07267cba38a81848503a132a2e16a2ab.ppt
- Количество слайдов: 10
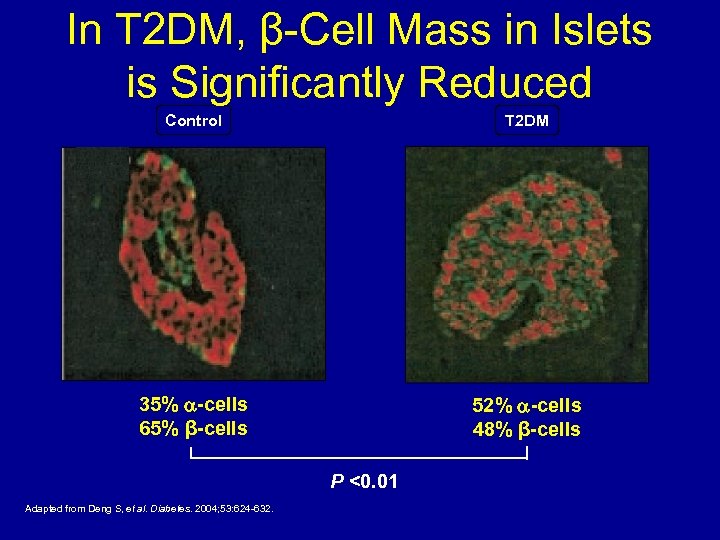
In T 2 DM, β-Cell Mass in Islets is Significantly Reduced Control T 2 DM 35% -cells 65% β-cells 52% -cells 48% β-cells P <0. 01 Adapted from Deng S, et al. Diabetes. 2004; 53: 624 -632.
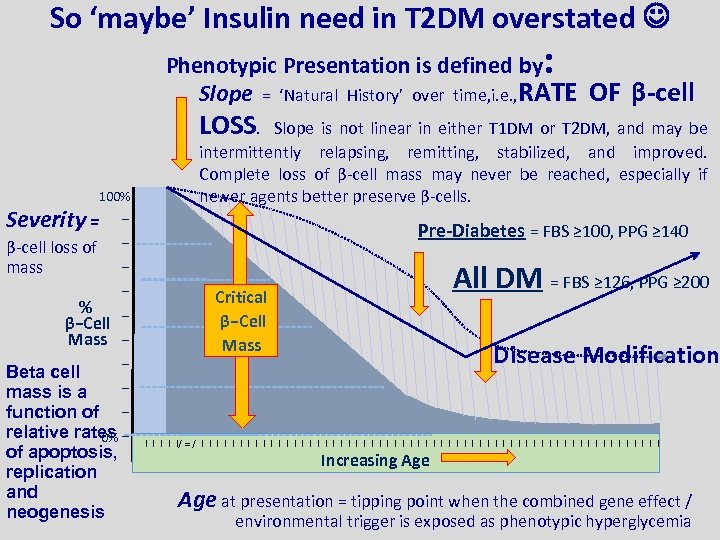
So ‘maybe’ Insulin need in T 2 DM overstated : Phenotypic Presentation is defined by Slope = ‘Natural History’ over time, i. e. , RATE OF β-cell LOSS. Slope is not linear in either T 1 DM or T 2 DM, and may be 100% Severity = − − β-cell loss of − mass − % β−Cell − Mass − − Beta cell − mass is a function of − relative rates − 0% of apoptosis, replication and neogenesis intermittently relapsing, remitting, stabilized, and improved. Complete loss of β-cell mass may never be reached, especially if newer agents better preserve β-cells. Pre-Diabetes = FBS ≥ 100, PPG ≥ 140 All DM = FBS ≥ 126, PPG ≥ 200 Critical β−Cell Mass Disease Modification I I I/ ≈ / I I I I I I I I I I I I I I I Increasing Age at presentation = tipping point when the combined gene effect / environmental trigger is exposed as phenotypic hyperglycemia
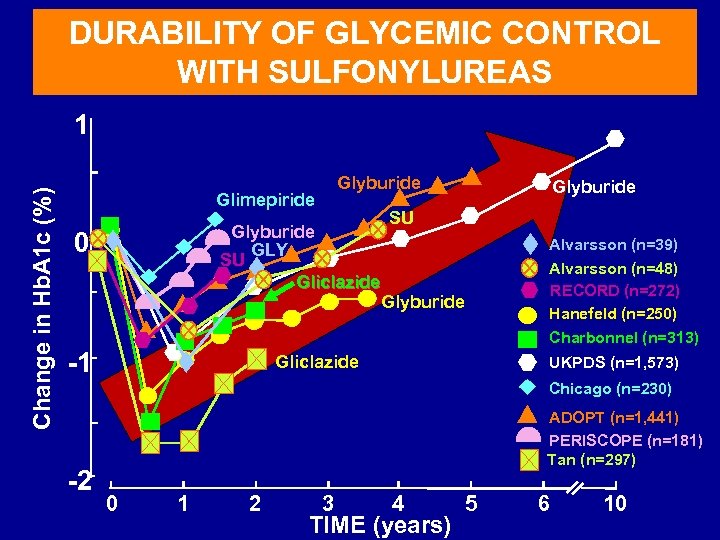
DURABILITY OF GLYCEMIC CONTROL WITH SULFONYLUREAS Change in Hb. A 1 c (%) 1 Glyburide Glimepiride Glyburide GLY SU Gliclazide 0 Glyburide SU Alvarsson (n=39) Alvarsson (n=48) RECORD (n=272) Hanefeld (n=250) Glyburide Charbonnel (n=313) -1 Gliclazide UKPDS (n=1, 573) Chicago (n=230) -2 ADOPT (n=1, 441) PERISCOPE (n=181) Tan (n=297) 0 1 2 3 4 TIME (years) 5 6 10
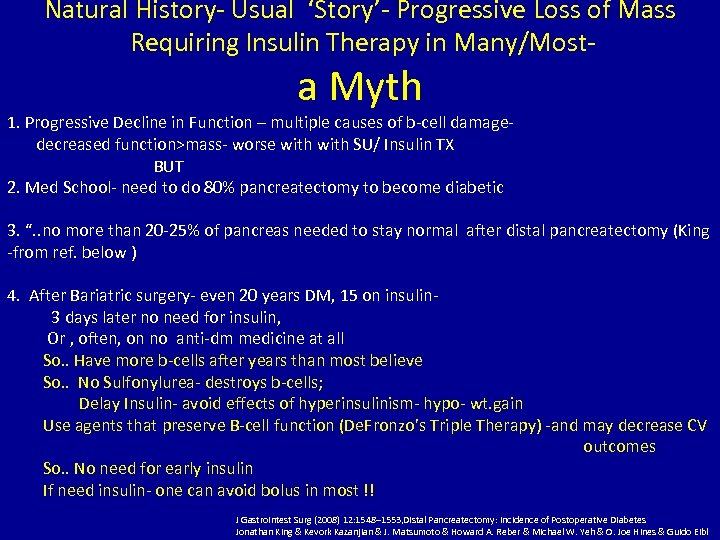
Natural History- Usual ‘Story’- Progressive Loss of Mass Requiring Insulin Therapy in Many/Most- a Myth 1. Progressive Decline in Function – multiple causes of b-cell damage decreased function>mass- worse with SU/ Insulin TX BUT 2. Med School- need to do 80% pancreatectomy to become diabetic 3. “. . no more than 20 -25% of pancreas needed to stay normal after distal pancreatectomy (King -from ref. below ). 4. After Bariatric surgery- even 20 years DM, 15 on insulin 3 days later no need for insulin, Or , often, on no anti-dm medicine at all So. . Have more b-cells after years than most believe So. . No Sulfonylurea- destroys b-cells; Delay Insulin- avoid effects of hyperinsulinism- hypo- wt. gain Use agents that preserve B-cell function (De. Fronzo’s Triple Therapy) -and may decrease CV outcomes So. . No need for early insulin If need insulin- one can avoid bolus in most !! J Gastrointest Surg (2008) 12: 1548– 1553, Distal Pancreatectomy: Incidence of Postoperative Diabetes Jonathan King & Kevork Kazanjian & J. Matsumoto & Howard A. Reber & Michael W. Yeh & O. Joe Hines & Guido Eibl
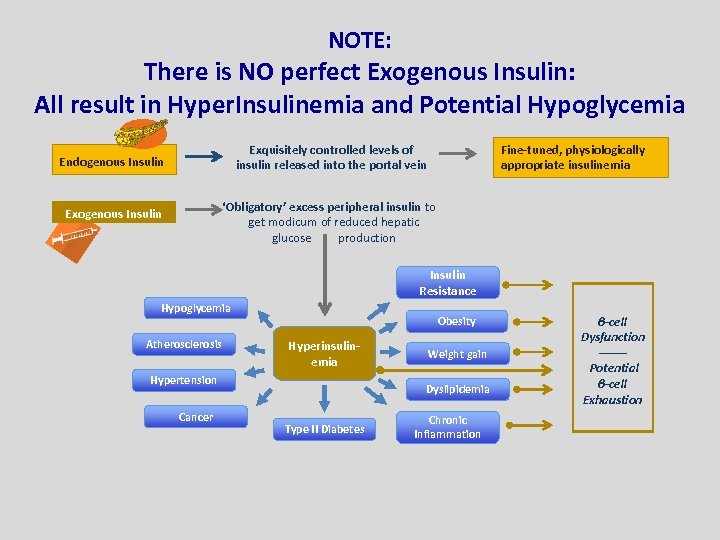
NOTE: There is NO perfect Exogenous Insulin: All result in Hyper. Insulinemia and Potential Hypoglycemia Exquisitely controlled levels of insulin released into the portal vein Endogenous Insulin Fine-tuned, physiologically appropriate insulinemia ‘Obligatory’ excess peripheral insulin to get modicum of reduced hepatic glucose production Exogenous Insulin Resistance Hypoglycemia Atherosclerosis Obesity Hyperinsulinemia Hypertension Cancer Weight gain Dyslipidemia Type II Diabetes Chronic Inflammation β-cell Dysfunction ------Potential β-cell Exhaustion
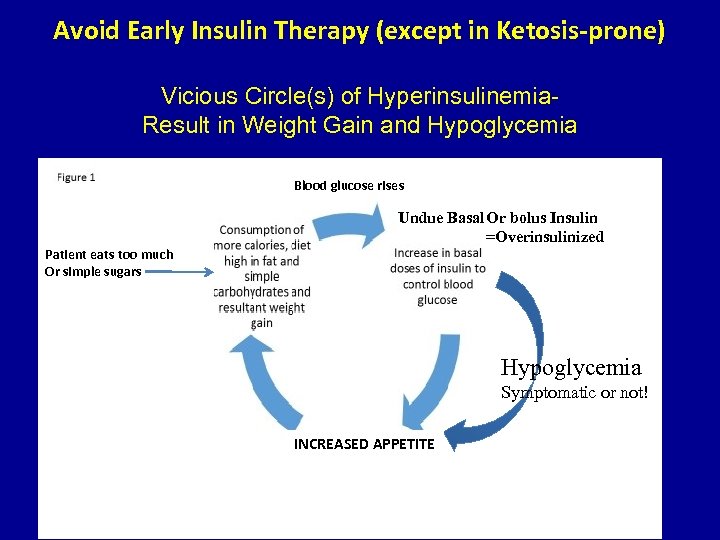
Avoid Early Insulin Therapy (except in Ketosis-prone) Vicious Circle(s) of Hyperinsulinemia. Result in Weight Gain and Hypoglycemia Blood glucose rises Undue Basal Or bolus Insulin =Overinsulinized Patient eats too much Or simple sugars Hypoglycemia Symptomatic or not! INCREASED APPETITE
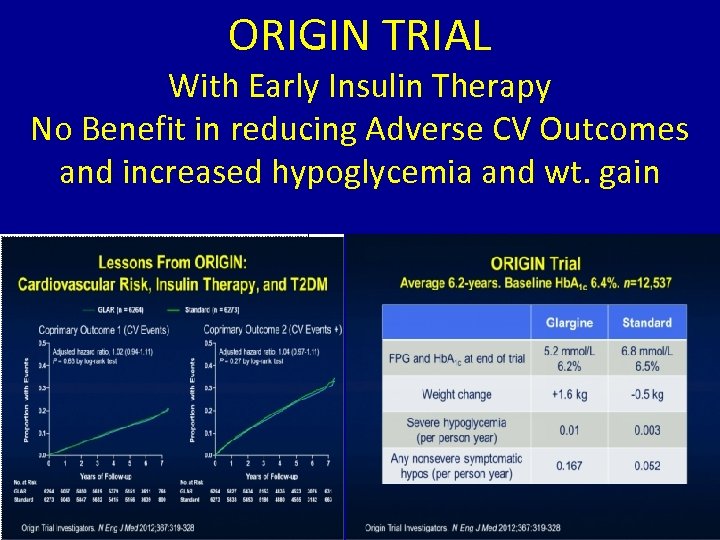
ORIGIN TRIAL With Early Insulin Therapy No Benefit in reducing Adverse CV Outcomes and increased hypoglycemia and wt. gain
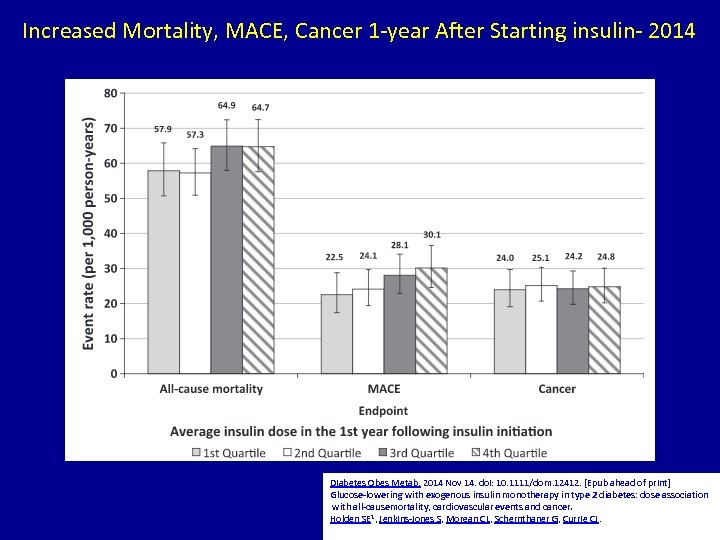
Increased Mortality, MACE, Cancer 1 -year After Starting insulin- 2014 Diabetes Obes Metab. 2014 Nov 14. doi: 10. 1111/dom. 12412. [Epub ahead of print] Glucose-lowering with exogenous insulin monotherapy in type 2 diabetes: dose association with all-causemortality, cardiovascular events and cancer. Holden SE 1, Jenkins-Jones S, Morgan CL, Schernthaner G, Currie CJ.
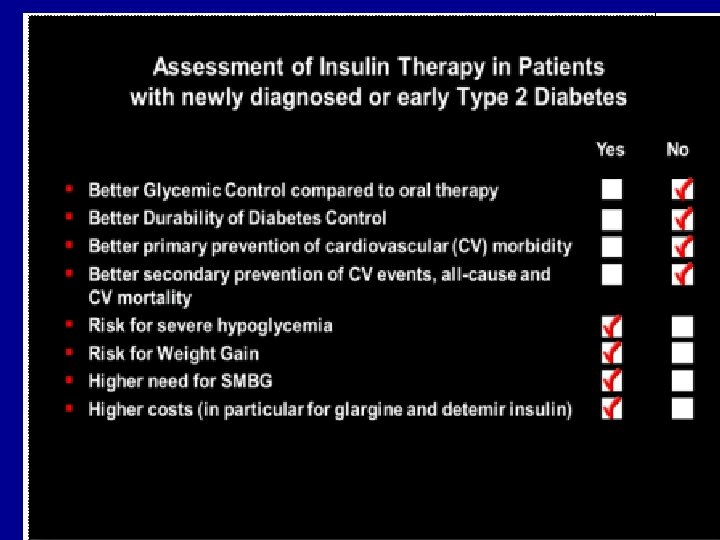
Value to Early Insulin Therapy. Outweighed By Hypoglycemia Weight Gain ….
07267cba38a81848503a132a2e16a2ab.ppt