c07387b892044eeef5eb9507460ed8fb.ppt
- Количество слайдов: 92
Intermediate examination RCEM Was MCEM B SAQ
Reading • Adult textbook of Emergency Medicine – Toxicology • OHAEM • OHCM • ATLS , ALS, APLS/EPLS • USMLE – Board series prep for Anatomy, Physiology and Biochemistry 2
3

Useful websites http: //www. collemergencymed. ac. uk http: //www. nice. org. uk/ http: //www. brit-thoracic. org. uk/default. aspx http: //www. das. uk. com/ ( Difficult airway society) http: //www. bashh. org/ ( Sexual health – Chlamydia, Gonorrhoea, etc) • http: //www. sign. ac. uk/ • http: //www. bcshguidelines. com/index. html (Haematology) • RCOG, Infectious disease society, European society of cardiology, etc • • • 4
Guidelines - NICE • Hip fracture • Epilepsy • Therapeutic Hypothermia • NSTEMI • COPD • Chest pain • Loss of consciousness • Stroke and TIA • Respiratory tract infections • Head Injury • AF • Rapid Tranquilization • Falls • Self harm 5
SIGN • Acute Upper and Lower GI bleed • Suspected bacterial UTI in adults 6
CEM • Sexual assault – statement • Ketamine sedation • Domestic violence • Pain – Adults and Children • Biers Block • First fit – flow chart • Tricyclics poisoning • • Allergic reaction Headache Safeguarding Children Antidote 7
BTS • • Pneumothorax Pneumonia Oxygen NIV – COPD and respiratory failure Diving PE Chest drain 8
Paediatrics • • Meningitis - NICE Sedation – NICE Maltreatment – NICE NAI – NICE Gastroenteritis – NICE UTI – NICE Bronchiolitis – SIGN • • • Limping child Discitis Kawasaki’s Perthe’s SUFE Accidental ingestion 9
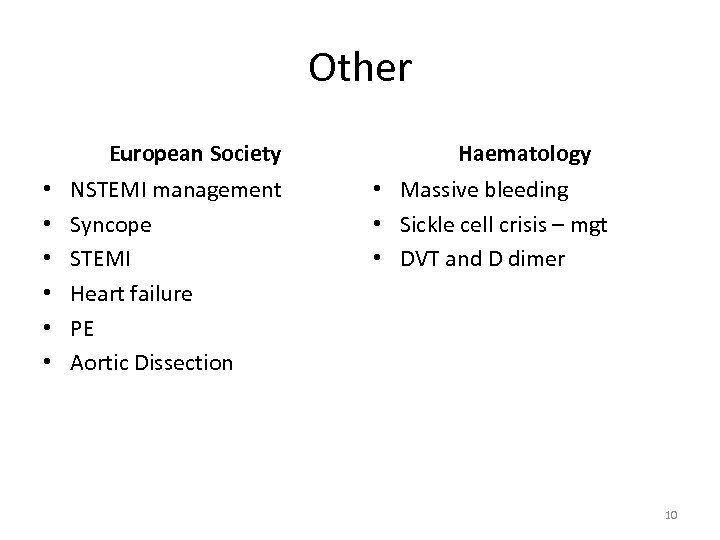
Other European Society • • • NSTEMI management Syncope STEMI Heart failure PE Aortic Dissection Haematology • Massive bleeding • Sickle cell crisis – mgt • DVT and D dimer 10
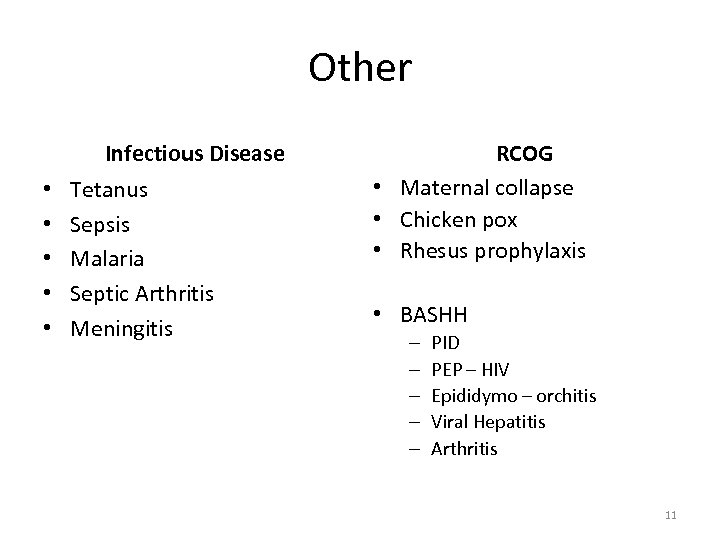
Other Infectious Disease • • • Tetanus Sepsis Malaria Septic Arthritis Meningitis RCOG • Maternal collapse • Chicken pox • Rhesus prophylaxis • BASHH – – – PID PEP – HIV Epididymo – orchitis Viral Hepatitis Arthritis 11
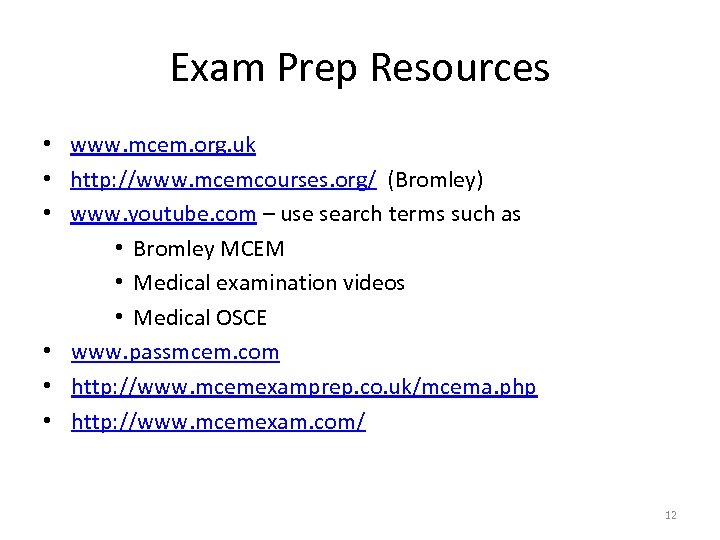
Exam Prep Resources • www. mcem. org. uk • http: //www. mcemcourses. org/ (Bromley) • www. youtube. com – use search terms such as • Bromley MCEM • Medical examination videos • Medical OSCE • www. passmcem. com • http: //www. mcemexamprep. co. uk/mcema. php • http: //www. mcemexam. com/ 12
13
http: //www. rcem. ac. uk/Training. Exams/Resources%20 for%20 exam%20 preparation
Regulations and Information Pack FRCEM Intermediate Certificate Examinations Applicable from 1 August 2016 The FRCEM Intermediate Certificate Examinations is conducted in English and candidates are advised that IELTS Level 7 is the expected standard for completion of the FRCEM examinations.
Intermediate SAQ (= part B MRCEM) 60 questions 3 hours Data interpretation Problem solving skills Clinical scenario and may have clinical data including radiographs, CT scans, ECGs, blood test results and clinical photographs. • The pass mark is ? It is set independently. • • • 16
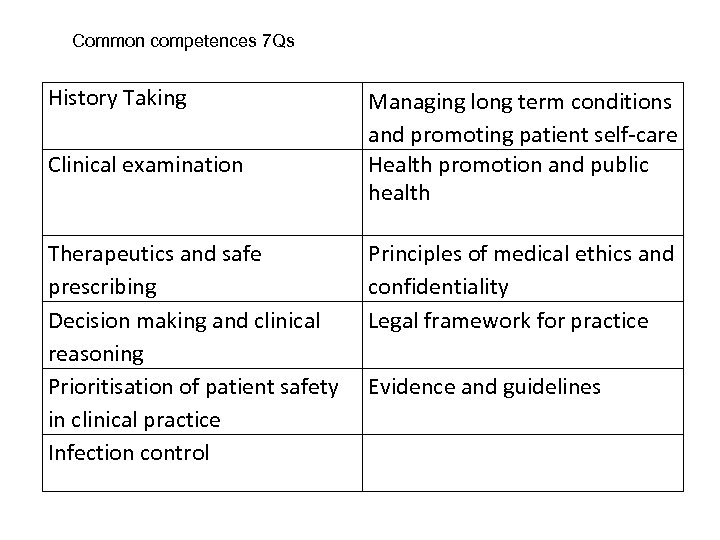
Common competences 7 Qs History Taking Clinical examination Therapeutics and safe prescribing Decision making and clinical reasoning Prioritisation of patient safety in clinical practice Infection control Managing long term conditions and promoting patient self-care Health promotion and public health Principles of medical ethics and confidentiality Legal framework for practice Evidence and guidelines
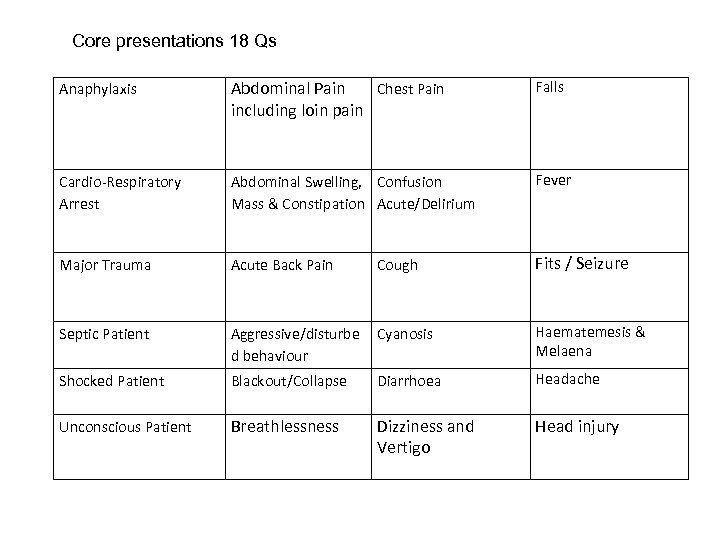
Core presentations 18 Qs Anaphylaxis Abdominal Pain Chest Pain including loin pain Falls Cardio-Respiratory Arrest Abdominal Swelling, Confusion Mass & Constipation Acute/Delirium Fever Major Trauma Acute Back Pain Cough Fits / Seizure Septic Patient Aggressive/disturbe d behaviour Cyanosis Haematemesis & Melaena Shocked Patient Blackout/Collapse Diarrhoea Headache Unconscious Patient Breathlessness Dizziness and Vertigo Head injury
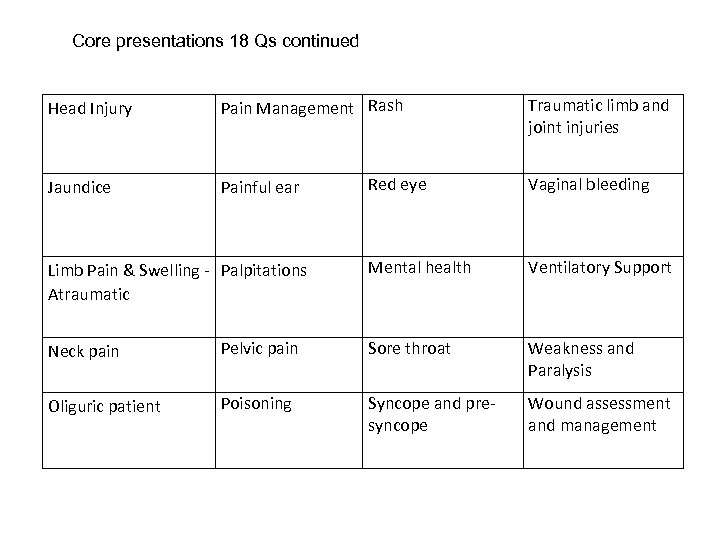
Core presentations 18 Qs continued Head Injury Pain Management Rash Jaundice Painful ear Limb Pain & Swelling - Palpitations Atraumatic Traumatic limb and joint injuries Red eye Vaginal bleeding Mental health Ventilatory Support Neck pain Pelvic pain Sore throat Weakness and Paralysis Oliguric patient Poisoning Syncope and presyncope Wound assessment and management
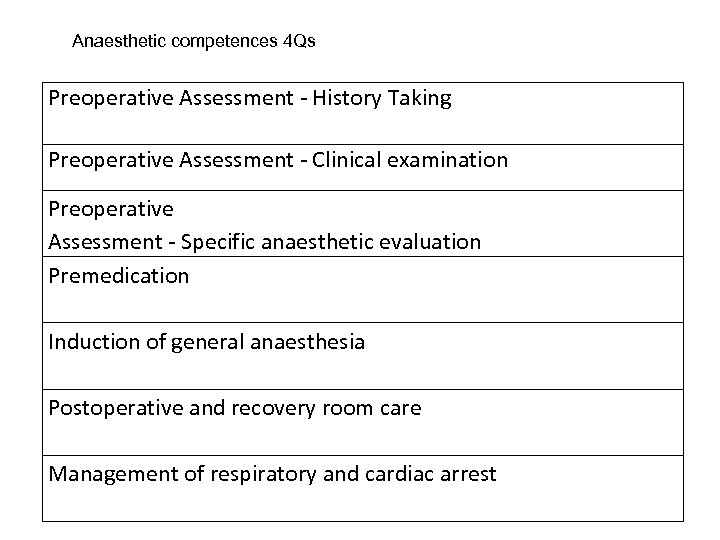
Anaesthetic competences 4 Qs Preoperative Assessment - History Taking Preoperative Assessment - Clinical examination Preoperative Assessment - Specific anaesthetic evaluation Premedication Induction of general anaesthesia Postoperative and recovery room care Management of respiratory and cardiac arrest
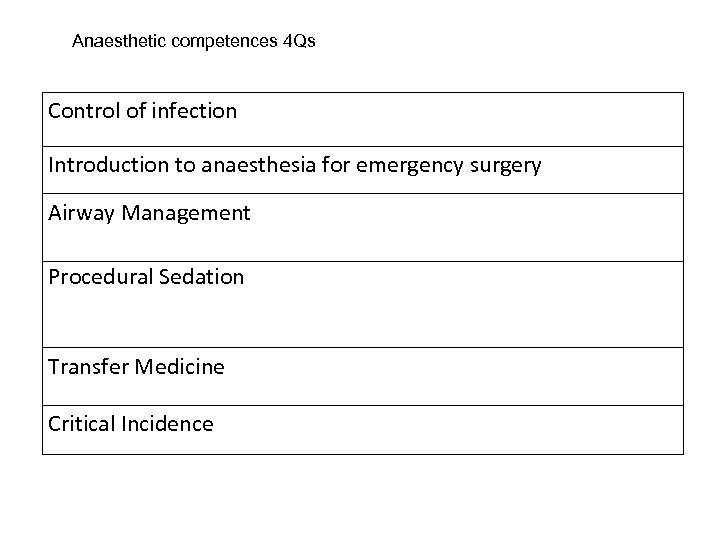
Anaesthetic competences 4 Qs Control of infection Introduction to anaesthesia for emergency surgery Airway Management Procedural Sedation Transfer Medicine Critical Incidence
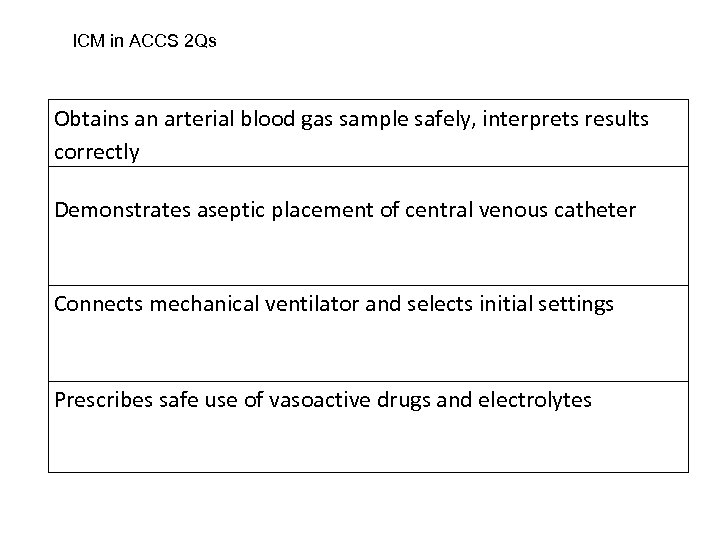
ICM in ACCS 2 Qs Obtains an arterial blood gas sample safely, interprets results correctly Demonstrates aseptic placement of central venous catheter Connects mechanical ventilator and selects initial settings Prescribes safe use of vasoactive drugs and electrolytes
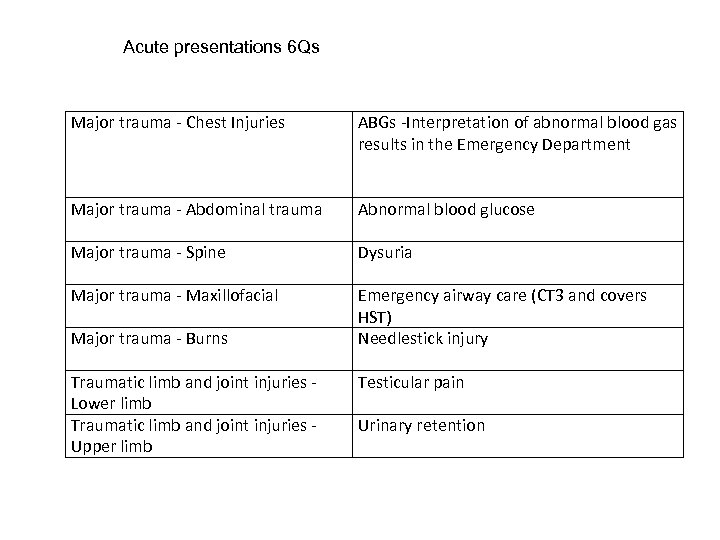
Acute presentations 6 Qs Major trauma - Chest Injuries ABGs -Interpretation of abnormal blood gas results in the Emergency Department Major trauma - Abdominal trauma Abnormal blood glucose Major trauma - Spine Dysuria Major trauma - Maxillofacial Emergency airway care (CT 3 and covers HST) Needlestick injury Major trauma - Burns Traumatic limb and joint injuries - Lower limb Traumatic limb and joint injuries - Upper limb Testicular pain Urinary retention
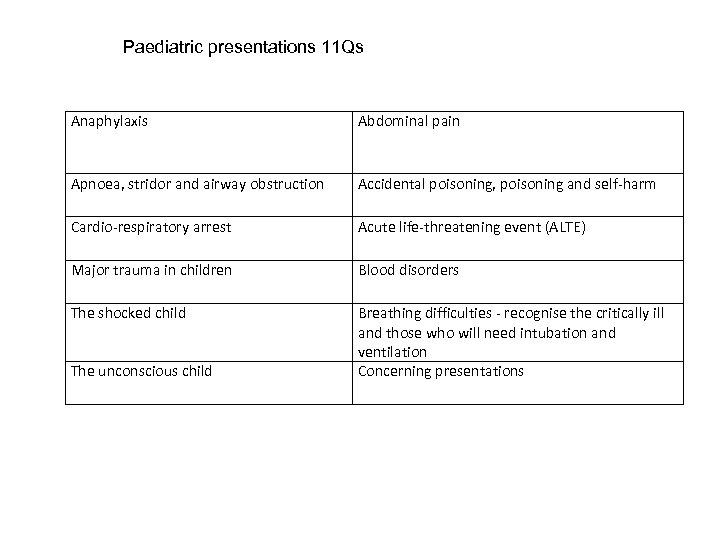
Paediatric presentations 11 Qs Anaphylaxis Abdominal pain Apnoea, stridor and airway obstruction Accidental poisoning, poisoning and self-harm Cardio-respiratory arrest Acute life-threatening event (ALTE) Major trauma in children Blood disorders The shocked child Breathing difficulties - recognise the critically ill and those who will need intubation and ventilation Concerning presentations The unconscious child
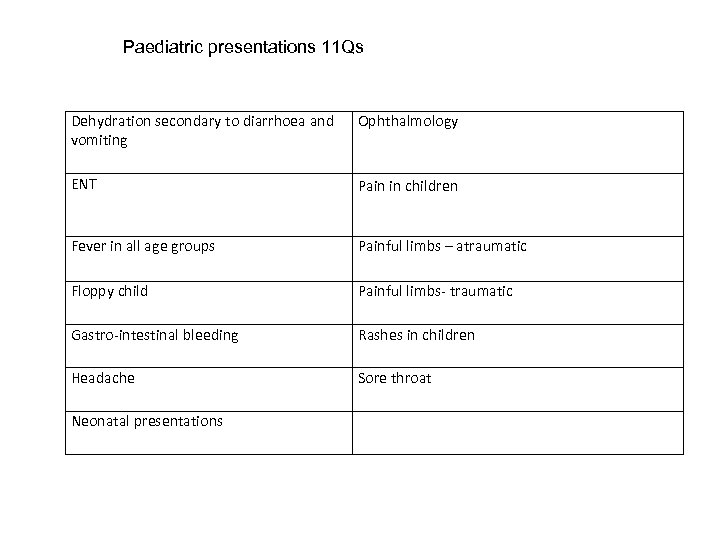
Paediatric presentations 11 Qs Dehydration secondary to diarrhoea and vomiting Ophthalmology ENT Pain in children Fever in all age groups Painful limbs – atraumatic Floppy child Painful limbs- traumatic Gastro-intestinal bleeding Rashes in children Headache Sore throat Neonatal presentations
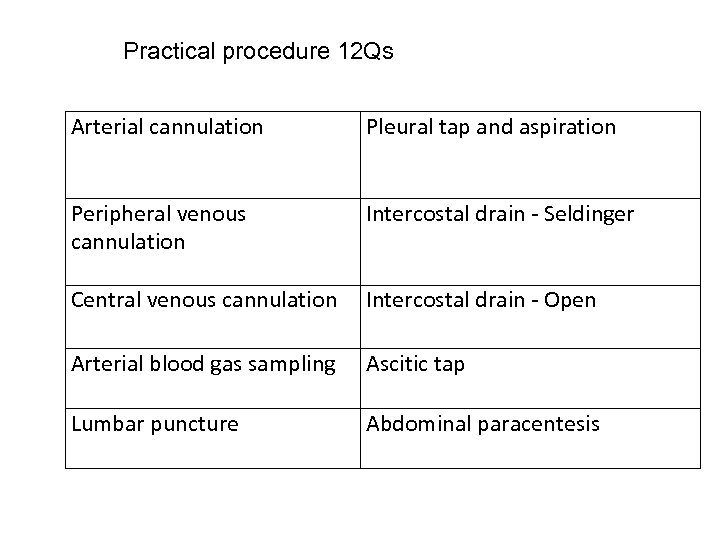
Practical procedure 12 Qs Arterial cannulation Pleural tap and aspiration Peripheral venous cannulation Intercostal drain - Seldinger Central venous cannulation Intercostal drain - Open Arterial blood gas sampling Ascitic tap Lumbar puncture Abdominal paracentesis
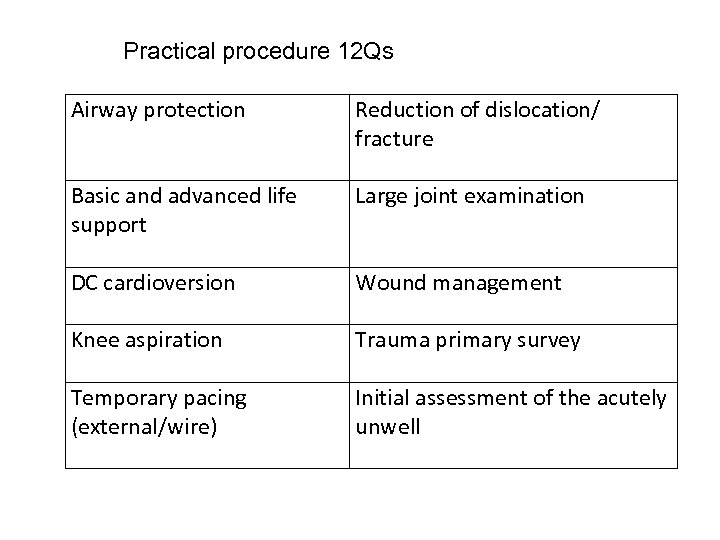
Practical procedure 12 Qs Airway protection Reduction of dislocation/ fracture Basic and advanced life support Large joint examination DC cardioversion Wound management Knee aspiration Trauma primary survey Temporary pacing (external/wire) Initial assessment of the acutely unwell
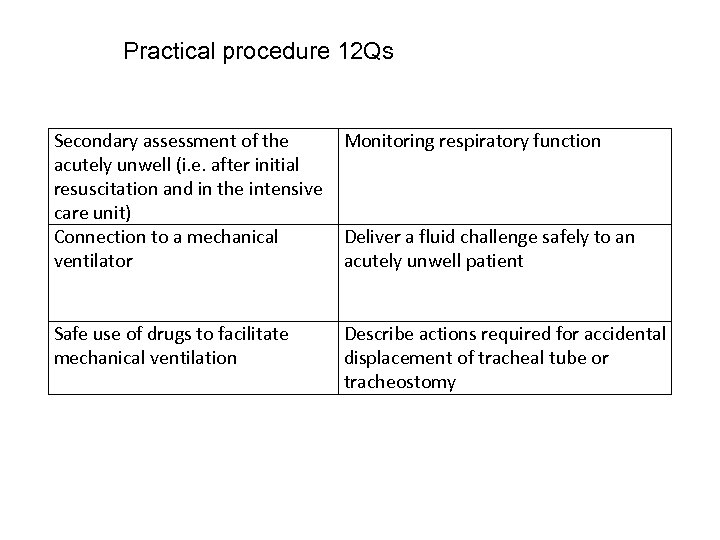
Practical procedure 12 Qs Secondary assessment of the Monitoring respiratory function acutely unwell (i. e. after initial resuscitation and in the intensive care unit) Connection to a mechanical Deliver a fluid challenge safely to an ventilator acutely unwell patient Safe use of drugs to facilitate mechanical ventilation Describe actions required for accidental displacement of tracheal tube or tracheostomy
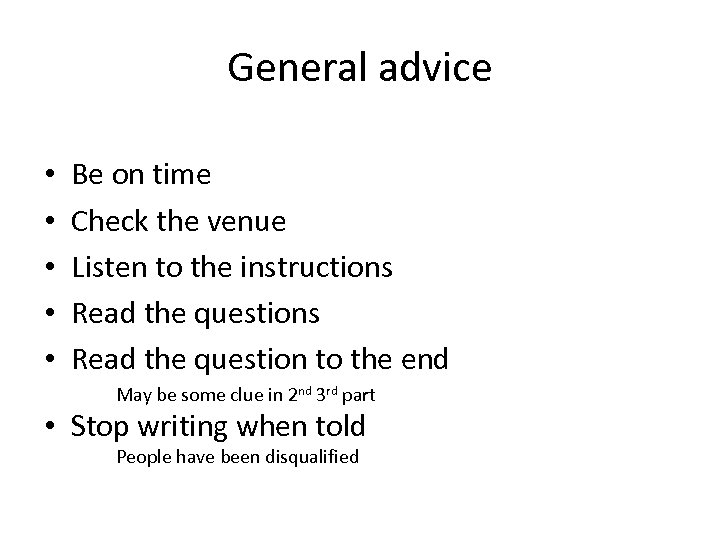
General advice • • • Be on time Check the venue Listen to the instructions Read the question to the end May be some clue in 2 nd 3 rd part • Stop writing when told People have been disqualified
SAQ intermediate No trick questions. Straight forward. Read the question. Each question may not be interrelated. • Most SAQ’s are predictable – Rash, toxicology, etc • • • Even if you don't know the diagnosis – you can still answer some of the questions. • Time is of essence • 3 minutes per Q • If you don't know skip and come back later 30

An 11 year old boy presents with his parents to the ED having developed a limp over the last week. • What is the abnormality on the x-ray? (1 mark) • Name and describe the radiological sign associated with this abnormality? (1 mark) • Name one complication associated with this condition. (1 mark)
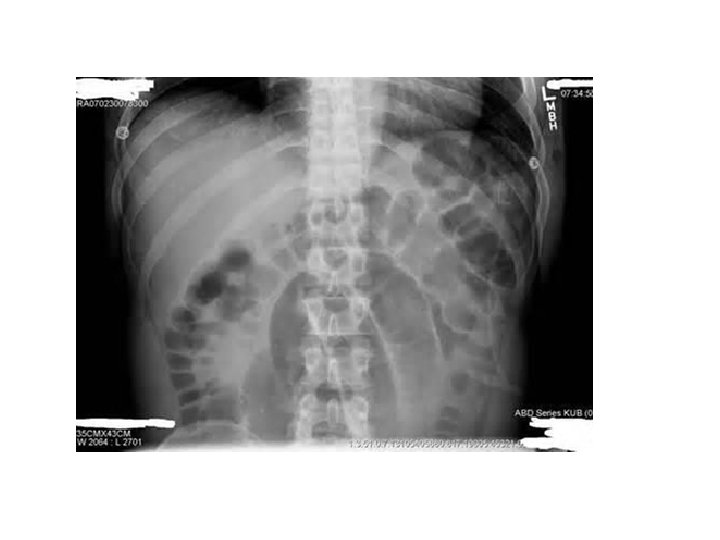
A 45 year old lady presents to the ED with a two day history of abdominal pain. Abdominal examination confirms generalised tenderness. • What is the diagnosis? (1 mark) • Name two other symptoms which the patient may complain of? (1 mark) • What would be your first two steps in your early management of this patient? (1 mark)
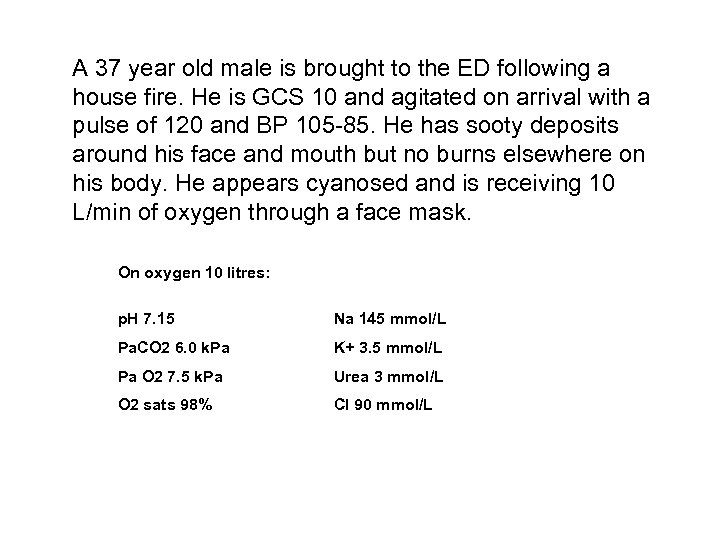
A 37 year old male is brought to the ED following a house fire. He is GCS 10 and agitated on arrival with a pulse of 120 and BP 105 -85. He has sooty deposits around his face and mouth but no burns elsewhere on his body. He appears cyanosed and is receiving 10 L/min of oxygen through a face mask. On oxygen 10 litres: p. H 7. 15 Na 145 mmol/L Pa. CO 2 6. 0 k. Pa K+ 3. 5 mmol/L Pa O 2 7. 5 k. Pa Urea 3 mmol/L O 2 sats 98% Cl 90 mmol/L
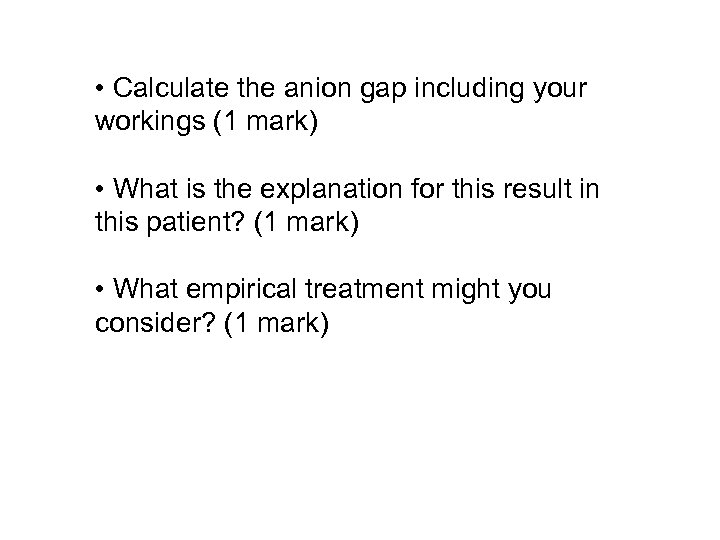
• Calculate the anion gap including your workings (1 mark) • What is the explanation for this result in this patient? (1 mark) • What empirical treatment might you consider? (1 mark)

A 17 year old male attend the ED complaining of a rash. He describes having a cold sore one week ago followed by the abrupt onset of a rash. The rash started peripherally and spread centrally. He is now unwell, febrile, tachycardic and is complaining of a headache. He also complains of a sore mouth and gritty eyes. He has haematuria on urine dipstick testing. • Describe the key feature of this rash? (1 mark) • What is the likely diagnosis? (1 mark) • What is the most likely infective agent that has precipitated the rash? (1 mark)
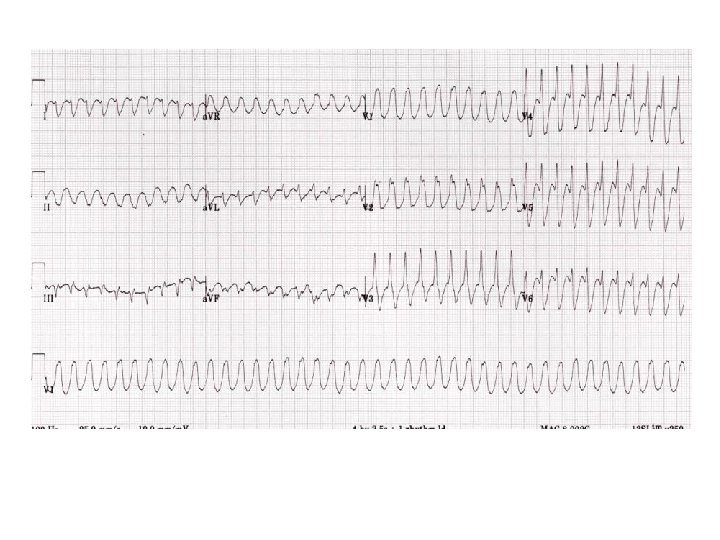
A 57 year old man has two hour history of palpitations. On examination he is sweaty and has a BP of 100/50 but denies chest pain or breathlessness. • Name two diagnoses which would explain this ECG picture? (2 marks) • He then drops his BP to 80/60. What treatment is required? (1 mark)

A 60 year old male plumber attends with a painful and swollen right knee. He has been sent to the ED by his boss as he is finding it difficult working. • What is the diagnosis (1) • What is the main complication this patient may develop? (1) • Outline two aspects of your treatment (1)
Paediatrics • A 4 year old boy presents with 2 days diarrhoea, dry cough and fever. His mother says he has been unwell for 0 ne month. o/e He is pale, lethargic has a sore mouth, jaundice and a palpable liver and spleen. He has a non blanching rash and obvious palpable cervical lymph nodes. ENT examination is unremarkable. He has no signs of meningism. No PMH and no prior hospital admissions • • Temp 39. 5 HR 150 Cap refill 3 secs O 2 sats 92% on air R 40 BM 5. 2 Wt 15 kg Hb 8. 6 g/dl WBC 0. 6 x 109 / L Platelets 58 109 / L Neutrophils 0. 45 x 109 / L
Given the clinical scenario and blood results, what is the most likely immediate problem (1 mark). Your SHO requests the following blood tests. Justify each. (1/2 mark each up to 2 marks) • • Coagulation screen LFTs meningococcal/pneumococcal pcr U & Es
Q 1 Given the clinical scenario and blood results, what is the most likely clinical diagnosis? (1 mark). Septicaemia secondary to bacterial infection with DIC (1 mark) Your SHO requests the following blood tests. Justify each. (1/2 mark each up to 2 marks) • Coagulation screen or DIC screen because of high fever and bruising. • LFTs because of palpable liver and jaundice • meningococcal/pneumococcal pcr because of fever and rash • U & Es to assess renal function
A 16 yr old attends ED with a painful shoulder. She is a known epileptic. She has woken up from sleep with this. She holds her arm against her chest and has very little movement and is in pain. An x-ray has been carried out
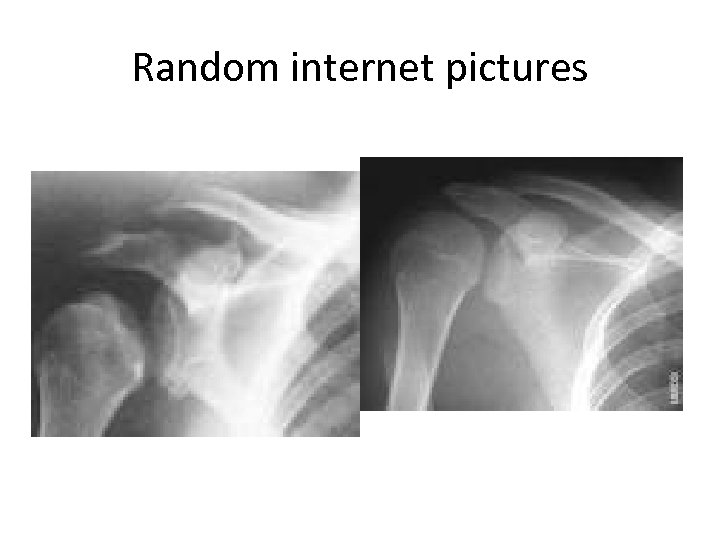
Random internet pictures
Q 1 Name the most likely diagnosis? (1 marks) Q 2 What is the most likely reason for the shoulder injury? (1 mark) Q 3. What two questions would you consider relevant in the medical history in this patient? (1 marks)
Q 1 Likely Posterior shoulder dislocation Q 2 What is the most likely reason for the shoulder injury? (1 mark) • Epileptic seizure while asleep Q 3. What two questions would you consider relevant in the medical history in this patient? (2 marks) • Medication history • Compliance (are you taking your anti-epileptics) • Alcohol history • Seizure history • Previous history of shoulder dislocation
A 62 yr old woman brought to ed by ambulance. She states she has taken 50 cocodamol (8/500) a few days ago. She has not eaten for 48 hours. O/E she is pale and very dehydrated. She is vomiting. Her vital signs are normal apart from HR 108. She is clinically jaundiced. No other findings Na 135 K 4. 3 U 9 Cr 276 Glu 2 ALT 2306 Alk P 132 Bili 64 Cor calcium 2. 24 Phos 2. 14 Bicarb 18 Hb 15. 4 WC 14. 8 Plat 255 INR 3. 5 Sal < 0. 1 Para < 0. 15
Q 1. Why are bilirubin and ALT raised but not the alkaline phosphatase? (1 mark) Q 2. How is paracetamol metabolised and how does it cause damage in overdose? (2 marks)
Q 1. Why are bilirubin and ALT raised but not the alkaline phosphatase? (1 mark) • Bilirubin and ALT are markers of hepatic dysfunction and necrosis. (1/2 mark) • Alk Phos usually increases relatively little and is more associated with intra -hepatic obstruction or bile duct injury (1/2 mark) Q 2. How is paracetamol metabolised and how does it cause damage in overdose? (2 marks) • Toxic metabolite (NACQI) usually conjugated with glutathione and rendered harmless. • In overdose, or reduced glutathione stores, the toxic metabolite binds to cells and leads to cell death , centrilobular necrosis (1 mark for each answer)
It is 23. 40 you are the reg on night shift. Your FY 2 has just seen a 6 month old who presents with swelling and bruising over L scalp area. The mother says she first noticed this 2 days ago. She told the FY 2 there was no H/O head injury. ED records show this to be the child’s 4 th attendance. The FY 2 ask for your advice.
Q 1. Give two details from this history that makes you concerned about nonaccidental injury (NAI). (2 marks) Q 2. If you suspect non-accidental injury, name two actions you will take in the department? (1 marks)
An 80 yr old woman attend because of inability to walk, weakness and altered sensation in arms and legs. NO PMH She tripped yesterday and cut her chin. She has a painful neck.
Q 1. What is the likely specific diagnosis (1 mark) Q 2. Name one feature that leads you to this diagnosis (1 mark) Q 3. What is the most common mechanism of injury responsible for this clinical (1 mark)
A 26 year old man is involved in a gas bottle explosion in a closed room. He has sustained flashover burns, mostly a mixture of superficial and deep partial thickness. Wt 80 KG
Q 1. List 2 clinical examination findings that would make you suspect thermal injury to the airway in this patient (1/2 mark each up to total 1 marks) Q 2. The burns are mixed partial and full thickness and make up 21% of his surface area. Using the Parkland /ATLS Formula how much IV fluid does this 80 Kg man require for the burn in the first 8 hrs ? Show your calculation and total. ( 2 marks)
Q 1. List 2 clinical examination findings that would make you suspect thermal injury to the airway in this patient (1/2 mark each up to total 1 marks) • Facial burns (½ mark) • Singeing of nasal hairs (½ mark) • Carbonaceous deposits in the oropharynx/mouth (½ mark) • Carbonaceous sputum (½ mark) • Hoarse voice/stridor (½ mark) • Signs of respiratory distress (½ mark) • Evidence of Pharyngeal/tongue oedema Q 2. The burns are mixed partial and full thickness and make up 21% of his surface area. Using the Parkland /ATLS Formula how much IV fluid does this 80 Kg man require for the burn in the first 8 hrs ? Show your calculation and total. ( 2 marks) • 4 ml x 80 kg x 21% burns = 6720 ml • ½ in the first 8 hrs = 3360 mls. • (some candidates may use a baseline of 2 or 3 mls – discuss re ? other calculations acceptable. )
70 yr old man with known COPD presents with 1 week increasing dyspnoea, cough and sputum. O/E he is pale, sweaty, marked chest crepitations L base. T 38 RR 34 HR 100 BP 100/70 O 2 on air 90% MTS 8/10 (confused)
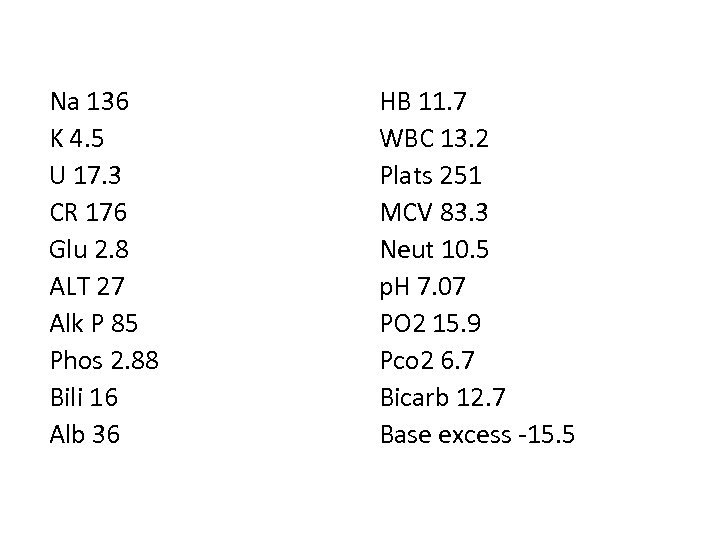
Na 136 K 4. 5 U 17. 3 CR 176 Glu 2. 8 ALT 27 Alk P 85 Phos 2. 88 Bili 16 Alb 36 HB 11. 7 WBC 13. 2 Plats 251 MCV 83. 3 Neut 10. 5 p. H 7. 07 PO 2 15. 9 Pco 2 6. 7 Bicarb 12. 7 Base excess -15. 5
Q. 10 Litres per minute of oxygen is administered an arterial blood gas is taken. Comment on the acid base and ventilation status of the patient and give reasons for the results, (3 marks )
Q 2. 10 Litres per minute of oxygen is administered an arterial blood gas is taken. Comment on the acid base and ventilation status of the patient and give reasons for the results, (4 marks ) • Mixed metabolic and respiratory acidosis (1 mark for acidosis, 1 mark for mixed)- probably sepsis and retained Co 2 (1/2 mark each) • Hypoxaemaia (Low oxygen) for the inspired concentration – likely secondary to V/Q mismatch
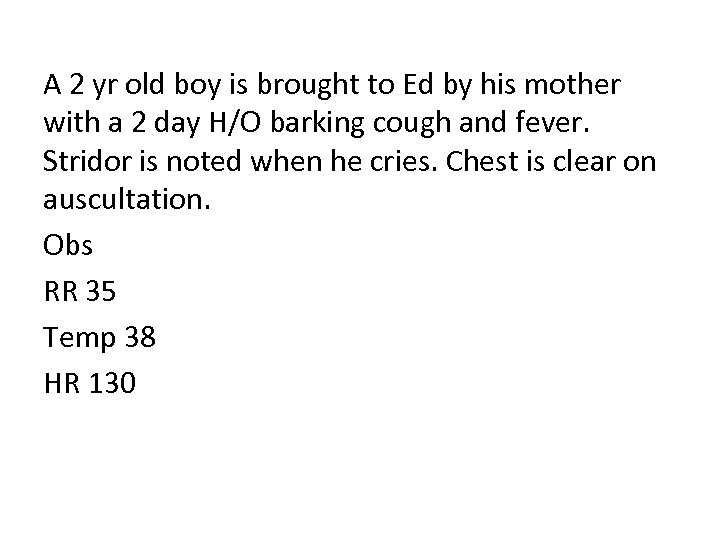
A 2 yr old boy is brought to Ed by his mother with a 2 day H/O barking cough and fever. Stridor is noted when he cries. Chest is clear on auscultation. Obs RR 35 Temp 38 HR 130
Q 1. What is the most likely clinical diagnosis? (1 mark) Q 2. Give 2 of the five components of the score that can be used to assist in the assessment of the severity of this condition. (2 marks)
Q 1. What is the most likely clinical diagnosis? (1 mark) Croup or viral laryngotracheobronchitis Q 2. Give 2 of the five components of the score that can be used to assist in the assessment of the severity of this condition. (2 marks) • • • Presence of stridor Level of consciousness / alertness Degree of air entry Presence of Cyanosis Retractions / Recession

A 70 year old lady presents with a painful red eye Q 1. A photograph of the patient’s eye is shown. List 2 findings in the photograph which are classic findings in acute angle glaucoma. (2 marks) Q 2. Give 2 treatments you would start in the ED
A 70 year old lady presents with a painful red eye Q 1. A photograph of the patient’s eye is shown. List 2 findings in the photograph which are classic findings in acute angle glaucoma. (2 marks) Q 2. Give 2 treatments you would start in the ED (1 mark) analgesia Acetazolamide topical β blockers (timolol)

A mother brings her 9 yr old son to ED with this purpuric rash. Child looks well, vital signs normal. Q 1. What is the most likely diagnoses (1 mark) Q 2. What 2 investigations or bedside tests would you carry out and why (2 marks)
A mother brings her 9 yr old son to ED with this purpuric rash. Child looks well, vital signs normal. Q 1. What is the most likely diagnoses (1 mark) HSP Q 2. What 2 investigations or bedside tests would you carry out and why (2 marks) • • • Normal urine analysis – no haematuria or proteinuria or for blood & protein FBC - not ITP leukaemia infection Normal coagulation screen – not clotting problem factor deficiency Normal electrolytes – no renal involvement Normal BP – for renal involvement
A 71 yr old diabetic man is brought in from his sheltered accommodation. His carer found him in bed this am, confused but uninjured and called an ambulance RR 27 SA O 2 on air 93% Pulse 115 irreg BP 90/53 Cap refill 3 secs GCS 13 Temp 36. 5 BM “high” Urine dip protein and white cells +
Q 1. What is your working diagnosis? (1 mark) Q 2. He is being monitored and you start fluids and oxygen and refer to the medical team for admission. List four further steps in your immediate management of this man in the ED. (2 marks)
Q 1. What is your working diagnosis? (1 mark) • Hyperosmolar / hyperglycaemic crisis Q 2. He is being monitored and you start fluids and oxygen and refer to the medical team for admission. List four further steps in your investigation or immediate management of this man in the ED. (2 marks) • • • • ECG Chest x-ray Full blood count Urea + electrolytes Blood Gas (venous or arterial) Venous Blood sugar level Urine Osmolarity Insulin infusion Supplemental K + if required after checking NG tube Urinary catheter Low molecular weight heparin Antibiotics if indicated Hourly BM 2 -4 hourly electrolytes

An 85 yr old lady presents to ED after catching her shin on a supermarket trolley. She has a 13 cm wound on her leg
Q 1. Name 2 classes of commonly prescribed drugs in the elderly which may prolong wound healing? (1 marks) Q 2. Give two reasons why suturing is generally not the preferred treatment option for these injuries (2 marks)
Q 1. Name 2 classes of commonly prescribed drugs in the elderly which may prolong wound healing? (2 marks) • Steroids • Anticoagulants Q 2. Give two reasons why suturing is generally not the preferred treatment option for these injuries (2 marks) • Tissues bruised and oedematous resulting in tissue tension • Frail skin leads to cutting-out of sutures • Undue tension compromises wound healing and increases the risk of infection.
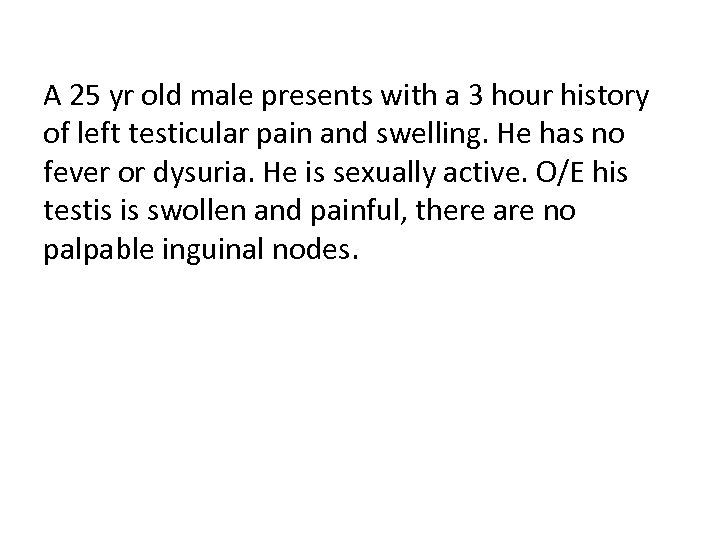
A 25 yr old male presents with a 3 hour history of left testicular pain and swelling. He has no fever or dysuria. He is sexually active. O/E his testis is swollen and painful, there are no palpable inguinal nodes.
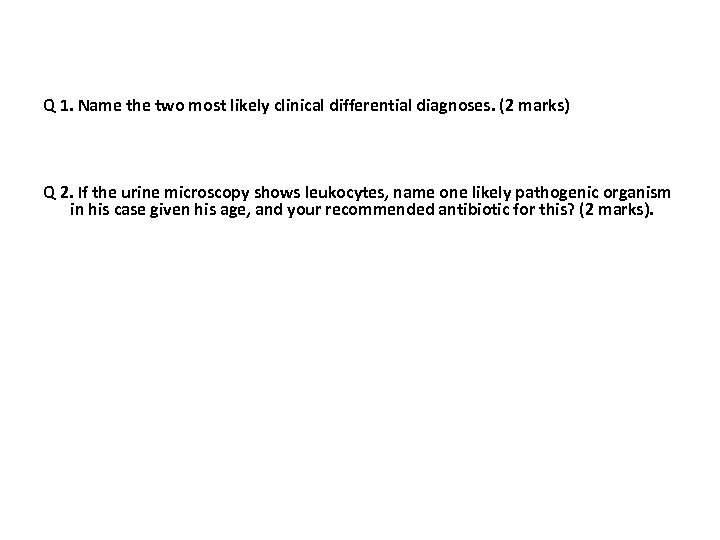
Q 1. Name the two most likely clinical differential diagnoses. (2 marks) Q 2. If the urine microscopy shows leukocytes, name one likely pathogenic organism in his case given his age, and your recommended antibiotic for this? (2 marks).
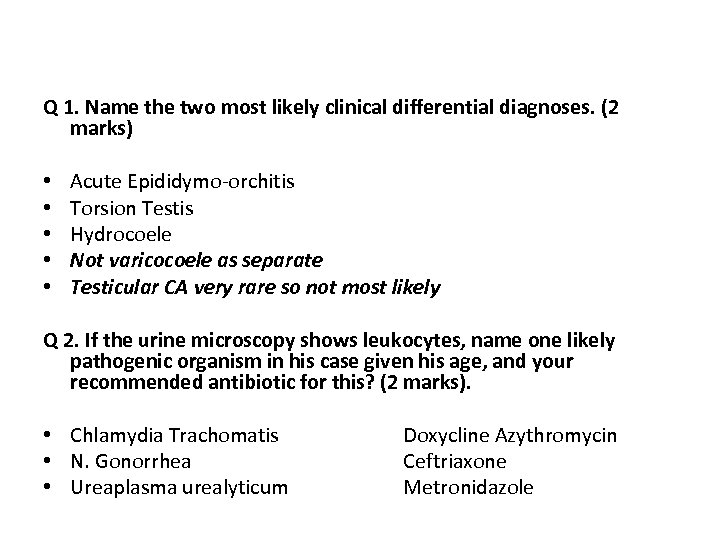
Q 1. Name the two most likely clinical differential diagnoses. (2 marks) • Acute Epididymo-orchitis • Torsion Testis • Hydrocoele • Not varicocoele as separate • Testicular CA very rare so not most likely Q 2. If the urine microscopy shows leukocytes, name one likely pathogenic organism in his case given his age, and your recommended antibiotic for this? (2 marks). • Chlamydia Trachomatis Doxycline Azythromycin • N. Gonorrhea Ceftriaxone • Ureaplasma urealyticum Metronidazole
3) State two common pathogens which might account for this man’s presentation. (2 marks) 4] Outline four steps in the management of this man assuming he is systemically well. (2 marks) 5] If this man failed to respond to the management you describe within 10 days, give two other pathologies you would suspect. (2 marks)
A 6 year old boy is brought to ED by his parents. They have just returned from a week in Goa. He has been unwell for 2 days with 15 episodes diarrhoea, abdo pain and swinging temp. No vomiting. He is 5% dehydrated, temp 38. 3. Nil else to find.
Q 1. What is the most likely diagnosis? (1 mark) Q 2. How would you choose to rehydrate this child and why? (1 mark) Q 3. Would you give anti-motility agents to this child? explain your answer (1 mark)
Q 1. What is the most likely diagnosis? (1 mark) Traveller’s Diarrhoea Q 2. How would you choose to rehydrate this child and why? (1 mark) Oral rehydration – water or oral replacement solutions as dehydration not severe & not vomiting Q 4. Would you give anti-motility agents to this child? explain your answer (1 mark) No - Antimotility agents are not generally used in children because of the increased risk of complications such as toxic megacolon and haemolytic ureamic syndrome
A 76 year old female presents to Ed with a H/O feeling unwell. She had night chills and vomiting for 2 days. She has recently been diagnosed with breast cancer and has had a lumpectomy and 1 cycle chemo 10 days ago. Vital signs O/A BP 106/58 HR 88 RR 22 Temp 34. 2 O 2 on air 99% She is now on high flow oxygen The Nurse practitioner shows you these results:
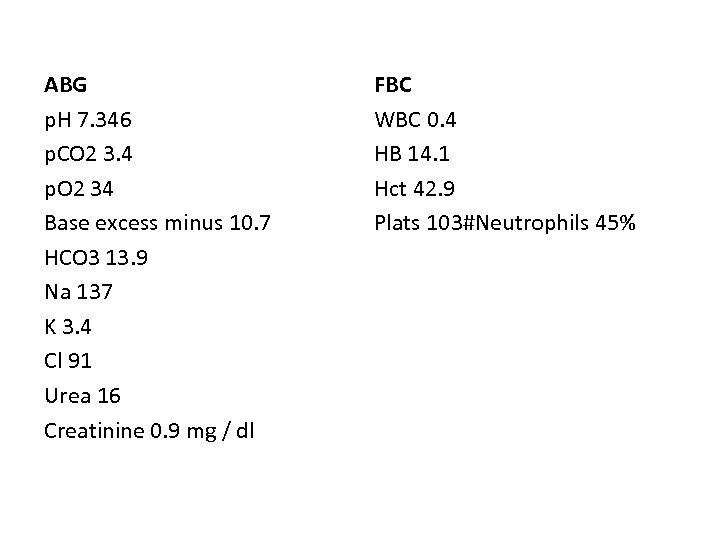
ABG p. H 7. 346 p. CO 2 3. 4 p. O 2 34 Base excess minus 10. 7 HCO 3 13. 9 Na 137 K 3. 4 Cl 91 Urea 16 Creatinine 0. 9 mg / dl FBC WBC 0. 4 HB 14. 1 Hct 42. 9 Plats 103#Neutrophils 45%
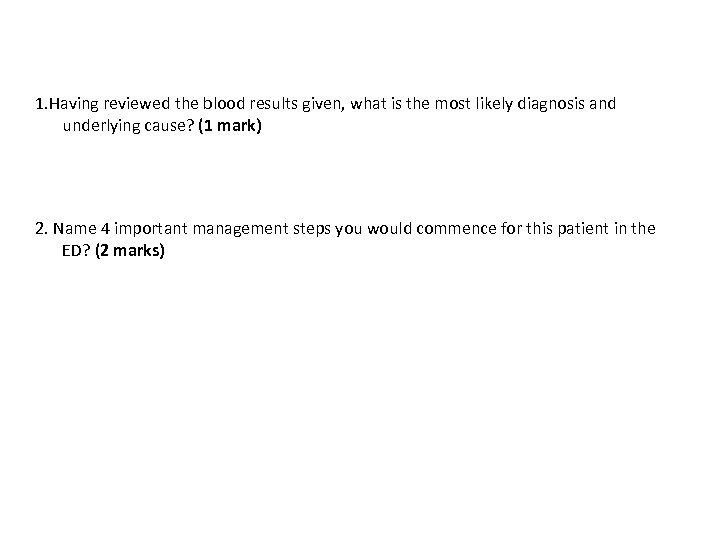
1. Having reviewed the blood results given, what is the most likely diagnosis and underlying cause? (1 mark) 2. Name 4 important management steps you would commence for this patient in the ED? (2 marks)
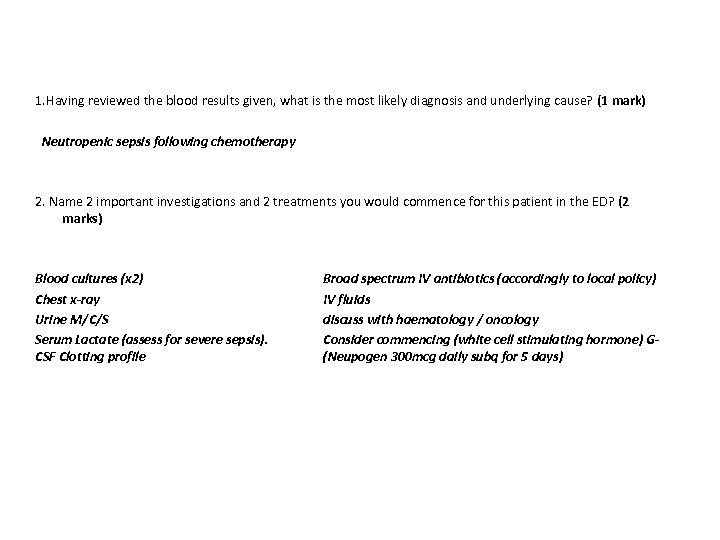
1. Having reviewed the blood results given, what is the most likely diagnosis and underlying cause? (1 mark) Neutropenic sepsis following chemotherapy 2. Name 2 important investigations and 2 treatments you would commence for this patient in the ED? (2 marks) Blood cultures (x 2) Chest x-ray Urine M/C/S Serum Lactate (assess for severe sepsis). CSF Clotting profile Broad spectrum IV antibiotics (accordingly to local policy) IV fluids discuss with haematology / oncology Consider commencing (white cell stimulating hormone) G(Neupogen 300 mcg daily subq for 5 days)
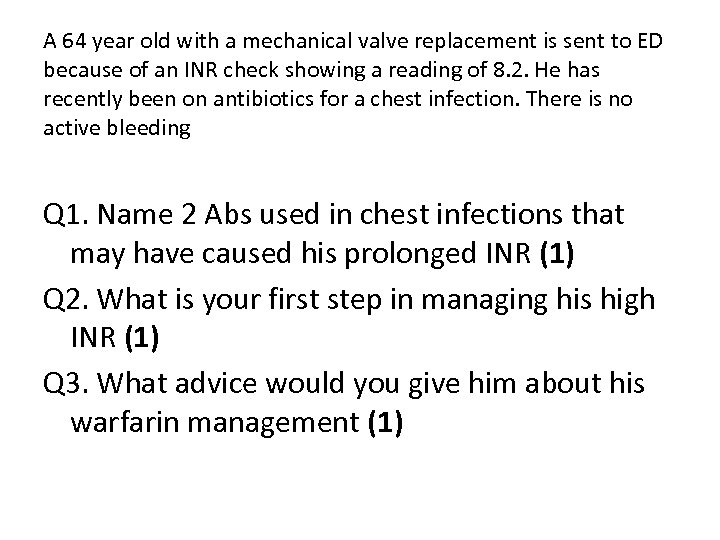
A 64 year old with a mechanical valve replacement is sent to ED because of an INR check showing a reading of 8. 2. He has recently been on antibiotics for a chest infection. There is no active bleeding Q 1. Name 2 Abs used in chest infections that may have caused his prolonged INR (1) Q 2. What is your first step in managing his high INR (1) Q 3. What advice would you give him about his warfarin management (1)
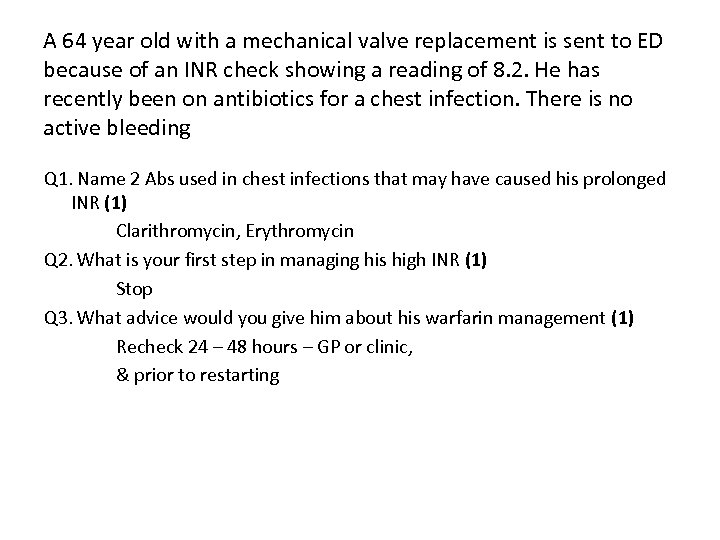
A 64 year old with a mechanical valve replacement is sent to ED because of an INR check showing a reading of 8. 2. He has recently been on antibiotics for a chest infection. There is no active bleeding Q 1. Name 2 Abs used in chest infections that may have caused his prolonged INR (1) Clarithromycin, Erythromycin Q 2. What is your first step in managing his high INR (1) Stop Q 3. What advice would you give him about his warfarin management (1) Recheck 24 – 48 hours – GP or clinic, & prior to restarting
c07387b892044eeef5eb9507460ed8fb.ppt