370ba82d35aadd3b731b43d16f6ddbb9.ppt
- Количество слайдов: 18
 Integrated care pathways Dr Jeremy Rogers MD MRCGP Senior Clinical Fellow in Health Informatics Northwest Institute of Bio-Health Informatics
Integrated care pathways Dr Jeremy Rogers MD MRCGP Senior Clinical Fellow in Health Informatics Northwest Institute of Bio-Health Informatics
 Talk Outline ICPs e. ICPs Challenges
Talk Outline ICPs e. ICPs Challenges
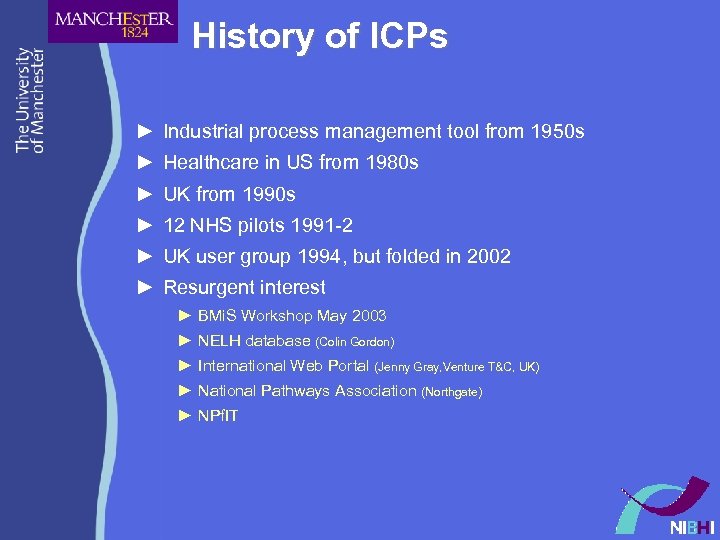 History of ICPs ► Industrial process management tool from 1950 s ► Healthcare in US from 1980 s ► UK from 1990 s ► 12 NHS pilots 1991 -2 ► UK user group 1994, but folded in 2002 ► Resurgent interest ► BMi. S Workshop May 2003 ► NELH database (Colin Gordon) ► International Web Portal (Jenny Gray, Venture T&C, UK) ► National Pathways Association (Northgate) ► NPf. IT
History of ICPs ► Industrial process management tool from 1950 s ► Healthcare in US from 1980 s ► UK from 1990 s ► 12 NHS pilots 1991 -2 ► UK user group 1994, but folded in 2002 ► Resurgent interest ► BMi. S Workshop May 2003 ► NELH database (Colin Gordon) ► International Web Portal (Jenny Gray, Venture T&C, UK) ► National Pathways Association (Northgate) ► NPf. IT
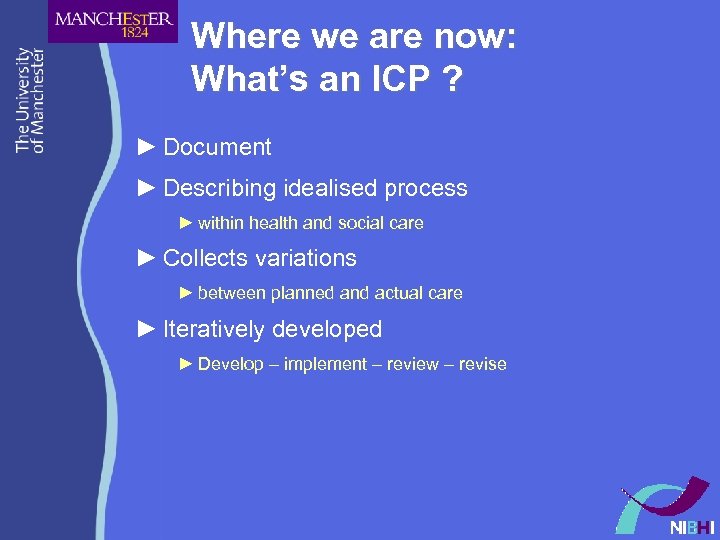 Where we are now: What’s an ICP ? ► Document ► Describing idealised process ► within health and social care ► Collects variations ► between planned and actual care ► Iteratively developed ► Develop – implement – review – revise
Where we are now: What’s an ICP ? ► Document ► Describing idealised process ► within health and social care ► Collects variations ► between planned and actual care ► Iteratively developed ► Develop – implement – review – revise
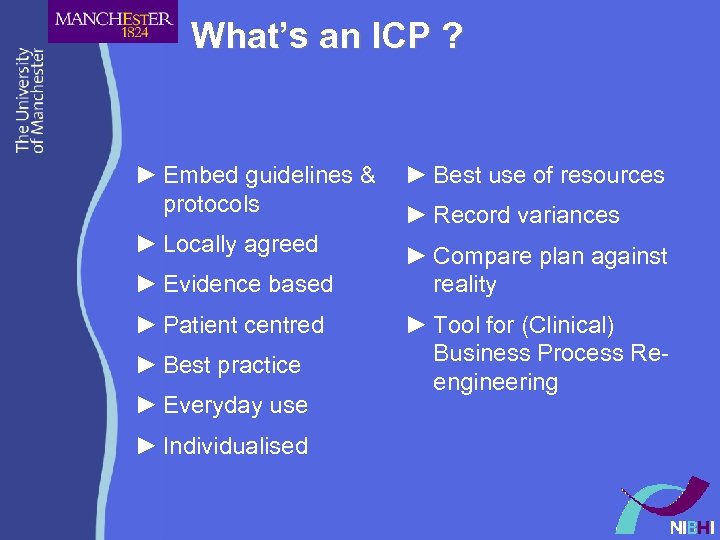 What’s an ICP ? ► Embed guidelines & protocols ► Best use of resources ► Locally agreed ► Compare plan against reality ► Evidence based ► Patient centred ► Best practice ► Everyday use ► Individualised ► Record variances ► Tool for (Clinical) Business Process Reengineering
What’s an ICP ? ► Embed guidelines & protocols ► Best use of resources ► Locally agreed ► Compare plan against reality ► Evidence based ► Patient centred ► Best practice ► Everyday use ► Individualised ► Record variances ► Tool for (Clinical) Business Process Reengineering
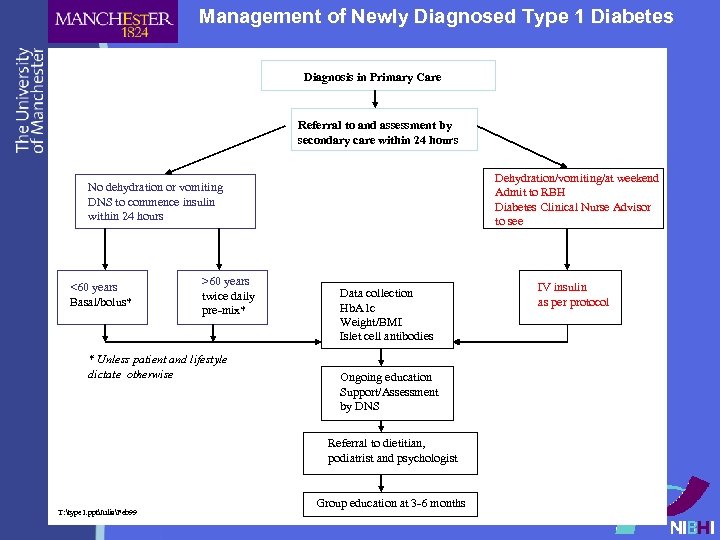 Management of Newly Diagnosed Type 1 Diabetes Diagnosis in Primary Care Referral to and assessment by secondary care within 24 hours Dehydration/vomiting/at weekend Admit to RBH Diabetes Clinical Nurse Advisor to see No dehydration or vomiting DNS to commence insulin within 24 hours <60 years Basal/bolus* >60 years twice daily pre-mix* * Unless patient and lifestyle dictate otherwise Data collection Hb. A 1 c Weight/BMI Islet cell antibodies Ongoing education Support/Assessment by DNS Referral to dietitian, podiatrist and psychologist T: type 1. pptJuliaFeb 99 Group education at 3 -6 months IV insulin as per protocol
Management of Newly Diagnosed Type 1 Diabetes Diagnosis in Primary Care Referral to and assessment by secondary care within 24 hours Dehydration/vomiting/at weekend Admit to RBH Diabetes Clinical Nurse Advisor to see No dehydration or vomiting DNS to commence insulin within 24 hours <60 years Basal/bolus* >60 years twice daily pre-mix* * Unless patient and lifestyle dictate otherwise Data collection Hb. A 1 c Weight/BMI Islet cell antibodies Ongoing education Support/Assessment by DNS Referral to dietitian, podiatrist and psychologist T: type 1. pptJuliaFeb 99 Group education at 3 -6 months IV insulin as per protocol
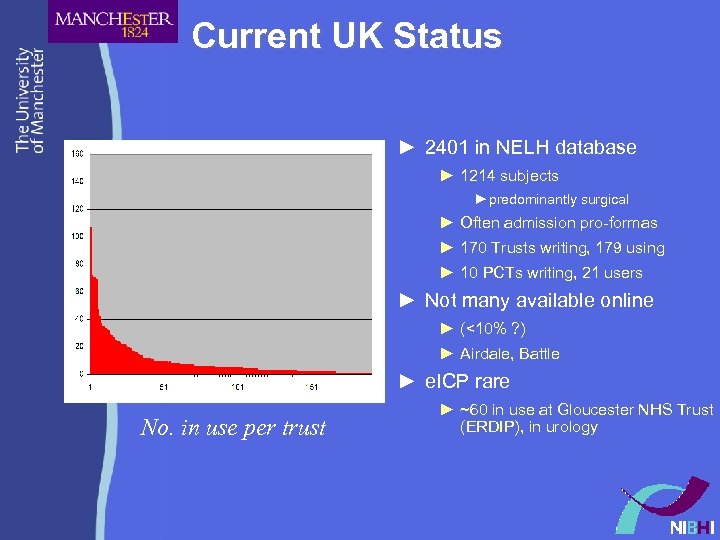 Current UK Status ► 2401 in NELH database ► 1214 subjects ►predominantly surgical ► Often admission pro-formas ► 170 Trusts writing, 179 using ► 10 PCTs writing, 21 users ► Not many available online ► (<10% ? ) ► Airdale, Battle ► e. ICP rare No. in use per trust ► ~60 in use at Gloucester NHS Trust (ERDIP), in urology
Current UK Status ► 2401 in NELH database ► 1214 subjects ►predominantly surgical ► Often admission pro-formas ► 170 Trusts writing, 179 using ► 10 PCTs writing, 21 users ► Not many available online ► (<10% ? ) ► Airdale, Battle ► e. ICP rare No. in use per trust ► ~60 in use at Gloucester NHS Trust (ERDIP), in urology
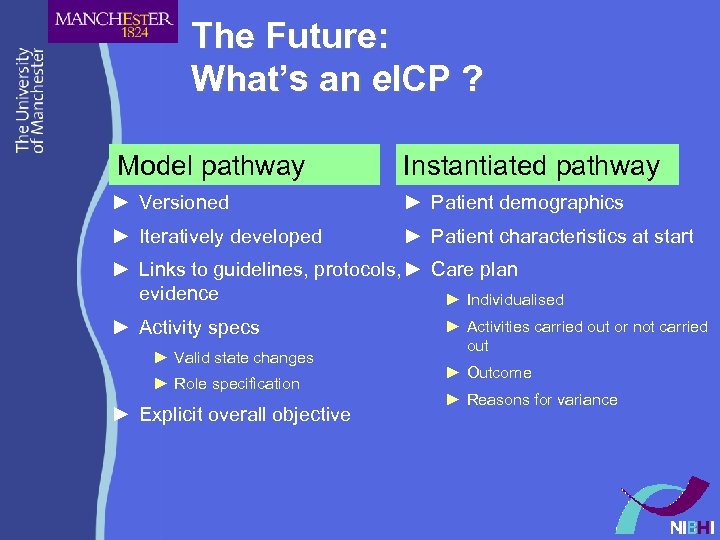 The Future: What’s an e. ICP ? Model pathway Instantiated pathway ► Versioned ► Patient demographics ► Iteratively developed ► Patient characteristics at start ► Links to guidelines, protocols, ► Care plan evidence ► Individualised ► Activity specs ► Valid state changes ► Role specification ► Explicit overall objective ► Activities carried out or not carried out ► Outcome ► Reasons for variance
The Future: What’s an e. ICP ? Model pathway Instantiated pathway ► Versioned ► Patient demographics ► Iteratively developed ► Patient characteristics at start ► Links to guidelines, protocols, ► Care plan evidence ► Individualised ► Activity specs ► Valid state changes ► Role specification ► Explicit overall objective ► Activities carried out or not carried out ► Outcome ► Reasons for variance
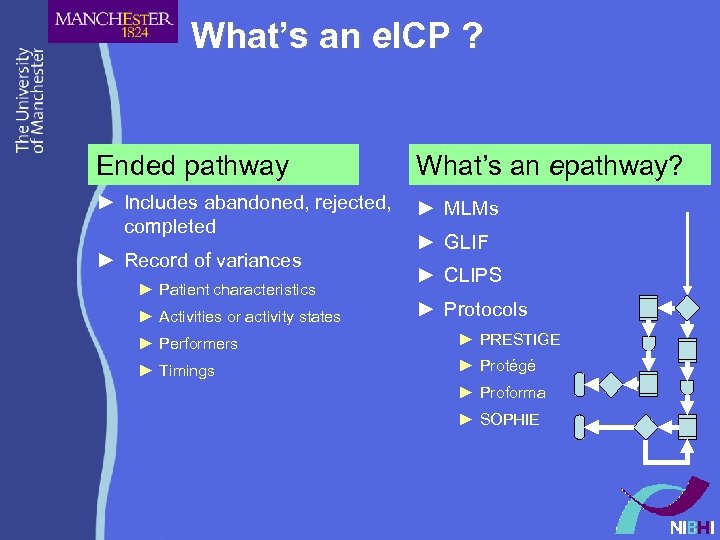 What’s an e. ICP ? Ended pathway What’s an epathway? ► Includes abandoned, rejected, completed ► MLMs ► Record of variances ► Patient characteristics ► Activities or activity states ► GLIF ► CLIPS ► Protocols ► Performers ► PRESTIGE ► Timings ► Protégé ► Proforma ► SOPHIE
What’s an e. ICP ? Ended pathway What’s an epathway? ► Includes abandoned, rejected, completed ► MLMs ► Record of variances ► Patient characteristics ► Activities or activity states ► GLIF ► CLIPS ► Protocols ► Performers ► PRESTIGE ► Timings ► Protégé ► Proforma ► SOPHIE
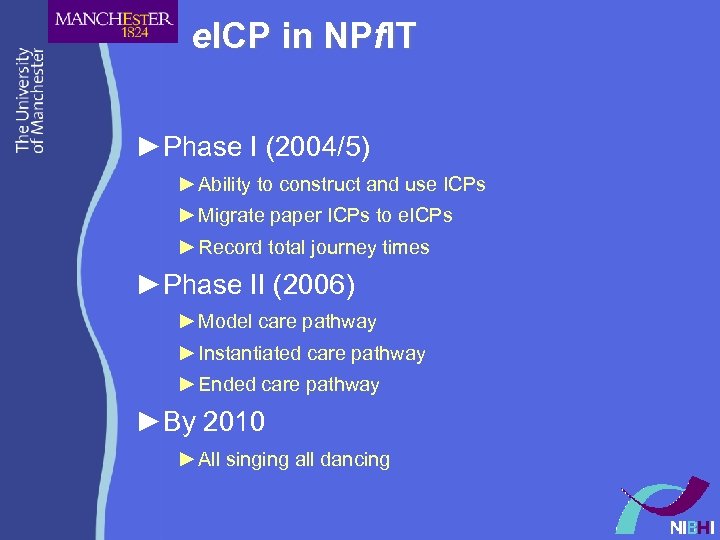 e. ICP in NPf. IT ►Phase I (2004/5) ► Ability to construct and use ICPs ► Migrate paper ICPs to e. ICPs ► Record total journey times ►Phase II (2006) ► Model care pathway ► Instantiated care pathway ► Ended care pathway ►By 2010 ► All singing all dancing
e. ICP in NPf. IT ►Phase I (2004/5) ► Ability to construct and use ICPs ► Migrate paper ICPs to e. ICPs ► Record total journey times ►Phase II (2006) ► Model care pathway ► Instantiated care pathway ► Ended care pathway ►By 2010 ► All singing all dancing
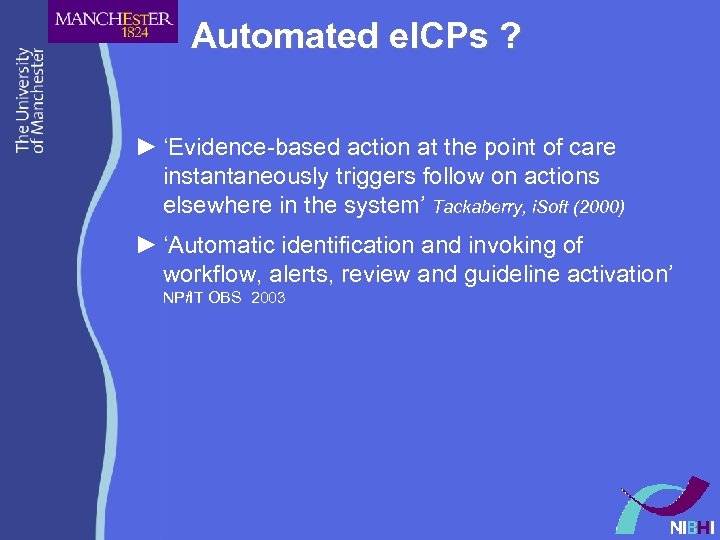 Automated e. ICPs ? ► ‘Evidence-based action at the point of care instantaneously triggers follow on actions elsewhere in the system’ Tackaberry, i. Soft (2000) ► ‘Automatic identification and invoking of workflow, alerts, review and guideline activation’ NPf. IT OBS 2003
Automated e. ICPs ? ► ‘Evidence-based action at the point of care instantaneously triggers follow on actions elsewhere in the system’ Tackaberry, i. Soft (2000) ► ‘Automatic identification and invoking of workflow, alerts, review and guideline activation’ NPf. IT OBS 2003
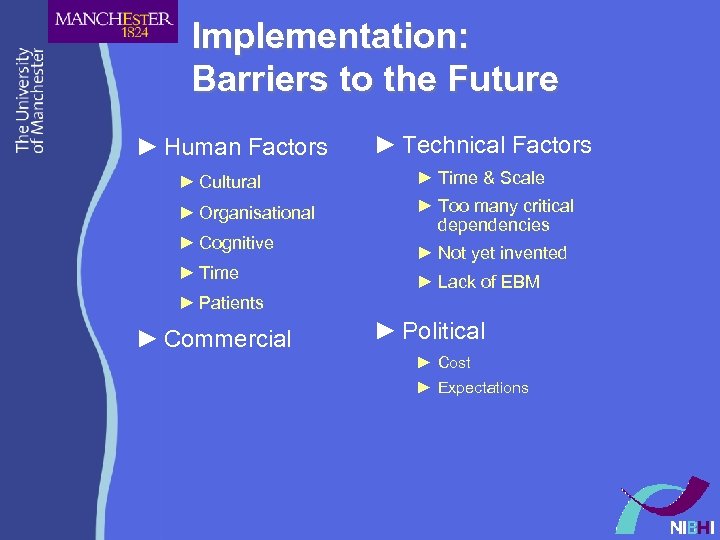 Implementation: Barriers to the Future ► Human Factors ► Technical Factors ► Cultural ► Time & Scale ► Organisational ► Too many critical dependencies ► Cognitive ► Time ► Not yet invented ► Lack of EBM ► Patients ► Commercial ► Political ► Cost ► Expectations
Implementation: Barriers to the Future ► Human Factors ► Technical Factors ► Cultural ► Time & Scale ► Organisational ► Too many critical dependencies ► Cognitive ► Time ► Not yet invented ► Lack of EBM ► Patients ► Commercial ► Political ► Cost ► Expectations
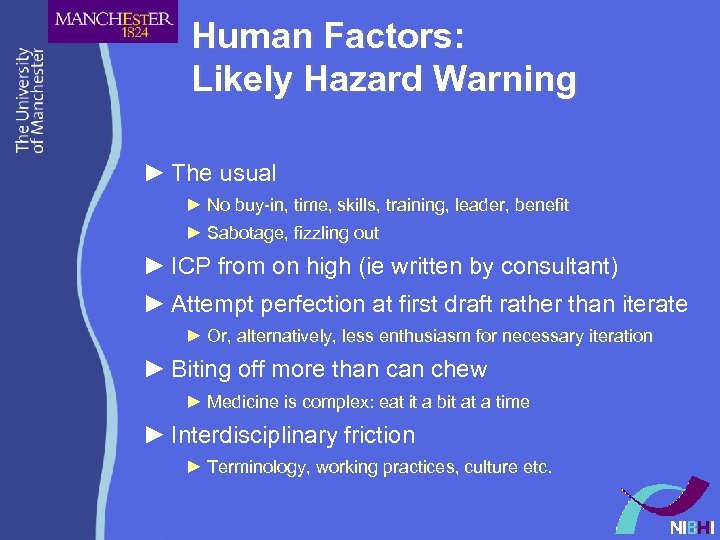 Human Factors: Likely Hazard Warning ► The usual ► No buy-in, time, skills, training, leader, benefit ► Sabotage, fizzling out ► ICP from on high (ie written by consultant) ► Attempt perfection at first draft rather than iterate ► Or, alternatively, less enthusiasm for necessary iteration ► Biting off more than chew ► Medicine is complex: eat it a bit at a time ► Interdisciplinary friction ► Terminology, working practices, culture etc.
Human Factors: Likely Hazard Warning ► The usual ► No buy-in, time, skills, training, leader, benefit ► Sabotage, fizzling out ► ICP from on high (ie written by consultant) ► Attempt perfection at first draft rather than iterate ► Or, alternatively, less enthusiasm for necessary iteration ► Biting off more than chew ► Medicine is complex: eat it a bit at a time ► Interdisciplinary friction ► Terminology, working practices, culture etc.
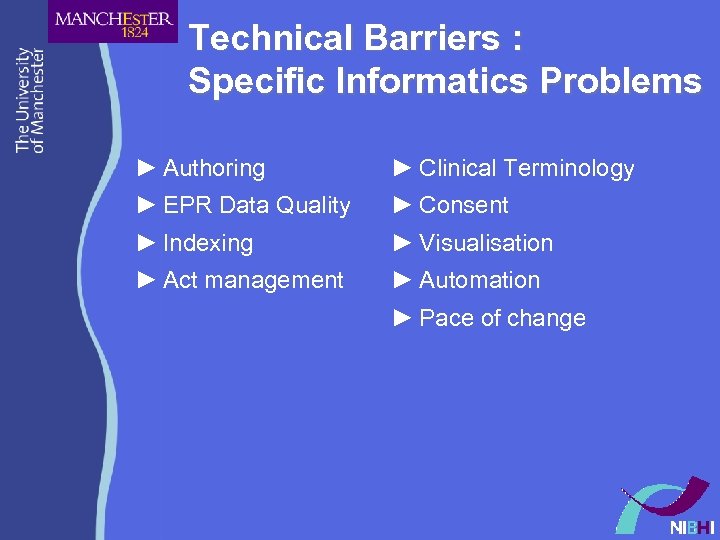 Technical Barriers : Specific Informatics Problems ► Authoring ► Clinical Terminology ► EPR Data Quality ► Consent ► Indexing ► Visualisation ► Act management ► Automation ► Pace of change
Technical Barriers : Specific Informatics Problems ► Authoring ► Clinical Terminology ► EPR Data Quality ► Consent ► Indexing ► Visualisation ► Act management ► Automation ► Pace of change
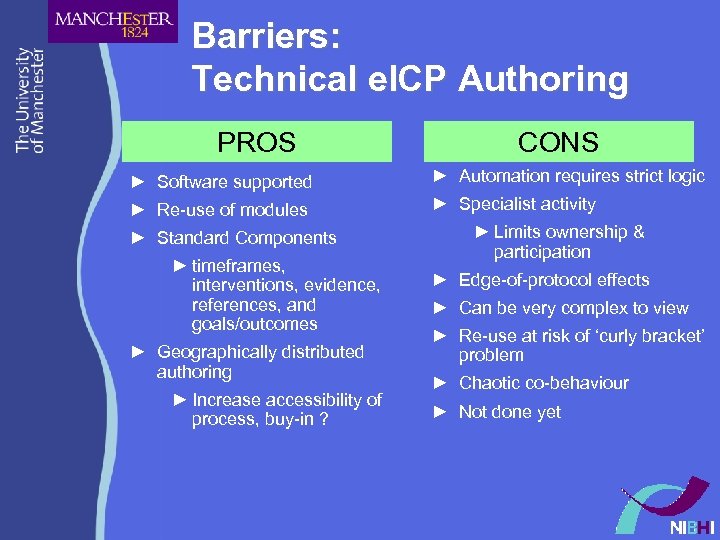 Barriers: Technical e. ICP Authoring PROS CONS ► Software supported ► Automation requires strict logic ► Re-use of modules ► Specialist activity ► Standard Components ► timeframes, interventions, evidence, references, and goals/outcomes ► Geographically distributed authoring ► Increase accessibility of process, buy-in ? ► Limits ownership & participation ► Edge-of-protocol effects ► Can be very complex to view ► Re-use at risk of ‘curly bracket’ problem ► Chaotic co-behaviour ► Not done yet
Barriers: Technical e. ICP Authoring PROS CONS ► Software supported ► Automation requires strict logic ► Re-use of modules ► Specialist activity ► Standard Components ► timeframes, interventions, evidence, references, and goals/outcomes ► Geographically distributed authoring ► Increase accessibility of process, buy-in ? ► Limits ownership & participation ► Edge-of-protocol effects ► Can be very complex to view ► Re-use at risk of ‘curly bracket’ problem ► Chaotic co-behaviour ► Not done yet
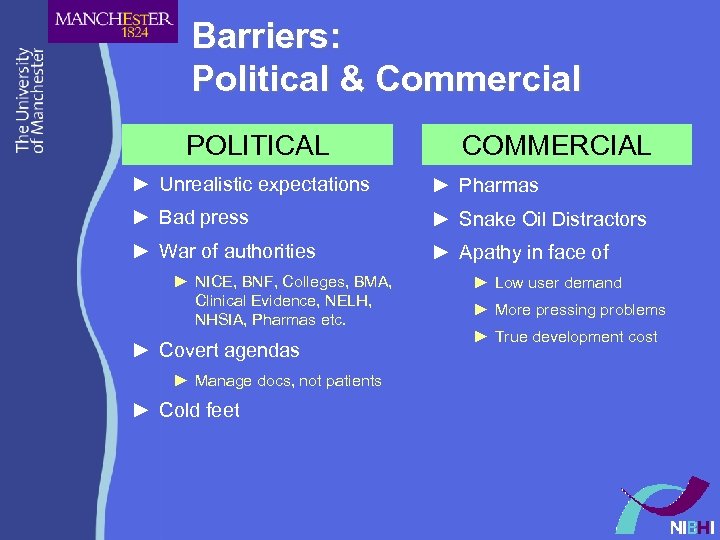 Barriers: Political & Commercial POLITICAL COMMERCIAL ► Unrealistic expectations ► Pharmas ► Bad press ► Snake Oil Distractors ► War of authorities ► Apathy in face of ► NICE, BNF, Colleges, BMA, Clinical Evidence, NELH, NHSIA, Pharmas etc. ► Covert agendas ► Manage docs, not patients ► Cold feet ► Low user demand ► More pressing problems ► True development cost
Barriers: Political & Commercial POLITICAL COMMERCIAL ► Unrealistic expectations ► Pharmas ► Bad press ► Snake Oil Distractors ► War of authorities ► Apathy in face of ► NICE, BNF, Colleges, BMA, Clinical Evidence, NELH, NHSIA, Pharmas etc. ► Covert agendas ► Manage docs, not patients ► Cold feet ► Low user demand ► More pressing problems ► True development cost


