2fb633c94cfbfb23a148781681b22511.ppt
- Количество слайдов: 87
 Improving Performance in Practice (IPIP) Change Package Coaching Practices Improving Healthcare State by State Martha Rome, RN, MPH Milwaukee, WI February 11, 2009 1
Improving Performance in Practice (IPIP) Change Package Coaching Practices Improving Healthcare State by State Martha Rome, RN, MPH Milwaukee, WI February 11, 2009 1
 Aims of IPIP • To dramatically improve patient outcomes by transforming the way we deliver primary care, focusing initially on measurable improvement in diabetes and asthma, but rapidly spreading to preventive services and other conditions • To assist different types of practices in using practice redesign strategies to improve efficiency and implement best practices • To align efforts and motivate action at the national, regional, state, practice and patient level 2
Aims of IPIP • To dramatically improve patient outcomes by transforming the way we deliver primary care, focusing initially on measurable improvement in diabetes and asthma, but rapidly spreading to preventive services and other conditions • To assist different types of practices in using practice redesign strategies to improve efficiency and implement best practices • To align efforts and motivate action at the national, regional, state, practice and patient level 2
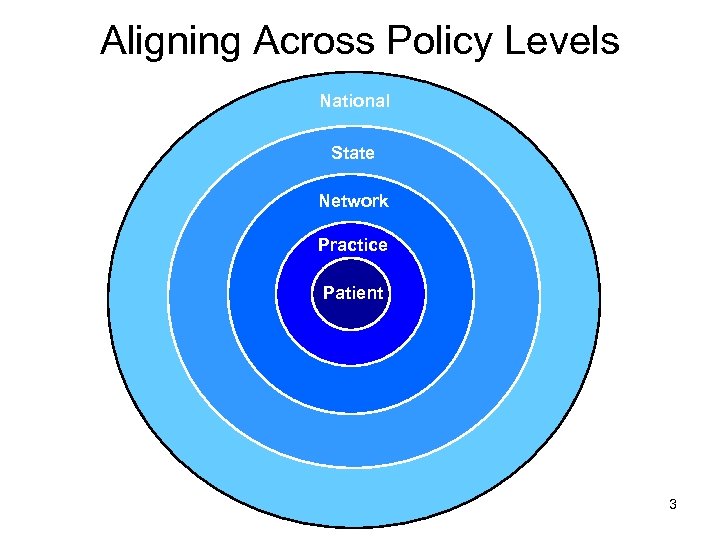 Aligning Across Policy Levels National State Network Practice Patient 3
Aligning Across Policy Levels National State Network Practice Patient 3
 Build will on state level and create state infrastructure • National specialty societies work through state chapters • Specialty Boards provide clear expectations for maintenance of certification • Partner with other organizations in the state – AHEC, QIO, payers, businesses, state government • Aligning state efforts creates the IPIP model • National Team supports states with: – – – Standard protocols Decision support tools Access to other practices who’ve done this work successfully Access to experts in the field Data aggregation and reports 4
Build will on state level and create state infrastructure • National specialty societies work through state chapters • Specialty Boards provide clear expectations for maintenance of certification • Partner with other organizations in the state – AHEC, QIO, payers, businesses, state government • Aligning state efforts creates the IPIP model • National Team supports states with: – – – Standard protocols Decision support tools Access to other practices who’ve done this work successfully Access to experts in the field Data aggregation and reports 4
 Model • Improvement networks/collaboratives • Quality Improvement Coaches: Support individual practices and improvement networks – Onsite consulting – Group meetings (in person and phone) • Reporting: monthly submission of performance measures 5
Model • Improvement networks/collaboratives • Quality Improvement Coaches: Support individual practices and improvement networks – Onsite consulting – Group meetings (in person and phone) • Reporting: monthly submission of performance measures 5
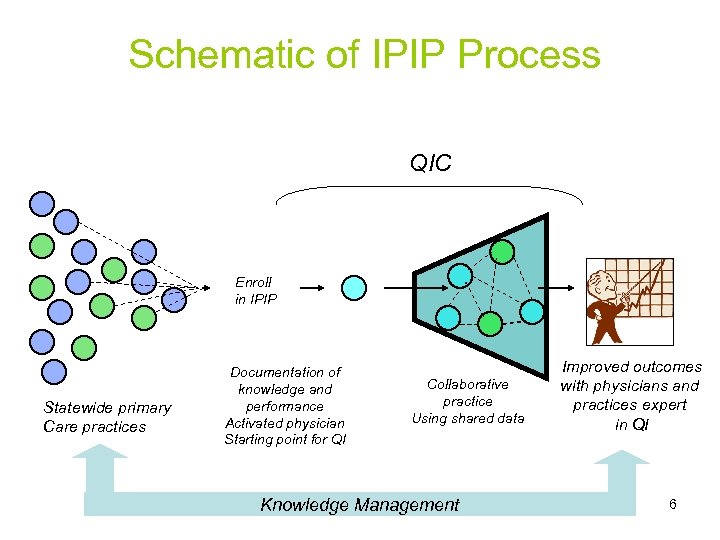 Schematic of IPIP Process QIC Enroll in IPIP Statewide primary Care practices Documentation of knowledge and performance Activated physician Starting point for QI Collaborative practice Using shared data Knowledge Management Improved outcomes with physicians and practices expert in QI 6
Schematic of IPIP Process QIC Enroll in IPIP Statewide primary Care practices Documentation of knowledge and performance Activated physician Starting point for QI Collaborative practice Using shared data Knowledge Management Improved outcomes with physicians and practices expert in QI 6
 Role of Quality Improvement Coaches • Intensive (often) on-site work with the practice team • Provide avenue to network activities and share best practices • Focused approach for implementation starting with key process changes – Move practices faster for basic implementation – Create group momentum with regard to implementation and standardization • Help practices ensure that all IPIP changes are implemented • Assist practices in developing teams & standardized work flow • Provide examples of tools (standing orders) and roles • Assist practices with regular monitoring of 7 implementation to ensure reliability
Role of Quality Improvement Coaches • Intensive (often) on-site work with the practice team • Provide avenue to network activities and share best practices • Focused approach for implementation starting with key process changes – Move practices faster for basic implementation – Create group momentum with regard to implementation and standardization • Help practices ensure that all IPIP changes are implemented • Assist practices in developing teams & standardized work flow • Provide examples of tools (standing orders) and roles • Assist practices with regular monitoring of 7 implementation to ensure reliability
 Living with chronic illness is like piloting a small plane 8
Living with chronic illness is like piloting a small plane 8
 To get safely to their destination pilots need: • Flight instruction • Preventive Maintenance • Safe Flight Plan • Air Traffic Control Surveillance • Self-Management Support • Effective Clinical Management • Treatment Plan • Close Follow-up 9
To get safely to their destination pilots need: • Flight instruction • Preventive Maintenance • Safe Flight Plan • Air Traffic Control Surveillance • Self-Management Support • Effective Clinical Management • Treatment Plan • Close Follow-up 9
 Usual care works well if your plane is about to crash 10
Usual care works well if your plane is about to crash 10
 The IOM Quality Report: Selected Quotes • “The current care systems cannot do the job. ” • “Trying harder will not work. ” • “Changing care systems will. ” 11
The IOM Quality Report: Selected Quotes • “The current care systems cannot do the job. ” • “Trying harder will not work. ” • “Changing care systems will. ” 11
 The Watchword Systems are perfectly designed to get the results they achieve 12
The Watchword Systems are perfectly designed to get the results they achieve 12
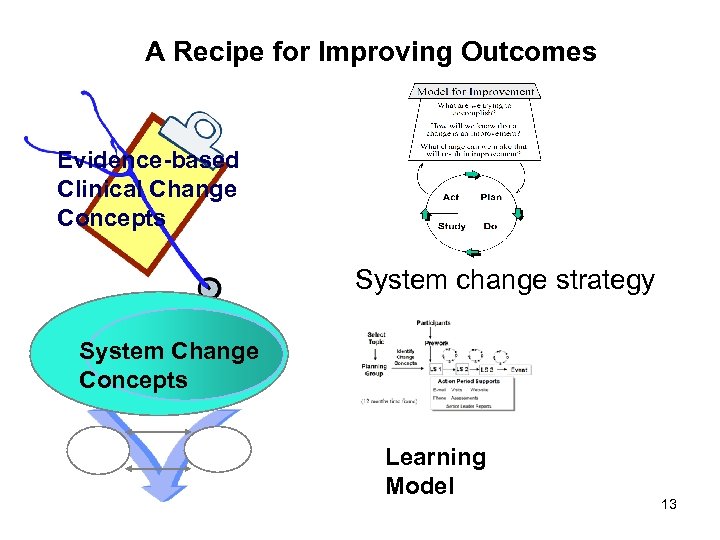 A Recipe for Improving Outcomes Evidence-based Clinical Change Concepts System change strategy System Change Concepts Learning Model 13
A Recipe for Improving Outcomes Evidence-based Clinical Change Concepts System change strategy System Change Concepts Learning Model 13
 Advantages of a General System Change Model • Applicable to most preventive and chronic care issues • Once system changes in place, accommodating new guideline or innovation much easier • Early participants in our collaboratives using it comprehensively 14
Advantages of a General System Change Model • Applicable to most preventive and chronic care issues • Once system changes in place, accommodating new guideline or innovation much easier • Early participants in our collaboratives using it comprehensively 14
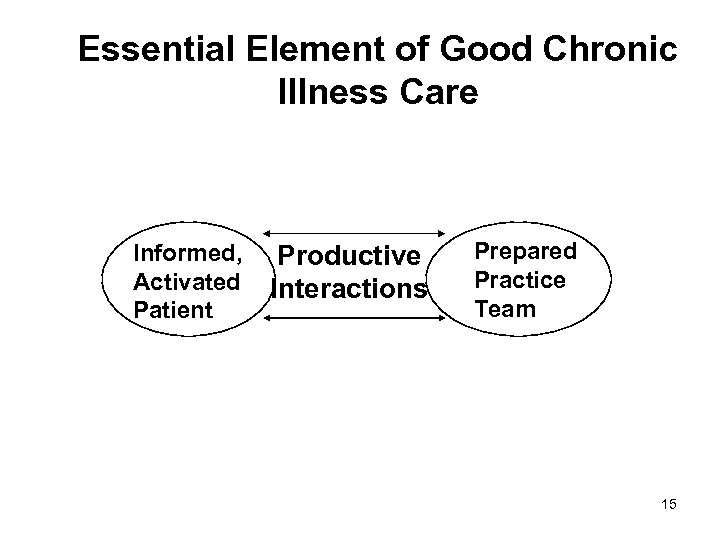 Essential Element of Good Chronic Illness Care Informed, Activated Patient Productive Interactions Prepared Practice Team 15
Essential Element of Good Chronic Illness Care Informed, Activated Patient Productive Interactions Prepared Practice Team 15
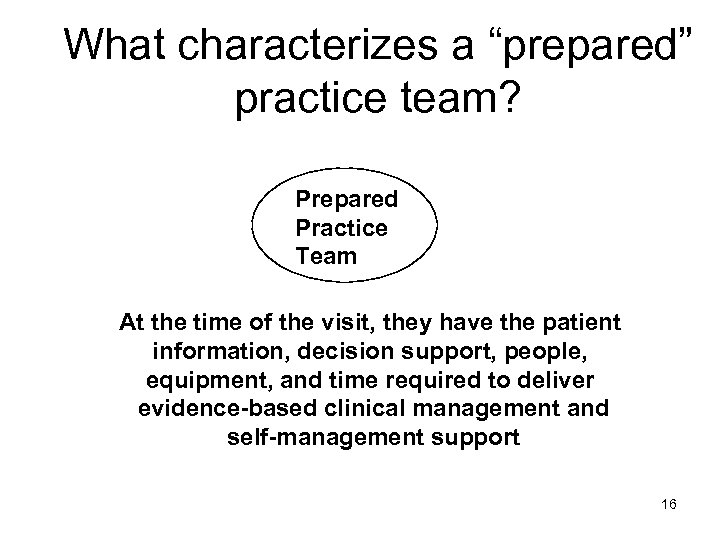 What characterizes a “prepared” practice team? Prepared Practice Team At the time of the visit, they have the patient information, decision support, people, equipment, and time required to deliver evidence-based clinical management and self-management support 16
What characterizes a “prepared” practice team? Prepared Practice Team At the time of the visit, they have the patient information, decision support, people, equipment, and time required to deliver evidence-based clinical management and self-management support 16
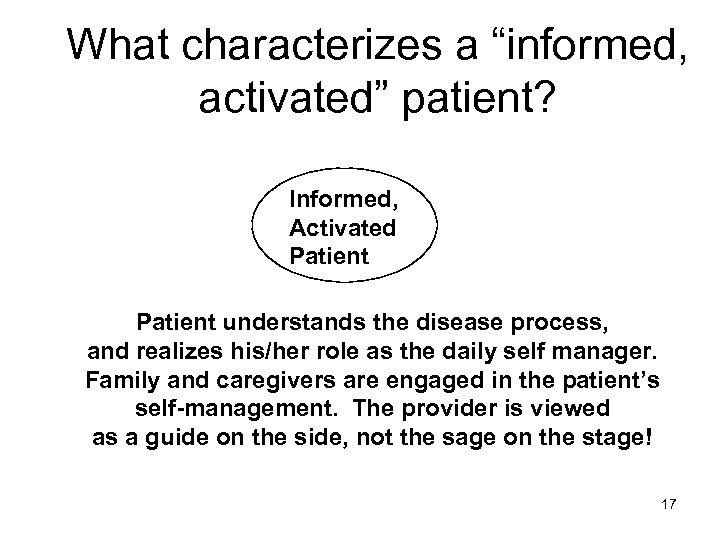 What characterizes a “informed, activated” patient? Informed, Activated Patient understands the disease process, and realizes his/her role as the daily self manager. Family and caregivers are engaged in the patient’s self-management. The provider is viewed as a guide on the side, not the sage on the stage! 17
What characterizes a “informed, activated” patient? Informed, Activated Patient understands the disease process, and realizes his/her role as the daily self manager. Family and caregivers are engaged in the patient’s self-management. The provider is viewed as a guide on the side, not the sage on the stage! 17
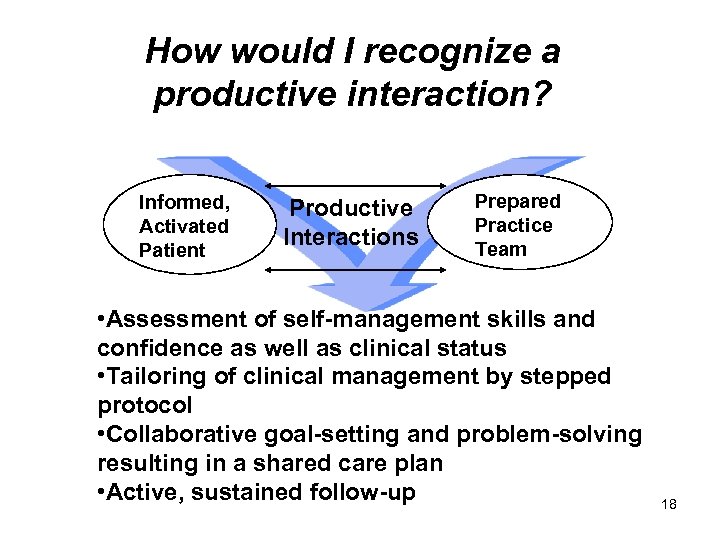 How would I recognize a productive interaction? Informed, Activated Patient Productive Interactions Prepared Practice Team • Assessment of self-management skills and confidence as well as clinical status • Tailoring of clinical management by stepped protocol • Collaborative goal-setting and problem-solving resulting in a shared care plan • Active, sustained follow-up 18
How would I recognize a productive interaction? Informed, Activated Patient Productive Interactions Prepared Practice Team • Assessment of self-management skills and confidence as well as clinical status • Tailoring of clinical management by stepped protocol • Collaborative goal-setting and problem-solving resulting in a shared care plan • Active, sustained follow-up 18
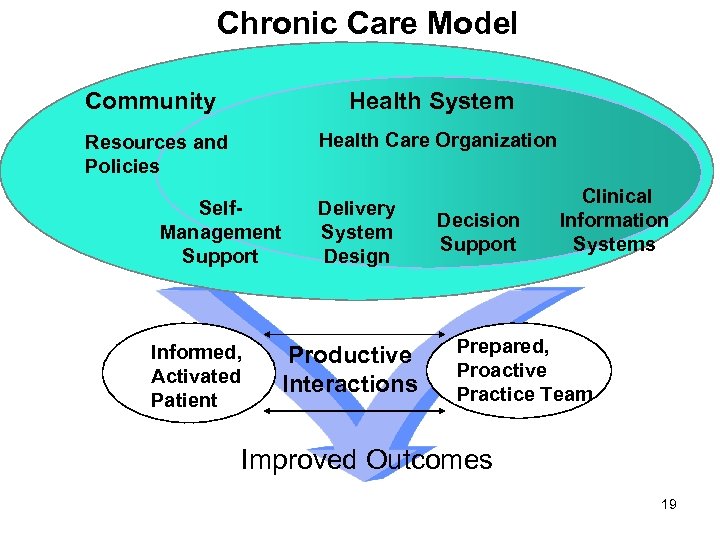 Chronic Care Model Community Health System Health Care Organization Resources and Policies Self. Management Support Informed, Activated Patient Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team Improved Outcomes 19
Chronic Care Model Community Health System Health Care Organization Resources and Policies Self. Management Support Informed, Activated Patient Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team Improved Outcomes 19
 Clinical Information System • Provide reminders for providers and patients. • Identify relevant patient subpopulations for proactive care. • Facilitate individual patient care planning. • Share information with providers and patients. • Monitor performance of team and system. 20
Clinical Information System • Provide reminders for providers and patients. • Identify relevant patient subpopulations for proactive care. • Facilitate individual patient care planning. • Share information with providers and patients. • Monitor performance of team and system. 20
 Delivery System Design • Define roles and distribute tasks amongst team members. • Use planned interactions to support evidencebased care. • Provide clinical case management services. • Ensure regular follow-up. • Give care that patients understand that fits their culture 21
Delivery System Design • Define roles and distribute tasks amongst team members. • Use planned interactions to support evidencebased care. • Provide clinical case management services. • Ensure regular follow-up. • Give care that patients understand that fits their culture 21
 Self-management Support • Emphasize the patient's central role. • Use effective self-management support strategies that include assessment, goalsetting, action planning, problem-solving and follow-up. • Organize resources to provide support 22
Self-management Support • Emphasize the patient's central role. • Use effective self-management support strategies that include assessment, goalsetting, action planning, problem-solving and follow-up. • Organize resources to provide support 22
 To Change Outcomes (e. g. , Hb. A 1 c) Requires Fundamental Practice Change • Interventions focused on guidelines, feedback, and role changes can improve processes • Interventions that address more than one area have more impact • Interventions that are patientcentered change outcomes. Renders et al, Diabetes Care, 2001; 24: 1821 23
To Change Outcomes (e. g. , Hb. A 1 c) Requires Fundamental Practice Change • Interventions focused on guidelines, feedback, and role changes can improve processes • Interventions that address more than one area have more impact • Interventions that are patientcentered change outcomes. Renders et al, Diabetes Care, 2001; 24: 1821 23
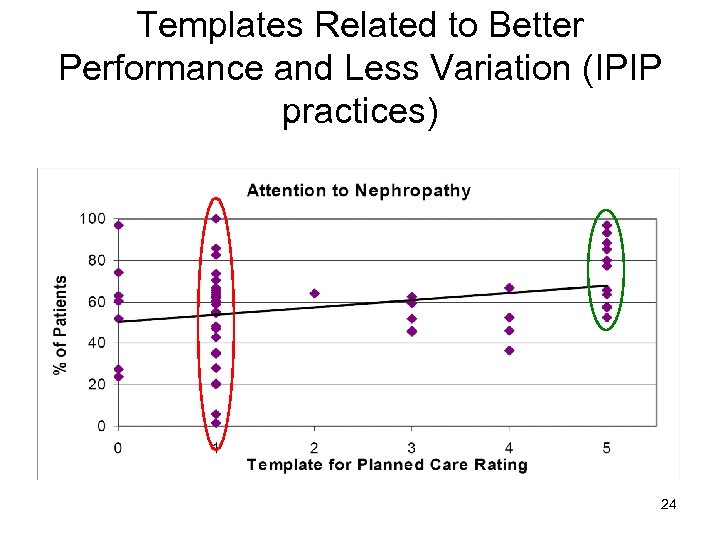 Templates Related to Better Performance and Less Variation (IPIP practices) 24
Templates Related to Better Performance and Less Variation (IPIP practices) 24
 IPIP Change Package • High-leverage Changes – Implement Registry – Use Template for Planned Care – Use Protocols – Adopt Self-management Support Strategies 25
IPIP Change Package • High-leverage Changes – Implement Registry – Use Template for Planned Care – Use Protocols – Adopt Self-management Support Strategies 25
 Implement IPIP Changes in Steps 1. Use Registry to identify asthmatics/diabetics prior to visit (this requires the work of implementing a registry or “fixing” the EHR) Use condition-specific decision support tool (e. g. , visit planner) Create customized flow diagram and protocols to standardize the care process 2. 3. • • • 4. Nursing Standing Orders to increase reliable execution [examples] Standard Protocol [example] Specific Care Team roles: who does what in the protocol Implement a self-management support system Throughout: Frequent monitoring of reliability and investigation of failures for ideas about how to improve standard performance 26
Implement IPIP Changes in Steps 1. Use Registry to identify asthmatics/diabetics prior to visit (this requires the work of implementing a registry or “fixing” the EHR) Use condition-specific decision support tool (e. g. , visit planner) Create customized flow diagram and protocols to standardize the care process 2. 3. • • • 4. Nursing Standing Orders to increase reliable execution [examples] Standard Protocol [example] Specific Care Team roles: who does what in the protocol Implement a self-management support system Throughout: Frequent monitoring of reliability and investigation of failures for ideas about how to improve standard performance 26
 Detailed Changes: Registry 1) Select and install a registry tool 2) Determine staff workflow to support registry use 3) Populate registry with patient data 4) Routinely maintain registry data 5) Use registry to manage patient care and support population management 27
Detailed Changes: Registry 1) Select and install a registry tool 2) Determine staff workflow to support registry use 3) Populate registry with patient data 4) Routinely maintain registry data 5) Use registry to manage patient care and support population management 27
 Detailed Changes: Templates 1) Select template tool from registry or create a flow sheet 2) Determine staff workflow to support use of template 3) Use template with all patients 4) Ensure registry updated each time template used 5) Monitor use of template 28
Detailed Changes: Templates 1) Select template tool from registry or create a flow sheet 2) Determine staff workflow to support use of template 3) Use template with all patients 4) Ensure registry updated each time template used 5) Monitor use of template 28
 Detailed Changes: Protocols Step 3: Use Protocols a. Select and customize evidence-based protocols to office b. Determine staff workflow to support protocols, including standing orders c. Use protocols with all patients d. Monitor use of protocols 29
Detailed Changes: Protocols Step 3: Use Protocols a. Select and customize evidence-based protocols to office b. Determine staff workflow to support protocols, including standing orders c. Use protocols with all patients d. Monitor use of protocols 29
 Protocols: Asthma-specific • Assess and document asthma severity and control • Prescribe appropriate asthma medications and monitor overuse of beta agonists • Use Asthma Management plans • Establish visit frequency protocol • Assess and treat co-morbidities • Assess, counsel, and prevent exposure to environmental triggers 30
Protocols: Asthma-specific • Assess and document asthma severity and control • Prescribe appropriate asthma medications and monitor overuse of beta agonists • Use Asthma Management plans • Establish visit frequency protocol • Assess and treat co-morbidities • Assess, counsel, and prevent exposure to environmental triggers 30
 Protocols: Diabetes Check and treat BP <130/80 Check and treat cholesterol Check A 1 C and treat hyperglycemia Assess aspirin and prescribe if not using Assess need for eye exam and make referral if needed • Assess nephropathy risk • Perform foot exam • Provide appropriate vaccines • • • 31
Protocols: Diabetes Check and treat BP <130/80 Check and treat cholesterol Check A 1 C and treat hyperglycemia Assess aspirin and prescribe if not using Assess need for eye exam and make referral if needed • Assess nephropathy risk • Perform foot exam • Provide appropriate vaccines • • • 31
 Self-management Support • Obtain patient education materials (e. g. , asthma action plans) • Determine staff workflow to support SMS • Provide training to staff in SMS techniques • Set patient goals collaboratively • Document and monitor patient progress toward goals • Link with community resources (schools, service organizations) 32
Self-management Support • Obtain patient education materials (e. g. , asthma action plans) • Determine staff workflow to support SMS • Provide training to staff in SMS techniques • Set patient goals collaboratively • Document and monitor patient progress toward goals • Link with community resources (schools, service organizations) 32
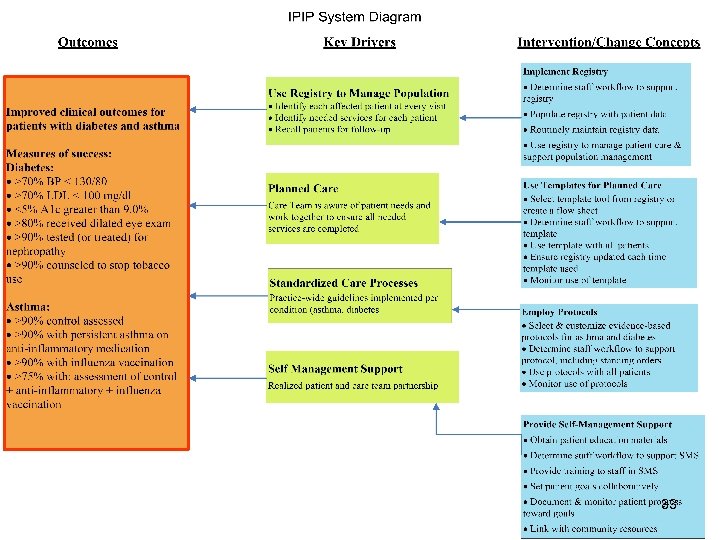 33
33
 Cincinnati Children’s Hospital PHO • 44 geographically dispersed, sites • Individual models and styles of practice • “First Wins” – Early adoption of registry – Concurrent data collection: written parent symptom review and clinical interview 34
Cincinnati Children’s Hospital PHO • 44 geographically dispersed, sites • Individual models and styles of practice • “First Wins” – Early adoption of registry – Concurrent data collection: written parent symptom review and clinical interview 34
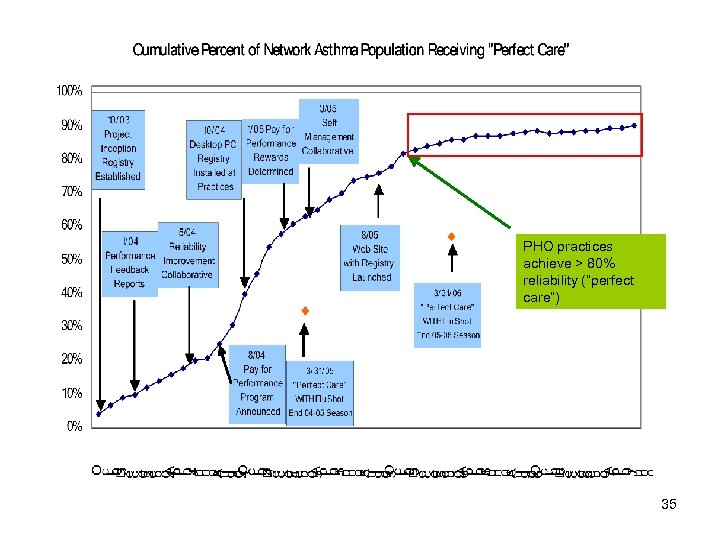 BMF Included PHO practices achieve > 80% reliability (“perfect care”) 35
BMF Included PHO practices achieve > 80% reliability (“perfect care”) 35
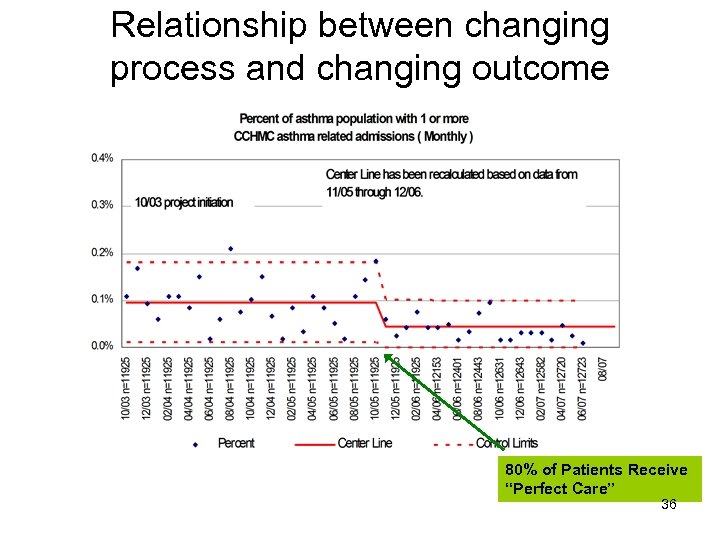 Relationship between changing process and changing outcome 80% of Patients Receive “Perfect Care” 36
Relationship between changing process and changing outcome 80% of Patients Receive “Perfect Care” 36
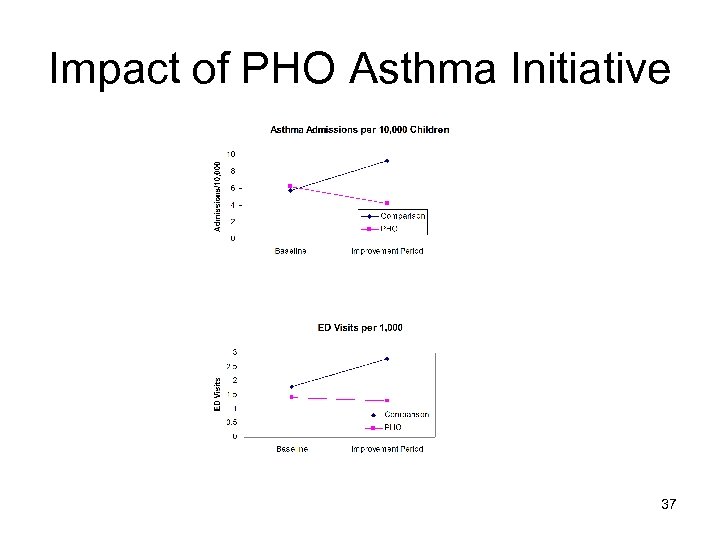 Impact of PHO Asthma Initiative 37
Impact of PHO Asthma Initiative 37
 UNITE HERE Health Center l Founded 1914 by ILGWU l Union mergers over the years, now UNITE HERE l Comprehensive Primary and Specialty Care Serves predominantly UNITE HERE members, their families and retirees and SEIU 32 BJ members l l 1000 office visits/week l 12 PCP’s, 40 specialists, all staff bilingual On Site Physical Therapy, Radiology and Pharmacy l 38
UNITE HERE Health Center l Founded 1914 by ILGWU l Union mergers over the years, now UNITE HERE l Comprehensive Primary and Specialty Care Serves predominantly UNITE HERE members, their families and retirees and SEIU 32 BJ members l l 1000 office visits/week l 12 PCP’s, 40 specialists, all staff bilingual On Site Physical Therapy, Radiology and Pharmacy l 38
 Primary Care Teams l High functioning multidisciplinary teams with 2 hours protected meeting time every other week l Huddles –Led by MA who does chart reviews day before –First 20 minute appointment blocked –Identify patients for health coach interventions l Cell phones and walkie-talkies Protocols developed & incorporated into EMR templates l 39
Primary Care Teams l High functioning multidisciplinary teams with 2 hours protected meeting time every other week l Huddles –Led by MA who does chart reviews day before –First 20 minute appointment blocked –Identify patients for health coach interventions l Cell phones and walkie-talkies Protocols developed & incorporated into EMR templates l 39
 Teamwork • PCAs trained in monofilament testing, glucose diaries and ABC cards • Standing orders for Pneumovax and ophthalmology appointments • Pharmacy gets A 1 C lists for medication review • Health Coaches for DM education, self management goal setting, BP checks and blood glucose checks 40
Teamwork • PCAs trained in monofilament testing, glucose diaries and ABC cards • Standing orders for Pneumovax and ophthalmology appointments • Pharmacy gets A 1 C lists for medication review • Health Coaches for DM education, self management goal setting, BP checks and blood glucose checks 40
 Transforming Medical Assistants into Health Coaches l Curriculum developed for in-house training l Didactic and observational testing Promotion to “Health Coach” after competency evaluation l Supervision by Nurse Practitioner and RN coordinator l 41
Transforming Medical Assistants into Health Coaches l Curriculum developed for in-house training l Didactic and observational testing Promotion to “Health Coach” after competency evaluation l Supervision by Nurse Practitioner and RN coordinator l 41
 Evidence Based Care • All providers use the DM template • Review and discussion of data at provider meetings • DM always on the agenda • Provider educational seminars • Provider chart reviews 42
Evidence Based Care • All providers use the DM template • Review and discussion of data at provider meetings • DM always on the agenda • Provider educational seminars • Provider chart reviews 42
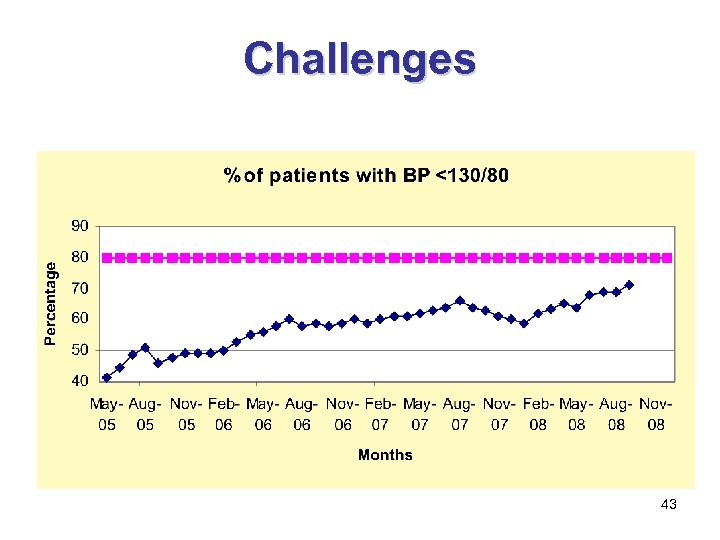 Challenges 43
Challenges 43
 Focus on Hypertension • Reinforced • • use of BP check visit – patient sees RN or Health Coach New protocol and training for MA to recheck BP if high prior to seeing PCP BP Loan Program Chart Reviews Discussion with PCPs at monthly meeting 44
Focus on Hypertension • Reinforced • • use of BP check visit – patient sees RN or Health Coach New protocol and training for MA to recheck BP if high prior to seeing PCP BP Loan Program Chart Reviews Discussion with PCPs at monthly meeting 44
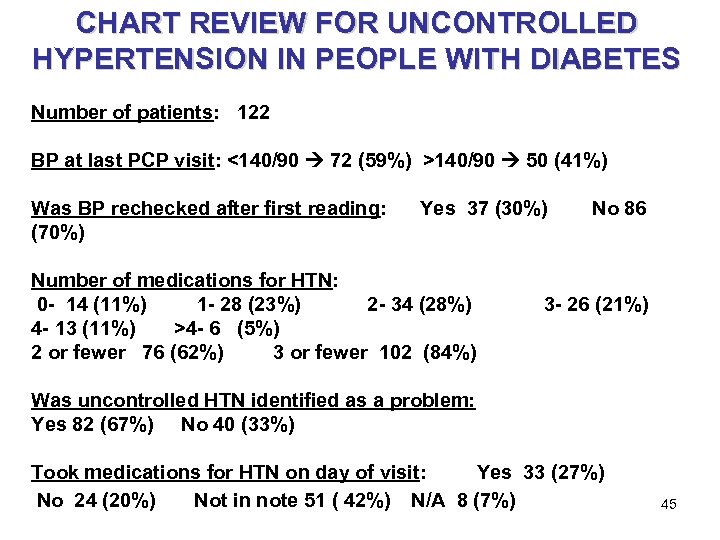 CHART REVIEW FOR UNCONTROLLED HYPERTENSION IN PEOPLE WITH DIABETES Number of patients: 122 BP at last PCP visit: <140/90 72 (59%) >140/90 50 (41%) Was BP rechecked after first reading: Yes 37 (30%) No 86 (70%) Number of medications for HTN: 0 - 14 (11%) 1 - 28 (23%) 2 - 34 (28%) 3 - 26 (21%) 4 - 13 (11%) >4 - 6 (5%) 2 or fewer 76 (62%) 3 or fewer 102 (84%) Was uncontrolled HTN identified as a problem: Yes 82 (67%) No 40 (33%) Took medications for HTN on day of visit: Yes 33 (27%) No 24 (20%) Not in note 51 ( 42%) N/A 8 (7%) 45
CHART REVIEW FOR UNCONTROLLED HYPERTENSION IN PEOPLE WITH DIABETES Number of patients: 122 BP at last PCP visit: <140/90 72 (59%) >140/90 50 (41%) Was BP rechecked after first reading: Yes 37 (30%) No 86 (70%) Number of medications for HTN: 0 - 14 (11%) 1 - 28 (23%) 2 - 34 (28%) 3 - 26 (21%) 4 - 13 (11%) >4 - 6 (5%) 2 or fewer 76 (62%) 3 or fewer 102 (84%) Was uncontrolled HTN identified as a problem: Yes 82 (67%) No 40 (33%) Took medications for HTN on day of visit: Yes 33 (27%) No 24 (20%) Not in note 51 ( 42%) N/A 8 (7%) 45
 PCP Discussions • Monthly PCP meetings • Results of chart reviews drive PCP • • • discussion Discuss clinical management of HTN Ask PCP with best results – what do you do? Share best practices - start with combination drugs 46
PCP Discussions • Monthly PCP meetings • Results of chart reviews drive PCP • • • discussion Discuss clinical management of HTN Ask PCP with best results – what do you do? Share best practices - start with combination drugs 46
 PCP Discussions • Identifies common misconceptions – • “uncontrolled patients are already on maximal doses of medications” Identifies target for improvement – importance of rechecking BP if uncontrolled and asking if patients took their medications on the day of the visit 47
PCP Discussions • Identifies common misconceptions – • “uncontrolled patients are already on maximal doses of medications” Identifies target for improvement – importance of rechecking BP if uncontrolled and asking if patients took their medications on the day of the visit 47
 The Multidisciplinary Team: The key to successful planned diabetes care and quality improvement in our practice Robb Malone, Pharm. D UNC General Internal Medicine January 20, 2009 48
The Multidisciplinary Team: The key to successful planned diabetes care and quality improvement in our practice Robb Malone, Pharm. D UNC General Internal Medicine January 20, 2009 48
 Water cooler discussions Change is scary leadership requires necessary complicated an opportunity Successfulhard change towell designed, active a improve team 49
Water cooler discussions Change is scary leadership requires necessary complicated an opportunity Successfulhard change towell designed, active a improve team 49
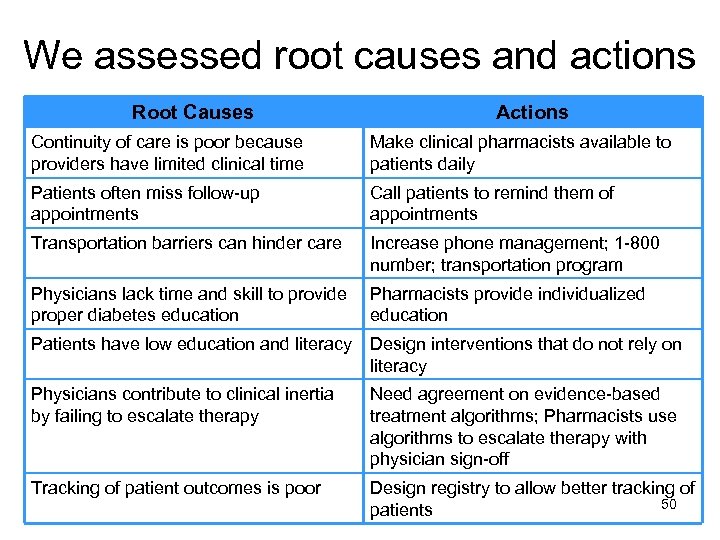 We assessed root causes and actions Root Causes Actions Continuity of care is poor because providers have limited clinical time Make clinical pharmacists available to patients daily Patients often miss follow-up appointments Call patients to remind them of appointments Transportation barriers can hinder care Increase phone management; 1 -800 number; transportation program Physicians lack time and skill to provide proper diabetes education Pharmacists provide individualized education Patients have low education and literacy Design interventions that do not rely on literacy Physicians contribute to clinical inertia by failing to escalate therapy Need agreement on evidence-based treatment algorithms; Pharmacists use algorithms to escalate therapy with physician sign-off Tracking of patient outcomes is poor Design registry to allow better tracking of 50 patients
We assessed root causes and actions Root Causes Actions Continuity of care is poor because providers have limited clinical time Make clinical pharmacists available to patients daily Patients often miss follow-up appointments Call patients to remind them of appointments Transportation barriers can hinder care Increase phone management; 1 -800 number; transportation program Physicians lack time and skill to provide proper diabetes education Pharmacists provide individualized education Patients have low education and literacy Design interventions that do not rely on literacy Physicians contribute to clinical inertia by failing to escalate therapy Need agreement on evidence-based treatment algorithms; Pharmacists use algorithms to escalate therapy with physician sign-off Tracking of patient outcomes is poor Design registry to allow better tracking of 50 patients
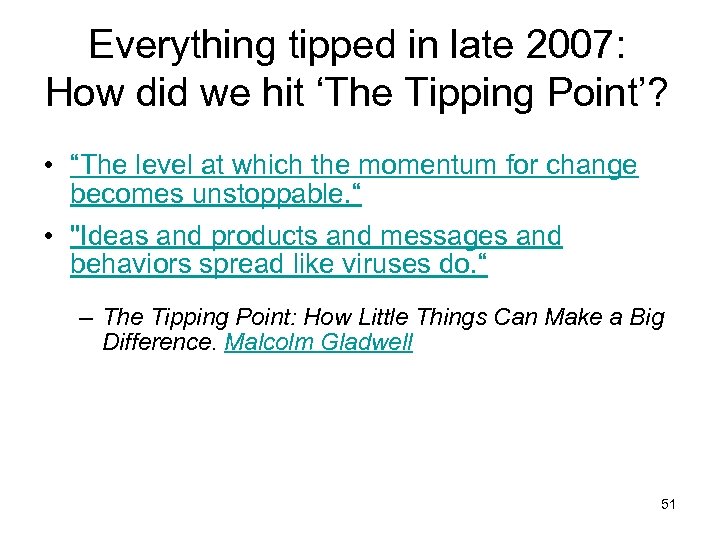 Everything tipped in late 2007: How did we hit ‘The Tipping Point’? • “The level at which the momentum for change becomes unstoppable. “ • "Ideas and products and messages and behaviors spread like viruses do. “ – The Tipping Point: How Little Things Can Make a Big Difference. Malcolm Gladwell Consensus driven growth that focused on the teamwork, contribution from all, and leadership development in QI Acceptance from the late majority and laggards 51
Everything tipped in late 2007: How did we hit ‘The Tipping Point’? • “The level at which the momentum for change becomes unstoppable. “ • "Ideas and products and messages and behaviors spread like viruses do. “ – The Tipping Point: How Little Things Can Make a Big Difference. Malcolm Gladwell Consensus driven growth that focused on the teamwork, contribution from all, and leadership development in QI Acceptance from the late majority and laggards 51
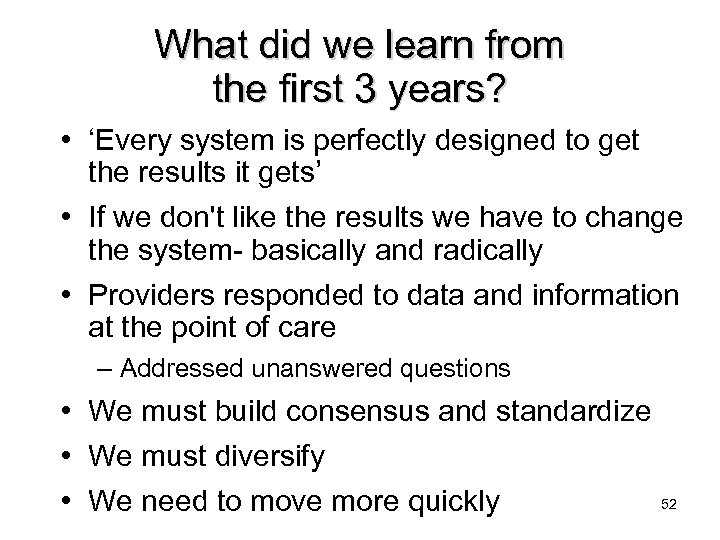 What did we learn from the first 3 years? • ‘Every system is perfectly designed to get the results it gets’ • If we don't like the results we have to change the system- basically and radically • Providers responded to data and information at the point of care – Addressed unanswered questions • We must build consensus and standardize • We must diversify • We need to move more quickly 52
What did we learn from the first 3 years? • ‘Every system is perfectly designed to get the results it gets’ • If we don't like the results we have to change the system- basically and radically • Providers responded to data and information at the point of care – Addressed unanswered questions • We must build consensus and standardize • We must diversify • We need to move more quickly 52
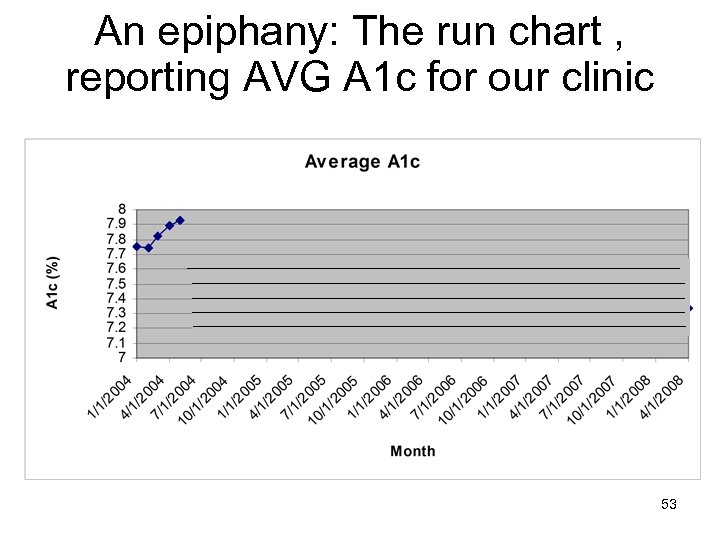 An epiphany: The run chart , reporting AVG A 1 c for our clinic 2004 53
An epiphany: The run chart , reporting AVG A 1 c for our clinic 2004 53
 Diabetes planned care • Patient registry • Robust decision support • Prompting and stratification of patients by risk – Stepped care approach • • • All patients eligible and recruited for care Patient-centered education Care coordination Expanded standardization and algorithmic care Extensive quality reporting Adoption of the Model for Improvement (MFI) 54
Diabetes planned care • Patient registry • Robust decision support • Prompting and stratification of patients by risk – Stepped care approach • • • All patients eligible and recruited for care Patient-centered education Care coordination Expanded standardization and algorithmic care Extensive quality reporting Adoption of the Model for Improvement (MFI) 54
 What we learned from 2003 to 2006 • A successful program includes: – A multidisciplinary team – A registry with decision support for proactive care – Consensus backed by evidence-based algorithms and standards • Persistence and leadership are key • Appropriately designed interventions or systems can overcome patient vulnerability • We continually evolve, change is necessary and represents opportunity – Embrace rapid cycle change and the MFI 55
What we learned from 2003 to 2006 • A successful program includes: – A multidisciplinary team – A registry with decision support for proactive care – Consensus backed by evidence-based algorithms and standards • Persistence and leadership are key • Appropriately designed interventions or systems can overcome patient vulnerability • We continually evolve, change is necessary and represents opportunity – Embrace rapid cycle change and the MFI 55
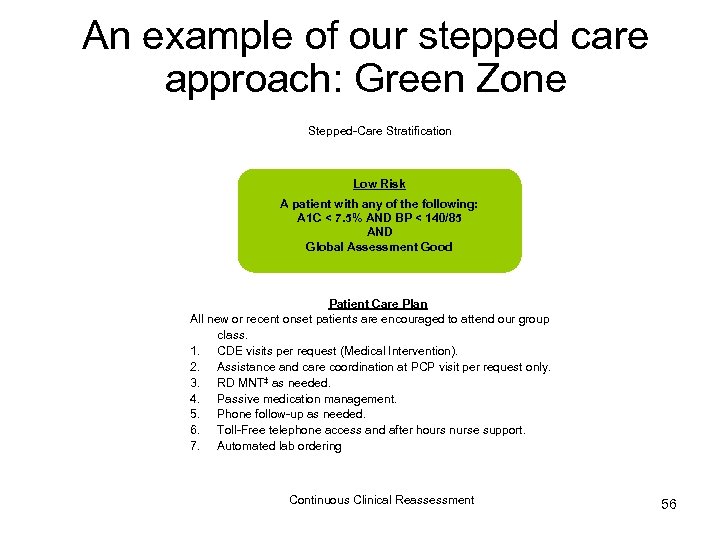 An example of our stepped care approach: Green Zone Stepped-Care Stratification ~ 40% of our patients Low Risk A patient with any of the following: A 1 C < 7. 5% AND BP < 140/85 AND Global Assessment Good Patient Care Plan All new or recent onset patients are encouraged to attend our group class. 1. CDE visits per request (Medical Intervention). 2. Assistance and care coordination at PCP visit per request only. 3. RD MNT‡ as needed. 4. Passive medication management. 5. Phone follow-up as needed. 6. Toll-Free telephone access and after hours nurse support. 7. Automated lab ordering Continuous Clinical Reassessment 56
An example of our stepped care approach: Green Zone Stepped-Care Stratification ~ 40% of our patients Low Risk A patient with any of the following: A 1 C < 7. 5% AND BP < 140/85 AND Global Assessment Good Patient Care Plan All new or recent onset patients are encouraged to attend our group class. 1. CDE visits per request (Medical Intervention). 2. Assistance and care coordination at PCP visit per request only. 3. RD MNT‡ as needed. 4. Passive medication management. 5. Phone follow-up as needed. 6. Toll-Free telephone access and after hours nurse support. 7. Automated lab ordering Continuous Clinical Reassessment 56
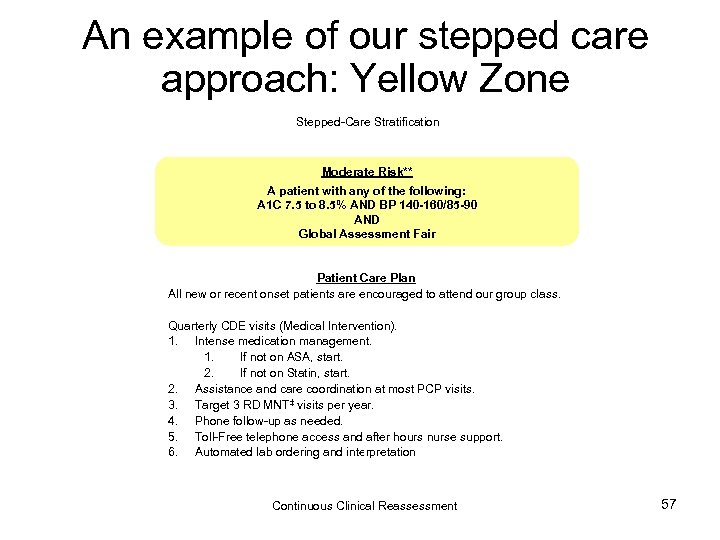 An example of our stepped care approach: Yellow Zone ~ 35% of our patients Stepped-Care Stratification Moderate Risk** A patient with any of the following: A 1 C 7. 5 to 8. 5% AND BP 140 -160/85 -90 AND Global Assessment Fair Patient Care Plan All new or recent onset patients are encouraged to attend our group class. Quarterly CDE visits (Medical Intervention). 1. Intense medication management. 1. If not on ASA, start. 2. If not on Statin, start. 2. Assistance and care coordination at most PCP visits. 3. Target 3 RD MNT‡ visits per year. 4. Phone follow-up as needed. 5. Toll-Free telephone access and after hours nurse support. 6. Automated lab ordering and interpretation Continuous Clinical Reassessment 57
An example of our stepped care approach: Yellow Zone ~ 35% of our patients Stepped-Care Stratification Moderate Risk** A patient with any of the following: A 1 C 7. 5 to 8. 5% AND BP 140 -160/85 -90 AND Global Assessment Fair Patient Care Plan All new or recent onset patients are encouraged to attend our group class. Quarterly CDE visits (Medical Intervention). 1. Intense medication management. 1. If not on ASA, start. 2. If not on Statin, start. 2. Assistance and care coordination at most PCP visits. 3. Target 3 RD MNT‡ visits per year. 4. Phone follow-up as needed. 5. Toll-Free telephone access and after hours nurse support. 6. Automated lab ordering and interpretation Continuous Clinical Reassessment 57
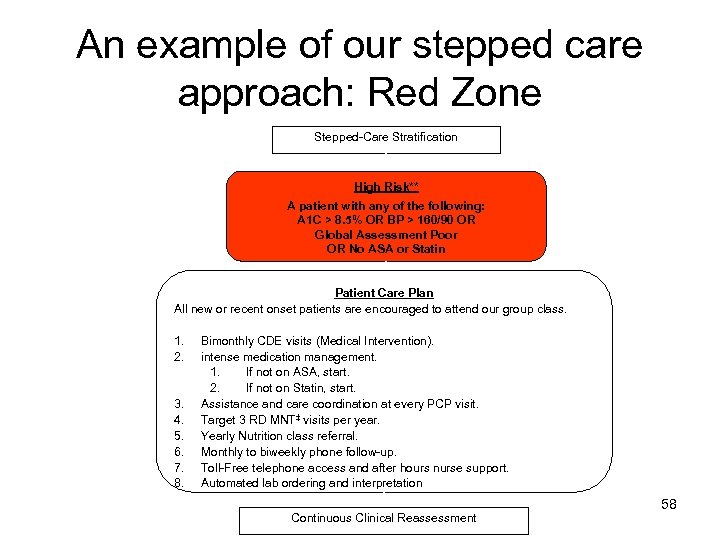 An example of our stepped care approach: Red Zone Stepped-Care Stratification ~ 25% of our patients High Risk** A patient with any of the following: A 1 C > 8. 5% OR BP > 160/90 OR Global Assessment Poor OR No ASA or Statin Patient Care Plan All new or recent onset patients are encouraged to attend our group class. 1. 2. 3. 4. 5. 6. 7. 8. Bimonthly CDE visits (Medical Intervention). intense medication management. 1. If not on ASA, start. 2. If not on Statin, start. Assistance and care coordination at every PCP visit. Target 3 RD MNT‡ visits per year. Yearly Nutrition class referral. Monthly to biweekly phone follow-up. Toll-Free telephone access and after hours nurse support. Automated lab ordering and interpretation Continuous Clinical Reassessment 58
An example of our stepped care approach: Red Zone Stepped-Care Stratification ~ 25% of our patients High Risk** A patient with any of the following: A 1 C > 8. 5% OR BP > 160/90 OR Global Assessment Poor OR No ASA or Statin Patient Care Plan All new or recent onset patients are encouraged to attend our group class. 1. 2. 3. 4. 5. 6. 7. 8. Bimonthly CDE visits (Medical Intervention). intense medication management. 1. If not on ASA, start. 2. If not on Statin, start. Assistance and care coordination at every PCP visit. Target 3 RD MNT‡ visits per year. Yearly Nutrition class referral. Monthly to biweekly phone follow-up. Toll-Free telephone access and after hours nurse support. Automated lab ordering and interpretation Continuous Clinical Reassessment 58
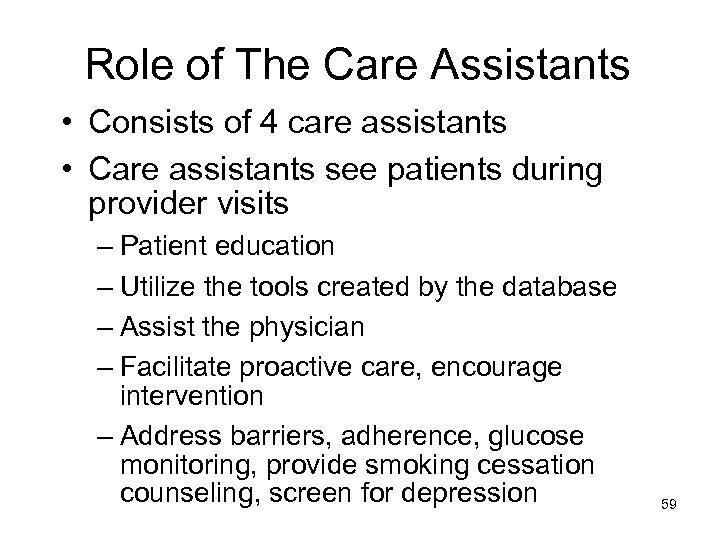 Role of The Care Assistants • Consists of 4 care assistants • Care assistants see patients during provider visits – Patient education – Utilize the tools created by the database – Assist the physician – Facilitate proactive care, encourage intervention – Address barriers, adherence, glucose monitoring, provide smoking cessation counseling, screen for depression 59
Role of The Care Assistants • Consists of 4 care assistants • Care assistants see patients during provider visits – Patient education – Utilize the tools created by the database – Assist the physician – Facilitate proactive care, encourage intervention – Address barriers, adherence, glucose monitoring, provide smoking cessation counseling, screen for depression 59
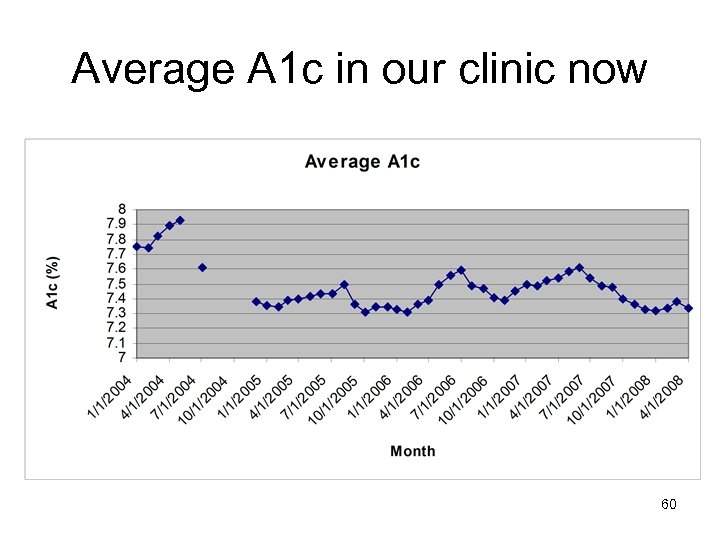 Average A 1 c in our clinic now 60
Average A 1 c in our clinic now 60
 Example 1 Lipid screening & management: A front desk intervention 61
Example 1 Lipid screening & management: A front desk intervention 61
 Status of Lipid Management September 2004 • 55% of patients had total cholesterol tested annually • Approximately 68% were prescribed statins • Average total cholesterol = 185 mg/dl • Average LDL = 99 mg/dl • We set a goal that 90% of patients would be screened annually and prescribed a statin 62
Status of Lipid Management September 2004 • 55% of patients had total cholesterol tested annually • Approximately 68% were prescribed statins • Average total cholesterol = 185 mg/dl • Average LDL = 99 mg/dl • We set a goal that 90% of patients would be screened annually and prescribed a statin 62
 Front Desk Process • List of patients with diabetes • Whether or not labs need to be drawn Plan/Do • We had patients that needed labs that were not getting triaged appropriately Study • Looked at front desk logs and process 63
Front Desk Process • List of patients with diabetes • Whether or not labs need to be drawn Plan/Do • We had patients that needed labs that were not getting triaged appropriately Study • Looked at front desk logs and process 63
 Front Desk Logs • About 60 patients with diabetes/week • 30 needed a lab drawn Study • Only 15 had it drawn (50%) 64
Front Desk Logs • About 60 patients with diabetes/week • 30 needed a lab drawn Study • Only 15 had it drawn (50%) 64
 Pizza for 90% Fidelity • 25/33 = 75% No pizza • 34/36 = 94% PIZZA Act-Plan Study 65
Pizza for 90% Fidelity • 25/33 = 75% No pizza • 34/36 = 94% PIZZA Act-Plan Study 65
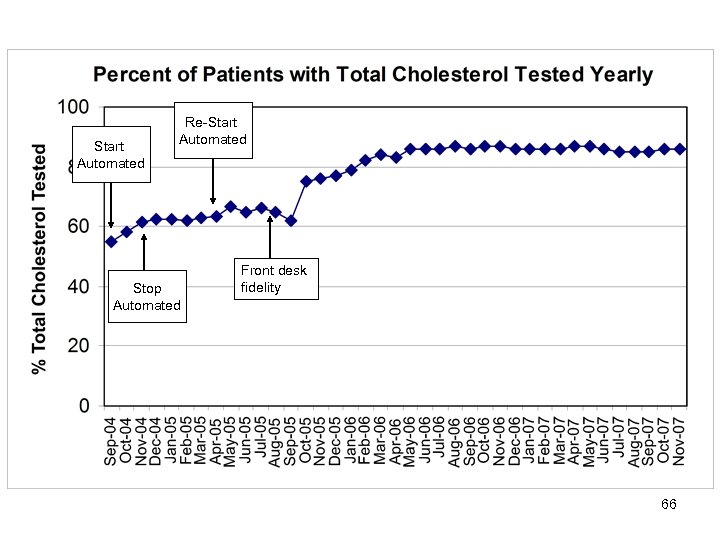 Start Automated Re-Start Automated Stop Automated Front desk fidelity 66
Start Automated Re-Start Automated Stop Automated Front desk fidelity 66
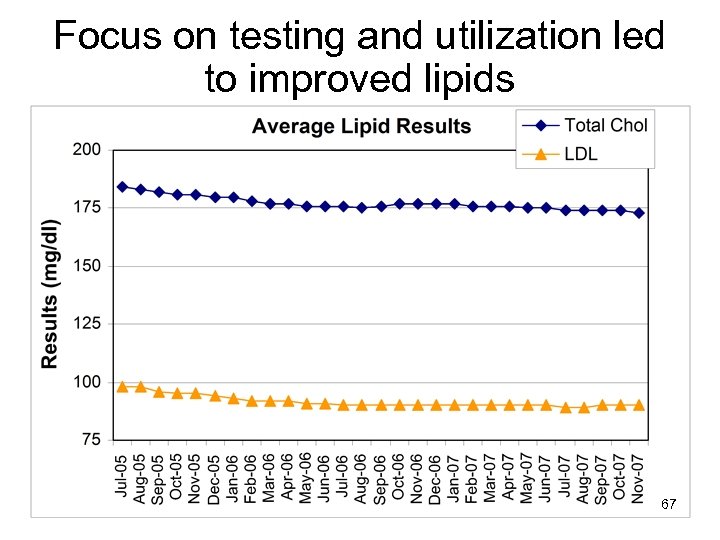 Focus on testing and utilization led to improved lipids 67
Focus on testing and utilization led to improved lipids 67
 Example 2 Process measure improvement: Nurse-directed interventions, improving the prompts 68
Example 2 Process measure improvement: Nurse-directed interventions, improving the prompts 68
 Process to engage nurses • Solidified divisional support for utilization of the intervention • Developed educational session with nurses – Meeting introduction by medical director – Revisited intent of the yellow sheets – Reiterated the role of the nurse as an integral member of our team – Reviewed evidence behind recommendations – Listened to nurses’ concerns • Developed rapid means of feedback 69
Process to engage nurses • Solidified divisional support for utilization of the intervention • Developed educational session with nurses – Meeting introduction by medical director – Revisited intent of the yellow sheets – Reiterated the role of the nurse as an integral member of our team – Reviewed evidence behind recommendations – Listened to nurses’ concerns • Developed rapid means of feedback 69
 Items to be included in nurse assessment • Assess as indicated on the prompt – Depression screening – Smoking assessment and intervention – Eye referrals – Monofilament testing – Pneumococcal vaccination 70
Items to be included in nurse assessment • Assess as indicated on the prompt – Depression screening – Smoking assessment and intervention – Eye referrals – Monofilament testing – Pneumococcal vaccination 70
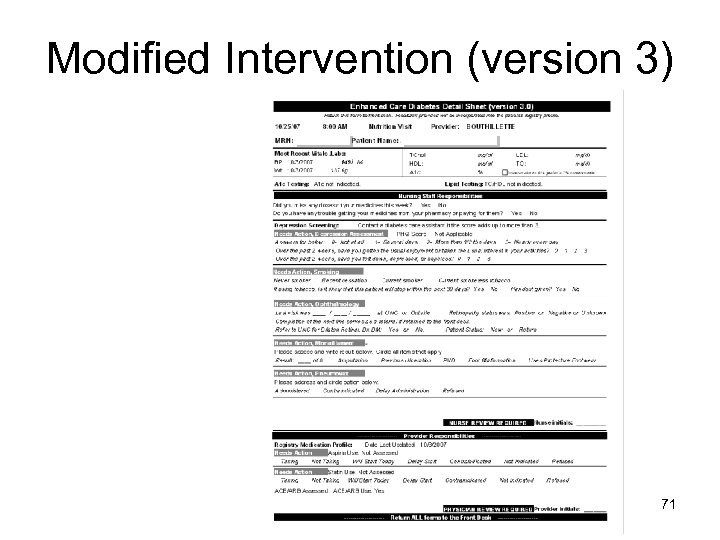 Modified Intervention (version 3) Feedback and change in clinical focus led to significant revision of the yellow sheets 71
Modified Intervention (version 3) Feedback and change in clinical focus led to significant revision of the yellow sheets 71
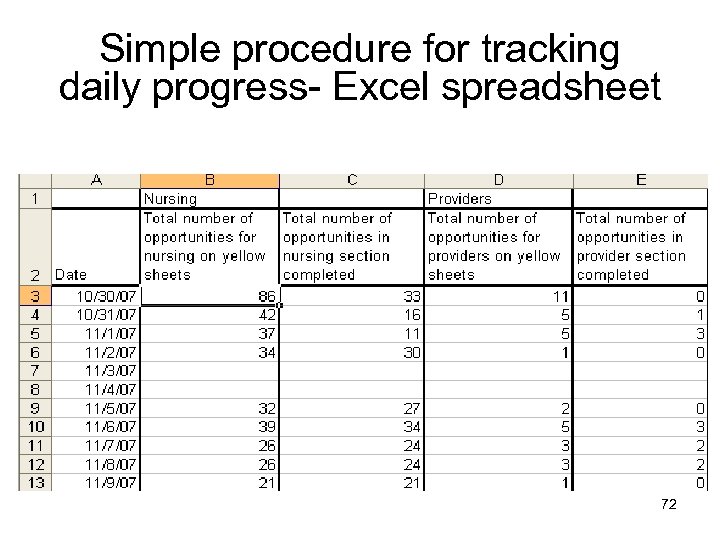 Simple procedure for tracking daily progress- Excel spreadsheet Completed by ancillary staff 72
Simple procedure for tracking daily progress- Excel spreadsheet Completed by ancillary staff 72
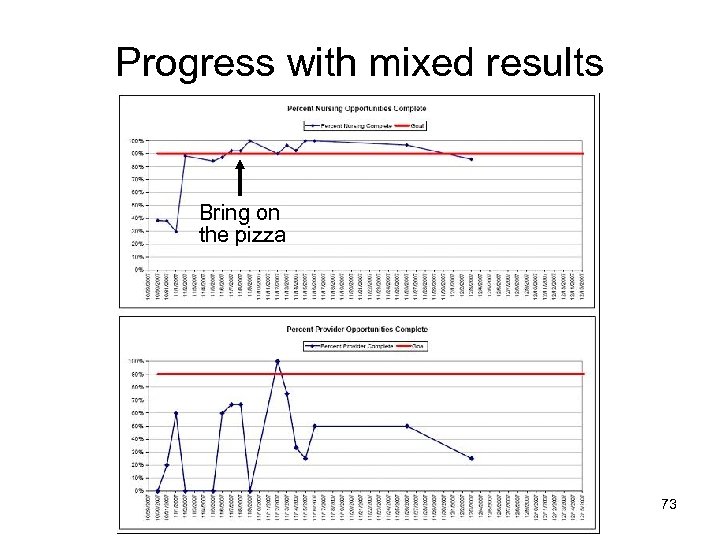 Progress with mixed results Bring on the pizza 73
Progress with mixed results Bring on the pizza 73
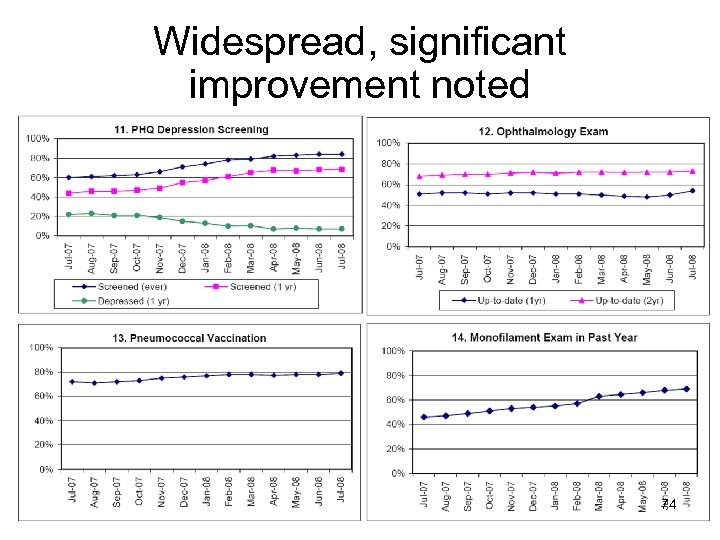 Widespread, significant improvement noted 74
Widespread, significant improvement noted 74
 Provider satisfaction has improved: How has this affected the life of a physician? • Delegating processes frees up time to focus on diagnostic and therapeutic issues • A weight has been lifted • Excellent to know how the practice performs • Data has changed our conversations • It is satisfying to show improved care 75
Provider satisfaction has improved: How has this affected the life of a physician? • Delegating processes frees up time to focus on diagnostic and therapeutic issues • A weight has been lifted • Excellent to know how the practice performs • Data has changed our conversations • It is satisfying to show improved care 75
 Diabetes Improvement Across the Practice--Lessons • Just working harder doesn’t lead to better outcomes • Just making a policy doesn’t mean the process gets done • Doctors in our system don’t follow algorithms or policies very well – Other members of the health care team are better…and that is OK • Each member must function at their highest level of skill • Distractions will arise, challenges will occur 76
Diabetes Improvement Across the Practice--Lessons • Just working harder doesn’t lead to better outcomes • Just making a policy doesn’t mean the process gets done • Doctors in our system don’t follow algorithms or policies very well – Other members of the health care team are better…and that is OK • Each member must function at their highest level of skill • Distractions will arise, challenges will occur 76
 In Summary: Change Package • Includes details about making changes, measures, assessment scales and tools • A resource for practices and QICs • Offers guidance and resources • Remember: Teams’ testing helps adapt and adopt strategies in their office 77
In Summary: Change Package • Includes details about making changes, measures, assessment scales and tools • A resource for practices and QICs • Offers guidance and resources • Remember: Teams’ testing helps adapt and adopt strategies in their office 77
 IPIP Expectations • Practices work on redesign of systems of care delivery • Target improvement in diabetes or asthma • This becomes how we practice healthcare — continuously tracking, sharing, and improving • Participation in IPIP meets one requirement for maintenance of certification and qualifies for Continuing Medical Education (CME) credit 78
IPIP Expectations • Practices work on redesign of systems of care delivery • Target improvement in diabetes or asthma • This becomes how we practice healthcare — continuously tracking, sharing, and improving • Participation in IPIP meets one requirement for maintenance of certification and qualifies for Continuing Medical Education (CME) credit 78
 Expectations re: Data • Collect data on performance measures (required) • Submit numerators and denominators to IPIP via QIC, state program or directly • Reliable, quality care is provided to the entire population by using registry (or EHR with population management functions) 79
Expectations re: Data • Collect data on performance measures (required) • Submit numerators and denominators to IPIP via QIC, state program or directly • Reliable, quality care is provided to the entire population by using registry (or EHR with population management functions) 79
 What do we mean by data? • Aggregate measures of quality – Based on national standards (NCQA, AQA, HEDIS) – Physician or practice-based – Additional details enhance understanding of context and meaning (levels of data quality) – Range of data sources (paper -> Electronic Health Record) 80
What do we mean by data? • Aggregate measures of quality – Based on national standards (NCQA, AQA, HEDIS) – Physician or practice-based – Additional details enhance understanding of context and meaning (levels of data quality) – Range of data sources (paper -> Electronic Health Record) 80
 Rely Upon Nationally Endorsed Measures • Early in IPIP development, it became clear that the scope of determining “ideal” measures was beyond IPIP • Other organizations exist to do this: NCQA, Physicians Consortium, National Quality Forum, Ambulatory Care Quality Alliance • IPIP decided to only require measures that had been endorsed by a one or more of the above organizations 81
Rely Upon Nationally Endorsed Measures • Early in IPIP development, it became clear that the scope of determining “ideal” measures was beyond IPIP • Other organizations exist to do this: NCQA, Physicians Consortium, National Quality Forum, Ambulatory Care Quality Alliance • IPIP decided to only require measures that had been endorsed by a one or more of the above organizations 81
 Benefits and Downsides • Mitigates the debate about individual opinions • Dramatically improves our ability to align • Reduces flexibility • Often leaves us with more “clunky” measures (less sensitive to changes) • Measures sometimes change slower than we would like (concerns about obsolete) 82
Benefits and Downsides • Mitigates the debate about individual opinions • Dramatically improves our ability to align • Reduces flexibility • Often leaves us with more “clunky” measures (less sensitive to changes) • Measures sometimes change slower than we would like (concerns about obsolete) 82
 Required IPIP measures are not the only measures practices should be using Use other measures to help ensure reliable processes and do small PDSAs 83
Required IPIP measures are not the only measures practices should be using Use other measures to help ensure reliable processes and do small PDSAs 83
 • The complete IPIP Change Package is in Word format on the Extranet. Look under Resources and then in the Change Package folder. 84
• The complete IPIP Change Package is in Word format on the Extranet. Look under Resources and then in the Change Package folder. 84
 85
85
 References • www. improvingchroniccare. org • http: //www. med. unc. edu/medicine/general m/documents/Diabetes. Research. pdf • www. ihi/org/extranet. 86
References • www. improvingchroniccare. org • http: //www. med. unc. edu/medicine/general m/documents/Diabetes. Research. pdf • www. ihi/org/extranet. 86
 • http: //www. med. unc. edu/medicine/general m/documents/Diabetes. Research. pdf 87
• http: //www. med. unc. edu/medicine/general m/documents/Diabetes. Research. pdf 87


