8069d30d68b324ea3f13bbf1031ea7e2.ppt
- Количество слайдов: 48
International Classification of Functioning, disability and health (ICF) Dr Alison Laver-Fawcett March 2017
Overview of this session • Background and introduction to the ICF • Relevance of the ICF for allied health professionals • Applying ICF • ICF Checklist • Assessments Worksheet and the ICF
• Models can be applied to help therapists to gain an overview of the whole and understand how discrete parts can or may inter-relate. • An explicit application of a model of function can help an individual therapist, a therapy service or a MDT to review their practice and facilitate communication about assessment, outcome measurement and intervention.
Why use a model like the ICF? • Many rehabilitation professionals work in interprofessional and inter-agency teams. • Models can help each team member identify their primary domain of concern for assessment, management and intervention. • A model can assist the team to identify: – areas where there is overlap in the assessment data collected; – any gaps or omissions where a level of functioning has not been adequately assessed or treated by team members.
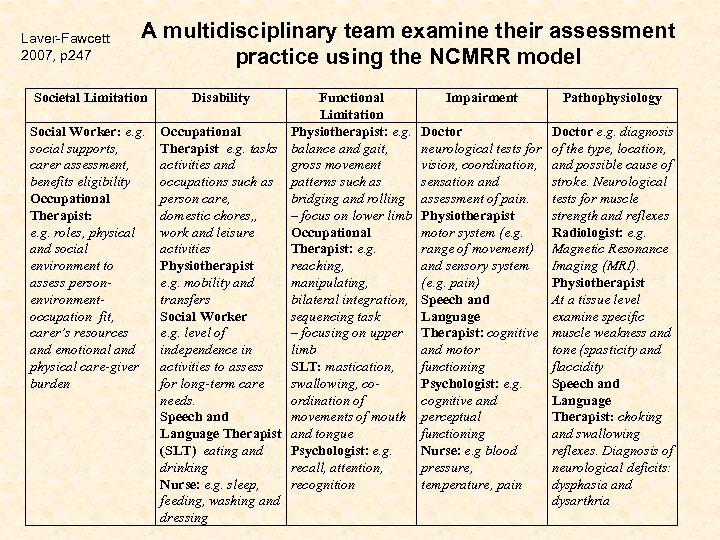
Laver-Fawcett 2007, p 247 A multidisciplinary team examine their assessment practice using the NCMRR model Societal Limitation Social Worker: e. g. social supports, carer assessment, benefits eligibility Occupational Therapist: e. g. roles, physical and social environment to assess personenvironmentoccupation fit, carer’s resources and emotional and physical care-giver burden Disability Functional Limitation Occupational Physiotherapist: e. g. Therapist e. g. tasks balance and gait, activities and gross movement occupations such as patterns such as person care, bridging and rolling domestic chores, , – focus on lower limb work and leisure Occupational activities Therapist: e. g. Physiotherapist reaching, e. g. mobility and manipulating, transfers bilateral integration, Social Worker sequencing task e. g. level of – focusing on upper independence in limb activities to assess SLT: mastication, for long-term care swallowing, coneeds. ordination of Speech and movements of mouth Language Therapist and tongue (SLT) eating and Psychologist: e. g. drinking recall, attention, Nurse: e. g. sleep, recognition feeding, washing and dressing Impairment Pathophysiology Doctor neurological tests for vision, coordination, sensation and assessment of pain. Physiotherapist motor system (e. g. range of movement) and sensory system (e. g. pain) Speech and Language Therapist: cognitive and motor functioning Psychologist: e. g. cognitive and perceptual functioning Nurse: e. g blood pressure, temperature, pain Doctor e. g. diagnosis of the type, location, and possible cause of stroke. Neurological tests for muscle strength and reflexes Radiologist: e. g. Magnetic Resonance Imaging (MRI). Physiotherapist At a tissue level examine specific muscle weakness and tone (spasticity and flaccidity Speech and Language Therapist: choking and swallowing reflexes. Diagnosis of neurological deficits: dysphasia and dysarthria
World Health Organisation • “WHO is the directing and coordinating authority for health within the United Nations system. It is responsible for providing leadership on global health matters, shaping the health research agenda, setting norms and standards, articulating evidence-based policy options, providing technical support to countries and monitoring and assessing health trends. ” • See WHO website for further information: http: //www. who. int/about/en/ [accessed 20. 3. 2017]
World Health Organisation (2002) Towards a Common Language for Functioning, Disability and Health (ICF). Geneva: WHO Can be downloaded as a pdf file from the WHO website http: //www. who. int/classifications/icf/en/ [accessed 21. 3. 2017] ICF provides a classification of health and health related domains ICF was endorsed by 191 WHO member states in May 2001 as the international standard to describe and measure health and disability
![ICF online Browser • http: //apps. who. int/classifications/icfbro wser/ [accessed 21. 3. 2017] 8 ICF online Browser • http: //apps. who. int/classifications/icfbro wser/ [accessed 21. 3. 2017] 8](https://present5.com/presentation/8069d30d68b324ea3f13bbf1031ea7e2/image-8.jpg)
ICF online Browser • http: //apps. who. int/classifications/icfbro wser/ [accessed 21. 3. 2017] 8
WHO and the ICIDH • One of the most widely recognised and accepted systems for defining function was developed by the World Health Organisation (WHO) and was called the International Classification of Impairments, Disabilities and Handicaps (ICIDH). • The purpose of the ICIDH was to provide a framework for classifying the consequences of injuries and disease (Hammell, 2004). The World Health Organisation (WHO) originally developed a three level hierarchy of dysfunction (1980).
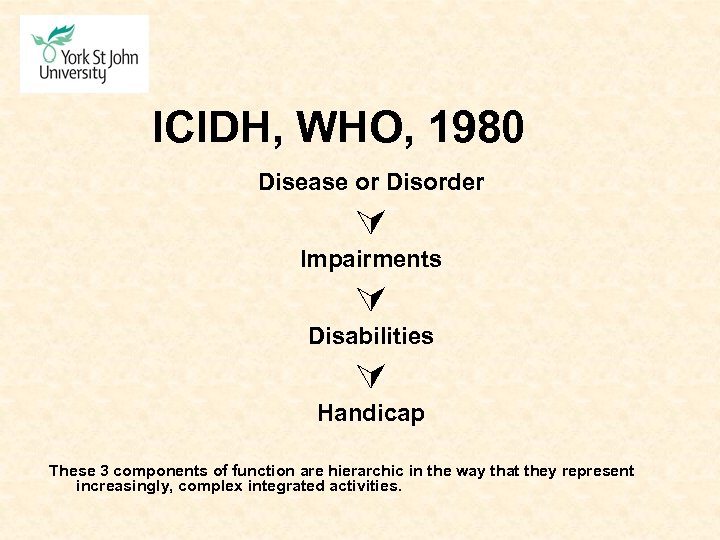
ICIDH, WHO, 1980 Disease or Disorder Impairments Disabilities Handicap These 3 components of function are hierarchic in the way that they represent increasingly, complex integrated activities.
Context for the ICF The original ICIDH (WHO, 1980) was revised for a number of reasons: • health and social care systems needed a uniform terminology; • there was a need for a tool that supports communication between people with disabilities and health and social care professionals; • there was a need to produce “a tool that documents outcomes using a classification system that is appropriate for and acceptable to all who use it” (Chard, 2004, p. 1)
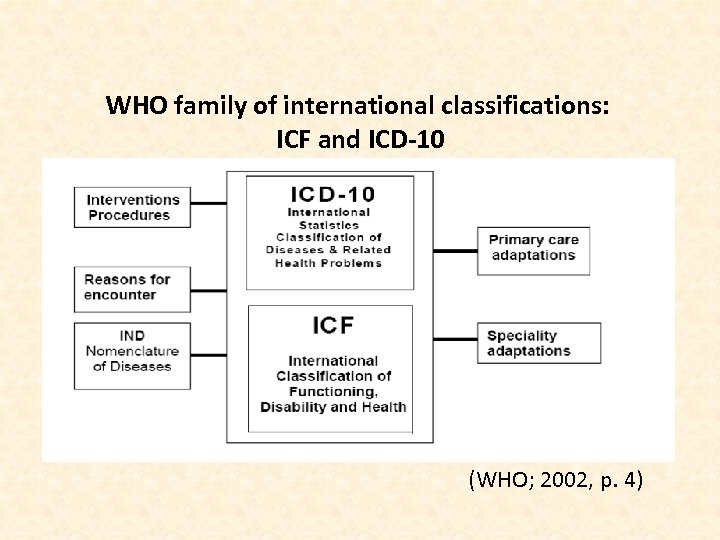
WHO family of international classifications: ICF and ICD-10 (WHO; 2002, p. 4)
ICF Aims • to provide a scientific basis for exploring the consequences of health conditions • to establish a common language to improve communication • to permit comparison of data across: – countries – health care disciplines – services – time • to provide a systematic coding scheme for health information systems
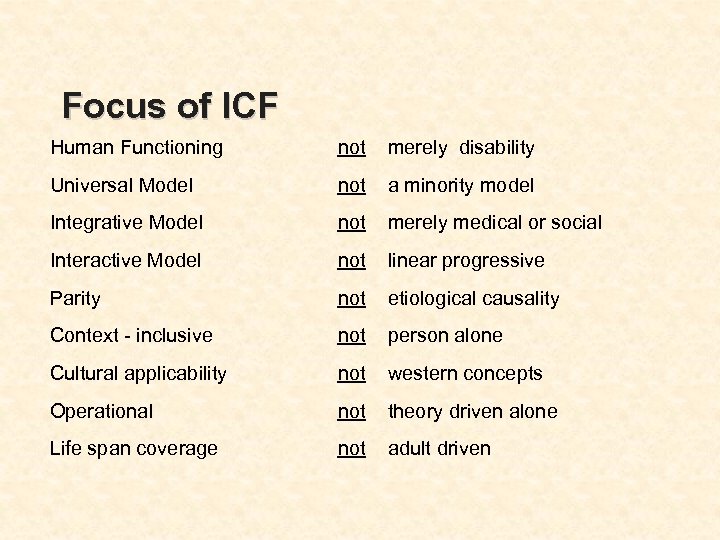
Focus of ICF Human Functioning not merely disability Universal Model not a minority model Integrative Model not merely medical or social Interactive Model not linear progressive Parity not etiological causality Context - inclusive not person alone Cultural applicability not western concepts Operational not theory driven alone Life span coverage not adult driven
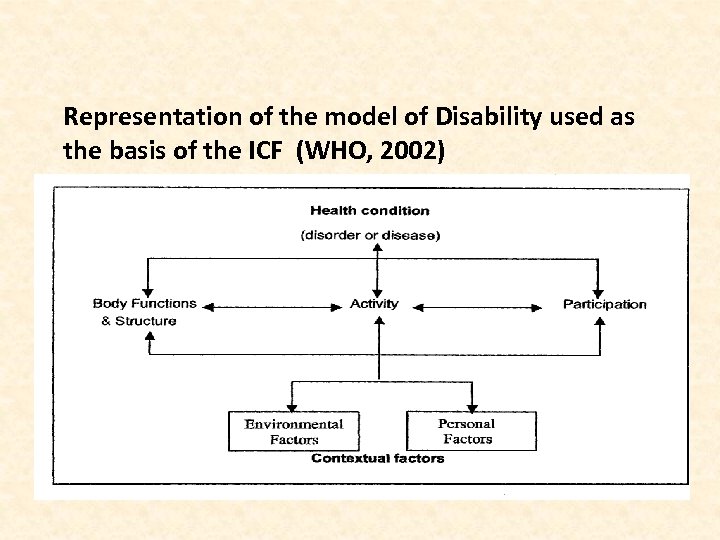
Representation of the model of Disability used as the basis of the ICF (WHO, 2002)
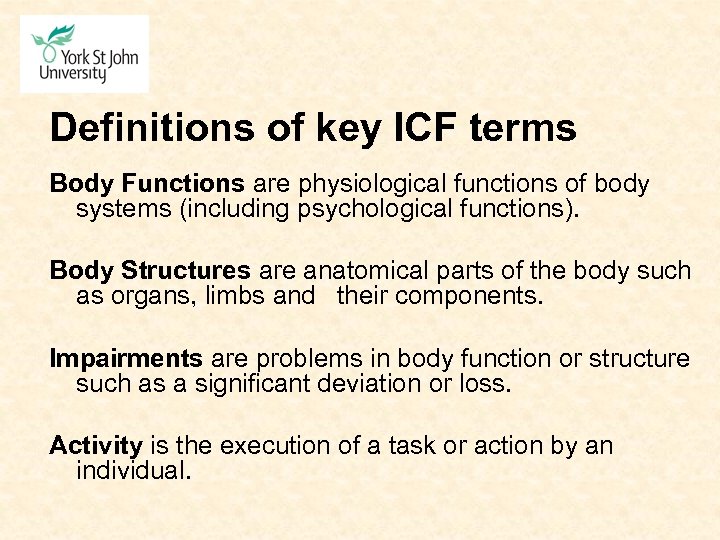
Definitions of key ICF terms Body Functions are physiological functions of body systems (including psychological functions). Body Structures are anatomical parts of the body such as organs, limbs and their components. Impairments are problems in body function or structure such as a significant deviation or loss. Activity is the execution of a task or action by an individual.
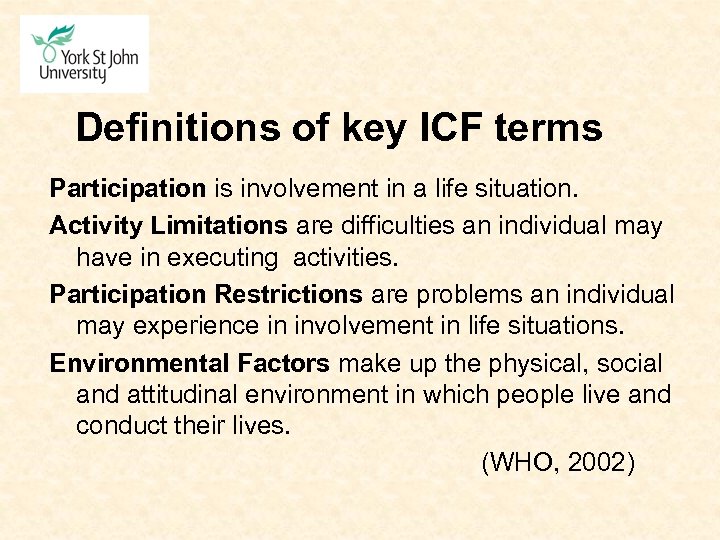
Definitions of key ICF terms Participation is involvement in a life situation. Activity Limitations are difficulties an individual may have in executing activities. Participation Restrictions are problems an individual may experience in involvement in life situations. Environmental Factors make up the physical, social and attitudinal environment in which people live and conduct their lives. (WHO, 2002)
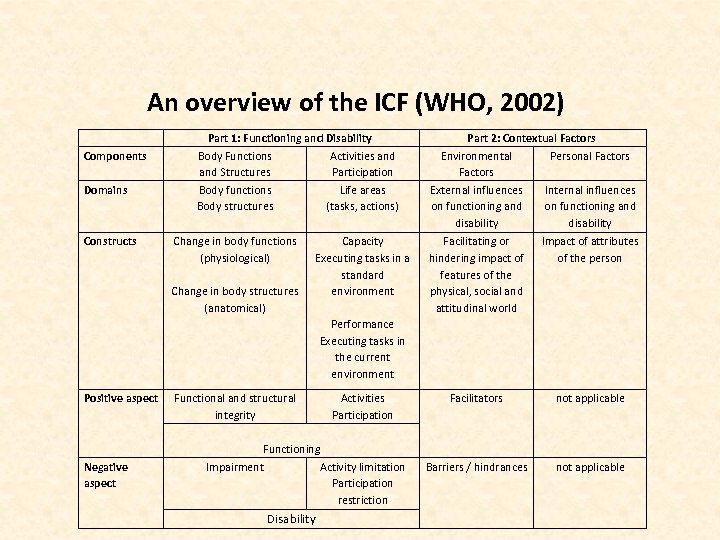
An overview of the ICF (WHO, 2002) Components Domains Constructs Part 1: Functioning and Disability Body Functions Activities and Structures Participation Body functions Life areas Body structures (tasks, actions) Change in body functions (physiological) Change in body structures (anatomical) Capacity Executing tasks in a standard environment Part 2: Contextual Factors Environmental Personal Factors External influences Internal influences on functioning and disability Facilitating or hindering impact of features of the physical, social and attitudinal world Impact of attributes of the person Facilitators not applicable Barriers / hindrances not applicable Performance Executing tasks in the current environment Positive aspect Negative aspect Functional and structural integrity Activities Participation Functioning Impairment Activity limitation Participation restriction Disability
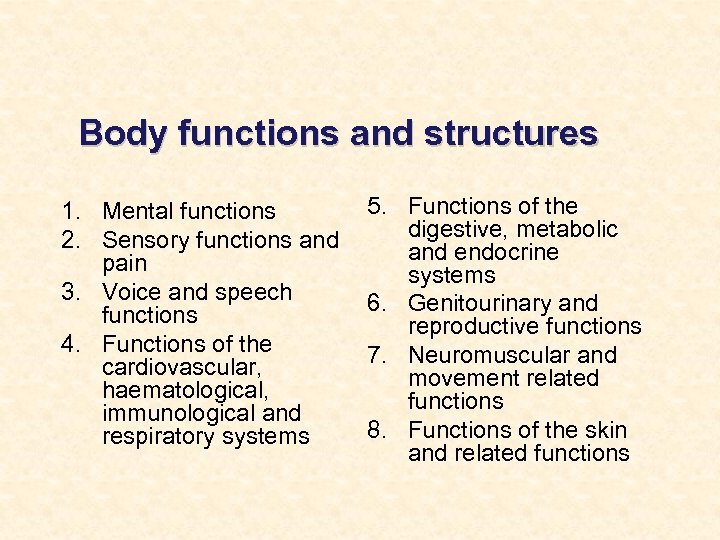
Body functions and structures 1. Mental functions 2. Sensory functions and pain 3. Voice and speech functions 4. Functions of the cardiovascular, haematological, immunological and respiratory systems 5. Functions of the digestive, metabolic and endocrine systems 6. Genitourinary and reproductive functions 7. Neuromuscular and movement related functions 8. Functions of the skin and related functions
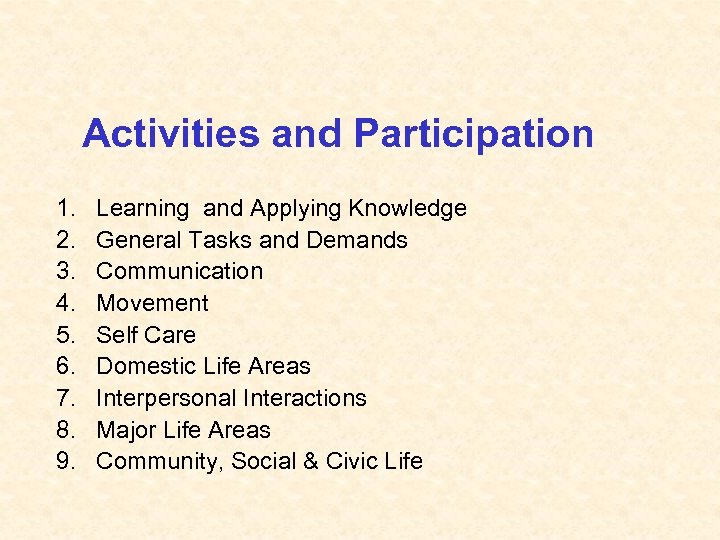
Activities and Participation 1. 2. 3. 4. 5. 6. 7. 8. 9. Learning and Applying Knowledge General Tasks and Demands Communication Movement Self Care Domestic Life Areas Interpersonal Interactions Major Life Areas Community, Social & Civic Life
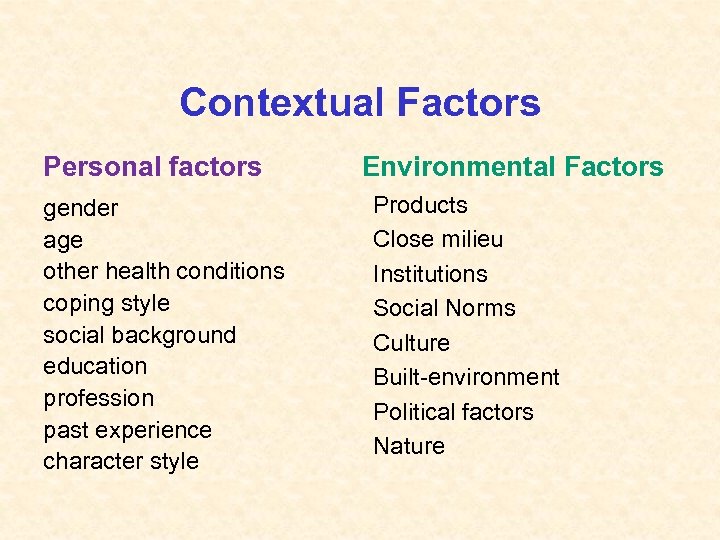
Contextual Factors Personal factors gender age other health conditions coping style social background education profession past experience character style Environmental Factors Products Close milieu Institutions Social Norms Culture Built-environment Political factors Nature
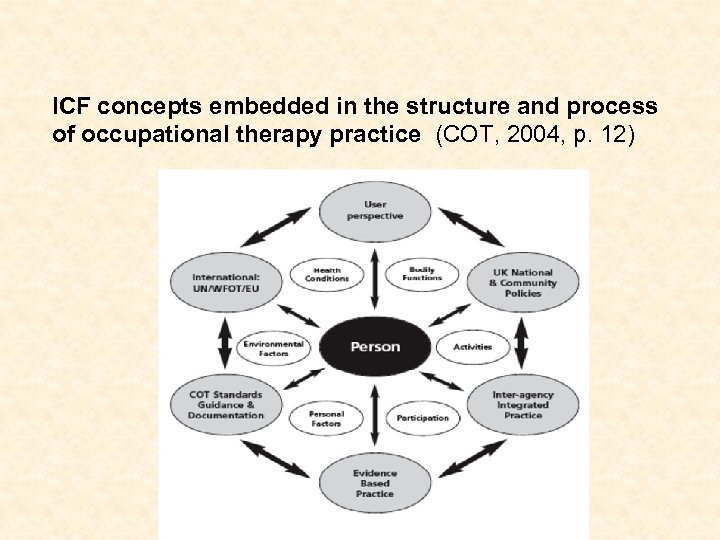
ICF concepts embedded in the structure and process of occupational therapy practice (COT, 2004, p. 12)
Applying the ICF at the individual level • For the assessment of individuals: – What is the person's level of functioning? • For individual treatment planning: – What treatments or interventions can maximize functioning? • For the evaluation of treatment and other interventions: – What are the outcomes of the treatment? – How useful were the interventions? • For communication among physicians, nurses, physiotherapists, occupational therapists and other health works, social service works and community agencies. • For self-evaluation by consumers: – How would I rate my capacity in mobility or communication? (WHO, 2002, p. 6)
ICF Applications: Service Provision At the institutional level… • For educational and training purposes • For resource planning and development: What health care and other services will be needed? • For quality improvement: How well do we serve our clients? What basic indicators for quality assurance are valid and reliable? • For management and outcome evaluation: How useful are the services we are providing? • For managed care models of health care delivery: How costeffective are the services we provide? How can the service be improved for better outcomes at a lower cost?
ICF Applications: Service Provision At the social level: • For eligibility criteria for state entitlements such as social security benefits, disability pensions, workers’ compensation and insurance: Are the criteria for eligibility for disability benefits evidence based, appropriate to social goals and justifiable? • For social policy development, including legislative reviews, model legislation, regulations and guidelines, and definitions for antidiscrimination legislation: • Will guaranteeing rights improve functioning at the societal level? • Can we measure this improvement and adjust our policy and law accordingly?
ICF Applications: Service Provision At the social level (continued) • For needs assessments: What are the needs of persons with various levels of disability -impairments, activity limitations and participation restrictions? • For environmental assessment for universal design, implementation of mandated accessibility, identification of environmental facilitators and barriers, and changes to social policy: How can we make the social and built environment more accessible for all person, those with and those without disabilities? Can we assess and measure improvement?
ICF Checklist • http: //www. who. int/classifications/icf checklist. pdf? ua=1 • [accessed 21. 3. 2017] 27
ICF Checklist © World Health Organization, September 2003. • The ICF Checklist is a practical tool to elicit and record information on the functioning and disability of an individual. This information can be summarized for case records (for example, in clinical practice or social work). The checklist should be used along with the ICF or ICF Pocket version. • When completing this checklist, use all information available. E. g • [1] written records [2] primary respondent [3] other informants [4] direct observation • Appendix 1: provides a Brief Health Information checklist (p 910) which can be completed by the respondent.
PART 1 a: IMPAIRMENTS of BODY FUNCTIONS First Qualifier: Extent of impairments • 0 No impairment means the person has no problem • 1 Mild impairment means a problem that is present less than 25% of the time, with an intensity a person can tolerate and which happens rarely over the last 30 days. • 2 Moderate impairment means that a problem that is present less than 50% of the time, with an intensity, which is interfering in the persons day to day life and which happens occasionally over the last 30 days.
PART 1 a: IMPAIRMENTS of BODY FUNCTIONS • 3 Severe impairment means that a problem that is present more than 50% of the time, with an intensity, which is partially disrupting the persons day to day life and which happens frequently over the last 30 days. • 4 Complete impairment means that a problem that is present more than 95% of the time, with an intensity, which is totally disrupting the persons day to day life and which happens every day over the last 30 days. • 8 Not specified means there is insufficient information to specify the severity of the impairment. • 9 Not applicable means it is inappropriate to apply a particular code (e. g. b 650 Menstruation functions for woman in pre-menarche or post-menopause age).
PART 2: ACTIVITY LIMITATIONS & PARTICIPATION RESTRICTION • The Performance qualifier indicates the extent of Participation restriction by describing the persons actual performance of a task or action in his or her current environment. Because the current environment brings in the societal context, performance can also be understood as "involvement in a life situation" or "the lived experience“ of people in the actual context in which they live. This context includes the environmental factors – all aspects of the physical, social and attitudinal world that can be coded using the Environmental. • The Performance qualifier measures the difficulty the respondent experiences in doing things, assuming that they want to do them.
PART 2: ACTIVITY LIMITATIONS & PARTICIPATION RESTRICTION • The Capacity qualifier indicates the extent of Activity limitation by describing the person ability to execute a task or an action. The Capacity qualifier focuses on limitations that are inherent or intrinsic features of the person themselves. These limitations should be direct manifestations of the respondent's health state, without the assistance. By assistance we mean the help of another person, or assistance provided by an adapted or specially designed tool or vehicle, or any form of environmental modification to a room, home, workplace etc. . The level of capacity should be judged relative to that normally expected of the person, or the person's capacity before they acquired their health condition. • Note: Use Appendix 2 if needed to elicit information on the Activities and Participation of the individual
Appendix 2: GENERAL QUESTIONS FOR PARTICIPATION & ACTIVITIES Under each domain there are two kinds of probes: • The first probe tries to get the respondent to focus on his or her capacity to do a task or action, and in particular to focus on limitations in capacity that are inherent or intrinsic features of the person themselves. These limitations should be direct manifestations of the respondent's health state, without the assistance. • By assistance we mean the help of another person, or assistance provided by an adapted or specially designed tool or vehicle, or any form of environmental modification to a room, home, workplace and so on. • The level of capacity should be judged relative to that normally expected of the person, or the person's capacity before they acquired their health condition.
GENERAL QUESTIONS FOR PARTICIPATION & ACTIVITIES • The second probe focuses on the respondent's actual performance of a task or action in the person's actual situation or surroundings, and elicits information about the effects of environmental barriers or facilitators. • It is important to emphasize that you are only interested in the extent of difficulty the respondent has in doing things, assuming that they want to do them. Not doing something is irrelevant if the person chooses not to do it.
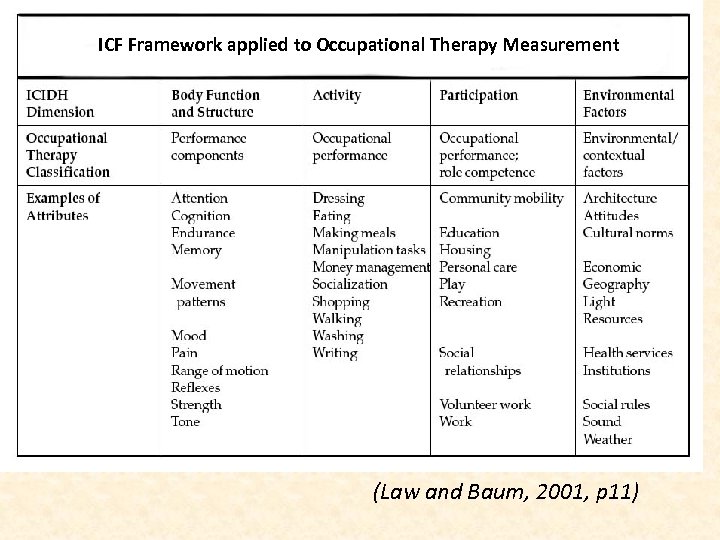
ICF Framework applied to Occupational Therapy Measurement (Law and Baum, 2001, p 11)
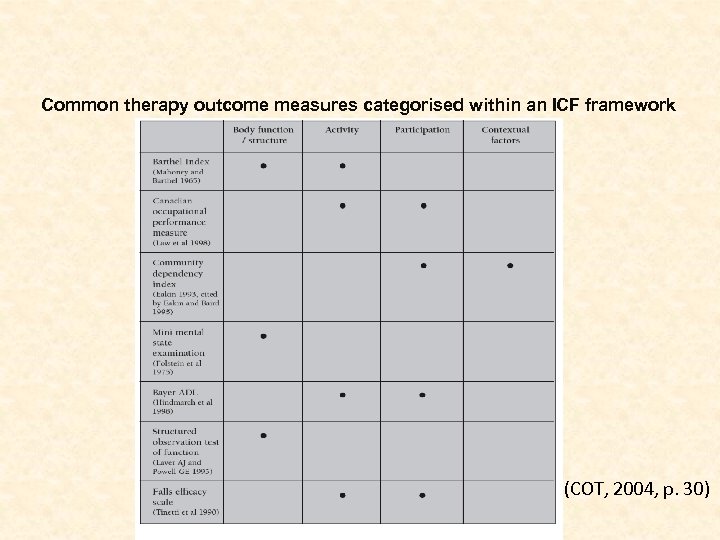
Common therapy outcome measures categorised within an ICF framework (COT, 2004, p. 30)
• Laver AJ, Powell, GE (1995) The Structured Observational Test of Function (SOTOF) NFER Nelson, Windsor
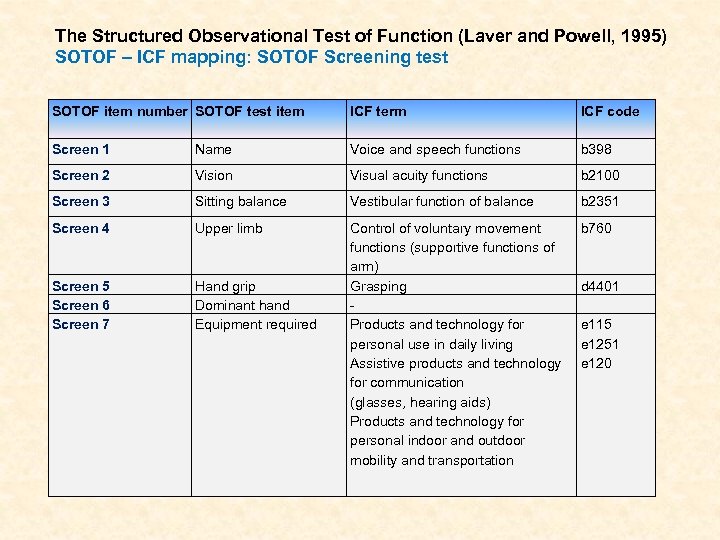
The Structured Observational Test of Function (Laver and Powell, 1995) SOTOF – ICF mapping: SOTOF Screening test SOTOF item number SOTOF test item ICF term ICF code Screen 1 Name Voice and speech functions b 398 Screen 2 Vision Visual acuity functions b 2100 Screen 3 Sitting balance Vestibular function of balance b 2351 Screen 4 Upper limb b 760 Screen 5 Screen 6 Screen 7 Hand grip Dominant hand Equipment required Control of voluntary movement functions (supportive functions of arm) Grasping Products and technology for personal use in daily living Assistive products and technology for communication (glasses, hearing aids) Products and technology for personal indoor and outdoor mobility and transportation d 4401 e 115 e 1251 e 120
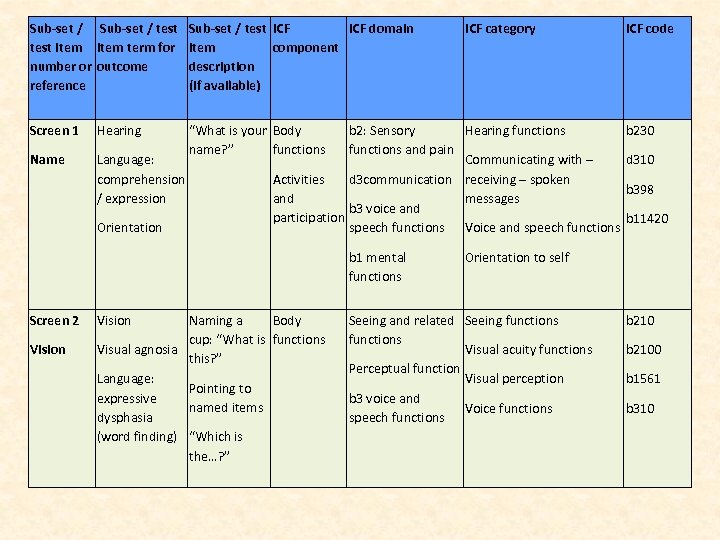
Sub-set / test item term for number or outcome reference Sub-set / test ICF domain item component description (if available) Screen 1 Hearing Name Language: comprehension / expression “What is your Body name? ” functions Orientation b 2: Sensory Hearing functions and pain Communicating with – Activities d 3 communication receiving – spoken and messages b 3 voice and participation speech functions Voice and speech functions b 1 mental functions Screen 2 Vision ICF category Naming a Body cup: “What is functions Visual agnosia this? ” Language: Pointing to expressive named items dysphasia (word finding) “Which is the…? ” ICF code b 230 d 310 b 398 b 11420 Orientation to self Seeing and related Seeing functions Visual acuity functions Perceptual function Visual perception b 3 voice and Voice functions speech functions b 2100 b 1561 b 310
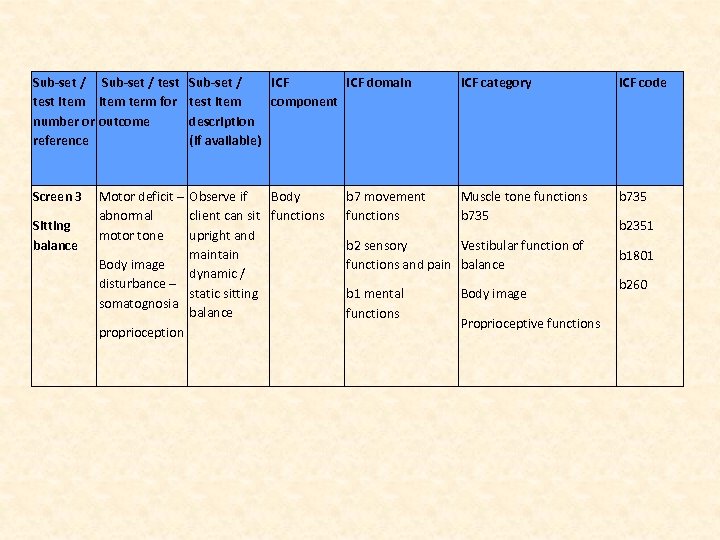
Sub-set / test item term for number or outcome reference Screen 3 Sitting balance Sub-set / ICF domain test item component description (if available) Motor deficit – Observe if Body abnormal client can sit functions motor tone upright and maintain Body image dynamic / disturbance – static sitting somatognosia balance proprioception b 7 movement functions ICF category ICF code Muscle tone functions b 735 b 2 sensory Vestibular function of functions and pain balance b 1 mental functions Body image Proprioceptive functions b 2351 b 1801 b 260
Future developments? • “. . . the ICF does not include a list of personal factors, as no international consensus could be achieved on the structure of such a list. This leads to many broad and disparate poorly defined variables” (Kuiper and Roelofs, 2008, p. 27) “. . . Therefore discussion is still open” (p. 28) • Occupational therapists work “as injury prevention and workplace modification consultants to industry and state governments” (p. 27) • Kuiper and Roelofs (2008) make a case for the inclusion of the term “occupational style” in the ICF work related personal factors.
Questions
Chapter 9
References Chard, G (2004) International Classification of Functioning, Disability and Health. British Journal of Occupational Therapy, 67 (1) 1 College of Occupational Therapists (COT; 2004) Guidance on the use of the International Classification of Functioning, Disability and Health (ICF) and the Ottawa Charter for Health Promotion in occupational therapy service. London: COT Hammell KW (2004) Deviating from the norm: a sceptical interrogation of the classificatory practices of the ICF. British Journal of Occupational Therapy 67 (9) 408 -411. Kuiper C, Roelofs P (2008) Occupational style, the prodigal son: The revival of a construct. WFOT Bulletin, 58 (November), 27 -32 Laver Fawcett AJ (2007) Principles of Assessment and Outcome Measurement for Occupational Therapists and Physiotherapists: Theory, Skills and Application. Chichester: John Wiley & Sons Law M, Baum C (2001) Measurement in Occupational Therapy. In M Law, C Baum, W Dunn (eds) Measuring Occupational Performance: Supporting Best Practice in Occupational Therapy. Thorofare: Slack
References (continued) Mac. Dermid J, Michlovitz S (2008) Incorporating outcome measures into evidencebased practice. In: Law M, Mac. Dermid J (eds) Evidence-Based Rehabilitation. Thorofare: Slack Unsworth C (2005) Measuring Outcomes using the Australian Therapy Outcome Measures for Occupational Therapy (Aus. TOMs - OT): Data Description and Tool Sensitivity. British Journal of Occupational Therapy, 68(8), 354 -366 World Federation of Occupational Therapists (WFOT) Council (2008) WFOT Council meeting. Ljubljana, Slovenia, 7 th – 12 th September, 2008. WFOT Bulletin, 58 (November), 5 -9 World Health Organisation (WHO; 2002) Towards a Common Language for Functioning, Disability and Health ICF. [online]. Geneva: WHO. Available from: http: //www. who. int/classifications/icf/en/ [Accessed 15 February 2009] World Health Organisation (WHO) (1980) International Classification of impairments, disabilities and handicaps: a manual of classification relating to the consequences of disease. Geneva: WHO
Further reading Example of a study by occupational therapists to compare occupational therapy concepts with ICF terminology: Haglund L, Henriksson C (2006) Concepts in occupational therapy in relation to the ICF. Occupational Therapy International. 10(4), 253 -268
Further reading Example of the ICF applied to a case study: Martin A, Burtner PA, Poole J, Phillips J (2008) Case Report: ICF-Level Changes in a Preschooler After Constraint-Induced Movement Therapy. American Journal of Occupational Therapy. 62(3), 282 -288

Contact details Alison J. Laver-Fawcett Senior Lecturer in Occupational Therapy School of Health Sciences York St John University Lord Mayor’s Walk York YO 31 7 EX 01904 -876419 a. laverfawcett@yorksj. ac. uk
8069d30d68b324ea3f13bbf1031ea7e2.ppt