fa620d6b343bbfa9e74002e644b24ec1.ppt
- Количество слайдов: 66

Indiana Health Coverage Programs
Learning Objectives I. Outline the basics of Medicaid and Indiana Health Coverage Programs (IHCP) II. Identify and define eligibility, goals and specifics of IHCP programs III. Discuss the standard elements of Medicaid and IHCP Eligibility IV. Examine eligibility notices, appeals and redeterminations for Medicaid and IHCP
What is Medicaid? • Enacted in 1965 by Title XIX of the Social Security Act • The federal government matches state spending on Medicaid • In Indiana, Medicaid is called Indiana Health Coverage Programs which is administered by the Office of Policy Planning (OMPP) and Family and Social Services Administration (FSSA) • Provides free or low-cost health insurance coverage to low-income: – Children – Pregnant women – Parents and caretakers – Blind – Disabled – Aged • Income limits are based on the Federal Poverty Level (FPL) • Offers variety of programs with varying criteria
Indiana’s Medicaid • The Office of Medicaid Policy and Planning (OMPP) is responsible for: – Administering Indiana Health Coverage Programs (IHCP) at the State level, including the following functions: • • Medical policy development Program and contract compliance Contracting with MCEs Addressing cost containment issues Establishing IHCP policies Program reimbursement Program integrity, including claims analysis and recovery
Indiana’s Medicaid • The Department of Family Resources (DFR) is the division of FSSA responsible for processing applications and making eligibility decisions. • The County Offices of the DFR administer IHCP at the local level • Online applications for Medicaid are located on the DFR’s Benefit Portal
New Eligibility Groups • As of January 1, 2014, the states must cover: – Former foster children • Under age 26 • Receiving Indiana Medicaid when aged out of the system • Not subject to income limits until age 26 – Children age 6 -18 • Up to 133% FPL – Pregnant Women: • Verification of pregnancy no longer required for Medicaid application • Counted as 2 people • Coverage continues 60 days postpartum
What are the Indiana Health Coverage Programs? • • • Hoosier Healthwise (HHW) Healthy Indiana Plan (HIP) Care Select Traditional Medicaid for Employees with Disabilities (M. E. D. Works) Home and Community-Based Service Waivers (HCBS Waivers) Medicare Savings Program Family Planning Services Spend-Down—Eliminated June 1, 2014 Breast and Cervical Cancer Programs
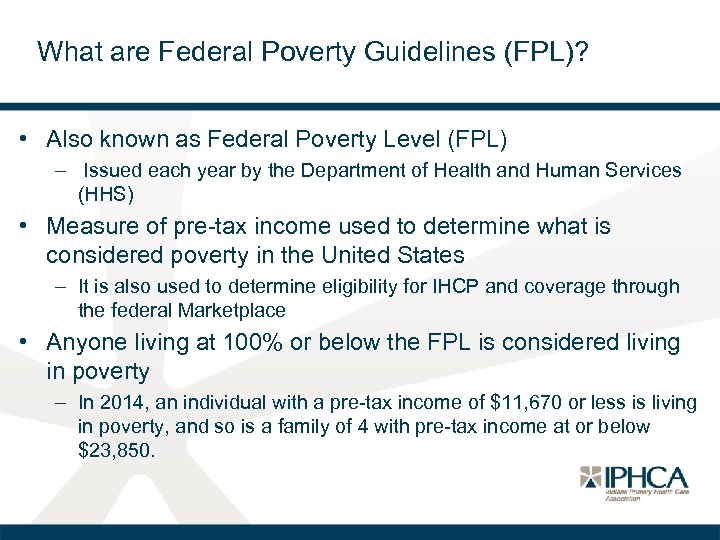
What are Federal Poverty Guidelines (FPL)? • Also known as Federal Poverty Level (FPL) – Issued each year by the Department of Health and Human Services (HHS) • Measure of pre-tax income used to determine what is considered poverty in the United States – It is also used to determine eligibility for IHCP and coverage through the federal Marketplace • Anyone living at 100% or below the FPL is considered living in poverty – In 2014, an individual with a pre-tax income of $11, 670 or less is living in poverty, and so is a family of 4 with pre-tax income at or below $23, 850.
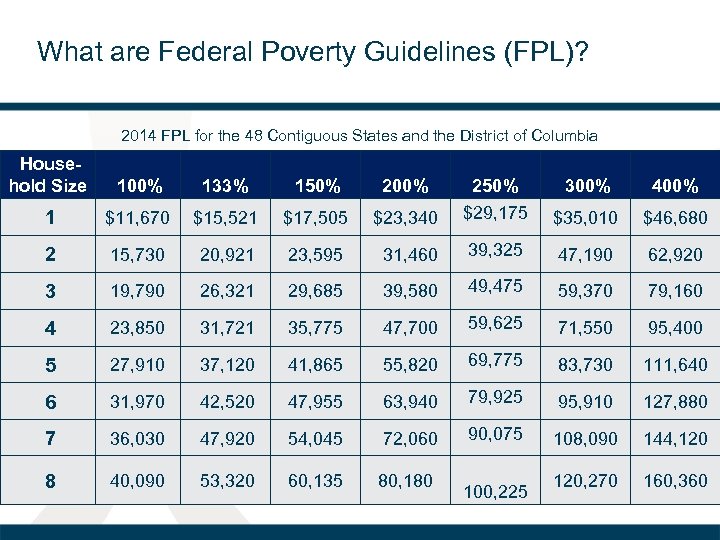
What are Federal Poverty Guidelines (FPL)? 2014 FPL for the 48 Contiguous States and the District of Columbia Household Size 100% 133% 150% 200% 1 $11, 670 $15, 521 $17, 505 2 15, 730 20, 921 3 19, 790 4 300% 400% $23, 340 250% $29, 175 $35, 010 $46, 680 23, 595 31, 460 39, 325 47, 190 62, 920 26, 321 29, 685 39, 580 49, 475 59, 370 79, 160 23, 850 31, 721 35, 775 47, 700 59, 625 71, 550 95, 400 5 27, 910 37, 120 41, 865 55, 820 69, 775 83, 730 111, 640 6 31, 970 42, 520 47, 955 63, 940 79, 925 95, 910 127, 880 7 36, 030 47, 920 54, 045 72, 060 90, 075 108, 090 144, 120 8 40, 090 53, 320 60, 135 80, 180 120, 270 160, 360 100, 225
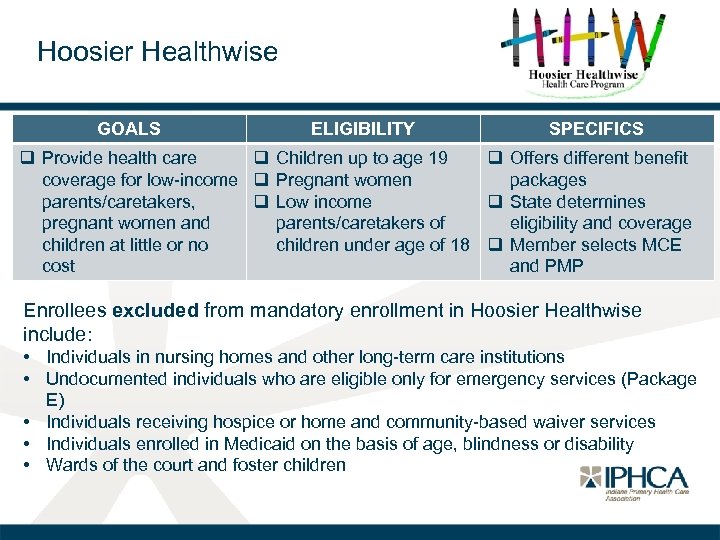
Hoosier Healthwise GOALS ELIGIBILITY SPECIFICS q Provide health care q Children up to age 19 q Offers different benefit coverage for low-income q Pregnant women packages parents/caretakers, q Low income q State determines pregnant women and parents/caretakers of eligibility and coverage children at little or no children under age of 18 q Member selects MCE cost and PMP Enrollees excluded from mandatory enrollment in Hoosier Healthwise include: • Individuals in nursing homes and other long-term care institutions • Undocumented individuals who are eligible only for emergency services (Package E) • Individuals receiving hospice or home and community-based waiver services • Individuals enrolled in Medicaid on the basis of age, blindness or disability • Wards of the court and foster children
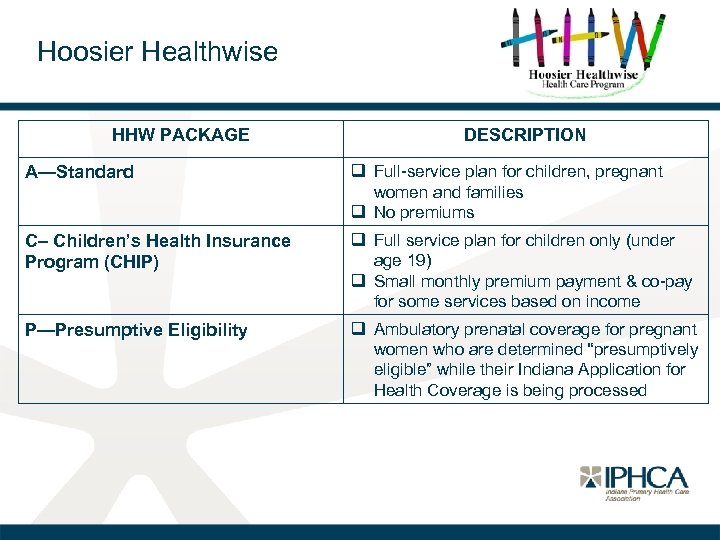
Hoosier Healthwise HHW PACKAGE DESCRIPTION A—Standard q Full-service plan for children, pregnant women and families q No premiums C– Children’s Health Insurance Program (CHIP) q Full service plan for children only (under age 19) q Small monthly premium payment & co-pay for some services based on income P—Presumptive Eligibility q Ambulatory prenatal coverage for pregnant women who are determined “presumptively eligible” while their Indiana Application for Health Coverage is being processed
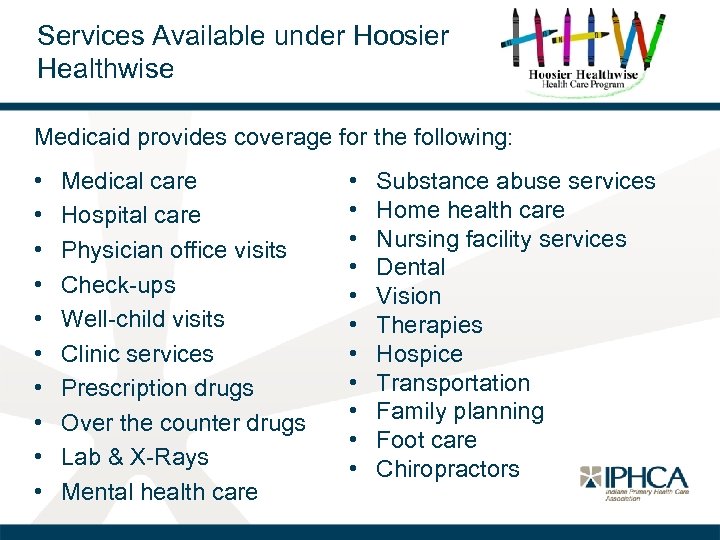
Services Available under Hoosier Healthwise Medicaid provides coverage for the following: • • • Medical care Hospital care Physician office visits Check-ups Well-child visits Clinic services Prescription drugs Over the counter drugs Lab & X-Rays Mental health care • • • Substance abuse services Home health care Nursing facility services Dental Vision Therapies Hospice Transportation Family planning Foot care Chiropractors
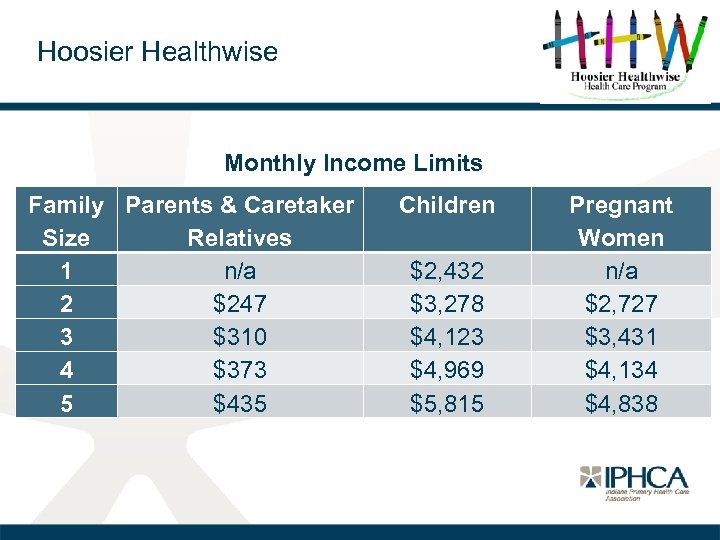
Hoosier Healthwise Monthly Income Limits Family Parents & Caretaker Size Relatives 1 n/a 2 $247 3 $310 4 $373 5 $435 Children $2, 432 $3, 278 $4, 123 $4, 969 $5, 815 Pregnant Women n/a $2, 727 $3, 431 $4, 134 $4, 838
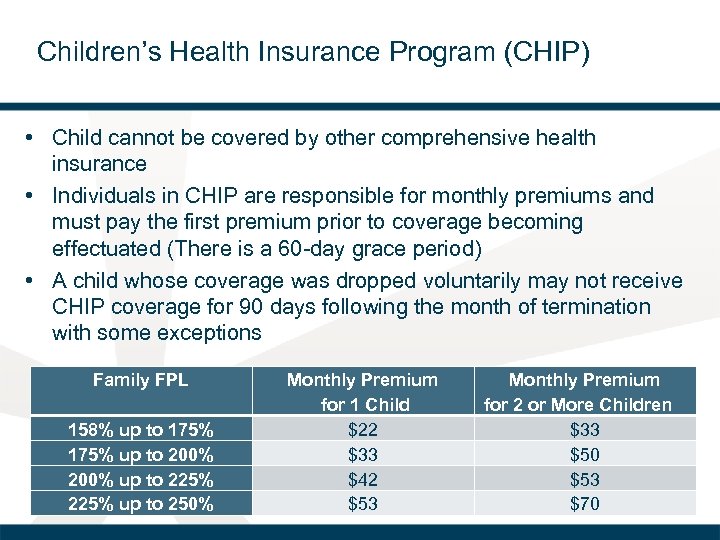
Children’s Health Insurance Program (CHIP) • Child cannot be covered by other comprehensive health insurance • Individuals in CHIP are responsible for monthly premiums and must pay the first premium prior to coverage becoming effectuated (There is a 60 -day grace period) • A child whose coverage was dropped voluntarily may not receive CHIP coverage for 90 days following the month of termination with some exceptions Family FPL 158% up to 175% up to 200% up to 225% up to 250% Monthly Premium for 1 Child $22 $33 $42 $53 Monthly Premium for 2 or More Children $33 $50 $53 $70
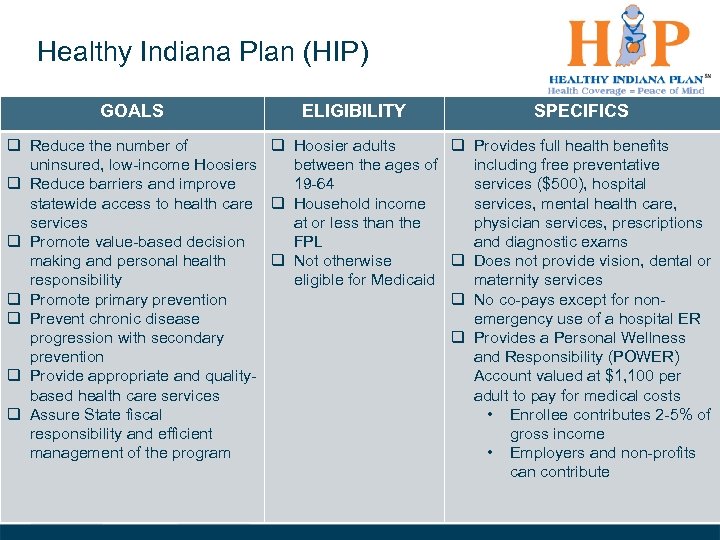
Healthy Indiana Plan (HIP) GOALS ELIGIBILITY SPECIFICS q Reduce the number of q Hoosier adults q Provides full health benefits uninsured, low-income Hoosiers between the ages of including free preventative q Reduce barriers and improve 19 -64 services ($500), hospital statewide access to health care q Household income services, mental health care, services at or less than the physician services, prescriptions q Promote value-based decision FPL and diagnostic exams making and personal health q Not otherwise q Does not provide vision, dental or responsibility eligible for Medicaid maternity services q Promote primary prevention q No co-pays except for nonq Prevent chronic disease emergency use of a hospital ER progression with secondary q Provides a Personal Wellness prevention and Responsibility (POWER) q Provide appropriate and quality. Account valued at $1, 100 per based health care services adult to pay for medical costs q Assure State fiscal • Enrollee contributes 2 -5% of responsibility and efficient gross income management of the program • Employers and non-profits can contribute
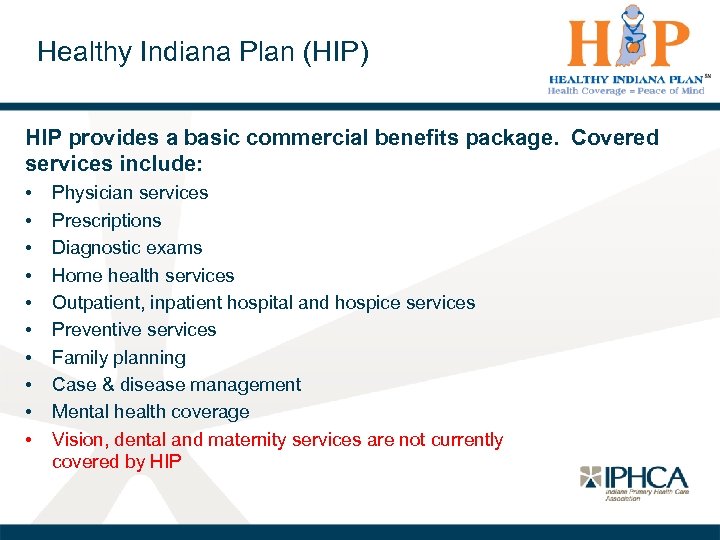
Healthy Indiana Plan (HIP) HIP provides a basic commercial benefits package. Covered services include: • • • Physician services Prescriptions Diagnostic exams Home health services Outpatient, inpatient hospital and hospice services Preventive services Family planning Case & disease management Mental health coverage Vision, dental and maternity services are not currently covered by HIP
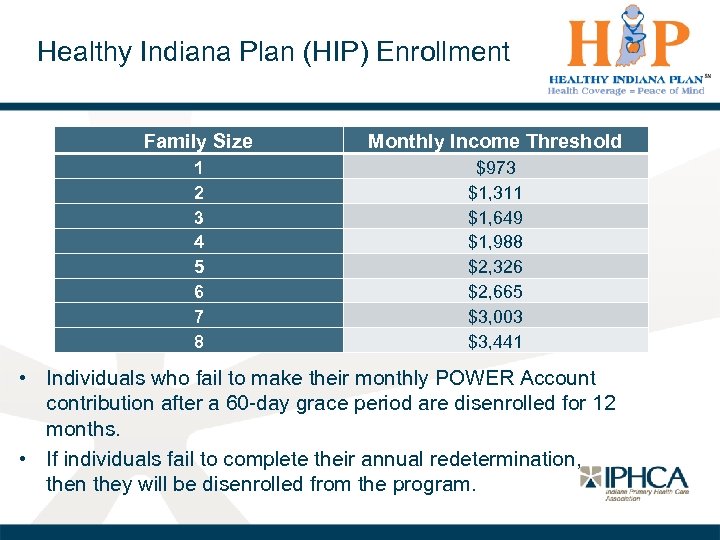
Healthy Indiana Plan (HIP) Enrollment Family Size Monthly Income Threshold 1 2 3 4 5 6 7 8 $973 $1, 311 $1, 649 $1, 988 $2, 326 $2, 665 $3, 003 $3, 441 • Individuals who fail to make their monthly POWER Account contribution after a 60 -day grace period are disenrolled for 12 months. • If individuals fail to complete their annual redetermination, then they will be disenrolled from the program.
Healthy Indiana Plan (HIP) Key Dates • In September 2013, the State received authorization from CMS to continue the HIP program for one year (through December 31, 2014). • Due to problems with the roll-out of the federal marketplace, HIP eligibility was extended to those over 100% FPL (including the 5% disregard) through April 2014 to allow for transition to the Marketplace. • On May 15, 2014, Indiana Governor Mike Pence announced a plan to expand HIP from 100% to 138% of the FPL. – As of July 2014, Indiana has submitted the HIP 2. 0 waiver application to CMS for approval
Managed Care Entities (MCEs) • MCEs provide the following services and functions to Hoosier Healthwise & HIP enrollees: – – – Case management and disease management Member services helpline Screening enrollees for special health care needs 24 -hour Nurse Call Line Managing grievances and appeals Provide member handbooks • Hoosier Healthwise & HIP enrollees select one of the three MCEs (Anthem, MDWise, MHS), or they are auto-assigned 14 days after enrollment
Managed Care Entities (MCEs) Some factors for beneficiaries to consider when selecting an MCE include the following: o Provider network • Is the individual’s doctor available in the MCE network? • Are the locations of network providers easily accessible for the enrollee? • Are the locations convenient to the individual’s work, home or school? o Special programs & enhanced services • Is there a service or program offered by the MCE that is particularly important or attractive to the enrollee?
Managed Care Entities (MCEs) Hoosier Healthwise enrollees can change HIP enrollees can change MCE: q In the first 60 days or until they q Anytime during the first 90 days with a make the first POWER Account health plan contribution q Annually during an open enrollment period q Annually at eligibility q Anytime when there is a “just cause” redetermination q Lack of access to medically necessary q Anytime there is a “just cause” as services covered under the MCE’s outlined for Hoosier Healthwise contract with State enrollees q The MCE does not, for moral or religious objections, cover the service the enrollee seeks q Lack of access to experienced providers q Poor quality of care q Enrollee needs related services performed that are not all available under the MCE network
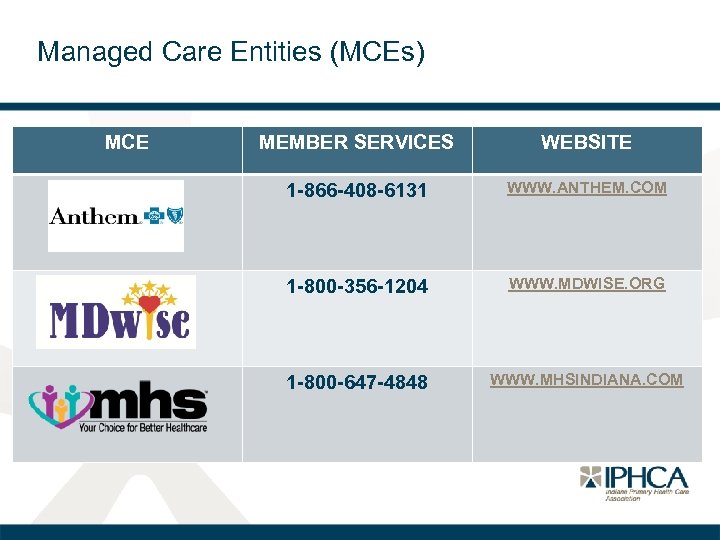
Managed Care Entities (MCEs) MCE MEMBER SERVICES WEBSITE 1 -866 -408 -6131 WWW. ANTHEM. COM 1 -800 -356 -1204 WWW. MDWISE. ORG 1 -800 -647 -4848 WWW. MHSINDIANA. COM
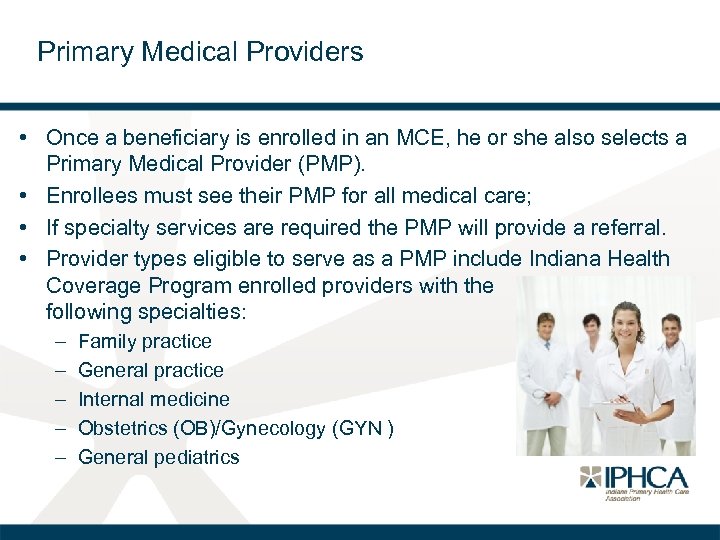
Primary Medical Providers • Once a beneficiary is enrolled in an MCE, he or she also selects a Primary Medical Provider (PMP). • Enrollees must see their PMP for all medical care; • If specialty services are required the PMP will provide a referral. • Provider types eligible to serve as a PMP include Indiana Health Coverage Program enrolled providers with the following specialties: – – – Family practice General practice Internal medicine Obstetrics (OB)/Gynecology (GYN ) General pediatrics
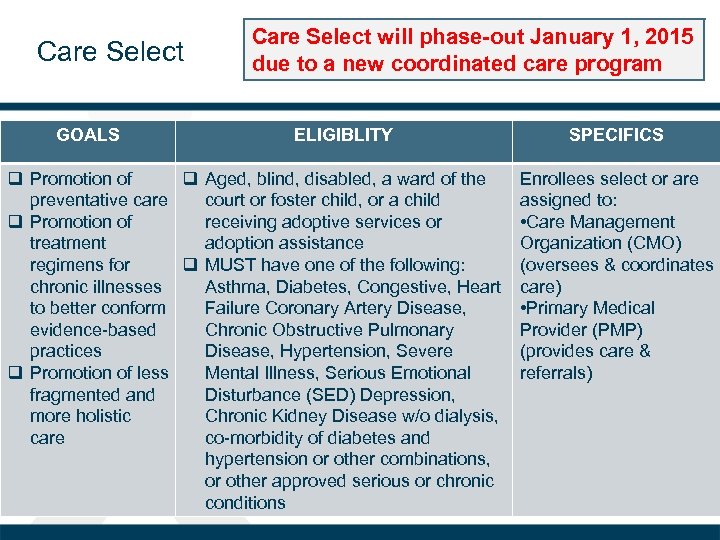
Care Select GOALS Care Select will phase-out January 1, 2015 due to a new coordinated care program ELIGIBLITY q Promotion of q Aged, blind, disabled, a ward of the preventative care court or foster child, or a child q Promotion of receiving adoptive services or treatment adoption assistance regimens for q MUST have one of the following: chronic illnesses Asthma, Diabetes, Congestive, Heart to better conform Failure Coronary Artery Disease, evidence-based Chronic Obstructive Pulmonary practices Disease, Hypertension, Severe q Promotion of less Mental Illness, Serious Emotional fragmented and Disturbance (SED) Depression, more holistic Chronic Kidney Disease w/o dialysis, care co-morbidity of diabetes and hypertension or other combinations, or other approved serious or chronic conditions SPECIFICS Enrollees select or are assigned to: • Care Management Organization (CMO) (oversees & coordinates care) • Primary Medical Provider (PMP) (provides care & referrals)
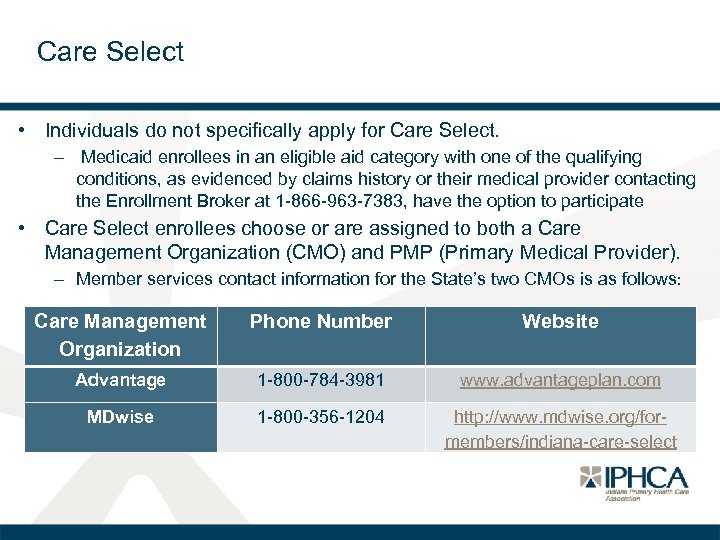
Care Select • Individuals do not specifically apply for Care Select. – Medicaid enrollees in an eligible aid category with one of the qualifying conditions, as evidenced by claims history or their medical provider contacting the Enrollment Broker at 1 -866 -963 -7383, have the option to participate • Care Select enrollees choose or are assigned to both a Care Management Organization (CMO) and PMP (Primary Medical Provider). – Member services contact information for the State’s two CMOs is as follows: Care Management Organization Phone Number Website Advantage 1 -800 -784 -3981 www. advantageplan. com MDwise 1 -800 -356 -1204 http: //www. mdwise. org/formembers/indiana-care-select
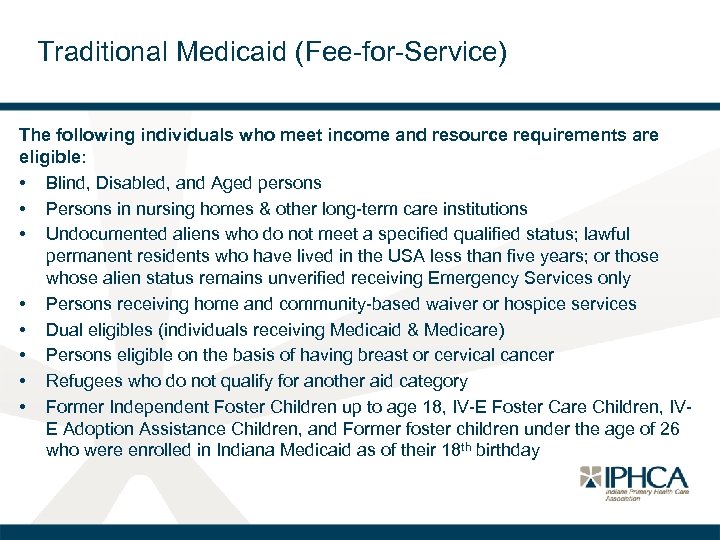
Traditional Medicaid (Fee-for-Service) The following individuals who meet income and resource requirements are eligible: • Blind, Disabled, and Aged persons • Persons in nursing homes & other long-term care institutions • Undocumented aliens who do not meet a specified qualified status; lawful permanent residents who have lived in the USA less than five years; or those whose alien status remains unverified receiving Emergency Services only • Persons receiving home and community-based waiver or hospice services • Dual eligibles (individuals receiving Medicaid & Medicare) • Persons eligible on the basis of having breast or cervical cancer • Refugees who do not qualify for another aid category • Former Independent Foster Children up to age 18, IV-E Foster Care Children, IVE Adoption Assistance Children, and Former foster children under the age of 26 who were enrolled in Indiana Medicaid as of their 18 th birthday
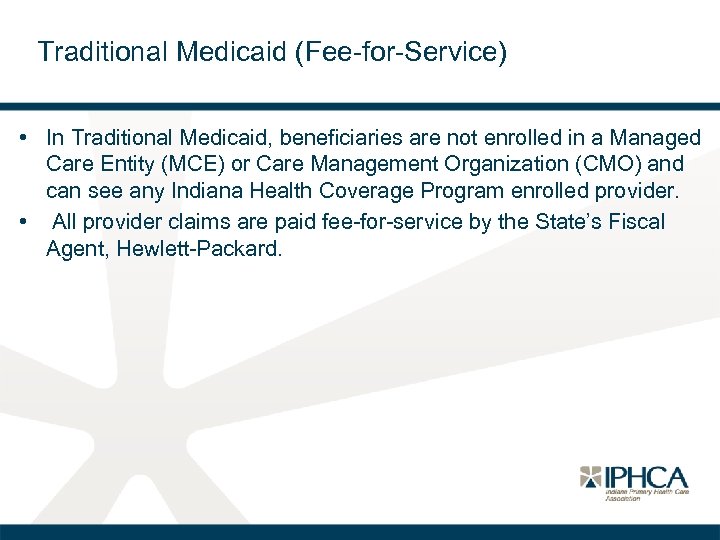
Traditional Medicaid (Fee-for-Service) • In Traditional Medicaid, beneficiaries are not enrolled in a Managed Care Entity (MCE) or Care Management Organization (CMO) and can see any Indiana Health Coverage Program enrolled provider. • All provider claims are paid fee-for-service by the State’s Fiscal Agent, Hewlett-Packard.
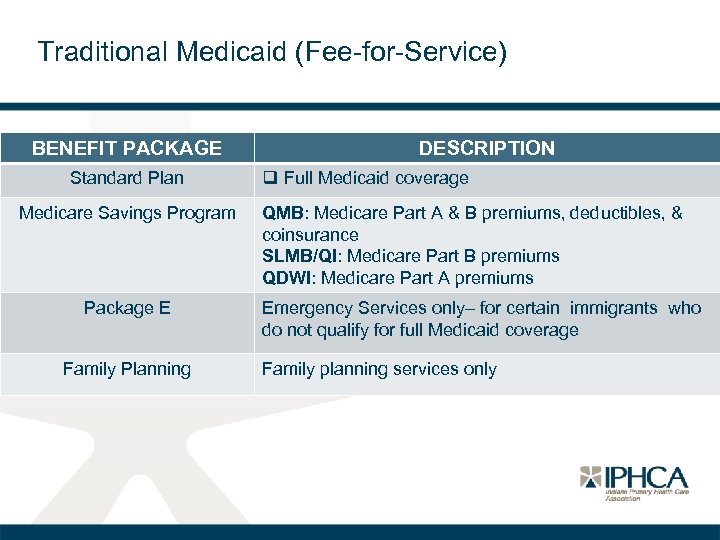
Traditional Medicaid (Fee-for-Service) BENEFIT PACKAGE Standard Plan Medicare Savings Program Package E Family Planning DESCRIPTION q Full Medicaid coverage QMB: Medicare Part A & B premiums, deductibles, & coinsurance SLMB/QI: Medicare Part B premiums QDWI: Medicare Part A premiums Emergency Services only– for certain immigrants who do not qualify for full Medicaid coverage Family planning services only
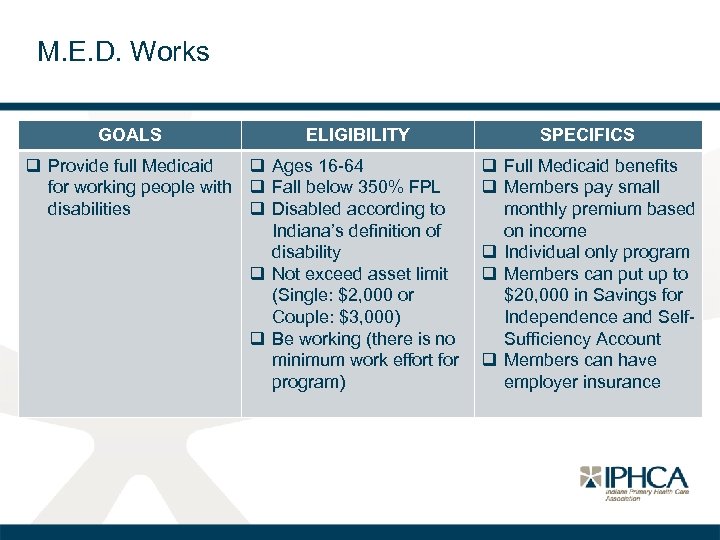
M. E. D. Works GOALS ELIGIBILITY q Provide full Medicaid q Ages 16 -64 for working people with q Fall below 350% FPL disabilities q Disabled according to Indiana’s definition of disability q Not exceed asset limit (Single: $2, 000 or Couple: $3, 000) q Be working (there is no minimum work effort for program) SPECIFICS q Full Medicaid benefits q Members pay small monthly premium based on income q Individual only program q Members can put up to $20, 000 in Savings for Independence and Self. Sufficiency Account q Members can have employer insurance
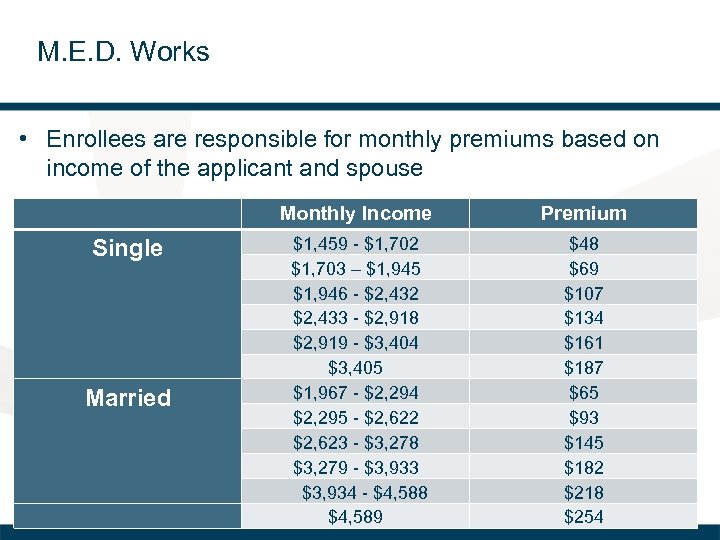
M. E. D. Works • Enrollees are responsible for monthly premiums based on income of the applicant and spouse Monthly Income Premium Single $1, 459 - $1, 702 $1, 703 – $1, 945 $1, 946 - $2, 432 $2, 433 - $2, 918 $2, 919 - $3, 404 $3, 405 $1, 967 - $2, 294 $2, 295 - $2, 622 $2, 623 - $3, 278 $3, 279 - $3, 933 $3, 934 - $4, 588 $4, 589 $48 $69 $107 $134 $161 $187 $65 $93 $145 $182 $218 $254 Married
590 Program • Provides coverage for residents of state-owned facilities • Does not cover incarcerated individuals residing in Department of Corrections (DOC) facilities • Eligible for Package A benefits with the exception of transportation
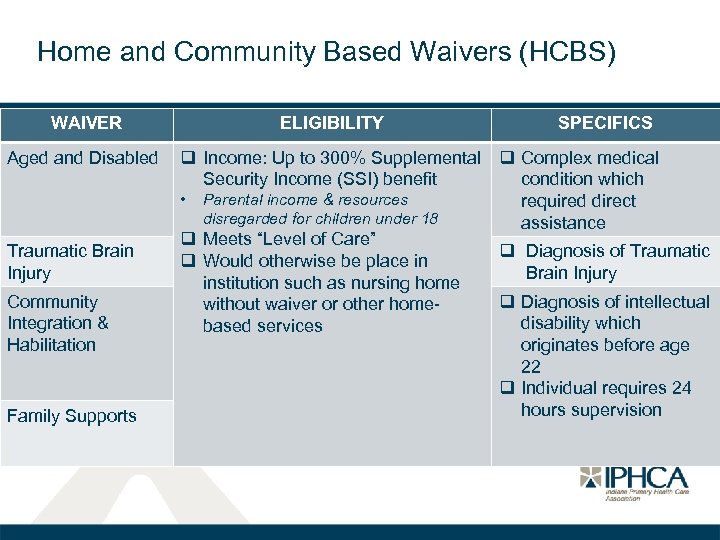
Home and Community Based Waivers (HCBS) WAIVER ELIGIBILITY SPECIFICS Aged and Disabled q Income: Up to 300% Supplemental q Complex medical Security Income (SSI) benefit condition which • Parental income & resources required direct disregarded for children under 18 assistance q Meets “Level of Care” Traumatic Brain q Diagnosis of Traumatic q Would otherwise be place in Injury Brain Injury institution such as nursing home Community q Diagnosis of intellectual without waiver or other home. Integration & disability which based services Habilitation originates before age 22 q Individual requires 24 hours supervision Family Supports
Home and Community Based Waivers (HCBS) • To apply for the Aged and Disabled waiver or the Traumatic Brain Injury Waiver, individuals can go the local Area Agencies on Aging (AAA) or call 1 -800 -986 -3505 for more information. • To apply for the Community Integration & Habilitation or Family Supports waiver, individuals can go the local Bureau of Developmental Disabilities Services (BDDS) office or call 1 -800545 -7763 for more information. • There are currently waiting lists for the Family Supports waiver and the Traumatic Brain Injury waiver.
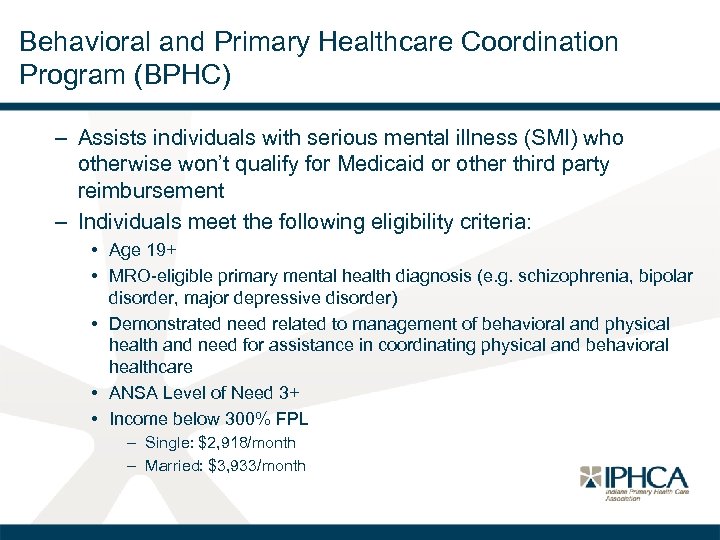
Behavioral and Primary Healthcare Coordination Program (BPHC) – Assists individuals with serious mental illness (SMI) who otherwise won’t qualify for Medicaid or other third party reimbursement – Individuals meet the following eligibility criteria: • Age 19+ • MRO-eligible primary mental health diagnosis (e. g. schizophrenia, bipolar disorder, major depressive disorder) • Demonstrated need related to management of behavioral and physical health and need for assistance in coordinating physical and behavioral healthcare • ANSA Level of Need 3+ • Income below 300% FPL – Single: $2, 918/month – Married: $3, 933/month
Behavioral and Primary Healthcare Coordination Program (BPHC) • Individuals may apply for the BPHC program through a Community Mental Health Center (CMHC) approved by the FSSA Division of Mental Health and Addiction (DMHA) as a BPHC provider. • A list of approved CMHCs can be found at http: //www. indianamedicaid. com/ihcp/Provider. Services/Pr ovider. Search. aspx.
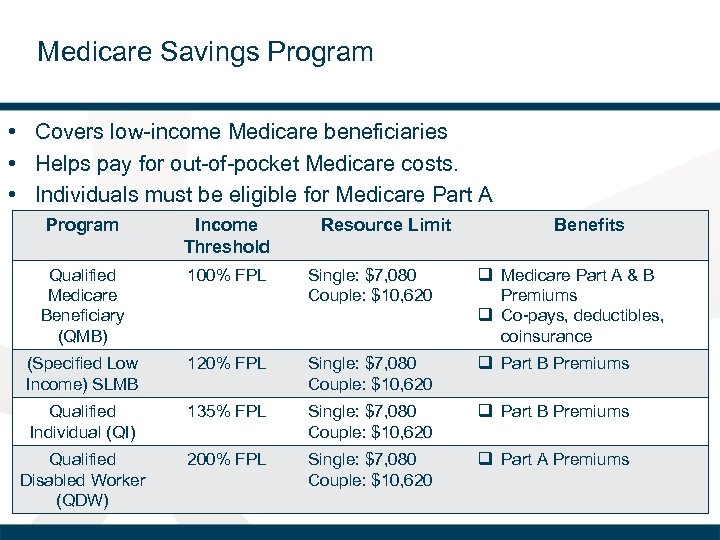
Medicare Savings Program • Covers low-income Medicare beneficiaries • Helps pay for out-of-pocket Medicare costs. • Individuals must be eligible for Medicare Part A Program Income Threshold Resource Limit Benefits Qualified Medicare Beneficiary (QMB) 100% FPL Single: $7, 080 Couple: $10, 620 q Medicare Part A & B Premiums q Co-pays, deductibles, coinsurance (Specified Low Income) SLMB 120% FPL Single: $7, 080 Couple: $10, 620 q Part B Premiums Qualified Individual (QI) 135% FPL Single: $7, 080 Couple: $10, 620 q Part B Premiums Qualified Disabled Worker (QDW) 200% FPL Single: $7, 080 Couple: $10, 620 q Part A Premiums
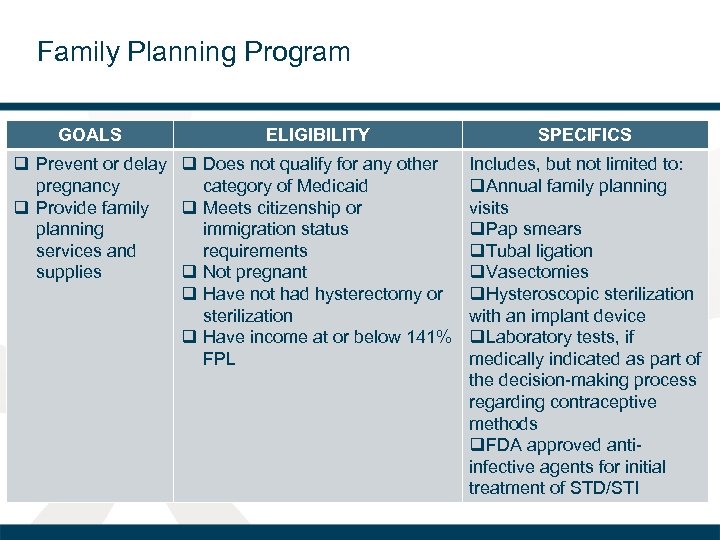
Family Planning Program GOALS ELIGIBILITY q Prevent or delay q Does not qualify for any other pregnancy category of Medicaid q Provide family q Meets citizenship or planning immigration status services and requirements supplies q Not pregnant q Have not had hysterectomy or sterilization q Have income at or below 141% FPL SPECIFICS Includes, but not limited to: q. Annual family planning visits q. Pap smears q. Tubal ligation q. Vasectomies q. Hysteroscopic sterilization with an implant device q. Laboratory tests, if medically indicated as part of the decision-making process regarding contraceptive methods q. FDA approved antiinfective agents for initial treatment of STD/STI
Family Planning Program Services not covered: • Abortions • Artificial insemination • IVF, fertility counseling or fertility drugs • Inpatient hospital stays • Treatment for any chronic condition Individuals must request to be considered for this program on their Indiana Application for Health Coverage if not eligible for full Medicaid benefits
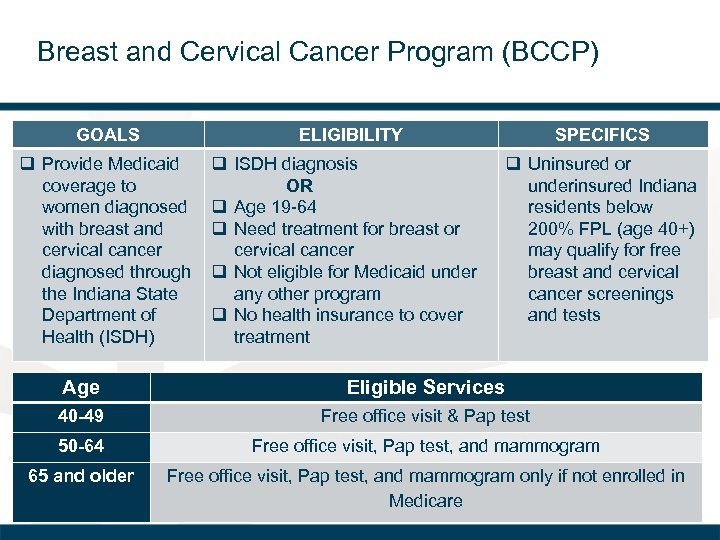
Breast and Cervical Cancer Program (BCCP) GOALS ELIGIBILITY q Provide Medicaid coverage to women diagnosed with breast and cervical cancer diagnosed through the Indiana State Department of Health (ISDH) q ISDH diagnosis OR q Age 19 -64 q Need treatment for breast or cervical cancer q Not eligible for Medicaid under any other program q No health insurance to cover treatment SPECIFICS q Uninsured or underinsured Indiana residents below 200% FPL (age 40+) may qualify for free breast and cervical cancer screenings and tests Age Eligible Services 40 -49 Free office visit & Pap test 50 -64 Free office visit, Pap test, and mammogram 65 and older Free office visit, Pap test, and mammogram only if not enrolled in Medicare
Presumptive Eligibility (PE) • Allows individuals meeting eligibility requirements access to services covered and paid for by Medicaid as they wait for their application determination for full Medicaid • Entails a simplified application process: – Applicant must know gross family income & citizenship status – Verification documents not required—applicant attests to information
Presumptive Eligibility (PE) • The PE period extends from the date an individual is determined presumptively eligible until… – When an Indiana Application for Health Coverage is filed: • Day on which a decision is made on that application – When an Indiana Application for Health Coverage is not filed: • Last day of the month following the month in which the PE determination was made
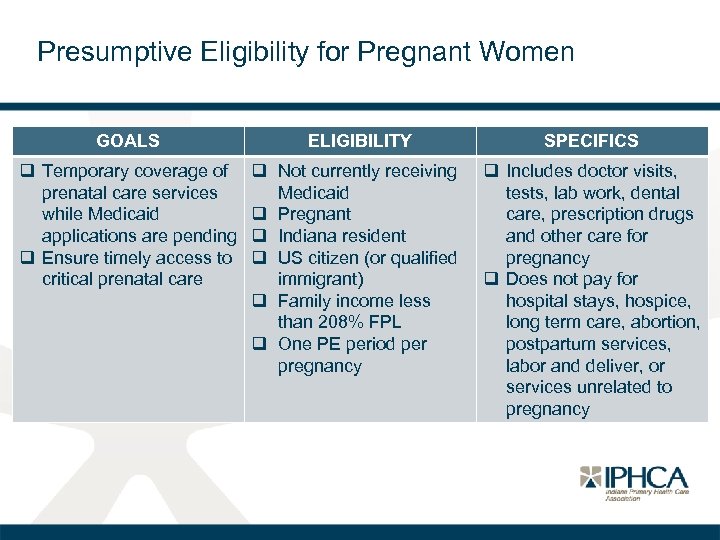
Presumptive Eligibility for Pregnant Women GOALS ELIGIBILITY SPECIFICS q Temporary coverage of prenatal care services while Medicaid applications are pending q Ensure timely access to critical prenatal care q Not currently receiving Medicaid q Pregnant q Indiana resident q US citizen (or qualified immigrant) q Family income less than 208% FPL q One PE period per pregnancy q Includes doctor visits, tests, lab work, dental care, prescription drugs and other care for pregnancy q Does not pay for hospital stays, hospice, long term care, abortion, postpartum services, labor and deliver, or services unrelated to pregnancy
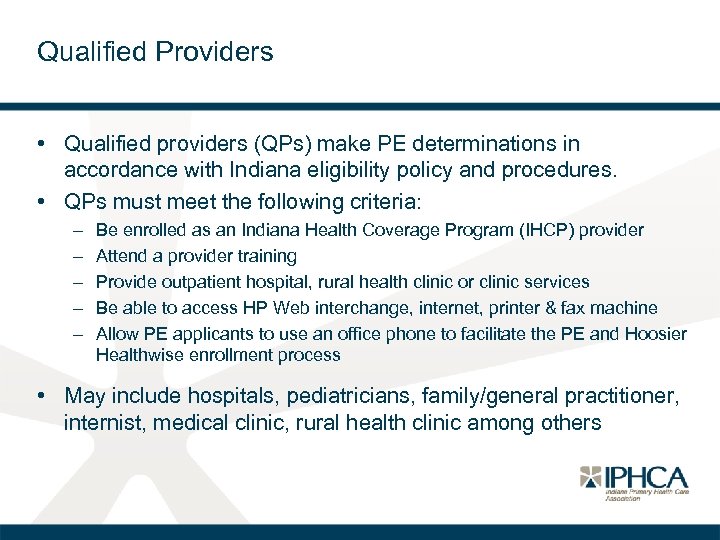
Qualified Providers • Qualified providers (QPs) make PE determinations in accordance with Indiana eligibility policy and procedures. • QPs must meet the following criteria: – – – Be enrolled as an Indiana Health Coverage Program (IHCP) provider Attend a provider training Provide outpatient hospital, rural health clinic or clinic services Be able to access HP Web interchange, internet, printer & fax machine Allow PE applicants to use an office phone to facilitate the PE and Hoosier Healthwise enrollment process • May include hospitals, pediatricians, family/general practitioner, internist, medical clinic, rural health clinic among others
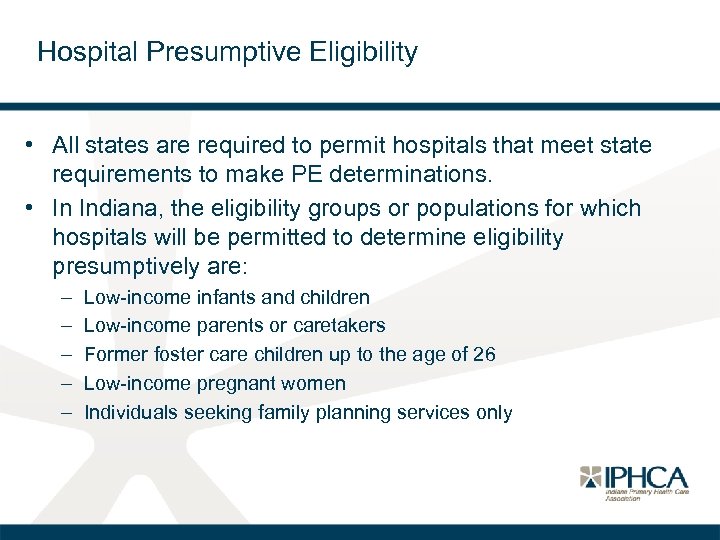
Hospital Presumptive Eligibility • All states are required to permit hospitals that meet state requirements to make PE determinations. • In Indiana, the eligibility groups or populations for which hospitals will be permitted to determine eligibility presumptively are: – – – Low-income infants and children Low-income parents or caretakers Former foster care children up to the age of 26 Low-income pregnant women Individuals seeking family planning services only
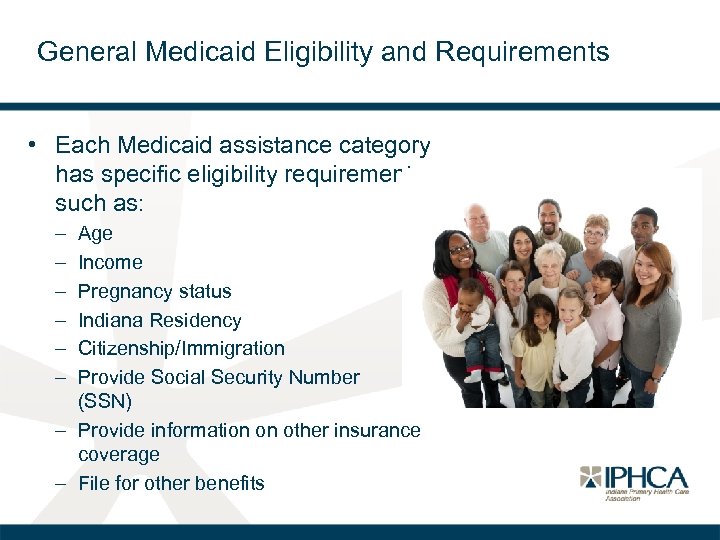
General Medicaid Eligibility and Requirements • Each Medicaid assistance category has specific eligibility requirements such as: – – – Age Income Pregnancy status Indiana Residency Citizenship/Immigration Provide Social Security Number (SSN) – Provide information on other insurance coverage – File for other benefits
Requirement: Residency • Applicant must be resident of the state • State of residency is: – Where individual lives – Including without a fixed address OR – Has entered the state with a job commitment OR seeking employment • A homeless individual or residents of shelters in Indiana meet this requirement • There is no minimum time period for state residency to be Medicaid eligible • Individuals are permitted to be temporarily absent from the state without losing eligibility
Requirement: Citizenship/Immigration Status • Individual must be US citizen, a US non-citizen national or an immigrant who is in a qualified immigration status o Lawful permanent residents are eligible for full Medicaid after 5 years • Electronic data sources through the Federal Hub verify status o If not, paper documentation is required, and a “reasonable opportunity” period is granted to otherwise Medicaid eligible individuals– this period lasts 90 days from the date on the eligibility notice • Those exempt from citizenship verification process: Individuals receiving SSI or SSDI Individuals enrolled in Medicare Individuals in foster care & who are assisted under Title IV-B Individuals who are beneficiaries of foster care maintenance or adoption assistance payments under Title IV-E o Newborns born to a Medicaid enrolled mother o o
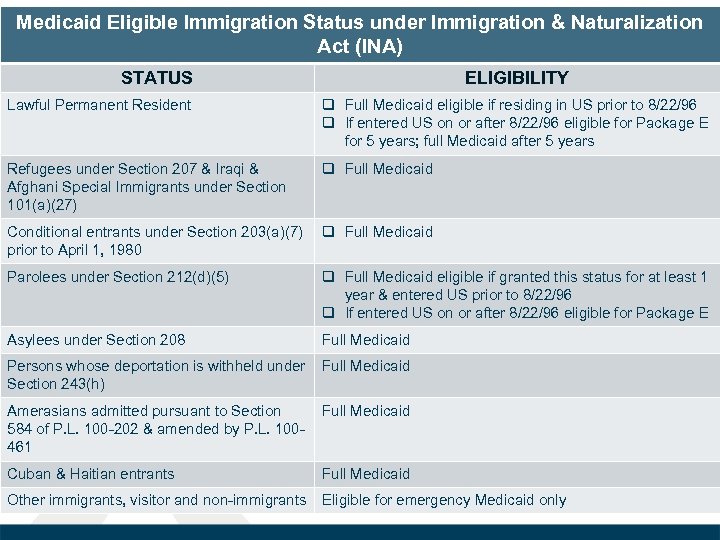
Medicaid Eligible Immigration Status under Immigration & Naturalization Act (INA) STATUS ELIGIBILITY Lawful Permanent Resident q Full Medicaid eligible if residing in US prior to 8/22/96 q If entered US on or after 8/22/96 eligible for Package E for 5 years; full Medicaid after 5 years Refugees under Section 207 & Iraqi & Afghani Special Immigrants under Section 101(a)(27) q Full Medicaid Conditional entrants under Section 203(a)(7) q Full Medicaid prior to April 1, 1980 Parolees under Section 212(d)(5) q Full Medicaid eligible if granted this status for at least 1 year & entered US prior to 8/22/96 q If entered US on or after 8/22/96 eligible for Package E Asylees under Section 208 Full Medicaid Persons whose deportation is withheld under Full Medicaid Section 243(h) Amerasians admitted pursuant to Section 584 of P. L. 100 -202 & amended by P. L. 100461 Full Medicaid Cuban & Haitian entrants Full Medicaid Other immigrants, visitor and non-immigrants Eligible for emergency Medicaid only
Requirement: Provide Social Security Number • Each Medicaid applicant must supply social security number (SSN) with the following exceptions: q Individual ineligible to receive SSN q Individual does not have SSN and may only be issued one for a valid non-work reasons q Individual refuses to obtain one due to well-established religious objections q Individual is only eligible for emergency services due to immigration status q Individual is a deemed newborn q Individual is receiving Refugee Cash Assistance and is eligible for Medicaid q Individual has already applied for SSN
Requirement: File for Other Benefits • Individuals must apply for all other benefits for which they may be eligible as a condition of eligibility unless good cause can be show for not doing so; these include: – – – – – Pensions from local, state or federal government Retirement benefits Disability Social Security benefits Veterans’ benefits Unemployment compensation benefits Military benefits Railroad retirement benefits Workers’ Compensation benefits Health and accident insurance payments
Requirement: Report and Use Other Insurance • Medicaid enrollees can have access to other insurance (third liability); however… – Individuals cannot have other insurance and enroll in CHIP or HIP – Applicants must provide information on other insurance they have or change in insurance status – Medicaid is the payer of last resort– other insurance is the primary payer
Modified Adjusted Gross Income (MAGI) • Methodology for income counting and determining household size and composition • Used to determine eligibility for Indiana Health Coverage Programs (IHCP) and tax credits on the Marketplace • Not counted toward income: • Assets such as homes, stocks or retirement account • Scholarships, awards or fellowships not used toward living expenses • Income disregards (except tax deductions) and nontaxable income • Child support received, Worker’s compensation and Veteran’s benefits
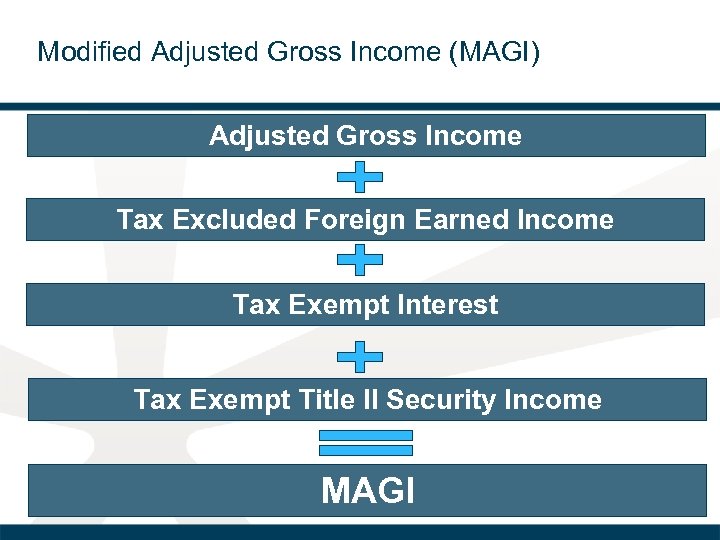
Modified Adjusted Gross Income (MAGI) Adjusted Gross Income Tax Excluded Foreign Earned Income Tax Exempt Interest Tax Exempt Title II Security Income MAGI
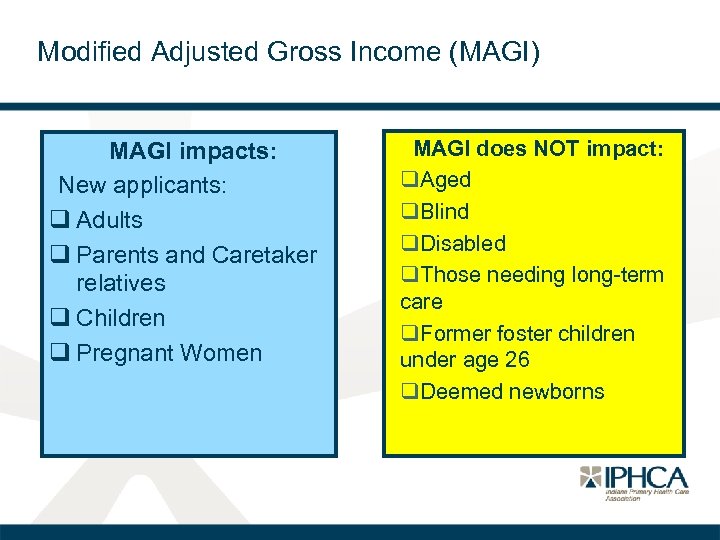
Modified Adjusted Gross Income (MAGI) MAGI impacts: New applicants: q Adults q Parents and Caretaker relatives q Children q Pregnant Women MAGI does NOT impact: q. Aged q. Blind q. Disabled q. Those needing long-term care q. Former foster children under age 26 q. Deemed newborns
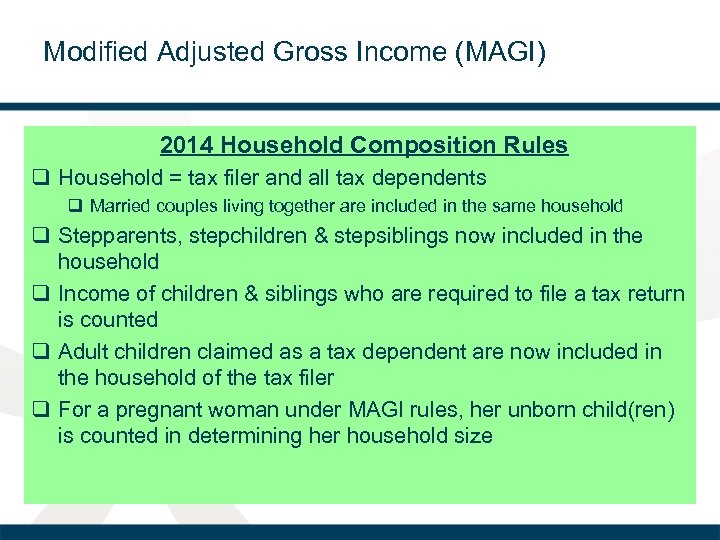
Modified Adjusted Gross Income (MAGI) 2014 Household Composition Rules q Household = tax filer and all tax dependents q Married couples living together are included in the same household q Stepparents, stepchildren & stepsiblings now included in the household q Income of children & siblings who are required to file a tax return is counted q Adult children claimed as a tax dependent are now included in the household of the tax filer q For a pregnant woman under MAGI rules, her unborn child(ren) is counted in determining her household size
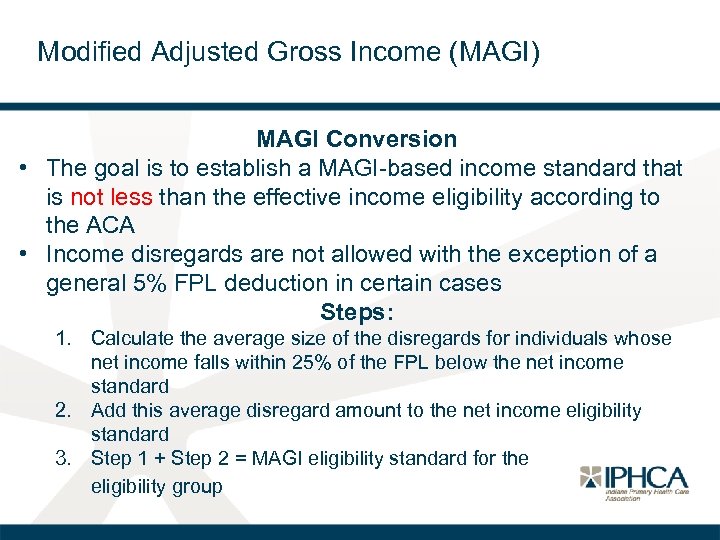
Modified Adjusted Gross Income (MAGI) MAGI Conversion • The goal is to establish a MAGI-based income standard that is not less than the effective income eligibility according to the ACA • Income disregards are not allowed with the exception of a general 5% FPL deduction in certain cases Steps: 1. Calculate the average size of the disregards for individuals whose net income falls within 25% of the FPL below the net income standard 2. Add this average disregard amount to the net income eligibility standard 3. Step 1 + Step 2 = MAGI eligibility standard for the eligibility group
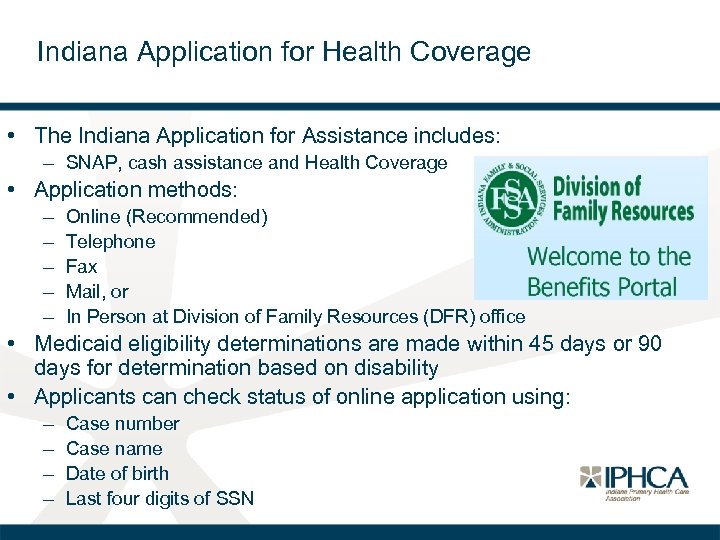
Indiana Application for Health Coverage • The Indiana Application for Assistance includes: – SNAP, cash assistance and Health Coverage • Application methods: – – – Online (Recommended) Telephone Fax Mail, or In Person at Division of Family Resources (DFR) office • Medicaid eligibility determinations are made within 45 days or 90 days for determination based on disability • Applicants can check status of online application using: – – Case number Case name Date of birth Last four digits of SSN
Authorized Representatives • Individual or organization which acts on a Medicaid applicant or beneficiary’s behalf in assisting with the application, redetermination process and ongoing communications with the state • Commonly a trusted family member, but can also be a third party entity • Designation must be in writing and signed by the applicant or beneficiary and the authorized representative – State Form 55366 can be used
Verifying Factors of Eligibility • States only permitted to collect paper documentation from Medicaid applicants when electronic data sources are not available or reasonably compatible • Data sources used to verify: – – – Social Security Administration Department of Homeland Security TALX Work Number State Wage Information Collection Agency State Unemployment Compensation Vital Statistics
Eligibility Notices • DFR provides written notice, via mail, to applications and beneficiaries regarding any decision affecting eligibility • Types of notices include, but not limited to: o o o Approvals Denials Terminations Suspensions of eligibility Changes in benefit package or aid category
Eligibility Notices What to expect with eligibility notices: • State sends notice within 24 hours + mailing time • Member ID card, referred to as the Hoosier Health Card, sent within 5 business days + mailing time – HIP enrollees receive member ID card from their MCE – CHIP & M. E. D. Works receive premium invoices – HIP eligible individuals receive POWER Account contribution notices • Individuals can be determined Medicaid eligible for up to 3 months of retroactive eligibility from the date of application – Does not apply to HIP or CHIP
Eligibility Appeals • Individuals wishing to challenge disability eligibility decisions appeal to the Social Security Administration (SSA) or Indiana Medicaid depending on the reason for the denial. – Regarding an SSA disability on file: appeal to SSA – Indiana Medical Review Team (MRT) decision: Indiana Medicaid
Eligibility Redeterminations • Conducted every 12 months for MAGI categories – The State renews if there is sufficient information, effective December 2014 – If there is not sufficient information, a pre-populated renewal form will be sent beginning in 2015 • Eligibility is terminated if the form is not submitted in a timely manner • If eligibility is terminated but the documents are submitted within 90 days of the original due date, the documents will be reviewed without the need to submit a new application • An individual enrolled in Medicaid on or before December 31, 2013 cannot be denied Medicaid eligibility solely because of the implementation of MAGI rules before March 31, 2014
Reporting Changes • Enrollees are required to report changes to the state (FSSA) • Examples of changes include: – – Change in address Income Family composition Babies born to Medicaid enrollees receive coverage for the first year of life without the need for a separate application • They will be covered under Hoosier Healthwise and enrolled in the mother’s Managed Care Entity (MCE)
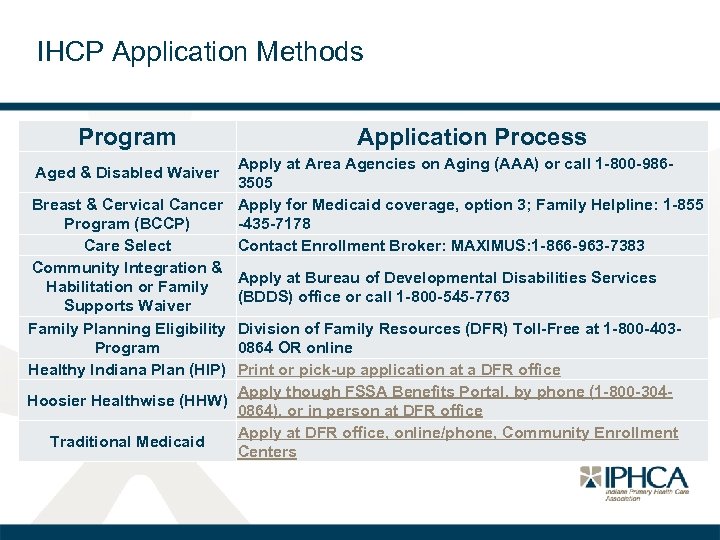
IHCP Application Methods Program Application Process Apply at Area Agencies on Aging (AAA) or call 1 -800 -9863505 Breast & Cervical Cancer Apply for Medicaid coverage, option 3; Family Helpline: 1 -855 Program (BCCP) -435 -7178 Care Select Contact Enrollment Broker: MAXIMUS: 1 -866 -963 -7383 Community Integration & Apply at Bureau of Developmental Disabilities Services Habilitation or Family (BDDS) office or call 1 -800 -545 -7763 Supports Waiver Family Planning Eligibility Division of Family Resources (DFR) Toll-Free at 1 -800 -403 Program 0864 OR online Healthy Indiana Plan (HIP) Print or pick-up application at a DFR office Apply though FSSA Benefits Portal, by phone (1 -800 -304 Hoosier Healthwise (HHW) 0864), or in person at DFR office Apply at DFR office, online/phone, Community Enrollment Traditional Medicaid Centers Aged & Disabled Waiver
Helpful Resources • Hoosier Healthwise Helpline – 1 -800 -889 -9949 • Healthy Indiana Plan (HIP) Helpline – 1 -877 -GET-HIP-9 • FSSA Benefits Portal – Apply for cash assistance, SNAP and health coverage • Indiana Medicaid Website – Eligibility Screening Tools – Guide to programs
fa620d6b343bbfa9e74002e644b24ec1.ppt