121292aedc828e8069093769b6aae32c.ppt
- Количество слайдов: 78
Impressions of Bangladesh
Further impressions / realities
Malnutrition
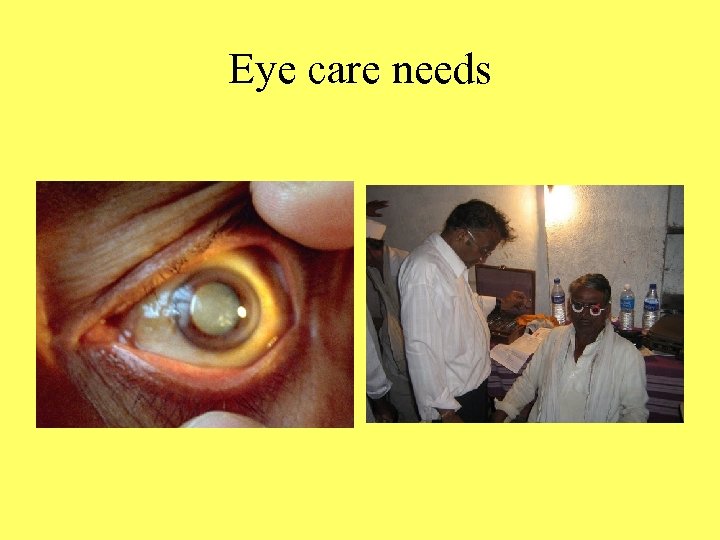
Eye care needs
Tackling blindness in Bangladesh
Vision for Blindness
National Blindness and Low Vision Survey of Bangladesh
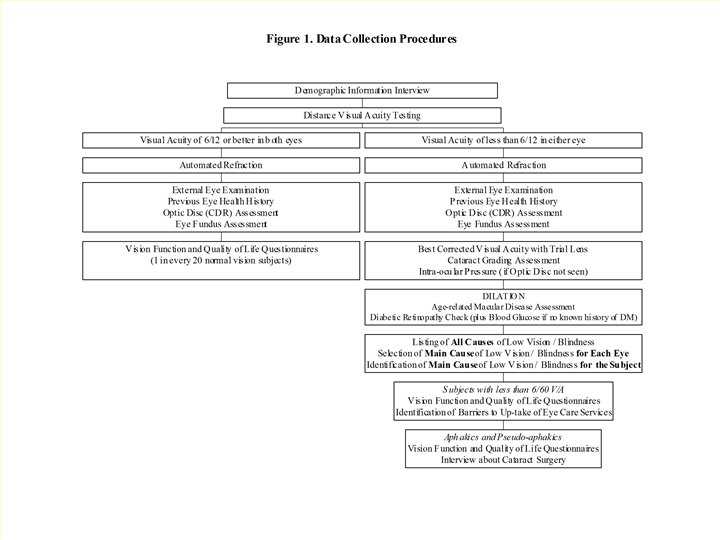
Project Aim To determine the national prevalence and causes of blindness and low vision amongst persons aged 30 years and older in Bangladesh, based on a nationally representative sample.
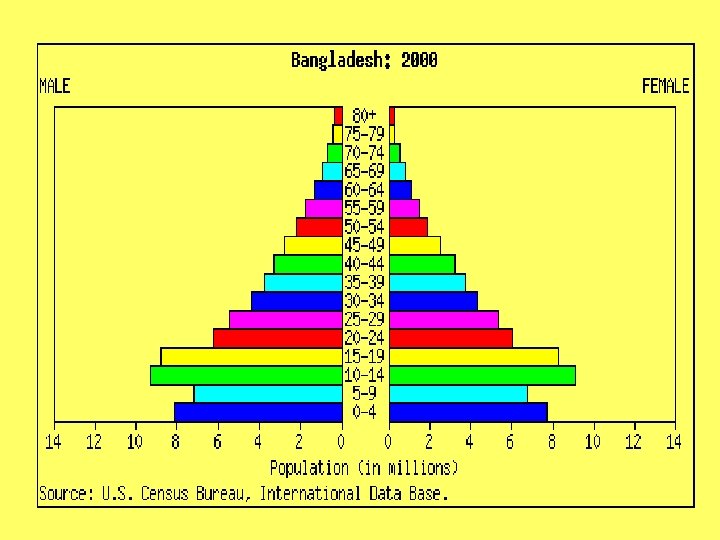
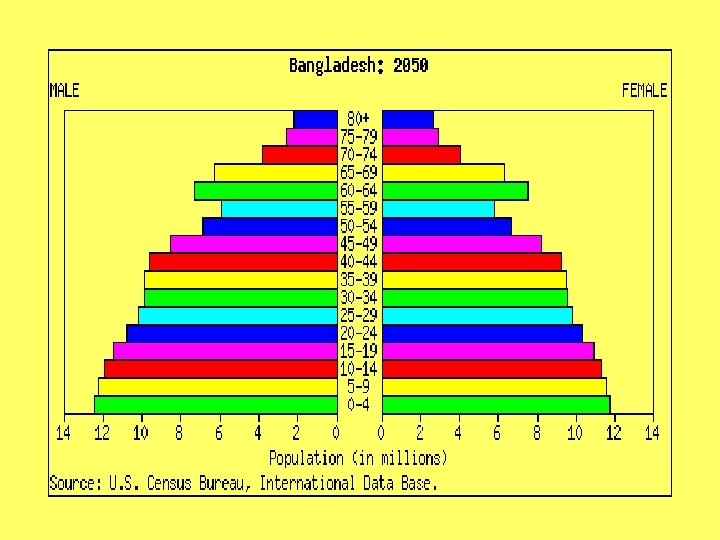
Demographic Information • Population (2000) – 130 million • Adults 30 and older - 44 million (33. 6%) • Six administrative divisions • 64 districts (zilas) / 490 thanas / 4491 unions • 59, 900 villages (mauzas) and urban wards (603)
Rural villages
Urban slums
Urban slum areas
Coastal areas
Chittagong Hill Tracts
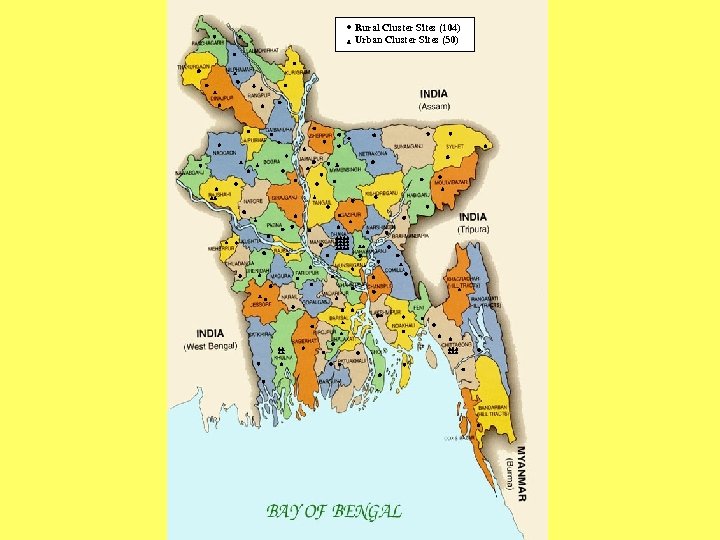
Rural Cluster Sites (104) Urban Cluster Sites (50)
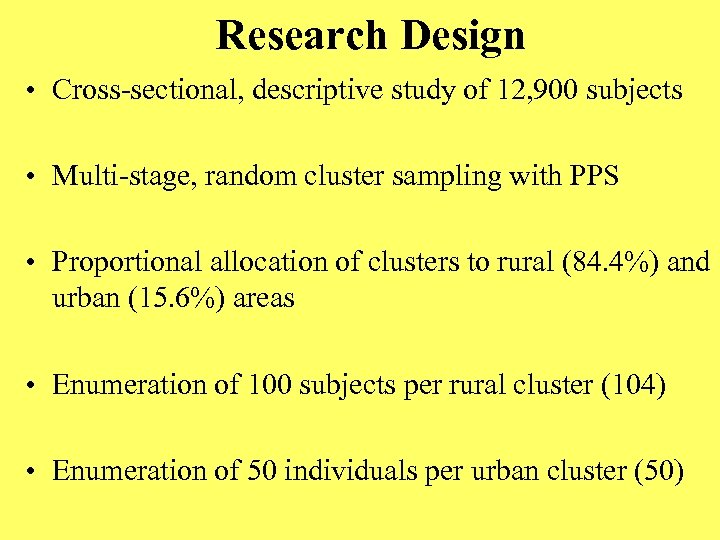
Research Design • Cross-sectional, descriptive study of 12, 900 subjects • Multi-stage, random cluster sampling with PPS • Proportional allocation of clusters to rural (84. 4%) and urban (15. 6%) areas • Enumeration of 100 subjects per rural cluster (104) • Enumeration of 50 individuals per urban cluster (50)
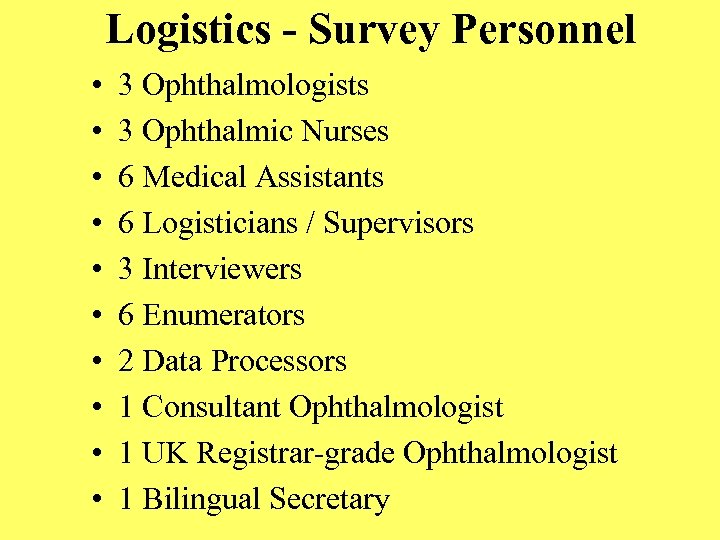
Logistics - Survey Personnel • • • 3 Ophthalmologists 3 Ophthalmic Nurses 6 Medical Assistants 6 Logisticians / Supervisors 3 Interviewers 6 Enumerators 2 Data Processors 1 Consultant Ophthalmologist 1 UK Registrar-grade Ophthalmologist 1 Bilingual Secretary
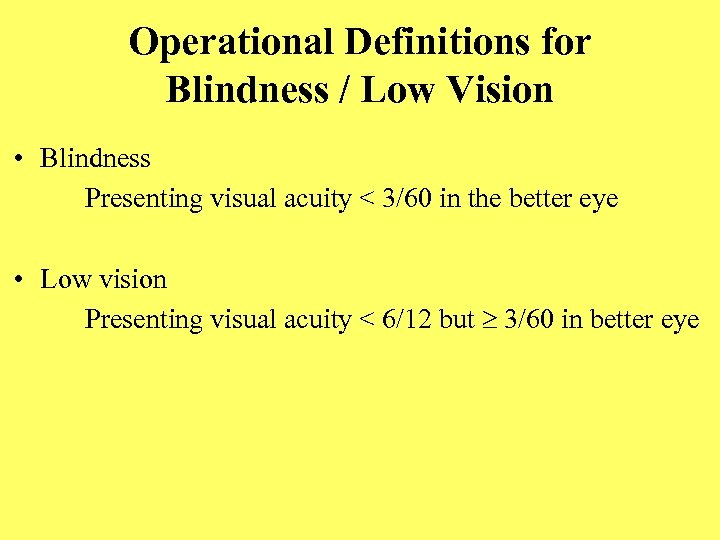
Operational Definitions for Blindness / Low Vision • Blindness Presenting visual acuity < 3/60 in the better eye • Low vision Presenting visual acuity < 6/12 but 3/60 in better eye
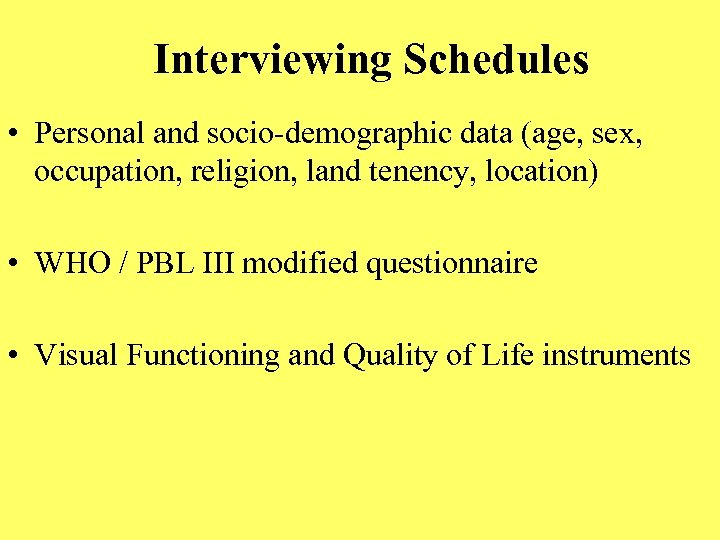
Interviewing Schedules • Personal and socio-demographic data (age, sex, occupation, religion, land tenency, location) • WHO / PBL III modified questionnaire • Visual Functioning and Quality of Life instruments
Prevalence survey “It is simple but it will not be easy. ” Professor Syed Modasser Ali Dhaka, Bangladesh
Urban settings

Results 11, 624 subjects examined 90. 9% response rate Response rate equally high in rural and urban areas

Visual acuity in the ‘better eye’ (Presenting and Corrected)
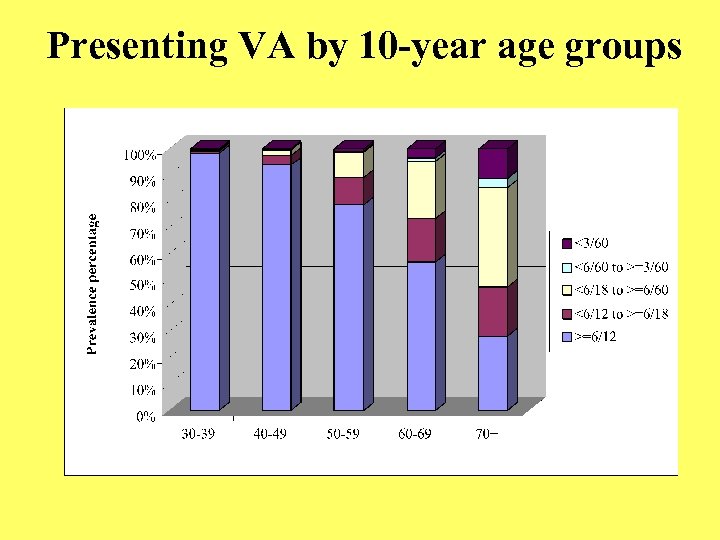
Presenting VA by 10 -year age groups
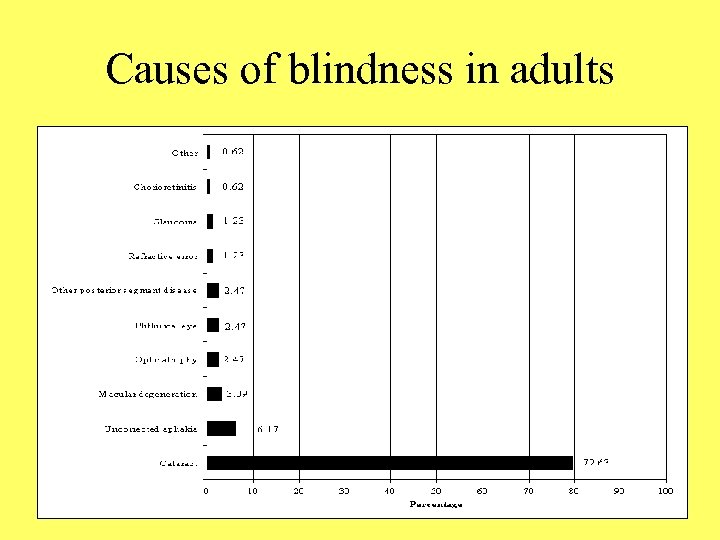
Causes of blindness in adults
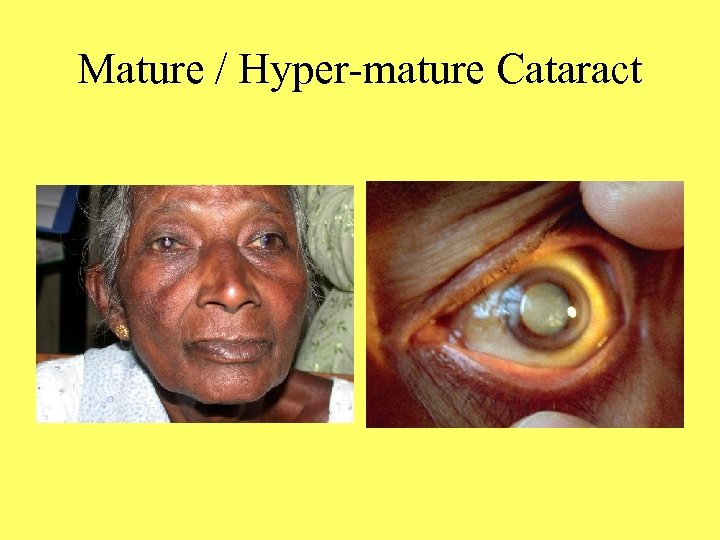
Mature / Hyper-mature Cataract
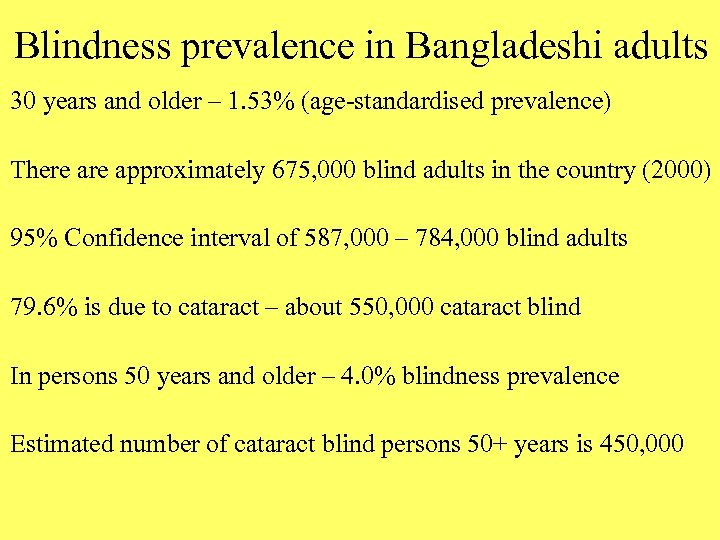
Blindness prevalence in Bangladeshi adults 30 years and older – 1. 53% (age-standardised prevalence) There approximately 675, 000 blind adults in the country (2000) 95% Confidence interval of 587, 000 – 784, 000 blind adults 79. 6% is due to cataract – about 550, 000 cataract blind In persons 50 years and older – 4. 0% blindness prevalence Estimated number of cataract blind persons 50+ years is 450, 000
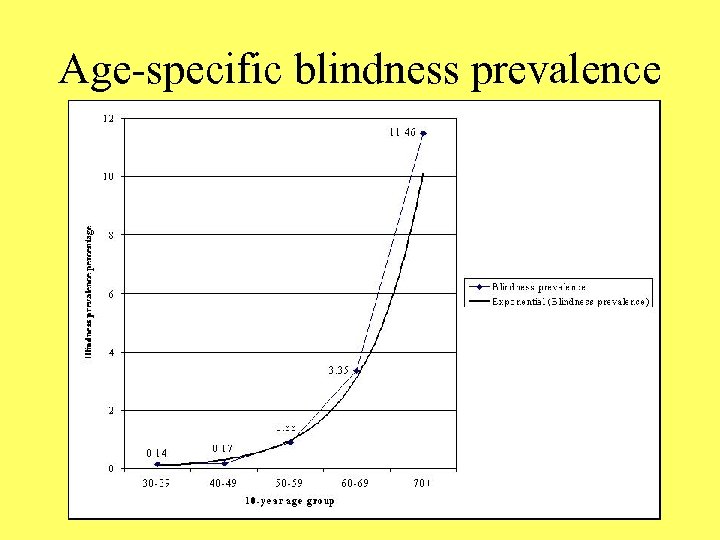
Age-specific blindness prevalence
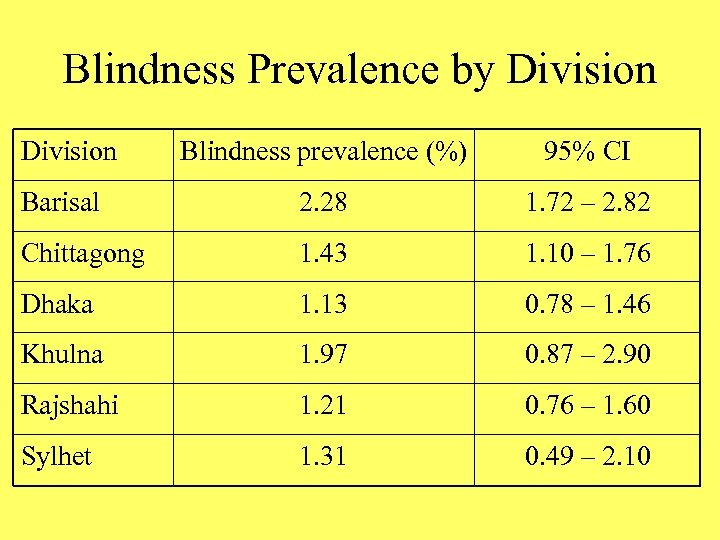
Blindness Prevalence by Division Blindness prevalence (%) 95% CI Barisal 2. 28 1. 72 – 2. 82 Chittagong 1. 43 1. 10 – 1. 76 Dhaka 1. 13 0. 78 – 1. 46 Khulna 1. 97 0. 87 – 2. 90 Rajshahi 1. 21 0. 76 – 1. 60 Sylhet 1. 31 0. 49 – 2. 10
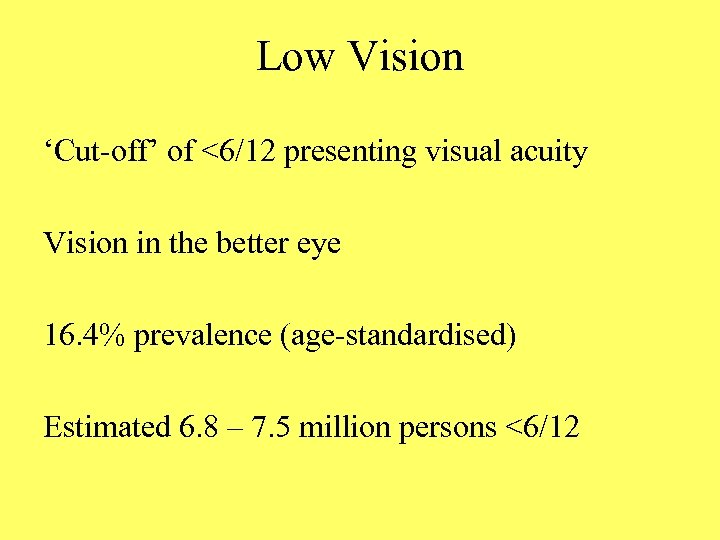
Low Vision ‘Cut-off’ of <6/12 presenting visual acuity Vision in the better eye 16. 4% prevalence (age-standardised) Estimated 6. 8 – 7. 5 million persons <6/12
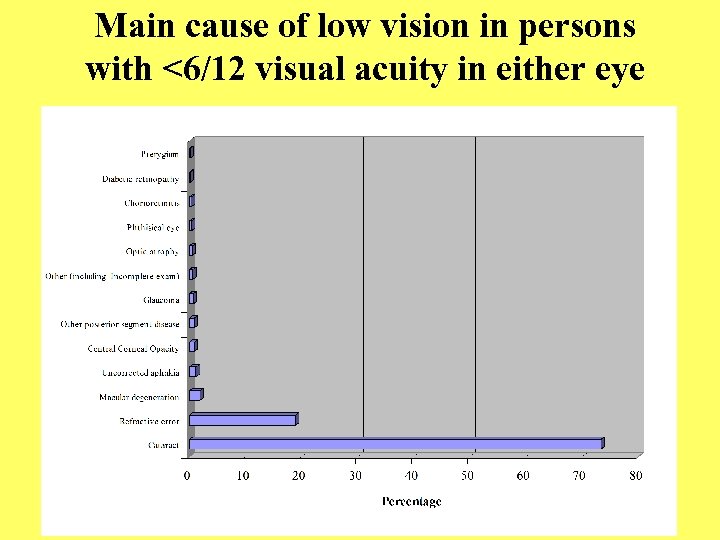
Main cause of low vision in persons with <6/12 visual acuity in either eye
Refractive Errors in Adults Second leading cause of visual impairment (18. 87%) Spectacle use is low (3. 0%) Refractive correction shown to be beneficial in survey

Risk factors for blindness / low vision • Increased age, particularly after 60 years of age • Female gender (95% CI 1. 18 - 2. 29) • Rural resident (95% CI OR 1. 34 - 1. 79) • Illiteracy (95% CI OR 5. 86 - 9. 20) • Manual labour in men (95% CI OR 1. 11 - 9. 35)
Need for Low Vision Services in Adults WHO definition VA <6/18 - PL after surgical treatment +/or refraction Prevalence of 0. 56% - estimated 250, 000 cases in country Causes: Retinal diseases (38. 4%) Corneal diseases (21. 5%) Glaucoma (15. 4%) Optic atrophy (10. 8%)
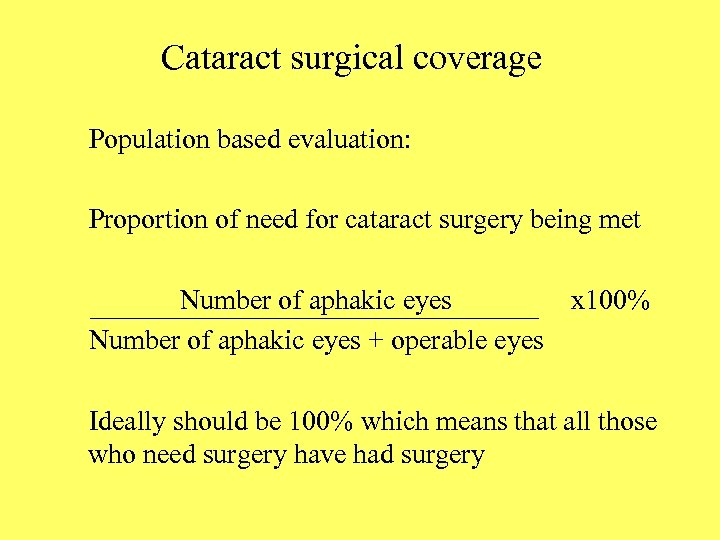
Cataract surgical coverage Population based evaluation: Proportion of need for cataract surgery being met Number of aphakic eyes x 100% Number of aphakic eyes + operable eyes Ideally should be 100% which means that all those who need surgery have had surgery
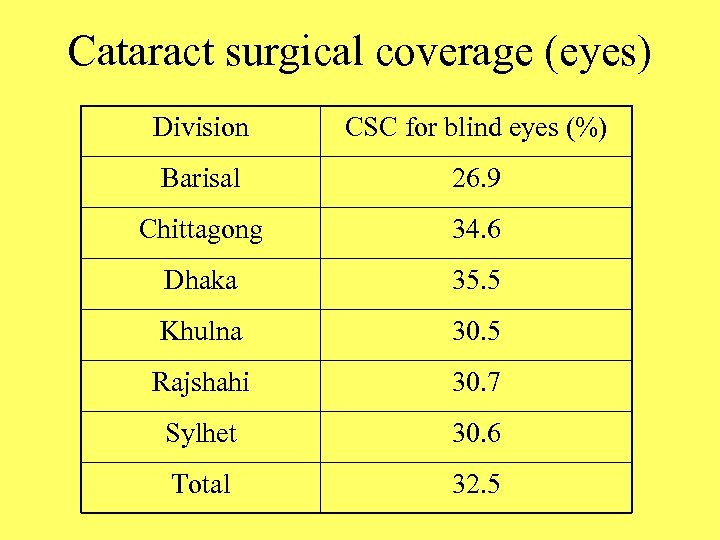
Cataract surgical coverage (eyes) Division CSC for blind eyes (%) Barisal 26. 9 Chittagong 34. 6 Dhaka 35. 5 Khulna 30. 5 Rajshahi 30. 7 Sylhet 30. 6 Total 32. 5
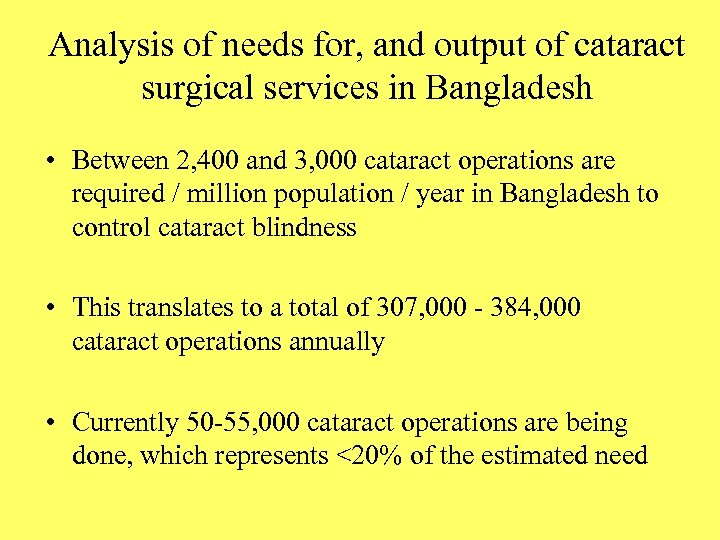
Analysis of needs for, and output of cataract surgical services in Bangladesh • Between 2, 400 and 3, 000 cataract operations are required / million population / year in Bangladesh to control cataract blindness • This translates to a total of 307, 000 - 384, 000 cataract operations annually • Currently 50 -55, 000 cataract operations are being done, which represents <20% of the estimated need
Persons having had cataract surgery
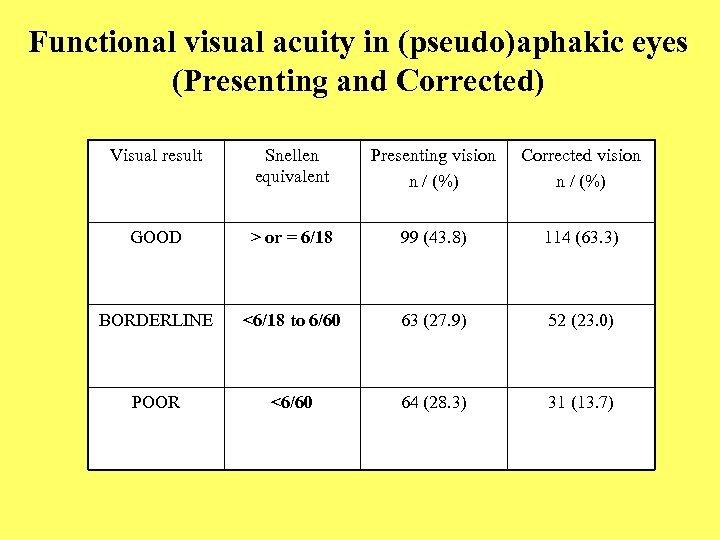
Functional visual acuity in (pseudo)aphakic eyes (Presenting and Corrected) Visual result Snellen equivalent Presenting vision n / (%) Corrected vision n / (%) GOOD > or = 6/18 99 (43. 8) 114 (63. 3) BORDERLINE <6/18 to 6/60 63 (27. 9) 52 (23. 0) POOR <6/60 64 (28. 3) 31 (13. 7)
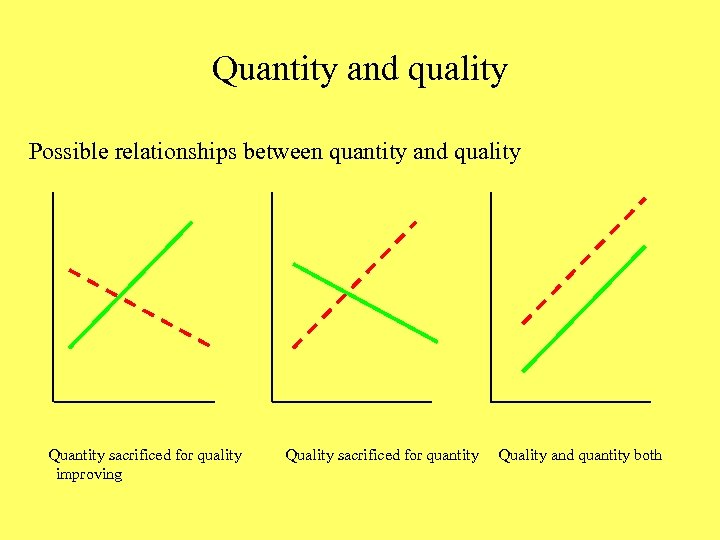
Quantity and quality Possible relationships between quantity and quality Quantity sacrificed for quality improving Quality sacrificed for quantity Quality and quantity both
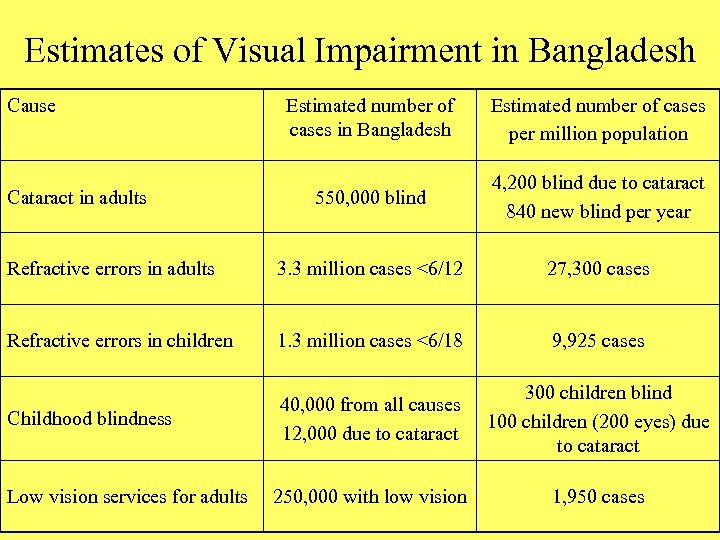
Estimates of Visual Impairment in Bangladesh Cause Estimated number of cases in Bangladesh Estimated number of cases per million population 550, 000 blind 4, 200 blind due to cataract 840 new blind per year Refractive errors in adults 3. 3 million cases <6/12 27, 300 cases Refractive errors in children 1. 3 million cases <6/18 9, 925 cases Childhood blindness 40, 000 from all causes 12, 000 due to cataract 300 children blind 100 children (200 eyes) due to cataract 250, 000 with low vision 1, 950 cases Cataract in adults Low vision services for adults
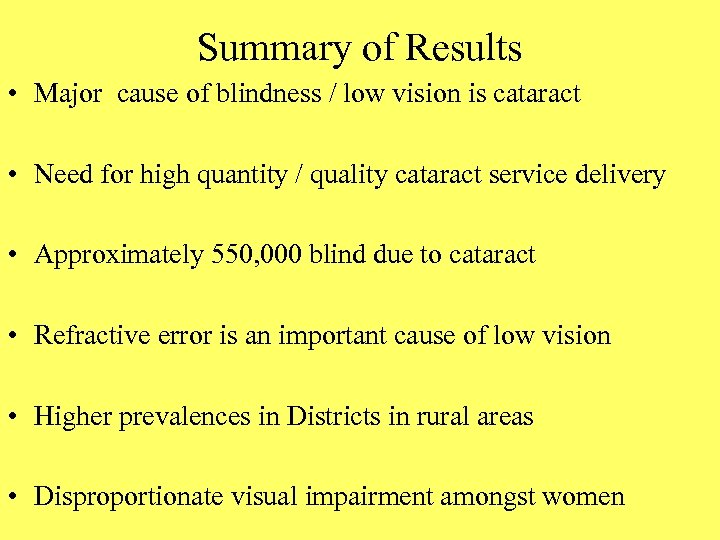
Summary of Results • Major cause of blindness / low vision is cataract • Need for high quantity / quality cataract service delivery • Approximately 550, 000 blind due to cataract • Refractive error is an important cause of low vision • Higher prevalences in Districts in rural areas • Disproportionate visual impairment amongst women
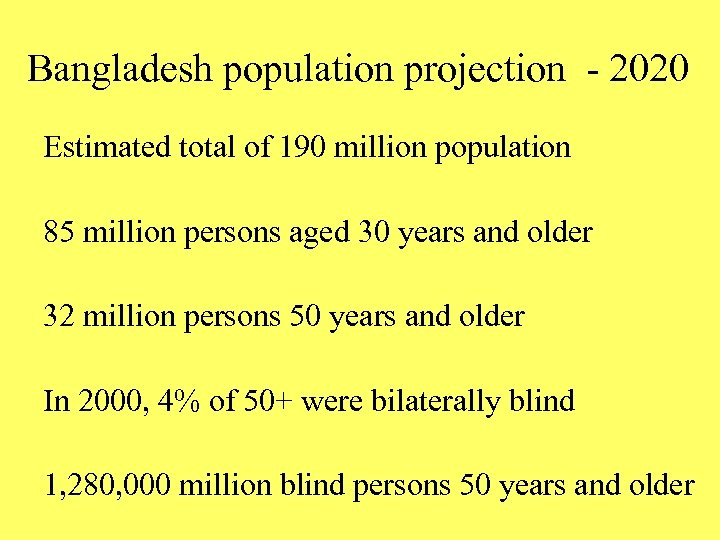
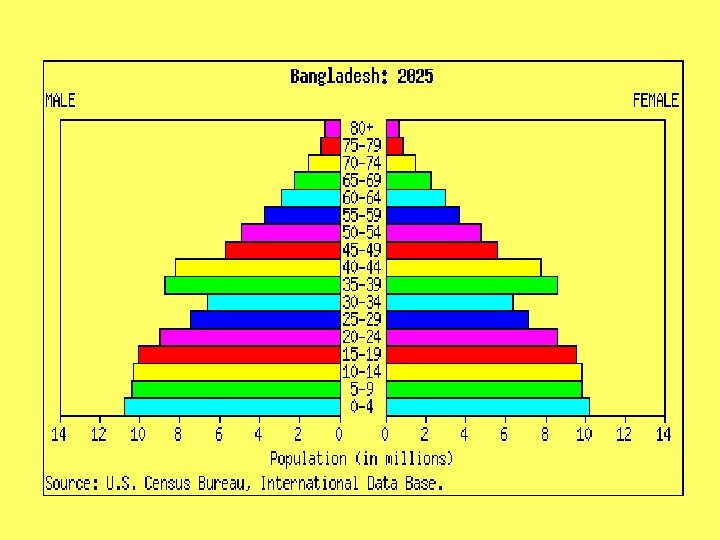
Bangladesh population projection - 2020 Estimated total of 190 million population 85 million persons aged 30 years and older 32 million persons 50 years and older In 2000, 4% of 50+ were bilaterally blind 1, 280, 000 million blind persons 50 years and older
Barriers to up-take of cataract surgery
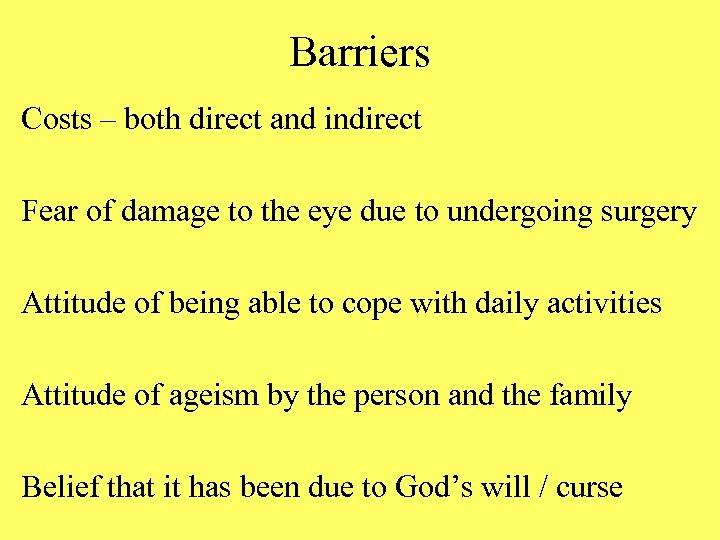
Barriers Costs – both direct and indirect Fear of damage to the eye due to undergoing surgery Attitude of being able to cope with daily activities Attitude of ageism by the person and the family Belief that it has been due to God’s will / curse
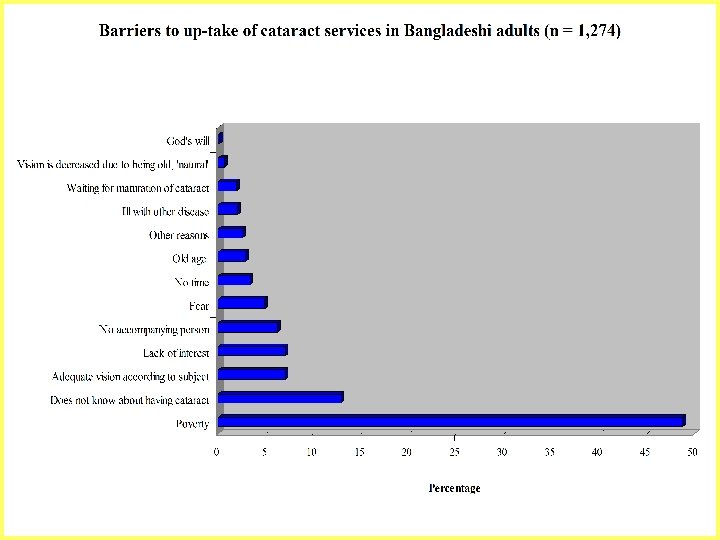
Complex socio-cultural (mis)understandings Beliefs and attitudes regarding blindness, ageing Perceptions as to: actual cost of surgery or purchase of spectacles value of undergoing cataract surgery relative ‘utility cost’ of treatment Lack of awareness about cataract as an eye condition Why? What? Whether? (Mis)understanding concerning ‘treatment seeking behaviour’ Who? Where? When? How often? How much?
Questions as to overcoming the barriers How can surgery be made affordable for all in need? What are the possible payment options to consider? How can one raise awareness about cataract? How can equity of delivery be assured? (targeting? ) How to / Whether to prioritise sight restoring surgery?
Ottawa Charter on Health Promotion Healthy public policy Personal skills development Community participation Healthy environments Re-organisation of health service delivery Equity Advocacy Social support
Role of health education in eye care What is the content of eye health education? Who is responsible for delivering the information? Have these persons been trained specifically for this task? To whom is the eye health education targeted? Is this part of PHC or as a separate activity, i. e. PEC only? Is this a ‘once-off’ information session or is it continuous?
Personnel required to reduce barriers Community participation Locally-based, health workers trained in eye care Local leaders, key informants, liaison persons, volunteers Community ophthalmologists / Public health personnel Ophthalmologists – organisation of hospital / out-reach care Eye care programme administrators and policy makers
‘Provider’ barriers Lack of prioritisation of eye care in health care Reproductive health Cyclone preparedness / disaster relief Arsenic poisoning of water supply Food security Lack of perceived importance (e. g. economically) Lack of resources (personnel, costs, equipment)

Eye Care Service Delivery
Eye care service provision Acceptable Accessible Affordable Appropriate
Resource availability ‘Manpower’ (all levels of human resources / personnel) Materials (theatres ‘eye beds’, surgical equipment, transport) Management (structures and information systems) Money (capital and running costs)
Money Sources of funding * Government funding * International non-government development organisations * Patient fees * Cost-recovery schemes * Charitable activities Cost recovery schemes – Do these exist? Do they work?
Examples of Good Practice S Choudhary Eye Hospital in Lahan, Nepal Aravind Eye Hospital in Madurai, India BNSB Hospital in Sirajganj District, Bangladesh
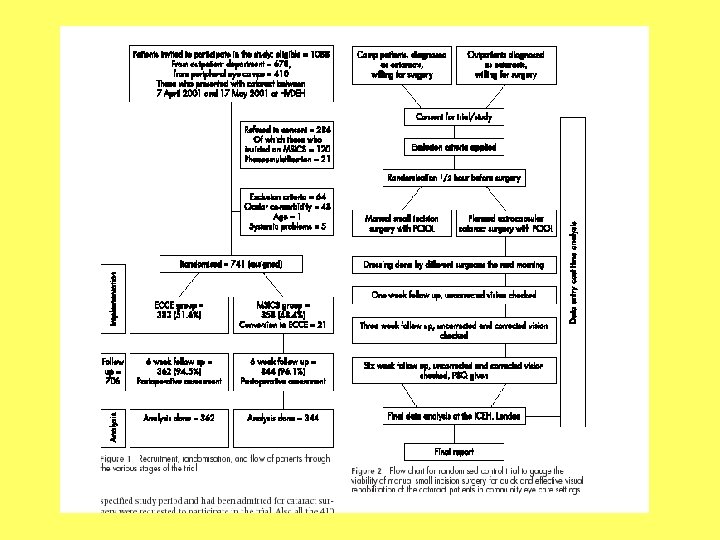
Community Eye Research Extracapsular cataract surgery compared with manual small incision cataract surgery in community eye care setting in western India: a randomised controlled trial P M Gogate, M Deshpande, R P Wormald, R Deshpande, S R Kulkarni BJO 2003
Increasing the quantity of cataract operations Two different situations: High output: increase efficiency overcome barriers Low output: overcome barriers
High output situations Improve resource utilisation: • day case surgery • reduce in-patient stay to increase bed occupancy • increase number of operating days • increase number of tables in operating theatre to increase number of cases / operating list • use of mid-level workers in OPD and theatre • ‘one stop’ assessment clinics with programmed date for surgery
‘Aravind model’ Local organisations arrange venue, advertise and mobilise patients, pay for venue, and transport to-and-from base Team from the hospital examines and treats patients Patients needing surgery are identified and transported to the base hospital for surgery After a short in-patient stay the persons are transported back Advantages: Disadvantages: High volume, high quality surgery Follow-up services not guaranteed

Aravind model
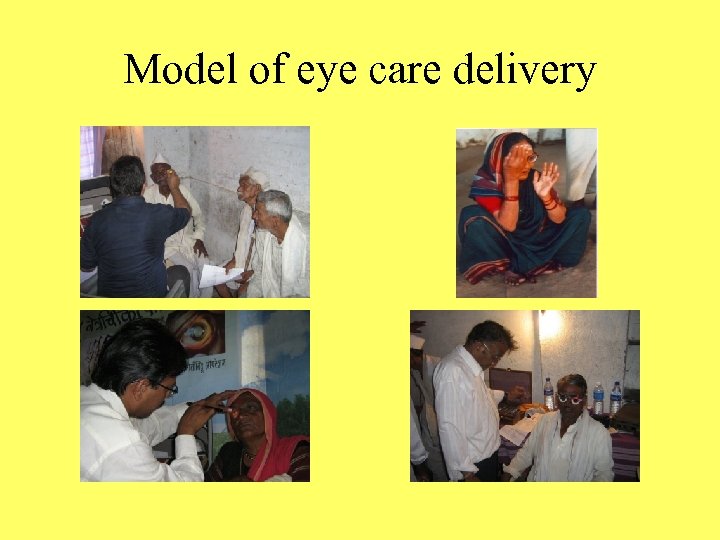
Model of eye care delivery
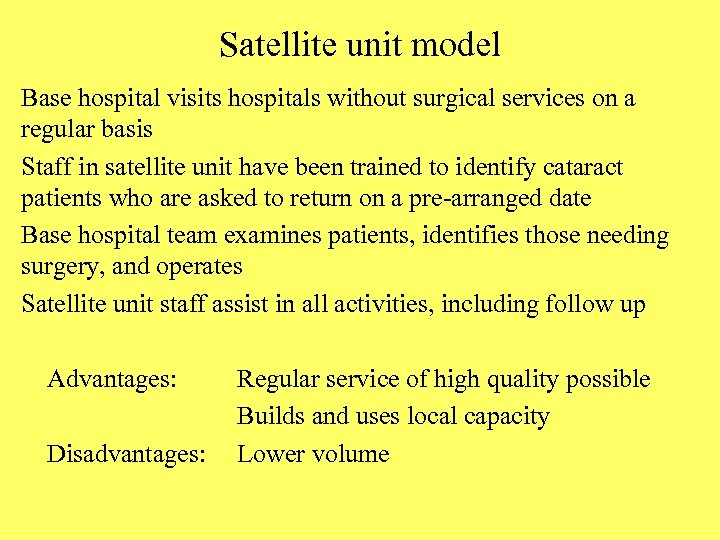
Satellite unit model Base hospital visits hospitals without surgical services on a regular basis Staff in satellite unit have been trained to identify cataract patients who are asked to return on a pre-arranged date Base hospital team examines patients, identifies those needing surgery, and operates Satellite unit staff assist in all activities, including follow up Advantages: Disadvantages: Regular service of high quality possible Builds and uses local capacity Lower volume
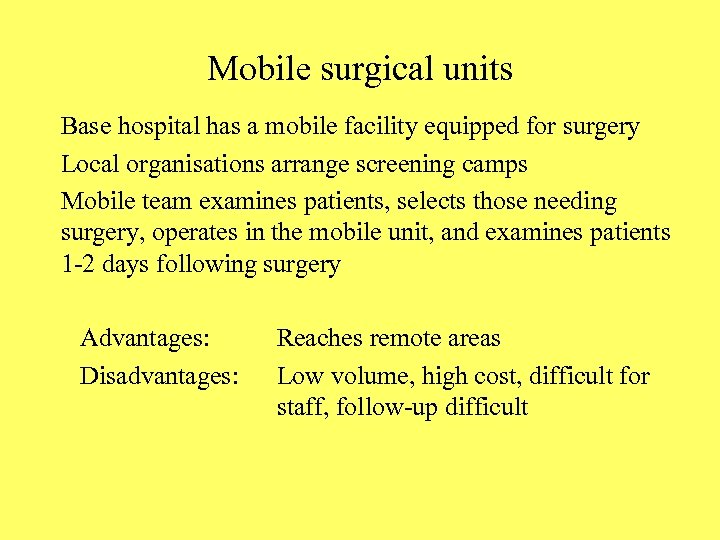
Mobile surgical units Base hospital has a mobile facility equipped for surgery Local organisations arrange screening camps Mobile team examines patients, selects those needing surgery, operates in the mobile unit, and examines patients 1 -2 days following surgery Advantages: Disadvantages: Reaches remote areas Low volume, high cost, difficult for staff, follow-up difficult
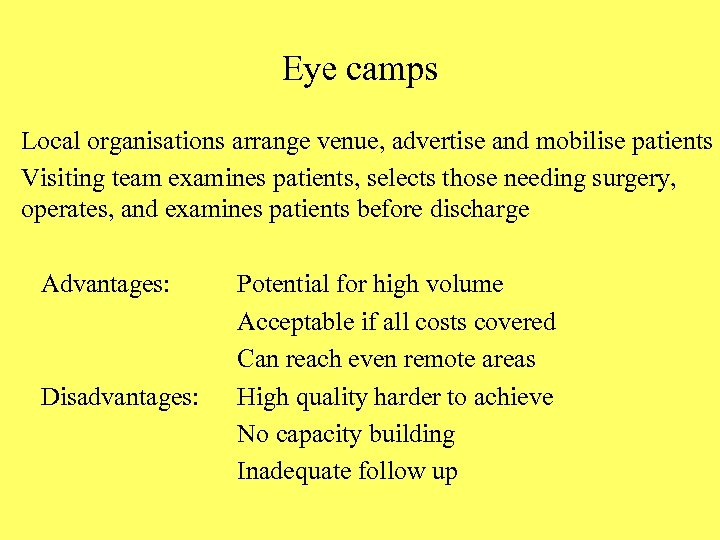
Eye camps Local organisations arrange venue, advertise and mobilise patients Visiting team examines patients, selects those needing surgery, operates, and examines patients before discharge Advantages: Disadvantages: Potential for high volume Acceptable if all costs covered Can reach even remote areas High quality harder to achieve No capacity building Inadequate follow up
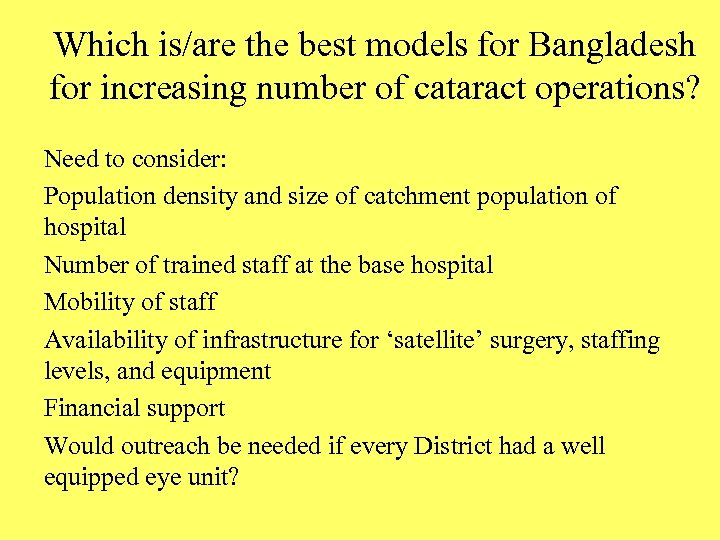
Which is/are the best models for Bangladesh for increasing number of cataract operations? Need to consider: Population density and size of catchment population of hospital Number of trained staff at the base hospital Mobility of staff Availability of infrastructure for ‘satellite’ surgery, staffing levels, and equipment Financial support Would outreach be needed if every District had a well equipped eye unit?
Clouds come floating into my life, no longer to carry rain or usher storm, but to add color to my sunset sky. Rabindranath Tagore
121292aedc828e8069093769b6aae32c.ppt