d. L
Risk Assessment Count major risk factors • For patients with multiple (2+) risk factors – Perform 10 -year risk assessment • For patients with 0– 1 risk factor – 10 year risk assessment not required – Most patients have 10 -year risk <10%
ATP III Assessment of CHD Risk For persons without known CHD, other forms of atherosclerotic disease, or diabetes: • Count the number of risk factors: – Cigarette smoking – Hypertension (BP 140/90 mm. Hg or on antihypertensive medication) – Low HDL cholesterol (<40 mg/d. L)† – Family history of premature CHD u CHD in male first degree relative <55 years u CHD in female first degree relative <65 years – Age (men 45 years; women 55 years) • Use Framingham scoring for persons with 2 risk factors* (or with metabolic syndrome) to determine the absolute 10 -year CHD risk. (downloadable risk algorithms at www. nhlbi. nih. gov)
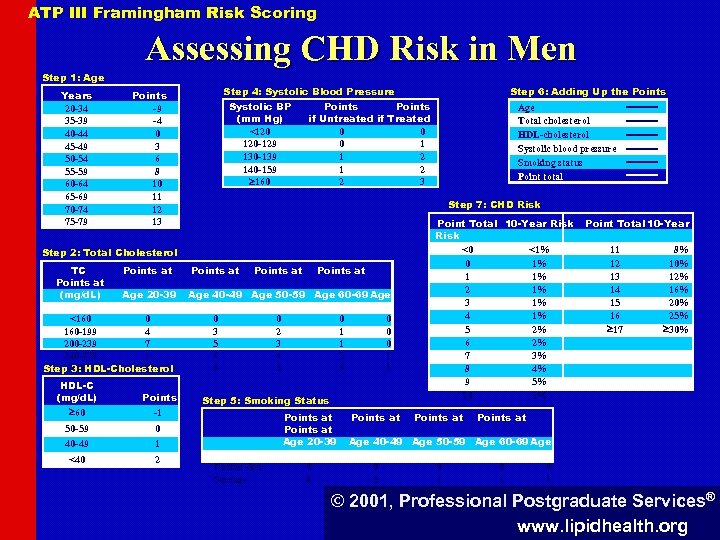
ATP III Framingham Risk Scoring Assessing CHD Risk in Men Step 1: Age Years 20 -34 35 -39 40 -44 45 -49 50 -54 55 -59 60 -64 65 -69 70 -74 75 -79 Step 4: Systolic Blood Pressure Points -9 -4 0 3 6 8 10 11 12 13 Systolic BP (mm Hg) <120 120 -129 130 -139 140 -159 160 Points if Untreated if Treated 0 0 0 1 1 2 2 3 HDL-C (mg/d. L) 60 Points -1 50 -59 1 <40 2 Points at Age 40 -49 Age 50 -59 Age 60 -69 Age 0 3 5 6 8 0 40 -49 Age Total cholesterol HDL-cholesterol Systolic blood pressure Smoking status Point total Step 7: CHD Risk Step 2: Total Cholesterol TC Points at (mg/d. L) Age 20 -39 70 -79 <160 0 160 -199 4 200 -239 7 240 -279 9 11 Step 280 3: HDL-Cholesterol Step 6: Adding Up the Points 0 2 3 4 5 0 1 1 2 3 0 0 0 1 1 Step 5: Smoking Status 70 -79 Nonsmoker Smoker Points at Age 20 -39 0 8 Points at Point Total 10 -Year Risk <0 <1% 0 1% 1 1% 2 1% 3 1% 4 1% 5 2% 6 2% 7 3% 8 4% 9 5% 10 6% Points at Point Total 10 -Year 11 12 13 14 15 16 17 8% 10% 12% 16% 20% 25% 30% Points at Age 40 -49 Age 50 -59 Age 60 -69 Age 0 5 0 3 0 1 © 2001, Professional Postgraduate Services® www. lipidhealth. org
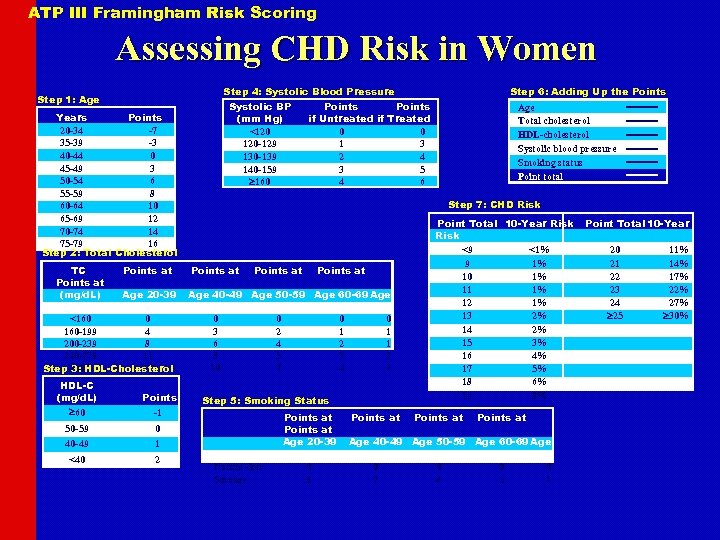
ATP III Framingham Risk Scoring Assessing CHD Risk in Women Step 4: Systolic Blood Pressure Step 1: Age Systolic BP (mm Hg) <120 120 -129 130 -139 140 -159 160 Years Points 20 -34 -7 35 -39 -3 40 -44 0 45 -49 3 50 -54 6 55 -59 8 60 -64 10 65 -69 12 70 -74 14 75 -79 16 Step 2: Total Cholesterol TC Points at (mg/d. L) Age 20 -39 70 -79 <160 0 160 -199 4 200 -239 8 240 -279 11 13 Step 280 3: HDL-Cholesterol HDL-C (mg/d. L) 60 Points -1 50 -59 1 <40 2 Points if Untreated if Treated 0 0 1 3 2 4 3 5 4 6 Age Total cholesterol HDL-cholesterol Systolic blood pressure Smoking status Point total Step 7: CHD Risk Points at Age 40 -49 Age 50 -59 Age 60 -69 Age 0 3 6 8 10 0 40 -49 Step 6: Adding Up the Points 0 2 4 5 7 0 1 2 3 4 0 1 1 2 2 Step 5: Smoking Status 70 -79 Nonsmoker Smoker Points at Age 20 -39 0 9 Points at Point Total 10 -Year Risk <9 <1% 9 1% 10 1% 11 1% 12 1% 13 2% 14 2% 15 3% 16 4% 17 5% 18 6% 19 8% Points at Age 40 -49 Age 50 -59 Age 60 -69 Age 0 7 0 4 0 2 0 1 Point Total 10 -Year 20 21 22 23 24 25 11% 14% 17% 22% 27% 30%
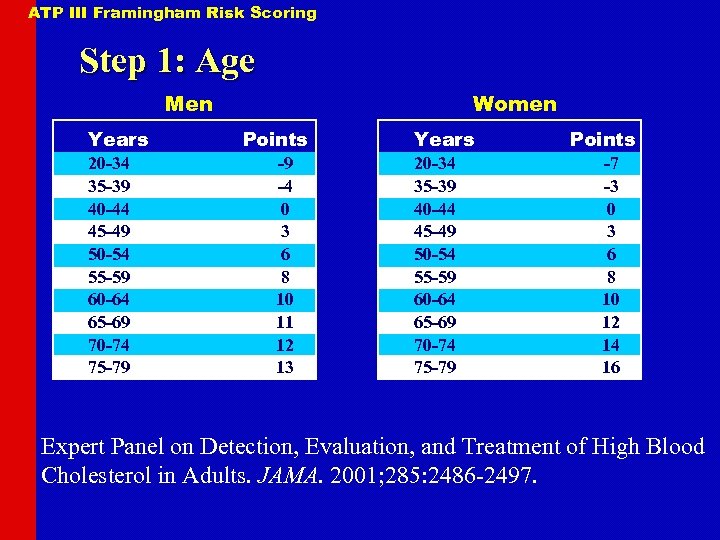
ATP III Framingham Risk Scoring Step 1: Age Men Years 20 -34 35 -39 40 -44 45 -49 50 -54 55 -59 60 -64 65 -69 70 -74 75 -79 Women Points -9 -4 0 3 6 8 10 11 12 13 Years 20 -34 35 -39 40 -44 45 -49 50 -54 55 -59 60 -64 65 -69 70 -74 75 -79 Points -7 -3 0 3 6 8 10 12 14 16 Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA. 2001; 285: 2486 -2497.
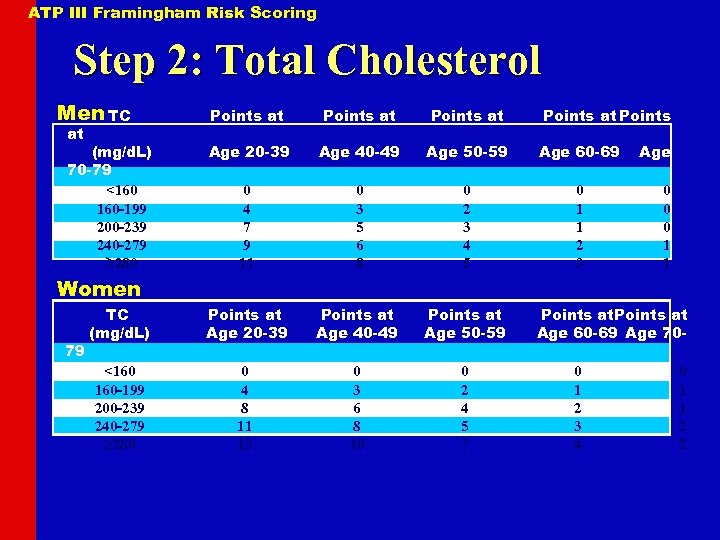
ATP III Framingham Risk Scoring Step 2: Total Cholesterol Men TC Points at Points Age 20 -39 Age 40 -49 Age 50 -59 Age 60 -69 0 4 7 9 11 0 3 5 6 8 0 2 3 4 5 0 1 1 2 3 TC (mg/d. L) Points at Age 20 -39 Points at Age 40 -49 Points at Age 50 -59 <160 160 -199 200 -239 240 -279 280 0 4 8 11 13 0 3 6 8 10 0 2 4 5 7 at (mg/d. L) 70 -79 <160 160 -199 200 -239 240 -279 280 Age 0 0 0 1 1 Women 79 Points at Age 60 -69 Age 700 1 2 3 4 0 1 1 2 2
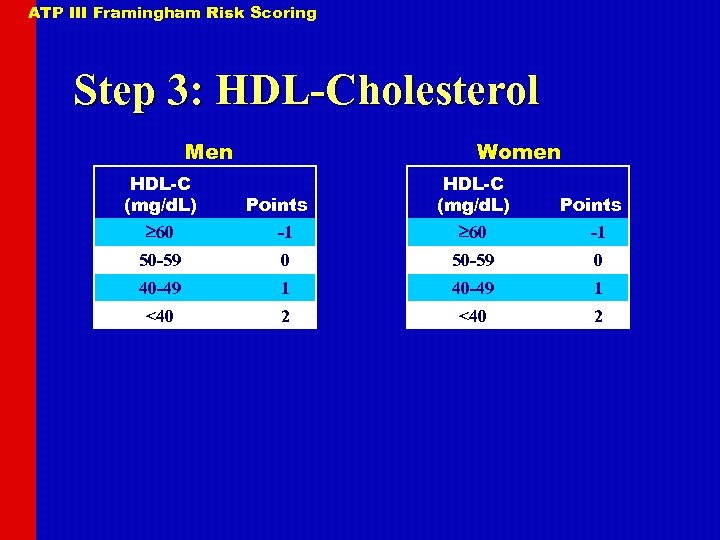
ATP III Framingham Risk Scoring Step 3: HDL-Cholesterol Men HDL-C (mg/d. L) 60 Women Points -1 HDL-C (mg/d. L) 60 Points -1 50 -59 0 40 -49 1 <40 2
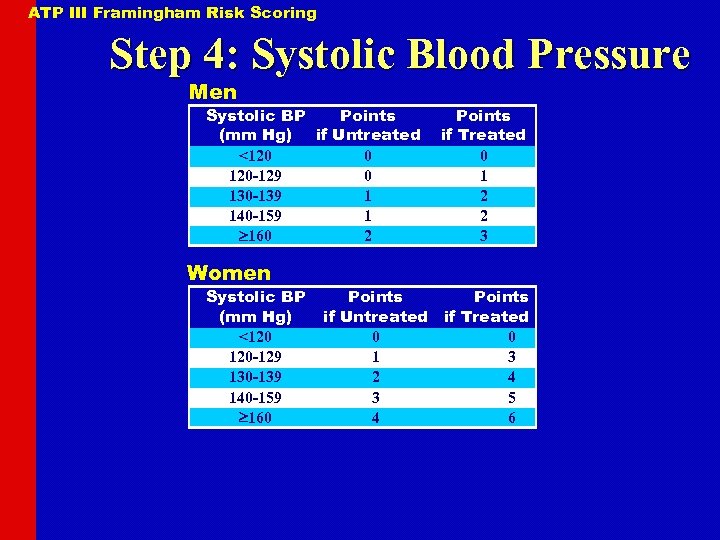
ATP III Framingham Risk Scoring Step 4: Systolic Blood Pressure Men Systolic BP Points (mm Hg) if Untreated <120 0 120 -129 0 130 -139 1 140 -159 1 160 2 Women Systolic BP (mm Hg) <120 120 -129 130 -139 140 -159 160 Points if Treated 0 1 2 2 3 Points if Untreated if Treated 0 0 1 3 2 4 3 5 4 6
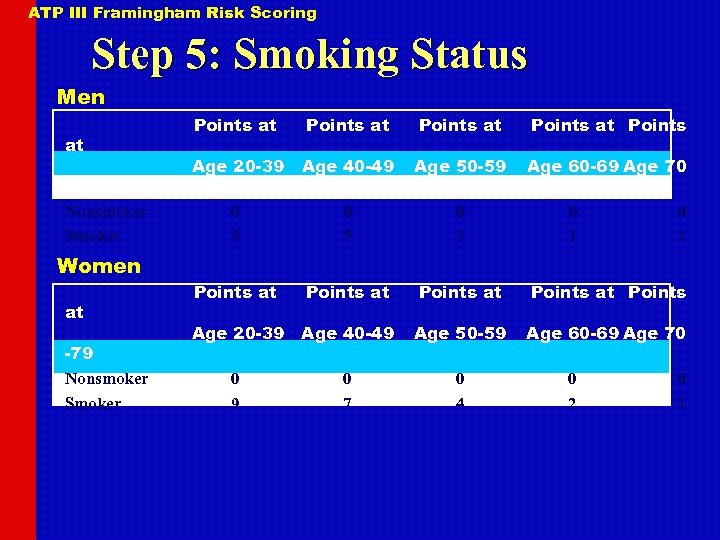
ATP III Framingham Risk Scoring Step 5: Smoking Status Men at -79 Nonsmoker Smoker Women at -79 Nonsmoker Smoker Points at Points Age 20 -39 Age 40 -49 Age 50 -59 Age 60 -69 Age 70 0 8 0 5 0 3 Points at Points Age 20 -39 Age 40 -49 Age 50 -59 Age 60 -69 Age 70 0 9 0 7 0 4 0 1 0 2 0 1
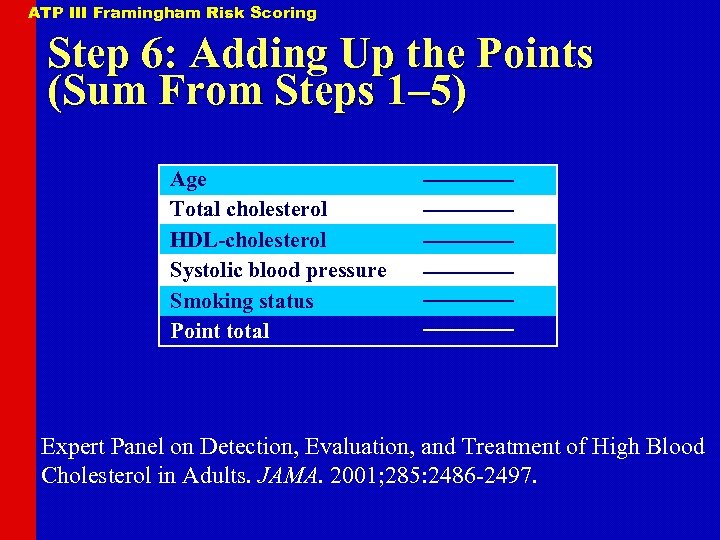
ATP III Framingham Risk Scoring Step 6: Adding Up the Points (Sum From Steps 1– 5) Age Total cholesterol HDL-cholesterol Systolic blood pressure Smoking status Point total Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA. 2001; 285: 2486 -2497.
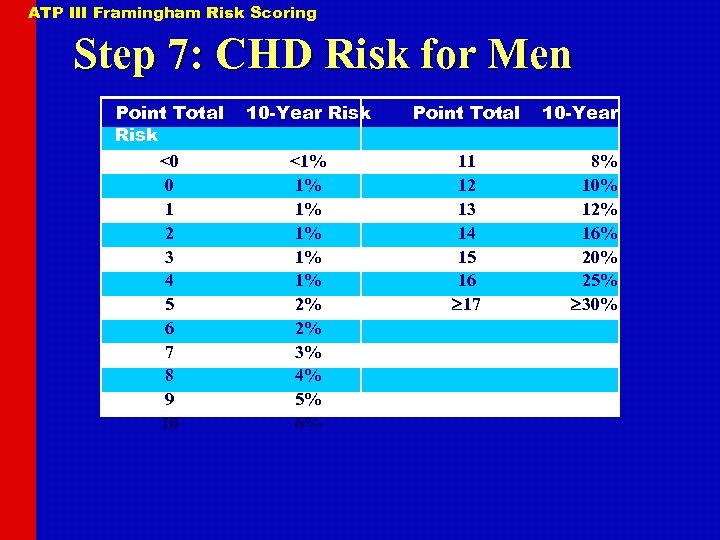
ATP III Framingham Risk Scoring Step 7: CHD Risk for Men Point Total Risk <0 0 1 2 3 4 5 6 7 8 9 10 10 -Year Risk Point Total <1% 1% 1% 2% 2% 3% 4% 5% 6% 11 12 13 14 15 16 17 10 -Year 8% 10% 12% 16% 20% 25% 30%
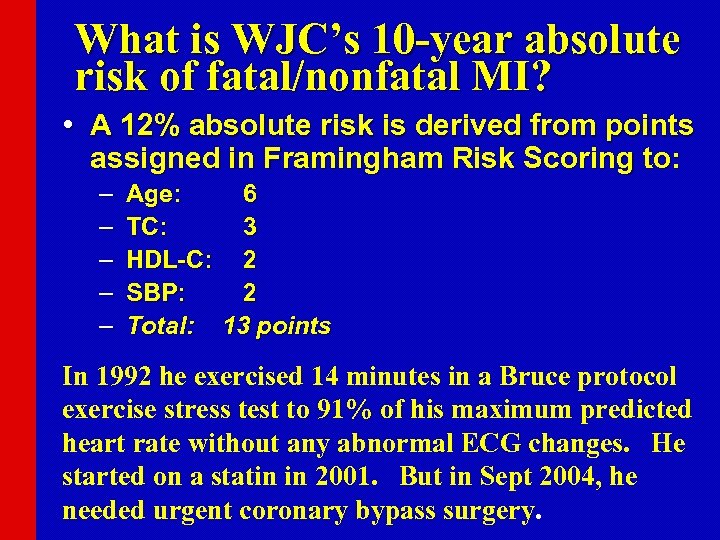
What is WJC’s 10 -year absolute risk of fatal/nonfatal MI? • A 12% absolute risk is derived from points assigned in Framingham Risk Scoring to: – – – Age: 6 TC: 3 HDL-C: 2 SBP: 2 Total: 13 points In 1992 he exercised 14 minutes in a Bruce protocol exercise stress test to 91% of his maximum predicted heart rate without any abnormal ECG changes. He started on a statin in 2001. But in Sept 2004, he needed urgent coronary bypass surgery.
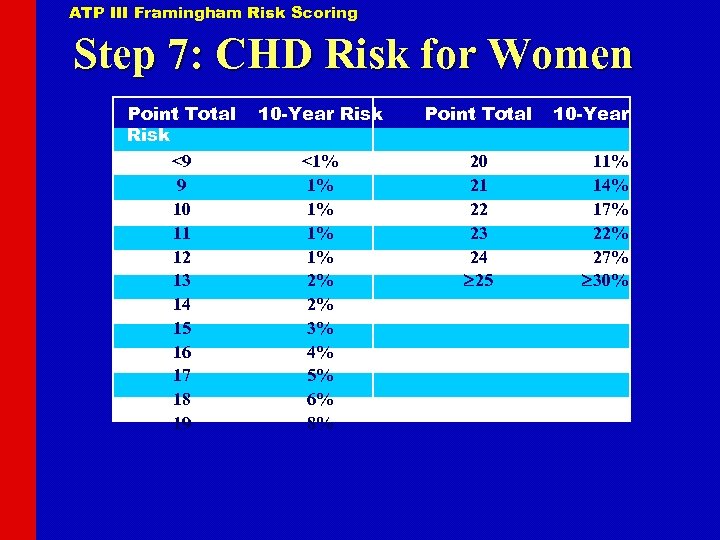
ATP III Framingham Risk Scoring Step 7: CHD Risk for Women Point Total Risk <9 9 10 11 12 13 14 15 16 17 18 19 10 -Year Risk Point Total <1% 1% 1% 2% 2% 3% 4% 5% 6% 8% 20 21 22 23 24 25 10 -Year 11% 14% 17% 22% 27% 30%
CHD Risk Equivalents • Risk for major coronary events equal to that in established CHD • 10 -year risk for hard CHD >20% Hard CHD = myocardial infarction + coronary death
Diabetes as a CHD Risk Equivalent • 10 -year risk for CHD 20% • High mortality with established CHD – High mortality with acute MI – High mortality post acute MI
CHD Risk Equivalents • Other clinical forms of atherosclerotic disease (peripheral arterial disease, abdominal aortic aneurysm, and symptomatic carotid artery disease) • Diabetes • Multiple risk factors that confer a 10 -year risk for CHD >20%
729beb825675f466c5cd1f91b92cdbb5.ppt