2a6e770b413912fa755f617ff3c6af3e.ppt
- Количество слайдов: 41
 Improving patient safety From analysis to action in practice Prof. Richard Grol
Improving patient safety From analysis to action in practice Prof. Richard Grol
 Major problem Heart Surgery Academic Medical Center Nijmegen Internal e-mail in Academical Medical Center Nijmegen by anaesthesiologist on 10 sept 2005, leaked to local newspaper “Yesterday we had a meeting on care pathway for cardio-thoracic surgery. Data were presented from the National Intensive Care Database. These showed that our heart center did not operate more serious patients , but had a mortality rate twice as high as the rest of the Netherlands. Also the reoperations because of bleedings were much higher. This is a very serious problem”
Major problem Heart Surgery Academic Medical Center Nijmegen Internal e-mail in Academical Medical Center Nijmegen by anaesthesiologist on 10 sept 2005, leaked to local newspaper “Yesterday we had a meeting on care pathway for cardio-thoracic surgery. Data were presented from the National Intensive Care Database. These showed that our heart center did not operate more serious patients , but had a mortality rate twice as high as the rest of the Netherlands. Also the reoperations because of bleedings were much higher. This is a very serious problem”
 Major problem Heart Surgery Academic Medical Center Nijmegen Mortality rate in 2004 almost 7% compared to 2, 7% nationally; publication in media leads to: • Patients skipping operations (one third of beds empty) • Internal and external investigations: very critical conclusions about performance, records, collaboration, teamwork, attitude of doctors, leadership, quality control, etc • Authorities close center for 6 months; Executive Board, director heart cente, other leaders (forced to) quit
Major problem Heart Surgery Academic Medical Center Nijmegen Mortality rate in 2004 almost 7% compared to 2, 7% nationally; publication in media leads to: • Patients skipping operations (one third of beds empty) • Internal and external investigations: very critical conclusions about performance, records, collaboration, teamwork, attitude of doctors, leadership, quality control, etc • Authorities close center for 6 months; Executive Board, director heart cente, other leaders (forced to) quit
 Next: • New Executive Board of Academic Medical Center, new director of heart center, new clinical leaders • Complete redesign of surgery processes, improved team work and collaboration, new surgeons, etc • New quality and safety policies for Academic Center with rigorous clinical audits of all departments and centers Mortality rates around 1% in 2010; similar reduction in complications, readmissions, etc
Next: • New Executive Board of Academic Medical Center, new director of heart center, new clinical leaders • Complete redesign of surgery processes, improved team work and collaboration, new surgeons, etc • New quality and safety policies for Academic Center with rigorous clinical audits of all departments and centers Mortality rates around 1% in 2010; similar reduction in complications, readmissions, etc
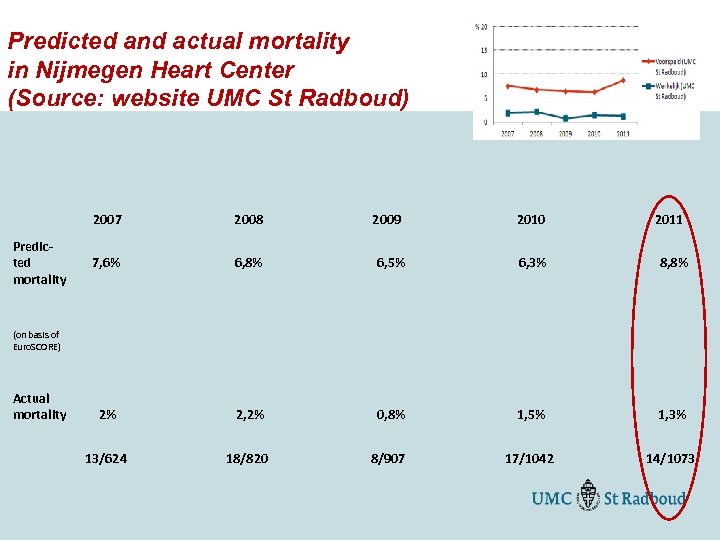 Predicted and actual mortality in Nijmegen Heart Center (Source: website UMC St Radboud) 2007 2008 2009 2010 2011 Predicted mortality 7, 6% 6, 8% 6, 5% 6, 3% 8, 8% (on basis of Euro. SCORE) Actual mortality 2% 2, 2% 0, 8% 1, 5% 1, 3% 13/624 18/820 8/907 17/1042 14/1073
Predicted and actual mortality in Nijmegen Heart Center (Source: website UMC St Radboud) 2007 2008 2009 2010 2011 Predicted mortality 7, 6% 6, 8% 6, 5% 6, 3% 8, 8% (on basis of Euro. SCORE) Actual mortality 2% 2, 2% 0, 8% 1, 5% 1, 3% 13/624 18/820 8/907 17/1042 14/1073
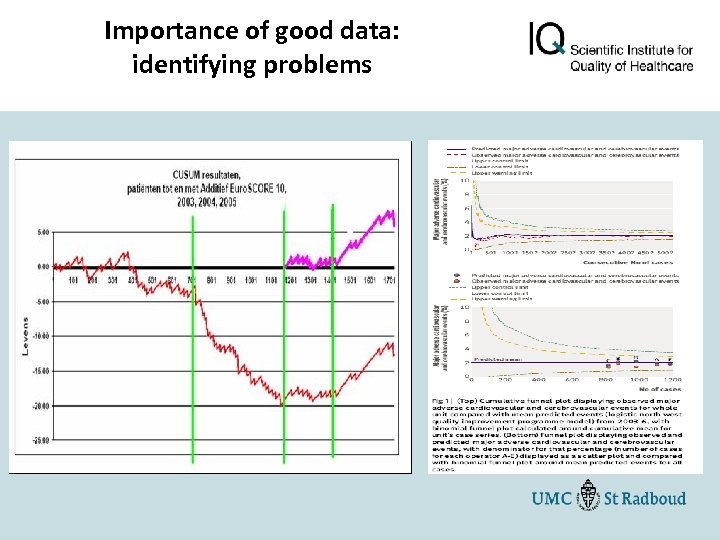 Importance of good data: identifying problems
Importance of good data: identifying problems
 Why this major improvement in heart surgery safety? • What external factors have contributed to this major improvement in quality and safety • What internal (hospital and ward related) factors have contributed to this major improvement in quality and safety? Please formulate hypotheses
Why this major improvement in heart surgery safety? • What external factors have contributed to this major improvement in quality and safety • What internal (hospital and ward related) factors have contributed to this major improvement in quality and safety? Please formulate hypotheses
 External factors • Closing of the center by the Inspectorate for 6 months • Public reporting about the problem in the media: “public shaming”, damage to reputation of the whole Academic Medical Center • Influence patients and referrers: patients skipped operations, less referrals for operations • Reliable data on performance: sense of urgency among leaders, physicians and board of trustees
External factors • Closing of the center by the Inspectorate for 6 months • Public reporting about the problem in the media: “public shaming”, damage to reputation of the whole Academic Medical Center • Influence patients and referrers: patients skipped operations, less referrals for operations • Reliable data on performance: sense of urgency among leaders, physicians and board of trustees
 Internal factors • Reliable data for continuous reflection, one physician responsible for data, datamanager • Care pathways, care processes completely standardized and controlled • Leader committed to quality and safety, role model • Committed professionals, involved in quality improvement • Intensive collaboration between disciplines and wards • Teams with skilled nurses • Culture of mutual trust, respect and openess • Hospital wide quality policies supporting continuous improvement at level of heart center •
Internal factors • Reliable data for continuous reflection, one physician responsible for data, datamanager • Care pathways, care processes completely standardized and controlled • Leader committed to quality and safety, role model • Committed professionals, involved in quality improvement • Intensive collaboration between disciplines and wards • Teams with skilled nurses • Culture of mutual trust, respect and openess • Hospital wide quality policies supporting continuous improvement at level of heart center •
 The facts Data on safety problems in hospitals in Netherlands • 6% of hospital patients “adverse event”, 40% avoidable • around 1950 avoidable deaths per year in 2010 • 40. 000 people admitted to hospital per year because of medication erros (HARM-study) • almost 7% of Dutch patiënts in hospital get infection; extra costs 200 -300 million euro (van Benthem 2010) • Unsafe care: 2 billion euro extra costs p/year for hospitals National Safety Plan: focus on reporting and analyzing incidents, aimed at 50% reduction in AE; not achieved so far
The facts Data on safety problems in hospitals in Netherlands • 6% of hospital patients “adverse event”, 40% avoidable • around 1950 avoidable deaths per year in 2010 • 40. 000 people admitted to hospital per year because of medication erros (HARM-study) • almost 7% of Dutch patiënts in hospital get infection; extra costs 200 -300 million euro (van Benthem 2010) • Unsafe care: 2 billion euro extra costs p/year for hospitals National Safety Plan: focus on reporting and analyzing incidents, aimed at 50% reduction in AE; not achieved so far
 How to improve safety: systematic review (Duckers et al, Med Care Res Rev 2009) • Reporting and follow-up of adverse events (9 studies): positive effects on quality of reporting and number of incidents reported, no effect on safety of care • Analysis of adverse events (2 studies): effect unclear • Improving safety or reducing risk (31 studies on medication safety, falls, diagnostic failures, etc) : -evidence for effect specific strategies limited -quality of studies moderate, few studies in primary care World Alliance for Patient Safety 2008: most investments in measuring, analyzing and reporting AE, little in improving safety
How to improve safety: systematic review (Duckers et al, Med Care Res Rev 2009) • Reporting and follow-up of adverse events (9 studies): positive effects on quality of reporting and number of incidents reported, no effect on safety of care • Analysis of adverse events (2 studies): effect unclear • Improving safety or reducing risk (31 studies on medication safety, falls, diagnostic failures, etc) : -evidence for effect specific strategies limited -quality of studies moderate, few studies in primary care World Alliance for Patient Safety 2008: most investments in measuring, analyzing and reporting AE, little in improving safety
 Causes of unsafe care divers, improvement difficult • Patient: knowledge, wishes, experiences, severity of disease, multi-morbidity, language problems, etc • Professional: knowledge, skills, experience, attitudes, stress, addiction, burn-out, etc • Team: collaboration, information, hand-over routines, mutual control, leadership, culture at ward or practice • Organisaton: leadership, governance, budget, logistics, processes, workload, staff, equipment, etc • Economic, legal and cultural context
Causes of unsafe care divers, improvement difficult • Patient: knowledge, wishes, experiences, severity of disease, multi-morbidity, language problems, etc • Professional: knowledge, skills, experience, attitudes, stress, addiction, burn-out, etc • Team: collaboration, information, hand-over routines, mutual control, leadership, culture at ward or practice • Organisaton: leadership, governance, budget, logistics, processes, workload, staff, equipment, etc • Economic, legal and cultural context
 Patient safety improvement: a 6 -point plan • Beyond measuring and analyzing adverse events, eg: - continuous monitoring, real time data and feedback - standardization, checklists and control - improved coordination and teamwork - involving patient in safety improvement - changing professional attitude - better leadership for safety • Integrate safety actions at different levels: patient, professional, teams, organizations, boards, payers, policy
Patient safety improvement: a 6 -point plan • Beyond measuring and analyzing adverse events, eg: - continuous monitoring, real time data and feedback - standardization, checklists and control - improved coordination and teamwork - involving patient in safety improvement - changing professional attitude - better leadership for safety • Integrate safety actions at different levels: patient, professional, teams, organizations, boards, payers, policy
 Invest in data- and feedbacksystems • Professionals over-estimate own performance (Davis, JAMA 2006); good data needed to convince and motivate • Feedback effective if (van der Weijden 2011): -real-time monitoring and feedback, -advice on how to improve care -regular feedback -data are trusted and seen as relevant by professionals -feedback embedded in peer review or clinical audit in teams • Support by experts needed
Invest in data- and feedbacksystems • Professionals over-estimate own performance (Davis, JAMA 2006); good data needed to convince and motivate • Feedback effective if (van der Weijden 2011): -real-time monitoring and feedback, -advice on how to improve care -regular feedback -data are trusted and seen as relevant by professionals -feedback embedded in peer review or clinical audit in teams • Support by experts needed
 Impact of Clinical Registries Rapport Society for Cardiothoracic Surgery in UK (2011): Monitoring and public reporting of mortality rates: 50% reduction in risk-adjusted mortality rates for cardio-thoracic surgery; substantial cost-reduction
Impact of Clinical Registries Rapport Society for Cardiothoracic Surgery in UK (2011): Monitoring and public reporting of mortality rates: 50% reduction in risk-adjusted mortality rates for cardio-thoracic surgery; substantial cost-reduction
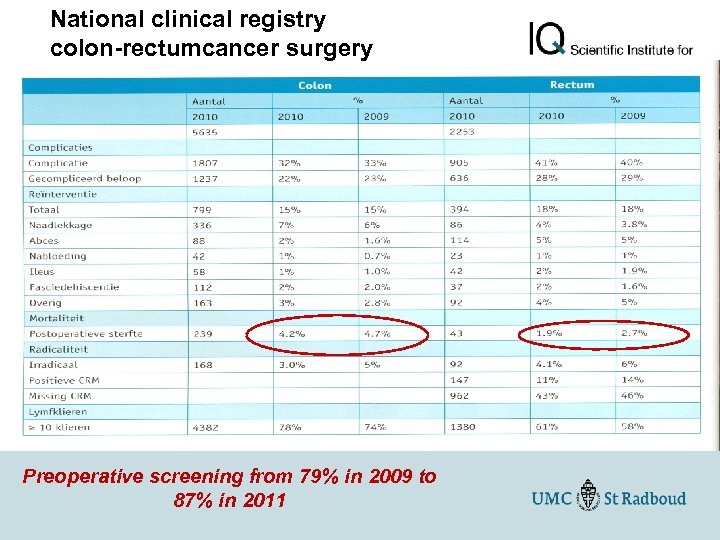 National clinical registry colon-rectumcancer surgery DSCA-cijfers 2009 -2010 Preoperative screening from 79% in 2009 to 87% in 2011
National clinical registry colon-rectumcancer surgery DSCA-cijfers 2009 -2010 Preoperative screening from 79% in 2009 to 87% in 2011
 How to involve patients in improving safety in healthcare • Enhance knowledge about condition and optimal treatment (guidelines) • Observation what happens and asking why it happens or not happens • Involvement in decisions about management of problem, use decision aids • Give feedback to care providers: positive and critical • Involve family or buddies to ask for information and be your guard
How to involve patients in improving safety in healthcare • Enhance knowledge about condition and optimal treatment (guidelines) • Observation what happens and asking why it happens or not happens • Involvement in decisions about management of problem, use decision aids • Give feedback to care providers: positive and critical • Involve family or buddies to ask for information and be your guard
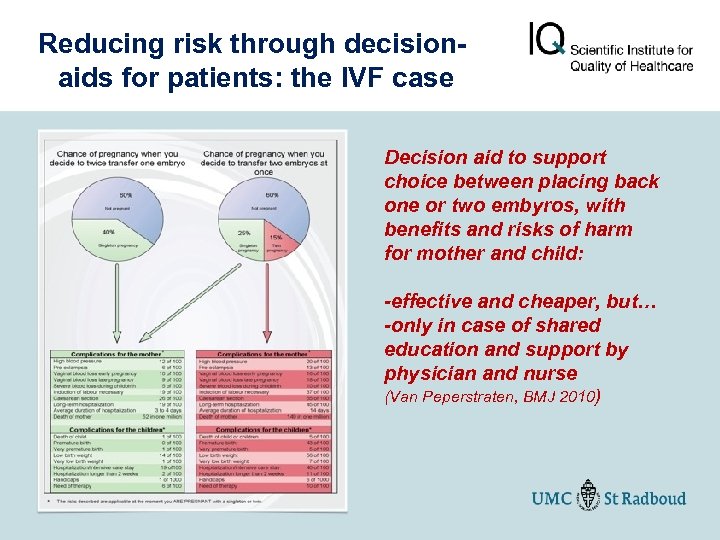 Reducing risk through decisionaids for patients: the IVF case Decision aid to support choice between placing back one or two embyros, with benefits and risks of harm for mother and child: -effective and cheaper, but… -only in case of shared education and support by physician and nurse (Van Peperstraten, BMJ 2010)
Reducing risk through decisionaids for patients: the IVF case Decision aid to support choice between placing back one or two embyros, with benefits and risks of harm for mother and child: -effective and cheaper, but… -only in case of shared education and support by physician and nurse (Van Peperstraten, BMJ 2010)
 Invest in coordination for better and safer care • Review of 22 systematic reviews (Wensing et al 2010): integrated and coordinated care for patients with heart failure, diabetes, depression etc is related to better quality of care, better patiënt outcomes and lower costs • John Ovretveit, report for Health Foundation 2011: -many adverse events caused by incomplete coordination; -strong evidence for effect of: disease management, multidisciplinary teams, coordinated discharge planning, postcharge care for chronic patients • Cochrane review of effect of integrated care pathways (Rotter et al 2009, 20 studies): impact on complication, LOS and costs in hospitals
Invest in coordination for better and safer care • Review of 22 systematic reviews (Wensing et al 2010): integrated and coordinated care for patients with heart failure, diabetes, depression etc is related to better quality of care, better patiënt outcomes and lower costs • John Ovretveit, report for Health Foundation 2011: -many adverse events caused by incomplete coordination; -strong evidence for effect of: disease management, multidisciplinary teams, coordinated discharge planning, postcharge care for chronic patients • Cochrane review of effect of integrated care pathways (Rotter et al 2009, 20 studies): impact on complication, LOS and costs in hospitals
 Invest in standardization and control Odysseus and the Sirens. . or tying yourself to the mast
Invest in standardization and control Odysseus and the Sirens. . or tying yourself to the mast
 Health care is managing of extreme complexity “Healthcare too complex to leave to control and decisions of individual clinicians; human memory and attention needed is fallible in complex care; therefore we should use teamwork, control and checklists” Example: average patient on IC needs 178 actions per day; errors in 1 -2%
Health care is managing of extreme complexity “Healthcare too complex to leave to control and decisions of individual clinicians; human memory and attention needed is fallible in complex care; therefore we should use teamwork, control and checklists” Example: average patient on IC needs 178 actions per day; errors in 1 -2%
 Effects of control measures to reduce antibiotic use (Davey et al, Cochrane review 2006) 66 studies with 60 interventions to reduce antibiotic use in hospitals: • In most studies (70 -80%) a significant effect was found on AB use, infections and clinical outcomes • Restrictive methods (autorisation by colleague, use of strict indications, automatic stop orders, electronic decision support, etc) more effective …. • …than educational methods (CME, information, feedback, reminders, outreach expert visitors, etc)
Effects of control measures to reduce antibiotic use (Davey et al, Cochrane review 2006) 66 studies with 60 interventions to reduce antibiotic use in hospitals: • In most studies (70 -80%) a significant effect was found on AB use, infections and clinical outcomes • Restrictive methods (autorisation by colleague, use of strict indications, automatic stop orders, electronic decision support, etc) more effective …. • …than educational methods (CME, information, feedback, reminders, outreach expert visitors, etc)
 Most adverse events in surgery (>50%), mostly infections and bleedings Sculpture: by Joep van Lieshout
Most adverse events in surgery (>50%), mostly infections and bleedings Sculpture: by Joep van Lieshout
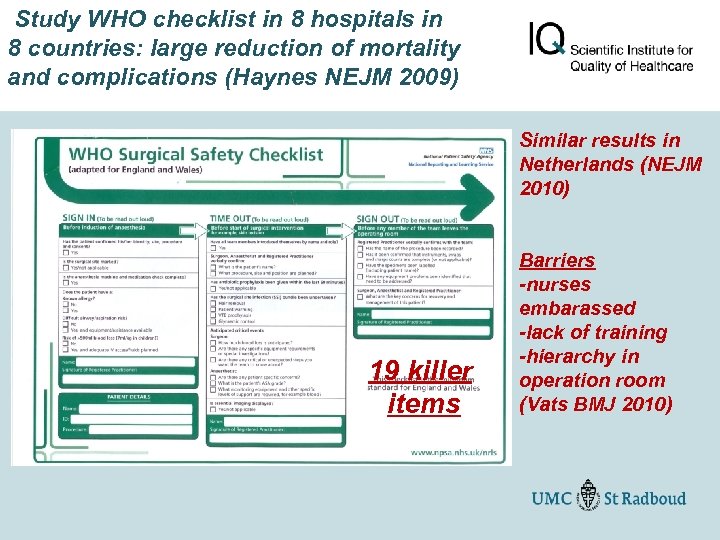 Study WHO checklist in 8 hospitals in 8 countries: large reduction of mortality and complications (Haynes NEJM 2009) Similar results in Netherlands (NEJM 2010) 19 killer items Barriers -nurses embarassed -lack of training -hierarchy in operation room (Vats BMJ 2010)
Study WHO checklist in 8 hospitals in 8 countries: large reduction of mortality and complications (Haynes NEJM 2009) Similar results in Netherlands (NEJM 2010) 19 killer items Barriers -nurses embarassed -lack of training -hierarchy in operation room (Vats BMJ 2010)
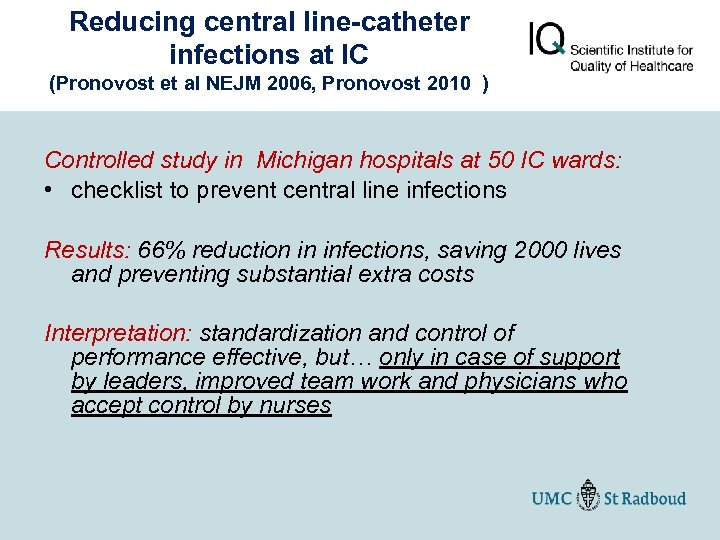 Reducing central line-catheter infections at IC (Pronovost et al NEJM 2006, Pronovost 2010 ) Controlled study in Michigan hospitals at 50 IC wards: • checklist to prevent central line infections Results: 66% reduction in infections, saving 2000 lives and preventing substantial extra costs Interpretation: standardization and control of performance effective, but… only in case of support by leaders, improved team work and physicians who accept control by nurses
Reducing central line-catheter infections at IC (Pronovost et al NEJM 2006, Pronovost 2010 ) Controlled study in Michigan hospitals at 50 IC wards: • checklist to prevent central line infections Results: 66% reduction in infections, saving 2000 lives and preventing substantial extra costs Interpretation: standardization and control of performance effective, but… only in case of support by leaders, improved team work and physicians who accept control by nurses
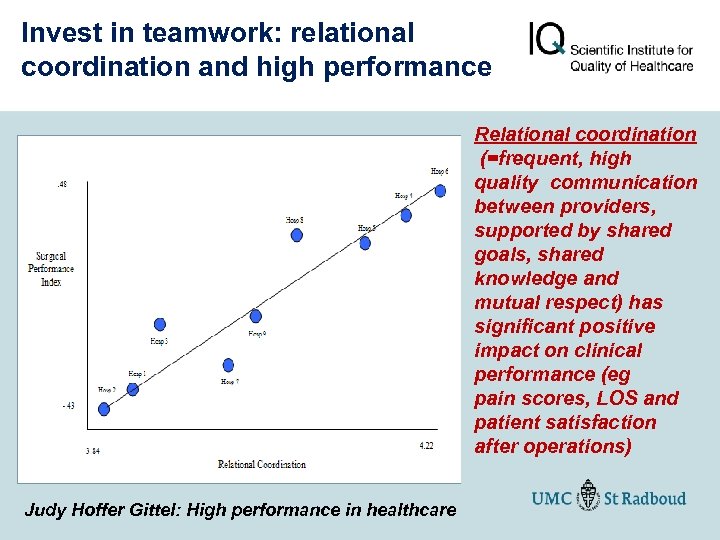 Invest in teamwork: relational coordination and high performance Relational coordination (=frequent, high quality communication between providers, supported by shared goals, shared knowledge and mutual respect) has significant positive impact on clinical performance (eg pain scores, LOS and patient satisfaction after operations) Judy Hoffer Gittel: High performance in healthcare
Invest in teamwork: relational coordination and high performance Relational coordination (=frequent, high quality communication between providers, supported by shared goals, shared knowledge and mutual respect) has significant positive impact on clinical performance (eg pain scores, LOS and patient satisfaction after operations) Judy Hoffer Gittel: High performance in healthcare
 Crucial role of nurse in improving quality and safety 18 reviews (Laurant 2009): nurse same quality of care, more satisfaction
Crucial role of nurse in improving quality and safety 18 reviews (Laurant 2009): nurse same quality of care, more satisfaction
 “Hudson River Hero” (or “Hudson River Teamwork”) Analysis of successful landing of plane in Hudson River and saving all passenger showed: • experienced pilot, leadership • strict use of checklists and procedures • optimal teamwork of crew
“Hudson River Hero” (or “Hudson River Teamwork”) Analysis of successful landing of plane in Hudson River and saving all passenger showed: • experienced pilot, leadership • strict use of checklists and procedures • optimal teamwork of crew
 Invest in new professional “We need physicians who are smart, well - trained, innovative, intensely focused on delivering the best care to patients and who can play well with others. While House had many of these skills, the teamwork part was his fatal flaw. If he worked for me, I would have fired him. So, rest in peace dr. House” (Robert Wachtman, chair ABIM, USA Today)
Invest in new professional “We need physicians who are smart, well - trained, innovative, intensely focused on delivering the best care to patients and who can play well with others. While House had many of these skills, the teamwork part was his fatal flaw. If he worked for me, I would have fired him. So, rest in peace dr. House” (Robert Wachtman, chair ABIM, USA Today)
 A new type of professional Improving quality and safety in healthcare demands a new type of professional attitude: • • Using data for critical reflection on own performance Being accountable to others (colleagues, society) Accepting control by others Becoming a team worker and collaborator Involving patients in decisions Admitting and communicating mistakes and incidents Being skilled in systematically improving care Long way to go for many professionals in many countries
A new type of professional Improving quality and safety in healthcare demands a new type of professional attitude: • • Using data for critical reflection on own performance Being accountable to others (colleagues, society) Accepting control by others Becoming a team worker and collaborator Involving patients in decisions Admitting and communicating mistakes and incidents Being skilled in systematically improving care Long way to go for many professionals in many countries
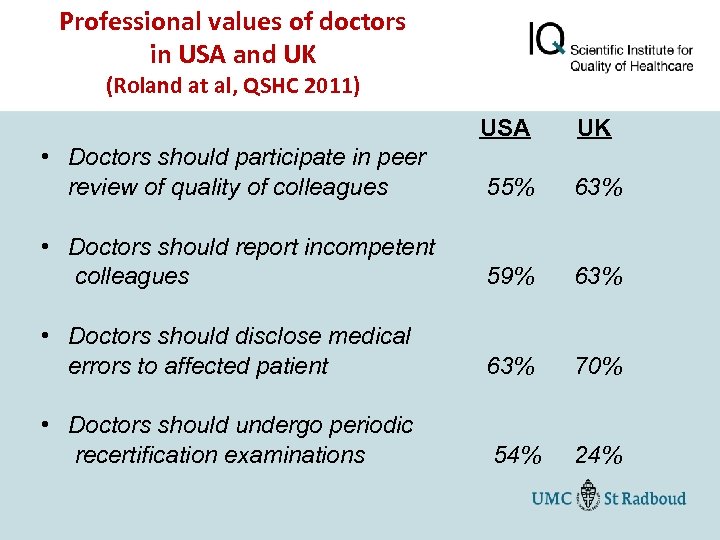 Professional values of doctors in USA and UK (Roland at al, QSHC 2011) USA UK • Doctors should participate in peer review of quality of colleagues 55% 63% • Doctors should report incompetent colleagues 59% 63% • Doctors should disclose medical errors to affected patient 63% 70% • Doctors should undergo periodic recertification examinations 54% 24%
Professional values of doctors in USA and UK (Roland at al, QSHC 2011) USA UK • Doctors should participate in peer review of quality of colleagues 55% 63% • Doctors should report incompetent colleagues 59% 63% • Doctors should disclose medical errors to affected patient 63% 70% • Doctors should undergo periodic recertification examinations 54% 24%
 Include topic of quality and safety improvement in (under)graduate curriculum of clinicians Concerned with new knowledge, skills, attitudes and routines in practice (“Improvement knowledge”); naive to expect that clinicians master these competencies without appropriate education Training and role models in teaching practices important
Include topic of quality and safety improvement in (under)graduate curriculum of clinicians Concerned with new knowledge, skills, attitudes and routines in practice (“Improvement knowledge”); naive to expect that clinicians master these competencies without appropriate education Training and role models in teaching practices important
 New doctors: test of social skills Medical schools in USA and Canada: Multiple-Mini. Interviews to test skills to communicate with patients and collaborate in teams
New doctors: test of social skills Medical schools in USA and Canada: Multiple-Mini. Interviews to test skills to communicate with patients and collaborate in teams
 “Current healthcare is fragmented and chaotic”
“Current healthcare is fragmented and chaotic”
 “Healthcare today needs a fundamentally different approach and a new breed of leaders”(Lee HBR 2010) • Leaders who create context for transparancy, organize team work, stimulate professional development, use of checklists and protocols and patiënt centeredness, etc • “Boards on Board”: leaders make quality and safety to top priority, are a role model, are competent in field of quality improvement, introduce long-term policies and methods, etc • Duckers 2010: when Executive Board stimulated quality improvement and medical specialists perceived an active role by Board, specialists more actively involved in quality and safety improvement activities
“Healthcare today needs a fundamentally different approach and a new breed of leaders”(Lee HBR 2010) • Leaders who create context for transparancy, organize team work, stimulate professional development, use of checklists and protocols and patiënt centeredness, etc • “Boards on Board”: leaders make quality and safety to top priority, are a role model, are competent in field of quality improvement, introduce long-term policies and methods, etc • Duckers 2010: when Executive Board stimulated quality improvement and medical specialists perceived an active role by Board, specialists more actively involved in quality and safety improvement activities
 Most effective measure to reduce hospital infections: hand hygiene! <50% adherence to guidelines on hand hygiene (physician performance poor)
Most effective measure to reduce hospital infections: hand hygiene! <50% adherence to guidelines on hand hygiene (physician performance poor)
 RCT on improving hand hygiene nurses in three hospitals (Brink et al, IQ 2009) Impact of two approaches on adherence to HH guidelines: state of art (feedback, posters, education, alcohol rub, etc) versus extended approach (team and leadership training) • State of art approach +23% • State of art approach + team and leadership training +38% -Impact on infections: 1, 35% less in extended approach -Impact on costs: 7000 euro less costs per ward in extended approach
RCT on improving hand hygiene nurses in three hospitals (Brink et al, IQ 2009) Impact of two approaches on adherence to HH guidelines: state of art (feedback, posters, education, alcohol rub, etc) versus extended approach (team and leadership training) • State of art approach +23% • State of art approach + team and leadership training +38% -Impact on infections: 1, 35% less in extended approach -Impact on costs: 7000 euro less costs per ward in extended approach
 Improving hand hygiene: impact leadership and team (Huis et al, thesis 2012) Major variation in change between 67 wards (-2% to +70%), by Team factors -data and feedback to wards about HH performance -mutual control on not following guidelines on HH in team -mutual support to improve routines Leadership factors -better HH as priority for ward and team -accounting about HH performance to hospital leaders -leaders motivae team to perform better on HH
Improving hand hygiene: impact leadership and team (Huis et al, thesis 2012) Major variation in change between 67 wards (-2% to +70%), by Team factors -data and feedback to wards about HH performance -mutual control on not following guidelines on HH in team -mutual support to improve routines Leadership factors -better HH as priority for ward and team -accounting about HH performance to hospital leaders -leaders motivae team to perform better on HH
 Patient safety improvement: a 6 -point plan • Beyond measuring and analyzing adverse events, eg: - continuous monitoring, real time data and feedback - standardization, checklists and control - improved coordination and teamwork - involving patient in safety improvement - changing professional attitude - better leadership for safety • Integrate safety actions at different levels: patient, professional, teams, organizations, boards, payers, policy
Patient safety improvement: a 6 -point plan • Beyond measuring and analyzing adverse events, eg: - continuous monitoring, real time data and feedback - standardization, checklists and control - improved coordination and teamwork - involving patient in safety improvement - changing professional attitude - better leadership for safety • Integrate safety actions at different levels: patient, professional, teams, organizations, boards, payers, policy
 Fragmentation in safety improvement Integration of safety improvement initiatives to be more effective
Fragmentation in safety improvement Integration of safety improvement initiatives to be more effective
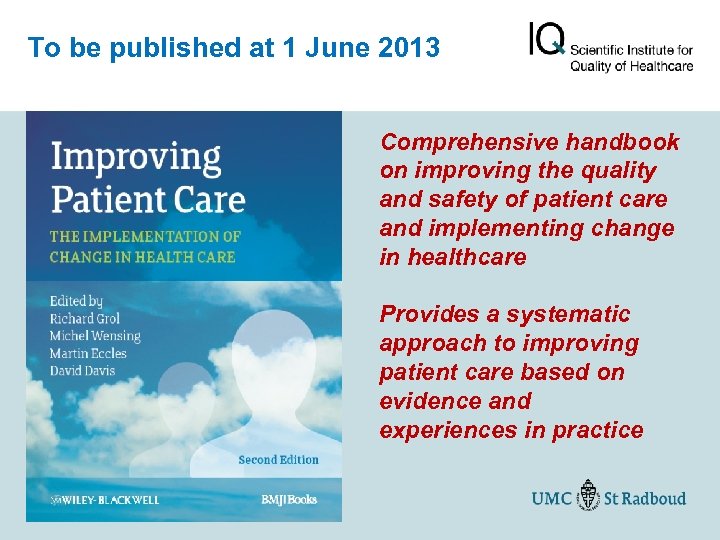 To be published at 1 June 2013 Comprehensive handbook on improving the quality and safety of patient care and implementing change in healthcare Provides a systematic approach to improving patient care based on evidence and experiences in practice
To be published at 1 June 2013 Comprehensive handbook on improving the quality and safety of patient care and implementing change in healthcare Provides a systematic approach to improving patient care based on evidence and experiences in practice


