56b13192556254a35256b0a160b15b8f.ppt
- Количество слайдов: 19
 Incitants du côté de la demande et de l’offre au Nicaragua (réseau de protection sociale) Ferdinando Regalia Head of Social Policy & Economics UNICEF, South Africa Results Based Financing Workshop June 23 rd – 27 th, 2008, Kigali
Incitants du côté de la demande et de l’offre au Nicaragua (réseau de protection sociale) Ferdinando Regalia Head of Social Policy & Economics UNICEF, South Africa Results Based Financing Workshop June 23 rd – 27 th, 2008, Kigali
 Red de Protección Social (RPS) p Commencé en 2000. ~ 170, 000 beneficiaires couverts au sommet du programme en 2004 (phase II) p Approche multisectiorelle. Multi-sector approach: éducation, santé, nutrition p Programme d’assistance sociale basé sur les incitations (CCT) n p Transferts: ~ 1/5 de la consommation des ménages avant programme Ciblé sur les pauvres (
Red de Protección Social (RPS) p Commencé en 2000. ~ 170, 000 beneficiaires couverts au sommet du programme en 2004 (phase II) p Approche multisectiorelle. Multi-sector approach: éducation, santé, nutrition p Programme d’assistance sociale basé sur les incitations (CCT) n p Transferts: ~ 1/5 de la consommation des ménages avant programme Ciblé sur les pauvres (
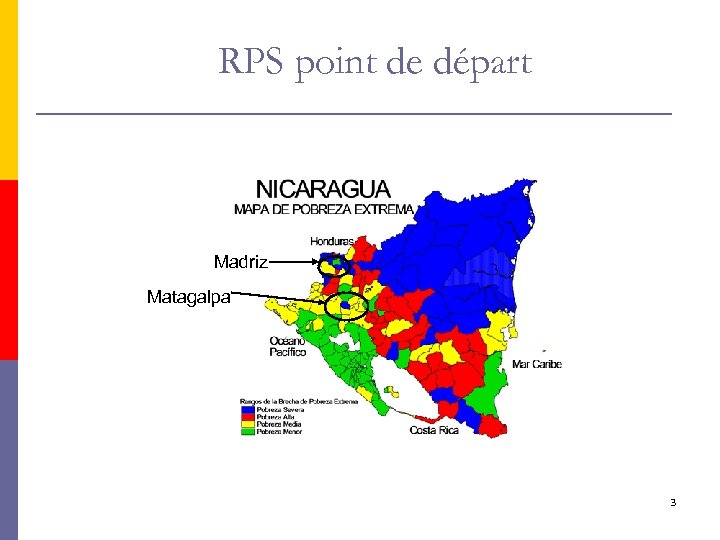 RPS point de départ Madriz Matagalpa 3
RPS point de départ Madriz Matagalpa 3
 Pourquoi des incitants du côté de la demande p Situation: les ménages pauvres consomment moins de services de santé préventifs que les non pauvres. Pourquoi? p Peut-être contraintes du côté de l’offre (bien que l’offre est médiocre de façon uniforme entre les localités) p …p-ê des contraintes du côté de la demande: n n p Coûts directs et indirects élevés pour accéder aux services. Connaissance imperfaite du bénéfice économique à long terme d’un investissement dans la santé, etc. . Difficiles de distinguer les contributions des contraitnes offre/demande ex ante 4
Pourquoi des incitants du côté de la demande p Situation: les ménages pauvres consomment moins de services de santé préventifs que les non pauvres. Pourquoi? p Peut-être contraintes du côté de l’offre (bien que l’offre est médiocre de façon uniforme entre les localités) p …p-ê des contraintes du côté de la demande: n n p Coûts directs et indirects élevés pour accéder aux services. Connaissance imperfaite du bénéfice économique à long terme d’un investissement dans la santé, etc. . Difficiles de distinguer les contributions des contraitnes offre/demande ex ante 4
 Pourquoi les incitants du côté de la demande ? (2) p Solution proposée: quelques contraintes côté demande (ex connaissance imparfaite, externalités) justifiaient de conditions une assistance à certains comportements (RBF) p Intéressant: l’utilisation des services à augmenter plus fortement parmi les très pauvres que les non-pauvres. n p Alors que tous les ménages étaient exposés à une augmentation uniforme en termes d’accès et de qualité des services de santé Challenges: n en 1999, connaissance réduite sur comment mettre en place un CCT. 5
Pourquoi les incitants du côté de la demande ? (2) p Solution proposée: quelques contraintes côté demande (ex connaissance imparfaite, externalités) justifiaient de conditions une assistance à certains comportements (RBF) p Intéressant: l’utilisation des services à augmenter plus fortement parmi les très pauvres que les non-pauvres. n p Alors que tous les ménages étaient exposés à une augmentation uniforme en termes d’accès et de qualité des services de santé Challenges: n en 1999, connaissance réduite sur comment mettre en place un CCT. 5
 Why supply-side incentives? p Situation: Systemic capacity bottlenecks of MOH n Unable to quickly expand services in remote localities p Proposed solution: service outsourcing to private providers through a competitive bidding process p Challenges: n small market of private providers n need to design incentives for health providers to develop efficient plans to rapidly expand coverage in underserved areas 6
Why supply-side incentives? p Situation: Systemic capacity bottlenecks of MOH n Unable to quickly expand services in remote localities p Proposed solution: service outsourcing to private providers through a competitive bidding process p Challenges: n small market of private providers n need to design incentives for health providers to develop efficient plans to rapidly expand coverage in underserved areas 6
 Why supply-side incentives? (2) p RBF: providers to be paid based on the achievement of measurable and predetermined targets, verified by independent sources 7
Why supply-side incentives? (2) p RBF: providers to be paid based on the achievement of measurable and predetermined targets, verified by independent sources 7
 What did RBF want to achieve? p D- and s-side incentives sought to increase: n Utilization of preventive health services (children 0 -5) • • Child growth and development monitoring (baseline: 60% among children < 3) including micronutrients and antiparasites. • n Regular check ups (baseline: 70% among children < 3) Up-to-date vaccinations (baseline: 39% among children 12 -23 months) Utilization of maternal health services (Phase II). • n Pre-natal and post-partum control Parents’ attendance to health educational workshops • Household sanitation, reproductive health, nutritional counseling 8
What did RBF want to achieve? p D- and s-side incentives sought to increase: n Utilization of preventive health services (children 0 -5) • • Child growth and development monitoring (baseline: 60% among children < 3) including micronutrients and antiparasites. • n Regular check ups (baseline: 70% among children < 3) Up-to-date vaccinations (baseline: 39% among children 12 -23 months) Utilization of maternal health services (Phase II). • n Pre-natal and post-partum control Parents’ attendance to health educational workshops • Household sanitation, reproductive health, nutritional counseling 8
 Stakeholders’ buy-in: d-side incentives p Planning stage: n MOH opposed d-side incentives, fearing surge in workload • n p Distribution of vaccines and other inputs, increasing referrals for curative services, etc. Government decided to go ahead anyway through SIF Implementation stage: high involvement by local stakeholders n Households’ targeting validation n Local authorities’ support for logistics n Randomized evaluation plans n Coordination of supply side response n Beneficiaries’ coordination through promoters 9
Stakeholders’ buy-in: d-side incentives p Planning stage: n MOH opposed d-side incentives, fearing surge in workload • n p Distribution of vaccines and other inputs, increasing referrals for curative services, etc. Government decided to go ahead anyway through SIF Implementation stage: high involvement by local stakeholders n Households’ targeting validation n Local authorities’ support for logistics n Randomized evaluation plans n Coordination of supply side response n Beneficiaries’ coordination through promoters 9
 Stakeholders’ buy-in: s-side incentives p MOH (central) aware of bottlenecks but resisted outsourcing n p Wage competition (potential exodus of health workers); no experience with contracting of services Terms of the agreement between MOH and RPS team n n Additional budget allocated to MOH for supervision n p MOH responsible for providers’ selection, training and certification (with RPS team’s support in procurement) Providers obliged to feed the MIS of the MOH Stronger buy–in by MOH regional offices n Understood faster than the central MOH the potential gains in coverage to be achieved through outsourcing and RBF 10
Stakeholders’ buy-in: s-side incentives p MOH (central) aware of bottlenecks but resisted outsourcing n p Wage competition (potential exodus of health workers); no experience with contracting of services Terms of the agreement between MOH and RPS team n n Additional budget allocated to MOH for supervision n p MOH responsible for providers’ selection, training and certification (with RPS team’s support in procurement) Providers obliged to feed the MIS of the MOH Stronger buy–in by MOH regional offices n Understood faster than the central MOH the potential gains in coverage to be achieved through outsourcing and RBF 10
 How d-incentives operate p RPS socioeconomic survey administered to all HHs in (geographically) targeted localities p All HHs eligible for d-incentives if extreme poverty incidence high. Otherwise Proxy Means Test applied p Eligible HHs enrolled into roster. Mothers or primary caregivers entitled to receive bi-monthly transfers p All HHs’ members identified by a bar code. Transfer recipients identified by a special i. d. card with picture p Eligible HHs’ members mapped to health providers, payment agencies and schools p Pre-printed forms with names and bar-codes distributed by RPS team to health providers 11
How d-incentives operate p RPS socioeconomic survey administered to all HHs in (geographically) targeted localities p All HHs eligible for d-incentives if extreme poverty incidence high. Otherwise Proxy Means Test applied p Eligible HHs enrolled into roster. Mothers or primary caregivers entitled to receive bi-monthly transfers p All HHs’ members identified by a bar code. Transfer recipients identified by a special i. d. card with picture p Eligible HHs’ members mapped to health providers, payment agencies and schools p Pre-printed forms with names and bar-codes distributed by RPS team to health providers 11
 How d-incentives operate (2) p Forms used by providers as planning tools to schedule all check ups with eligible HHs’ members. Information used by MOH to plan supply of inputs p HHs’ attendance recorded by health providers. Forms regularly collected by RPS team and information downloaded to RPS MIS p HHs’ record of compliance used to prepare payment orders. Two months lag between compliance updating and payments processing p Non compliance triggers suspension of transfers (10%). Repeated non compliance triggers expulsion (1%) p Spot checks of the compliance verification process 12
How d-incentives operate (2) p Forms used by providers as planning tools to schedule all check ups with eligible HHs’ members. Information used by MOH to plan supply of inputs p HHs’ attendance recorded by health providers. Forms regularly collected by RPS team and information downloaded to RPS MIS p HHs’ record of compliance used to prepare payment orders. Two months lag between compliance updating and payments processing p Non compliance triggers suspension of transfers (10%). Repeated non compliance triggers expulsion (1%) p Spot checks of the compliance verification process 12
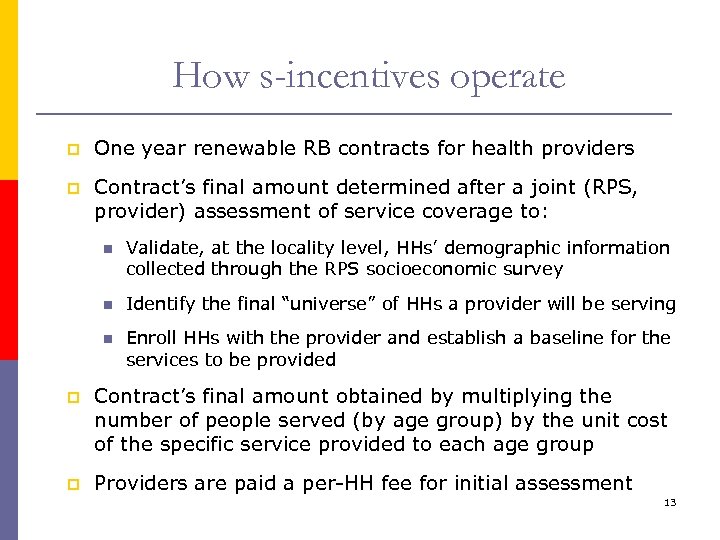 How s-incentives operate p One year renewable RB contracts for health providers p Contract’s final amount determined after a joint (RPS, provider) assessment of service coverage to: n Validate, at the locality level, HHs’ demographic information collected through the RPS socioeconomic survey n Identify the final “universe” of HHs a provider will be serving n Enroll HHs with the provider and establish a baseline for the services to be provided p Contract’s final amount obtained by multiplying the number of people served (by age group) by the unit cost of the specific service provided to each age group p Providers are paid a per-HH fee for initial assessment 13
How s-incentives operate p One year renewable RB contracts for health providers p Contract’s final amount determined after a joint (RPS, provider) assessment of service coverage to: n Validate, at the locality level, HHs’ demographic information collected through the RPS socioeconomic survey n Identify the final “universe” of HHs a provider will be serving n Enroll HHs with the provider and establish a baseline for the services to be provided p Contract’s final amount obtained by multiplying the number of people served (by age group) by the unit cost of the specific service provided to each age group p Providers are paid a per-HH fee for initial assessment 13
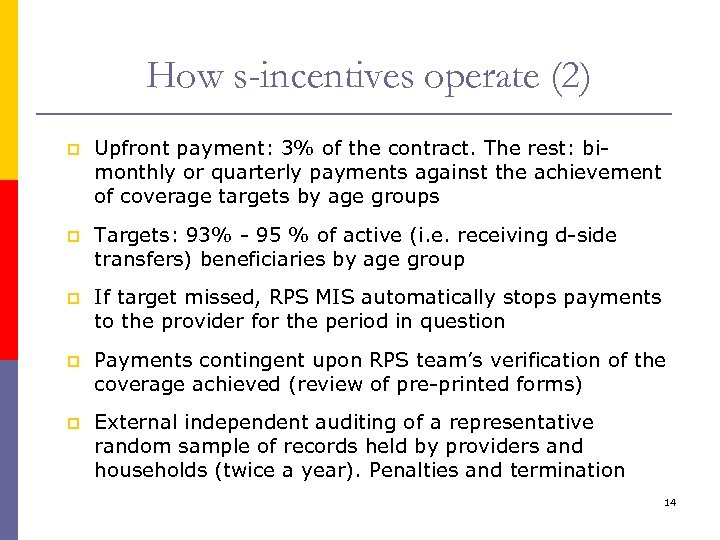 How s-incentives operate (2) p Upfront payment: 3% of the contract. The rest: bimonthly or quarterly payments against the achievement of coverage targets by age groups p Targets: 93% - 95 % of active (i. e. receiving d-side transfers) beneficiaries by age group p If target missed, RPS MIS automatically stops payments to the provider for the period in question p Payments contingent upon RPS team’s verification of the coverage achieved (review of pre-printed forms) p External independent auditing of a representative random sample of records held by providers and households (twice a year). Penalties and termination 14
How s-incentives operate (2) p Upfront payment: 3% of the contract. The rest: bimonthly or quarterly payments against the achievement of coverage targets by age groups p Targets: 93% - 95 % of active (i. e. receiving d-side transfers) beneficiaries by age group p If target missed, RPS MIS automatically stops payments to the provider for the period in question p Payments contingent upon RPS team’s verification of the coverage achieved (review of pre-printed forms) p External independent auditing of a representative random sample of records held by providers and households (twice a year). Penalties and termination 14
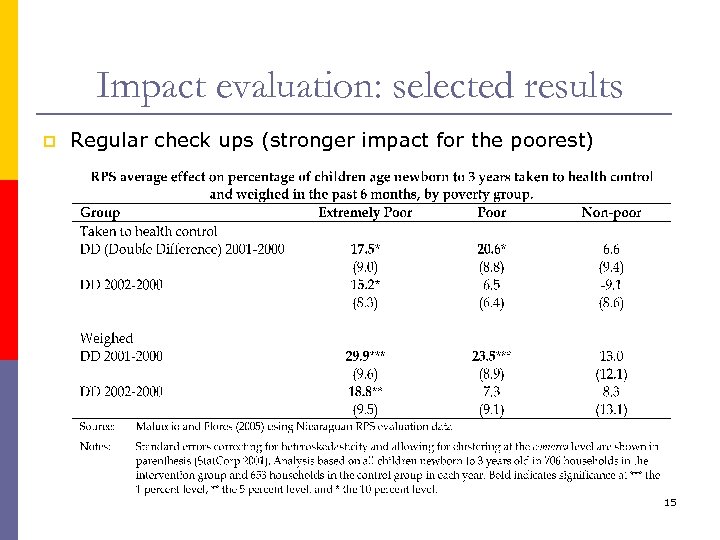 Impact evaluation: selected results p Regular check ups (stronger impact for the poorest) 15
Impact evaluation: selected results p Regular check ups (stronger impact for the poorest) 15
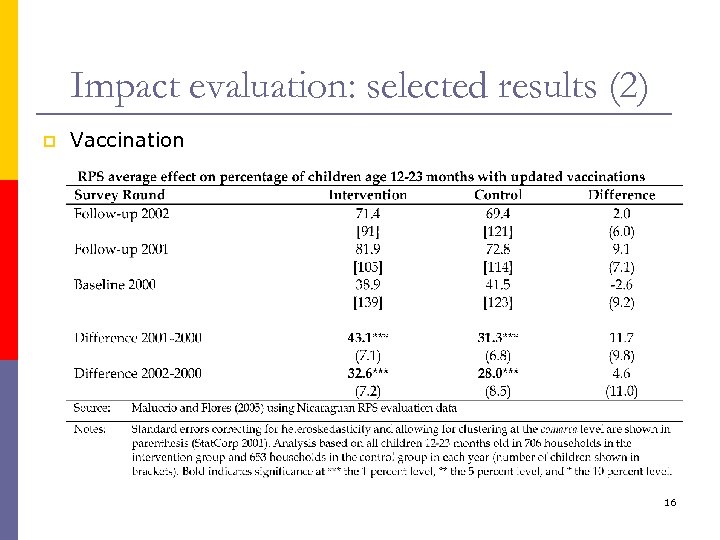 Impact evaluation: selected results (2) p Vaccination 16
Impact evaluation: selected results (2) p Vaccination 16
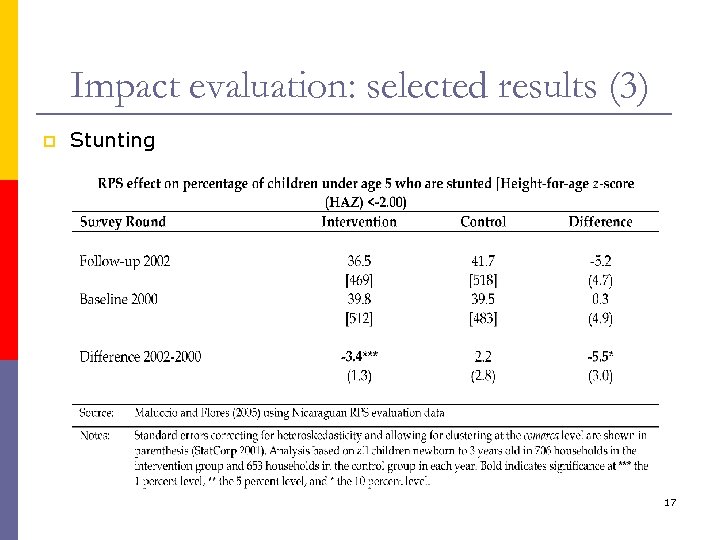 Impact evaluation: selected results (3) p Stunting 17
Impact evaluation: selected results (3) p Stunting 17
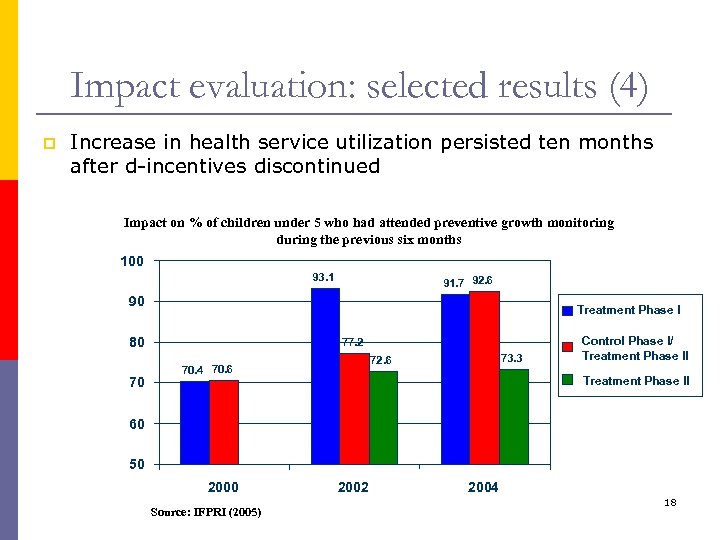 Impact evaluation: selected results (4) p Increase in health service utilization persisted ten months after d-incentives discontinued Impact on % of children under 5 who had attended preventive growth monitoring during the previous six months 100 93. 1 91. 7 92. 6 90 Treatment Phase I 80 70 77. 2 73. 3 72. 6 70. 4 70. 6 Control Phase I/ Treatment Phase II 60 50 2000 Source: IFPRI (2005) 2002 2004 18
Impact evaluation: selected results (4) p Increase in health service utilization persisted ten months after d-incentives discontinued Impact on % of children under 5 who had attended preventive growth monitoring during the previous six months 100 93. 1 91. 7 92. 6 90 Treatment Phase I 80 70 77. 2 73. 3 72. 6 70. 4 70. 6 Control Phase I/ Treatment Phase II 60 50 2000 Source: IFPRI (2005) 2002 2004 18
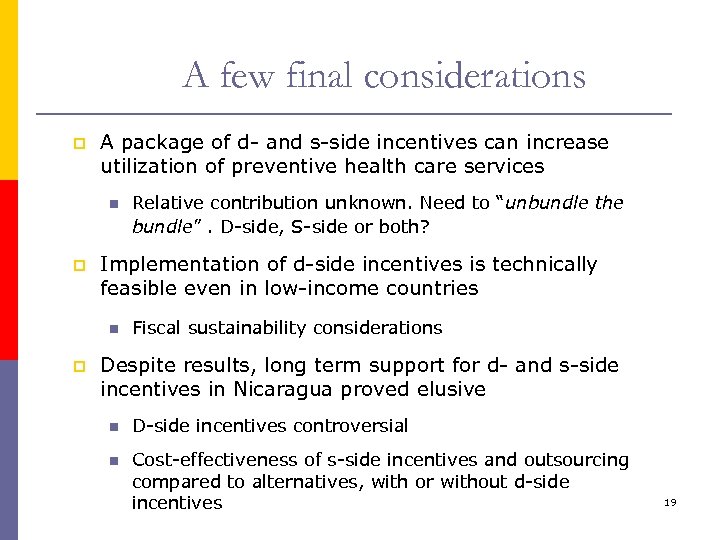 A few final considerations p A package of d- and s-side incentives can increase utilization of preventive health care services n p Implementation of d-side incentives is technically feasible even in low-income countries n p Relative contribution unknown. Need to “unbundle the bundle”. D-side, S-side or both? Fiscal sustainability considerations Despite results, long term support for d- and s-side incentives in Nicaragua proved elusive n D-side incentives controversial n Cost-effectiveness of s-side incentives and outsourcing compared to alternatives, with or without d-side incentives 19
A few final considerations p A package of d- and s-side incentives can increase utilization of preventive health care services n p Implementation of d-side incentives is technically feasible even in low-income countries n p Relative contribution unknown. Need to “unbundle the bundle”. D-side, S-side or both? Fiscal sustainability considerations Despite results, long term support for d- and s-side incentives in Nicaragua proved elusive n D-side incentives controversial n Cost-effectiveness of s-side incentives and outsourcing compared to alternatives, with or without d-side incentives 19


