cf44db054f7a9c3616ead83a32883ca5.ppt
- Количество слайдов: 67
Incorporating Mental Health Into Maternal Health Brian Stafford, MD, MPH Medical Director The Kempe Center’s Postpartum Depression Intervention Program CITYMATCH CONFERENCE Denver, CO Aug, 2007
Outline n n n Perinatal Mental Health and Mental Illness Barriers to Treatment Public Health’s Role Mental Health’s Role Primary Care’s Role Brian Stafford, MD, MPH
Perinatal Mental Health n n A developmental crisis A time of increased contact with Medical and Public Health but not necessarily mental health Brian Stafford, MD, MPH

Pregnancy n High Risk for Medical Complications n High Risk for Mental Health Complications Brian Stafford, MD, MPH
Examples n Most common complications of pregnancy are: Spontaneous Abortion n Postpartum Depression n Antenatal Depression n Diabetes n Prematurity n Perinatal Loss n Brian Stafford, MD, MPH
Depression World Health Organization • 2020 n depression will be 2 nd greatest cause of premature death and disability worldwide in both sexes • Already n number one cause of disease burden in women Brian Stafford, MD, MPH
Perinatal Mood Disturbance n Definitions: Antenatal Anxiety n Antenatal Depression n Postpartum Blues n Postpartum Psychosis n Postpartum Depression n Postpartum PTSD n Postpartum Anxiety n Brian Stafford, MD, MPH

“Baby Blues” n n 50 - 85% of women Hours to days after childbirth lasting up to two weeks n n Onset typically within 10 days Mild, short-lived: n • • Anger Sense of unworthiness, inadequacy, failure, guilt Crying Irritability/ Impatience Restlessness Sadness Tiredness (fatigue), Insomnia, or both Mood swings Brian Stafford, MD, MPH
Postpartum Anxiety n New Onset or Exacerbation Generalized n Panic n Phobic n Social Phobia n OCD –like n Exacerbation is worse n Preoccupation with baby n Brian Stafford, MD, MPH
Postpartum Psychosis n n n Rare - Less than 1% of women (1 -2/1000) Bipolar Disorder/ Schizophrenia/Schizoaffective Disorder/Psychotic Depression Signs and symptoms even more severe and may occur early (within first 3 months postpartum – usually first 2 weeks) • • Anger and agitation Insomnia Confusion and disorientation Thoughts of harming self (suicide) or baby (infanticide) Hallucinations and delusions Paranoia Strange thoughts or statements Brian Stafford, MD, MPH
Postpartum PTSD: Less well understood n Pregnancy and delivery and newborn period is a time of potential trauma n Pregnancy Risk to mother n Risk to baby n n Delivery Risk to mother n Risk to baby n n Congenital or other neonatal issue n (Anxiety, PTSD, Depression, Grief) Brian Stafford, MD, MPH

Postpartum Depression (PPD) n n n 10 - 20% of women Signs and symptoms more intense and longer lasting Symptoms of baby blues PLUS • Emotional numbness, feeling trapped • Fear of hurting self or baby • Impaired thinking, concentration • Lack of joy • Less interest in sex • Excessive concern/lack of concern for baby • Significant weight loss or gain • Withdrawal from family and friends “overwhelmed”, “anxious” as common descriptors Brian Stafford, MD, MPH
Postpartum Depression n Not as mild or transient as the blues Not as severely disorienting as psychosis Range of severity n Mild to Extreme Impairment The same but different n n n Co-morbidity (Anxiety) Violation of expectation Brian Stafford, MD, MPH
Major Depressive Episode n n Depressed mood Diminished interest or pleasure in everyday activities • • • n n n Insomnia or hypersomnia Significant weight loss or weight gain Fatigue or loss of energy Feelings of worthlessness or excessive or inappropriate guilt Diminished concentration or indecisiveness Recurrent thought of death, suicidal ideation, or suicide plan Impairment in functioning Five or more of these symptoms present during 2 -week period; change in previous functioning Symptoms can not be explained by another condition (substance use, medical condition) or another diagnosis (e. g. , Bereavement) (taken from criteria as outlined in DSM-IV) Brian Stafford, MD, MPH
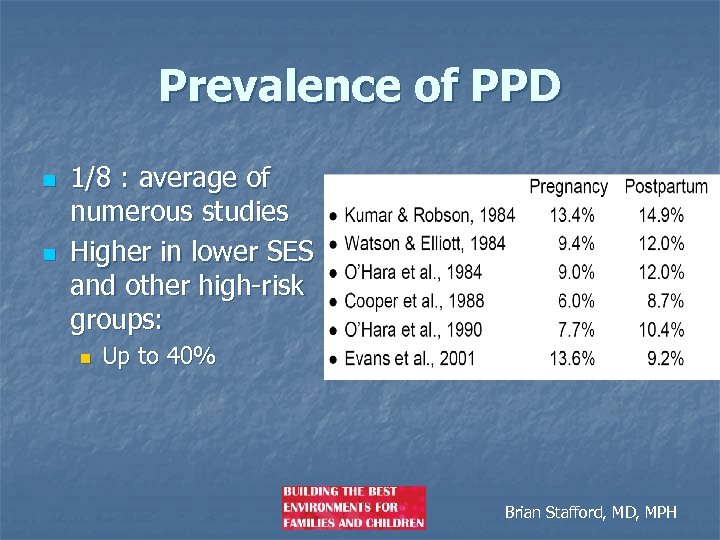
Prevalence of PPD n n 1/8 : average of numerous studies Higher in lower SES and other high-risk groups: n Up to 40% Brian Stafford, MD, MPH
Factors to Consider in Determining Risk ü ü ü ü Risk is Cumulative Additive effects ü ü Mental Health History (major depression, psychosis) Previous Pregnancy Experience Loss SES Family/ Marital Relationship Childhood Experiences Mood During Pregnancy & Post-Delivery Experience During Pregnancy/ Delivery Infant Variables Multiples Societal/Cultural Influences/ Expectations Brian Stafford, MD, MPH

Protective Factors ü ü ü ü Early Recognition and Seeking Help Previous Pregnancy Experience Peer/Marital Support Respite Care Focus on Mother Enhanced feelings of Competence SLEEP $$$$$ Brian Stafford, MD, MPH
What causes Postpartum Depression? n n n n n Hormonal Stress Loss Sleep Untreated anxiety Role transition Support Expectation Own receipt of care Personality features Brian Stafford, MD, MPH
Qualitative Experience (CT BECK) n n n n Violation of an expectation Thief that steals motherhood Horrifying Anxiety Relentless Obsessive Thinking Enveloping Fogginess Death of Self Struggle to Survive Regaining Control Brian Stafford, MD, MPH
Consequences of Postpartum Depression Maternal Consequences n n n n Suffering Lack of joy in child Missed work Suicide attempts Social Impairment Marital discord Somatic Sx Health Care Consequences n n Less frequent HSV More Urgent Care /ER Ineffective Anticipatory Guidance Behind on immunizations Brian Stafford, MD, MPH

PPD and Infant Development n PPD directly impacts the infant’s experience and may have longerterm consequences on development • • • Social Emotional Cognitive Language Attention Mother-Infant Relationship/ Interaction Brian Stafford, MD, MPH
Treatment Approaches: Biological n Biological: n Medication: n n Antidepressants Anti-anxiety n Hormone Therapy Estrogen patch Sleep Massage Exercise n Sunlight n n Brian Stafford, MD, MPH

Treatment Approaches: Psychological n Psychotherapies: Cognitive Behavioral n Interpersonal Therapy n Psychodynamic n Supportive Individual n Family n Group n DBT/EMDR n Brian Stafford, MD, MPH

Treatment Approaches: Social n Social: Family n Friends n Church n Nurse Visitors n Brian Stafford, MD, MPH

Treatment Approaches: Alternative n Alternative Narrative Journaling n Meditation n Art n Music n Brian Stafford, MD, MPH

Treatment Approaches: Integrative n Perspectives: n n Lead to treatment Bio-Psycho-Social Approach Brian Stafford, MD, MPH

Treatment Approaches n Two general approaches n n n Alleviation of maternal symptoms Improvement of mother-infant relationship Are interventions targeted only at mom enough to protect against negative child outcomes? Brian Stafford, MD, MPH
Treatment Approaches n n Studies show that individual therapies may provide significant improvement in maternal mood and stress level Little evidence that such treatments benefit infants of mothers with PPD n Lower attachment security status n Higher negative affect n More internalizing and externalizing problems Brian Stafford, MD, MPH
Treatment Approaches Are PPD interventions targeted only at mom enough to protect against negative child outcomes? Brian Stafford, MD, MPH

Dyadic Treatment Approaches n n Concept of PPD as mother-infant relationship disorder (Cramer, 1993) Dyadic therapy as preferred model for PPD treatment n Mother-infant relationship as focal point of treatment n Goal to increase maternal sensitivity, responsivity, engagement n Promote positive attachment behaviors Brian Stafford, MD, MPH
Dyadic Treatment Approaches n General Findings n n n Improved child outcomes even when maternal sx don’t improve Buffering effect against future episodes of maternal depression Those infants with dyadic PPD tx more closely resemble infants of non-depressed mothers in terms of cognitive ability Brian Stafford, MD, MPH

Integrative Approach n n n Psychiatric Evaluation Medication Management MITG: Group Therapy n n Open Groups n n n Social Support Individual therapy Family Therapy Infant Developmental Group Mother’s Group Dyadic (Mother-baby Group) Brian Stafford, MD, MPH
Step-Wise Interventions n n n Not all people need meds Not all moms need individual psychotherapy Not all moms need group psychotherapy n n n Some moms need education and have supportive adaptive environments Some moms need meds Some moms need psychotherapy Some moms need group psychotherapy Some moms need all of the above Brian Stafford, MD, MPH
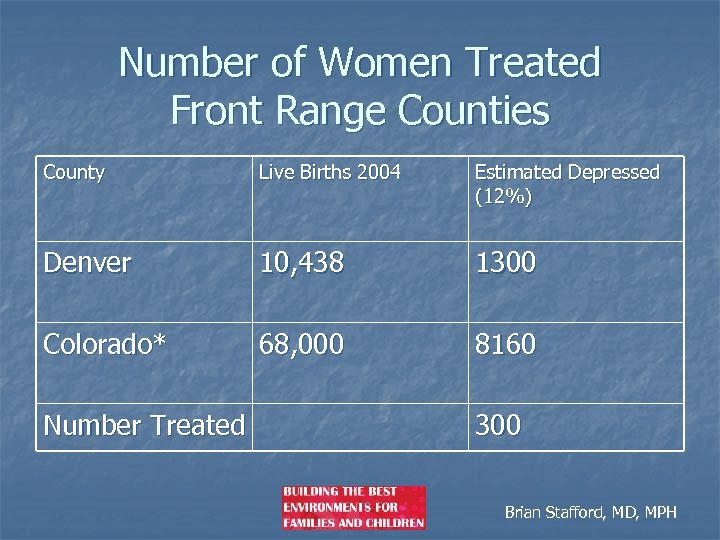
Number of Women Treated Front Range Counties County Live Births 2004 Estimated Depressed (12%) Denver 10, 438 1300 Colorado* 68, 000 8160 Number Treated 300 Brian Stafford, MD, MPH
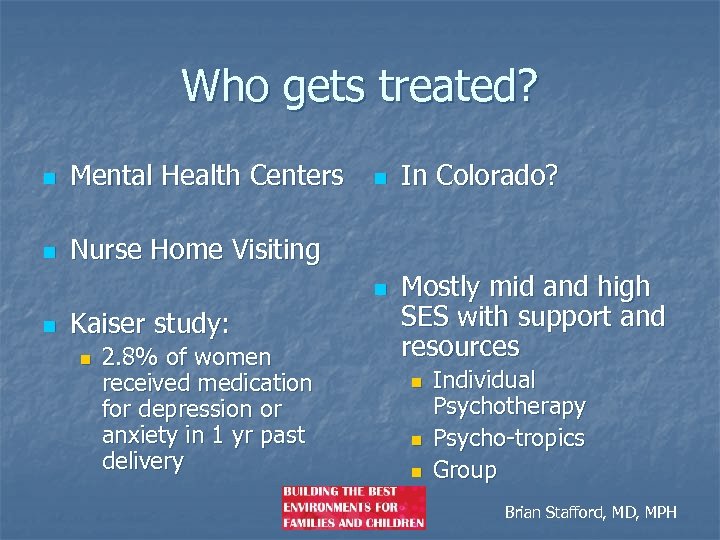
Who gets treated? n Mental Health Centers n Nurse Home Visiting n n n Kaiser study: n 2. 8% of women received medication for depression or anxiety in 1 yr past delivery In Colorado? Mostly mid and high SES with support and resources n n n Individual Psychotherapy Psycho-tropics Group Brian Stafford, MD, MPH
The FACTS: Postpartum Depression is highly prevalent n Postpartum Depression is not time-limited n Postpartum Depression is a major risk factor for an infant’s development n Postpartum Depression is highly treatable n Postpartum Depression does not get treated n Brian Stafford, MD, MPH

Barriers n n Lack of Awareness Lack of Formal Screening n Public Awareness n Professional Training n n Lack of Resources Lack of Training Mental Health Parity Satellite Support Groups n Mandatory Screening n Conference Brian Stafford, MD, MPH
Barriers to Treatment n n n Public Awareness Stigma Professional Education System Barriers Resources System Linkages Brian Stafford, MD, MPH
Barriers To Treatment n. Public Awareness and Stigma Brian Stafford, MD, MPH
The Media’s View Brian Stafford, MD, MPH
The Common View of the Postpartum Period Brian Stafford, MD, MPH
The Reality n n n n Tired Alone at home Most friends are at work Lots of care for baby Little time for self Lack of sleep Overwhelmed Brian Stafford, MD, MPH
Barriers to Treatment Professional Training and Practice - - lack of primary care identification lack of professional awareness of condition lack of expertise in perinatal and infant mental health issues lack of awareness regarding psychopharmacological issues Brian Stafford, MD, MPH
Barriers to Treatment n Public Health: Screening in WIC n Screening in Nurse Visitation n n Primary Care: Screening at OB n Screening at FP n Screening at Pediatric n Brian Stafford, MD, MPH
Challenges of Detecting PPD u u u Depressed mood Lack of pleasure/ interest Feelings of worthlessness/ guilt Agitation or retardation Feelings of worthlessness/ guilt Thoughts of death or suicide Weight loss * Loss of energy * Sleep Disturbance * Diminished concentration/ Indecisiveness * Reports of “overwhelmed”, “anxious” u (60% PPD have co-morbid anxiety meeting diagnostic criteria) Symptoms often confused with more typical reactions to childbirth. BE AWAREthese may be indicators of the presence of PPD Brian Stafford, MD, MPH
Screening for PPD n n Relationship-based? Educate and Normalize PPD n Very Common and Very Treatable • Include Assessment of Partner Brian Stafford, MD, MPH
Early Identification Crucial • • • Need to rule out medical concerns (e. g. , thyroid, anemia) Attend to risk factors in prenatal period Routine postnatal screening • • Observation Interview (ASK and LISTEN) • • • Do not minimize reports of symptoms Consider Timing/ Circumstances Screening: • Self-Report Measures • CES-D • Edinburgh Postnatal Depression Scale (EPDS) • Beck Depression Inventory (BDI) • Postpartum Depression Predictors Inventory (Beck, 1998) Brian Stafford, MD, MPH

Barriers to Treatment n Perinatal Mental Health Expertise n Infant Mental Health Expertise n System Issues with MH Access in both the public and private sector Brian Stafford, MD, MPH
Assessment of Postpartum Mood Disturbance n n Empathic and Relationship Based n Normalize the overwhelming and frightening experience n Subjective Experience Safety n Mom and baby n Obsessive ruminations versus psychotic preoccupation Assessment of Other Pathology n Worries n Thoughts Assessment as Intervention Brian Stafford, MD, MPH
Barriers to Treatment n System Organizational and Infrastructural n n n Unknown referral sources Medicaid funding Institutional barriers n n n Engagement Stigma Phone Centers Transportation Time Brian Stafford, MD, MPH

Barriers To Treatment Consumer Awareness and Social Stigma • nature and incidence is high • • (most common side effect of pregnancy) condition is highly treatable institutional stigma other socio-cultural factors Brian Stafford, MD, MPH
Challenges of Detecting/Treating PPD n n n n Expected period of adjustment (especially for first -time mothers) Stigma associated with being a “good mother” Fear of “going crazy” or being separated from baby Not knowing which doctor to turn to for help n Post-delivery in hospital n 6 week OB/GYN visit n Well baby checks Physician’s minimization of distress Managed care Mental Health Professional Availability Lack of knowledge / appropriate education Brian Stafford, MD, MPH
Resources n n n n n Kempe Center’s Postpartum Depression Intervention Program: (303 -864 -5845) Depression After Delivery (800 -944 -4773) Postpartum Support International (805 -967 -7636) National Women’s Health Information Center (NWHIC) (800 -994 -9662) Postpartum Education for Parents (805 -564 -3888) American College of Obstetricians and Gynecologists (ACOG) (800 -762 -2264) National Institute of Mental Health (301 -496 -9576) American Psychological Association (800 -374 -2721) Brian Stafford, MD, MPH

Collaboration The nature of these barriers require: n specific expertise n unique resources n and collaborative partnerships. Brian Stafford, MD, MPH

Our Joint Purpose: To target these barriers in a strategic, innovative, collaborative, and evidencedbased/best-practice approach that begins to create clinical expertise in the treatment of perinatal mood disorders in local mental health centers and targets other system barriers toward the identification, referral, and treatment of these individuals. Brian Stafford, MD, MPH
The anticipated benefits of this project will be as follows: n n to improve services to low-income and other high-risk women and dyads to improve delivery of perinatal mental health services by community mental health professionals and to link them with infant mental health services n to improve primary care surveillance, screening, counseling, and referral n to improve access to care in local mental health center programs n to educate professionals, organizations, and legislators about the barriers to appropriate identification and treatment Brian Stafford, MD, MPH
The anticipated benefits: n to adapt an evidence-based intervention to culturally, linguistically, and demographically unique populations n to increase community / public awareness of the nature and treatability of perinatal mental illness n n to increase public health surveillance on perinatal mental illness through collaboration between the BHI, FBH, CDPHE, a 1 -800 hotline referral system, and local systems of care to create system linkages by providing evidenced-based education, a public awareness campaign, and other technical support through collaboration with strong and uniquely capable public, private, and non-profit organizations Brian Stafford, MD, MPH
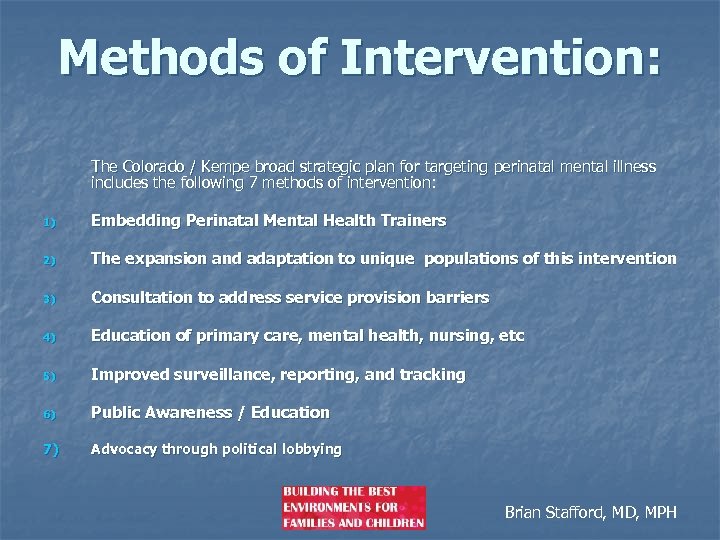
Methods of Intervention: The Colorado / Kempe broad strategic plan for targeting perinatal mental illness includes the following 7 methods of intervention: 1) Embedding Perinatal Mental Health Trainers 2) The expansion and adaptation to unique populations of this intervention 3) Consultation to address service provision barriers 4) Education of primary care, mental health, nursing, etc 5) Improved surveillance, reporting, and tracking 6) Public Awareness / Education 7) Advocacy through political lobbying Brian Stafford, MD, MPH
The creation of system linkages in cooperation with: 1) 2) 3) 4) 5) primary care prenatal nursing programs public health social services agencies and community mental health Brian Stafford, MD, MPH
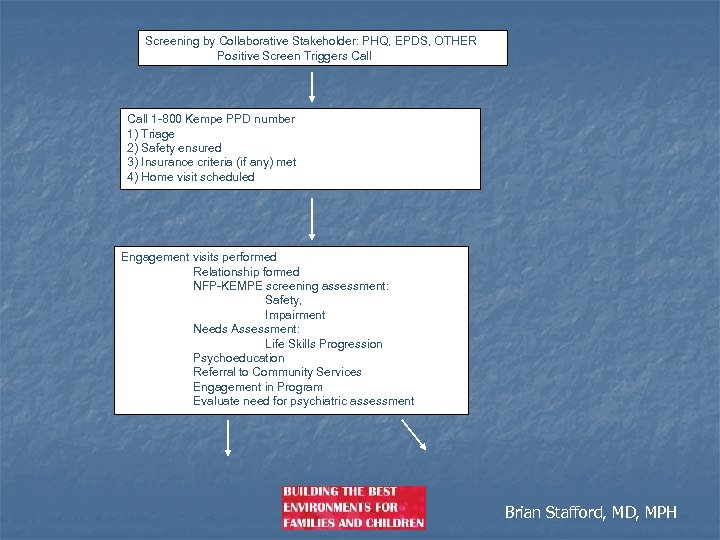
Screening by Collaborative Stakeholder: PHQ, EPDS, OTHER Positive Screen Triggers Call 1 -800 Kempe PPD number 1) Triage 2) Safety ensured 3) Insurance criteria (if any) met 4) Home visit scheduled Engagement visits performed Relationship formed NFP-KEMPE screening assessment: Safety, Impairment Needs Assessment: Life Skills Progression Psychoeducation Referral to Community Services Engagement in Program Evaluate need for psychiatric assessment Brian Stafford, MD, MPH
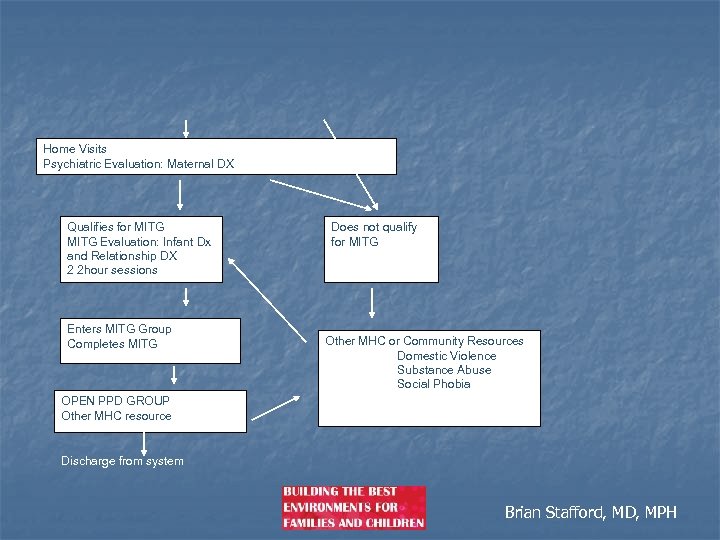
Home Visits Psychiatric Evaluation: Maternal DX Qualifies for MITG Evaluation: Infant Dx and Relationship DX 2 2 hour sessions Enters MITG Group Completes MITG Does not qualify for MITG Other MHC or Community Resources Domestic Violence Substance Abuse Social Phobia OPEN PPD GROUP Other MHC resource Discharge from system Brian Stafford, MD, MPH
The Science of Prevention and Perinatal Mood Disturbance n n There is no clear evidence to recommend the implementation of antenatal and postnatal classes, early postpartum follow-up, continuity of care models, psychological debriefing in hospital, and interpersonal psychotherapy. There is emerging evidence, however, to support the importance of additional professional support provided postnatally. Brian Stafford, MD, MPH
Issues n n n Universal interventions are offered to all women Selective interventions are offered to women at increased risk of developing postnatal depression Indicated interventions are offered to women who have been identified as depressed or probably depressed. Brian Stafford, MD, MPH
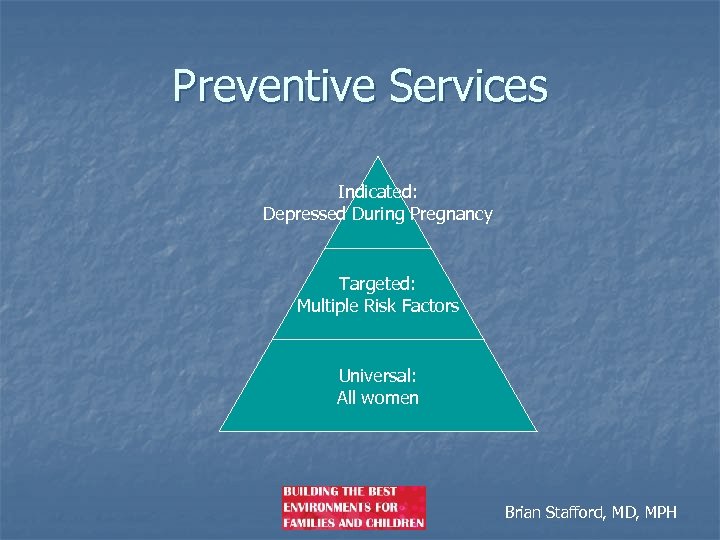
Preventive Services Indicated: Depressed During Pregnancy Targeted: Multiple Risk Factors Universal: All women Brian Stafford, MD, MPH
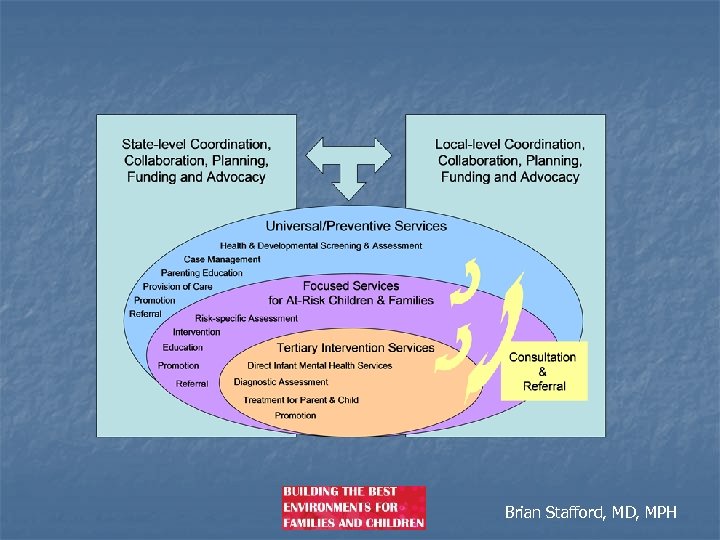
Brian Stafford, MD, MPH

Putting all the pieces together Legislative Advocacy Mental Health Expertise Public Awareness Primary Care Public Health Screening System Linkages Brian Stafford, MD, MPH
Thanks for Listening! n Your Thoughts? Brian Stafford, MD, MPH
cf44db054f7a9c3616ead83a32883ca5.ppt