1279d177d394b4bd3884ca93f79dbeb9.ppt
- Количество слайдов: 37
Integrating Best Practices for Performance Improvement, Quality Improvement, and Participatory Learning and Action to Improve Health Services APPENDIX F Session A Facilitative Supervision for Quality Improvement Curriculum 2008
Resources: Guidance for Program Staff Integrating Best Practices for Performance Improvement (PI), Quality Improvement (QI), and Participatory Learning and Action (PLA) to Improve Health Services
What Are These Approaches? n Performance improvement (PI) n Quality improvement (QI) n Participatory learning and action (PLA)
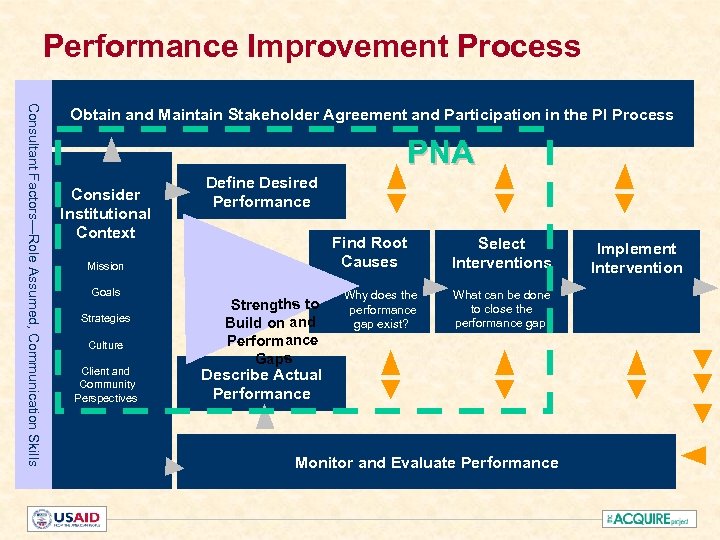
Performance Improvement Process Consultant Factors—Role Assumed, Communication Skills Obtain and Maintain Stakeholder Agreement and Participation in the PI Process PNA Consider Institutional Context Define Desired Performance Find Root Causes Mission Goals Strategies Culture Client and Community Perspectives Strengths to Build on and Performance Gaps Why does the performance gap exist? Select Interventions What can be done to close the performance gap? Describe Actual Performance Monitor and Evaluate Performance Implement Intervention
Performance Factors n Job expectations n Performance feedback n Physical environment and tools n Motivation n Skills and knowledge to do the job
PI Tools and Interventions (1) n PNA stakeholders meeting n Typical tools to define actual performance: – Interviews with providers/staff/supervisors – Observation of client-provider interaction – Facility audit/assessment – Review of service statistics – Client interviews – Group discussions in the community
PI Tools and Interventions (2) n Interventions range widely in size and scale, based on the needs identified. The facilitator helps participants to diagnose gaps in performance and identify appropriate interventions. Interventions focus on strengthening the performance factors and may come from any source of knowledge, experience, and best practices.
PI Tools and Interventions (3) n Intervention examples: – Training – Supervision strengthening – Marketing/communication – Community mobilization
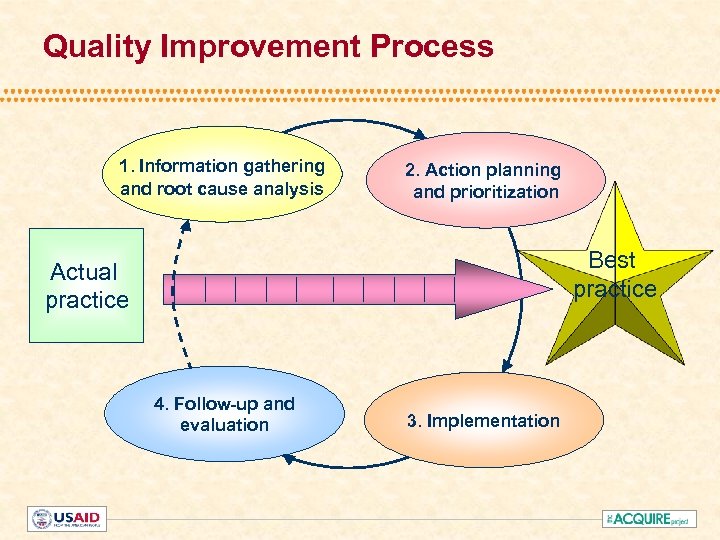
Quality Improvement Process 1. Information gathering and root cause analysis 2. Action planning and prioritization Best practice Actual practice 4. Follow-up and evaluation 3. Implementation
Underlying Principles n A customer mindset n Staff involvement and ownership n Focus on systems and processes n Cost-consciousness and efficiency n Continuous quality improvement n Staff development and capacity building

Clients’ Rights and Staff Needs Rights of clients n Information n Access to services n Informed choice n Safe services n Privacy and confidentiality n Dignity, comfort, and expression of opinion n Continuity of care Staff needs n Facilitative supervision and management n Information, training, and development n Supplies, equipment, and infrastructure
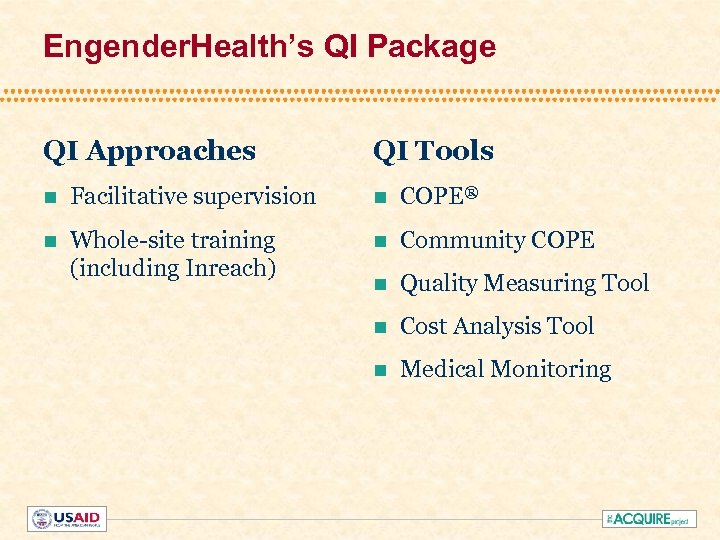
Engender. Health’s QI Package QI Approaches QI Tools n Facilitative supervision n COPE® n Whole-site training (including Inreach) n Community COPE n Quality Measuring Tool n Cost Analysis Tool n Medical Monitoring
Facilitative Supervision n Facilitative supervision is a system of management whereby supervisors at all levels in an institution focus on the needs of the staff they oversee. n The most important role of the facilitative supervisor is to enable staff to: – Manage the QI and PI process – Meet the needs of clients – Implement institutional goals
When Training Is the Answer: Whole-Site Training (WST) WST is an approach to training that: n Meets the learning needs of all staff at a servicedelivery site n Views a service-delivery site as a system and treats staff as members of the team that makes the system work n Makes training more cost-efficient
Inreach involves orienting and informing staff within the facility about available services. It: n Reduces missed opportunities to provide needed services to clients n Establishes linkages and referrals between departments n Ensures that signs and information for clients are available throughout the facility
COPE: A Continuous QI Process n Client- n Oriented, n Provider- n Efficient services
COPE Tools n Self-assessment guides, including record-review checklist n Client interviews n Client-flow analysis (CFA) n Action plan
The COPE Toolbox n COPE Handbook n COPE Toolbooks: – Family planning – Reproductive health – Child health – Maternal health – Community involvement – Adolescent reproductive health – Emergency obstetric care – PMTCT services – Cervical cancer – HIV treatment and care – HIV testing and counseling
Medical Monitoring—What Is It? Medical monitoring: n Is an objective assessment of actual services, to identify and close gaps between actual and desired practices. The two main components to assess are “readiness” of the facility and ”processes of care” n Ensures that clinical standards, norms, and policies are implemented properly
Community COPE n Based on experience in several countries (Bangladesh, Kenya, Nepal, and others) n Some tools adapted from Participatory Learning and Action (PLA) n Used after sites are experienced with COPE n Helps establish links between site and community n Uses combined strength to improve services
Cost-Analysis Tool n Measures direct costs of providing services – Cost of service providers’ time – Cost of supplies used n Can be used to – Set user fees for different services – Negotiate subsidies – Compare costs of changes in type of procedure and provider (Decisions must be based on best medical practice, client’s situation, etc. )
Quality Measuring Tool (QMT) The QMT: n Is based on COPE n Measures progress in improving quality over time n Quantifies the results of efforts to improve quality n Encourages staff participation in monitoring
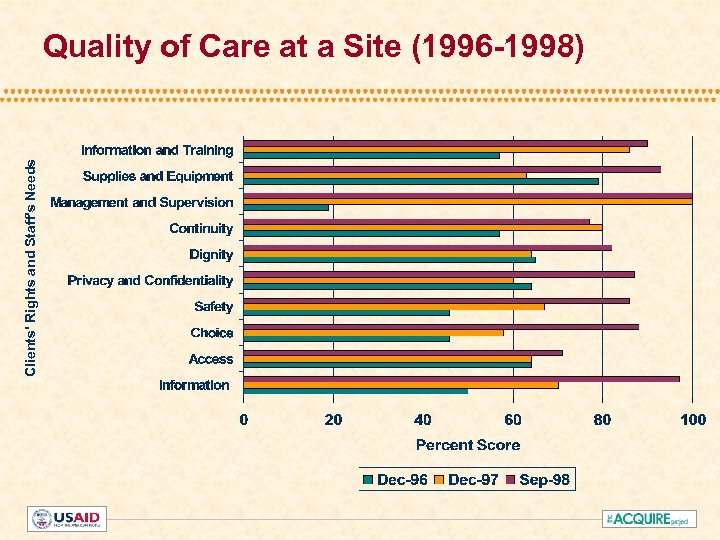
Clients' Rights and Staff's Needs Quality of Care at a Site (1996 -1998)
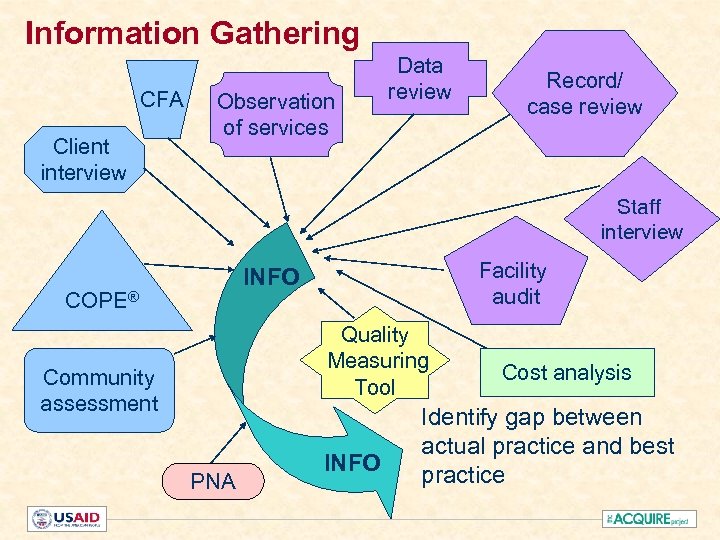
Information Gathering CFA Client interview Observation of services Data review Record/ case review Staff interview Facility audit INFO COPE® Quality Measuring Tool Community assessment PNA INFO Cost analysis Identify gap between actual practice and best practice
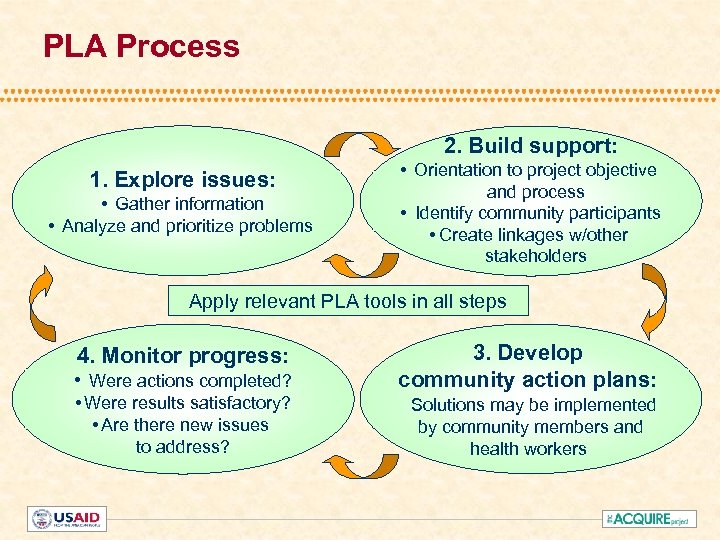
PLA Process 2. Build support: 1. Explore issues: • Gather information • Analyze and prioritize problems • Orientation to project objective and process • Identify community participants • Create linkages w/other stakeholders Apply relevant PLA tools in all steps • Were actions completed? 3. Develop community action plans: • Were results satisfactory? • Are there new issues to address? Solutions may be implemented by community members and health workers 4. Monitor progress:
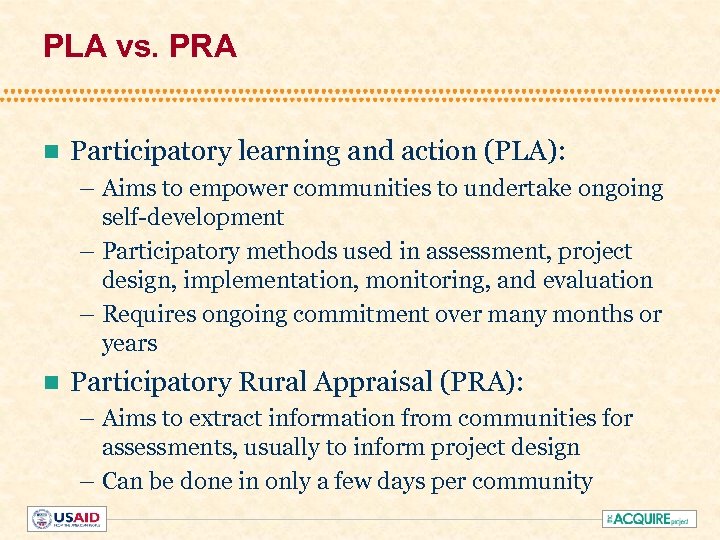
PLA vs. PRA n Participatory learning and action (PLA): – Aims to empower communities to undertake ongoing self-development – Participatory methods used in assessment, project design, implementation, monitoring, and evaluation – Requires ongoing commitment over many months or years n Participatory Rural Appraisal (PRA): – Aims to extract information from communities for assessments, usually to inform project design – Can be done in only a few days per community
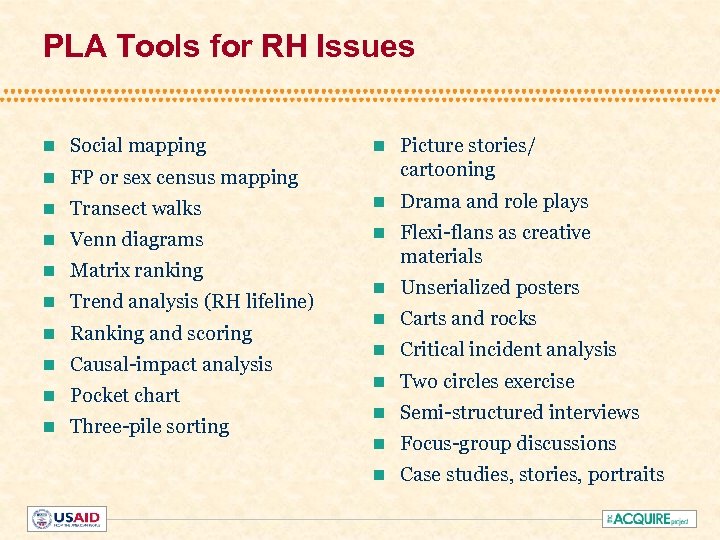
PLA Tools for RH Issues n Social mapping n Picture stories/ cartooning n FP or sex census mapping n Transect walks n Drama and role plays n Venn diagrams n n Matrix ranking Flexi-flans as creative materials n Trend analysis (RH lifeline) n Unserialized posters n Ranking and scoring n Carts and rocks n Causal-impact analysis n Critical incident analysis n Pocket chart n Two circles exercise n Three-pile sorting n Semi-structured interviews n Focus-group discussions n Case studies, stories, portraits
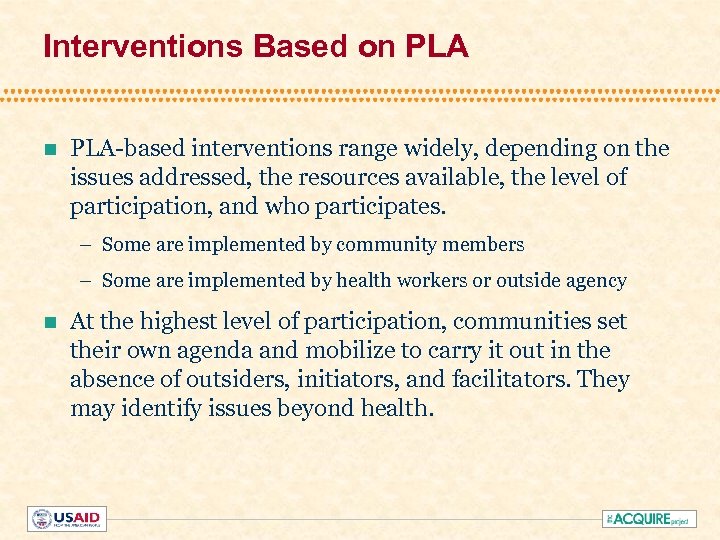
Interventions Based on PLA-based interventions range widely, depending on the issues addressed, the resources available, the level of participation, and who participates. – Some are implemented by community members – Some are implemented by health workers or outside agency n At the highest level of participation, communities set their own agenda and mobilize to carry it out in the absence of outsiders, initiators, and facilitators. They may identify issues beyond health.
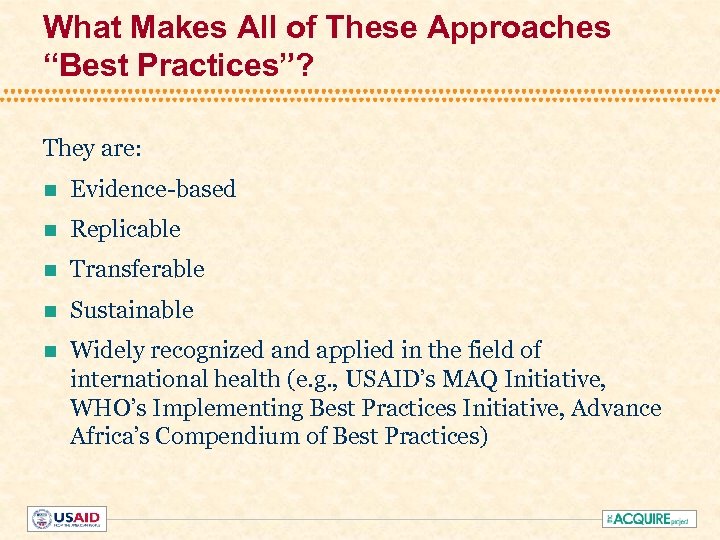
What Makes All of These Approaches “Best Practices”? They are: n Evidence-based n Replicable n Transferable n Sustainable n Widely recognized and applied in the field of international health (e. g. , USAID’s MAQ Initiative, WHO’s Implementing Best Practices Initiative, Advance Africa’s Compendium of Best Practices)
Why Integrate These Approaches? n ACQUIRE partners bring proven, effective approaches to improve provider performance and quality of services. n The approaches are mutually reinforcing. n Together, they promote the ACQUIRE Project results: – Access – Quality – Use of RH services
What Are the Similarities in These Approaches? n All are participatory. n All rely on a step-by-step process to identify gaps and solutions. n All include root-cause analysis of gaps. n All include stakeholder involvement and empowerment.
What Are the Differences in These Approaches? (1) n PI focuses on provider performance and provider perspective n QI focuses on clients’ rights and staff needs and the client perspective
What Are the Differences in These Approaches? (2) n Both PLA and Community COPE emphasize the community perspective, but: – Community COPE focuses on involving communities in improving facility-based health care – PLA includes more tools and addresses community empowerment more broadly around health and/or other issues – Under ACQUIRE, PLA methods have also been applied to tailor information and marketing materials and referral systems based on community perceptions of underutilized methods
What Do We Recommend? (1) n PI is most appropriate at national, regional, and district levels, but can be applied to specific cadres of providers. n Engender. Health’s QI tools address multiple levels, with a focus on the facility level. n Community COPE and PLA are complementary. – e. g. , use any of the PLA tools when doing Community COPE
What Do We Recommend? (2) n Use PIA to identify needs at higher program levels. n When implementing any of the approaches, at the datagathering stage, consider adapting tools from any of the other approaches. – In a PNA, consider using QMT, the COPE client interview guide, or any PLA tool. – Within PLA, consider using Community COPE tools. n Apply QI and PLA as ongoing processes to improve quality and address the needs identified.
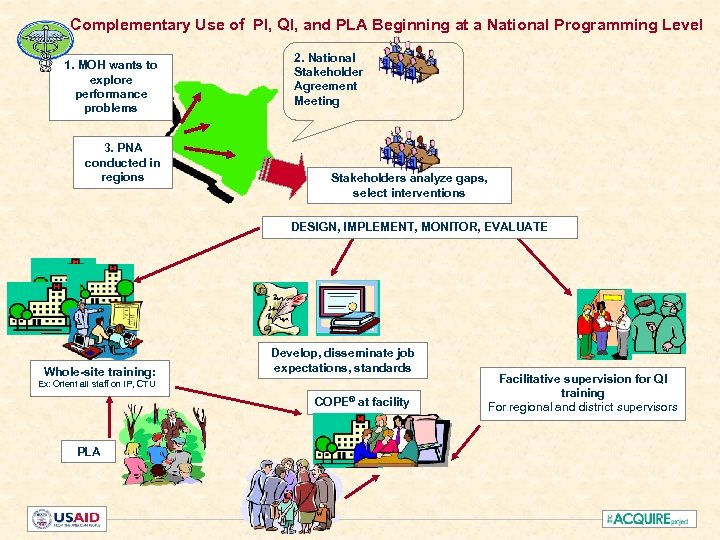
Complementary Use of PI, QI, and PLA Beginning at a National Programming Level 1. MOH wants to explore performance problems 3. PNA conducted in regions 2. National Stakeholder Agreement Meeting Stakeholders analyze gaps, select interventions DESIGN, IMPLEMENT, MONITOR, EVALUATE Whole-site training: Develop, disseminate job expectations, standards Ex: Orient all staff on IP, CTU COPE® at facility PLA Facilitative supervision for QI training For regional and district supervisors
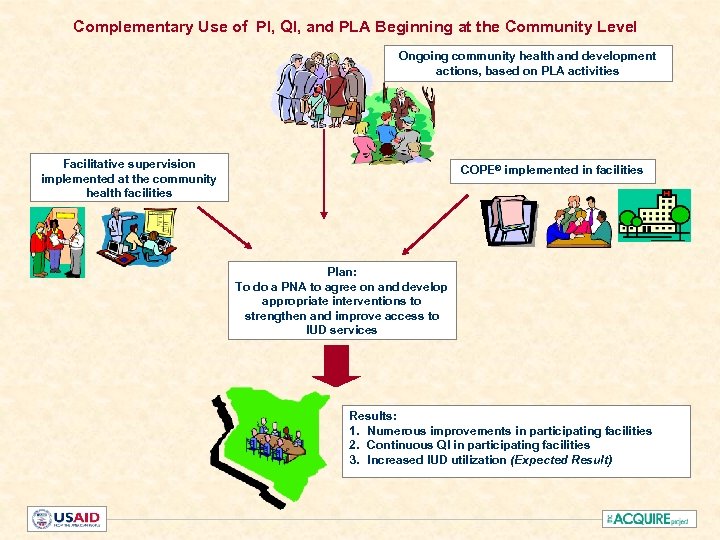
Complementary Use of PI, QI, and PLA Beginning at the Community Level Ongoing community health and development actions, based on PLA activities Facilitative supervision implemented at the community health facilities COPE® implemented in facilities Plan: To do a PNA to agree on and develop appropriate interventions to strengthen and improve access to IUD services Results: 1. Numerous improvements in participating facilities 2. Continuous QI in participating facilities 3. Increased IUD utilization (Expected Result)
1279d177d394b4bd3884ca93f79dbeb9.ppt