a52fc047fbe0dfc52a59eeb7f6df0a26.ppt
- Количество слайдов: 122
In the Name of God Obstetrics Study Guide 2 Mitra Ahmad Soltani 2008 Med-ed-online. org
References 1 - All India Medical Pre PG. Fetal maturity &length of foetus. 2007. See: www. aippg. net/forum/viewtopic. php? t=33005 2 -Brinholz J. Gestational age. American Journal of Roentgenography. 1984. 142 (4): 849 3 - Cunningham G, Gant N, Leveno K, et al. Williams Obsterics. 22 nd Ed. New York : Mc Graw Hill, 2005. 4 - Durham J. Transition to Parenthood: How accurate is your due date. 2004 see: www. transitiontoparenthood. com/ttp/parented/pregnancy/duedate. htm and www. pregnancy. about. com/library/weekly/aa 042197. htm 5 - Friedman E. Obstetrical Decision Making. Harvard Medical School. 1981 6 - Military Obstetrics and Gynecology. Brookside. Press. Estimating Gestational age. 2006 See: www. brooksidepress. org/. . . /Pregnancy /estimating_ gestational_age. htm 7 -Mitchell P. A Comparison of Gestational Age Information Derived from the Birth Certificate, 1990 – 1998. Alaska Vital Sign. 2000. 8 (1): 1 -7 See: www. hss. state. ak. us/dph/bvs/PDFs/vitalsigns/avs_0801. pdf 8 - Mittendorf R, Williams M, Berkey C, Cotter P. . The Length of Uncomplicated Human Gestation. Obstetrics & Gynecology. 1990. 75(6): 929 -932 Pictures and material on Breech and C/S are adapted from emedicine e-Journal with permission: 9 -Fischer R. Breech Presentation. emedicine. 2006 10 - Sehdev H. Cesarean Delivery. emedicine. 2005
Gestational Age Determination
1 - Nägele’s Rule • This was developed in the 1850’s by Dr. Nägele. To calculate this, one should add 7 days, and then subtract 3 months from LMP. • ((LMP + 7 days) - 3 months) = Expected Date of Delivery • Example: ((the LMP on 1 st April + 7 days) - 3 months) = January 8 • This “rule” doesn’t take into account the fact that many women are uncertain of the date of their last menstrual period, not all women have 28 day cycles, and not all women ovulate on day 14 of their cycle.
2 - Mittendorf’s Rule • To calculate “Mittendorf’s Rule”, one should add 15 days for first time Caucasian women, or add 10 days if non-white or this is not the first baby. Then subtract 3 months. • ((LMP + 15 days) - 3 months) = Expected Date of Delivery for first time pregnant Caucasian women • Example: (( LMP on 1 st April + 15 days) - 3 months) = January 16
3 - Ultrasound: • Measurement of a Crown-Rump Length during the first trimester (1 -13 weeks) will give a gestational age that is usually accurate to within 3 days of the actual due date. • During the second trimester (14 -28 weeks), measurement of the biparietal diameter will accurately predict the due date within 10 -14 days in most cases. • In the third trimester, the accuracy of ultrasound in predicting the due date is less, with a plus or minus confidence range of as much as 3 weeks.
FL • Femur length measurements can have a correlation coefficient of 0. 995 with gestational age in a group of healthy fetuses with known date of conception. • Nevertheless, it still cannot be used exclusively because it may be relatively short in the presence of growth retardation, or long when growth acceleration has occurred, introducing comparable errors in age estimate if the underlying growth pattern is not appreciated.
4 - Heart Tone: • Fetal heartbeat can be heard through Doppler starting at 9 -12 weeks and by stethoscope at 18 -20 weeks. • This event, however, is less accurate because the mother is not permanently attached to a Doppler device so the first heart beat can not be clued definitely.
5 - Mac. Donald's Rule • Fundal Height (the distance from the symphysis pubis joint to the fundus of uterus) can be a rough estimate of gestational age. • Typically, from week 24 to week 34, fundal height in centimetres correlates with weeks of gestation. For example, at 28 weeks, the fundus is probably about 28 cm.
If a tape measure is unavailable, some rough guidelines can be used: • At 12 weeks, the uterus is just barely palpable above the pubic bone, using only an abdominal hand. • At 16 weeks, the top of the uterus is 1/2 way between the pubic bone and the umbilicus.
• At 20 -22 weeks, the top of the uterus is right at the umbilicus. • At full term, the top of the uterus is at the level of the ribs. (xyphoid process).
6 - Quickening • Some believe the baby will come five months after quickening, the first time the mother feels the baby move. • This is hard to evaluate, as women can be more or less sensitive to these sensations, and may notice them at different times in their pregnancies. • First time mothers typically notice movement around 18 -20 weeks. Mothers who have been pregnant before notice it as early as 16 weeks.
7 -Length of fetus • a- Crown-Rump Length: CRL is measured in first half of pregnancy; that is, up to 20 weeks measure from the Vertex to Coccyx. The fetal length is more helpful in prematurity than in post maturity, because after term the confidence interval for estimation surpasses 3 weeks.
CHL- Hasse’s rule • b- Crown-Heel Length : • CHL in the first half of pregnancy is the number of lunar months x 4. The CHL of a 4 month fetus is 16 cm : 4 x 4=16 cm • From the end of 20 weeks in the second half of pregnancy, CHL in cm is the result of multiplication of the number of lunar months at the time of the assessment by 5. The CHL of an 8 month fetus is 40 cm: 8 x 5 =40 cm
Normally, at the end of the following weeks gestation: • Before 20 -24 wks, the height of the fundus from pubic symphysis to umbilicus multiplied by 2/7 equals duration of pregnancy in lunar months or x 8/7=duration of pregnancy in weeks. • After 20 weeks, the fetal length in inches is equal to half of the number of gestational age in weeks. For example at 28 wk the height of the fundus from pubic symphysis to umbilicus is 14 inches.
8 -Estimation of fetal weight in grams: Johnson’s Formula • (applicable only in Vertex presentation): Fundal height (cm) above the pubic symphysis minus 12 if Vertex above Ischial Spine or minus 11 if below Ischial Spines- should be multiplied by 155. This will be fetal weight in grams. • e. g. , 32(fundal height)-12(constant) x 155( constant) => 20 x 155=3100 gms
9 -Changes in Weight Gain: • Normally there is a steady increase in weight of a pregnant woman until the last 2 -3 weeks of pregnancy. The woman stops gaining weight at about term. It may remain stationary or may begin to fall which means that pregnancy is at least mature.
Weight gain • In normal pregnancy –the weight gain should not exceed 2 ½ kilograms in any one month or 0. 9 kg in a week. The maximum permissible weight gain throughout the whole period of pregnancy is about 10 or 11 kg (about 24 lbs) although 12 ½ kg is allowed— 1/3 rd of this weight—increases in the first 20 weeks, and another 1/3 rd in the next 10 weeks. The Remaining 1/3 rd would be gained between 30 weeks to term.
10 - The age from conception: • The date of conception from a basal body temperature chart or known time of intercourse is the best measures for gestational age determination. But, relatively few women can state the events.
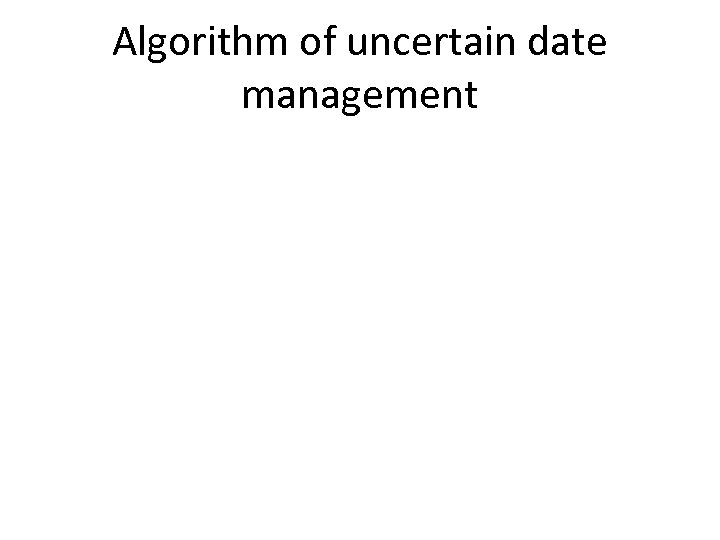
Algorithm of uncertain date management
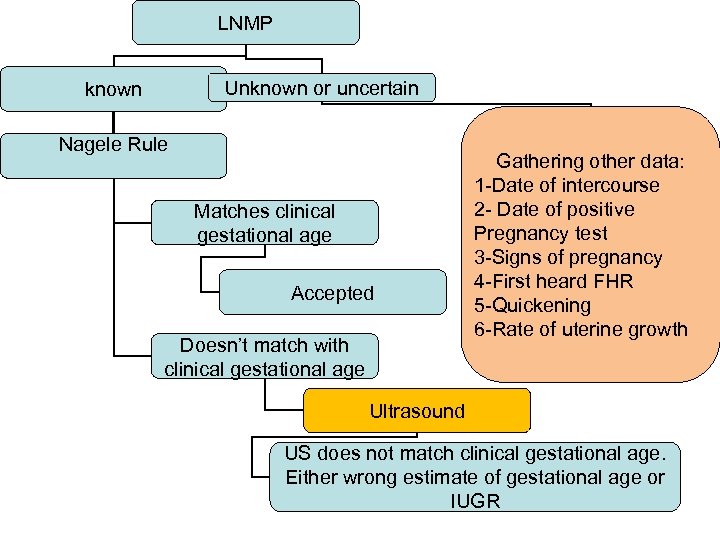
LNMP Unknown or uncertain known Nagele Rule Matches clinical gestational age Accepted Doesn’t match with clinical gestational age Gathering other data: 1 -Date of intercourse 2 - Date of positive Pregnancy test 3 -Signs of pregnancy 4 -First heard FHR 5 -Quickening 6 -Rate of uterine growth Ultrasound US does not match clinical gestational age. Either wrong estimate of gestational age or IUGR
ROM
SROM • Membrane rupture without spontaneous uterine contractions happens in 8% of term pregnancies. • At Parkland Hospital labor is stimulated with oxytocin when ruptured membranes are diagnosed at term and labor does not spontaneously ensue.
Which is an unreliable sign for chorioamnionitis? A-T=>38 c B-maternal and fetal tachycardia C-fundal tenderness D-maternal leukocytosis Answer: d
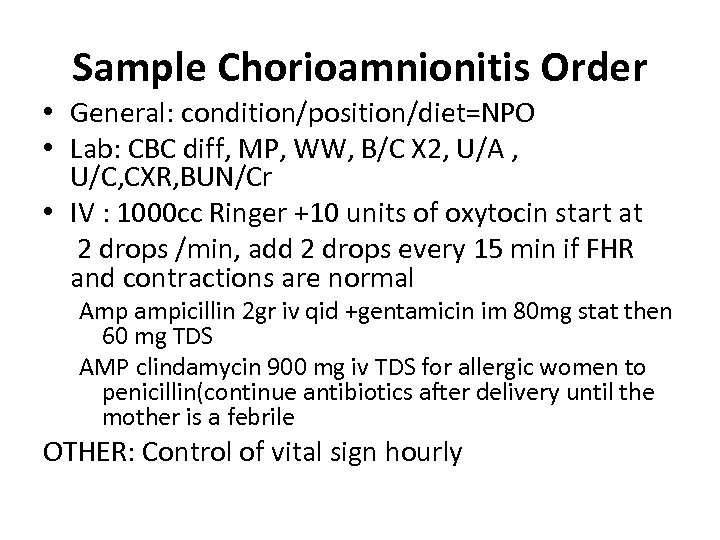
Sample Chorioamnionitis Order • General: condition/position/diet=NPO • Lab: CBC diff, MP, WW, B/C X 2, U/A , U/C, CXR, BUN/Cr • IV : 1000 cc Ringer +10 units of oxytocin start at 2 drops /min, add 2 drops every 15 min if FHR and contractions are normal Amp ampicillin 2 gr iv qid +gentamicin im 80 mg stat then 60 mg TDS AMP clindamycin 900 mg iv TDS for allergic women to penicillin(continue antibiotics after delivery until the mother is a febrile OTHER: Control of vital sign hourly
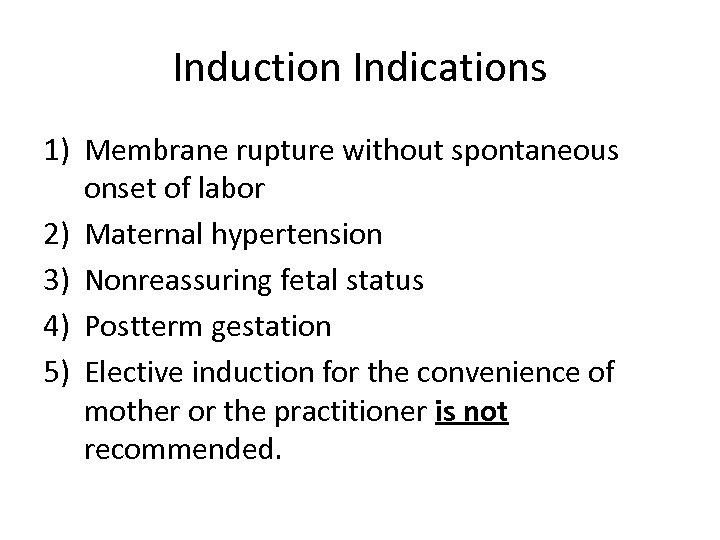
Induction Indications 1) Membrane rupture without spontaneous onset of labor 2) Maternal hypertension 3) Nonreassuring fetal status 4) Postterm gestation 5) Elective induction for the convenience of mother or the practitioner is not recommended.
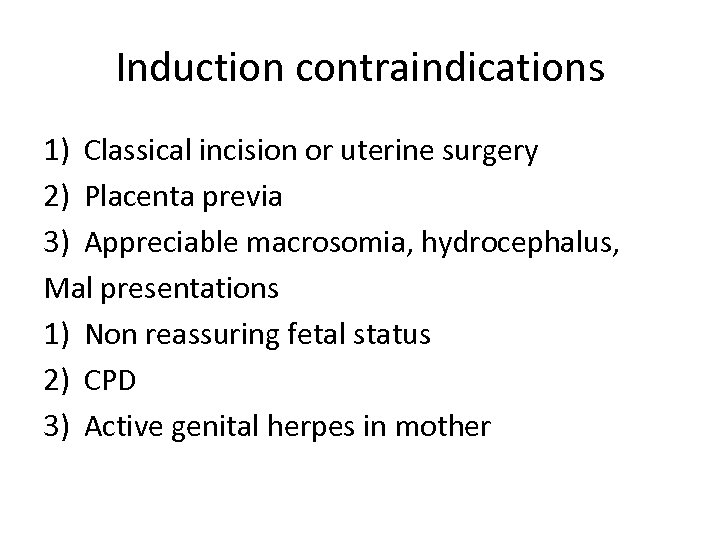
Induction contraindications 1) Classical incision or uterine surgery 2) Placenta previa 3) Appreciable macrosomia, hydrocephalus, Mal presentations 1) Non reassuring fetal status 2) CPD 3) Active genital herpes in mother
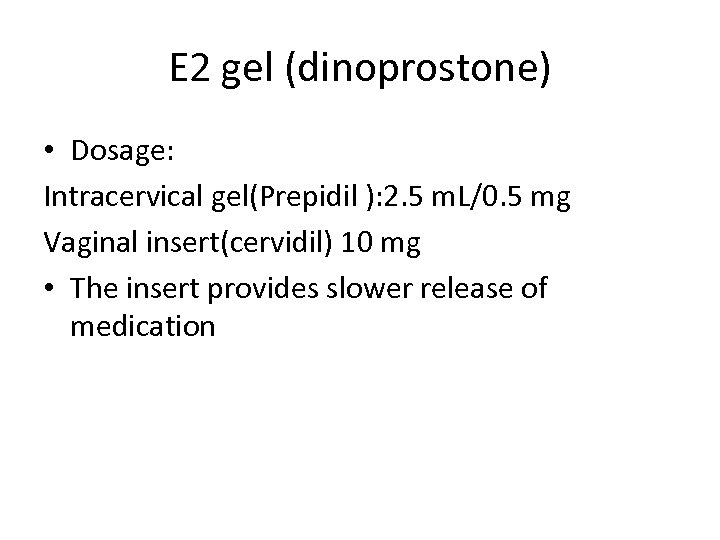
E 2 gel (dinoprostone) • Dosage: Intracervical gel(Prepidil ): 2. 5 m. L/0. 5 mg Vaginal insert(cervidil) 10 mg • The insert provides slower release of medication
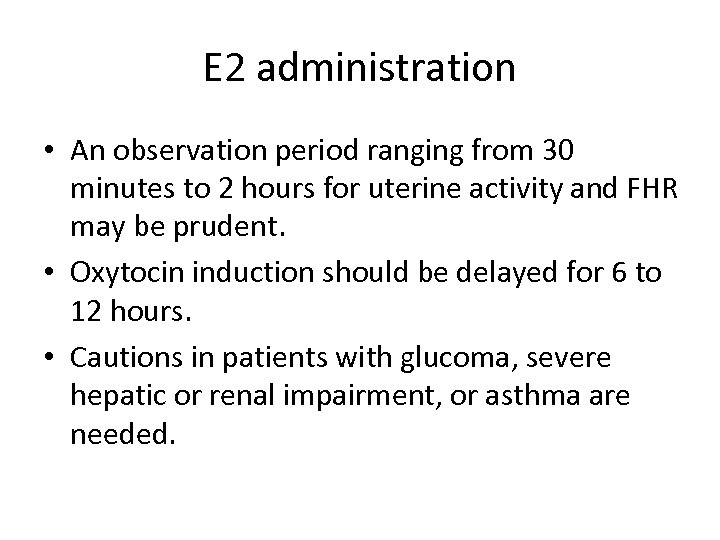
E 2 administration • An observation period ranging from 30 minutes to 2 hours for uterine activity and FHR may be prudent. • Oxytocin induction should be delayed for 6 to 12 hours. • Cautions in patients with glucoma, severe hepatic or renal impairment, or asthma are needed.
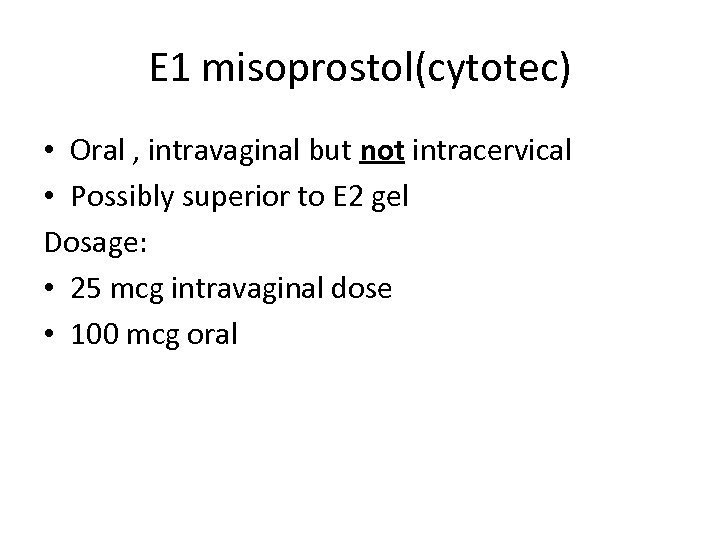
E 1 misoprostol(cytotec) • Oral , intravaginal but not intracervical • Possibly superior to E 2 gel Dosage: • 25 mcg intravaginal dose • 100 mcg oral
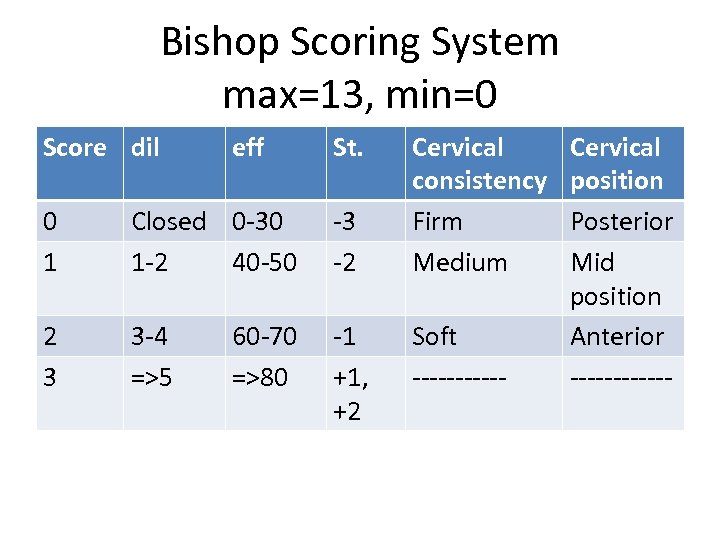
Bishop Scoring System max=13, min=0 Score dil eff St. 0 1 Closed 0 -30 1 -2 40 -50 -3 -2 2 3 3 -4 =>5 -1 +1, +2 60 -70 =>80 Cervical consistency Firm Medium Soft ------ Cervical position Posterior Mid position Anterior ------
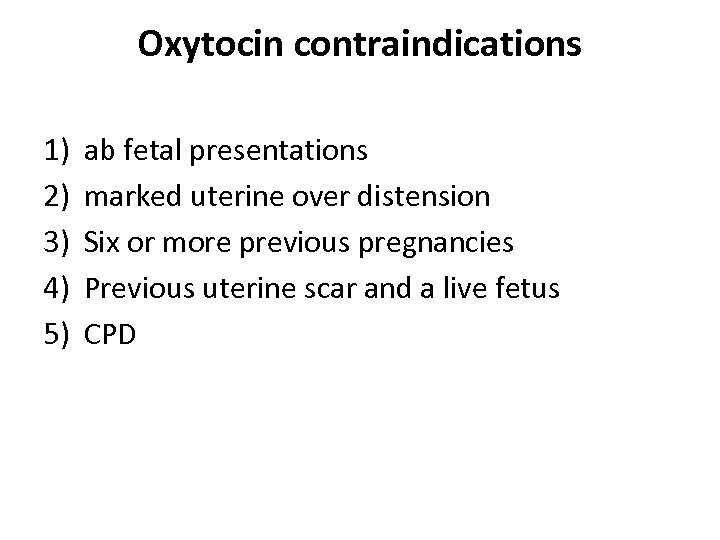
Oxytocin contraindications 1) 2) 3) 4) 5) ab fetal presentations marked uterine over distension Six or more previous pregnancies Previous uterine scar and a live fetus CPD
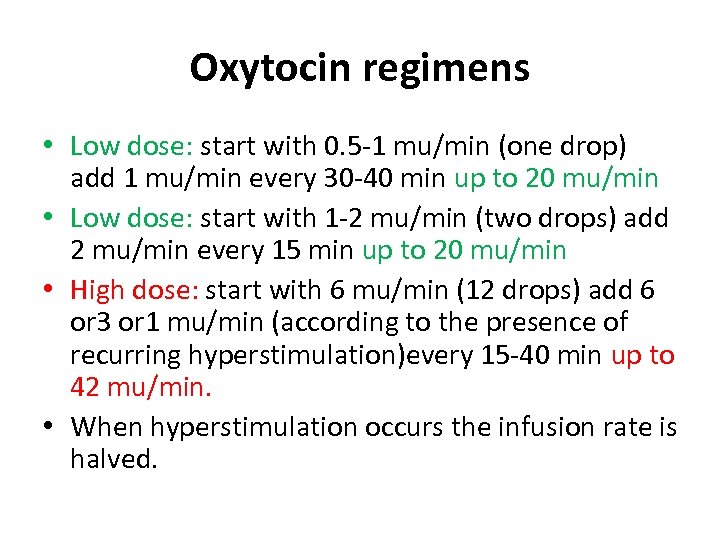
Oxytocin regimens • Low dose: start with 0. 5 -1 mu/min (one drop) add 1 mu/min every 30 -40 min up to 20 mu/min • Low dose: start with 1 -2 mu/min (two drops) add 2 mu/min every 15 min up to 20 mu/min • High dose: start with 6 mu/min (12 drops) add 6 or 3 or 1 mu/min (according to the presence of recurring hyperstimulation)every 15 -40 min up to 42 mu/min. • When hyperstimulation occurs the infusion rate is halved.
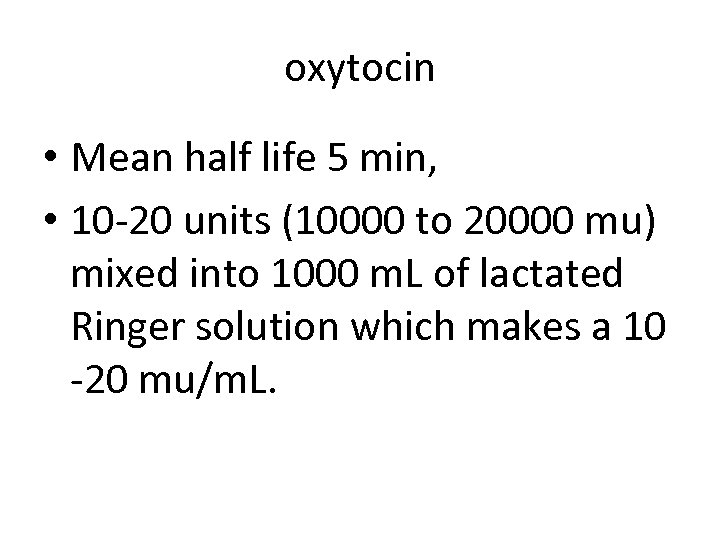
oxytocin • Mean half life 5 min, • 10 -20 units (10000 to 20000 mu) mixed into 1000 m. L of lactated Ringer solution which makes a 10 -20 mu/m. L.
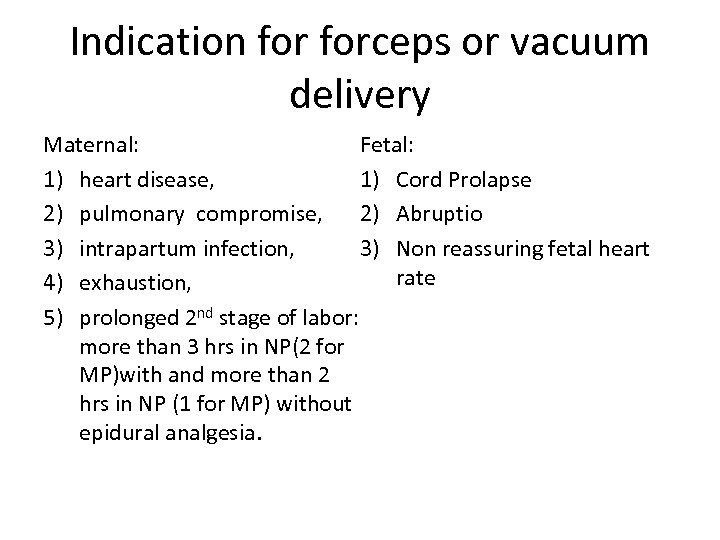
Indication forceps or vacuum delivery Fetal: Maternal: 1) Cord Prolapse 1) heart disease, 2) pulmonary compromise, 2) Abruptio 3) Non reassuring fetal heart 3) intrapartum infection, rate 4) exhaustion, 5) prolonged 2 nd stage of labor: more than 3 hrs in NP(2 for MP)with and more than 2 hrs in NP (1 for MP) without epidural analgesia.
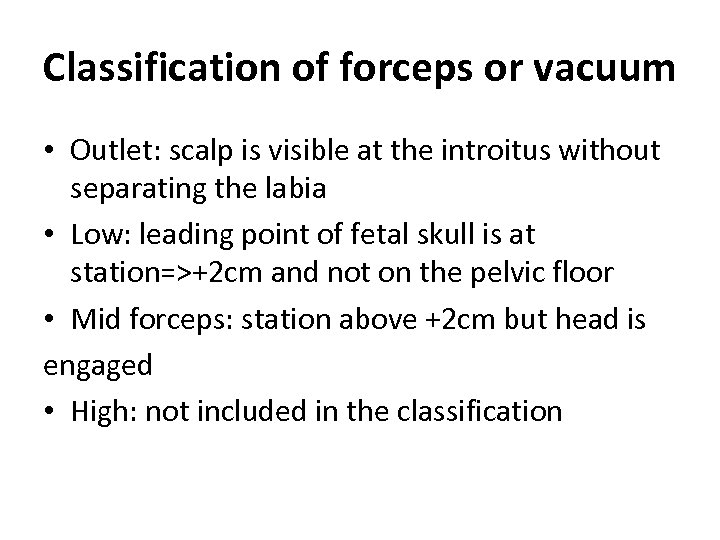
Classification of forceps or vacuum • Outlet: scalp is visible at the introitus without separating the labia • Low: leading point of fetal skull is at station=>+2 cm and not on the pelvic floor • Mid forceps: station above +2 cm but head is engaged • High: not included in the classification
Contraindication for vacuum delivery 1) 2) 3) 4) 5) 6) Nonvertex presentations Extreme prematurity Fetal coagulopathies known macrosomia Above zero stations Lack of experienced operator who would abandoned the procedure if it does not proceed easily or if the cup “pops off” more than three times.
Vacuum technique • The center of the cup should be over the sagittal suture and about 3 cm in front of the posterior fontanel. • The full circumference of the cup should be palpated both prior to as well as after the vacuum has been created and prior to traction. • The suction should be increased to a negative pressure of 0. 8 kg/cm². • Traction should be coordinated with maternal expulsive efforts.
Breech Presentation Pictures and material are adapted from : Fischer R. Breech Presentation. emedicine. 2006 with permission
Incidence • Breech presentation occurs in 3 -4% of all deliveries. • 25% of births prior to 28 weeks' gestation • 7% of births at 32 weeks' gestation • 1 -3% of births at term
Predisposing factors 1) Fetus to AF ratio(prematurity, polyhydramnios) 2) Intrauterine space(uterine malformations or fibroids, placenta previa, multiple gestation) 3) and fetal abnormalities (eg, CNS malformations, neck masses, aneuploidy),
Types • Frank breech (50 -70%) - Hips flexed, knees extended (pike position) • Complete breech (5 -10%) - Hips flexed, knees flexed (cannonball position) • Footling or incomplete (10 -30%) - One or both hips extended, foot presenting
Vaginal Delivery • Spontaneous breech delivery: No traction or manipulation of the infant is used. This occurs predominantly in very preterm deliveries. • Assisted breech delivery: This is the most common type of vaginal breech delivery. The infant is allowed to spontaneously deliver up to the umbilicus, and then maneuvers are initiated to assist in the delivery of the remainder of the body, arms, and head.
Total Breech Extraction • Total breech extraction: The fetal feet are grasped, and the entire fetus is extracted. • Total breech extraction should be used only for a noncephalic second twin. • Total breech extraction for the singleton breech is associated with a birth injury rate of 25% and a mortality rate of approximately 10%.
Footling breech presentation: A singleton gestation should not be pulled by the feet because this action may precipitate head entrapment in an incompletely dilated cervix or may precipitate nuchal arms. As long as the fetal heart rate is stable and no physical evidence of a prolapsed cord is evident, management may be expectant while awaiting full cervical dilation.

Assisted vaginal breech delivery 1: Thick meconium passage is common as the breech is squeezed through the birth canal. This is usually not associated with meconium aspiration because the meconium passes out of the vagina and does not mix with the amniotic fluid.

Assisted vaginal breech delivery 2: The Ritgen maneuver is applied to take pressure off the perineum during vaginal delivery. Episiotomies are often performed for assisted vaginal breech deliveries, even in multiparous women, to prevent soft tissue dystocia.

Assisted vaginal breech delivery 3: No downward or outward traction is applied to the fetus until the umbilicus has been reached.

Assisted vaginal breech delivery 4: With a towel wrapped around the fetal hips, gentle downward and outward traction is applied in conjunction with maternal expulsive efforts until the scapula is reached. An assistant should be applying gentle fundal pressure to keep the fetal head flexed.

Assisted vaginal breech delivery 5: The anterior arm is followed to the elbow, and the arm is swept out of the vagina.

Assisted vaginal breech delivery 6: The fetus is rotated 180°, and the contralateral arm is delivered in a similar manner as the first. The infant is then rotated 90° to the backup position in preparation for delivery of the head.

Assisted vaginal breech delivery 7: The fetal head is maintained in a flexed position by using the Mauriceau maneuver, which is performed by placing the index and middle fingers over the maxillary prominence on either side of the nose. The fetal body is supported in a neutral position, with care to not overextend the neck.

Piper forceps application: • Piper forceps are specialized forceps used only for the after-coming head of a breech presentation. • They are used to keep the fetal head flexed during extraction of the head. • An assistant is needed to hold the infant while the operator gets on one knee to apply the forceps from below.

Assisted vaginal breech delivery 8: Low 1 -minute Apgar scores are not uncommon after a vaginal breech delivery. A pediatrician should be present for the delivery in the event that neonatal resuscitation is needed.

Pinard Maneuver • The Pinard maneuver may be needed with a frank breech to facilitate delivery of the legs, only after the fetal umbilicus has been reached. Pressure is exerted against the inner aspect of the knee. Flexion of the knee follows, and the lower leg is swept medially and out of the vagina.

Mauriceau Smellie Veit maneuver • The flexed position of fetal head can be accomplished by using the Mauriceau Smellie Veit maneuver, in which the operator's index and middle fingers lift up on the fetal maxillary prominences, while the assistant applies suprapubic pressure.

Risks 1 1) Lower Apgar scores, especially at 1 minute
Risks 2 Fetal head entrapment. This occurs in 0 -8. 5% of vaginal breech deliveries. This percentage is higher with preterm fetuses (<32 wk). Dührssen incisions (ie, 1 -3 cervical incisions made to facilitate delivery of the head) may be necessary to relieve cervical entrapment. The Zavanelli maneuver involves replacement of the fetus into the abdominal cavity followed by cesarean delivery.
Risks 3 Nuchal arms, in which one or both arms are wrapped around the back of the neck, are present in 0 -5% of vaginal breech deliveries and in 9% of breech extractions. Nuchal arms may result in neonatal trauma (including brachial plexus injuries) in 25% of cases. Risks may be reduced by avoiding rapid extraction of the infant during delivery of the body. To relieve nuchal arms, rotate the infant so that the fetal face turns toward the maternal symphysis pubis; this reduces the tension holding the arm around the back of the fetal head.
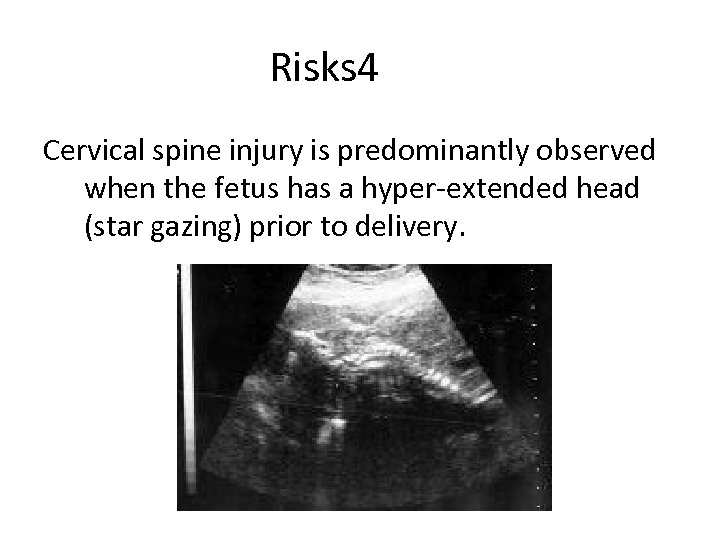
Risks 4 Cervical spine injury is predominantly observed when the fetus has a hyper-extended head (star gazing) prior to delivery.
Risk 5 • Cord prolapse occurs in 7. 5% of all breeches. This incidence varies with the type of breech: 0 -2% with frank breech, 5 -10% with complete breech, and 10 -25% with footling breech. • Cord prolapse occurs twice as often in multiparas (6%) than in primigravidas (3%). • Cord prolapse may not always result in severe fetal heart rate decelerations because of the lack of presenting parts to compress the umbilical cord (ie, that which predisposes also protects).
Candidates for vaginal delivery 1 - gestational age>37 weeks 2 - EFW< 4000 g, 3 -A frank breech presentation is preferred when vaginal delivery is attempted. Complete breeches and footling breeches are still candidates, as long as the presenting part is well applied to the cervix and both obstetrical and anesthesia services are readily available in the event of a cord prolapse, 4 -The fetus should show no neck hyperextension on ultrasound images
C/S of breech • Maneuvers for cesarean delivery are similar to those for vaginal breech delivery, including the Pinard maneuver (wrapping the hips with a towel for traction, head flexion during traction, rotation and sweeping out of arm) and the Mauriceau Smellie Veit maneuver.
C/S of Breech • Some practitioners routinely perform low vertical uterine incisions for preterm breeches prior to 32 weeks' gestation to avoid head entrapment and the kind of difficult delivery that cesarean delivery was meant to avoid. • If a low transverse incision is attempted, the physician should try to keep the membranes intact as long as possible and move quickly once the breech is extracted in order to deliver the head before the uterus begins to contract.
Candidates for External cephalic version • • No marked CPD No placenta previa Early gestational age is preferred Vertical pocket of 2 cm or greater
ECV Prepare for the possibility of cesarean delivery: • Obtain a type • an anesthesia consult • The patient should be NPO for at least 8 hours prior to the procedure. Perform an ultrasound to confirm breech, check growth and amniotic fluid volume, and rule out anomalies associated with breech. Perform a NST (biophysical profile as backup) prior to ECV to confirm fetal well-being.
ECV • ECV is accomplished by judicious manipulation of the fetal head toward the pelvis while the breech is brought up toward the fundus. Attempt a forward roll first and then a backward roll if the initial attempts are unsuccessful. • Following an ECV attempt, whether successful or not, repeat the nonstress test (biophysical profile if needed) prior to discharge. Also, administer Rh immune globulin to women who are Rh-negative. • In those with an unsuccessful ECV, the practitioner has the option of sending the patient home or proceeding with a cesarean delivery.
Risks of ECV • • fractured fetal bones, precipitation of labor premature rupture of membranes, abruptio placentae, fetomaternal hemorrhage (0 -5%), cord entanglement ( <1. 5%) , transient slowing of the fetal heart rate (in as many as 40% of cases). This risk is believed to be a vagal response to head compression with ECV. It usually resolves within a few minutes after cessation of the ECV attempt and is not usually associated with adverse sequelae for the fetus.
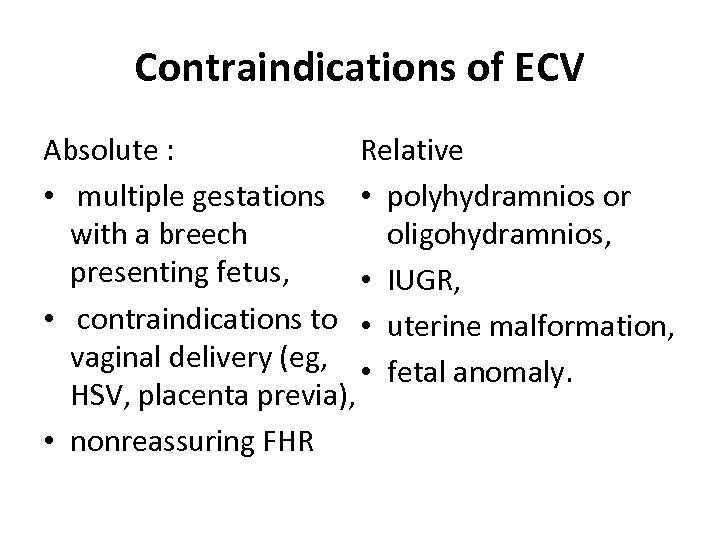
Contraindications of ECV Relative Absolute : • multiple gestations • polyhydramnios or oligohydramnios, with a breech presenting fetus, • IUGR, • contraindications to • uterine malformation, vaginal delivery (eg, • fetal anomaly. HSV, placenta previa), • nonreassuring FHR
C/S Adapted from : Sehdev H. Cesarean Delivery. emedicine. 2005 With permission
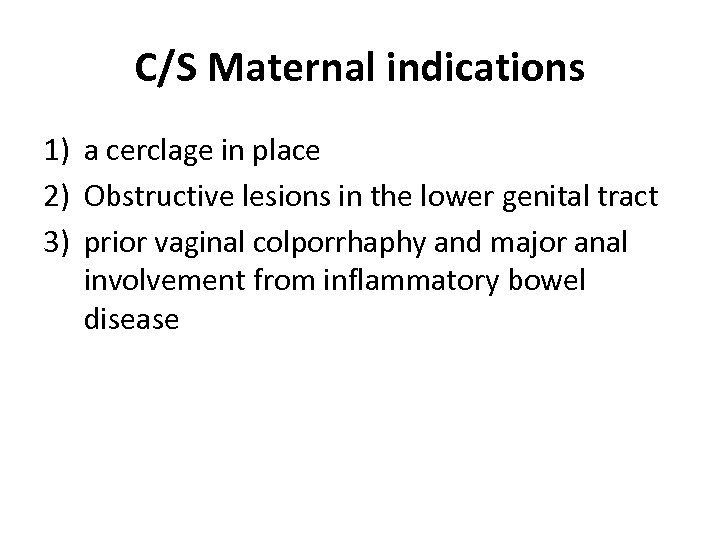
C/S Maternal indications 1) a cerclage in place 2) Obstructive lesions in the lower genital tract 3) prior vaginal colporrhaphy and major anal involvement from inflammatory bowel disease
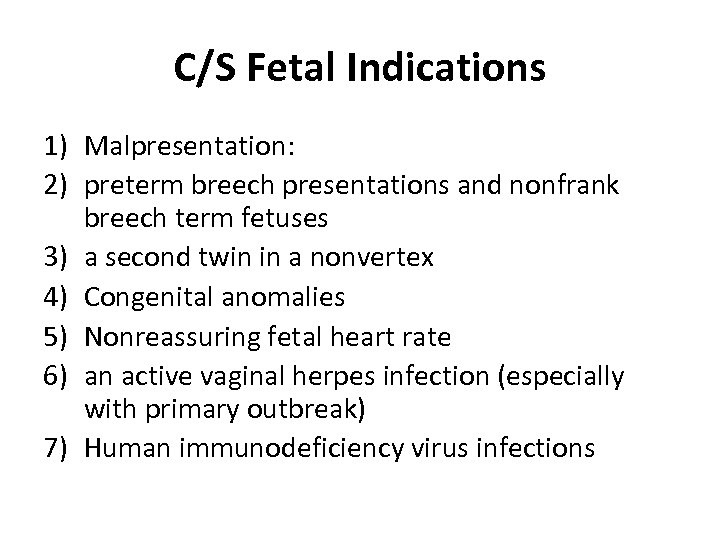
C/S Fetal Indications 1) Malpresentation: 2) preterm breech presentations and nonfrank breech term fetuses 3) a second twin in a nonvertex 4) Congenital anomalies 5) Nonreassuring fetal heart rate 6) an active vaginal herpes infection (especially with primary outbreak) 7) Human immunodeficiency virus infections
C/S Maternal and fetal indications: • Abnormal placentation • Abnormal labor due to CPD • Contraindications to labor: In women who have a uterine scar (prior myomectomy in which the uterine cavity was entered or cesarean delivery in which the upper contractile portion of the uterus was incised)
C/S contraindication • When maternal status is compromised by a surgery, • If the fetus has a known karyotypic abnormality (trisomy 13 or 18), • known congenital anomaly that may lead to death (anencephaly),
VBAC candidates • • One or two prior low-transverse c/s Clinically adequate pelvis No other uterine scars or previous rupture Availability for emergency cesarean delivery
Criteria for timing of elective repeated Cesarean Delivery At least one of these criteria must be met in a woman with normal cycles and no immediate antecedent use of OCP: • FH sound documented for 20 wks by nonelectronic fetoscope or 30 wks by Doppler. • 36 wks since a positive serum or urine chorionic gonadotropin test was performed. • CRL obtained by US at 6 -11 wks supports a gestational age at least 39 wks. • US at 12 -20 wks supports a gestational age at least 39 wks.
Abdominal incision 1 Infraumbilical incision : • a vertical incision may provide easier access into the abdomen, with better visualization for a patient with significant intra-abdominal adhesions from prior surgeries.
Abdominal incision 2 -vertical • Upon reaching the rectus sheath, either the rectus sheath can be incised with a scalpel for the entire length of the incision or a small incision in the fascia can be made with a scalpel • Then extended superiorly and inferiorly with scissors. • Then, the rectus muscles (and pyramidalis muscles) are separated in the midline by sharp and blunt dissection. This act exposes the transversalis fascia and the peritoneum.
Abdominal incision 3 • The peritoneum is identified and entered at the superior aspect of the incision to avoid bladder injury. Prior to entering the peritoneum, care is taken to avoid incising adjacent bowel or omentum. • Once the peritoneal cavity is entered, the peritoneal incision is extended sharply to the upper aspect of the incision superiorly and to the reflection over the bladder inferiorly.
Abdominal incision 4 Transverse incisions The Pfannenstiel incision is curved slightly cephalad at the level of the pubic hairline. The incision extends slightly beyond the lateral borders of the rectus muscle bilaterally and is carried to the fascia. Then, the fascia is incised bilaterally for the full length of the incision. Then, the underlying rectus muscle is separated from the fascia both superiorly and inferiorly with blunt and sharp dissection.
Abdominal incisions 5 transverse incisions • A Maylard incision is made approximately 2 -3 cm above the symphysis and is quicker than a Pfannenstiel incision. It involves a transverse incision of the anterior rectus sheath and rectus muscle bilaterally. • Identify and possibly ligate the superficial inferior epigastric vessels (located in the lateral third of each rectus).
Abdominal incision 6 • For most cesarean deliveries, only the medial two thirds of each rectus muscle usually needs to be divided. If more than two thirds of the rectus muscle is divided, identify and ligate the deep inferior epigastric vessels. The transversalis fascia and peritoneum are identified and incised transversely.
Uterine incision 1 • Dissect the bladder free of the lower uterine segment. Grasp the loose uterovesical peritoneum with forceps, and incise it with Metzenbaum scissors. The incision is extended bilaterally in an upward curvilinear fashion.
Uterine incision 2 • The lower flap is grasped gently, and the bladder is separated from the lower uterus with blunt and sharp dissection. A bladder blade is placed to both displace and protect the bladder inferiorly and to provide exposure for the lower uterine segment (the contractile portion of the uterus).
Uterine incision 3 • One of essentially 2 incisions can be made on the uterus, either a transverse or vertical incision. • In more than 90% of cesarean deliveries, a low transverse (Monroe-Kerr) incision is made. The incision is made 1 -2 cm above the original upper margin of the bladder with a scalpel. The initial incision is small and is continued into the uterine wall until either the fetal membranes are visualized or the cavity is entered.
Uterine incision 4 • The incision is extended bilaterally and slightly cephalad. The incision can be extended with either sharp dissection or blunt dissection (usually with the index fingers of the surgeon). • Blunt dissection has the potential for unpredictable extension, and care should be taken to avoid injury to the uterine vessels. The presenting part of the fetus is identified, and the fetus is delivered either as a vertex presentation or as a breech.
Indications for classical (vertical) uterine incisions • the lower uterine segment can not be exposed or entered safely (adhesion, myoma, carcinoma) • there is a transverse lie of a large fetus • Placenta previa of anterior implantation • Massive maternal obesity • Lower uterine segment is not thinned out (like cases of very small fetuses)
Uterine incision 5 • In a vertical(classical) incision again, the bladder is dissected inferiorly to expose the lower segment, and the bladder blade is placed.
Uterine incision 6 • The vertical incision again is initiated with a scalpel in the inferior portion of the lower uterine segment. • When the cavity is entered, the incision is extended superiorly with sharp dissection. The fetus is identified and delivered. Note the extent of the superior portion of the uterine incision.
Uterine incision 7 • With a true low vertical incision, the risk of uterine rupture with a trial of labor is approximately 1 -4%, with most recent reports finding a risk for uterine rupture of less than 2%. • If the incision should be either extended into the contractile portion of the uterus or is made almost completely in the upper contractile portion, the risk of uterine rupture in future pregnancies is 4 -10%.
Uterine incision 8 A vertical incision also may be considered in: • those cases where a hysterectomy may be planned • in the setting of a placenta accreta • if the patient has a coexisting cervical cancer • A vertical incision is associated with increased blood loss and longer operating time (takes longer to close) with less risk of injury to the uterine vessels than a low transverse incision.
repair 1 • Externalizing the uterine fundus facilitates uterine massage, the ability to assess whether the uterus is atonic, and the examination of the adnexa. • The uterine cavity usually is wiped clean of all membranes with a dry laparotomy sponge, and the cervix can be dilated with an instrument, such as a Kelly clamp, if the patient underwent delivery with a previously undilated cervix. Typically, an Allis clamp is placed at the angles of the uterine incision.
repair 2 • Repair of a low transverse uterine incision can be performed in either a 1 -layer or 2 -layer fashion with zero or double-zero chromic or Vicryl suture. • The first layer should include stitches placed lateral to each angle, with prior palpation of the location of the lateral uterine vessels. Most physicians use a continuous locking stitch. • If the first layer is hemostatic, a second layer (Lembert stitch), which is used to imbricate the incision, does not need to be placed.
repair 3 • Closure of a vertical incision usually requires several layers because the incision is through a thicker portion of the uterus. • Again, note the extent of a vertical uterine incision because it impacts how a patient should be counseled regarding future pregnancies.
repair 4 • When the uterus is closed, attention must be paid to its overall tone. • If the uterus does not feel firm and contracted with massage and intravenous oxytocin, consider intramuscular injections of prostaglandin (15 -methyl-prostaglandin, Hemabate) or methylergonovine and repeat as appropriate.
repair 5 • If the uterine incision is hemostatic, the uterine fundus is replaced into the abdominal cavity (unless a concurrent tubal ligation is to be performed).
Repair 6 • The vesicouterine peritoneum and parietal peritoneum can be reapproximated with a running chromic stitch. Many physicians prefer to not close the peritoneum because these surfaces reapproximate within 24 -48 hours and can heal without scar formation. Furthermore, the rectus muscles to do not need to be reapproximated.
repair 7 • The subfascial tissue is inspected for bleeding, and, if hemostatic, the fascia is closed. • The fascia can be closed with a running stitch, and synthetic braided sutures are preferred over chromic sutures. • If the patient is at risk for poor wound healing (eg, those with chronic steroid use), then a delayed absorbable or permanent suture can be used. • Place stitches at approximately 1 -cm intervals and more than 1 cm away from the incision line.
repair 8 • The subcutaneous tissue does not have to be reapproximated, but in patients who are obese (subcutaneous depth >2 cm), a drain may be placed and connected to an external bulb suction apparatus. • The skin edges can be closed either with a subcuticular stitch or with staples (removed 3 or 4 d postoperatively).
Patient should know why and what type • Overall, patients attempting a vaginal birth after a prior cesarean delivery can expect success approximately 70% of the time. • If a patient had a cesarean delivery for presumed CPD attempting a vaginal birth with the next pregnancy is associated with a decreased risk of success.
Why and what kind • If the cesarean delivery was performed because of an abnormal fetal heart pattern or for a malpresentation, then expectations for a successful vaginal birth can be higher than 70%.
Why and what kind • If the uterine incision was vertical, the risk of uterine rupture is increased above the approximate 1% risk associated with a low transverse incision. • If the incision extended into the upper contractile portion, the risk of uterine rupture can approach 10%, with 50% of these occurring prior to the onset of labor.
Why and what kind • The risk of placenta accreta in a patient with previa is approximately 4% with no prior cesarean deliveries; the risk increases to approximately 25% with 1 prior cesarean delivery and to 40% with 2 prior cesarean deliveries.
Sample C/S orders
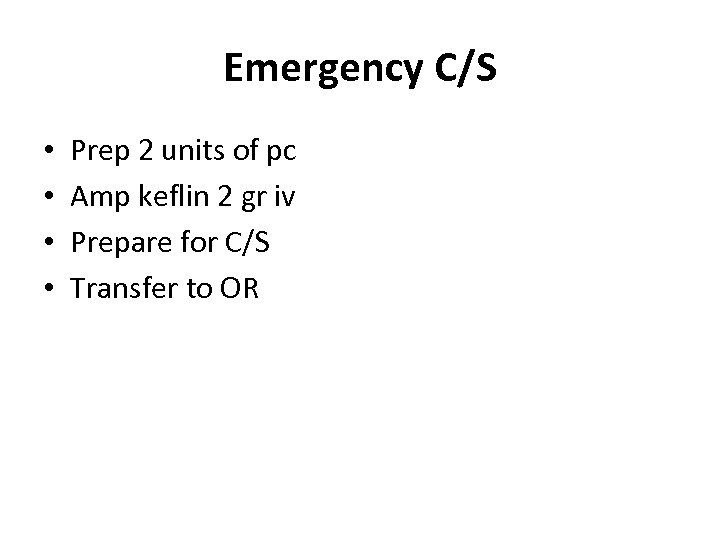
Emergency C/S • • Prep 2 units of pc Amp keflin 2 gr iv Prepare for C/S Transfer to OR
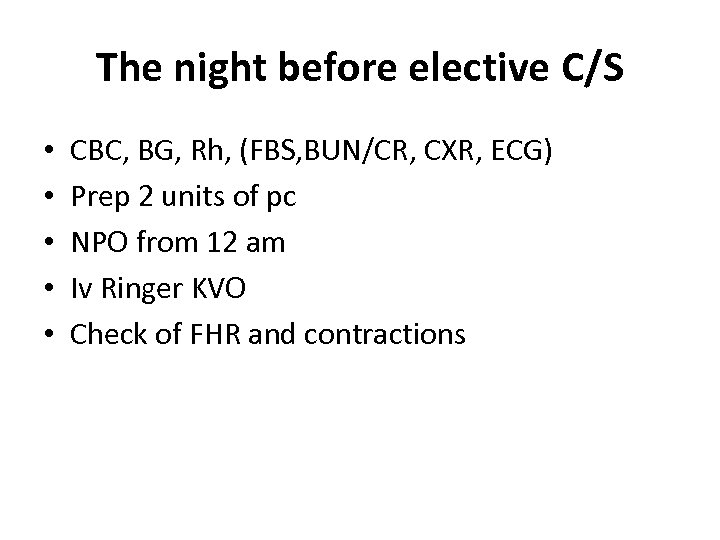
The night before elective C/S • • • CBC, BG, Rh, (FBS, BUN/CR, CXR, ECG) Prep 2 units of pc NPO from 12 am Iv Ringer KVO Check of FHR and contractions
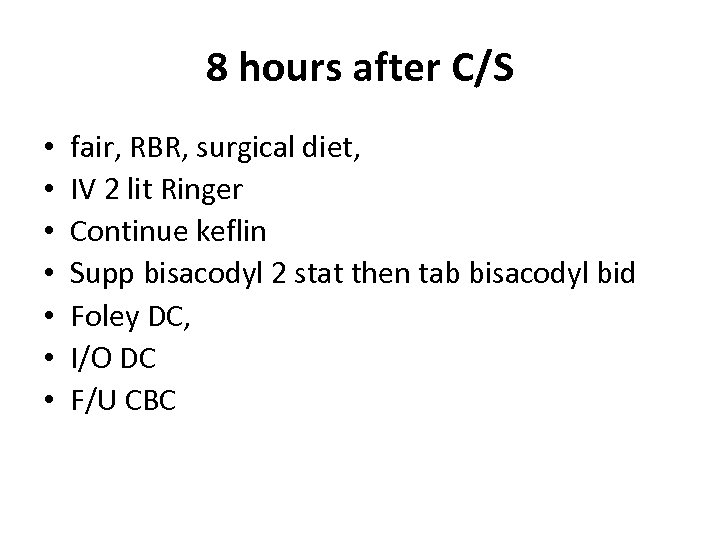
8 hours after C/S • • fair, RBR, surgical diet, IV 2 lit Ringer Continue keflin Supp bisacodyl 2 stat then tab bisacodyl bid Foley DC, I/O DC F/U CBC
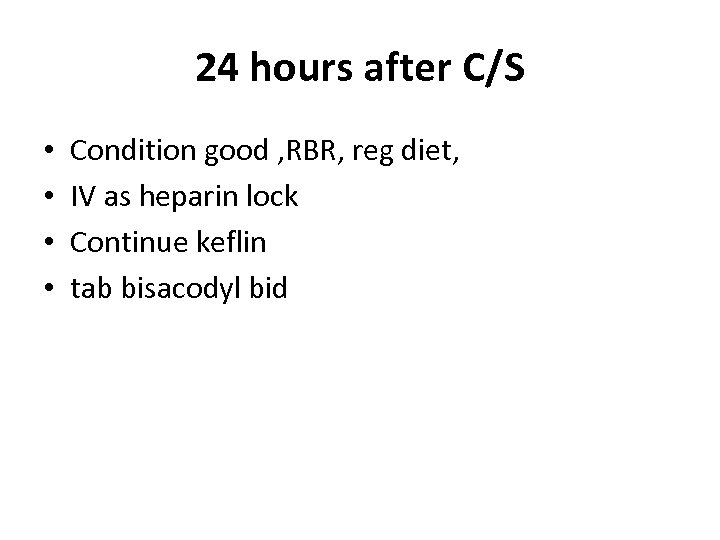
24 hours after C/S • • Condition good , RBR, reg diet, IV as heparin lock Continue keflin tab bisacodyl bid
36 -48 hours after C/S • Remove dressing • Discharge with Cap cephalexin 500 mg qid Cap mefenamic acid 500 mg tds Cap hematinic (according to Hb)
Diabetic elective C/S NPO from 12 am Prep 2 units of PC 1000 cc Ringer IV fluid q 8 hrs the night before surgery Amp keflin 2 gr iv stat half an hour before surgery • Before operation: 10 units of regular +1000 cc DW 5% 150 cc/hr • Check of BS q 6 h after operation Inform in cases of ROM or bleeding or pain
a52fc047fbe0dfc52a59eeb7f6df0a26.ppt