6915ecdc2adea5bf81dc7eac9bdca6a5.ppt
- Количество слайдов: 34
IMPROVING DIABETES CARE FOR ADULTS: A Population-Based Approach Patrick J. O’Connor, MD, MPH Senior Clinical Investigator Health. Partners Research Foundation
Today’s Objectives – Leadership and Resources: The Burden of Diabetes and the Cost of Doing Nothing – Population Health Impact and Cost of Competing Diabetes Improvement Priorities – The “Enhanced Primary Care Model” – Results and Future Challenges
Burden of Diabetes in the US Morbidity and Mortality – Mortality: #3 cause, with 182, 000 deaths each year – Prevalence doubling every 10 -15 years – The death rate in the diabetic population is slowly decreasing for men but increasing for women – 70% of deaths in adults with DM are related to MI or CVA – Clinical trials provide evidence that control of hyperglycemia, dyslipidemia, and hypertension and use of ASA lower the risk of macro and micro complications. CDC, 1998.
Primary Prevention of Type 2 Diabetes – Physical Activity – Weight Management – Finnish Study 57% Reduction in Incidence - mean age around 60 years with IGT - dietary instruction 8 weekly sessions, then q 3 mo - structured physical activity 3 x a week - lost about 5 Kg.
Economic Burden of Diabetes in Adults The Cost of Doing Nothing
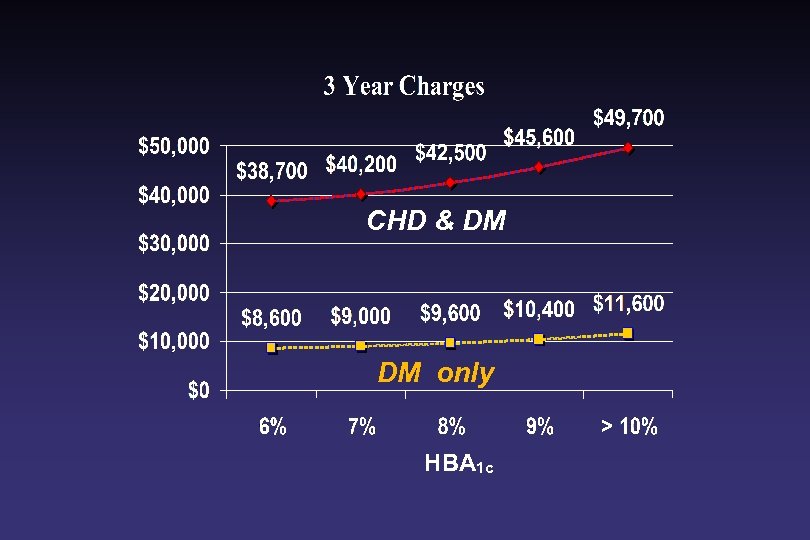
CHD & DM DM only HBA 1 c

Selecting Improvement Goals All Goals Are Not Equal
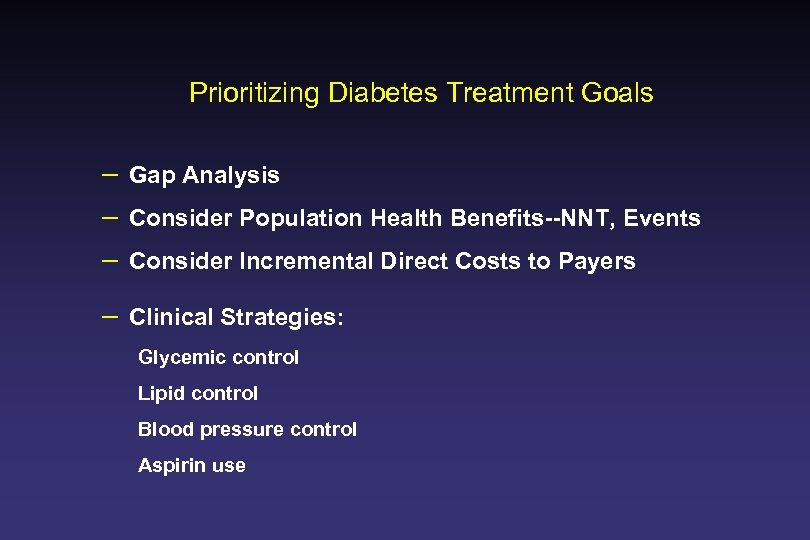
Prioritizing Diabetes Treatment Goals – Gap Analysis – Consider Population Health Benefits--NNT, Events – Consider Incremental Direct Costs to Payers – Clinical Strategies: Glycemic control Lipid control Blood pressure control Aspirin use
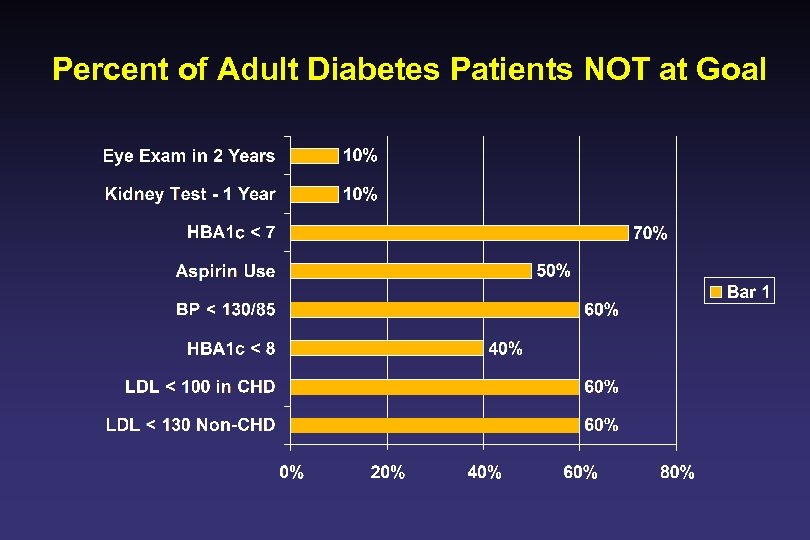
Percent of Adult Diabetes Patients NOT at Goal
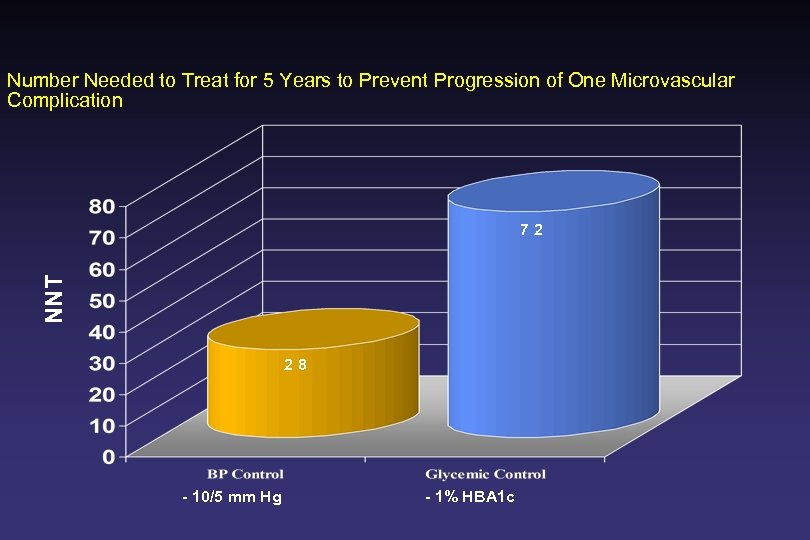
Number Needed to Treat for 5 Years to Prevent Progression of One Microvascular Complication NNT 72 28 - 10/5 mm Hg - 1% HBA 1 c
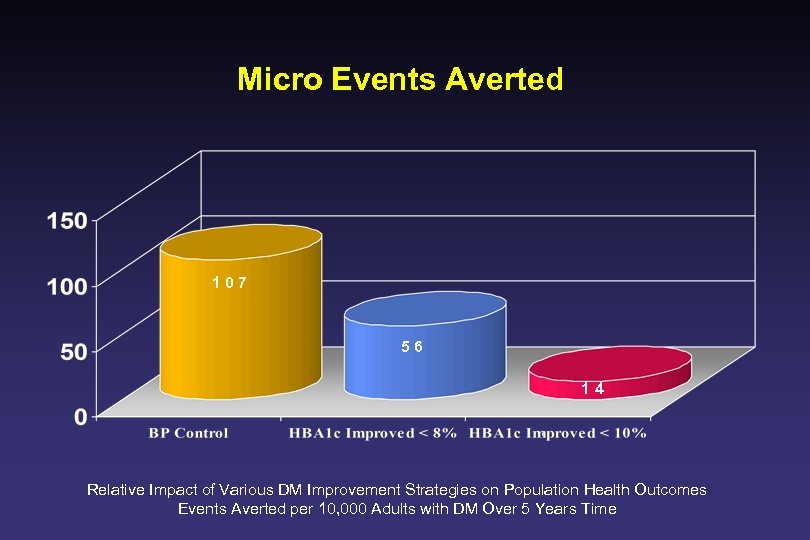
Micro Events Averted 107 56 14 Relative Impact of Various DM Improvement Strategies on Population Health Outcomes Events Averted per 10, 000 Adults with DM Over 5 Years Time
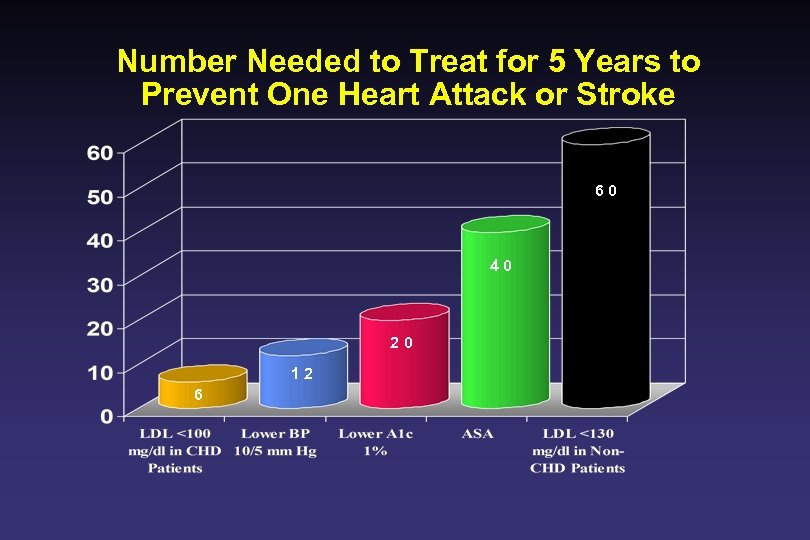
Number Needed to Treat for 5 Years to Prevent One Heart Attack or Stroke 60 40 20 12 6
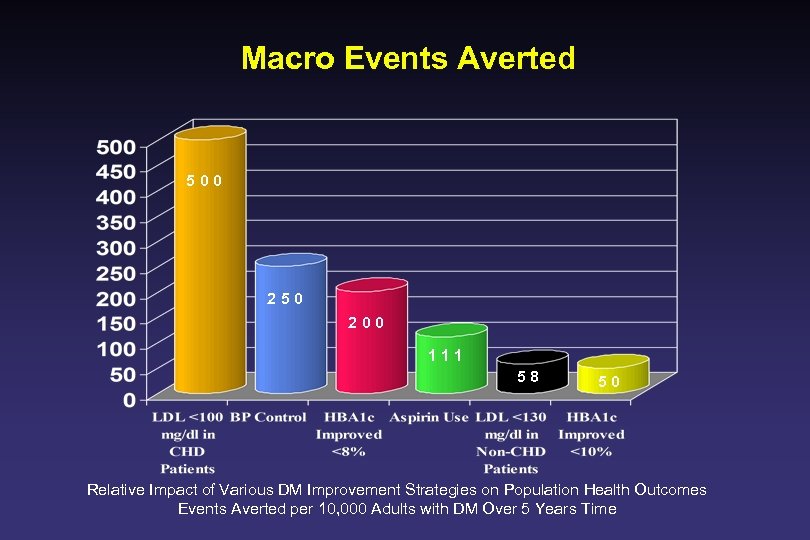
Macro Events Averted 500 250 200 111 58 50 Relative Impact of Various DM Improvement Strategies on Population Health Outcomes Events Averted per 10, 000 Adults with DM Over 5 Years Time
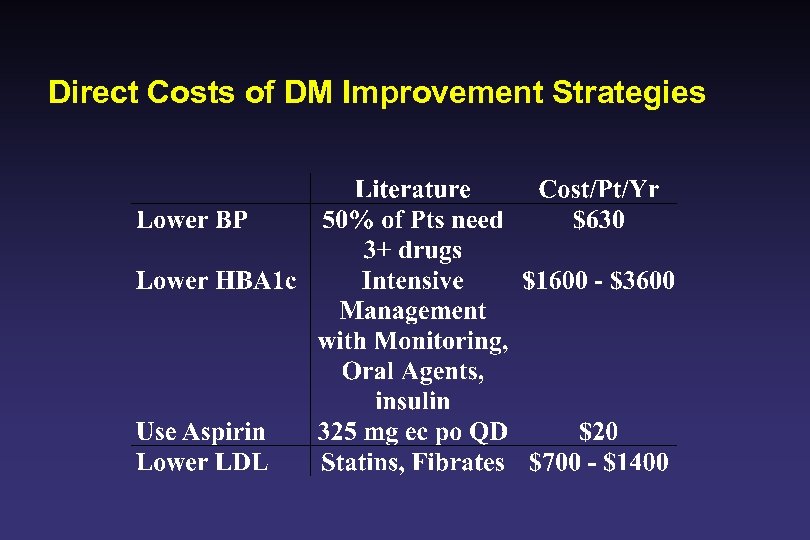
Direct Costs of DM Improvement Strategies
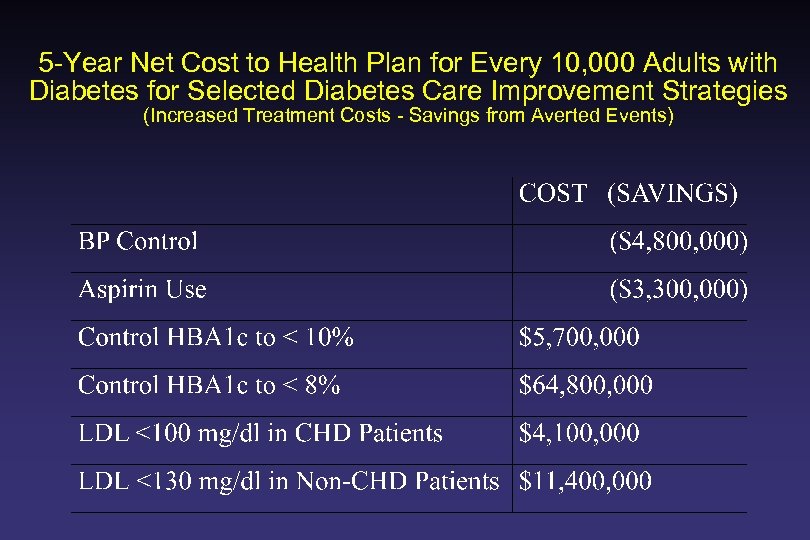
5 -Year Net Cost to Health Plan for Every 10, 000 Adults with Diabetes for Selected Diabetes Care Improvement Strategies (Increased Treatment Costs - Savings from Averted Events)
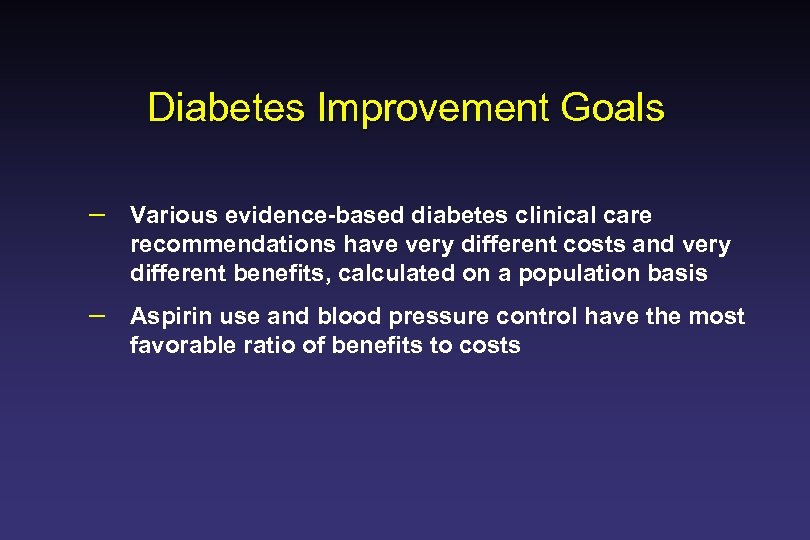
Diabetes Improvement Goals – Various evidence-based diabetes clinical care recommendations have very different costs and very different benefits, calculated on a population basis – Aspirin use and blood pressure control have the most favorable ratio of benefits to costs
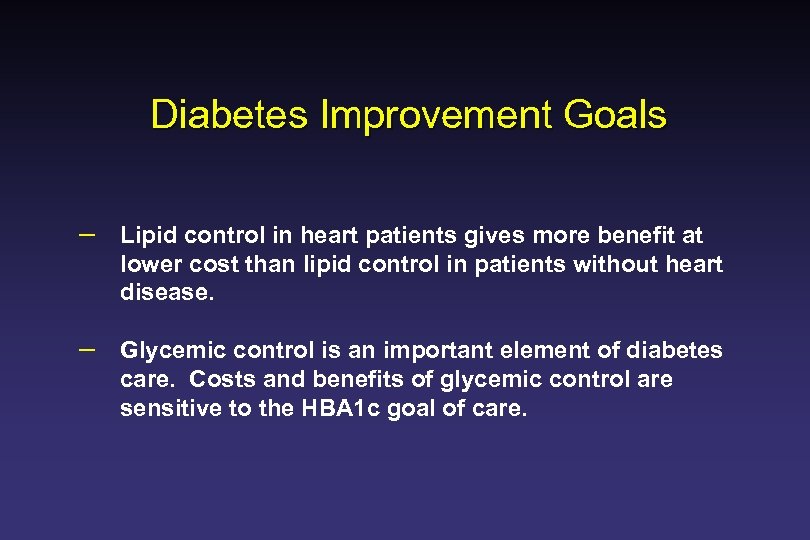
Diabetes Improvement Goals – Lipid control in heart patients gives more benefit at lower cost than lipid control in patients without heart disease. – Glycemic control is an important element of diabetes care. Costs and benefits of glycemic control are sensitive to the HBA 1 c goal of care.
The Enhanced Primary Care Model Better than Carve Out Disease Management
Enhanced Primary Care Model--Advantages - Invest in Care System - -Extend Benefits to Multiple Clinical Domains - Strengthen, not Weaken Continuity and Coordination of Care - Seamless to Patients - Better Population Penetration
Successful Chronic Disease Care: Messages to Docs – Do This, or Die (Economic and Breadth of Practice Issues) – Don’t Blame Patients---Solve Problems – Doing things together is more important than doing things alone - Partner with the Patient - Team up with nurses, educators, other docs
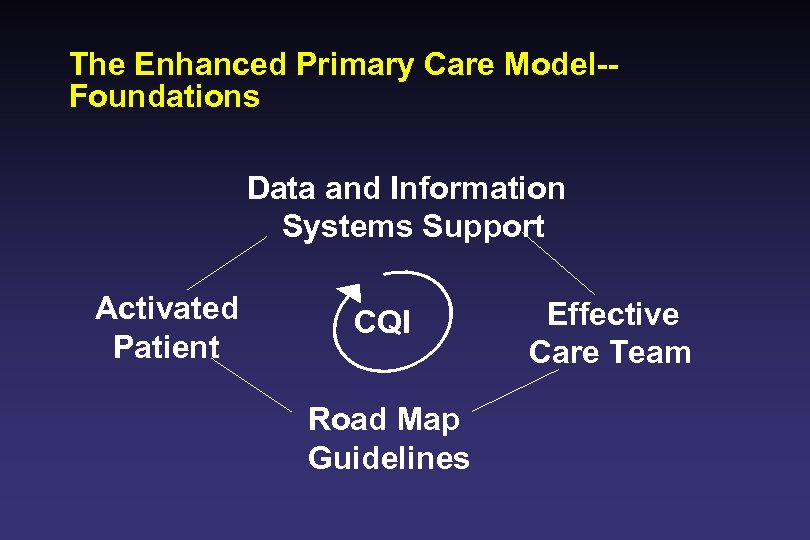
The Enhanced Primary Care Model-Foundations Data and Information Systems Support Activated Patient CQI Road Map Guidelines Effective Care Team
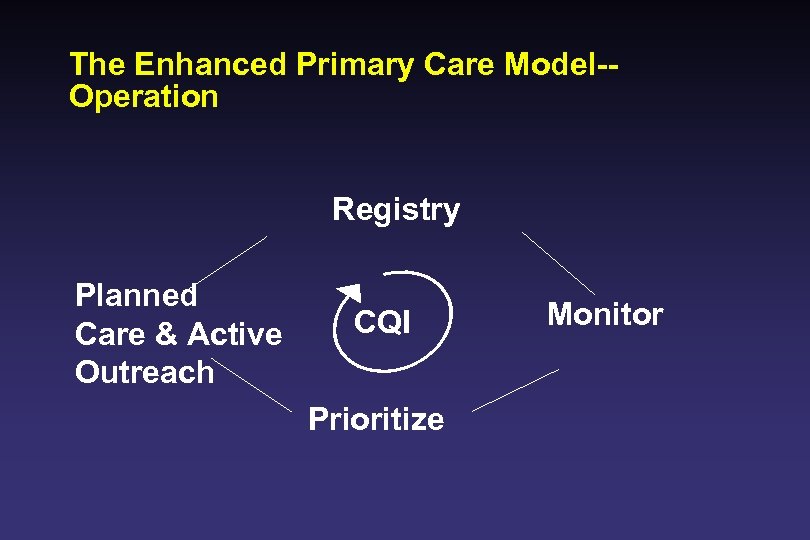
The Enhanced Primary Care Model-Operation Registry Planned Care & Active Outreach CQI Prioritize Monitor
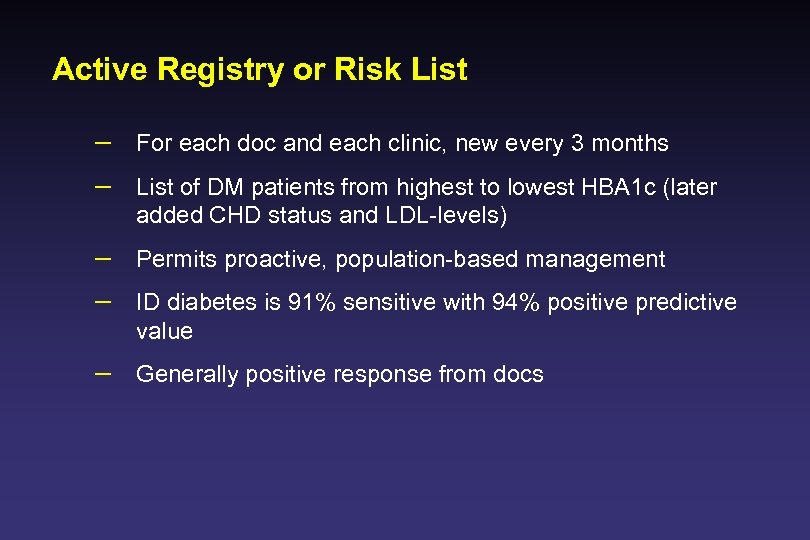
Active Registry or Risk List – For each doc and each clinic, new every 3 months – List of DM patients from highest to lowest HBA 1 c (later added CHD status and LDL-levels) – Permits proactive, population-based management – ID diabetes is 91% sensitive with 94% positive predictive value – Generally positive response from docs
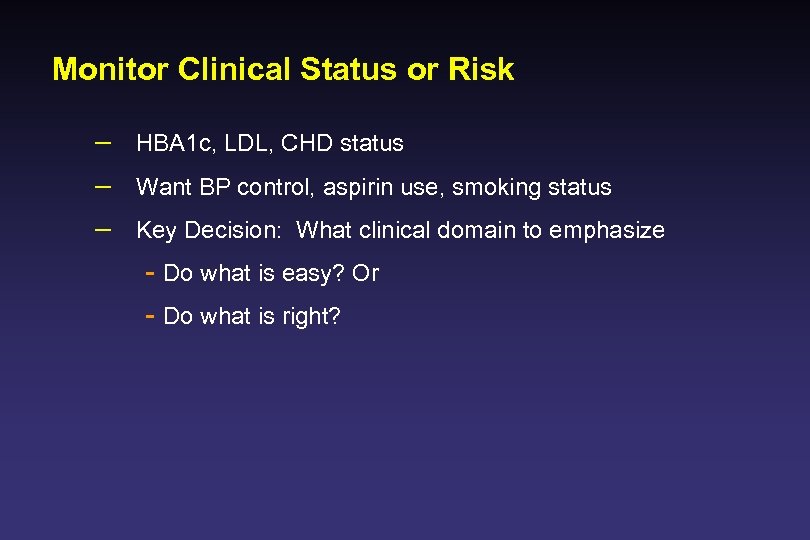
Monitor Clinical Status or Risk – HBA 1 c, LDL, CHD status – Want BP control, aspirin use, smoking status – Key Decision: What clinical domain to emphasize - Do what is easy? Or - Do what is right?
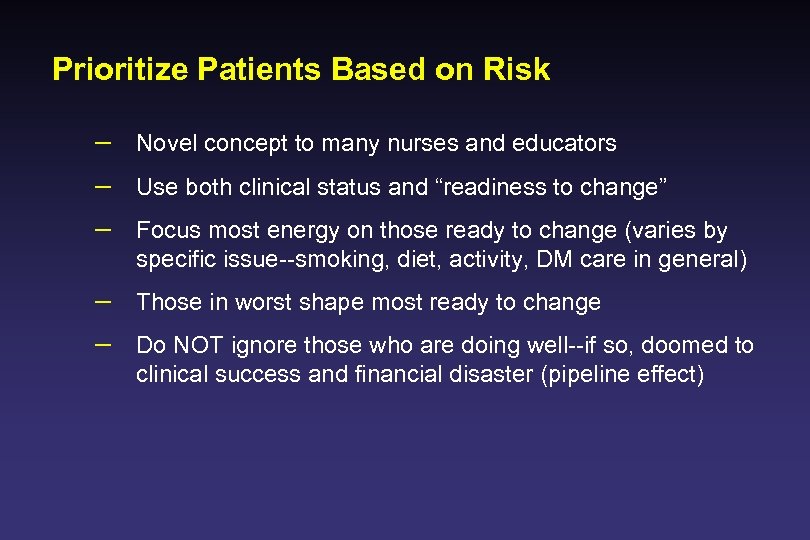
Prioritize Patients Based on Risk – Novel concept to many nurses and educators – Use both clinical status and “readiness to change” – Focus most energy on those ready to change (varies by specific issue--smoking, diet, activity, DM care in general) – Those in worst shape most ready to change – Do NOT ignore those who are doing well--if so, doomed to clinical success and financial disaster (pipeline effect)
Active Outreach -- Proactive Care – – – Need more than just docs to do this Empower nurses and educators Respect patient’s constitutional rights and privacy Calls come directly from clinic, usually a nurse pt knows First check: Medication intensity Second check: Motivational and educational needs
Visit Planning – – – A form of decision support Do the hard way, by hand--too expensive Do the easy way AMR/automated systems Flow sheets are the poor clinic’s solution to this problem Have not done yet, but results better than those who have made this a primary emphasis of improvement – AMR clinic with DM GL is good, but not best clinic
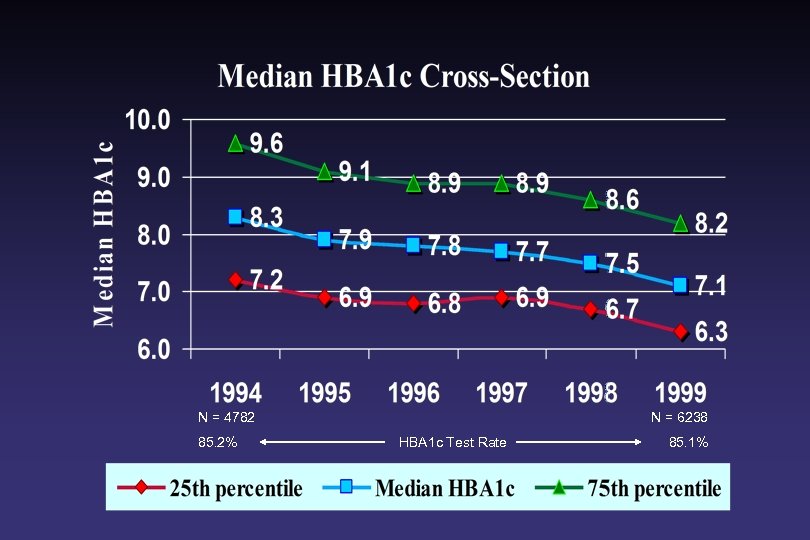
N = 4782 85. 2% N = 6238 HBA 1 c Test Rate 85. 1%
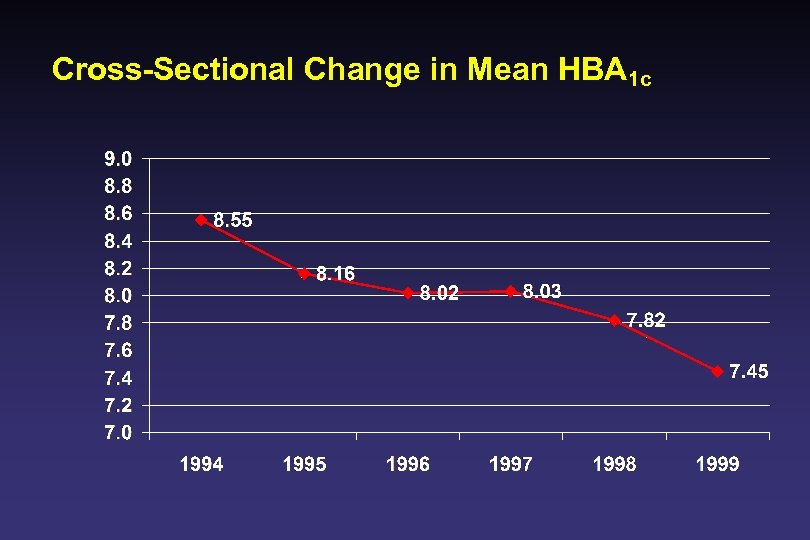
Cross-Sectional Change in Mean HBA 1 c
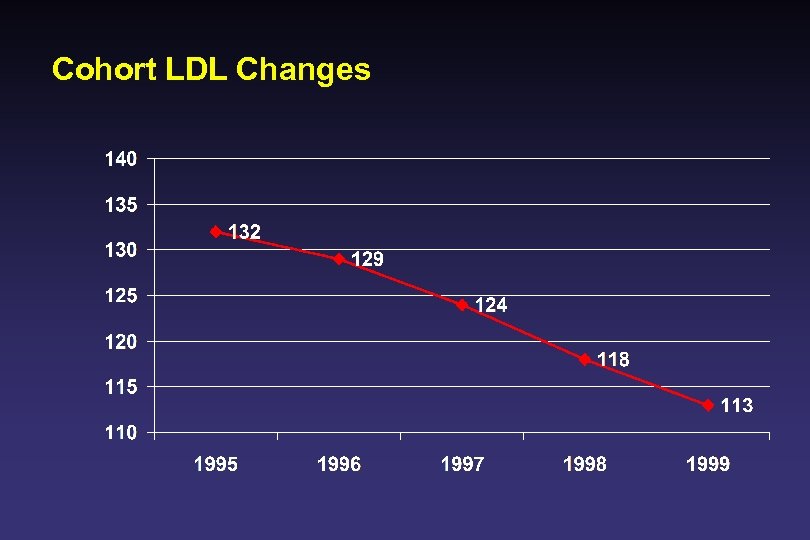
Cohort LDL Changes
Chronic Disease Care – – – Identify Problems Prioritize Problems in Partnership with Patient Initiate Treatment Monitor Response Titrate to Goal
Summary – 40% reduction in macrovascular risk – 25% reduction in microvascular risk – In well organized (enhanced) primary care clinics with a part time on-site DM nurse educator (not necessarily CDE) – Patient Education NOT associated with significantly better A 1 c – Improvement NOT due to: carve out disease management, endocrinology consults (<5% per year), less than 2% of patients use either TZD, alpha glucosidase, or meglitamides
Key Components – Medical Group Physician Involvement and Leadership – Resources--show ”cost of doing nothing” – Intelligent use of information: identify patients with diabetes, monitor, prioritize, proactive outreach & visit planning – Organize clinics to give proactive, population-based care – Intensify Treatment--Titrate to Goal – Consider Evidence AND Value when selecting improvement goals
Future Directions – – – Variation Continues--Plenty of room for more improvement Ascertain most appropriate level for QI intervention Focus on blood pressure reduction Focus on “Patient Activation” Focus on Visit Planning Focus on Physician decision making process and methods to change physician behavior – Development of “Patient Archetypes” to advance care
6915ecdc2adea5bf81dc7eac9bdca6a5.ppt