c93ae5eaa01f8f8dcc0f2d6700601b82.ppt
- Количество слайдов: 24
Improving cooperation for better chronic care Chris Ham HSMC University of Birmingham 3 April 2008 Bellagio
Some history • The journey from infectious diseases (19001950) to acute illnesses (1950 -2000) to chronic diseases (2000 -) • The acute care paradigm based on episodic care, hospital based treatment and increasing specialisation is anachronistic • A new paradigm is needed to respond to the increasing burden of chronic disease (Kane et al, 2005) 3 April 2008 Bellagio
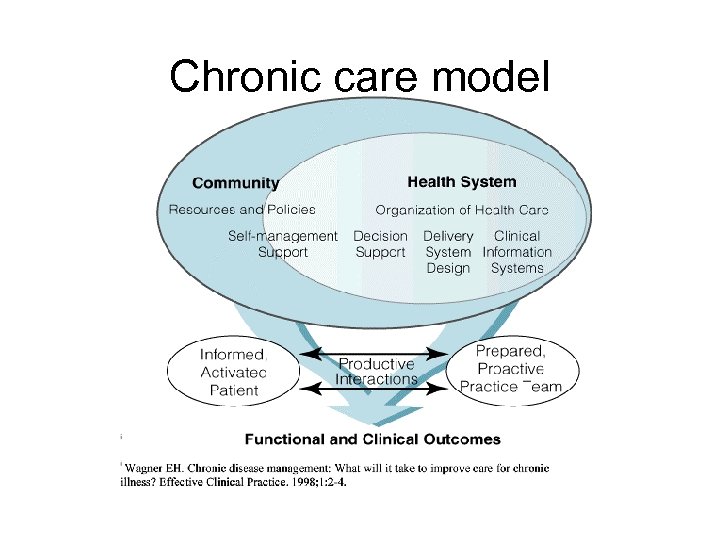
Chronic care model
The influence of the Chronic Care Model • The WHO’s Innovative Care for Chronic Conditions Framework • The Expanded Chronic Care Model (BC) • The NHS and Social Care Model in England (and variants in Scotland Wales) • The Model has also been adapted in other countries e. g. Australia and NZ C Ham and D Singh (2006) Improving care for people with long term conditions: a review of UK and international frameworks, HSMC, University of Birmingham 3 April 2008 Bellagio
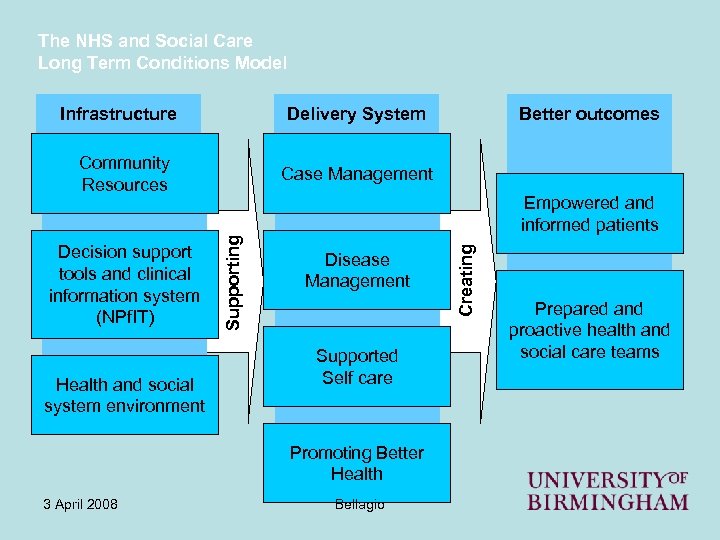
The NHS and Social Care Long Term Conditions Model Delivery System Infrastructure Community Resources Health and social system environment Case Management Disease Management Supported Self care Promoting Better Health 3 April 2008 Bellagio Creating Empowered and informed patients Supporting Decision support tools and clinical information system (NPf. IT) Better outcomes Prepared and proactive health and social care teams
Some important elements in the Chronic Care Model • Informed and expert patients, taking control of their conditions • Team based care using the skills of doctors, nurses and others • Collaboration and partnership between patients and teams • Integration of care – primary and secondary care; health and social care 3 April 2008 Bellagio
Gaps in chronic care • Commonwealth Fund Survey of six countries, 2005 • Advice on self management was not routine in any country • There were variations in the use of nurses to provide diabetes care • Among patients with diabetes and hypertension, those receiving all tests fell short of recommended care 3 April 2008 Bellagio
Gaps (2) • Sizable majorities of patients reported their medications had not been reviewed • Many patients reported that physicians had not explained side effects • There were shortcomings in physicianpatient communication • There were also shortcomings in care coordination (the next big thing? ) 3 April 2008 Bellagio
Moving forward • How can these gaps in care be filled? • How can international experience and research evidence be used? • What are the implications for policy and practice? • What are the characteristics of the high performing chronic care system? 3 April 2008 Bellagio
10 characteristics • Ensuring universal coverage • Care free at the point of use • A focus on prevention e. g. the new contract for family physicians in the NHS • Priority for self management • An emphasis on primary health care (the importance of the medical home) 3 April 2008 Bellagio
10 characteristics contd. • An emphasis on population management/risk assessment • Care should be integrated (let’s debate what that means) • IT should be used, especially the electronic care record and telehealth • Care should be coordinated (see new OECD report) • These 9 characteristics need to be linked into a coherent whole 3 April 2008 Bellagio
Four supporting strategies • Physician leadership • Measuring outcomes and using the results to drive performance improvement • Aligning incentives e. g. the new contract for family physicians in the NHS • Engaging the community e. g. NZ experience of working with Maori 3 April 2008 Bellagio
Paying GPs for quality • GPs paid using mixture of capitation, salary and fee for service in the past • New payments (April 2004) emphasise quality of care • Payments are based on ‘quality and outcomes framework’ (QOF) • QOF is based on 10 common chronic conditions 3 April 2008 Bellagio
The QOF (1) • GPs earn points if they meet performance targets • Targets cover aspects of care such as blood pressure recording and control • Points convert into extra income for GPs • The incentives are big: up to one third extra income if targets are met 3 April 2008 Bellagio
The QOF (2) • Clinical indicators make up around 50% of the QOF • Organisation of care, patient experience, and providing additional services make up the other 50% • Performance is based on self assessment – a high trust contract • External audit is used to supplement self assessment 3 April 2008 Bellagio

Some US examples of integrated care • • • Kaiser Permanente Group Health Cooperative Veterans Health Administration Health Partners Alaskan Medical Service None is perfect, but all seem to perform better than other forms of care 3 April 2008 Bellagio

Some other examples • Integrated health boards in Scotland • Integrated health boards in New Zealand • Integrated health and social care organisations in Northern Ireland • Care Trusts bringing together health and social care in parts of England • Esther project in Jonkoping, Sweden 3 April 2008 Bellagio
A detour to the UK • The UK has a strong primary care orientation • Patients are registered with a primary care team that serves as a medical home (typically 3 -4 physicians, nurses and others) • The best teams provide high quality care based on registration, recall and review • Major weaknesses in the UK are variable standards of primary care and poor integration/coordination with secondary care 3 April 2008 Bellagio
A detour (2) • The NHS suffers from the historical division in British medicine, separating family physicians from hospital specialists • US integrated systems like Kaiser hold lessons for the NHS, especially in multispecialty medical practice • But the NHS has the potential to achieve closer integration of health and social care, and in some places this is happening • New policies like practice based commissioning may support closer integration 3 April 2008 Bellagio
What is integration? • Vertical or virtual? • Organisational, clinical or service integration? • Integrated provision of care or integrated provision and funding? • Integration of all services or focused integration for specific diseases/care groups e. g. frail older people? 3 April 2008 Bellagio
Care coordination • Coordination is particularly important for people with multiple chronic conditions • Primary care (where it works well) can provide coordination • Other approaches have also been used e. g. case managers/community matrons • Patients/families may be care coordinators by default or by design (e. g. by holding budgets) • More than one approach is likely to be needed 3 April 2008 Bellagio
Barriers to integration • • • Organisational fragmentation Budgetary fragmentation Perverse incentives Professional fragmentation Conservatism and inertia 3 April 2008 Bellagio
Context is critical • Different systems need to find their own solutions reflecting different contexts • How are the systems represented here rising to these challenges? • Are there other and emerging approaches to care integration we can learn from? • How can approaches be adapted to fit different contexts? 3 April 2008 Bellagio
Language • The language we use may be a barrier to improvement – patients/clients need the right care in the right place at the right time • Is it still helpful to talk about primary care, secondary care and social care? • Or do we need to find a new vocabulary to suit the times? 3 April 2008 Bellagio
c93ae5eaa01f8f8dcc0f2d6700601b82.ppt