dd3814d1bcec594cb298d34a3f896e2a.ppt
- Количество слайдов: 48
INFLAMMATION, INFECTION AND IMMUNITY
Objectives • Describe how inflammatory changes act as bodily defense mechanisms • Identify signs and symptoms of inflammation • Discuss the process of repair and healing • Discuss the actions of commonly found infectious agents • Compare community acquired and health care associated infections
Objectives • Describe the centers of disease control isolation guidelines for – Airborne – Droplet – Contact – Transmission based precautions
Objectives • Discuss the nursing care of patients with infections • Describe the CDC standard precautions guidelines for infection control • Describe the immune response • Describe the nursing care of patients with HIV and those with allergies • Describe the process of autoimmunity
INFLAMMATORY CHANGES HOW DO THEY PROTECT THE BODY? Series of bodily actions that defend the body: 1. Hemodynamic: a. Capillary bed dilation b. Increased blood flow to the area (WBC’s) c. Evidence: - Warmth (calor) Redness (Rubor)
Inflammatory Changes 2. Increased Permeability: a. pavementing: - WBC’s line small blood vessel walls - passing thru the walls and invade area - Europhiles, monocytes - phagocytosis b. protein rich fluid: - also permeates thru the walls - leads to swelling/pain (tumor/dolor)
Inflammatory Changes 3. Chemical Mediators found in body tissues and : cause the hemodynamic changes and vascular permeability: a. cytokines and eicosanoids - bradykinin – blood vessel dilation - blood vessel permeability - pain and s/s of inflammation
Inflammatory Changes 3. Chemical Mediators: cause the hemodynamic changes and vascular permeability: b. complement system: - immunological reactions - involving antigen-antibody reactions - leads to a massive release of histamine - leads to the S/S of anaphylactic shock:
Inflammatory Changes The S/S of anaphylactic shock: 1. Massive vasodilation 2. Vascular permeability 3. Smooth muscle contraction Leads to signs and symptoms of anaphylaxis: - hypotension - swelling - bronchoconstriction
Inflammatory Changes 4. anti-inflammation: a. release of cortisol: - hormone produced by the adrenals - slows release of histamine, - stabilizes lysosomal membranes - prevents the influx of leukocytes b. slows down or stops the inflammatory process c. protects the body from excess inflammation patients with chronic or inborn inflammatory diseases - benefit from corticosteroid injections
Identifying S/s of inflammation 1. Local S/s of inflammation: a. Heat b. Swelling c. Redness d. Pain - Leading to loss of function
Identifying S/s of inflammation Systemic S/s of inflammation: 1. Fever related to; a. b. c. d. e. Pyrogens Phagocytosis Bacterial endotoxins Antigen-antibody complexes Certain viruses
Identifying S/s of inflammation Systemic S/s of inflammation: 2. Other S/s’s: a. headaches b. muscle aches c. chills d. sweating e. leukocytosis : - seen without an infxn - related to inflammation only - disappears within hours

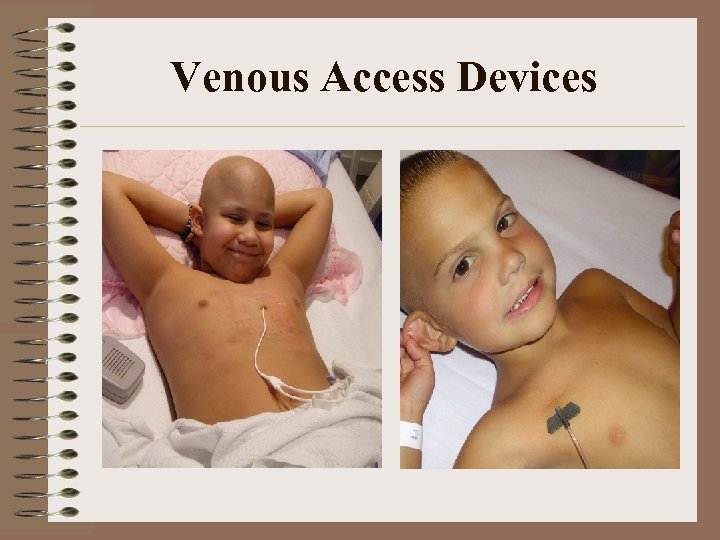
Venous Access Devices
Wound Healing 1. Starts from the onset of inflammation: 2. Speed of healing: - Depends on the type of tissue, and health 3. Macrophages: - Clean up inflammatory debris 4. Fibroblasts: a. Lay down elastin and collagen at Wd edges b. Gradually migrate to the base of the Wd c. Forms granulation tissue
Wound Healing 5. Epithelial cells: - migrate over the wound and form a scab 6. Regeneration: - scab falls off - damaged cells are replaced by new cells - AKA – regeneration - some tissue does not regenerate well - leads to scar formation
Wound Healing Age and general health: - affect speed of tissue regeneration - delayed in older person due to: * decreased tissue elasticity * decreased blood supply Nutritional deficiencies: - regeneration may also be impaired by - vitamin – C, Zinc, other minerals deficiencies
Wound Healing Infection and or ulceration of a wound: - May lead to tissue loss - Granulation tissue forms around Wd - It may eventually fill the wd if it is small - If the Wd is large: • • • The wound is cleaned and debridement is used It helps regeneration and healing Wet to dry dressings are used
Wound Healing Primary intention: - clean wound that is sutured - heals from outside in Secondary intention : - infected wound - allowed to heal from inside out Delayed primary closure: - a sutured wound that was once infected
Actions of infectious agents • Bacteria: • One celled, Multiplies rapidly within the infected person • Classified by: – shape: • Round (cocci) – – classified how they group together Diplococi (groups o two) Clusters ( staphylococci) Chains ( streptococci)
Actions of infectious agents • Bacteria: – shape • Rod shaped – Bacilli further subdivided into » Fusiform » Spirochetes – whether they require oxygen to survive: • Aerobes • Anaerobes – ability to take up and or retain stains.
Actions of infectious agents • Bacteria: – ability to take up and or retain stains: • Gram positive: – Have a thick covering that retains the stain • Gram negative: – Have a thin wall and do not retain the stain • Acid fast stain: – Used to detect mycobacterium tuberculosis • Immunoflourescent stains: – Reveal different organisms and antibodies when exposed to ultraviolet light • Each classification gives the details of how to kill it or its design (via O 2 or cell wall )
Actions of infectious agents • Viruses: – Visible thru the electron microscope – May be RNA or DNA viruses – Have a protein capsule but no cell wall – Replication is dependent on a host – Live within the host’s cells (killing them is hard) – DNA viruses Cause: • Colds, measles, chickenpox, hepatitis – RNA viruses cause: • HIV • Few antivirals meds (prevention is KEY)
Actions of infectious agents • Fungi: – Vegetable-like organisms – Feed on organic matter – Few produce diseases in humans • • • Tinea corporis (ring worm) Tinea pedis (athletes foot) Tinea capitis ( scalp fungal infection) Tinea cruris (jock itch) crural fold) Majocchi’s Granuloma: (epidermal fungal infxn) – Many are superficial skin infections
Actions of infectious agents • Fungi: (cont’d) – Fungal infections may be life threatening i. e. : • Cryptococcus • Aspergillus – Immunocompromised individuals • Chemo • HIV • Transplant patients – Fungal infections “ • Called mycoses • Spore forming (resistant to antiseptics/disinfectants) – Pts, may be treated with topical & systemic antimycotics
Actions of Infectious Agents • Protozoa: – Once celled organism – Plamsodium species produces disease in humans • • Malaria Amoebic dysentery Giardiasis Trypanosoma gambiense (sleeping sickness) – Spread by fecal contamination of food or water
Actions of Infectious Agents • Protozoa: (Cont’d) – Pneumocystis jiroveci: • Common in patients with HIV • Low immunity leads to pneumocystic pneumonia
Actions of Infectious Agents • Rickettsiae: – Are between bacteria and viruses in size – Appear as rods, cocci, or varied shapes – Multiply in the cells of animals • Rats, squirrels – Transmitted to humans thru flea and tick bites • • Rocky mountain spotted fever Typhus These diseases are found in areas of poor sanitation Where rodent and insects are not controlled
Actions of Infectious Agents • Helminths: – Worms – Hand to mouth transmission – Commonly found in GI tract • Abd pain and bloating or asymptomatic – Children: • Pin worm: (Rectal irritation) • Tape worms (GI tract) (wt loss, Abd pain, bloating) • Hook worms: via soles of the feet and may migrate to lungs, or GI tract ( liver, intestine etc) – Producing abd pain, diarrhea, anemia
Actions of Infectious Agents • Mycoplasmas: – Gram negative, multi-shaped organism – No cell walls – Called pleuropneumonia-like organisms – Cause: • Atypical pneumonia in humans • Reiter syndrome : (multi-system inflammatory disease in humans) • Usually responsible for respiratory tract infections in children and adult • Respond well to erythromycin
Actions of Infectious Agents • Prions: – Do not have a nucleus – Transmittable and leads to: • Have a long incubation period and very resistant to ABX • brain damage – Brain develops holes or becomes spongiform • Progressive degenerative diseases of nervous system • Creutzfeldt-Jakob disease • Bovine spongiform encephalopathy (mad cow’s Disease )
Community acquired infections • Transmitted in daily contact with people – Flu viruses (predictable times of the year) – Child hood diseases ; September (school) • Related to – Poverty – Low immunization rates – overcrowded environments – Resistant strains of pathogens (TB, MRSA) – Infected immigrants
Community acquired infections • Food borne illnesses: – More common in the summer – Food poisoning (picnics, hot weather : mayo) • Staphylococcus • Salmonella – Hepatitis outbreaks • Poor hygiene by food handlers – Sexually transmitted infections : • • Gonorrhea Syphilis HIV All require reporting to the public authorities (laws vary)
Prevention and control • Child hood immunizations – Ignoring or indifference is leading to reemergence of child hood diseases R/T: • Fees • Unable to meet schedules for immunizations etc – Repeat vaccinations for older children – State laws require certain immunizations • Before a child starts school
Prevention and control Cont’d • Blocking the chain of transmission: – Education in : • Food handling • Refrigeration • TB screening – Early Isolation of the exposed patient (positive TB test)from the public • Control of Vectors (mosquito spraying) • ABX to children exposed to : – – communicable diseases Streptococcal infections Sanitation of water supplies, Cooking meat, eggs, poultry well done
Prevention and control (Cont’d) • Personal measures to control the spread of communicable disease: – Proper hygiene – Hand washing – Personal barriers (condoms) – Staying home when s/s of an infectious disease appear breaks the chain of infection
Health Care Associated infections • HAI’s : – AKA- Nosocomial infections – Carry a higher morbidity (danger to in house pt) – Occur within the health care facility – May affect the patient and the health care worker – More serious than community acquired infxn – Vancomycin Resistant enterococcus (VRE) • May be related to overuse or misuse of ABX • ABX alter the normal flora replacing good microbes with bad ones that are more difficult to get rid off – Thru mutations
HAI’s • MDRO’s: (multidrug-resistant organisms) – Microorganisms that are resistant to one or more classes of antimicrobials – Such as: • • MRSA VRE E- Coli Klebsiella Pneumonia and others – General measures that help impede resistant strains of microbes : • Vaccinations • Appropriate use of ABX (C&S specific) )
HAI’s • Health care worker is at high risk of contracting HAI: – Hepatitis B – Legionnaires disease – Staph – Pseudomonas • Iatrogenic infections: caused by treatments given to patients – Immunosuppressant drugs for transplants – Super infections ( clostridium Dificile) • Normally lives within us and kept in check by normal flora
Nursing Care of patients with infections • Key to preventing the spread of infections in the hospital is thru medical and surgical asepsis: – Medical asepsis: • Often called clean technique – – Changing bed linen Sanitizing bedpans Individual med cups for each pt Frequent hand washing
Medical Asepsis • Hand hygiene: – Dirty hands are the primary mode of infectious transmissions – Need to remind yourself to : • frequently wash your hands (friction, running water, soap) • Alcohol based waterless antiseptic • Surgical scrub
Surgical Asepsis • Sterile technique – Technique that Prevents unsterile surfaces to come in contact with the patient • Standard precautions: – Used for the care of all patients • Transmission based precautions – Disease specific isolation techniques • • • Reduce the risk of airborne infections Airborne, contact droplet, protective
Surgical Asepsis • Some standard precautions may be used in specific situations • ie: – Respiratory hygiene – Cough etiquette – Safe injection practices – Masks for insertion of catheters/ LP’s – Make sure you read box 13 -3
CDC Standard Precautions for infection control
The immune response • Two types: – Antibody mediated is a response to an antigen • B lymphocytes • Antibodies – Antigen binds to a receptor on the lymphocyte – Results in production of antibodies – Which will look for the antigen and stick to it – Neutrophils and macrophages will recognize them and clean up
Antibodies • 5 classes: – Ig. G : most abundant crosses placental barrier • Provides passive newborn immunity – Ig. M – Ig. A – Ig. E : is vital for allergic reactions and parasitic infections – Ig. D
dd3814d1bcec594cb298d34a3f896e2a.ppt