810f522b3de0ea823422cf87a58708d1.ppt
- Количество слайдов: 77
 Induced Hypothermia How EMS can improve the long term outcomes for resuscitated patients
Induced Hypothermia How EMS can improve the long term outcomes for resuscitated patients
 Wake EMS Induced Hypothermia Team J. Brent Myers, MD, MPH Medical Director Paul R. Hinchey, MD, MBA, EMT-P Assistant Medical Director Joseph Zalkin, EMT-P Assistant Chief Professional Development Jon Olson, MBA, MHA, EMT-P District Chief Operations Ryan Lewis, EMT-P District Chief Quality Assurance Donald Garner, EMT-P District Chief Training
Wake EMS Induced Hypothermia Team J. Brent Myers, MD, MPH Medical Director Paul R. Hinchey, MD, MBA, EMT-P Assistant Medical Director Joseph Zalkin, EMT-P Assistant Chief Professional Development Jon Olson, MBA, MHA, EMT-P District Chief Operations Ryan Lewis, EMT-P District Chief Quality Assurance Donald Garner, EMT-P District Chief Training
 Induced Hypothermia(IH) • • • What is Induced Hypothermia? Why IH at Wake EMS? How does it work? When is it indicated? How will it be applied?
Induced Hypothermia(IH) • • • What is Induced Hypothermia? Why IH at Wake EMS? How does it work? When is it indicated? How will it be applied?
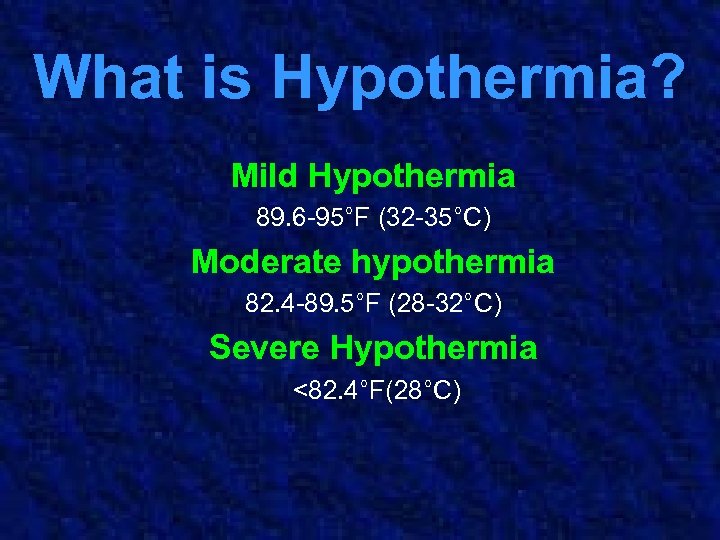 What is Hypothermia? Mild Hypothermia 89. 6 -95°F (32 -35°C) Moderate hypothermia 82. 4 -89. 5°F (28 -32°C) Severe Hypothermia <82. 4°F(28°C)
What is Hypothermia? Mild Hypothermia 89. 6 -95°F (32 -35°C) Moderate hypothermia 82. 4 -89. 5°F (28 -32°C) Severe Hypothermia <82. 4°F(28°C)
 What is Induced Hypothermia? Active cooling of the body to below normal levels
What is Induced Hypothermia? Active cooling of the body to below normal levels
 So why would ……a little you intentionally history will induce help…. . hypothermia?
So why would ……a little you intentionally history will induce help…. . hypothermia?
 In March of 2005, nine months prior to the November 2005 release of the AHA resuscitation guidelines, Wake County EMS System implemented new CPR protocols using the latest in resuscitation techniques and available technology.
In March of 2005, nine months prior to the November 2005 release of the AHA resuscitation guidelines, Wake County EMS System implemented new CPR protocols using the latest in resuscitation techniques and available technology.
 The Technique • Changed CPR: – Emphasis on effective uninterrupted compression – Decreased emphasis on importance of ventilation – Slower ventilatory rates
The Technique • Changed CPR: – Emphasis on effective uninterrupted compression – Decreased emphasis on importance of ventilation – Slower ventilatory rates
 The Technology • Use of ETCO 2: – As confirmation of ETT placement – Goal directed respiratory rate
The Technology • Use of ETCO 2: – As confirmation of ETT placement – Goal directed respiratory rate
 The Technology • EZ IO drill: – Rapid IV access if initial IV attempt fails
The Technology • EZ IO drill: – Rapid IV access if initial IV attempt fails
 So……. what happened?
So……. what happened?
 What does that have to do with hypothermia?
What does that have to do with hypothermia?
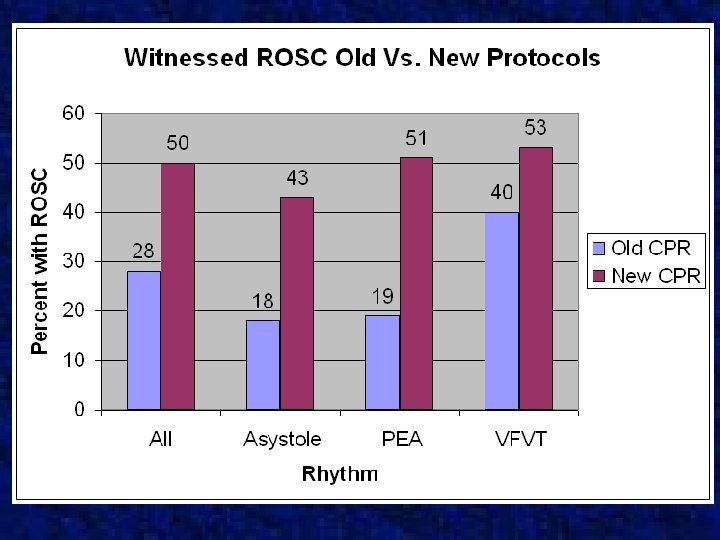
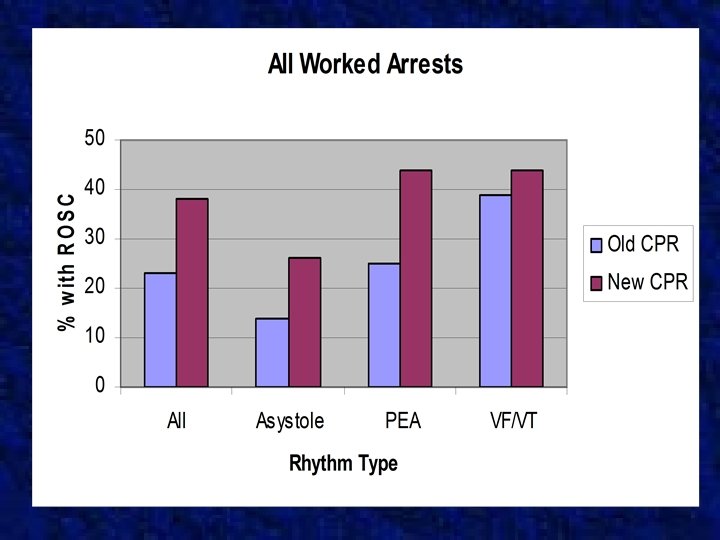
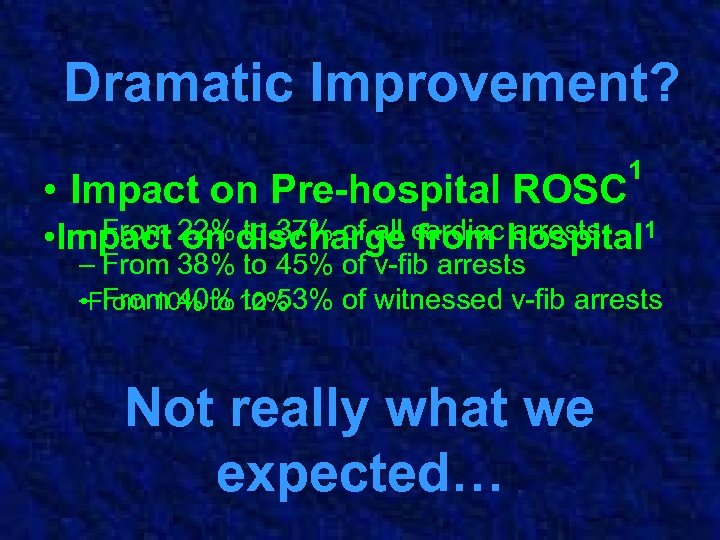 Dramatic Improvement? • Impact on Pre-hospital ROSC 1 – From on to 37% of all from arrests • Impact 22%discharge cardiac hospital 1 – From 38% to 45% of v-fib arrests – From 40% to 53% of witnessed v-fib arrests • From 10% to 12% Not really what we expected…
Dramatic Improvement? • Impact on Pre-hospital ROSC 1 – From on to 37% of all from arrests • Impact 22%discharge cardiac hospital 1 – From 38% to 45% of v-fib arrests – From 40% to 53% of witnessed v-fib arrests • From 10% to 12% Not really what we expected…
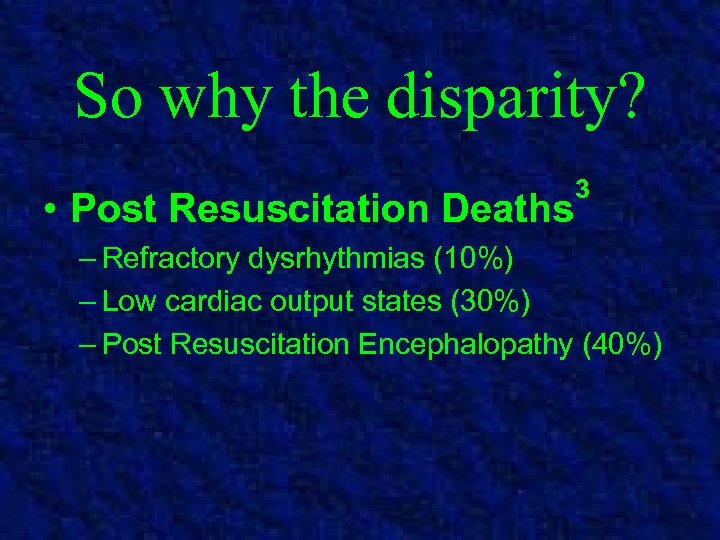 So why the disparity? • Post Resuscitation Deaths 3 – Refractory dysrhythmias (10%) – Low cardiac output states (30%) – Post Resuscitation Encephalopathy (40%)
So why the disparity? • Post Resuscitation Deaths 3 – Refractory dysrhythmias (10%) – Low cardiac output states (30%) – Post Resuscitation Encephalopathy (40%)
 Post Resuscitation PRE is caused by a series of events that begin Encephalopathy (PRE) is the singleimmediately following post largest contributor to reperfusion deaths and with resuscitation of the brain poor ROSC……… neurologic outcomes.
Post Resuscitation PRE is caused by a series of events that begin Encephalopathy (PRE) is the singleimmediately following post largest contributor to reperfusion deaths and with resuscitation of the brain poor ROSC……… neurologic outcomes.
 PRE • Initial hypoperfusion insult followed by period of hyperperfusion with ROSC 8, 11 • Cell injury 3 – Oxygen free radical formation – Inflammatory cascade – Glutamate mediated cell death • Loss of Autoregulation 3, 8, 11 – Patchy intracerebral vasoconstriction – Intravascular sludging and hypoperfusion – Perfusion/demand mismatch
PRE • Initial hypoperfusion insult followed by period of hyperperfusion with ROSC 8, 11 • Cell injury 3 – Oxygen free radical formation – Inflammatory cascade – Glutamate mediated cell death • Loss of Autoregulation 3, 8, 11 – Patchy intracerebral vasoconstriction – Intravascular sludging and hypoperfusion – Perfusion/demand mismatch
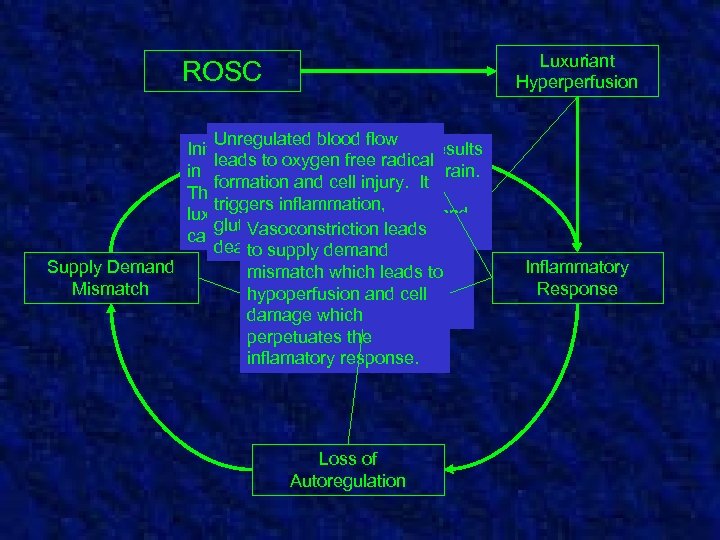 Luxuriant Hyperperfusion ROSC Unregulated blood flow Initial restoration of blood flow results leads to oxygen free radical in unregulated perfusion of the brain. formation and cell injury. It This period is referred to as the triggers inflammation, luxuriant hyperperfusion period and glutamate post resuscitation The mediated cell can last. Vasoconstriction leads from 10 -30 minutes. deathbrainedema. diffuse, to and develops supply demand Supply Demand mismatch which leads to patchy vasoconstriction Mismatch hypoperfusion and cell and intravascular damage which sludging. perpetuates the inflamatory response. Loss of Autoregulation Inflammatory Response
Luxuriant Hyperperfusion ROSC Unregulated blood flow Initial restoration of blood flow results leads to oxygen free radical in unregulated perfusion of the brain. formation and cell injury. It This period is referred to as the triggers inflammation, luxuriant hyperperfusion period and glutamate post resuscitation The mediated cell can last. Vasoconstriction leads from 10 -30 minutes. deathbrainedema. diffuse, to and develops supply demand Supply Demand mismatch which leads to patchy vasoconstriction Mismatch hypoperfusion and cell and intravascular damage which sludging. perpetuates the inflamatory response. Loss of Autoregulation Inflammatory Response
 Factors in PRE • Inflammation and Edema • Vasoconstriction and Sludging • Supply Demand Mismatch
Factors in PRE • Inflammation and Edema • Vasoconstriction and Sludging • Supply Demand Mismatch
 Induced hypothermia is part of a multifaceted approach to optimizing neurologic resuscitation.
Induced hypothermia is part of a multifaceted approach to optimizing neurologic resuscitation.
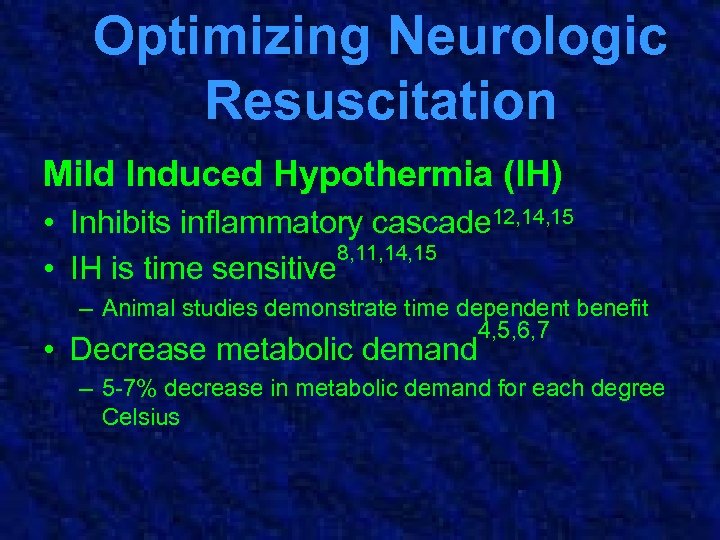 Optimizing Neurologic Resuscitation Mild Induced Hypothermia (IH) • Inhibits inflammatory cascade 12, 14, 15 8, 11, 14, 15 • IH is time sensitive – Animal studies demonstrate time dependent benefit 4, 5, 6, 7 • Decrease metabolic demand – 5 -7% decrease in metabolic demand for each degree Celsius
Optimizing Neurologic Resuscitation Mild Induced Hypothermia (IH) • Inhibits inflammatory cascade 12, 14, 15 8, 11, 14, 15 • IH is time sensitive – Animal studies demonstrate time dependent benefit 4, 5, 6, 7 • Decrease metabolic demand – 5 -7% decrease in metabolic demand for each degree Celsius
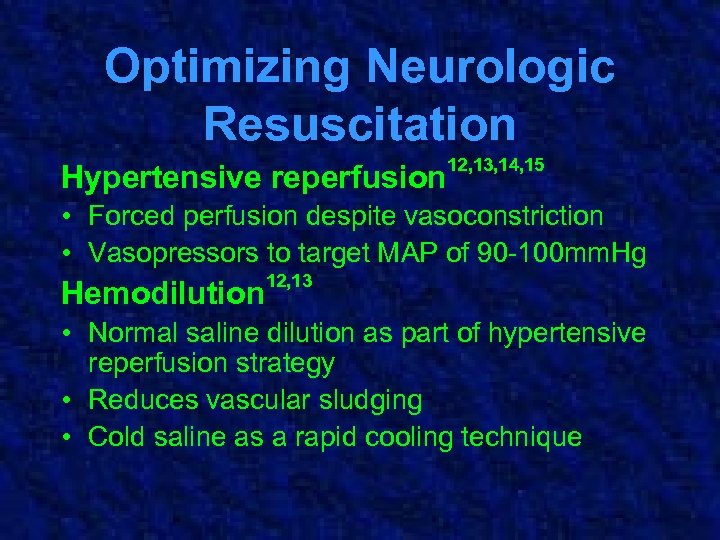 Optimizing Neurologic Resuscitation Hypertensive reperfusion 12, 13, 14, 15 • Forced perfusion despite vasoconstriction • Vasopressors to target MAP of 90 -100 mm. Hg Hemodilution 12, 13 • Normal saline dilution as part of hypertensive reperfusion strategy • Reduces vascular sludging • Cold saline as a rapid cooling technique
Optimizing Neurologic Resuscitation Hypertensive reperfusion 12, 13, 14, 15 • Forced perfusion despite vasoconstriction • Vasopressors to target MAP of 90 -100 mm. Hg Hemodilution 12, 13 • Normal saline dilution as part of hypertensive reperfusion strategy • Reduces vascular sludging • Cold saline as a rapid cooling technique
 There are several landmark studies on the subject
There are several landmark studies on the subject
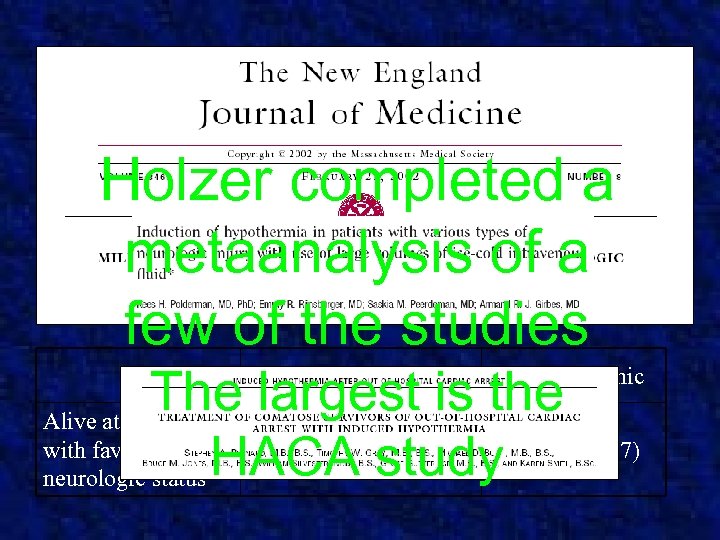 Holzer completed a metaanalysis of a few of the studies The largest is the Alive at 6 months 55% (75/136) 39% (54/137) with favorable neurologic status HACA study Hypothermic Normothermic
Holzer completed a metaanalysis of a few of the studies The largest is the Alive at 6 months 55% (75/136) 39% (54/137) with favorable neurologic status HACA study Hypothermic Normothermic
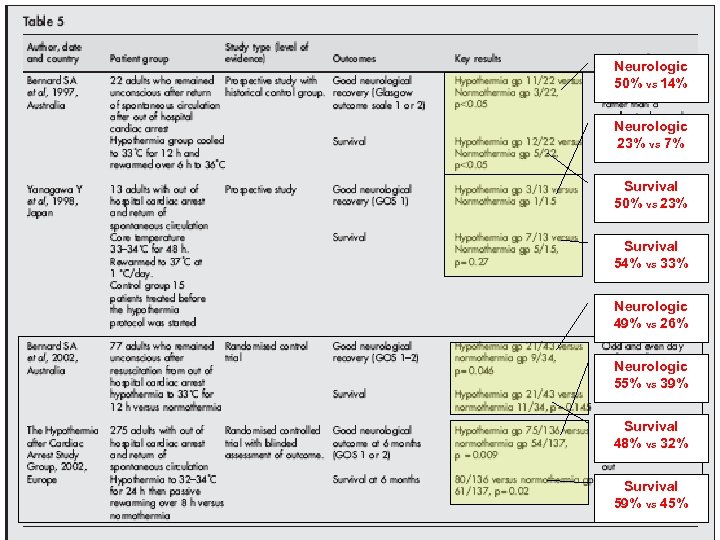 Summary of Studies Neurologic 50% vs 14% Neurologic 23% vs 7% Survival 50% vs 23% Survival 54% vs 33% Neurologic 49% vs 26% Neurologic 55% vs 39% Survival 48% vs 32% Survival 59% vs 45%
Summary of Studies Neurologic 50% vs 14% Neurologic 23% vs 7% Survival 50% vs 23% Survival 54% vs 33% Neurologic 49% vs 26% Neurologic 55% vs 39% Survival 48% vs 32% Survival 59% vs 45%
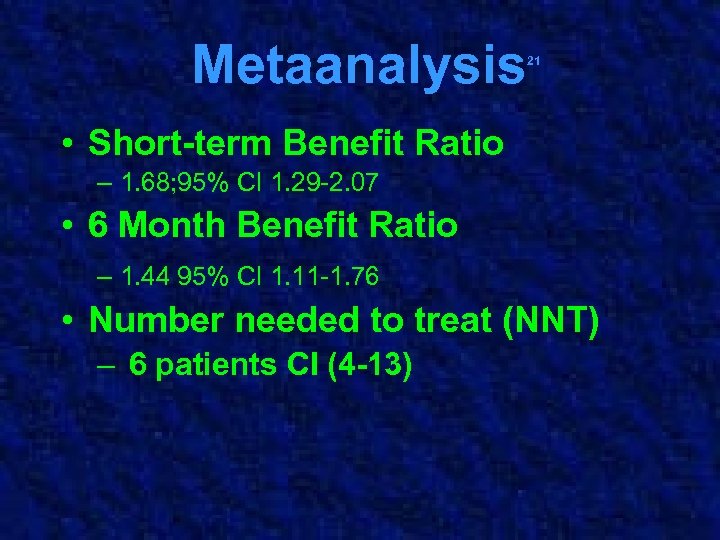 Metaanalysis 21 • Short-term Benefit Ratio – 1. 68; 95% CI 1. 29 -2. 07 • 6 Month Benefit Ratio – 1. 44 95% CI 1. 11 -1. 76 • Number needed to treat (NNT) – 6 patients CI (4 -13)
Metaanalysis 21 • Short-term Benefit Ratio – 1. 68; 95% CI 1. 29 -2. 07 • 6 Month Benefit Ratio – 1. 44 95% CI 1. 11 -1. 76 • Number needed to treat (NNT) – 6 patients CI (4 -13)
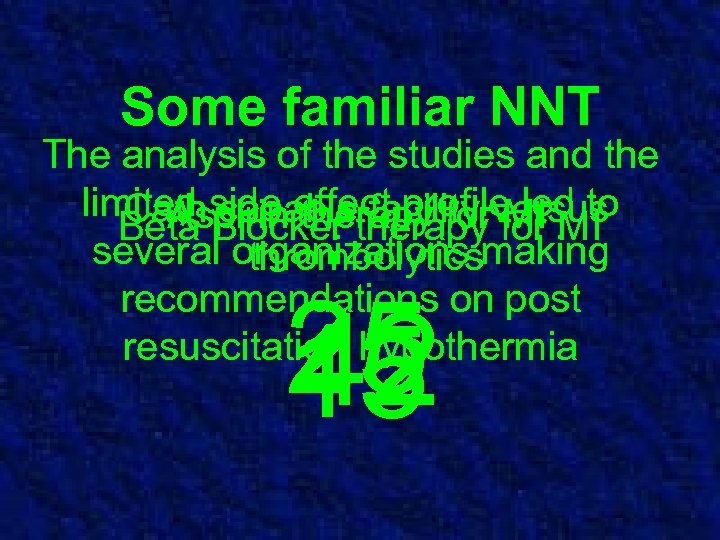 Some familiar NNT The analysis of the studies and the limited side effect profile led to Cath Blocker therapy versus capable facility MI Aspirin therapy for MI Beta several organizations making thrombolytics recommendations on post resuscitation hypothermia 25 42 15
Some familiar NNT The analysis of the studies and the limited side effect profile led to Cath Blocker therapy versus capable facility MI Aspirin therapy for MI Beta several organizations making thrombolytics recommendations on post resuscitation hypothermia 25 42 15
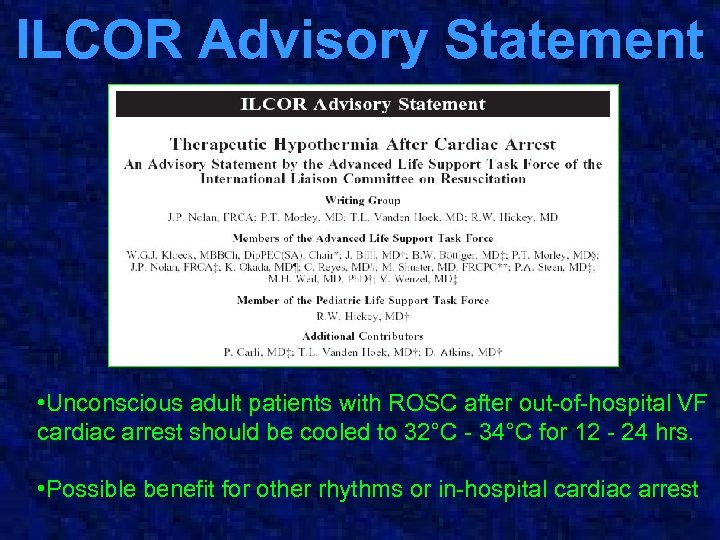 ILCOR Advisory Statement • Unconscious adult patients with ROSC after out-of-hospital VF cardiac arrest should be cooled to 32°C - 34°C for 12 - 24 hrs. • Possible benefit for other rhythms or in-hospital cardiac arrest
ILCOR Advisory Statement • Unconscious adult patients with ROSC after out-of-hospital VF cardiac arrest should be cooled to 32°C - 34°C for 12 - 24 hrs. • Possible benefit for other rhythms or in-hospital cardiac arrest
 Aha statement Post Resuscitation Treatment • • • Induced hypothermia Prevention of hyperthermia Tight glucose control Prevent hypocapnia Maintain elevated MAP
Aha statement Post Resuscitation Treatment • • • Induced hypothermia Prevention of hyperthermia Tight glucose control Prevent hypocapnia Maintain elevated MAP
 As part of the effort to reduce the disparity between our resuscitation rates we had to look at the Firstand hospital discharge rates, Wake County EMS System began effects of hypothermia…. . looking at the use of induced hypothermia in August of 2005.
As part of the effort to reduce the disparity between our resuscitation rates we had to look at the Firstand hospital discharge rates, Wake County EMS System began effects of hypothermia…. . looking at the use of induced hypothermia in August of 2005.
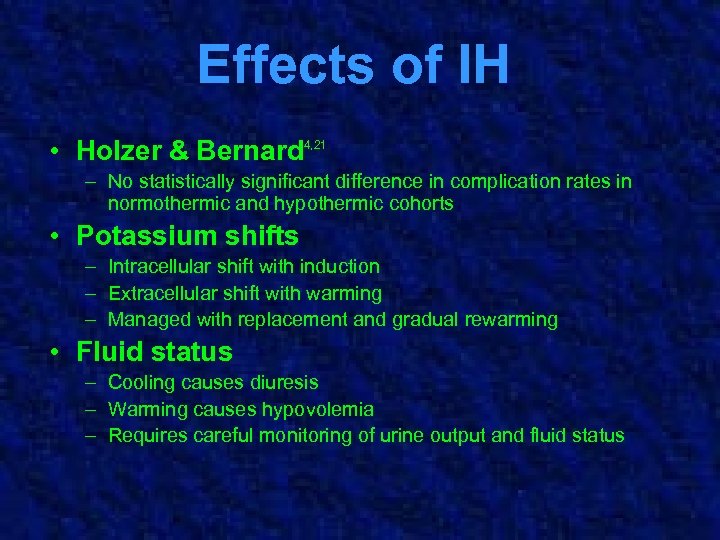 Effects of IH • Holzer & Bernard 4, 21 – No statistically significant difference in complication rates in normothermic and hypothermic cohorts • Potassium shifts – Intracellular shift with induction – Extracellular shift with warming – Managed with replacement and gradual rewarming • Fluid status – Cooling causes diuresis – Warming causes hypovolemia – Requires careful monitoring of urine output and fluid status
Effects of IH • Holzer & Bernard 4, 21 – No statistically significant difference in complication rates in normothermic and hypothermic cohorts • Potassium shifts – Intracellular shift with induction – Extracellular shift with warming – Managed with replacement and gradual rewarming • Fluid status – Cooling causes diuresis – Warming causes hypovolemia – Requires careful monitoring of urine output and fluid status
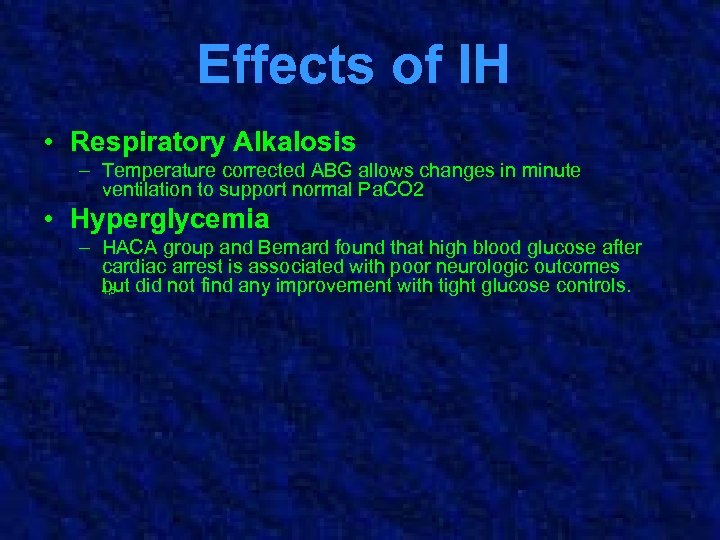 Effects of IH • Respiratory Alkalosis – Temperature corrected ABG allows changes in minute ventilation to support normal Pa. CO 2 • Hyperglycemia – HACA group and Bernard found that high blood glucose after cardiac arrest is associated with poor neurologic outcomes but did not find any improvement with tight glucose controls. 4, 5
Effects of IH • Respiratory Alkalosis – Temperature corrected ABG allows changes in minute ventilation to support normal Pa. CO 2 • Hyperglycemia – HACA group and Bernard found that high blood glucose after cardiac arrest is associated with poor neurologic outcomes but did not find any improvement with tight glucose controls. 4, 5
 Complications of IH in Other Applications • Neutropenia – Neutropenia and increased incidence of pneumonia seen in patients exposed to prolonged hypothermia (>24 hrs) in other applications • Coagulopathy 18, 19, 20 – May alter clotting cascade, platelet function • Cardiac dysrhythmias – Little risk for clinically significant dysrhythmias if temperatures are maintained >30°C 17
Complications of IH in Other Applications • Neutropenia – Neutropenia and increased incidence of pneumonia seen in patients exposed to prolonged hypothermia (>24 hrs) in other applications • Coagulopathy 18, 19, 20 – May alter clotting cascade, platelet function • Cardiac dysrhythmias – Little risk for clinically significant dysrhythmias if temperatures are maintained >30°C 17
 After finding limited side effects we developed a comprehensive protocol from field implementation to hospital discharge.
After finding limited side effects we developed a comprehensive protocol from field implementation to hospital discharge.
 Wake County Plan Objective is cost effective, prehospital initiation of induced hypothermia in patients with ROSC.
Wake County Plan Objective is cost effective, prehospital initiation of induced hypothermia in patients with ROSC.
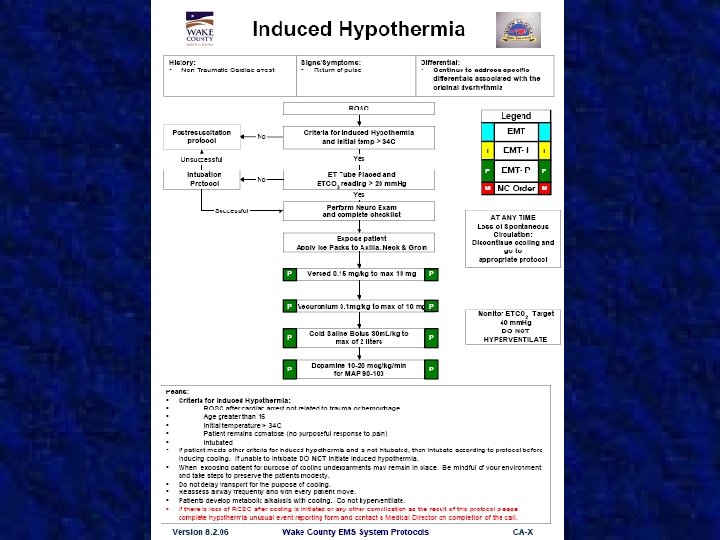
 Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose Confirmed Intubation
Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose Confirmed Intubation
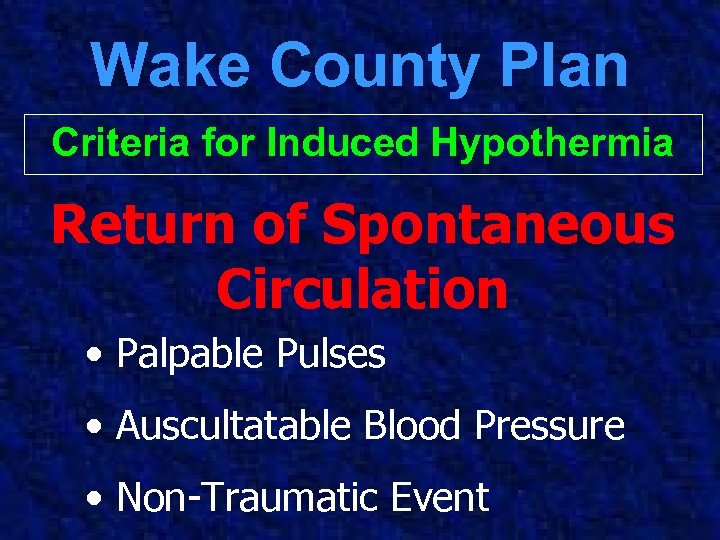 Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation • Palpable Pulses • Auscultatable Blood Pressure • Non-Traumatic Event
Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation • Palpable Pulses • Auscultatable Blood Pressure • Non-Traumatic Event
 Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose • No purposeful movements
Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose • No purposeful movements
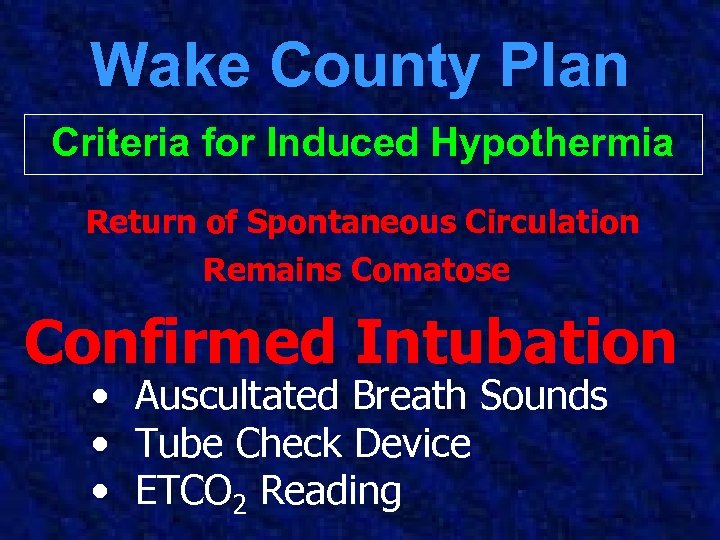 Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose Confirmed Intubation • Auscultated Breath Sounds • Tube Check Device • ETCO 2 Reading
Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose Confirmed Intubation • Auscultated Breath Sounds • Tube Check Device • ETCO 2 Reading
 Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose Confirmed Intubation
Wake County Plan Criteria for Induced Hypothermia Return of Spontaneous Circulation Remains Comatose Confirmed Intubation
 Wake County Plan Protocol for Induced Hypothermia Expose the Patient
Wake County Plan Protocol for Induced Hypothermia Expose the Patient
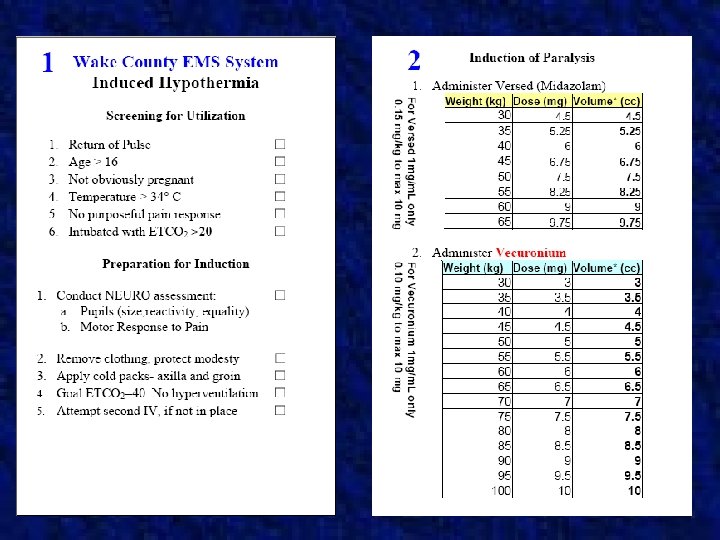
 Wake County Plan Protocol for Induced Hypothermia Slowly administer Versed 0. 15 mg/kg up to 10 mg
Wake County Plan Protocol for Induced Hypothermia Slowly administer Versed 0. 15 mg/kg up to 10 mg
 Wake County Plan Protocol for Induced Hypothermia Administer Vecuronium 0. 1 mg/kg to max of 10 mg
Wake County Plan Protocol for Induced Hypothermia Administer Vecuronium 0. 1 mg/kg to max of 10 mg
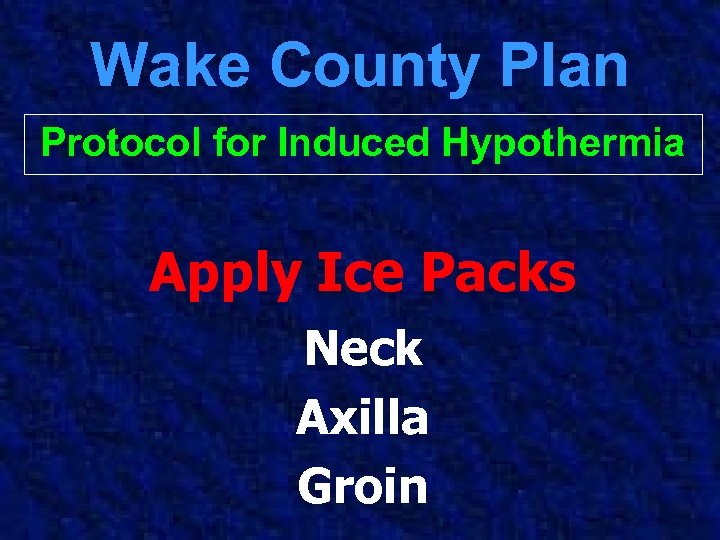 Wake County Plan Protocol for Induced Hypothermia Apply Ice Packs Neck Axilla Groin
Wake County Plan Protocol for Induced Hypothermia Apply Ice Packs Neck Axilla Groin
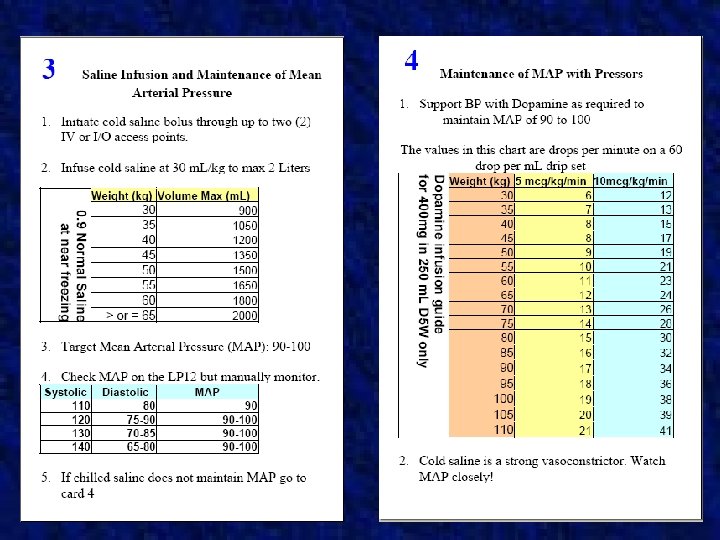
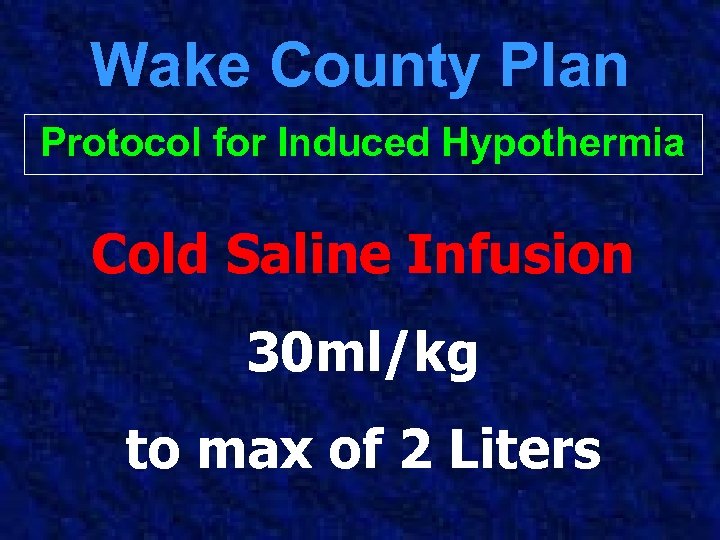 Wake County Plan Protocol for Induced Hypothermia Cold Saline Infusion 30 ml/kg to max of 2 Liters
Wake County Plan Protocol for Induced Hypothermia Cold Saline Infusion 30 ml/kg to max of 2 Liters
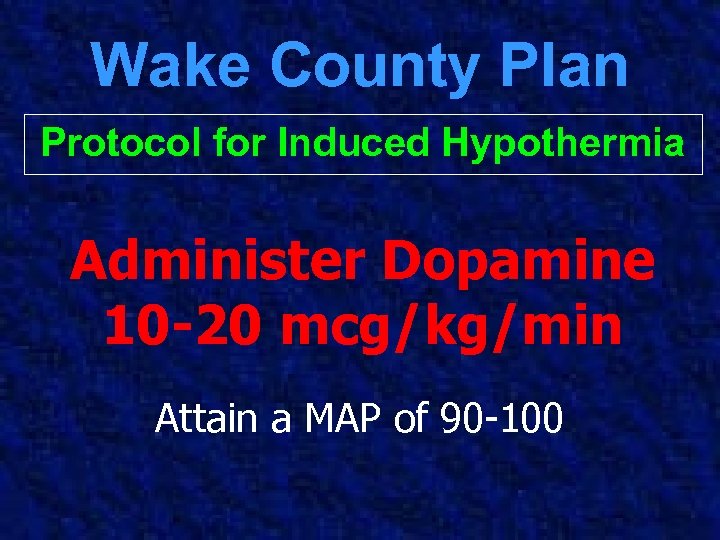 Wake County Plan Protocol for Induced Hypothermia Administer Dopamine 10 -20 mcg/kg/min Attain a MAP of 90 -100
Wake County Plan Protocol for Induced Hypothermia Administer Dopamine 10 -20 mcg/kg/min Attain a MAP of 90 -100
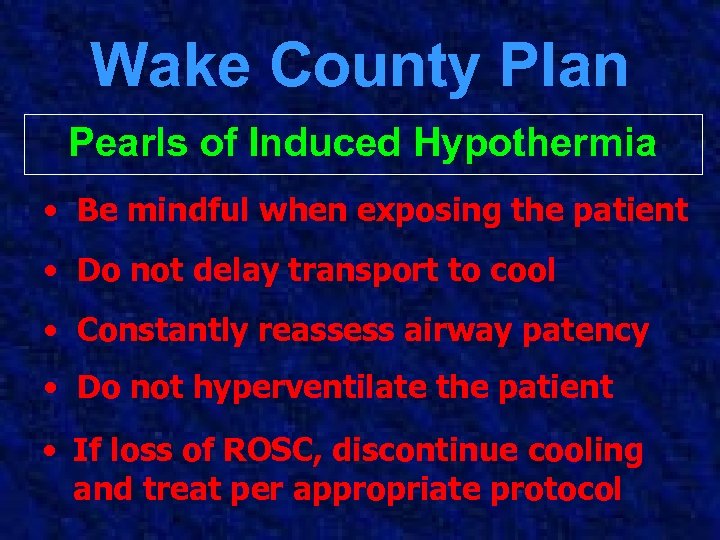 Wake County Plan Pearls of Induced Hypothermia • Be mindful when exposing the patient • Do not delay transport to cool • Constantly reassess airway patency • Do not hyperventilate the patient • If loss of ROSC, discontinue cooling and treat per appropriate protocol
Wake County Plan Pearls of Induced Hypothermia • Be mindful when exposing the patient • Do not delay transport to cool • Constantly reassess airway patency • Do not hyperventilate the patient • If loss of ROSC, discontinue cooling and treat per appropriate protocol
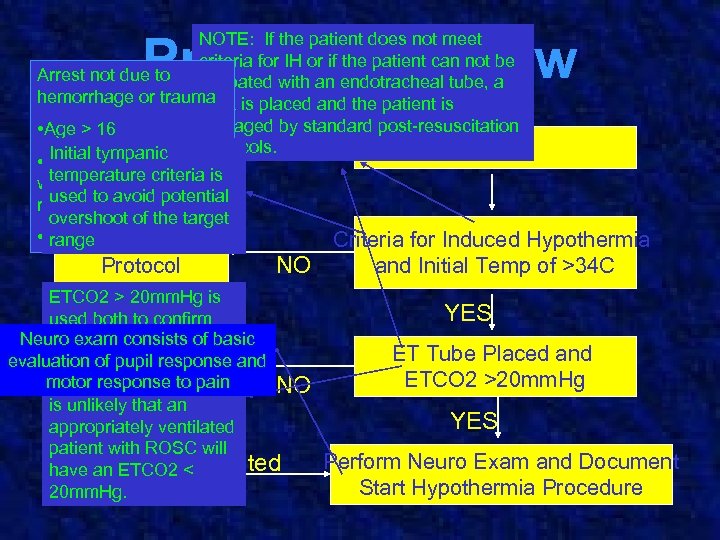 Protocol Review NOTE: If the patient does not meet criteria for IH or if the patient can not be Arrest not due to intubated with an endotracheal tube, a hemorrhage or trauma is placed and the patient is LMA managed by standard post-resuscitation • Age > 16 protocols. ROSC Initial tympanic • Remains comatose temperature criteria with no purposeful is used to to pain response avoid potential overshoot of the target • Patient is intubated range Post-Resuscitation Criteria for Induced Hypothermia Protocol NO ETCO 2 > 20 mm. Hg is used both to confirm Neuro exam consists of as tube placement and basic evaluation Intubation of pupil response an additional measure and Protocol motor response to pain of successful ROSC. It NO is unlikely that an appropriately ventilated patient with ROSC will have an ETCO 2 Intubated < 20 mm. Hg. and Initial Temp of >34 C YES ET Tube Placed and ETCO 2 >20 mm. Hg YES Perform Neuro Exam and Document Start Hypothermia Procedure
Protocol Review NOTE: If the patient does not meet criteria for IH or if the patient can not be Arrest not due to intubated with an endotracheal tube, a hemorrhage or trauma is placed and the patient is LMA managed by standard post-resuscitation • Age > 16 protocols. ROSC Initial tympanic • Remains comatose temperature criteria with no purposeful is used to to pain response avoid potential overshoot of the target • Patient is intubated range Post-Resuscitation Criteria for Induced Hypothermia Protocol NO ETCO 2 > 20 mm. Hg is used both to confirm Neuro exam consists of as tube placement and basic evaluation Intubation of pupil response an additional measure and Protocol motor response to pain of successful ROSC. It NO is unlikely that an appropriately ventilated patient with ROSC will have an ETCO 2 Intubated < 20 mm. Hg. and Initial Temp of >34 C YES ET Tube Placed and ETCO 2 >20 mm. Hg YES Perform Neuro Exam and Document Start Hypothermia Procedure
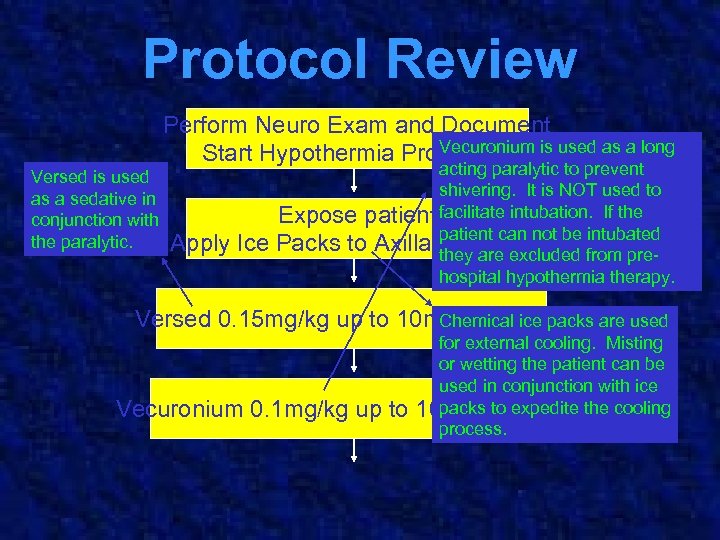 Protocol Review Perform Neuro Exam and Document Vecuronium Start Hypothermia Procedure is used as a long Versed is used as a sedative in conjunction with the paralytic. Apply Ice acting paralytic to prevent shivering. It is NOT used to Expose patient facilitate intubation. If the patient can not be intubated Packs to Axilla andare excluded from pre. Groin they hospital hypothermia therapy. Versed 0. 15 mg/kg up to 10 mg max dose are used Chemical ice packs Vecuronium 0. 1 mg/kg up to for external cooling. Misting or wetting the patient can be used in conjunction with ice packs to expedite 10 mg max dosethe cooling process.
Protocol Review Perform Neuro Exam and Document Vecuronium Start Hypothermia Procedure is used as a long Versed is used as a sedative in conjunction with the paralytic. Apply Ice acting paralytic to prevent shivering. It is NOT used to Expose patient facilitate intubation. If the patient can not be intubated Packs to Axilla andare excluded from pre. Groin they hospital hypothermia therapy. Versed 0. 15 mg/kg up to 10 mg max dose are used Chemical ice packs Vecuronium 0. 1 mg/kg up to for external cooling. Misting or wetting the patient can be used in conjunction with ice packs to expedite 10 mg max dosethe cooling process.
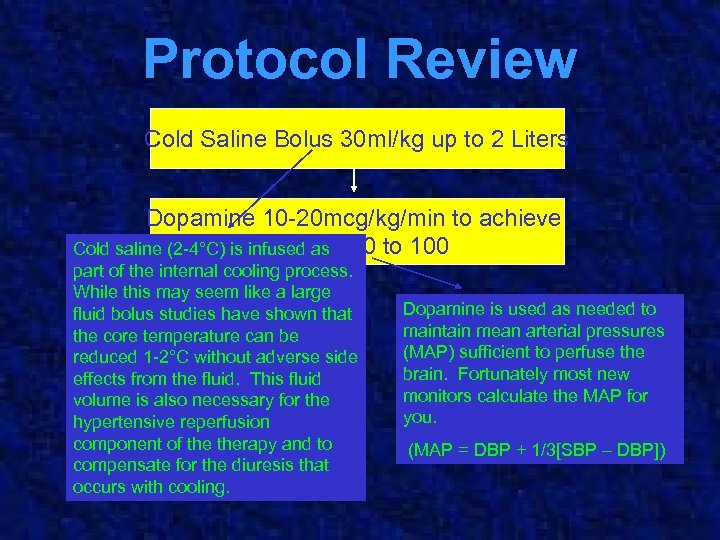 Protocol Review Cold Saline Bolus 30 ml/kg up to 2 Liters Dopamine 10 -20 mcg/kg/min to achieve MAP of Cold saline (2 -4°C) is infused as 90 to 100 part of the internal cooling process. While this may seem like a large fluid bolus studies have shown that the core temperature can be reduced 1 -2°C without adverse side effects from the fluid. This fluid volume is also necessary for the hypertensive reperfusion component of therapy and to compensate for the diuresis that occurs with cooling. Dopamine is used as needed to maintain mean arterial pressures (MAP) sufficient to perfuse the brain. Fortunately most new monitors calculate the MAP for you. (MAP = DBP + 1/3[SBP – DBP])
Protocol Review Cold Saline Bolus 30 ml/kg up to 2 Liters Dopamine 10 -20 mcg/kg/min to achieve MAP of Cold saline (2 -4°C) is infused as 90 to 100 part of the internal cooling process. While this may seem like a large fluid bolus studies have shown that the core temperature can be reduced 1 -2°C without adverse side effects from the fluid. This fluid volume is also necessary for the hypertensive reperfusion component of therapy and to compensate for the diuresis that occurs with cooling. Dopamine is used as needed to maintain mean arterial pressures (MAP) sufficient to perfuse the brain. Fortunately most new monitors calculate the MAP for you. (MAP = DBP + 1/3[SBP – DBP])
 Seem like a lot to remember? So Ryan Lewis created checklists to reduce We thought so… errors and expedite initiation…
Seem like a lot to remember? So Ryan Lewis created checklists to reduce We thought so… errors and expedite initiation…
 Managing Cold Saline Keeping it cold enough to be effective
Managing Cold Saline Keeping it cold enough to be effective
 Managing Cold Saline 36 -39°F (2 -4 °C) is the target temperature The big to keep it was. . . …how question there?
Managing Cold Saline 36 -39°F (2 -4 °C) is the target temperature The big to keep it was. . . …how question there?
 Managing Cold Saline Model 15 Freezer 14 qt Capacity 27 pounds 0 – 40 Degrees Fahrenheit 3. 9 Amp Draw on 12 V System Fits neatly in floorboard of SUV Approx $400 retail
Managing Cold Saline Model 15 Freezer 14 qt Capacity 27 pounds 0 – 40 Degrees Fahrenheit 3. 9 Amp Draw on 12 V System Fits neatly in floorboard of SUV Approx $400 retail
 Managing Cold Saline Initial Deployment on which respond to all EMS District Chief Vehicles cardiac arrests
Managing Cold Saline Initial Deployment on which respond to all EMS District Chief Vehicles cardiac arrests
 Managing Cold Saline Initial Deployment on Reduces initial. Chief Vehicles EMS District start up costs
Managing Cold Saline Initial Deployment on Reduces initial. Chief Vehicles EMS District start up costs
 Managing Cold Saline • Maintaining stock in refrigerator in Station at 45 degrees • 6 Liters in 12 V freezer units on select response units • Add 12 V freezers to all system ambulances as budget permits
Managing Cold Saline • Maintaining stock in refrigerator in Station at 45 degrees • 6 Liters in 12 V freezer units on select response units • Add 12 V freezers to all system ambulances as budget permits
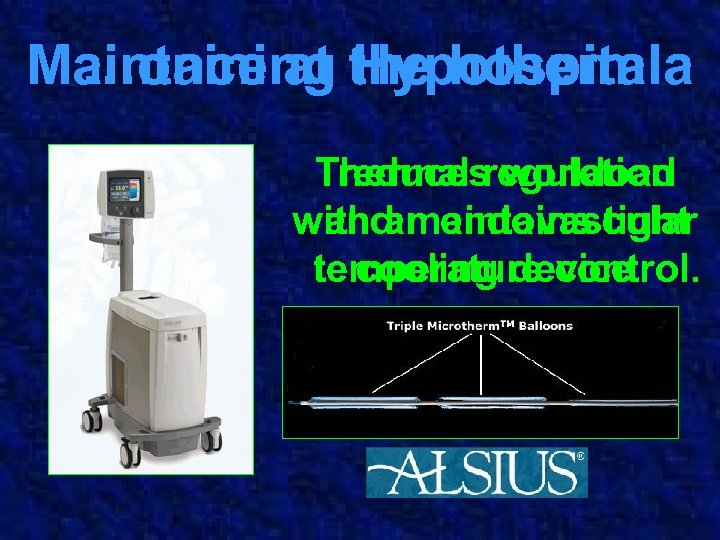 Maintaining the hospital …once at Hypothermia Thermal regulation reduces workload with an endovascular and maintains tight temperature control. cooling device
Maintaining the hospital …once at Hypothermia Thermal regulation reduces workload with an endovascular and maintains tight temperature control. cooling device
 Endovascular Device Placed directly into the Inferior Vena Cava Circulates temperature controlled saline through the catheter module Monitors temperature to within 0. 1 -0. 3 C of pulmonary artery temp Used for both cooling and rewarming
Endovascular Device Placed directly into the Inferior Vena Cava Circulates temperature controlled saline through the catheter module Monitors temperature to within 0. 1 -0. 3 C of pulmonary artery temp Used for both cooling and rewarming
 Is this Research? • Current AHA resuscitation guidelines are based on prospective randomized trials • We felt it was unethical to conduct a randomized trial with a treatment that is now recommended care • Current Wake EMS IH protocol represents a change in therapy to meet the new standard of care.
Is this Research? • Current AHA resuscitation guidelines are based on prospective randomized trials • We felt it was unethical to conduct a randomized trial with a treatment that is now recommended care • Current Wake EMS IH protocol represents a change in therapy to meet the new standard of care.
 Future Research? • Will evaluate efficacy with historical case control based on prior resuscitation and discharge rates. • Currently there is no data on prehospital application of IH therapy: – Evaluate effectiveness of saline induced cooling process – Evaluate prehospital application
Future Research? • Will evaluate efficacy with historical case control based on prior resuscitation and discharge rates. • Currently there is no data on prehospital application of IH therapy: – Evaluate effectiveness of saline induced cooling process – Evaluate prehospital application
 How do you track patient outcomes from pre-hospital care through to discharge without losing them in follow-up?
How do you track patient outcomes from pre-hospital care through to discharge without losing them in follow-up?
 EMS Banding System • Developed by Joseph Zalkin the system provides unique EMS ID # • ID is scanned into EMS electronic call report AND hospital electronic chart • Provides unique tracking number throughout admission to discharge
EMS Banding System • Developed by Joseph Zalkin the system provides unique EMS ID # • ID is scanned into EMS electronic call report AND hospital electronic chart • Provides unique tracking number throughout admission to discharge
 What other steps are we taking to improve survival? • Introduction of endotracheal introducer (Bougie) • Res-Q-Pod
What other steps are we taking to improve survival? • Introduction of endotracheal introducer (Bougie) • Res-Q-Pod
 Why do we do all this? • EMS is unique medical practice environment whose impact extends beyond arrival at the ED doors • In cardiac arrest our goal is discharge to home • Less than 50% of ROSC are sent home • Hospitals currently utilizing IH • IH improves long term outcome • IH is time dependent • IH is cost effective • EMS drives hospital implementation
Why do we do all this? • EMS is unique medical practice environment whose impact extends beyond arrival at the ED doors • In cardiac arrest our goal is discharge to home • Less than 50% of ROSC are sent home • Hospitals currently utilizing IH • IH improves long term outcome • IH is time dependent • IH is cost effective • EMS drives hospital implementation
 Summary • IH is part of multifaceted AHA recommended strategy to improve neurologic outcomes in CA • It requires limited training, minimal cost of implementation and has few significant complications • IH is ideally suited to EMS because it: – Impacts outcomes – Is time sensitive – Is cost effective
Summary • IH is part of multifaceted AHA recommended strategy to improve neurologic outcomes in CA • It requires limited training, minimal cost of implementation and has few significant complications • IH is ideally suited to EMS because it: – Impacts outcomes – Is time sensitive – Is cost effective
 This Just In!
This Just In!
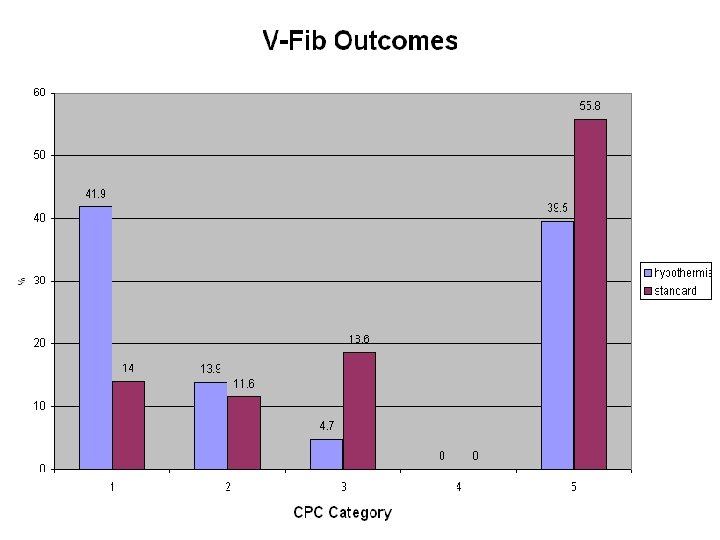
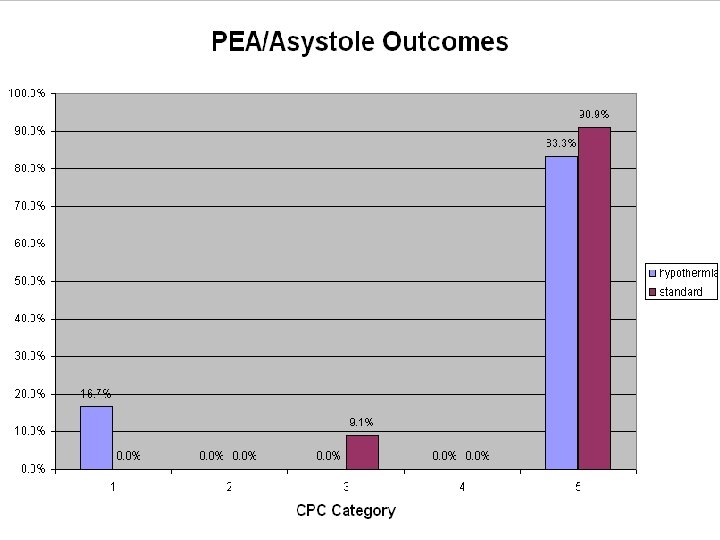
 • 109 out of hospital cardiac arrest from all rhythms • Retrospective study using historical controls • 55 induced hypothermia and 54 controls • Hypothermia to 33 deg C with external device for 24 hrs • Patients treated with versed, fentanyl and vecuronium • MAP were maintained 90 -100 mm. Hg
• 109 out of hospital cardiac arrest from all rhythms • Retrospective study using historical controls • 55 induced hypothermia and 54 controls • Hypothermia to 33 deg C with external device for 24 hrs • Patients treated with versed, fentanyl and vecuronium • MAP were maintained 90 -100 mm. Hg
 • Survey of 2, 248 physicians in UK, US and Finland • Emergency, Cardiology, and Critical Care Physicians • 74% of US and 64% of Non-US never used hypothermia • 16% of US ED physicians and 34% of US Intensivists • Reasons cited • Not enough data • Not a part of ACLS guidelines • Too technically difficult to use
• Survey of 2, 248 physicians in UK, US and Finland • Emergency, Cardiology, and Critical Care Physicians • 74% of US and 64% of Non-US never used hypothermia • 16% of US ED physicians and 34% of US Intensivists • Reasons cited • Not enough data • Not a part of ACLS guidelines • Too technically difficult to use
 Citations 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Wake County EMS Database Edgren, E et al Assessment of neurological prognosis of comatose survivors of cardiac arrest. Lancet 1994; 343: 1055 -59. Myerburg, R et al. Clinical, electrophysiologic and hemodynamic profile of patients resuscitated from prehospital cardiac arrest. Am J Med. 1980; 68: 568 -76. Hypothermia After Cardiac Arrest (HACA) Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346: 549 -56. Bernard, SA et al. Treatment of comatose survivors of out of hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002; 346: 557 -63. Yanagawa, Y, et al. Preliminary clinical outcome study of mild resuscitative hypothermia after out of hospital cardiopulmonary arrest. Resuscitation 1998; 36: 61 -66. Bernard, SA, et al. Clinical trial of induced hypothermia in comatose survivors of out of hospital cardiac arrest. Ann Emerg Med. 1997; 30: 146 -53. Persse, DE et al. Managing the post-resuscitation patient in the field. PEC 2002; 6: 114 -22. Part 7. 5: Postresuscitation Support. Circulation 2005; 112: 84 -88. Kollmar, R. Early effects of acid-base management during hypothermia on cerebral infarct volume, edema, and cerebral blood flow in acure focal cerebral ischemia in rats. Anesthesiology 2002; 97: 868 -74. Persse, D. Et al. Managing the post resuscitation patient in the field. PEC 2002; 6: 114 -122 Leonov Y, et al. Hypertension with hemodilution prevents multifocal cerebral hypoperfusion after cardiac arrest in dogs. Stroke. 1992; 23: 45 -53. Sterz F, et al. Hypertension with or without hemodilution after cardiac arrest in dogs. Stroke. 1990; 21: 1178 -84. Kuboyama K, et al. Delay in cooling negates beneficial effects of mild resuscitative hypothermia after cardiac arrest in dogs. Crit Care Med. 1993; 21: 1348 -58. Markarian GZ, et al. Mild hypothermia: therapeutic window after experimental cerebral ischemia. Neurosurgery 1996, 38: 542 -551. Nolan, JP. Therapeutic hypothermia after cardiac arrest: An advisory statement by the advanced life support task force of the international liaison committee on resuscitation. Circulation 2003; 108: 118 -121. Danzl DF. Accidental hypothermia. N Engl J Med. 1994; 331: 1756 -60. Patt, A. Effect of hypothermia induced coagulopathies in trauma. Surg Lcin North Am. 1988; 68: 775 -85. Roher MJ. Effect of hypothermia on the coagulation cascade. Crit Care Med. 1992; 20: 1402 -05. Valerie CR. Hypothermia induced platelet dysfunction Ann Surg. 1987; 205: 175 -81. Holzer M. Hypothermia for neuroprotection after cardiac arrest: Systematic review and individual patient data meta-analysis. Crit Care Med 2005; 33: 414 -18.
Citations 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Wake County EMS Database Edgren, E et al Assessment of neurological prognosis of comatose survivors of cardiac arrest. Lancet 1994; 343: 1055 -59. Myerburg, R et al. Clinical, electrophysiologic and hemodynamic profile of patients resuscitated from prehospital cardiac arrest. Am J Med. 1980; 68: 568 -76. Hypothermia After Cardiac Arrest (HACA) Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346: 549 -56. Bernard, SA et al. Treatment of comatose survivors of out of hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002; 346: 557 -63. Yanagawa, Y, et al. Preliminary clinical outcome study of mild resuscitative hypothermia after out of hospital cardiopulmonary arrest. Resuscitation 1998; 36: 61 -66. Bernard, SA, et al. Clinical trial of induced hypothermia in comatose survivors of out of hospital cardiac arrest. Ann Emerg Med. 1997; 30: 146 -53. Persse, DE et al. Managing the post-resuscitation patient in the field. PEC 2002; 6: 114 -22. Part 7. 5: Postresuscitation Support. Circulation 2005; 112: 84 -88. Kollmar, R. Early effects of acid-base management during hypothermia on cerebral infarct volume, edema, and cerebral blood flow in acure focal cerebral ischemia in rats. Anesthesiology 2002; 97: 868 -74. Persse, D. Et al. Managing the post resuscitation patient in the field. PEC 2002; 6: 114 -122 Leonov Y, et al. Hypertension with hemodilution prevents multifocal cerebral hypoperfusion after cardiac arrest in dogs. Stroke. 1992; 23: 45 -53. Sterz F, et al. Hypertension with or without hemodilution after cardiac arrest in dogs. Stroke. 1990; 21: 1178 -84. Kuboyama K, et al. Delay in cooling negates beneficial effects of mild resuscitative hypothermia after cardiac arrest in dogs. Crit Care Med. 1993; 21: 1348 -58. Markarian GZ, et al. Mild hypothermia: therapeutic window after experimental cerebral ischemia. Neurosurgery 1996, 38: 542 -551. Nolan, JP. Therapeutic hypothermia after cardiac arrest: An advisory statement by the advanced life support task force of the international liaison committee on resuscitation. Circulation 2003; 108: 118 -121. Danzl DF. Accidental hypothermia. N Engl J Med. 1994; 331: 1756 -60. Patt, A. Effect of hypothermia induced coagulopathies in trauma. Surg Lcin North Am. 1988; 68: 775 -85. Roher MJ. Effect of hypothermia on the coagulation cascade. Crit Care Med. 1992; 20: 1402 -05. Valerie CR. Hypothermia induced platelet dysfunction Ann Surg. 1987; 205: 175 -81. Holzer M. Hypothermia for neuroprotection after cardiac arrest: Systematic review and individual patient data meta-analysis. Crit Care Med 2005; 33: 414 -18.
 For More Information Paul Hinchey paul. hinchey@co. wake. nc. us Jonathan Olson jolson@co. wake. nc. us
For More Information Paul Hinchey paul. hinchey@co. wake. nc. us Jonathan Olson jolson@co. wake. nc. us


