b6e8688310e9400f31d1b1a121622238.ppt
- Количество слайдов: 33
 Improve the Patient Referral Process at the Mercy Family Medicine Residency Program Des Moines, Ia December 2, 2011 Connie Mitchell LBSW, MHA
Improve the Patient Referral Process at the Mercy Family Medicine Residency Program Des Moines, Ia December 2, 2011 Connie Mitchell LBSW, MHA
 Mercy Family Medicine Residency Program
Mercy Family Medicine Residency Program
 Objectives s Participants will: • Be able to use the Work-Out methodology to make process change • Understand how education occurs while change is implemented • Importance of measuring outcomes with a process change • See how Work-Out was used to make changes to the referral process
Objectives s Participants will: • Be able to use the Work-Out methodology to make process change • Understand how education occurs while change is implemented • Importance of measuring outcomes with a process change • See how Work-Out was used to make changes to the referral process
 Background s The patient referral process is one of the most important functions of primary care. s Referrals can cause unnecessary delays and challenges for patients, physicians and clinic staff. s As discovered in interviews with the Mercy Family Medicine Residency (MFMRP) Referral Liaison and clinic physician staff, rework and delays exist in the current clinic referral process.
Background s The patient referral process is one of the most important functions of primary care. s Referrals can cause unnecessary delays and challenges for patients, physicians and clinic staff. s As discovered in interviews with the Mercy Family Medicine Residency (MFMRP) Referral Liaison and clinic physician staff, rework and delays exist in the current clinic referral process.
 Literature Review s Errors or lost referrals(Weiner, Perkins, and Callahan, 2008) s Physicians dissatisfaction (Modak, Sexton, Lux, Helmreick and Thomas, 2007) s Time is not reimbursable ( Farber, Siu and Bloom, 2007)
Literature Review s Errors or lost referrals(Weiner, Perkins, and Callahan, 2008) s Physicians dissatisfaction (Modak, Sexton, Lux, Helmreick and Thomas, 2007) s Time is not reimbursable ( Farber, Siu and Bloom, 2007)
 Literature Review s The transfer of information improves patient satisfaction (Ireson, Slavova, Steletenkamp, and Scutchfield, 2009). s Standardized referral forms improve quality of patient care ( Berta et al. , 2008). s Use of electronic medical records or web-based systems: • Improves the flow of patient information(Weiner et al. , 2009). • Increases physician satisfaction in the referral process (Kim, Chen, Keith, Yee, and Kushel (2009).
Literature Review s The transfer of information improves patient satisfaction (Ireson, Slavova, Steletenkamp, and Scutchfield, 2009). s Standardized referral forms improve quality of patient care ( Berta et al. , 2008). s Use of electronic medical records or web-based systems: • Improves the flow of patient information(Weiner et al. , 2009). • Increases physician satisfaction in the referral process (Kim, Chen, Keith, Yee, and Kushel (2009).
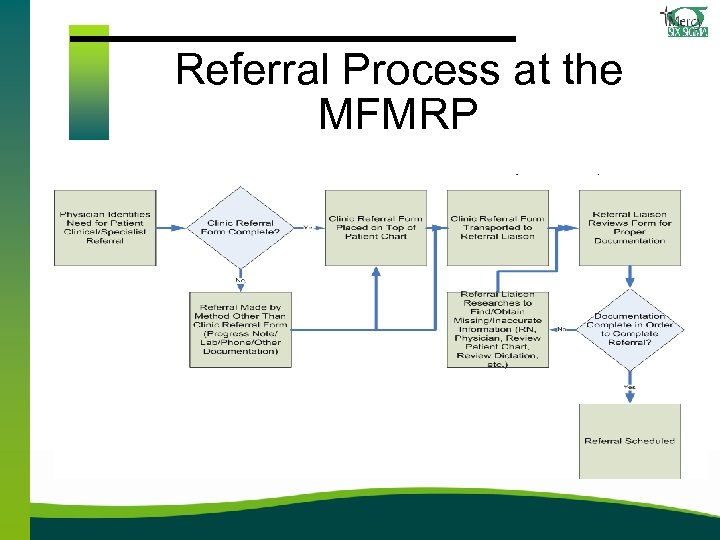 Referral Process at the MFMRP
Referral Process at the MFMRP
 Problem/Need s In a twenty day timeframe: • • 54 of 219 referrals were incomplete 76 errors on the 219 referrals. s Defective referral sheets require that the Patient Referral Liaison follow-up to obtain additional information and/or clarification of existing information. s This creates re-work for staff, delays for referral processing, delays in obtaining insurance pre-authorizations/pre-certifications, decreased patient/staff satisfaction, potential for duplication of referrals and delays in patient care, is a financial concern. s The problem is ongoing. s The problem links to Mercy's commitment to improve productivity, customer service, and education of resident physicians working at the Mercy Family Medicine Residency Program.
Problem/Need s In a twenty day timeframe: • • 54 of 219 referrals were incomplete 76 errors on the 219 referrals. s Defective referral sheets require that the Patient Referral Liaison follow-up to obtain additional information and/or clarification of existing information. s This creates re-work for staff, delays for referral processing, delays in obtaining insurance pre-authorizations/pre-certifications, decreased patient/staff satisfaction, potential for duplication of referrals and delays in patient care, is a financial concern. s The problem is ongoing. s The problem links to Mercy's commitment to improve productivity, customer service, and education of resident physicians working at the Mercy Family Medicine Residency Program.
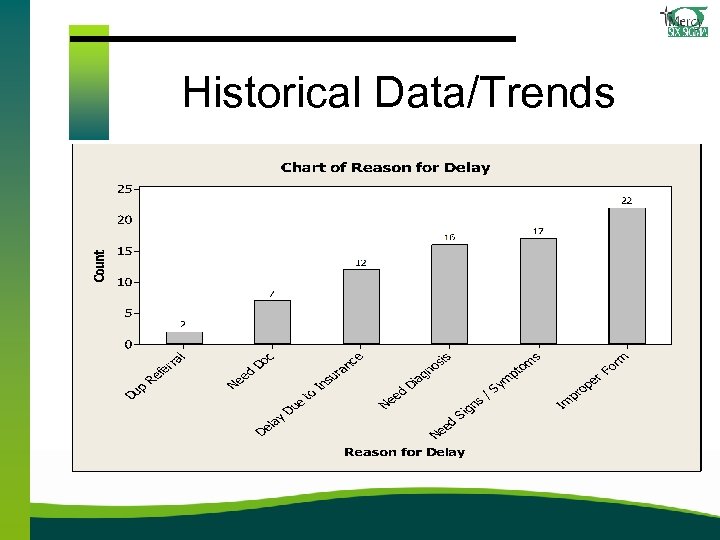 Historical Data/Trends
Historical Data/Trends
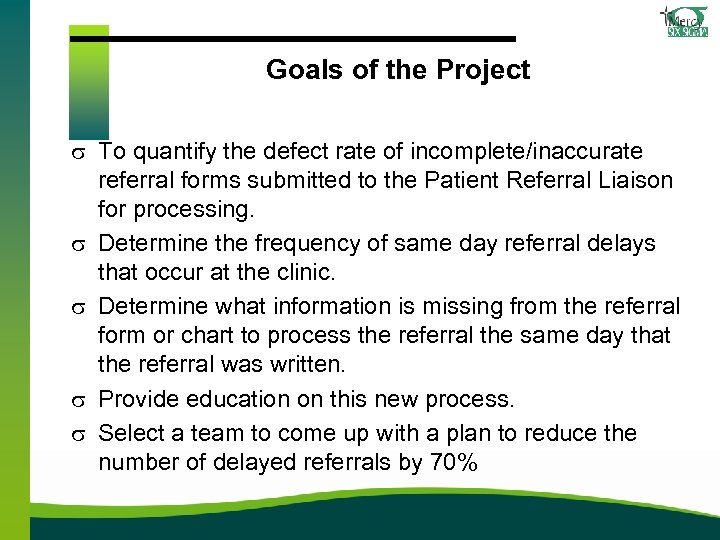 Goals of the Project s To quantify the defect rate of incomplete/inaccurate referral forms submitted to the Patient Referral Liaison for processing. s Determine the frequency of same day referral delays that occur at the clinic. s Determine what information is missing from the referral form or chart to process the referral the same day that the referral was written. s Provide education on this new process. s Select a team to come up with a plan to reduce the number of delayed referrals by 70%
Goals of the Project s To quantify the defect rate of incomplete/inaccurate referral forms submitted to the Patient Referral Liaison for processing. s Determine the frequency of same day referral delays that occur at the clinic. s Determine what information is missing from the referral form or chart to process the referral the same day that the referral was written. s Provide education on this new process. s Select a team to come up with a plan to reduce the number of delayed referrals by 70%
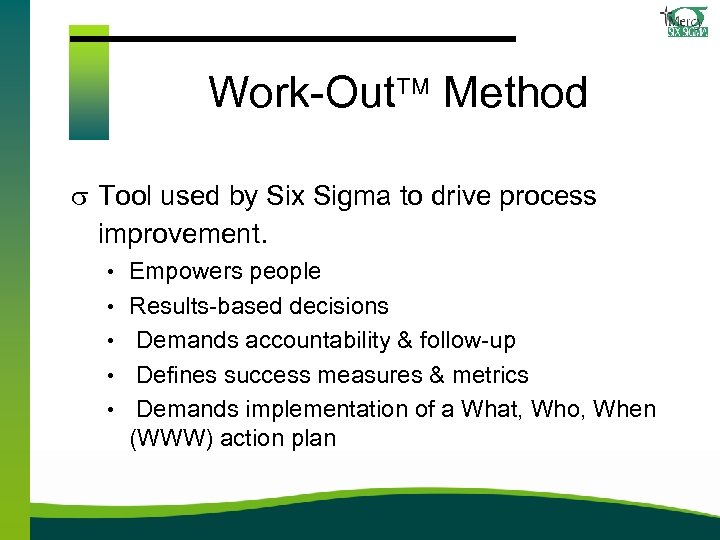 Work-Out Method s Tool used by Six Sigma to drive process improvement. • Empowers people • Results-based decisions • Demands accountability & follow-up • Defines success measures & metrics • Demands implementation of a What, Who, When (WWW) action plan
Work-Out Method s Tool used by Six Sigma to drive process improvement. • Empowers people • Results-based decisions • Demands accountability & follow-up • Defines success measures & metrics • Demands implementation of a What, Who, When (WWW) action plan
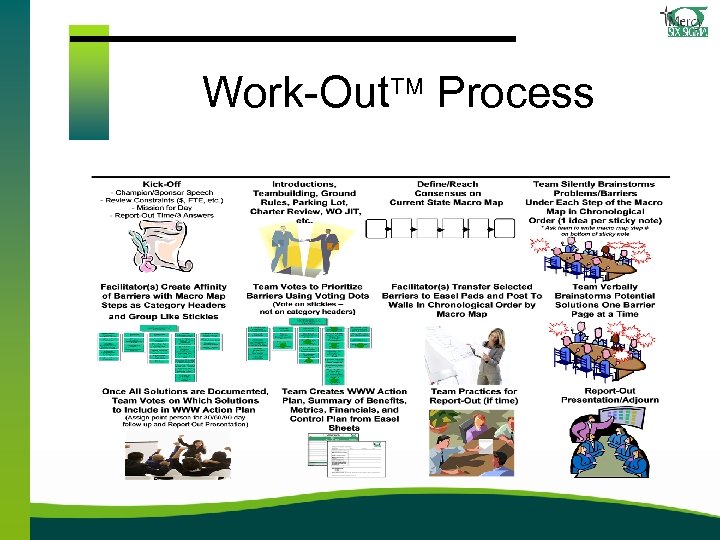 Work-Out Process
Work-Out Process
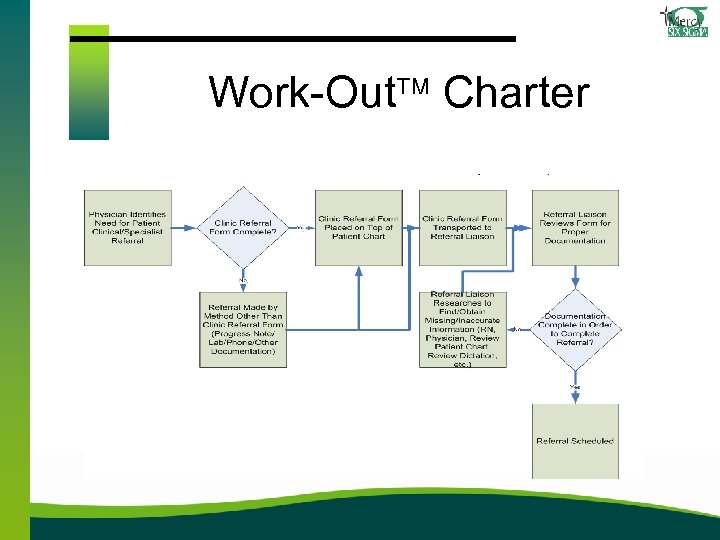 Work-Out Charter
Work-Out Charter
 Work-Out Team s Members of the team are experience, have knowledge about the concern, and have a stake in the issue. s Team is challenged to develop solutions and an action plan to make change.
Work-Out Team s Members of the team are experience, have knowledge about the concern, and have a stake in the issue. s Team is challenged to develop solutions and an action plan to make change.
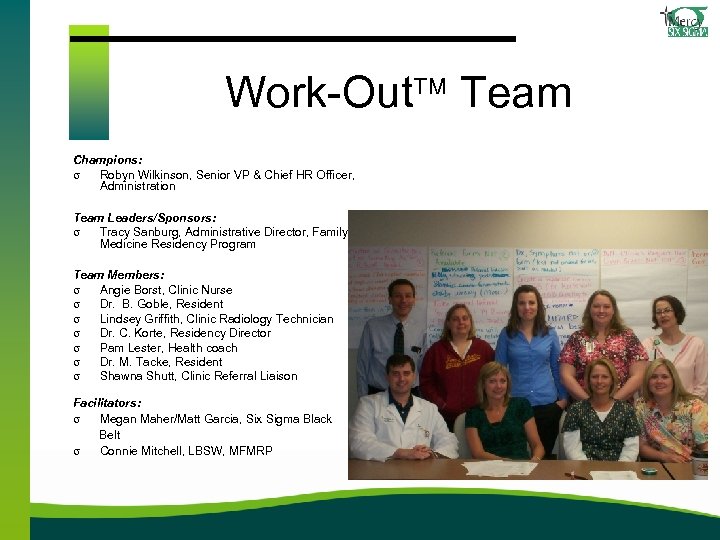 Work-Out Team Champions: s Robyn Wilkinson, Senior VP & Chief HR Officer, Administration Team Leaders/Sponsors: s Tracy Sanburg, Administrative Director, Family Medicine Residency Program Team Members: s Angie Borst, Clinic Nurse s Dr. B. Goble, Resident s Lindsey Griffith, Clinic Radiology Technician s Dr. C. Korte, Residency Director s Pam Lester, Health coach s Dr. M. Tacke, Resident s Shawna Shutt, Clinic Referral Liaison Facilitators: s Megan Maher/Matt Garcia, Six Sigma Black Belt s Connie Mitchell, LBSW, MFMRP
Work-Out Team Champions: s Robyn Wilkinson, Senior VP & Chief HR Officer, Administration Team Leaders/Sponsors: s Tracy Sanburg, Administrative Director, Family Medicine Residency Program Team Members: s Angie Borst, Clinic Nurse s Dr. B. Goble, Resident s Lindsey Griffith, Clinic Radiology Technician s Dr. C. Korte, Residency Director s Pam Lester, Health coach s Dr. M. Tacke, Resident s Shawna Shutt, Clinic Referral Liaison Facilitators: s Megan Maher/Matt Garcia, Six Sigma Black Belt s Connie Mitchell, LBSW, MFMRP
 Mission s Reduce the number of incomplete / inaccurate referral sheets from 24% to 7% by December 2010. s A secondary goal of eliminating errors in the referral process.
Mission s Reduce the number of incomplete / inaccurate referral sheets from 24% to 7% by December 2010. s A secondary goal of eliminating errors in the referral process.
 Scope s For the purpose of this project, the referral process began when a physician identifies a need for a clinical/specialty referral for a patient and ended when the referral was scheduled.
Scope s For the purpose of this project, the referral process began when a physician identifies a need for a clinical/specialty referral for a patient and ended when the referral was scheduled.
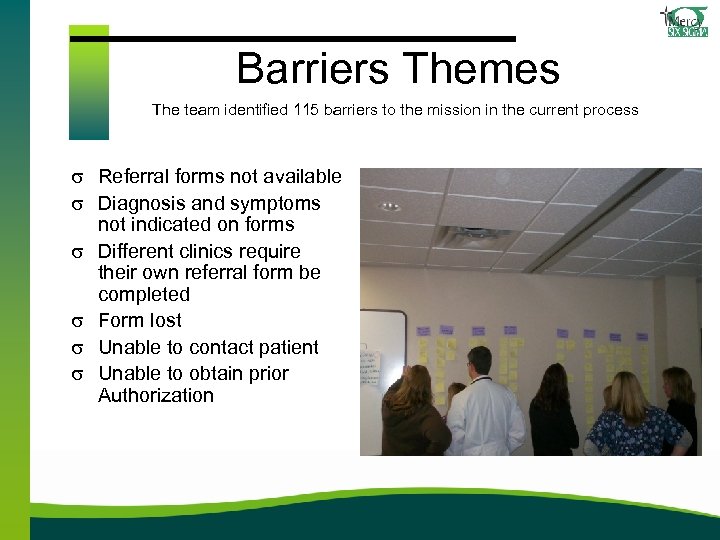 Barriers Themes The team identified 115 barriers to the mission in the current process s Referral forms not available s Diagnosis and symptoms not indicated on forms s Different clinics require their own referral form be completed s Form lost s Unable to contact patient s Unable to obtain prior Authorization
Barriers Themes The team identified 115 barriers to the mission in the current process s Referral forms not available s Diagnosis and symptoms not indicated on forms s Different clinics require their own referral form be completed s Form lost s Unable to contact patient s Unable to obtain prior Authorization
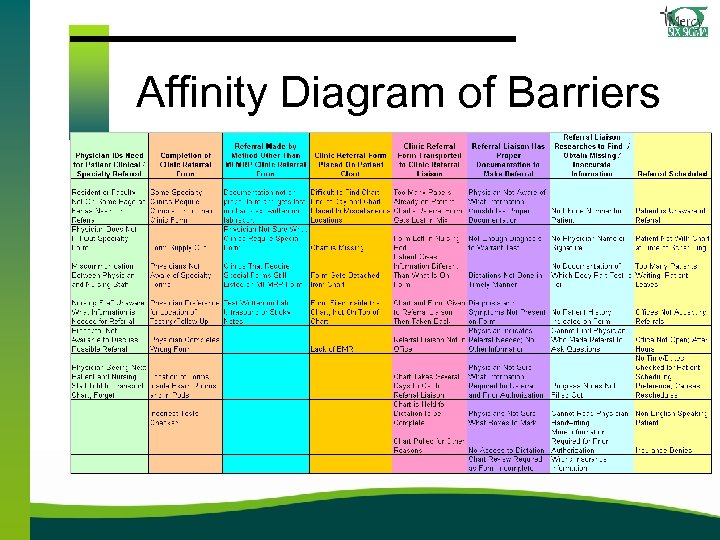 Affinity Diagram of Barriers
Affinity Diagram of Barriers
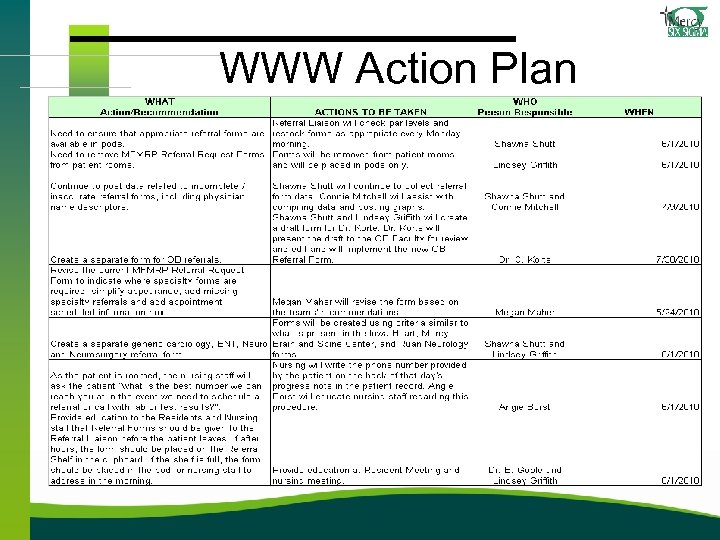 WWW Action Plan
WWW Action Plan
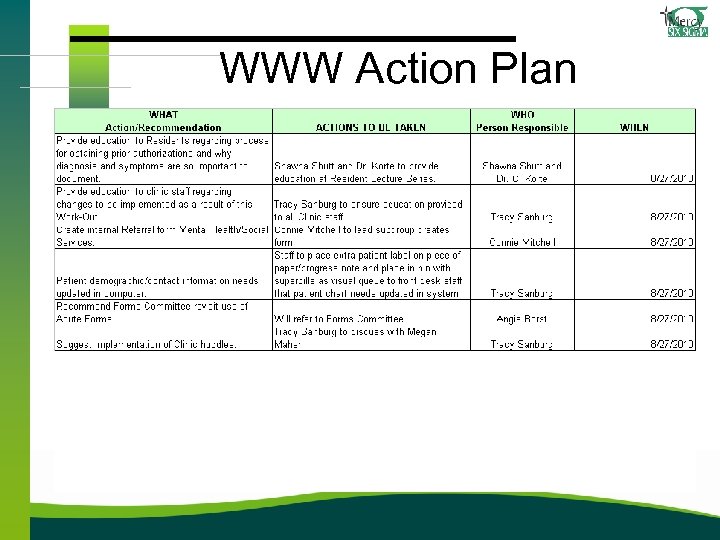 WWW Action Plan
WWW Action Plan
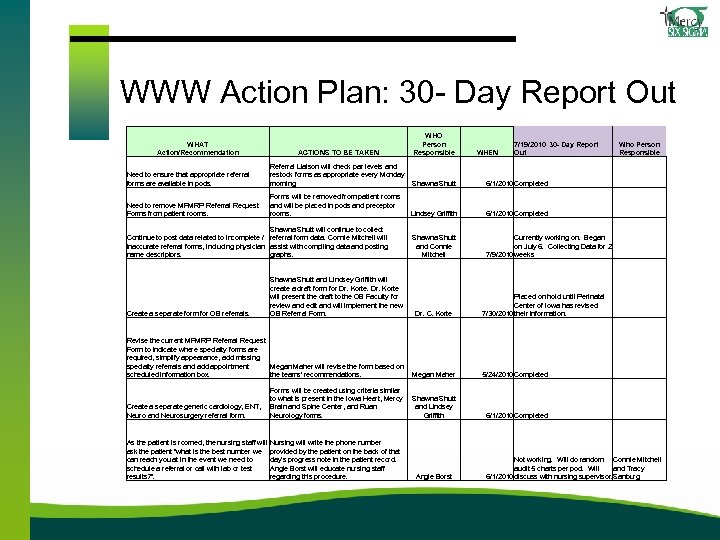 WWW Action Plan: 30 - Day Report Out WHAT Action/Recommendation ACTIONS TO BE TAKEN WHO Person Responsible WHEN 7/19/2010 30 - Day Report Out Who Person Responsible Need to ensure that appropriate referral forms are available in pods. Referral Liaison will check par levels and restock forms as appropriate every Monday morning. Shawna Shutt 6/1/2010 Completed Need to remove MFMRP Referral Request Forms from patient rooms. Forms will be removed from patient rooms and will be placed in pods and preceptor rooms. Lindsey Griffith 6/1/2010 Completed Shawna Shutt and Connie Mitchell Currently working on. Began on July 6. Collecting Data for 2 7/9/2010 weeks Dr. C. Korte Placed on hold until Perinatal Center of Iowa has revised 7/30/2010 their information. Shawna Shutt will continue to collect Continue to post data related to incomplete / referral form data. Connie Mitchell will inaccurate referral forms, including physician assist with compiling data and posting name descriptors. graphs. Create a separate form for OB referrals. Shawna Shutt and Lindsey Griffith will create a draft form for Dr. Korte will present the draft to the OB Faculty for review and edit and will implement the new OB Referral Form. Revise the current MFMRP Referral Request Form to indicate where specialty forms are required, simplify appearance, add missing specialty referrals and add appointment Megan Maher will revise the form based on scheduled information box. the teams' recommendations. Megan Maher Create a separate generic cardiology, ENT, Neuro and Neurosurgery referral form. Forms will be created using criteria similar to what is present in the Iowa Heart, Mercy Brain and Spine Center, and Ruan Neurology forms. As the patient is roomed, the nursing staff will Nursing will write the phone number ask the patient "what is the best number we provided by the patient on the back of that can reach you at in the event we need to day's progress note in the patient record. schedule a referral or call with lab or test Angie Borst will educate nursing staff results? ". regarding this procedure. Shawna Shutt and Lindsey Griffith Angie Borst 5/24/2010 Completed 6/1/2010 Completed Not working. Will do random Connie Mitchell audit 5 charts per pod. Will and Tracy 6/1/2010 discuss with nursing supervisor. Sanburg
WWW Action Plan: 30 - Day Report Out WHAT Action/Recommendation ACTIONS TO BE TAKEN WHO Person Responsible WHEN 7/19/2010 30 - Day Report Out Who Person Responsible Need to ensure that appropriate referral forms are available in pods. Referral Liaison will check par levels and restock forms as appropriate every Monday morning. Shawna Shutt 6/1/2010 Completed Need to remove MFMRP Referral Request Forms from patient rooms. Forms will be removed from patient rooms and will be placed in pods and preceptor rooms. Lindsey Griffith 6/1/2010 Completed Shawna Shutt and Connie Mitchell Currently working on. Began on July 6. Collecting Data for 2 7/9/2010 weeks Dr. C. Korte Placed on hold until Perinatal Center of Iowa has revised 7/30/2010 their information. Shawna Shutt will continue to collect Continue to post data related to incomplete / referral form data. Connie Mitchell will inaccurate referral forms, including physician assist with compiling data and posting name descriptors. graphs. Create a separate form for OB referrals. Shawna Shutt and Lindsey Griffith will create a draft form for Dr. Korte will present the draft to the OB Faculty for review and edit and will implement the new OB Referral Form. Revise the current MFMRP Referral Request Form to indicate where specialty forms are required, simplify appearance, add missing specialty referrals and add appointment Megan Maher will revise the form based on scheduled information box. the teams' recommendations. Megan Maher Create a separate generic cardiology, ENT, Neuro and Neurosurgery referral form. Forms will be created using criteria similar to what is present in the Iowa Heart, Mercy Brain and Spine Center, and Ruan Neurology forms. As the patient is roomed, the nursing staff will Nursing will write the phone number ask the patient "what is the best number we provided by the patient on the back of that can reach you at in the event we need to day's progress note in the patient record. schedule a referral or call with lab or test Angie Borst will educate nursing staff results? ". regarding this procedure. Shawna Shutt and Lindsey Griffith Angie Borst 5/24/2010 Completed 6/1/2010 Completed Not working. Will do random Connie Mitchell audit 5 charts per pod. Will and Tracy 6/1/2010 discuss with nursing supervisor. Sanburg
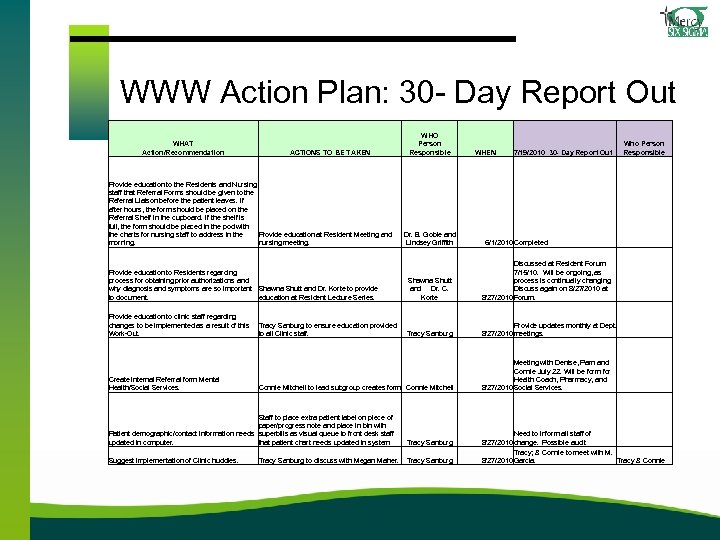 WWW Action Plan: 30 - Day Report Out WHAT Action/Recommendation ACTIONS TO BE TAKEN Provide education to the Residents and Nursing staff that Referral Forms should be given to the Referral Liaison before the patient leaves. If after hours, the form should be placed on the Referral Shelf in the cupboard. If the shelf is full, the form should be placed in the pod with Provide education at Resident Meeting and the charts for nursing staff to address in the nursing meeting. morning. WHO Person Responsible Dr. B. Goble and Lindsey Griffith WHEN Who Person Responsible 7/19/2010 30 - Day Report Out 6/1/2010 Completed Provide education to Residents regarding process for obtaining prior authorizations and why diagnosis and symptoms are so important Shawna Shutt and Dr. Korte to provide to document. education at Resident Lecture Series. Shawna Shutt and Dr. C. Korte Discussed at Resident Forum 7/15/10. Will be ongoing, as process is continually changing. Discuss again on 8/27/2010 at 8/27/2010 Forum. Provide education to clinic staff regarding changes to be implemented as a result of this Work-Out. Tracy Sanburg Provide updates monthly at Dept. 8/27/2010 meetings. Connie Mitchell to lead subgroup creates form. Connie Mitchell Meeting with Denise, Pam and Connie July 22. Will be form for Health Coach, Pharmacy, and 8/27/2010 Social Services. Create internal Referral form Mental Health/Social Services. Tracy Sanburg to ensure education provided to all Clinic staff. Staff to place extra patient label on piece of paper/progress note and place in bin with Patient demographic/contact information needs superbills as visual queue to front desk staff updated in computer. that patient chart needs updated in system Tracy Sanburg Suggest implementation of Clinic huddles. Tracy Sanburg to discuss with Megan Maher. Need to inform all staff of 8/27/2010 change. Possible audit Tracy; & Connie to meet with M. 8/27/2010 Garcia. Tracy & Connie
WWW Action Plan: 30 - Day Report Out WHAT Action/Recommendation ACTIONS TO BE TAKEN Provide education to the Residents and Nursing staff that Referral Forms should be given to the Referral Liaison before the patient leaves. If after hours, the form should be placed on the Referral Shelf in the cupboard. If the shelf is full, the form should be placed in the pod with Provide education at Resident Meeting and the charts for nursing staff to address in the nursing meeting. morning. WHO Person Responsible Dr. B. Goble and Lindsey Griffith WHEN Who Person Responsible 7/19/2010 30 - Day Report Out 6/1/2010 Completed Provide education to Residents regarding process for obtaining prior authorizations and why diagnosis and symptoms are so important Shawna Shutt and Dr. Korte to provide to document. education at Resident Lecture Series. Shawna Shutt and Dr. C. Korte Discussed at Resident Forum 7/15/10. Will be ongoing, as process is continually changing. Discuss again on 8/27/2010 at 8/27/2010 Forum. Provide education to clinic staff regarding changes to be implemented as a result of this Work-Out. Tracy Sanburg Provide updates monthly at Dept. 8/27/2010 meetings. Connie Mitchell to lead subgroup creates form. Connie Mitchell Meeting with Denise, Pam and Connie July 22. Will be form for Health Coach, Pharmacy, and 8/27/2010 Social Services. Create internal Referral form Mental Health/Social Services. Tracy Sanburg to ensure education provided to all Clinic staff. Staff to place extra patient label on piece of paper/progress note and place in bin with Patient demographic/contact information needs superbills as visual queue to front desk staff updated in computer. that patient chart needs updated in system Tracy Sanburg Suggest implementation of Clinic huddles. Tracy Sanburg to discuss with Megan Maher. Need to inform all staff of 8/27/2010 change. Possible audit Tracy; & Connie to meet with M. 8/27/2010 Garcia. Tracy & Connie
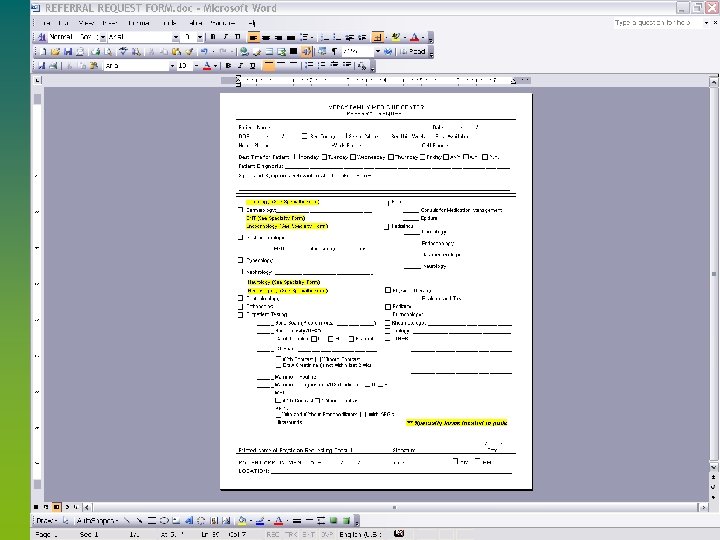
 Action Steps Completed s Revised referral form s All referral forms were placed in a central location s Designated person was assigned to stock the referral forms weekly s Education was provided “Referral 101” s Standardize a location for referral forms and charts at end of day
Action Steps Completed s Revised referral form s All referral forms were placed in a central location s Designated person was assigned to stock the referral forms weekly s Education was provided “Referral 101” s Standardize a location for referral forms and charts at end of day
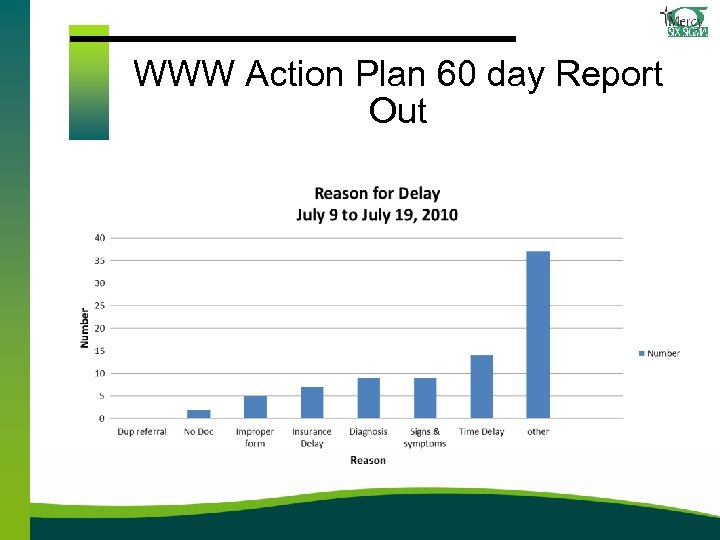 WWW Action Plan 60 day Report Out
WWW Action Plan 60 day Report Out
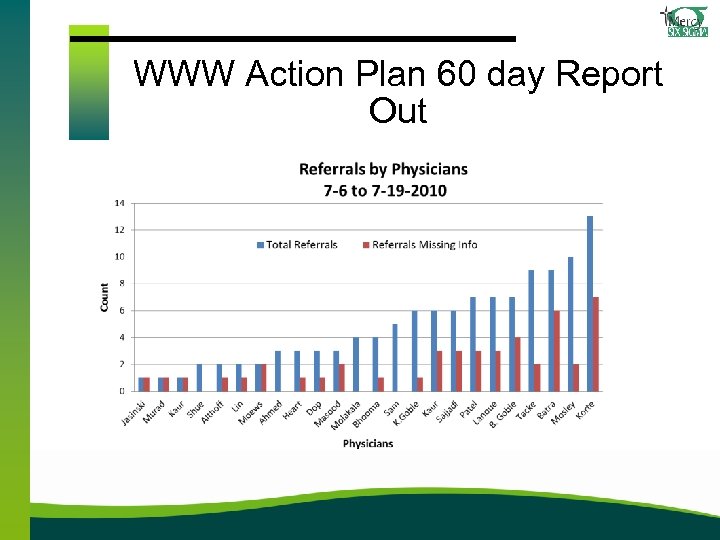 WWW Action Plan 60 day Report Out
WWW Action Plan 60 day Report Out
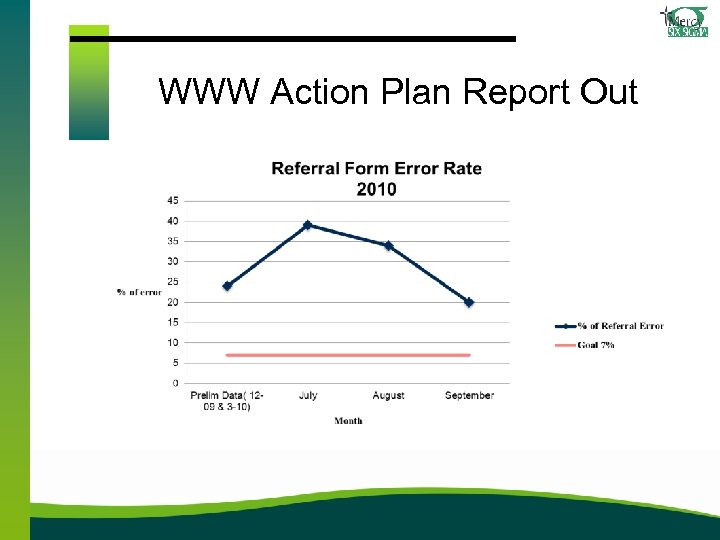 WWW Action Plan Report Out
WWW Action Plan Report Out
 Additional Successful WWW Action Plan Tasks s New OB referral form was developed s Education was ongoing for this process s Internal referral form for Allied staff within the clinic was developed s “Huddle” concept was discussed but not implemented s Not necessary for the team to continue to meet
Additional Successful WWW Action Plan Tasks s New OB referral form was developed s Education was ongoing for this process s Internal referral form for Allied staff within the clinic was developed s “Huddle” concept was discussed but not implemented s Not necessary for the team to continue to meet
 WWW Action Plan items not implemented s Current patient telephone numbers on the chart
WWW Action Plan items not implemented s Current patient telephone numbers on the chart
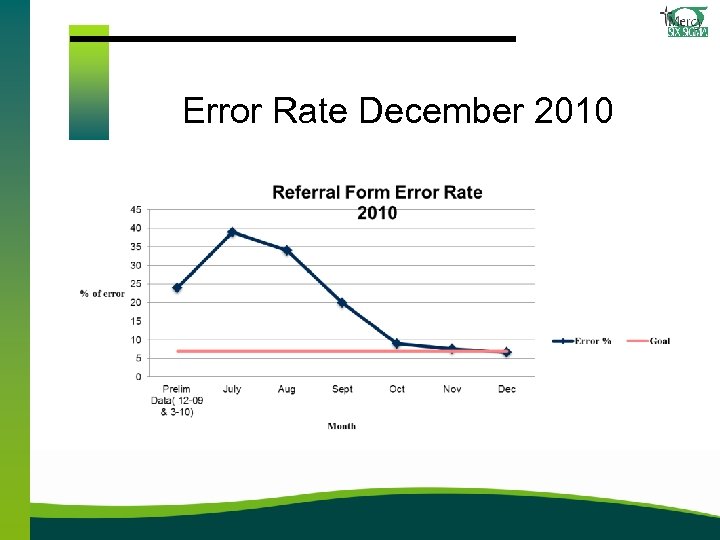 Error Rate December 2010
Error Rate December 2010
 References Berta, W. , Barnsley, J. , Bloom, J. , Cockerill, R. , Davis, D. , Jaakkimainen, L. , Mior, A. M. , . . . Vayda, E. (2008). Enhancing continuity of information: Essential components of a referral document. Canadian Family Physician, 54(10), 1432 -1433. e 1 -6. Retrieved from http: //www. cfp. ca/ Bodenheimer, T. , Lo, B. , & Casalino, L. (1999). Primary care physicians should be coordinators, not gatekeepers. Journal of the American Medical Association, 281(2), 2045 -2049. doi: 10. 1001/jama. 281. 2045 Centers for Medicare & Medicaid Services. (2010). CMS manual system. Retrieved from Centers for Medicare and Medicaid Services website: http: //www. cms. gov/transmittals/downloads/R 327 P 1. pdf Farber, J. , Siu, A. , & Bloom, P. (2007). How much time do physicians spend providing care outside of office visits? Annuals of Internal Medicine, 147(10), 693 -698. Retrieved from http: //www. cinahl. com/cgi -bin/refsvc. html/ Ireson, C. L. , Slavova, S. , Steltenkamp, C. L. , & Scutchfield, F. D. (2009). Bridging the care continuum: Patient information needs for specialist referrals. BMC Health Services Research, 9, 163 -179. doi: 10. 1186/1472 -6963 -9 -163 Kim, Y. , Chen, A. H. , Keith, E. , Yee, H. F. , & Kushel, M. B. (2009). Not perfect, but better: Primary care providers' experiences with electronic referrals in a safety net health system. Journal of General Internal Medicine, 24(5), 614 -619. doi: 10. 1007/s 11606 -009 -0955 -3
References Berta, W. , Barnsley, J. , Bloom, J. , Cockerill, R. , Davis, D. , Jaakkimainen, L. , Mior, A. M. , . . . Vayda, E. (2008). Enhancing continuity of information: Essential components of a referral document. Canadian Family Physician, 54(10), 1432 -1433. e 1 -6. Retrieved from http: //www. cfp. ca/ Bodenheimer, T. , Lo, B. , & Casalino, L. (1999). Primary care physicians should be coordinators, not gatekeepers. Journal of the American Medical Association, 281(2), 2045 -2049. doi: 10. 1001/jama. 281. 2045 Centers for Medicare & Medicaid Services. (2010). CMS manual system. Retrieved from Centers for Medicare and Medicaid Services website: http: //www. cms. gov/transmittals/downloads/R 327 P 1. pdf Farber, J. , Siu, A. , & Bloom, P. (2007). How much time do physicians spend providing care outside of office visits? Annuals of Internal Medicine, 147(10), 693 -698. Retrieved from http: //www. cinahl. com/cgi -bin/refsvc. html/ Ireson, C. L. , Slavova, S. , Steltenkamp, C. L. , & Scutchfield, F. D. (2009). Bridging the care continuum: Patient information needs for specialist referrals. BMC Health Services Research, 9, 163 -179. doi: 10. 1186/1472 -6963 -9 -163 Kim, Y. , Chen, A. H. , Keith, E. , Yee, H. F. , & Kushel, M. B. (2009). Not perfect, but better: Primary care providers' experiences with electronic referrals in a safety net health system. Journal of General Internal Medicine, 24(5), 614 -619. doi: 10. 1007/s 11606 -009 -0955 -3
 References Maher, M. (2009, November). Work-out facilitation skills. Lecture presented at Mercy Medical Center. Modak, I. , Sexton, J. B. , Lux, T. R. , Helmreick, R. L. , & Thomas, E. J. (2007). Measuring safety culture in the ambulatory setting: The safety attitudes questionnaire--ambulatory version. Journal of General Internal Medicine, 22(1), 1 -5. doi: 10. 1007/s 11606 -007 -0114 -7 Tucci, R. (n. d. ). Building a better tool set for accelerating change. Retrieved January 4, 2010, from http: //www. isixsigma. com/library/content/c 021104 a. asp. Weiner, M. , Perkins, A. J. , & Callahan, C. M. (2008). Errors in completion of referrals among older urban adults in ambulatory care. Journal of Evaluation in Clinical Practice, 16, 76 -81. doi: 10. 1111/j. 13652753. 2008. 01117. x Weiner, M. , Hoyek, G. , Wang, L. , Dexter, P. R. , Zerr, A. D. , Perkins, A. J. , James, F. , & Juneja, R. (2009). A web -based generalist-specialist system to improve scheduling of outpatient specialty consultations in an academic
References Maher, M. (2009, November). Work-out facilitation skills. Lecture presented at Mercy Medical Center. Modak, I. , Sexton, J. B. , Lux, T. R. , Helmreick, R. L. , & Thomas, E. J. (2007). Measuring safety culture in the ambulatory setting: The safety attitudes questionnaire--ambulatory version. Journal of General Internal Medicine, 22(1), 1 -5. doi: 10. 1007/s 11606 -007 -0114 -7 Tucci, R. (n. d. ). Building a better tool set for accelerating change. Retrieved January 4, 2010, from http: //www. isixsigma. com/library/content/c 021104 a. asp. Weiner, M. , Perkins, A. J. , & Callahan, C. M. (2008). Errors in completion of referrals among older urban adults in ambulatory care. Journal of Evaluation in Clinical Practice, 16, 76 -81. doi: 10. 1111/j. 13652753. 2008. 01117. x Weiner, M. , Hoyek, G. , Wang, L. , Dexter, P. R. , Zerr, A. D. , Perkins, A. J. , James, F. , & Juneja, R. (2009). A web -based generalist-specialist system to improve scheduling of outpatient specialty consultations in an academic


