e25d1ca808b0f3ea8e5a714399e0ce43.ppt
- Количество слайдов: 54

Informed By Consent Presented Associate Professor Catherine Tay National University of Singapore (NUS) Faculty of Business Administration Bachelor of Laws (Hons), London Master of Laws, London Barrister-at-Law (England) Advocate & Solicitor, Singapore Author of ‘Medical Negligence’ Book 1
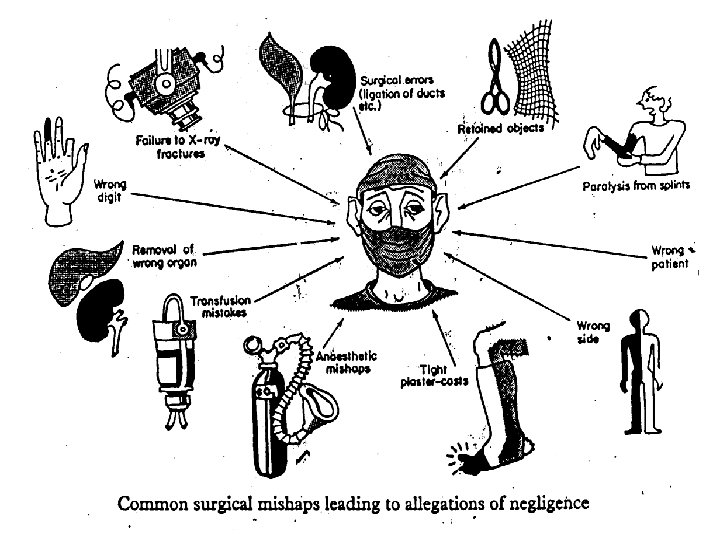
Informed Consent n Things can go wrong in surgical procedure and bad outcome and adverse results may result due to human error, negligent or not. 2
Informed Consent n You did not inform me of the risk which became a reality. I would not have consented to the operation if I had known of the risks, so you have - caused my injury and - failed in your medical duty of care to inform 3
Inforrmed Consent n Is there sufficient information to patient’s consent? 4
Inforrmed Consent n n Consent is an ethical principle Medical treatment can only be performed with consent of competent pt 5
Informed Consent n Giving treatment without consent is failure to respect patient’s autonomy violating an individual’s right of self-determination 6
Informed Consent n Consent must be freely given with patient understanding - the nature - risks - benefits - alternatives - limitations of proposed treatment. 7
Informed Consent n Any medical treatment given without consent is an action for trespass where damages are payable 8
Inforrmed Consent n The consent form is for patient to acknowledge that the nature & purpose of treatment has been - fully explained - understood and - consented to. 9
Informed Consent n Pt never consented to doctor’s negligence but only to risks & complications involved 10
Inforrmed Consent n In an emergency, where pt is unable to consent eg unconsciousness, a doctor is justified to carry out emergency treatment based on - doctrine of necessity or - implied consent 11
Informed Consent n Implied Consent It is presumed that pt would have consented to treatment as it was necessary to save his life or from serious harm 12
Doctor’s Legal Duty to Disclose information n n What is the level or standard of disclosure to be expected in medical law? A pt can only give real consent to treatment if he has sufficient information to make a decision for an informed consent 13
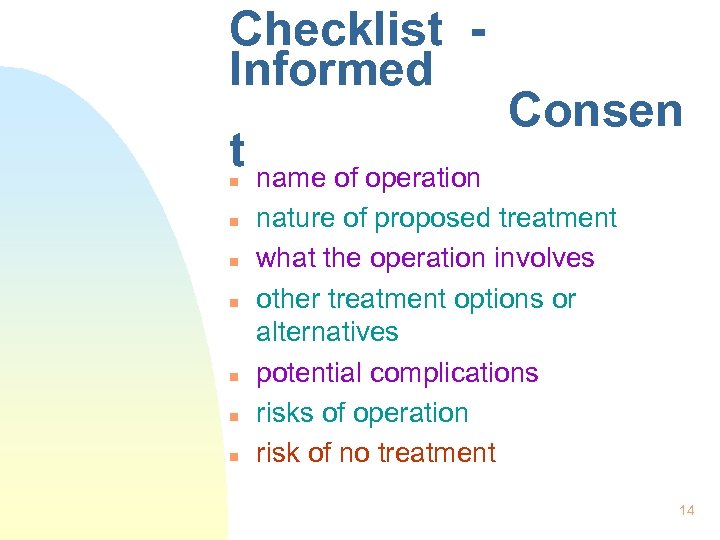
Checklist Informed t name of operation Consen n n n nature of proposed treatment what the operation involves other treatment options or alternatives potential complications risks of operation risk of no treatment 14
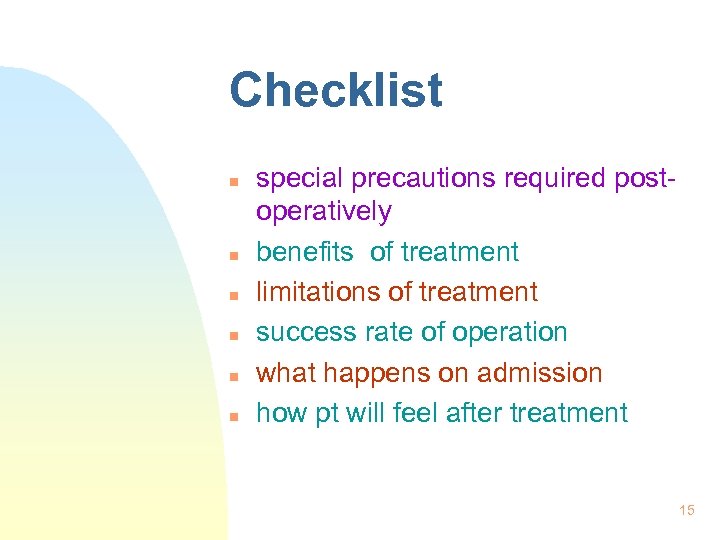
Checklist n n n special precautions required postoperatively benefits of treatment limitations of treatment success rate of operation what happens on admission how pt will feel after treatment 15
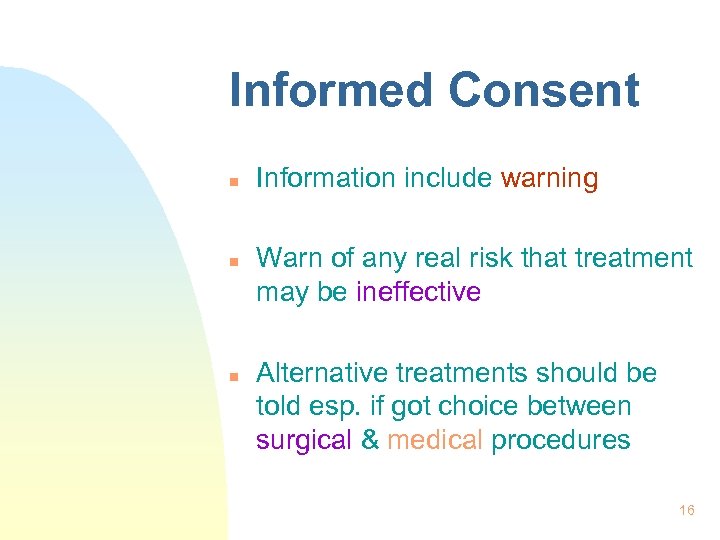
Informed Consent n n n Information include warning Warn of any real risk that treatment may be ineffective Alternative treatments should be told esp. if got choice between surgical & medical procedures 16
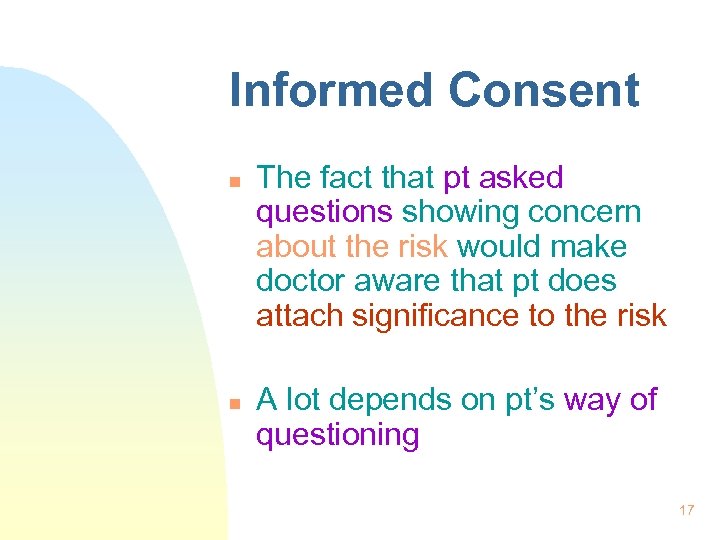
Informed Consent n n The fact that pt asked questions showing concern about the risk would make doctor aware that pt does attach significance to the risk A lot depends on pt’s way of questioning 17
Rogers v Whittaker (1992) n n A 1: 14, 000 of blindness turned into a risk which it was found to be negligent not to disclose A risk, even if it is a mere possibility, should be regarded as ‘material’ if its occurrence causes serious consequences 18
Informed Consent n Once pt ask “How serious? ” the operation is, doctor should discuss - the relative conveniences - expertise - possible risks. 19
Informed Consent n n To say less is misleading & inadequate Good communication is stressed and is highly desirable between doctor-pt relationship 20
Medical Negligence n n Failure by doctor to disclose risks of treatment can result in action for negligence The test which medical negligence is assessed is Bolam test , now modified by Bolitho case 21
Bolitho case n Failure of hospital doctor to examine & intubate child experiencing respiratory distress, leading to brain damage through asphyxia 22
Bolitho case (1997) n Pt had expert evidence that a reasonably competent doctor would have intubated in those circumstance - Doctor had own expert witnesses saying that non-intubation was clinically justifiable response 23
Bolam Test n A doctor is not negligent if what he has done is accepted current practice by a responsible body of medical opinion 24
Bolitho case n n n House of Lords case The court must be satisfied that the body of opinion is logical Clearly this rejection of Bolam test 25
Bolitho case n n It is now a matter for court & not medical opinion to decide standard of professional care Bolitho case represented a significant nail on Bolam’s coffin 26
Kamalam v Eastern Planttaion Agency (1996) n n Malaysian case – where Bolam test not folllowed A Malaysian judge can now decide on his own disregarding expert medical evidence on the sufficiency of consent – informed consent 27
Informed Consent n n Medical opinions are still required to assist the court in its deliberation Bolam test has been challenged & rejected in America, Canada, Australia, South Africa & Malaysia 28
Singapore cases n n n Dennis Matthew Harte v Dr Tan Hun Hoe & Gleneagles Hospital Ltd [1999] Gumapathy Muniandy v Dr James Khoo & 2 others – July 2001 Pai Lily v Yeo Peng Hock Henry [2000] 29
Informed Consent n Highly desirable for doctor to record in his medical notes that - risks and alternatives were disclosed & - understood by pts, apart from pt signing consent form 30
Medical Ethics n It is no harm to disclose all ‘material risks’ & information to pts as they have a right to do what they want with their own bodies 31
Medical Ethics n n Pts could choose to do nothing after being informed of options/alternatives& consequences of no treatment This is respecting pt’s autonomy or self-determination in biomedical ethics 32
Medical Ethics n n Doctors must abide by the high professional standards Hippocratic Oath is a moral code concerning beneficence & nonmaleficence ie. the pillars of medical ethics – do good, do no harm 33
Medical Ethics n n Declaration of Geneva Singapore Physician Pledge 34
Principles of Biomedical Ethics 1. Autonomy - decision-making - respect for individuals - patient’s rights 2. Beneficence Do Good 35
Medical Ethics 3. Non-Maleficence Do No Harm 4. Justice equitable distribution of benefits & burdens 36

Medical Ethics 5. Fidelity - truth-telling - confidentiality 6. Veracity - honesty 37
Medical Ethics n n n Medical ethics must lead medical law A good medical law is an ethical law Doctor must practice sound medical ethics 38
Complaints & Complaints n n Doctors who fail to establish relationship with patients will endanger trust & confidence Doctor who takes time to explain what and why he propose to do & how much it cost are less likely to be subject of complaints 39
Proving Medical Negligence 1. Duty of Care 2. Standard of Medical Care 3. Causation 4. Remoteness (ie suffer damage) 40
NEGLIGENCE n n n Is failure to exercise reasonable care and skill, or Omission to do something which a reasonable man would do, or Something which a reasonable man would not do 41
Negligence n n Careful doctor but still negligent Things can go wrong – 1. Diagnosis 2. Treatment 3. Information Disclosure 42
Standard of Medical Care n n n Careful doctor but still Negligent Keeping abreast with latest developments and technology & incorporate them in his practice Not expected to read every article in medical journals 43
n n n Doctor judged by standard or awareness and sophistication to be expected of a doctor in his sort of profession All doctors not expected to have level of awareness available to a professor To be judged on what is to be expected of doctor/dentist in regular practice 44
n n n If GP fail to refer patient to consultant when reasonable GP would, GP is negligent No allowance made for inexperience and age 60 year old GP in private practice, must meet same standard of alertness as 30 year GP 45
n n Medical Negligence is a Civil Wrong TORT Tort = Wrongful Act 46
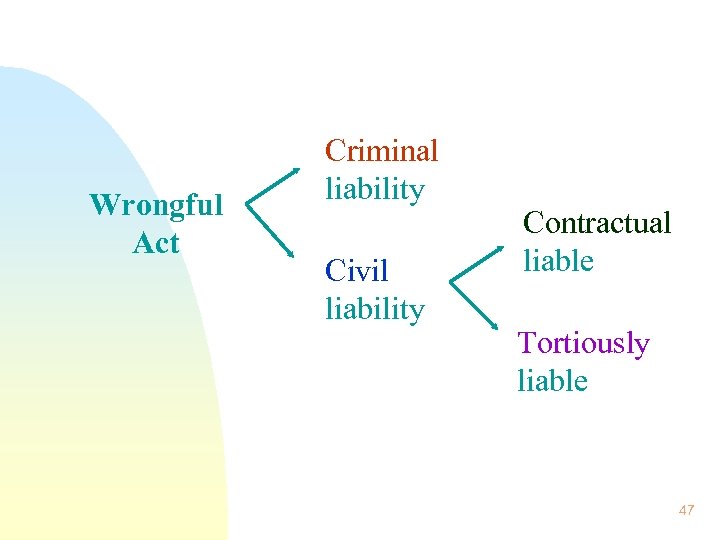
Wrongful Act Criminal liability Civil liability Contractual liable Tortiously liable 47
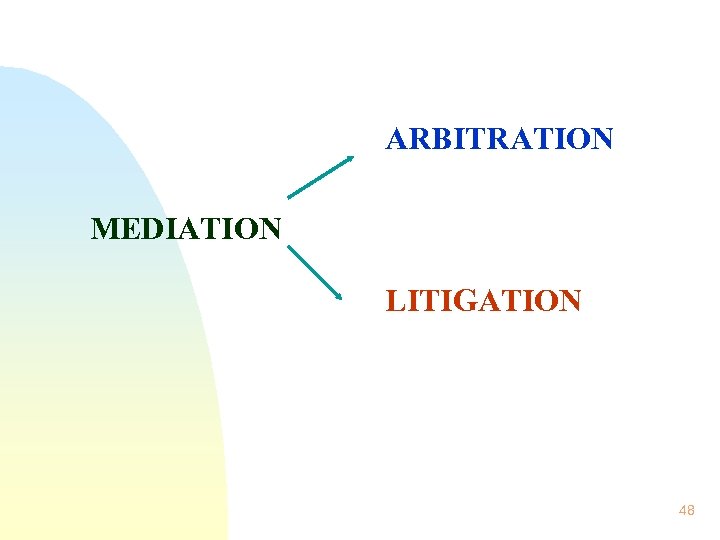
ARBITRATION MEDIATION LITIGATION 48
49

Medical errors As to errors of clinical judgement the House of Lords in an important medical negligence case of Whitehouse V Jordan (1981) had this to say: “… Merely to describe something as an error of judgement tells nothing about whether it is negligent or not. The true position is that an error of judgement may, or may not, be negligent; it depends on the nature of the error. If it is one that would not have been made by a reasonably competent professional man professing to have the standard and type of skill that the defendant held himself out as having, and acting with ordinary care, then it is negligent. If, on the other hand, it is an error that such a man, acting with ordinary care, might have made, then it is not negligent. ” 52
n Penal Code section 93 - recognises that patient got right to know, even if communication may cause death by shock 53
END OF SEMINAR THANK YOU Associate Professor Catherine Tay National University of Singapore Dept of Business Policy Email: fbatayc @ leonis. nus. edu. sg Website : www. catherinetay. com. sg Tel : 4695704 or 96951656 54
e25d1ca808b0f3ea8e5a714399e0ce43.ppt