e59626b9c13fae1981cf07440638d118.ppt
- Количество слайдов: 144
 Insomnia Victoria E Judd M. D.
Insomnia Victoria E Judd M. D.
 Sleep Quotes • People who say they sleep like a baby usually don't have one. ~Leo J. Burke • If people were meant to pop out of bed, we'd all sleep in toasters. Author unknown • O sleep, O gentle sleep, Nature's soft nurse, how have I frighted thee, That thou no more wilt weigh my eyelids down And steep my sense in forgetfulness? ~William Shakespeare, Henry IV, Part I
Sleep Quotes • People who say they sleep like a baby usually don't have one. ~Leo J. Burke • If people were meant to pop out of bed, we'd all sleep in toasters. Author unknown • O sleep, O gentle sleep, Nature's soft nurse, how have I frighted thee, That thou no more wilt weigh my eyelids down And steep my sense in forgetfulness? ~William Shakespeare, Henry IV, Part I
 Insomnia • No disclosures
Insomnia • No disclosures
 Objectives • • • Learn about sleep List pathogenesis/types of insomnia Discuss epidemiology of insomnia Learn about the impact of insomnia List common etiologies of insomnia Discuss therapy -Cognitive-behavioral therapy -Pharmacologic treatment
Objectives • • • Learn about sleep List pathogenesis/types of insomnia Discuss epidemiology of insomnia Learn about the impact of insomnia List common etiologies of insomnia Discuss therapy -Cognitive-behavioral therapy -Pharmacologic treatment
 Sleep Is • • Active Complex Highly Regulated Involves different areas in the brain Purpose is not understood Essential to life/necessary We all do it
Sleep Is • • Active Complex Highly Regulated Involves different areas in the brain Purpose is not understood Essential to life/necessary We all do it
 Sleep Deprivation • Our 24/7 lifestyle can be deleterious • Trying to push through the night and stifle a yawn, yet that yawn is the first sign that you’re not so awake as you might like to think – after 18 hours in the absence of sleep, your reaction time slows from ¼ of a second to ½ of a second, and then becomes still longer
Sleep Deprivation • Our 24/7 lifestyle can be deleterious • Trying to push through the night and stifle a yawn, yet that yawn is the first sign that you’re not so awake as you might like to think – after 18 hours in the absence of sleep, your reaction time slows from ¼ of a second to ½ of a second, and then becomes still longer
 Sleep Deprivation • One starts experiencing several bouts of ‘micro-sleep’ – and so, while driving you zone out for say 20 seconds and drift out of your lane, or if studying late then you find yourself rereading the same passage – thus your reaction time becomes roughly equivalent to a person with a blood alcohol level of 0. 08, sufficient to get you arrested in 49 states
Sleep Deprivation • One starts experiencing several bouts of ‘micro-sleep’ – and so, while driving you zone out for say 20 seconds and drift out of your lane, or if studying late then you find yourself rereading the same passage – thus your reaction time becomes roughly equivalent to a person with a blood alcohol level of 0. 08, sufficient to get you arrested in 49 states
 Sleep Deprivation • Charles Augustus Lindbergh, in 1927, in his Spirit of St. Louis, during his 1 st solo Atlantic crossing from Long Island to Paris, experienced visual hallucinations which remitted with recovery sleep • There is a 10% increase in MVA’s following switching to daylight savings when the day is shortened by 1 hour
Sleep Deprivation • Charles Augustus Lindbergh, in 1927, in his Spirit of St. Louis, during his 1 st solo Atlantic crossing from Long Island to Paris, experienced visual hallucinations which remitted with recovery sleep • There is a 10% increase in MVA’s following switching to daylight savings when the day is shortened by 1 hour
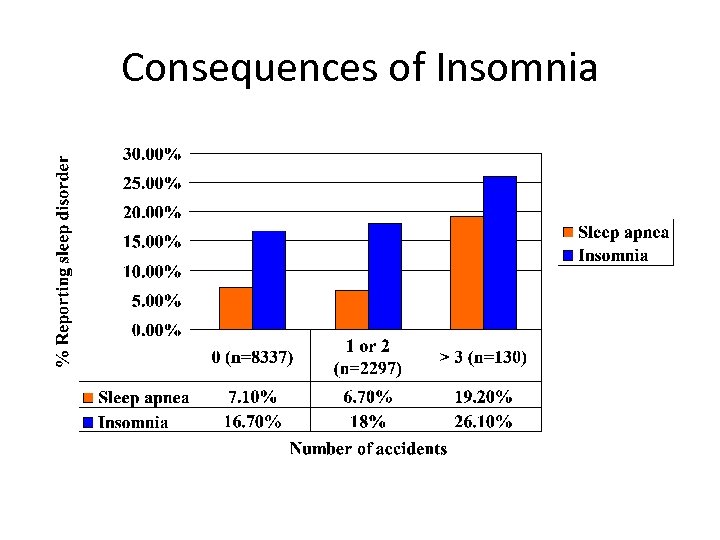 Consequences of Insomnia
Consequences of Insomnia
 Sleep Deprivation • Mood disturbance with irritability, transient paranoia, disorientation, performance deficits, severe fatigue or hypomania – all sequelae of prolonged sleep deprivation • Chronic sleep deprivation may reach a point at which the very ability to catch up on sleep is damaged, such that what’s lost is lost • Bodes ill for students, soldiers, et. al, trying to acquire new information while sleep-deprived
Sleep Deprivation • Mood disturbance with irritability, transient paranoia, disorientation, performance deficits, severe fatigue or hypomania – all sequelae of prolonged sleep deprivation • Chronic sleep deprivation may reach a point at which the very ability to catch up on sleep is damaged, such that what’s lost is lost • Bodes ill for students, soldiers, et. al, trying to acquire new information while sleep-deprived
 Sleep Disorders • Sleep disorders are common • Sleep disorders are serious • Sleep disorders are treatable • Sleep disorders are underdiagnosed
Sleep Disorders • Sleep disorders are common • Sleep disorders are serious • Sleep disorders are treatable • Sleep disorders are underdiagnosed
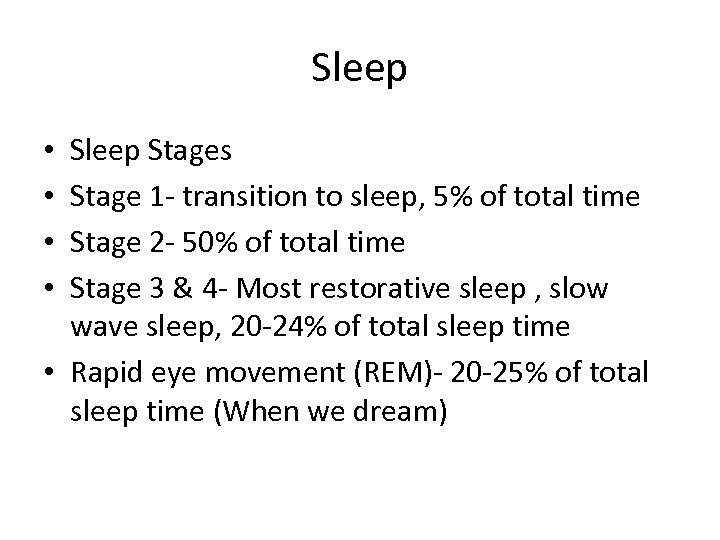 Sleep Stages Stage 1 - transition to sleep, 5% of total time Stage 2 - 50% of total time Stage 3 & 4 - Most restorative sleep , slow wave sleep, 20 -24% of total sleep time • Rapid eye movement (REM)- 20 -25% of total sleep time (When we dream) • •
Sleep Stages Stage 1 - transition to sleep, 5% of total time Stage 2 - 50% of total time Stage 3 & 4 - Most restorative sleep , slow wave sleep, 20 -24% of total sleep time • Rapid eye movement (REM)- 20 -25% of total sleep time (When we dream) • •
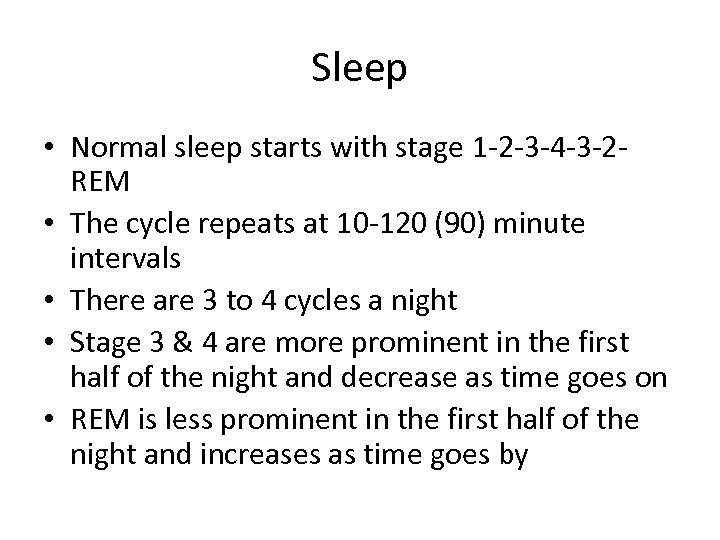 Sleep • Normal sleep starts with stage 1 -2 -3 -4 -3 -2 REM • The cycle repeats at 10 -120 (90) minute intervals • There are 3 to 4 cycles a night • Stage 3 & 4 are more prominent in the first half of the night and decrease as time goes on • REM is less prominent in the first half of the night and increases as time goes by
Sleep • Normal sleep starts with stage 1 -2 -3 -4 -3 -2 REM • The cycle repeats at 10 -120 (90) minute intervals • There are 3 to 4 cycles a night • Stage 3 & 4 are more prominent in the first half of the night and decrease as time goes on • REM is less prominent in the first half of the night and increases as time goes by
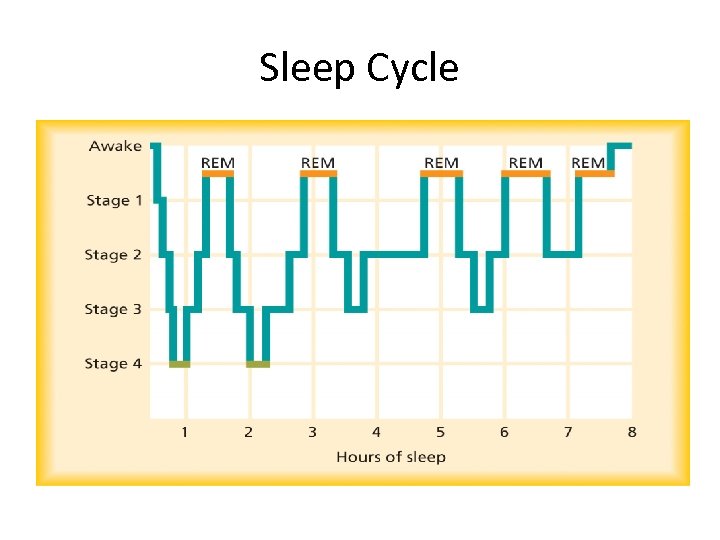 Sleep Cycle
Sleep Cycle
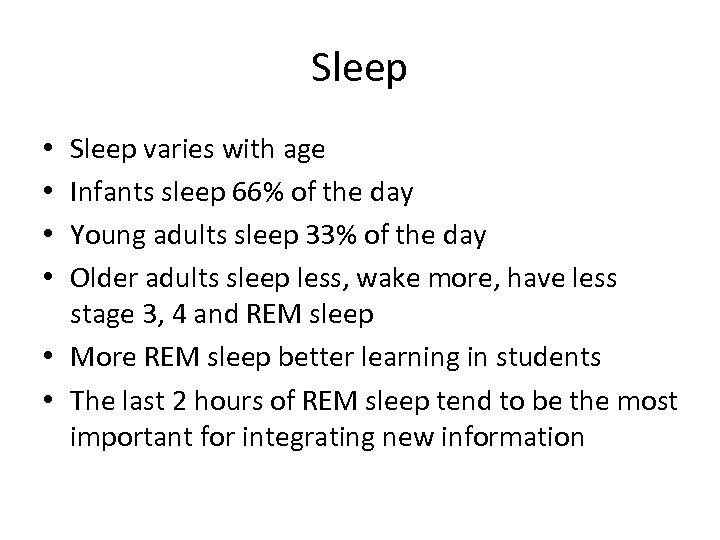 Sleep varies with age Infants sleep 66% of the day Young adults sleep 33% of the day Older adults sleep less, wake more, have less stage 3, 4 and REM sleep • More REM sleep better learning in students • The last 2 hours of REM sleep tend to be the most important for integrating new information • •
Sleep varies with age Infants sleep 66% of the day Young adults sleep 33% of the day Older adults sleep less, wake more, have less stage 3, 4 and REM sleep • More REM sleep better learning in students • The last 2 hours of REM sleep tend to be the most important for integrating new information • •
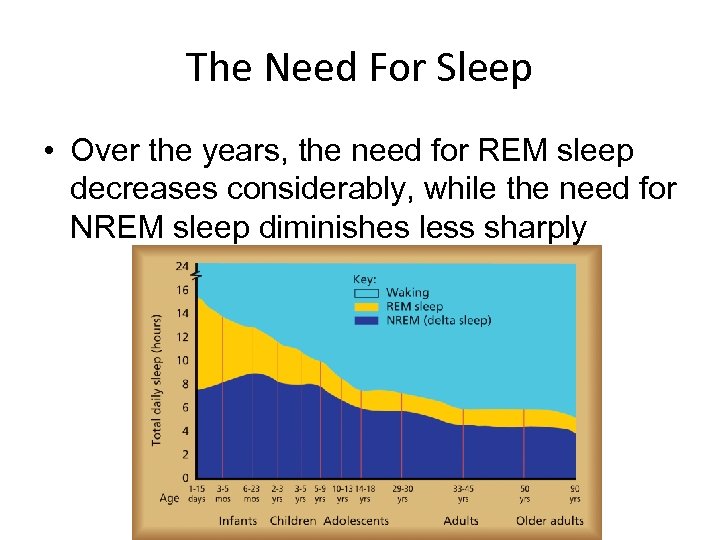 The Need For Sleep • Over the years, the need for REM sleep decreases considerably, while the need for NREM sleep diminishes less sharply
The Need For Sleep • Over the years, the need for REM sleep decreases considerably, while the need for NREM sleep diminishes less sharply
 Insomnia - DSM IV criteria 1. Difficulty initiating or maintaining sleep, or non-restorative sleep, for at least 1 month. 2. Clinically significant distress or impairment in social/occupational functioning 3. Not exclusively due to another sleep disorder 4. Not exclusively due to another mental disorder 5. Not due to the physiological effects of a substance or a medical disorder
Insomnia - DSM IV criteria 1. Difficulty initiating or maintaining sleep, or non-restorative sleep, for at least 1 month. 2. Clinically significant distress or impairment in social/occupational functioning 3. Not exclusively due to another sleep disorder 4. Not exclusively due to another mental disorder 5. Not due to the physiological effects of a substance or a medical disorder
 Insomnia is present when all three of the following criteria are met: • A complaint of difficulty initiating sleep, difficulty maintaining sleep, or waking up too early. • The above sleep difficulty occurs despite adequate opportunity and circumstances for sleep. • The impaired sleep produces deficits in daytime function.
Insomnia is present when all three of the following criteria are met: • A complaint of difficulty initiating sleep, difficulty maintaining sleep, or waking up too early. • The above sleep difficulty occurs despite adequate opportunity and circumstances for sleep. • The impaired sleep produces deficits in daytime function.
 Features of Insomnia • Problems initiating sleep (greater than 30 minutes) • Frequent and/or prolonged nocturnal awakenings • Early morning awakenings with an inability to return to sleep • Poor sleep quality and sleep efficiency • Cognitive arousal typically reported • Severity is judged along several dimensions, including frequency, intensity and duration of sleep difficulties. Also impact on daytime functioning, mood and quality of life.
Features of Insomnia • Problems initiating sleep (greater than 30 minutes) • Frequent and/or prolonged nocturnal awakenings • Early morning awakenings with an inability to return to sleep • Poor sleep quality and sleep efficiency • Cognitive arousal typically reported • Severity is judged along several dimensions, including frequency, intensity and duration of sleep difficulties. Also impact on daytime functioning, mood and quality of life.
 Insomnia-Hyperarousal • In experimental models of insomnia, healthy subjects deprived of sleep do not demonstrate the same abnormalities in metabolism, daytime sleepiness, and personality as subjects with insomnia. In an experimental model in which healthy subjects were given caffeine, causing a state of hyperarousal, the healthy subjects had changes in metabolism, daytime sleepiness, and personality similar to the subjects with insomnia. • These results support a theory that insomnia is a manifestation of hyperarousal. In other words, the poor sleep itself may not be the cause of the daytime dysfunction, but merely the nocturnal manifestation of a general disorder of hyperarousability.
Insomnia-Hyperarousal • In experimental models of insomnia, healthy subjects deprived of sleep do not demonstrate the same abnormalities in metabolism, daytime sleepiness, and personality as subjects with insomnia. In an experimental model in which healthy subjects were given caffeine, causing a state of hyperarousal, the healthy subjects had changes in metabolism, daytime sleepiness, and personality similar to the subjects with insomnia. • These results support a theory that insomnia is a manifestation of hyperarousal. In other words, the poor sleep itself may not be the cause of the daytime dysfunction, but merely the nocturnal manifestation of a general disorder of hyperarousability.
 Impact of Insomnia • Biological • Poor function of immune system • Functional impairments • Increased risk of accidents • More likely to report lack of concentration and motivation • Reduced productivity, work/school absenteeism • Increased use of health care services
Impact of Insomnia • Biological • Poor function of immune system • Functional impairments • Increased risk of accidents • More likely to report lack of concentration and motivation • Reduced productivity, work/school absenteeism • Increased use of health care services
 Impact of Insomnia • Psychological health • Increases risk of developing depression, anxiety or substance dependence • Risk factor in suicide – (Ohayon et al. , 1997: Harvey, 2001: Ancoli. Israel & Roth, 1999: Mc. Crae & Lichstein, 2001)
Impact of Insomnia • Psychological health • Increases risk of developing depression, anxiety or substance dependence • Risk factor in suicide – (Ohayon et al. , 1997: Harvey, 2001: Ancoli. Israel & Roth, 1999: Mc. Crae & Lichstein, 2001)
 Impact of Insomnia • Knutson et al found that the quantity and quality of sleep correlate with future blood pressure. In an ancillary to the Coronary Artery Risk Development in Young Adults (CARDIA) cohort study, measurement of sleep for 3 consecutive days in 578 subjects showed that shorter sleep duration and lower sleep maintenance predicted both significantly higher blood pressure levels and adverse changes in blood pressure over the next 5 years.
Impact of Insomnia • Knutson et al found that the quantity and quality of sleep correlate with future blood pressure. In an ancillary to the Coronary Artery Risk Development in Young Adults (CARDIA) cohort study, measurement of sleep for 3 consecutive days in 578 subjects showed that shorter sleep duration and lower sleep maintenance predicted both significantly higher blood pressure levels and adverse changes in blood pressure over the next 5 years.
 Types of Insomnia, Time • Transient insomnia: episodic – Acute illness – Jet lag – Shift change • Short-term insomnia: few days to 3 weeks – Major life event – Substance abuse • Chronic insomnia : longer than 4 weeks – Chronic illness – Psychiatric illness
Types of Insomnia, Time • Transient insomnia: episodic – Acute illness – Jet lag – Shift change • Short-term insomnia: few days to 3 weeks – Major life event – Substance abuse • Chronic insomnia : longer than 4 weeks – Chronic illness – Psychiatric illness
 Circadian Related Insomnia, Time • • Time zone change (jet lag) syndrome Shift work sleep disorder Irregular sleep-wake pattern Delayed sleep phase syndrome Advanced sleep phase syndrome Non-24 -hour sleep-wake disorder Circadian rhythm sleep disorder Shifts with age (adolescent or elderly)
Circadian Related Insomnia, Time • • Time zone change (jet lag) syndrome Shift work sleep disorder Irregular sleep-wake pattern Delayed sleep phase syndrome Advanced sleep phase syndrome Non-24 -hour sleep-wake disorder Circadian rhythm sleep disorder Shifts with age (adolescent or elderly)
 Chronic Insomnia • Complaint of poor sleep causing distress or impairment for 1 to 6 months or longer • Average less than 6. 5 hours sleep per day • Or 3 episodes per week of: – Taking longer than 30 minutes to fall asleep – Waking up during the night for at least an hour • Not accounted for by another sleep disorder, mental illness, medical illness or substance abuse.
Chronic Insomnia • Complaint of poor sleep causing distress or impairment for 1 to 6 months or longer • Average less than 6. 5 hours sleep per day • Or 3 episodes per week of: – Taking longer than 30 minutes to fall asleep – Waking up during the night for at least an hour • Not accounted for by another sleep disorder, mental illness, medical illness or substance abuse.
 Types of Insomnia Primary insomnia • Idiopathic insomnia — Insomnia arising in infancy or childhood with a persistent, unremitting course • Psychophysiologic insomnia — Insomnia due to a maladaptive conditioned response in which the patient learns to associate the bed environment with heightened arousal rather than sleep; onset often associated with an event causing acute insomnia, with the sleep disturbance persisting despite resolution of the precipitating factor • Paradoxical insomnia (sleep-state misperception) — Insomnia characterized by a marked mismatch between the patient’s description of sleep duration and objective polysomnographic findings
Types of Insomnia Primary insomnia • Idiopathic insomnia — Insomnia arising in infancy or childhood with a persistent, unremitting course • Psychophysiologic insomnia — Insomnia due to a maladaptive conditioned response in which the patient learns to associate the bed environment with heightened arousal rather than sleep; onset often associated with an event causing acute insomnia, with the sleep disturbance persisting despite resolution of the precipitating factor • Paradoxical insomnia (sleep-state misperception) — Insomnia characterized by a marked mismatch between the patient’s description of sleep duration and objective polysomnographic findings
 Types of Insomnia • • • Secondary insomnia Adjustment insomnia — Insomnia associated with active psychosocial stressors Inadequate sleep hygiene — Insomnia associated with lifestyle habits that impair sleep Insomnia due to a psychiatric disorder — Insomnia due to an active psychiatric disorder, such as anxiety or depression Insomnia due to a medical condition — Insomnia due to a condition such as the restless legs syndrome, chronic pain, nocturnal cough or dyspnea, or hot flashes Insomnia due to a drug or substance — Insomnia due to consumption or discontinuation of medication, drugs of abuse, alcohol, or caffeine
Types of Insomnia • • • Secondary insomnia Adjustment insomnia — Insomnia associated with active psychosocial stressors Inadequate sleep hygiene — Insomnia associated with lifestyle habits that impair sleep Insomnia due to a psychiatric disorder — Insomnia due to an active psychiatric disorder, such as anxiety or depression Insomnia due to a medical condition — Insomnia due to a condition such as the restless legs syndrome, chronic pain, nocturnal cough or dyspnea, or hot flashes Insomnia due to a drug or substance — Insomnia due to consumption or discontinuation of medication, drugs of abuse, alcohol, or caffeine
 Proper Diagnosis • The medical interview is everything • Focus on underlying causes • Sleep partner should be present for the interview if possible • Full medication list is required (OTC, Rx, Natural) • Substances and alcohol use
Proper Diagnosis • The medical interview is everything • Focus on underlying causes • Sleep partner should be present for the interview if possible • Full medication list is required (OTC, Rx, Natural) • Substances and alcohol use
 Interview • Sleep history…is there trouble with: - falling asleep? - maintaining sleep? - not being able to go back to sleep? - early awakenings? - not feeling rested? - daytime consequences?
Interview • Sleep history…is there trouble with: - falling asleep? - maintaining sleep? - not being able to go back to sleep? - early awakenings? - not feeling rested? - daytime consequences?
 Interview • Daytime consequences can you function/stay awake to drive? • Do you experience (or bed-partner report): Leg or arm jerking while asleep? (periodic limb movement disorder) • Loud snoring/gasping/choking, or stopping breathing when asleep? (sleep apnea) • Uncomfortable feelings in your legs that go away with moving them? (restless leg syndrome)
Interview • Daytime consequences can you function/stay awake to drive? • Do you experience (or bed-partner report): Leg or arm jerking while asleep? (periodic limb movement disorder) • Loud snoring/gasping/choking, or stopping breathing when asleep? (sleep apnea) • Uncomfortable feelings in your legs that go away with moving them? (restless leg syndrome)
 Interview • Patients with insomnia typically feel fatigued during the day, but are unable to fall asleep if given a chance to lie down to take a nap. • Patients with poor nocturnal sleep due to other sleep disorders readily fall asleep during the day. ( Except poor sleep hygiene. )
Interview • Patients with insomnia typically feel fatigued during the day, but are unable to fall asleep if given a chance to lie down to take a nap. • Patients with poor nocturnal sleep due to other sleep disorders readily fall asleep during the day. ( Except poor sleep hygiene. )
 Interview • Usual bedtime • Usual morning awakening time • Time spent in bed awake prior to sleeping, and following the onset of sleep • Estimated time spent asleep • Do you take anything to make you sleep? • Do you drink to help you go to sleep? • What else do you do in your bedroom?
Interview • Usual bedtime • Usual morning awakening time • Time spent in bed awake prior to sleeping, and following the onset of sleep • Estimated time spent asleep • Do you take anything to make you sleep? • Do you drink to help you go to sleep? • What else do you do in your bedroom?
 Interview • • Anything disruptive to sleep? Computer Noises Lights Snoring partner/roommate Partner/roommate with different bed/wake times TV Pets Not feeling safe where you sleep
Interview • • Anything disruptive to sleep? Computer Noises Lights Snoring partner/roommate Partner/roommate with different bed/wake times TV Pets Not feeling safe where you sleep
 Interview • Do you consume: nicotine, caffeine, alcohol, other stimulants, decongestants prior to bedtime? • Half lives are important! • Do you smoke/eat when you wake up, or perform other tasks like cleaning? • Do you check the clock when you wake up early? • What is your pre-bedtime routine: exercise, work, TV, eating?
Interview • Do you consume: nicotine, caffeine, alcohol, other stimulants, decongestants prior to bedtime? • Half lives are important! • Do you smoke/eat when you wake up, or perform other tasks like cleaning? • Do you check the clock when you wake up early? • What is your pre-bedtime routine: exercise, work, TV, eating?
 Interview-Stimulants Some Common Sources: • Coffee: a cup of Joe with ~100 -150 mg of caffeine = 1 mg of amphetamine • Red Bull: 250 m. L = 80 mg of caffeine • Baker’s Chocolate: 1 oz = 26 mg of caffeine • Tea: variable
Interview-Stimulants Some Common Sources: • Coffee: a cup of Joe with ~100 -150 mg of caffeine = 1 mg of amphetamine • Red Bull: 250 m. L = 80 mg of caffeine • Baker’s Chocolate: 1 oz = 26 mg of caffeine • Tea: variable
 Interview • • Medical issues Medication changes Lifestyle issues Work stress School stress Financial stress Relationship stress Complaints from partner
Interview • • Medical issues Medication changes Lifestyle issues Work stress School stress Financial stress Relationship stress Complaints from partner
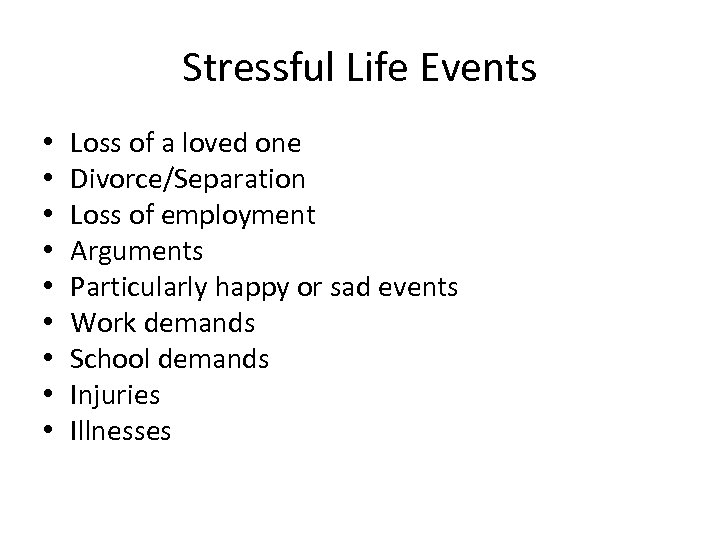 Stressful Life Events • • • Loss of a loved one Divorce/Separation Loss of employment Arguments Particularly happy or sad events Work demands School demands Injuries Illnesses
Stressful Life Events • • • Loss of a loved one Divorce/Separation Loss of employment Arguments Particularly happy or sad events Work demands School demands Injuries Illnesses
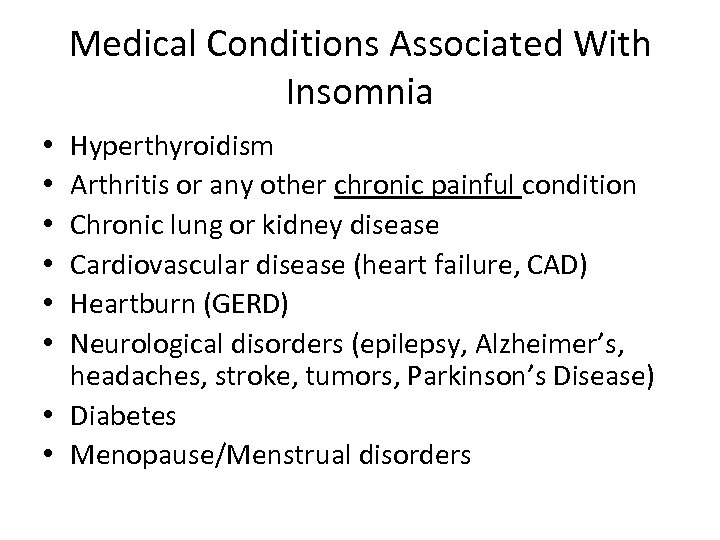 Medical Conditions Associated With Insomnia Hyperthyroidism Arthritis or any other chronic painful condition Chronic lung or kidney disease Cardiovascular disease (heart failure, CAD) Heartburn (GERD) Neurological disorders (epilepsy, Alzheimer’s, headaches, stroke, tumors, Parkinson’s Disease) • Diabetes • Menopause/Menstrual disorders • • •
Medical Conditions Associated With Insomnia Hyperthyroidism Arthritis or any other chronic painful condition Chronic lung or kidney disease Cardiovascular disease (heart failure, CAD) Heartburn (GERD) Neurological disorders (epilepsy, Alzheimer’s, headaches, stroke, tumors, Parkinson’s Disease) • Diabetes • Menopause/Menstrual disorders • • •
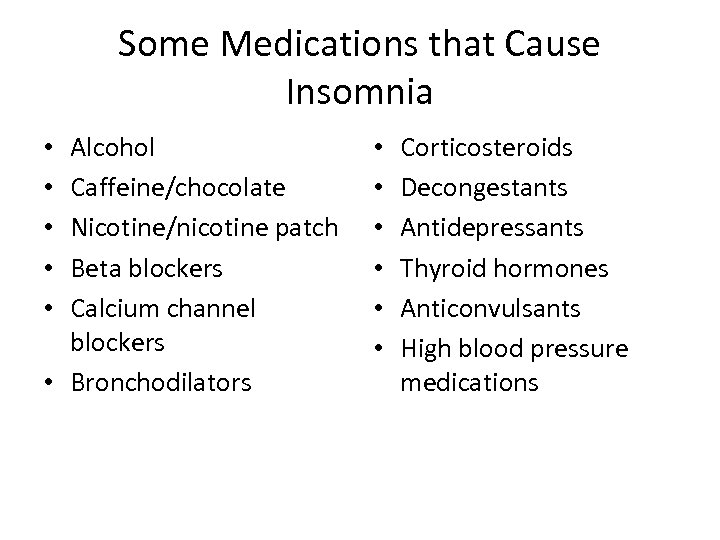 Some Medications that Cause Insomnia Alcohol Caffeine/chocolate Nicotine/nicotine patch Beta blockers Calcium channel blockers • Bronchodilators • • • Corticosteroids Decongestants Antidepressants Thyroid hormones Anticonvulsants High blood pressure medications
Some Medications that Cause Insomnia Alcohol Caffeine/chocolate Nicotine/nicotine patch Beta blockers Calcium channel blockers • Bronchodilators • • • Corticosteroids Decongestants Antidepressants Thyroid hormones Anticonvulsants High blood pressure medications
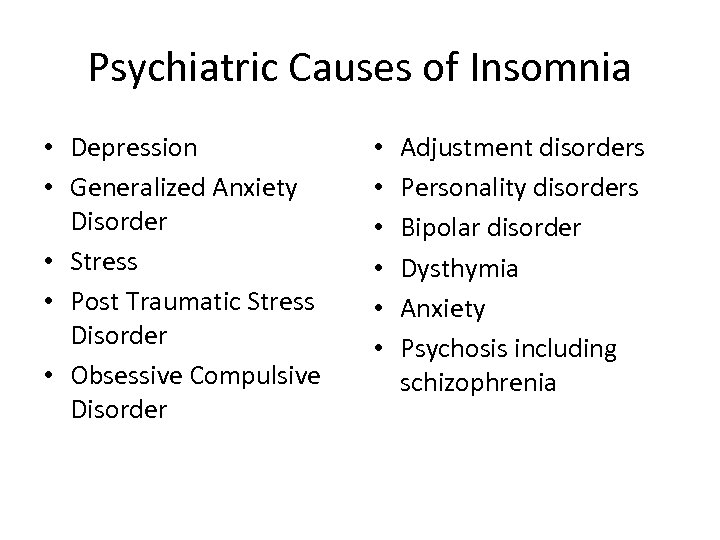 Psychiatric Causes of Insomnia • Depression • Generalized Anxiety Disorder • Stress • Post Traumatic Stress Disorder • Obsessive Compulsive Disorder • • • Adjustment disorders Personality disorders Bipolar disorder Dysthymia Anxiety Psychosis including schizophrenia
Psychiatric Causes of Insomnia • Depression • Generalized Anxiety Disorder • Stress • Post Traumatic Stress Disorder • Obsessive Compulsive Disorder • • • Adjustment disorders Personality disorders Bipolar disorder Dysthymia Anxiety Psychosis including schizophrenia
 Types of Insomnia • Comorbid insomnia – Sleep disturbance is comorbid with an underlying problem
Types of Insomnia • Comorbid insomnia – Sleep disturbance is comorbid with an underlying problem
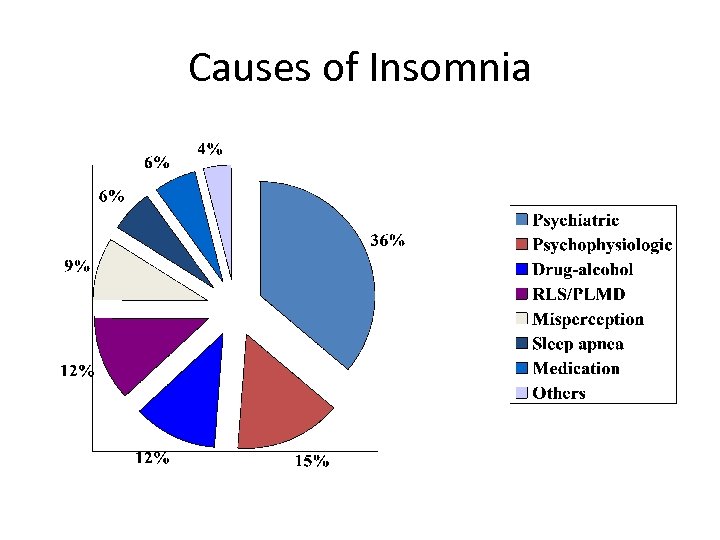 Causes of Insomnia
Causes of Insomnia
 Epidemiology • More than half of adults in the U. S. said they experienced insomnia at least a few nights a week during the past year • Nearly one-third said they had insomnia nearly every night • Increases with age • The most frequent health complaint after pain • Twice as common in women as in men
Epidemiology • More than half of adults in the U. S. said they experienced insomnia at least a few nights a week during the past year • Nearly one-third said they had insomnia nearly every night • Increases with age • The most frequent health complaint after pain • Twice as common in women as in men
 Epidemiology • 69 % have insomnia-occasional 50 % and chronic 19 % • 35 percent insomnia during the previous year (50% serious) • Approximately 10 % of individuals develop chronic insomnia with related daytime consequences
Epidemiology • 69 % have insomnia-occasional 50 % and chronic 19 % • 35 percent insomnia during the previous year (50% serious) • Approximately 10 % of individuals develop chronic insomnia with related daytime consequences
 Insomnia • • • Variables associated with the onset of insomnia include: a previous episode of insomnia a family history of insomnia a predisposition toward being more easily aroused from sleep poorer self-rated health more body pain
Insomnia • • • Variables associated with the onset of insomnia include: a previous episode of insomnia a family history of insomnia a predisposition toward being more easily aroused from sleep poorer self-rated health more body pain
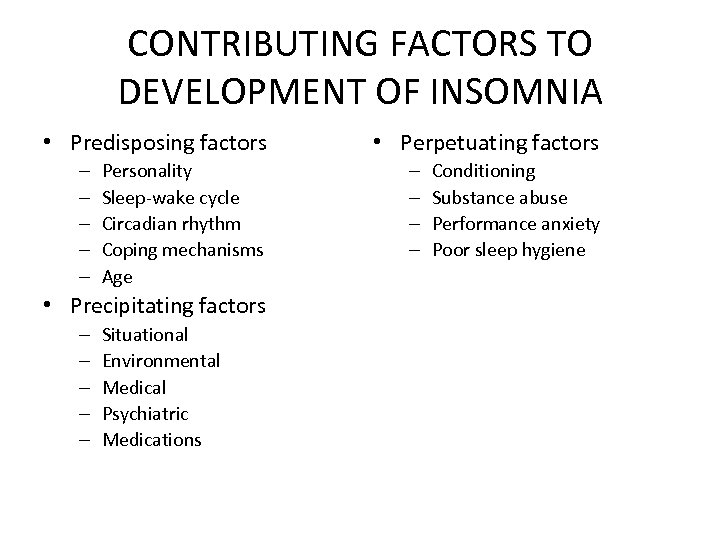 CONTRIBUTING FACTORS TO DEVELOPMENT OF INSOMNIA • Predisposing factors – – – Personality Sleep-wake cycle Circadian rhythm Coping mechanisms Age • Precipitating factors – – – Situational Environmental Medical Psychiatric Medications • Perpetuating factors – – Conditioning Substance abuse Performance anxiety Poor sleep hygiene
CONTRIBUTING FACTORS TO DEVELOPMENT OF INSOMNIA • Predisposing factors – – – Personality Sleep-wake cycle Circadian rhythm Coping mechanisms Age • Precipitating factors – – – Situational Environmental Medical Psychiatric Medications • Perpetuating factors – – Conditioning Substance abuse Performance anxiety Poor sleep hygiene
 Most Common Daytime Complaints • Fatigue or malaise • Poor attention or concentration • Social, school, or vocational dysfunction • Mood disturbance-More sadness, depression, and anxiety • Daytime sleepiness • Cognitive impairment • School or work days missed
Most Common Daytime Complaints • Fatigue or malaise • Poor attention or concentration • Social, school, or vocational dysfunction • Mood disturbance-More sadness, depression, and anxiety • Daytime sleepiness • Cognitive impairment • School or work days missed
 Most Common Daytime Complaints • Reduced motivation or energy • Increased errors or accidents • Tension, headache, or gastrointestinal symptoms • Ongoing worry about sleep • Risk taking behavior • Deficits in academic performance • Poorer Health
Most Common Daytime Complaints • Reduced motivation or energy • Increased errors or accidents • Tension, headache, or gastrointestinal symptoms • Ongoing worry about sleep • Risk taking behavior • Deficits in academic performance • Poorer Health
 Consequences of Insomnia • The National Sleep Foundation found that students who reported insufficient sleep performed worse on tests had lower grades. Those who reported getting enough sleep had A’s and B’s. • Thus students who are chronically sleepy may chose easier courses in college. Thus limiting their future options.
Consequences of Insomnia • The National Sleep Foundation found that students who reported insufficient sleep performed worse on tests had lower grades. Those who reported getting enough sleep had A’s and B’s. • Thus students who are chronically sleepy may chose easier courses in college. Thus limiting their future options.
 Consequences of Insomnia • Even though students may compensate by getting extra sleep on the weekend, this is not enough to compensate for the lost sleep during the week, resulting in a mounting sleep deficit.
Consequences of Insomnia • Even though students may compensate by getting extra sleep on the weekend, this is not enough to compensate for the lost sleep during the week, resulting in a mounting sleep deficit.
 Consequences of Insomnia • • Worsens psychiatric disorders Prolongs medical illnesses Reduced quality of life Higher health care costs
Consequences of Insomnia • • Worsens psychiatric disorders Prolongs medical illnesses Reduced quality of life Higher health care costs
 Depression and Insomnia • Insomnia is both a risk factor for depression and a consequence of depression • Could effective management of insomnia decrease the incidence of depression? • Could effective management of insomnia modify the risk for relapsing depression?
Depression and Insomnia • Insomnia is both a risk factor for depression and a consequence of depression • Could effective management of insomnia decrease the incidence of depression? • Could effective management of insomnia modify the risk for relapsing depression?
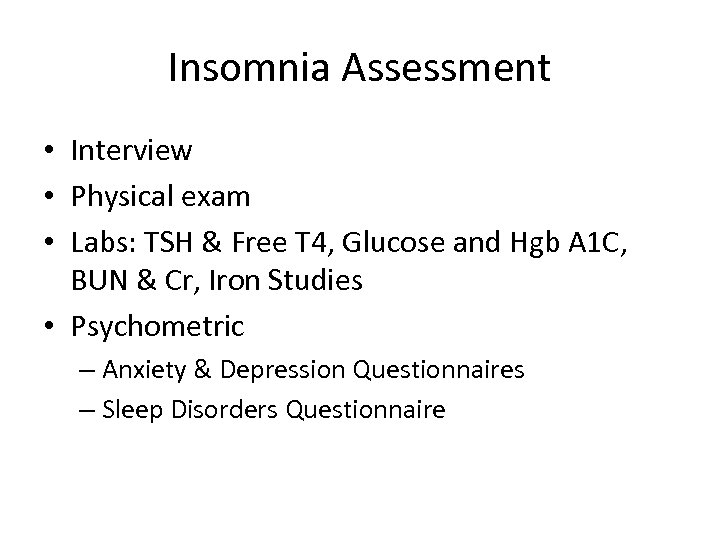 Insomnia Assessment • Interview • Physical exam • Labs: TSH & Free T 4, Glucose and Hgb A 1 C, BUN & Cr, Iron Studies • Psychometric – Anxiety & Depression Questionnaires – Sleep Disorders Questionnaire
Insomnia Assessment • Interview • Physical exam • Labs: TSH & Free T 4, Glucose and Hgb A 1 C, BUN & Cr, Iron Studies • Psychometric – Anxiety & Depression Questionnaires – Sleep Disorders Questionnaire
 Measures of Sleep • Insomnia Severity Index • Epworth Sleepiness Scale (not good for insomnia) • Sleep Diaries • Reports of partner
Measures of Sleep • Insomnia Severity Index • Epworth Sleepiness Scale (not good for insomnia) • Sleep Diaries • Reports of partner
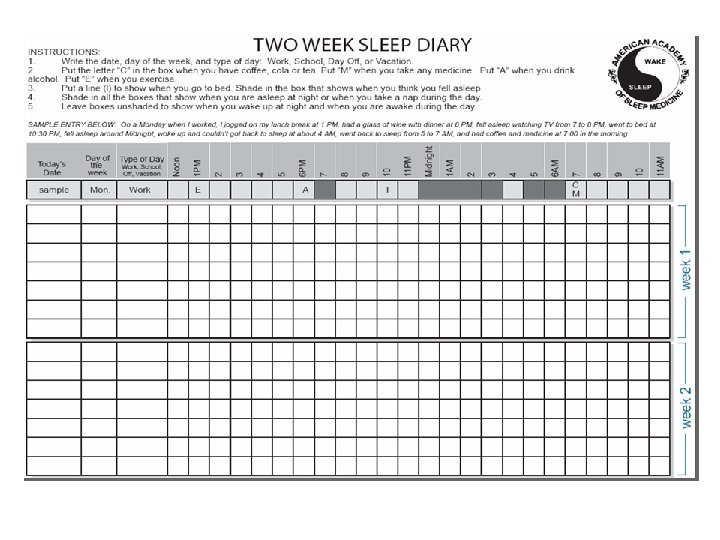
 How to keep track of your sleep • Daily sleep diary or sleep log – Bedtime – Falling asleep time – Nighttime awakenings – Time to get back to sleep – Waking up time – Getting out of bed time – Naps
How to keep track of your sleep • Daily sleep diary or sleep log – Bedtime – Falling asleep time – Nighttime awakenings – Time to get back to sleep – Waking up time – Getting out of bed time – Naps
 Non-drug treatments • Cognitive-behavioral therapy (CBTI) – Stimulus control – Cognitive therapy – Sleep restriction – Relaxation training – Sleep hygiene – Cognitive therapy
Non-drug treatments • Cognitive-behavioral therapy (CBTI) – Stimulus control – Cognitive therapy – Sleep restriction – Relaxation training – Sleep hygiene – Cognitive therapy
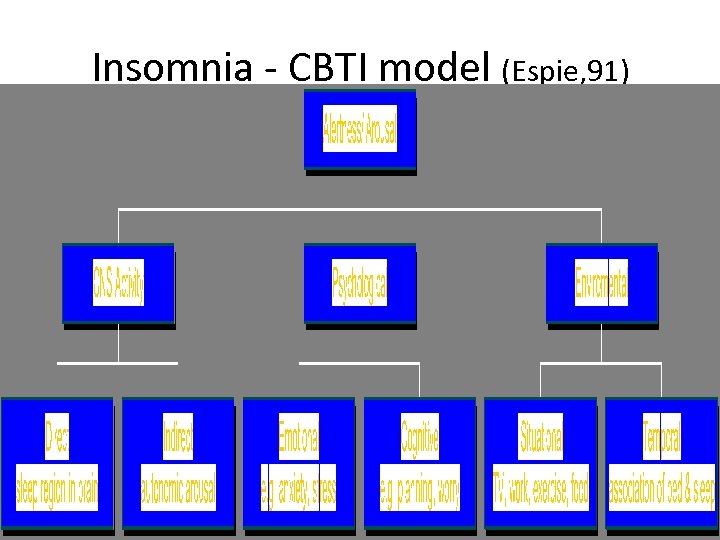 Insomnia - CBTI model (Espie, 91)
Insomnia - CBTI model (Espie, 91)
 CBTI • • Stimulus control Sleep hygiene Sleep restriction Relaxation Paradoxical intention Cognitive restructuring Worry postponement
CBTI • • Stimulus control Sleep hygiene Sleep restriction Relaxation Paradoxical intention Cognitive restructuring Worry postponement
 Insomnia Stimulus Control • Insomnia is a conditioned response to temporal and environmental cues • Promote consistent sleep / wake cycle • Re-associate the bedroom with sleeping • Well established stand alone treatment
Insomnia Stimulus Control • Insomnia is a conditioned response to temporal and environmental cues • Promote consistent sleep / wake cycle • Re-associate the bedroom with sleeping • Well established stand alone treatment
 BEHAVIORAL TREATMENTS • Stimulus control therapy – Assumes that there is a learned associated between wakefulness and the bedroom – To break the cycle, the patient must not spend time wide awake in the bedroom – Go to bed only when sleepy – Do not use the bedroom for sleep-incompatible activities – Leave the bedroom if awake for more than 20 minutes – Return to bed only when sleepy – Repeat if necessary – Do not nap during the day – Arise at the same time every morning
BEHAVIORAL TREATMENTS • Stimulus control therapy – Assumes that there is a learned associated between wakefulness and the bedroom – To break the cycle, the patient must not spend time wide awake in the bedroom – Go to bed only when sleepy – Do not use the bedroom for sleep-incompatible activities – Leave the bedroom if awake for more than 20 minutes – Return to bed only when sleepy – Repeat if necessary – Do not nap during the day – Arise at the same time every morning
 Insomnia Sleep Hygiene Education • Factors that affect sleep, e. g. caffeine, alcohol, etc. • Not primary cause of insomnia but can maintain problem • Limited benefits if used alone, Not sufficient as a stand alone treatment • Specific behaviors will directly interfere with the ability to sleep • The behaviors can be changed with education
Insomnia Sleep Hygiene Education • Factors that affect sleep, e. g. caffeine, alcohol, etc. • Not primary cause of insomnia but can maintain problem • Limited benefits if used alone, Not sufficient as a stand alone treatment • Specific behaviors will directly interfere with the ability to sleep • The behaviors can be changed with education
 Sleep Hygiene • Having good sleep hygiene knowledge is weakly associated with good sleep hygiene but is not related to overall sleep quality. • Practicing good sleep hygiene is strongly related to good sleep quality.
Sleep Hygiene • Having good sleep hygiene knowledge is weakly associated with good sleep hygiene but is not related to overall sleep quality. • Practicing good sleep hygiene is strongly related to good sleep quality.
 Sleep Hygiene Ø Fix a bedtime and an awakening time Ø Avoid napping during the day Ø Avoid alcohol, nicotine, chocolate before bed Ø Avoid caffeine containing beverages 4 – 6 hours before bedtime Ø Avoid heavy, spicy, acidic or sugary foods before bed Ø Regular exercise is good, not before bedtime Ø Comfortable bedding Ø Bedroom cool, dark, quiet Ø Bedroom reserved for sleep and sex – NOT a work room
Sleep Hygiene Ø Fix a bedtime and an awakening time Ø Avoid napping during the day Ø Avoid alcohol, nicotine, chocolate before bed Ø Avoid caffeine containing beverages 4 – 6 hours before bedtime Ø Avoid heavy, spicy, acidic or sugary foods before bed Ø Regular exercise is good, not before bedtime Ø Comfortable bedding Ø Bedroom cool, dark, quiet Ø Bedroom reserved for sleep and sex – NOT a work room
 Sleep Hygiene • Avoid trying to sleep – You can’t make yourself sleep, but you can set the stage for sleep to occur naturally • Avoid a visible bedroom clock with a lighted dial – Don’t let yourself repeatedly check the time! – Turn the clock around or put it under the bed
Sleep Hygiene • Avoid trying to sleep – You can’t make yourself sleep, but you can set the stage for sleep to occur naturally • Avoid a visible bedroom clock with a lighted dial – Don’t let yourself repeatedly check the time! – Turn the clock around or put it under the bed

 More healthy sleep habits • Expose yourself to bright light at the right time – Morning, if you have trouble falling asleep at night – Night, if you want to stay awake longer at night • Establish a regular sleep schedule – Get up at the same time 7 days a week – Go to bed at the same time each night • Exercise every day - exercise improves sleep! • Deal with your worries before bedtime – Plan for the next day before bedtime – Set a worry time earlier in the evening – Keep a journal
More healthy sleep habits • Expose yourself to bright light at the right time – Morning, if you have trouble falling asleep at night – Night, if you want to stay awake longer at night • Establish a regular sleep schedule – Get up at the same time 7 days a week – Go to bed at the same time each night • Exercise every day - exercise improves sleep! • Deal with your worries before bedtime – Plan for the next day before bedtime – Set a worry time earlier in the evening – Keep a journal
 More healthy sleep habits • Adjust the bedroom environment – Sleep is better in a cool room, around 65 F. – Darker is better – If you get up during the night to use the bathroom, use minimum light – Use a white noise machine, a fan, or ear plugs to drown out other sounds – Make sure your bed and pillow are comfortable – If you have a partner who snores, kicks, etc. , you may have to move to another bed (try white noise first) (try ear plugs) – Change resident hall quiet hours
More healthy sleep habits • Adjust the bedroom environment – Sleep is better in a cool room, around 65 F. – Darker is better – If you get up during the night to use the bathroom, use minimum light – Use a white noise machine, a fan, or ear plugs to drown out other sounds – Make sure your bed and pillow are comfortable – If you have a partner who snores, kicks, etc. , you may have to move to another bed (try white noise first) (try ear plugs) – Change resident hall quiet hours
 Healthy Sleep Habits • Boring activities: reading the phone book, count, etc. • TV/video games do not count as relaxing or boring—the flashing lights stimulate the brain.
Healthy Sleep Habits • Boring activities: reading the phone book, count, etc. • TV/video games do not count as relaxing or boring—the flashing lights stimulate the brain.
 Insomnia Sleep Restriction • Reducing time in bed to match sleep obtained • To increase sleep efficiency • Adherence is problematic • Probably efficacious treatment
Insomnia Sleep Restriction • Reducing time in bed to match sleep obtained • To increase sleep efficiency • Adherence is problematic • Probably efficacious treatment
 Sleep Restriction - best if done with a professional • Cut bedtime to the actual amount of time you spend asleep (not in bed), but no less than 4 hours per night • No additional sleep is allowed outside these hours • Record on your daily sleep log the actual amount of sleep obtained
Sleep Restriction - best if done with a professional • Cut bedtime to the actual amount of time you spend asleep (not in bed), but no less than 4 hours per night • No additional sleep is allowed outside these hours • Record on your daily sleep log the actual amount of sleep obtained
 Sleep Restriction (cont’d) • Compute sleep efficiency (total time asleep divided by total time in bed) • Based on average of 5 nights’ sleep efficiency, increase sleep time by 15 minutes if efficiency is >85 -90% • With elderly, increase sleep time if efficiency >80% and allow 30 minute nap.
Sleep Restriction (cont’d) • Compute sleep efficiency (total time asleep divided by total time in bed) • Based on average of 5 nights’ sleep efficiency, increase sleep time by 15 minutes if efficiency is >85 -90% • With elderly, increase sleep time if efficiency >80% and allow 30 minute nap.
 Sleep Restriction • If sleep efficiency falls to less than 80%, decrease time in bed by 15 minutes • Have set, daytime hours (whenever possible). • As sleep consolidation improves, time in bed (and asleep) increases. • Creates a mild state of sleep deprivation, and thus promotes more rapid sleep onset and more efficient sleep
Sleep Restriction • If sleep efficiency falls to less than 80%, decrease time in bed by 15 minutes • Have set, daytime hours (whenever possible). • As sleep consolidation improves, time in bed (and asleep) increases. • Creates a mild state of sleep deprivation, and thus promotes more rapid sleep onset and more efficient sleep
 Insomnia Relaxation • To deactivate arousal system • Various types - muscular, imaging, hypnosis, etc. • Well established treatment
Insomnia Relaxation • To deactivate arousal system • Various types - muscular, imaging, hypnosis, etc. • Well established treatment
 BEHAVIORAL TREATMENTS Plan a relaxation period before bed, develop a bedtime routine. Relaxation Therapy: • Progressive muscle relaxation* best • EMG Biofeedback* best • Meditation • Imagery training • Self-hypnosis • Diaphragmatic breathing
BEHAVIORAL TREATMENTS Plan a relaxation period before bed, develop a bedtime routine. Relaxation Therapy: • Progressive muscle relaxation* best • EMG Biofeedback* best • Meditation • Imagery training • Self-hypnosis • Diaphragmatic breathing
 Relaxation training • More effective than no treatment, but not as effective as sleep restriction • More useful with younger compared with older adults • Engage in any activities that you find relaxing shortly before bed or while in bed – Can include listening to a relaxation tape, soothing music, muscle relaxation exercises, a pleasant image
Relaxation training • More effective than no treatment, but not as effective as sleep restriction • More useful with younger compared with older adults • Engage in any activities that you find relaxing shortly before bed or while in bed – Can include listening to a relaxation tape, soothing music, muscle relaxation exercises, a pleasant image
 Insomnia Paradoxical Intention • Engage in the feared outcome (not sleeping) • Break cycle of performance anxiety • Large variance in response
Insomnia Paradoxical Intention • Engage in the feared outcome (not sleeping) • Break cycle of performance anxiety • Large variance in response
 Paradoxical Intention Treatment • Paradoxical intention treatment is based on the concept that performance anxiety helps prevent proper sleep. • The treatment involves persuading the individual with insomnia to engage in the most feared behavior, which to that individual is "staying awake. " • As the patient stops trying to fall asleep, the performance anxiety of trying to fall asleep slowly disappears. • Studies show this approach is more effective than control groups.
Paradoxical Intention Treatment • Paradoxical intention treatment is based on the concept that performance anxiety helps prevent proper sleep. • The treatment involves persuading the individual with insomnia to engage in the most feared behavior, which to that individual is "staying awake. " • As the patient stops trying to fall asleep, the performance anxiety of trying to fall asleep slowly disappears. • Studies show this approach is more effective than control groups.
 Insomnia Cognitive Restructuring • Identify thought processes to reduce anxiety • Includes self-talk, distraction, rationalization • Helpful in altering dysfunctional sleep beliefs • Postponing worry episodes • Limited benefits if used alone, Not sufficient as a stand alone treatment
Insomnia Cognitive Restructuring • Identify thought processes to reduce anxiety • Includes self-talk, distraction, rationalization • Helpful in altering dysfunctional sleep beliefs • Postponing worry episodes • Limited benefits if used alone, Not sufficient as a stand alone treatment
 Cognitive Restructuring • Identify beliefs about sleep that are incorrect • Challenge their truthfulness • Substitute realistic thoughts
Cognitive Restructuring • Identify beliefs about sleep that are incorrect • Challenge their truthfulness • Substitute realistic thoughts
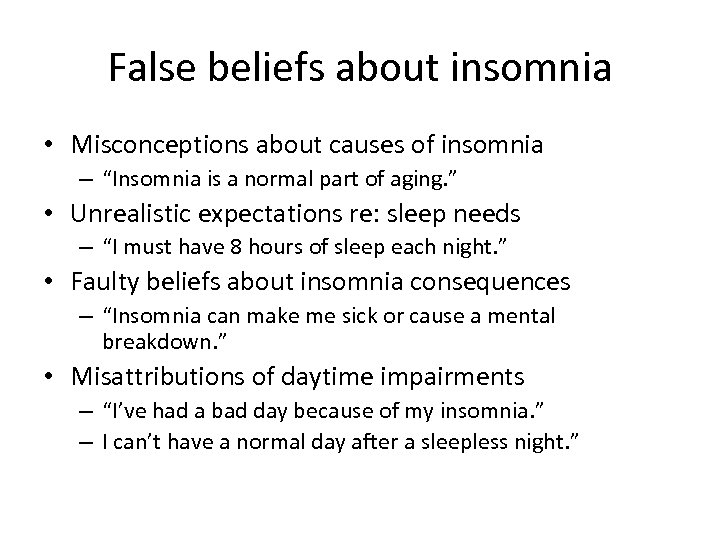 False beliefs about insomnia • Misconceptions about causes of insomnia – “Insomnia is a normal part of aging. ” • Unrealistic expectations re: sleep needs – “I must have 8 hours of sleep each night. ” • Faulty beliefs about insomnia consequences – “Insomnia can make me sick or cause a mental breakdown. ” • Misattributions of daytime impairments – “I’ve had a bad day because of my insomnia. ” – I can’t have a normal day after a sleepless night. ”
False beliefs about insomnia • Misconceptions about causes of insomnia – “Insomnia is a normal part of aging. ” • Unrealistic expectations re: sleep needs – “I must have 8 hours of sleep each night. ” • Faulty beliefs about insomnia consequences – “Insomnia can make me sick or cause a mental breakdown. ” • Misattributions of daytime impairments – “I’ve had a bad day because of my insomnia. ” – I can’t have a normal day after a sleepless night. ”
 More common myths about insomnia • Misconceptions about control and predictability of sleep – “I can’t predict when I’ll sleep well or badly. ” • Myths about what behaviors lead to good sleep – “When I have trouble getting to sleep, I should stay in bed and try harder. ”
More common myths about insomnia • Misconceptions about control and predictability of sleep – “I can’t predict when I’ll sleep well or badly. ” • Myths about what behaviors lead to good sleep – “When I have trouble getting to sleep, I should stay in bed and try harder. ”
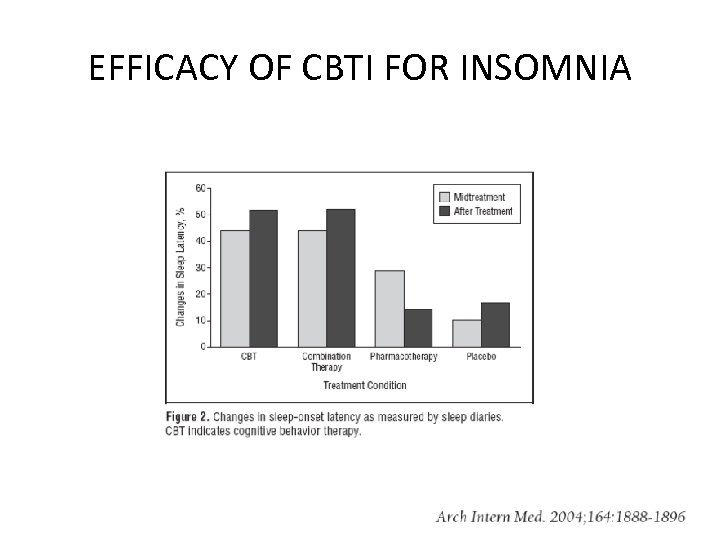 EFFICACY OF CBTI FOR INSOMNIA
EFFICACY OF CBTI FOR INSOMNIA
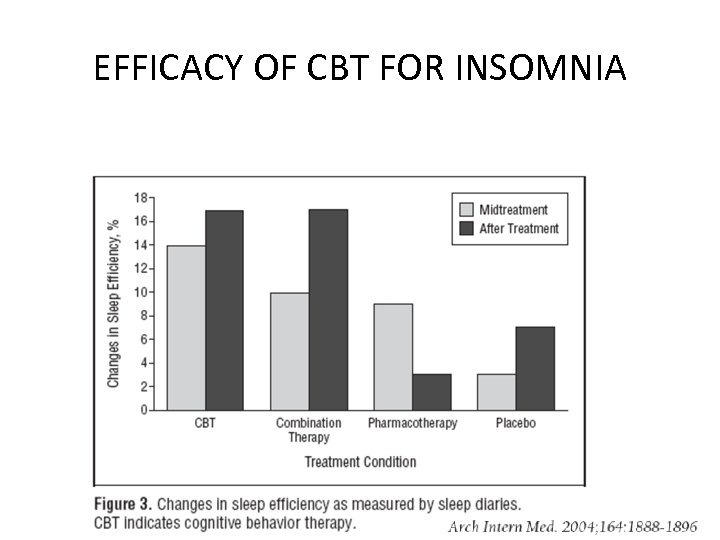 EFFICACY OF CBT FOR INSOMNIA
EFFICACY OF CBT FOR INSOMNIA
 Benefits of CBTI n Benefits are long-lasting, even after therapy is over n Relatively free of medical risks n No significant interactions with other medical treatments
Benefits of CBTI n Benefits are long-lasting, even after therapy is over n Relatively free of medical risks n No significant interactions with other medical treatments
 The Down Side of CBTI n Monetary cost (repeated visits to a provider) n Improvement may not occur for several weeks n Requires time and motivation n Daytime sleepiness during sleep restriction n Lack of access to a trained therapist n Lack of therapist expertise
The Down Side of CBTI n Monetary cost (repeated visits to a provider) n Improvement may not occur for several weeks n Requires time and motivation n Daytime sleepiness during sleep restriction n Lack of access to a trained therapist n Lack of therapist expertise
 Combined Treatment n CBTI can be used along with medications. n For example, medications can provide rapid relief and CBTI can lead to long-lasting results. n The use of medication prior to the initiation of behavioral therapy appears to be less effective.
Combined Treatment n CBTI can be used along with medications. n For example, medications can provide rapid relief and CBTI can lead to long-lasting results. n The use of medication prior to the initiation of behavioral therapy appears to be less effective.
 Treatment of Insomnia Pharmacologic: • Sleeping Pills-Prescription • Over the Counter
Treatment of Insomnia Pharmacologic: • Sleeping Pills-Prescription • Over the Counter
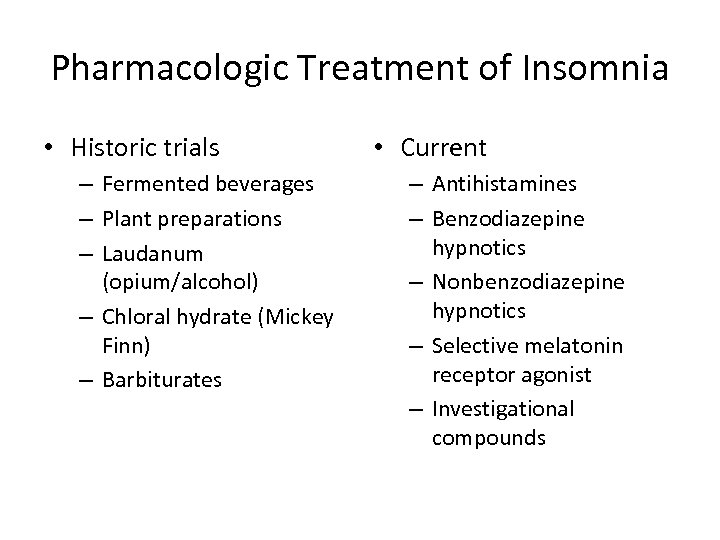 Pharmacologic Treatment of Insomnia • Historic trials – Fermented beverages – Plant preparations – Laudanum (opium/alcohol) – Chloral hydrate (Mickey Finn) – Barbiturates • Current – Antihistamines – Benzodiazepine hypnotics – Nonbenzodiazepine hypnotics – Selective melatonin receptor agonist – Investigational compounds
Pharmacologic Treatment of Insomnia • Historic trials – Fermented beverages – Plant preparations – Laudanum (opium/alcohol) – Chloral hydrate (Mickey Finn) – Barbiturates • Current – Antihistamines – Benzodiazepine hypnotics – Nonbenzodiazepine hypnotics – Selective melatonin receptor agonist – Investigational compounds
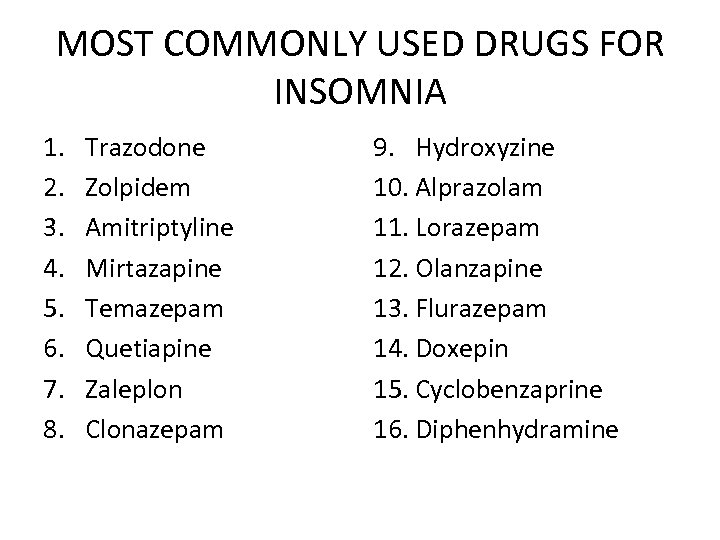 MOST COMMONLY USED DRUGS FOR INSOMNIA 1. 2. 3. 4. 5. 6. 7. 8. Trazodone Zolpidem Amitriptyline Mirtazapine Temazepam Quetiapine Zaleplon Clonazepam 9. Hydroxyzine 10. Alprazolam 11. Lorazepam 12. Olanzapine 13. Flurazepam 14. Doxepin 15. Cyclobenzaprine 16. Diphenhydramine
MOST COMMONLY USED DRUGS FOR INSOMNIA 1. 2. 3. 4. 5. 6. 7. 8. Trazodone Zolpidem Amitriptyline Mirtazapine Temazepam Quetiapine Zaleplon Clonazepam 9. Hydroxyzine 10. Alprazolam 11. Lorazepam 12. Olanzapine 13. Flurazepam 14. Doxepin 15. Cyclobenzaprine 16. Diphenhydramine
 Treatment of Insomnia • • • If you have to use drugs: (Pharmacotherapy Guidelines): Use the lowest therapeutic dose Use for the shortest duration necessary Discontinue medication gradually Be alert for rebound insomnia Use agents with short half-lives to minimize daytime sedation Best if started with CBTI
Treatment of Insomnia • • • If you have to use drugs: (Pharmacotherapy Guidelines): Use the lowest therapeutic dose Use for the shortest duration necessary Discontinue medication gradually Be alert for rebound insomnia Use agents with short half-lives to minimize daytime sedation Best if started with CBTI
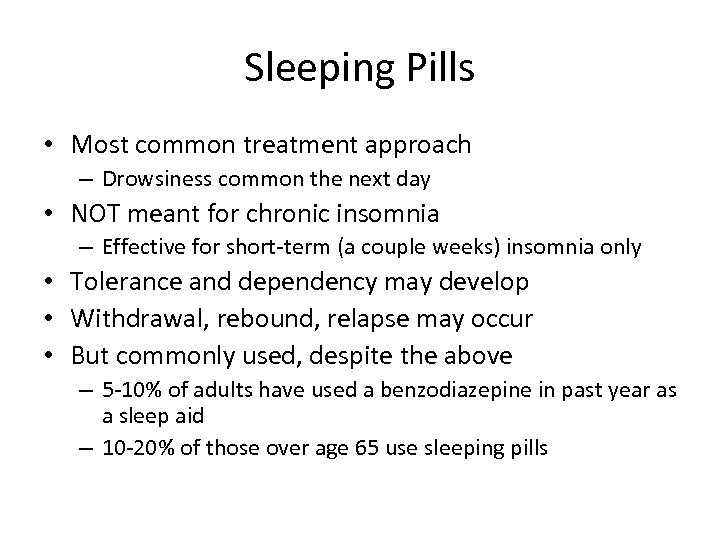 Sleeping Pills • Most common treatment approach – Drowsiness common the next day • NOT meant for chronic insomnia – Effective for short-term (a couple weeks) insomnia only • Tolerance and dependency may develop • Withdrawal, rebound, relapse may occur • But commonly used, despite the above – 5 -10% of adults have used a benzodiazepine in past year as a sleep aid – 10 -20% of those over age 65 use sleeping pills
Sleeping Pills • Most common treatment approach – Drowsiness common the next day • NOT meant for chronic insomnia – Effective for short-term (a couple weeks) insomnia only • Tolerance and dependency may develop • Withdrawal, rebound, relapse may occur • But commonly used, despite the above – 5 -10% of adults have used a benzodiazepine in past year as a sleep aid – 10 -20% of those over age 65 use sleeping pills
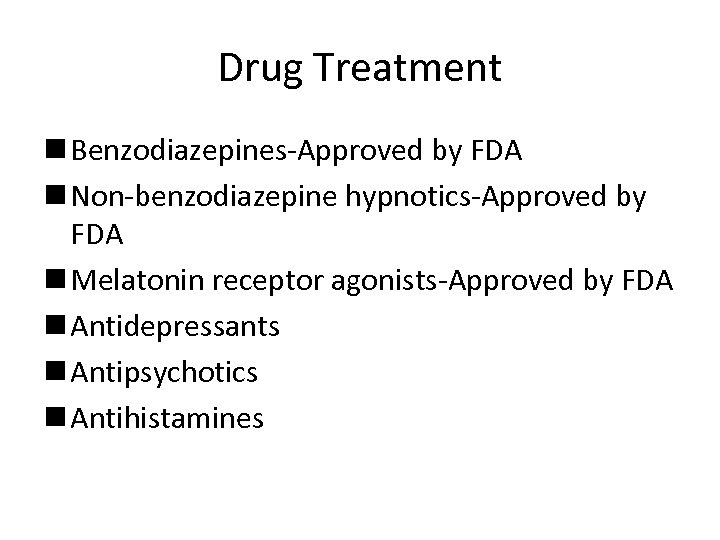 Drug Treatment n Benzodiazepines-Approved by FDA n Non-benzodiazepine hypnotics-Approved by FDA n Melatonin receptor agonists-Approved by FDA n Antidepressants n Antipsychotics n Antihistamines
Drug Treatment n Benzodiazepines-Approved by FDA n Non-benzodiazepine hypnotics-Approved by FDA n Melatonin receptor agonists-Approved by FDA n Antidepressants n Antipsychotics n Antihistamines
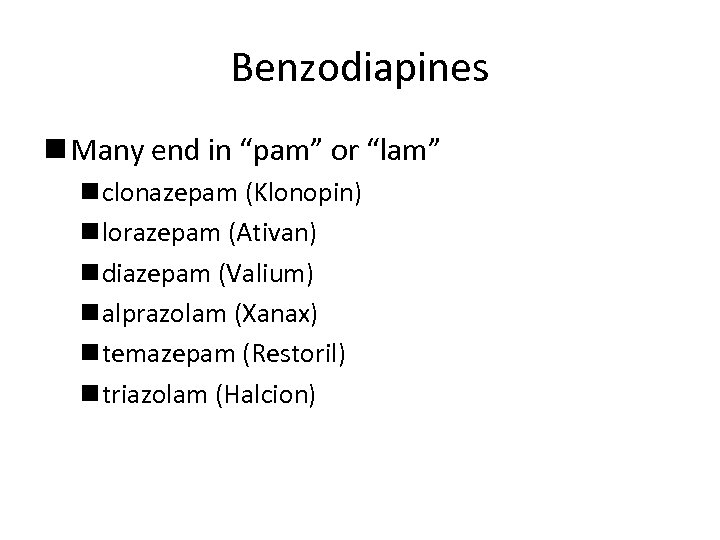 Benzodiapines n Many end in “pam” or “lam” n clonazepam (Klonopin) n lorazepam (Ativan) n diazepam (Valium) n alprazolam (Xanax) n temazepam (Restoril) n triazolam (Halcion)
Benzodiapines n Many end in “pam” or “lam” n clonazepam (Klonopin) n lorazepam (Ativan) n diazepam (Valium) n alprazolam (Xanax) n temazepam (Restoril) n triazolam (Halcion)
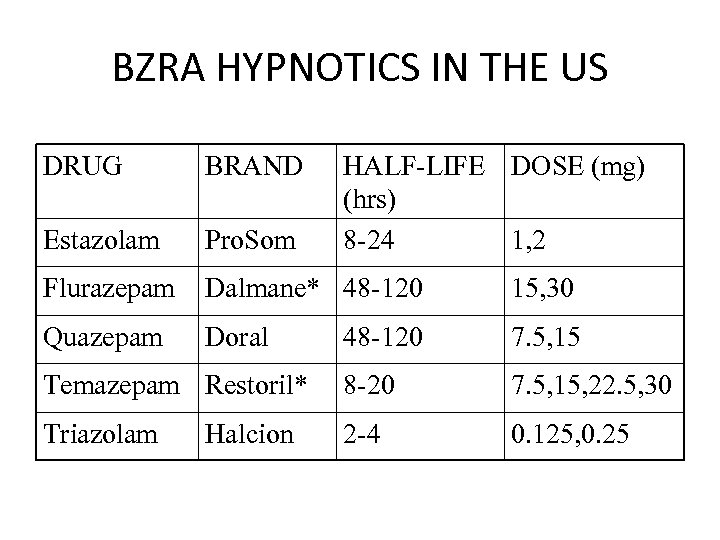 BZRA HYPNOTICS IN THE US DRUG BRAND Estazolam Pro. Som Flurazepam Dalmane* 48 -120 15, 30 Quazepam Doral 48 -120 7. 5, 15 Temazepam Restoril* 8 -20 7. 5, 15, 22. 5, 30 Triazolam 2 -4 0. 125, 0. 25 Halcion HALF-LIFE DOSE (mg) (hrs) 8 -24 1, 2
BZRA HYPNOTICS IN THE US DRUG BRAND Estazolam Pro. Som Flurazepam Dalmane* 48 -120 15, 30 Quazepam Doral 48 -120 7. 5, 15 Temazepam Restoril* 8 -20 7. 5, 15, 22. 5, 30 Triazolam 2 -4 0. 125, 0. 25 Halcion HALF-LIFE DOSE (mg) (hrs) 8 -24 1, 2
 BZRA PRESCRIBING GUIDELINES • • Bedtime dosing Avoid hazardous activities after dose Allow sufficient time in bed Dose adjustments – Elderly and debilitated patients – Hepatic impairment • • Nightly vs. as needed dosing Middle of the night dosing? Taper dose on discontinuation? Do not use in pregnant patients
BZRA PRESCRIBING GUIDELINES • • Bedtime dosing Avoid hazardous activities after dose Allow sufficient time in bed Dose adjustments – Elderly and debilitated patients – Hepatic impairment • • Nightly vs. as needed dosing Middle of the night dosing? Taper dose on discontinuation? Do not use in pregnant patients
 Benefits of Benzodiazepines n Enhance sleep n Decrease anxiety n Muscle relaxant
Benefits of Benzodiazepines n Enhance sleep n Decrease anxiety n Muscle relaxant
 BZRA DISCONTINUATION EFFECTS • Rebound insomnia: sleep worsened relative to baseline for 1 -2 days • Recrudescence: return of original insomnia symptoms • Withdrawal: new cluster of symptoms not present prior to treatment
BZRA DISCONTINUATION EFFECTS • Rebound insomnia: sleep worsened relative to baseline for 1 -2 days • Recrudescence: return of original insomnia symptoms • Withdrawal: new cluster of symptoms not present prior to treatment
 BZRA ADVERSE EFFECTS • • Residual effects Dizziness Headache Blurred vision Nausea/diarrhea Fatigue Anterograde amnesia Sonambulism/complex sleep behavior
BZRA ADVERSE EFFECTS • • Residual effects Dizziness Headache Blurred vision Nausea/diarrhea Fatigue Anterograde amnesia Sonambulism/complex sleep behavior
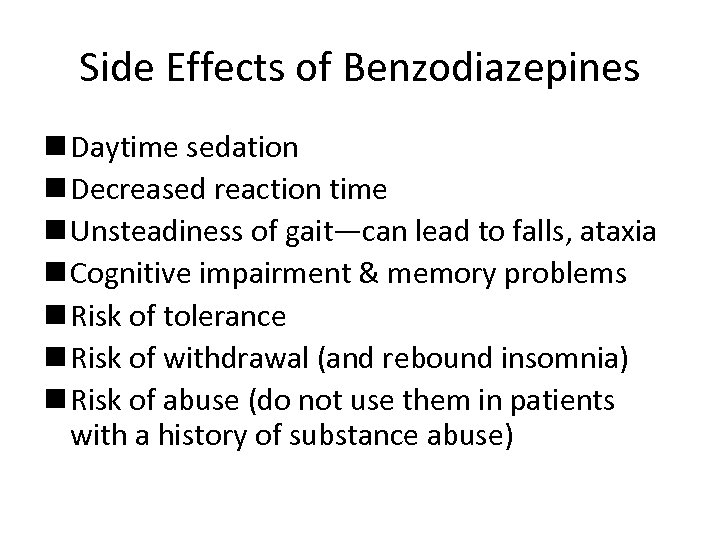 Side Effects of Benzodiazepines n Daytime sedation n Decreased reaction time n Unsteadiness of gait—can lead to falls, ataxia n Cognitive impairment & memory problems n Risk of tolerance n Risk of withdrawal (and rebound insomnia) n Risk of abuse (do not use them in patients with a history of substance abuse)
Side Effects of Benzodiazepines n Daytime sedation n Decreased reaction time n Unsteadiness of gait—can lead to falls, ataxia n Cognitive impairment & memory problems n Risk of tolerance n Risk of withdrawal (and rebound insomnia) n Risk of abuse (do not use them in patients with a history of substance abuse)
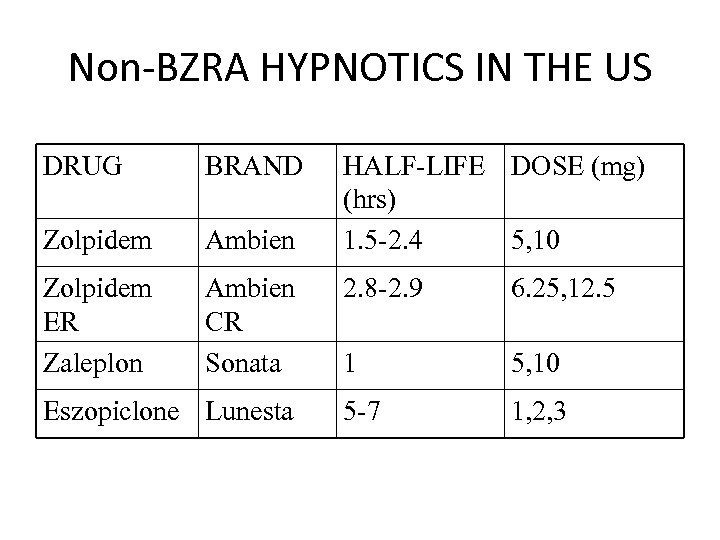 Non-BZRA HYPNOTICS IN THE US DRUG BRAND Zolpidem Ambien Zolpidem ER Zaleplon Ambien CR Sonata Eszopiclone Lunesta HALF-LIFE DOSE (mg) (hrs) 1. 5 -2. 4 5, 10 2. 8 -2. 9 6. 25, 12. 5 1 5, 10 5 -7 1, 2, 3
Non-BZRA HYPNOTICS IN THE US DRUG BRAND Zolpidem Ambien Zolpidem ER Zaleplon Ambien CR Sonata Eszopiclone Lunesta HALF-LIFE DOSE (mg) (hrs) 1. 5 -2. 4 5, 10 2. 8 -2. 9 6. 25, 12. 5 1 5, 10 5 -7 1, 2, 3
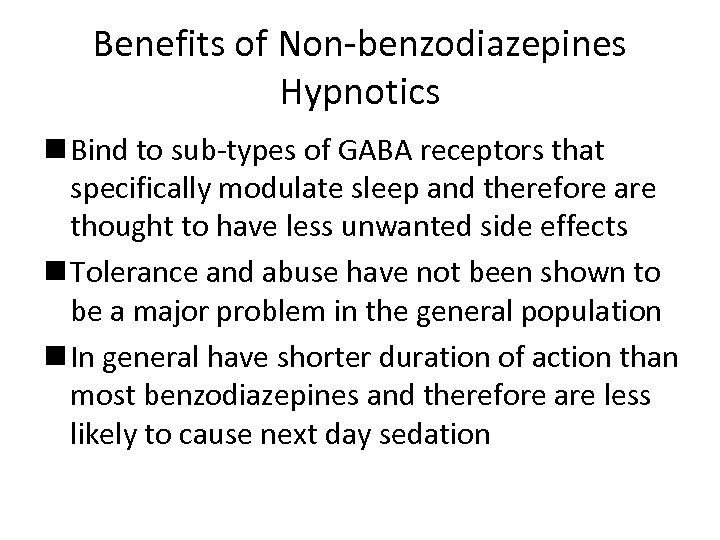 Benefits of Non-benzodiazepines Hypnotics n Bind to sub-types of GABA receptors that specifically modulate sleep and therefore are thought to have less unwanted side effects n Tolerance and abuse have not been shown to be a major problem in the general population n In general have shorter duration of action than most benzodiazepines and therefore are less likely to cause next day sedation
Benefits of Non-benzodiazepines Hypnotics n Bind to sub-types of GABA receptors that specifically modulate sleep and therefore are thought to have less unwanted side effects n Tolerance and abuse have not been shown to be a major problem in the general population n In general have shorter duration of action than most benzodiazepines and therefore are less likely to cause next day sedation
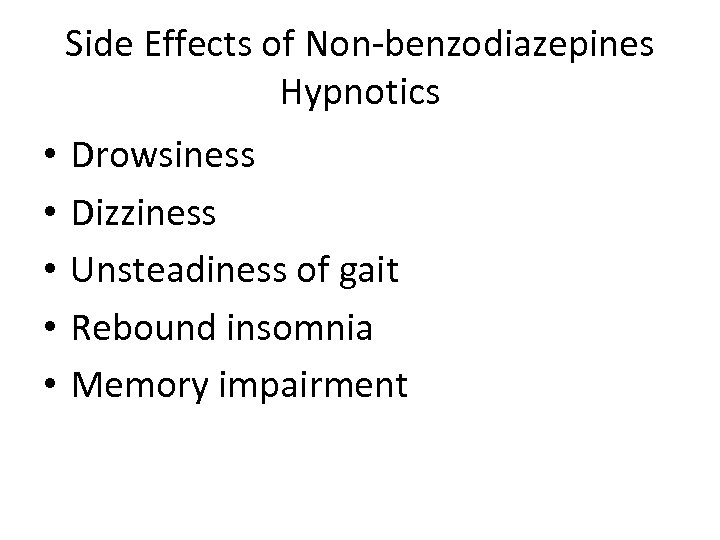 Side Effects of Non-benzodiazepines Hypnotics • • • Drowsiness Dizziness Unsteadiness of gait Rebound insomnia Memory impairment
Side Effects of Non-benzodiazepines Hypnotics • • • Drowsiness Dizziness Unsteadiness of gait Rebound insomnia Memory impairment
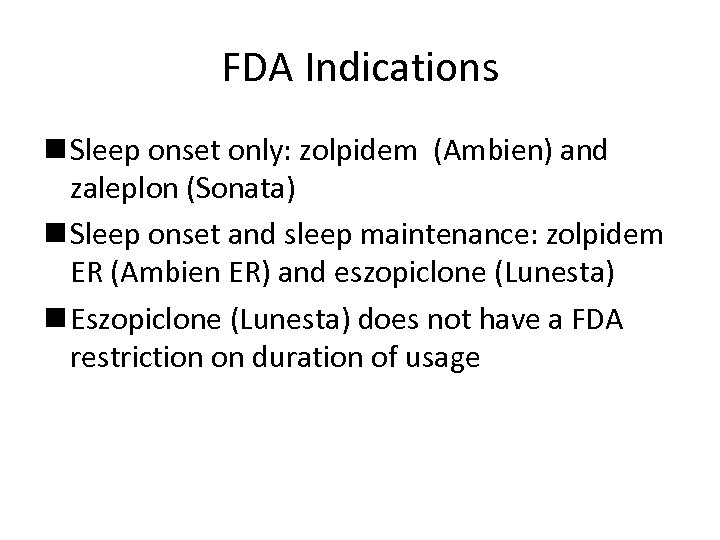 FDA Indications n Sleep onset only: zolpidem (Ambien) and zaleplon (Sonata) n Sleep onset and sleep maintenance: zolpidem ER (Ambien ER) and eszopiclone (Lunesta) n Eszopiclone (Lunesta) does not have a FDA restriction on duration of usage
FDA Indications n Sleep onset only: zolpidem (Ambien) and zaleplon (Sonata) n Sleep onset and sleep maintenance: zolpidem ER (Ambien ER) and eszopiclone (Lunesta) n Eszopiclone (Lunesta) does not have a FDA restriction on duration of usage
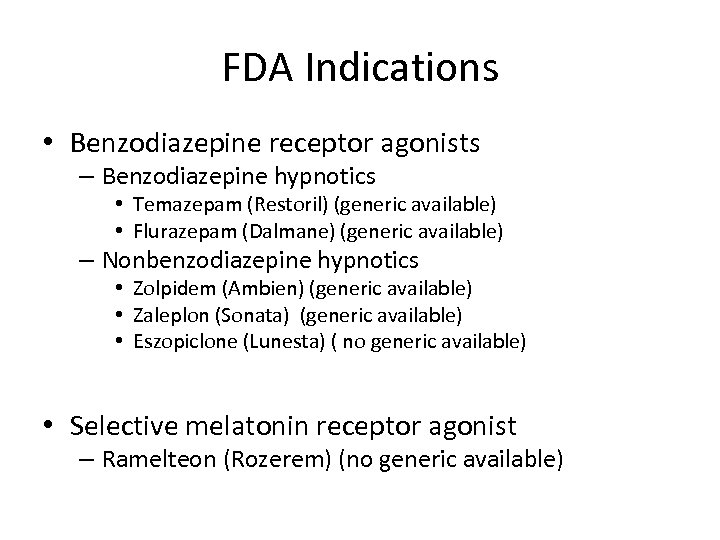 FDA Indications • Benzodiazepine receptor agonists – Benzodiazepine hypnotics • Temazepam (Restoril) (generic available) • Flurazepam (Dalmane) (generic available) – Nonbenzodiazepine hypnotics • Zolpidem (Ambien) (generic available) • Zaleplon (Sonata) (generic available) • Eszopiclone (Lunesta) ( no generic available) • Selective melatonin receptor agonist – Ramelteon (Rozerem) (no generic available)
FDA Indications • Benzodiazepine receptor agonists – Benzodiazepine hypnotics • Temazepam (Restoril) (generic available) • Flurazepam (Dalmane) (generic available) – Nonbenzodiazepine hypnotics • Zolpidem (Ambien) (generic available) • Zaleplon (Sonata) (generic available) • Eszopiclone (Lunesta) ( no generic available) • Selective melatonin receptor agonist – Ramelteon (Rozerem) (no generic available)
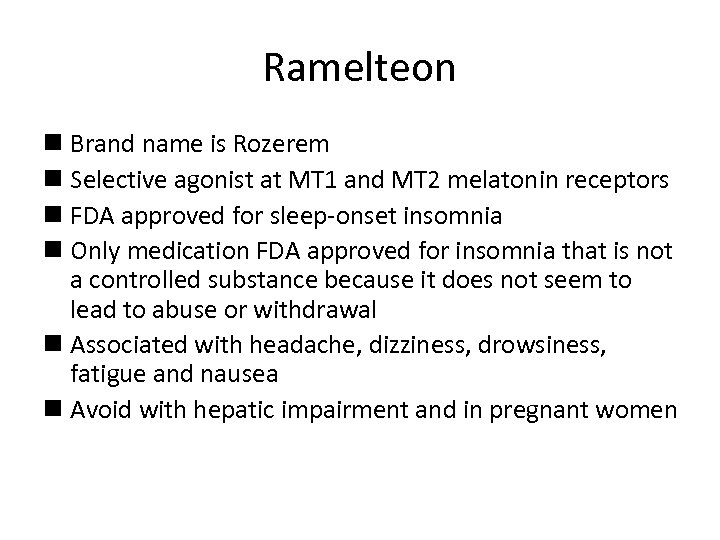 Ramelteon n Brand name is Rozerem n Selective agonist at MT 1 and MT 2 melatonin receptors n FDA approved for sleep-onset insomnia n Only medication FDA approved for insomnia that is not a controlled substance because it does not seem to lead to abuse or withdrawal n Associated with headache, dizziness, drowsiness, fatigue and nausea n Avoid with hepatic impairment and in pregnant women
Ramelteon n Brand name is Rozerem n Selective agonist at MT 1 and MT 2 melatonin receptors n FDA approved for sleep-onset insomnia n Only medication FDA approved for insomnia that is not a controlled substance because it does not seem to lead to abuse or withdrawal n Associated with headache, dizziness, drowsiness, fatigue and nausea n Avoid with hepatic impairment and in pregnant women
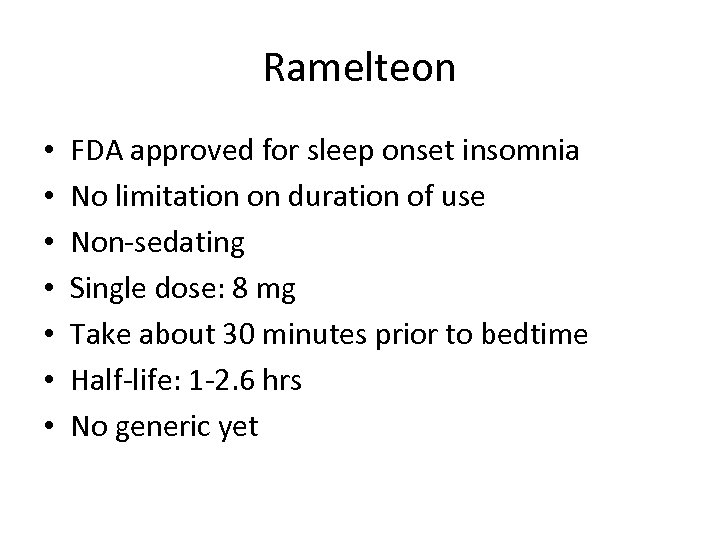 Ramelteon • • FDA approved for sleep onset insomnia No limitation on duration of use Non-sedating Single dose: 8 mg Take about 30 minutes prior to bedtime Half-life: 1 -2. 6 hrs No generic yet
Ramelteon • • FDA approved for sleep onset insomnia No limitation on duration of use Non-sedating Single dose: 8 mg Take about 30 minutes prior to bedtime Half-life: 1 -2. 6 hrs No generic yet
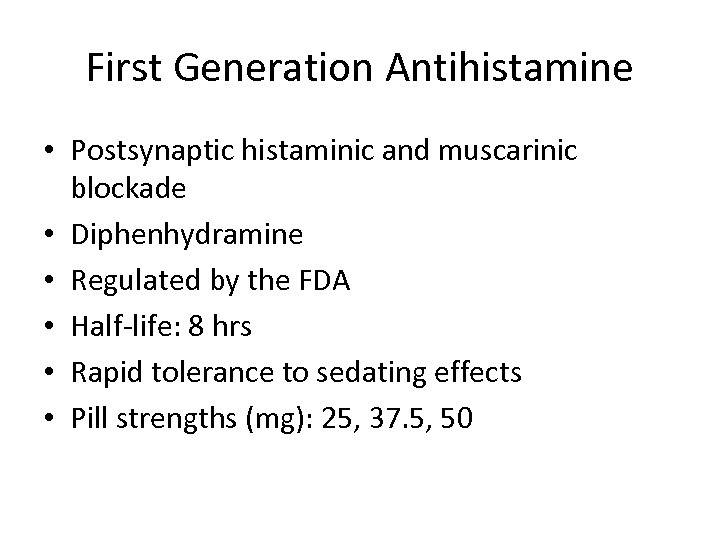 First Generation Antihistamine • Postsynaptic histaminic and muscarinic blockade • Diphenhydramine • Regulated by the FDA • Half-life: 8 hrs • Rapid tolerance to sedating effects • Pill strengths (mg): 25, 37. 5, 50
First Generation Antihistamine • Postsynaptic histaminic and muscarinic blockade • Diphenhydramine • Regulated by the FDA • Half-life: 8 hrs • Rapid tolerance to sedating effects • Pill strengths (mg): 25, 37. 5, 50
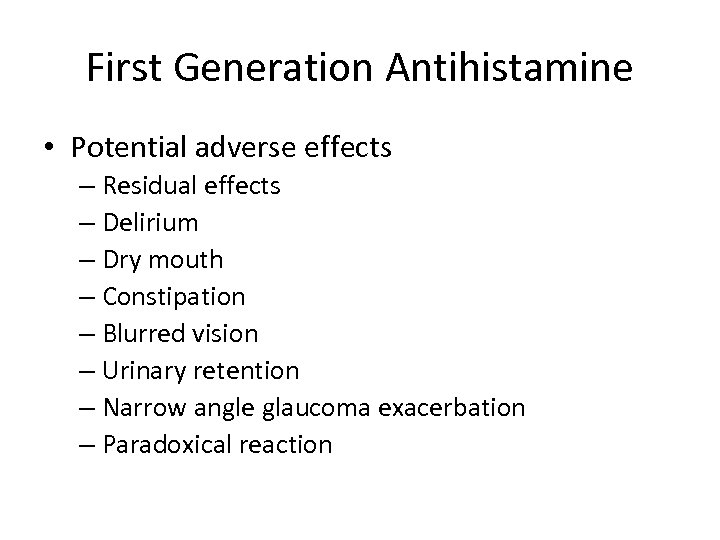 First Generation Antihistamine • Potential adverse effects – Residual effects – Delirium – Dry mouth – Constipation – Blurred vision – Urinary retention – Narrow angle glaucoma exacerbation – Paradoxical reaction
First Generation Antihistamine • Potential adverse effects – Residual effects – Delirium – Dry mouth – Constipation – Blurred vision – Urinary retention – Narrow angle glaucoma exacerbation – Paradoxical reaction
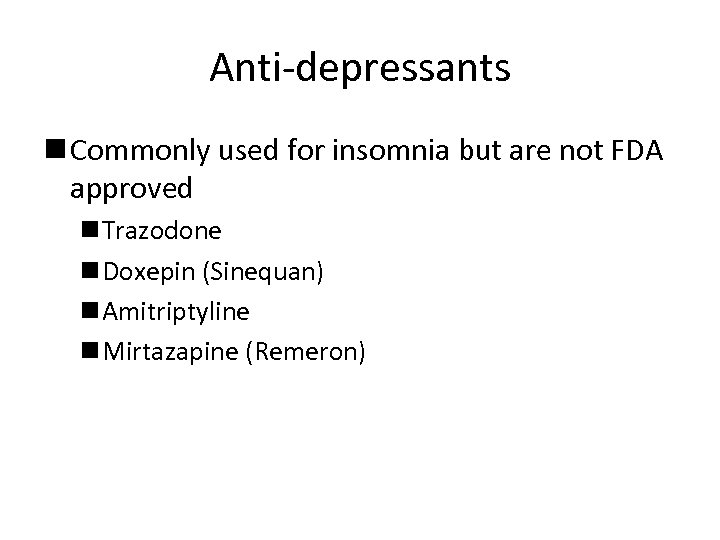 Anti-depressants n Commonly used for insomnia but are not FDA approved n Trazodone n Doxepin (Sinequan) n Amitriptyline n Mirtazapine (Remeron)
Anti-depressants n Commonly used for insomnia but are not FDA approved n Trazodone n Doxepin (Sinequan) n Amitriptyline n Mirtazapine (Remeron)
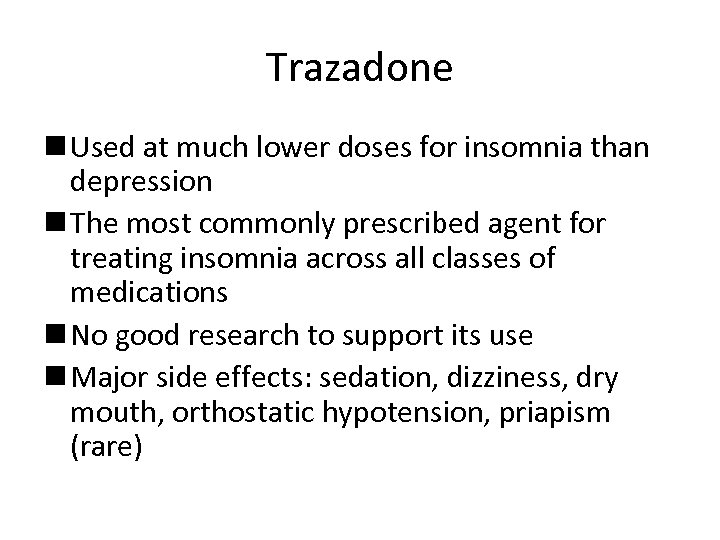 Trazadone n Used at much lower doses for insomnia than depression n The most commonly prescribed agent for treating insomnia across all classes of medications n No good research to support its use n Major side effects: sedation, dizziness, dry mouth, orthostatic hypotension, priapism (rare)
Trazadone n Used at much lower doses for insomnia than depression n The most commonly prescribed agent for treating insomnia across all classes of medications n No good research to support its use n Major side effects: sedation, dizziness, dry mouth, orthostatic hypotension, priapism (rare)
 The Tricyclic Antidepressants n amitriptyline (Elavil) n doxepin (Sinequan) n Side effects: dry mouth, urinary retention, dizziness, daytime sedation, suppression of REM sleep, QT prolongation n Used at much lower doses for insomnia than depression
The Tricyclic Antidepressants n amitriptyline (Elavil) n doxepin (Sinequan) n Side effects: dry mouth, urinary retention, dizziness, daytime sedation, suppression of REM sleep, QT prolongation n Used at much lower doses for insomnia than depression
 Mirtazapine n Brand name: Remeron n Associated with weight gain, increased appetite, daytime sedation and dizziness
Mirtazapine n Brand name: Remeron n Associated with weight gain, increased appetite, daytime sedation and dizziness
 Antipsychotics n Called the “atypical antipsychotics” n Block dopamine from binding to receptors in the brain n Only use is for treating comorbid insomnia in patients with primary indication for their use n Examples: n risperidone (Risperdal) n olanzapine (Zyprexa) n quetiapine (Seroquel) n ziprasidone (Geodon)
Antipsychotics n Called the “atypical antipsychotics” n Block dopamine from binding to receptors in the brain n Only use is for treating comorbid insomnia in patients with primary indication for their use n Examples: n risperidone (Risperdal) n olanzapine (Zyprexa) n quetiapine (Seroquel) n ziprasidone (Geodon)
 Anticonvulsants • Low doses have some sedating and sleep promoting effects • The data is sparse
Anticonvulsants • Low doses have some sedating and sleep promoting effects • The data is sparse
 Dietary Supplements • • Not FDA regulated Valerian Kava-Kava Melatonin Passion flower Skullcap Lavender Hops
Dietary Supplements • • Not FDA regulated Valerian Kava-Kava Melatonin Passion flower Skullcap Lavender Hops
 Dietary/Herbal Sleep Preparations (pea-shooters in the armamentarium) Mostly: L-Tryptophan, Valerian, & Kava-kava • L-Tryptophan: precursor of Serotonin, a substrate for Melatonin – in milk (doesn’t need to be warmed) & turkey – FDA has limited availability after > 1, 500 cases of Eosinophilia Myalgia Syndrome with at least 37 deaths in 1989
Dietary/Herbal Sleep Preparations (pea-shooters in the armamentarium) Mostly: L-Tryptophan, Valerian, & Kava-kava • L-Tryptophan: precursor of Serotonin, a substrate for Melatonin – in milk (doesn’t need to be warmed) & turkey – FDA has limited availability after > 1, 500 cases of Eosinophilia Myalgia Syndrome with at least 37 deaths in 1989
 Dietary/Herbal (continued) • Valerian (derivative of Valeriana officinalis plant): mechanism may be via inhibiting GABA reuptake or inhibiting postsynaptic potentials through activation of adenosine receptors in cortical neurons – in one study, little difference vs. Benadryl* - inhibitor of CYP 3 A 4 – withdrawal when extensive use, similar to that seen with BZD’s – risk of hepatotoxicity & delirium * Sleep, 2005, 28: 1465 -1471
Dietary/Herbal (continued) • Valerian (derivative of Valeriana officinalis plant): mechanism may be via inhibiting GABA reuptake or inhibiting postsynaptic potentials through activation of adenosine receptors in cortical neurons – in one study, little difference vs. Benadryl* - inhibitor of CYP 3 A 4 – withdrawal when extensive use, similar to that seen with BZD’s – risk of hepatotoxicity & delirium * Sleep, 2005, 28: 1465 -1471
 Dietary/Herbal (continued) • Kava-kava: from root of Piper methysticum plant endogenous to Western Pacific, and used as hypnotic & anxiolytic – banned in many countries due to reports of serious hepatoxicity ___________ • Others: Melatonin (OTC), Chamomilla (Sleepy. Time Tea), & Passiflora
Dietary/Herbal (continued) • Kava-kava: from root of Piper methysticum plant endogenous to Western Pacific, and used as hypnotic & anxiolytic – banned in many countries due to reports of serious hepatoxicity ___________ • Others: Melatonin (OTC), Chamomilla (Sleepy. Time Tea), & Passiflora
 Do Not Mix Medications • Heath Ledger had insomnia and passed away from an accidental overdose of the following medications: • oxycodone • hydrocodone • diazepam • temazepam • alprazolam • doxylamine
Do Not Mix Medications • Heath Ledger had insomnia and passed away from an accidental overdose of the following medications: • oxycodone • hydrocodone • diazepam • temazepam • alprazolam • doxylamine
 Other Treatments of Insomnia • Acupuncture
Other Treatments of Insomnia • Acupuncture
 Cultural Issues of Insomnia • How long to sleep at night • How long to nap • Is insomnia to due too much work, physical ailments, etc. • Is insomnia a disease, a complaint, a disorder, a symptom, a finding
Cultural Issues of Insomnia • How long to sleep at night • How long to nap • Is insomnia to due too much work, physical ailments, etc. • Is insomnia a disease, a complaint, a disorder, a symptom, a finding
 Brief Behavioral Treatment Plan for Insomnia • • Initial Visit (1) Screen positive for possible insomnia. (2) Assign sleep log and teach how to complete it on daily basis for 2 weeks. (3) Teach how to calculate a daily sleep efficiency score. Sleep efficiency is calculated by taking the ratio of actual time spent asleep to time spent in bed (expressed as a percentage, with higher numbers indicating better sleep efficiency).
Brief Behavioral Treatment Plan for Insomnia • • Initial Visit (1) Screen positive for possible insomnia. (2) Assign sleep log and teach how to complete it on daily basis for 2 weeks. (3) Teach how to calculate a daily sleep efficiency score. Sleep efficiency is calculated by taking the ratio of actual time spent asleep to time spent in bed (expressed as a percentage, with higher numbers indicating better sleep efficiency).
 Brief Behavioral Treatment Plan for Insomnia • • First Treatment Session (2 weeks later) (1) Review of sleep log, including sleep efficiency score, especially to see the amount of time napping. (2) Discussion of bedtime habits (e. g. , television watching, reading, worrying, etc. ). (3) Brief sleep education consisting of individual differences in sleep needs, the effects of aging on sleep, and the influence of sleep drive and circadian rhythms on sleep. (4) Teach stimulus control techniques including: (a) eliminating nonsleep-related activities from bed and bedroom, (b) following a consistent sleep-wake schedule, and (c) avoiding daytime napping.
Brief Behavioral Treatment Plan for Insomnia • • First Treatment Session (2 weeks later) (1) Review of sleep log, including sleep efficiency score, especially to see the amount of time napping. (2) Discussion of bedtime habits (e. g. , television watching, reading, worrying, etc. ). (3) Brief sleep education consisting of individual differences in sleep needs, the effects of aging on sleep, and the influence of sleep drive and circadian rhythms on sleep. (4) Teach stimulus control techniques including: (a) eliminating nonsleep-related activities from bed and bedroom, (b) following a consistent sleep-wake schedule, and (c) avoiding daytime napping.
 Brief Behavioral Treatment Plan for Insomnia Second Treatment Session (4 weeks after initial visit) • (1) Review of first treatment session instructions. • (2) Problem-solving of any potential treatment adherence problems. • (3) Possible modification of patient's sleep strategy and instructions to encourage future independent trouble-shooting.
Brief Behavioral Treatment Plan for Insomnia Second Treatment Session (4 weeks after initial visit) • (1) Review of first treatment session instructions. • (2) Problem-solving of any potential treatment adherence problems. • (3) Possible modification of patient's sleep strategy and instructions to encourage future independent trouble-shooting.
 Brief Behavioral Treatment Plan for Insomnia • Edinger and Sampson conducted a randomized trial of primary care patients with insomnia. • Their abbreviated behavioral therapy of two 25 -minute sessions was compared with a control group receiving 2 sessions of standard sleep hygiene instructions. • Those in the treatment group had greater improvements in their sleep efficiency and reductions in their time awake after sleep onset than the control group. • This treatment can be successfully done by nonmental health professionals, providers, working in primary care settings.
Brief Behavioral Treatment Plan for Insomnia • Edinger and Sampson conducted a randomized trial of primary care patients with insomnia. • Their abbreviated behavioral therapy of two 25 -minute sessions was compared with a control group receiving 2 sessions of standard sleep hygiene instructions. • Those in the treatment group had greater improvements in their sleep efficiency and reductions in their time awake after sleep onset than the control group. • This treatment can be successfully done by nonmental health professionals, providers, working in primary care settings.
 Take Home Points • In practice parameters for nonpharmacologic treatments for chronic insomnia, the American Academy of Sleep Medicine recommends stimulus control as the approach with the best scientific evidence for effectiveness. • Progressive muscle relaxation, paradoxical intention, and biofeedback are 3 treatments that have the next best scientific evidence for effectiveness, while sleep restriction and multicomponent cognitive behavioral therapy are recommended as options. • Focusing on sleep hygiene and single component cognitive therapy may also be effective, but these approaches do not currently have sufficient scientific evidence to recommend them as evidencebased treatment. This is due to the insufficient number of clinical trials studying the effectiveness of these treatments alone, without their being part of any combined treatment regimen.
Take Home Points • In practice parameters for nonpharmacologic treatments for chronic insomnia, the American Academy of Sleep Medicine recommends stimulus control as the approach with the best scientific evidence for effectiveness. • Progressive muscle relaxation, paradoxical intention, and biofeedback are 3 treatments that have the next best scientific evidence for effectiveness, while sleep restriction and multicomponent cognitive behavioral therapy are recommended as options. • Focusing on sleep hygiene and single component cognitive therapy may also be effective, but these approaches do not currently have sufficient scientific evidence to recommend them as evidencebased treatment. This is due to the insufficient number of clinical trials studying the effectiveness of these treatments alone, without their being part of any combined treatment regimen.
 Take Home Points • In the immediate short term (i. e. , first week), medications can produce improvement at a much greater rate than nonmedication treatments. • In the intermediate term (i. e. , 3 -8 weeks), a meta-analysis indicates that behavioral treatment for insomnia is just as effective as medication treatment.
Take Home Points • In the immediate short term (i. e. , first week), medications can produce improvement at a much greater rate than nonmedication treatments. • In the intermediate term (i. e. , 3 -8 weeks), a meta-analysis indicates that behavioral treatment for insomnia is just as effective as medication treatment.
 Take Home Points • There is the possibility that this effectiveness of behavioral treatment is because it is more intensive than medication treatment in that there is a greater duration of contact with the healthcare professional. • Over the long term (i. e. , 6 -24 months), patients receiving nonpharmacologic therapies enjoy long lasting relief while many of those treated with medication return to their baseline insomnia levels. • In summary, behavioral therapy is best for chronic insomnia and helpful for all types.
Take Home Points • There is the possibility that this effectiveness of behavioral treatment is because it is more intensive than medication treatment in that there is a greater duration of contact with the healthcare professional. • Over the long term (i. e. , 6 -24 months), patients receiving nonpharmacologic therapies enjoy long lasting relief while many of those treated with medication return to their baseline insomnia levels. • In summary, behavioral therapy is best for chronic insomnia and helpful for all types.
 Take Home Points n Insomnia is defined by having daytime symptoms. n There are two pathways for treating insomnia: medications and CBTI. They can be used at the same time. n All treatments have their pluses and their minuses. Provider’s look at the patient’s impairment and weigh that against the risk of treatment.
Take Home Points n Insomnia is defined by having daytime symptoms. n There are two pathways for treating insomnia: medications and CBTI. They can be used at the same time. n All treatments have their pluses and their minuses. Provider’s look at the patient’s impairment and weigh that against the risk of treatment.
 Take Home Points • Patients with insomnia typically feel fatigued during the day, but are unable to fall asleep if given a chance to lie down to take a nap. • Patients with poor nocturnal sleep due to other sleep disorders readily fall asleep during the day.
Take Home Points • Patients with insomnia typically feel fatigued during the day, but are unable to fall asleep if given a chance to lie down to take a nap. • Patients with poor nocturnal sleep due to other sleep disorders readily fall asleep during the day.
 Take Home Points n Many of the most common drugs for insomnia are not FDA approved for that purpose. n No drug for insomnia is completely safe or free of the risk of side effects. n Be sure that your patients informs you of all medications they are taking, including overthe-counter and herbal ones.
Take Home Points n Many of the most common drugs for insomnia are not FDA approved for that purpose. n No drug for insomnia is completely safe or free of the risk of side effects. n Be sure that your patients informs you of all medications they are taking, including overthe-counter and herbal ones.
 Take Home Points • Multidimensional Cognitive Behavioral Therapy works better than both placebo and pharmacotherapy (medicines) in short and long term cases • Interventions for sleep practices may need to be culture specific
Take Home Points • Multidimensional Cognitive Behavioral Therapy works better than both placebo and pharmacotherapy (medicines) in short and long term cases • Interventions for sleep practices may need to be culture specific
 Recommendations • Acknowledge that students sleep habits are significant concerns • Educational programs have been shown to be more effective the pharmacologic and CBTI long term • Examine course schedules, offer sections later in the day • Examine how campus and community environments contribute to sleep difficulties
Recommendations • Acknowledge that students sleep habits are significant concerns • Educational programs have been shown to be more effective the pharmacologic and CBTI long term • Examine course schedules, offer sections later in the day • Examine how campus and community environments contribute to sleep difficulties
 Recommendations • Do activities, schedules, sports, work routines contribute to sleep difficulties • Review life style issues; sleep, etc at all clinic visits
Recommendations • Do activities, schedules, sports, work routines contribute to sleep difficulties • Review life style issues; sleep, etc at all clinic visits


