9ad3b64e0d34f744957b79d2bf9beaeb.ppt
- Количество слайдов: 33
 Implementing Toyota Lean Principles in a Family Medicine Residency David Mistretta, MA Jeffrey Mathieu, MD Lehigh Valley Hospital Family Medicine Residency Allentown, PA
Implementing Toyota Lean Principles in a Family Medicine Residency David Mistretta, MA Jeffrey Mathieu, MD Lehigh Valley Hospital Family Medicine Residency Allentown, PA
 Quick Intro to Toyota Refers to the Toyota Production System (yes, that Toyota!) • Has its origin in post-World War II Japan • Toyota Group re-started operations under severe materiel shortages • Two major concepts credited by Taiichi Ohno (father of the Toyota Production System): Henry Ford’s idea of a true production system; Edward Deming’s use of Statistical Processes
Quick Intro to Toyota Refers to the Toyota Production System (yes, that Toyota!) • Has its origin in post-World War II Japan • Toyota Group re-started operations under severe materiel shortages • Two major concepts credited by Taiichi Ohno (father of the Toyota Production System): Henry Ford’s idea of a true production system; Edward Deming’s use of Statistical Processes
 What Does “Lean” Mean? Describes a philosophy that incorporates tools and techniques that: • Optimize time • Optimize human resources • Optimize assets • Increase productivity • Improve quality and service
What Does “Lean” Mean? Describes a philosophy that incorporates tools and techniques that: • Optimize time • Optimize human resources • Optimize assets • Increase productivity • Improve quality and service
 Will I Be Motivated to Buy a New Car After This? • • Getting “it” right the first time (it = quality) Eliminating waste Satisfying customers (internal and external) Fostering an atmosphere of continuous improvement and learning (Kaizen events) Grooming leaders from within Teaching all employees to be problem solvers Long term commitment
Will I Be Motivated to Buy a New Car After This? • • Getting “it” right the first time (it = quality) Eliminating waste Satisfying customers (internal and external) Fostering an atmosphere of continuous improvement and learning (Kaizen events) Grooming leaders from within Teaching all employees to be problem solvers Long term commitment
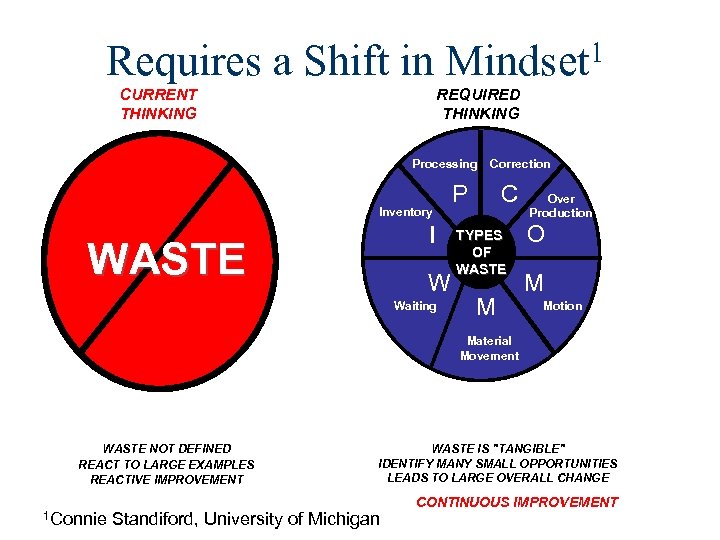 Requires a Shift in Mindset 1 CURRENT THINKING REQUIRED THINKING Processing Inventory I WASTE W Waiting Correction P C TYPES OF WASTE M Over Production O M Motion Material Movement WASTE NOT DEFINED REACT TO LARGE EXAMPLES REACTIVE IMPROVEMENT 1 Connie WASTE IS "TANGIBLE" IDENTIFY MANY SMALL OPPORTUNITIES LEADS TO LARGE OVERALL CHANGE Standiford, University of Michigan CONTINUOUS IMPROVEMENT
Requires a Shift in Mindset 1 CURRENT THINKING REQUIRED THINKING Processing Inventory I WASTE W Waiting Correction P C TYPES OF WASTE M Over Production O M Motion Material Movement WASTE NOT DEFINED REACT TO LARGE EXAMPLES REACTIVE IMPROVEMENT 1 Connie WASTE IS "TANGIBLE" IDENTIFY MANY SMALL OPPORTUNITIES LEADS TO LARGE OVERALL CHANGE Standiford, University of Michigan CONTINUOUS IMPROVEMENT
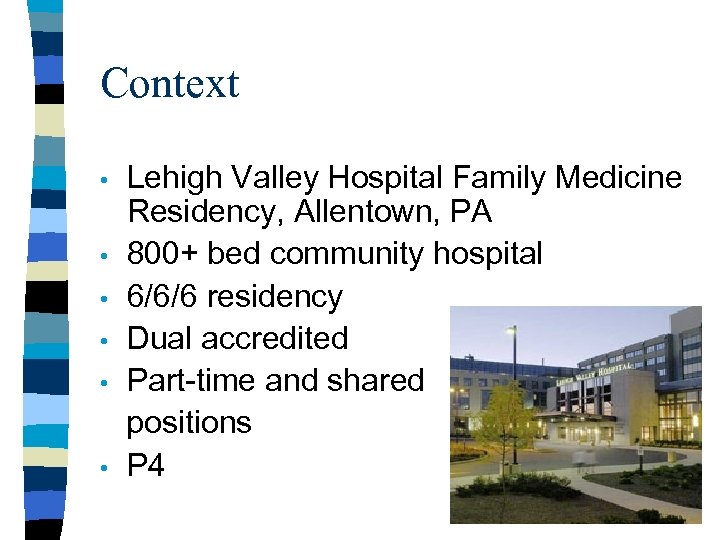 Context • • • Lehigh Valley Hospital Family Medicine Residency, Allentown, PA 800+ bed community hospital 6/6/6 residency Dual accredited Part-time and shared positions P 4
Context • • • Lehigh Valley Hospital Family Medicine Residency, Allentown, PA 800+ bed community hospital 6/6/6 residency Dual accredited Part-time and shared positions P 4
 P 4 • • • Outpatient focused PGY 1 year Community-Based Continuity Clinics No OB delivery requirement Learning Lab modules with didactic and clinical components Eliminate Time Based Competency
P 4 • • • Outpatient focused PGY 1 year Community-Based Continuity Clinics No OB delivery requirement Learning Lab modules with didactic and clinical components Eliminate Time Based Competency
 Vision By creating a home for a teaching and learning community of healing, the FHC prepares personal physicians to share the best relationship-centered care with patients and our community.
Vision By creating a home for a teaching and learning community of healing, the FHC prepares personal physicians to share the best relationship-centered care with patients and our community.
 Why Toyota works at LVHFC • • • Stewardship ULTRA FACT Metrics Dashboard Kaizen Events
Why Toyota works at LVHFC • • • Stewardship ULTRA FACT Metrics Dashboard Kaizen Events
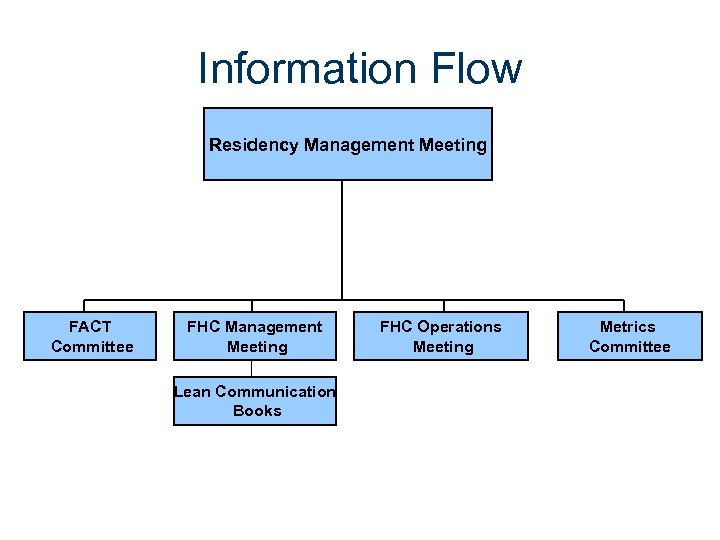 Information Flow Residency Management Meeting FACT Committee FHC Management Meeting Lean Communication Books FHC Operations Meeting Metrics Committee
Information Flow Residency Management Meeting FACT Committee FHC Management Meeting Lean Communication Books FHC Operations Meeting Metrics Committee
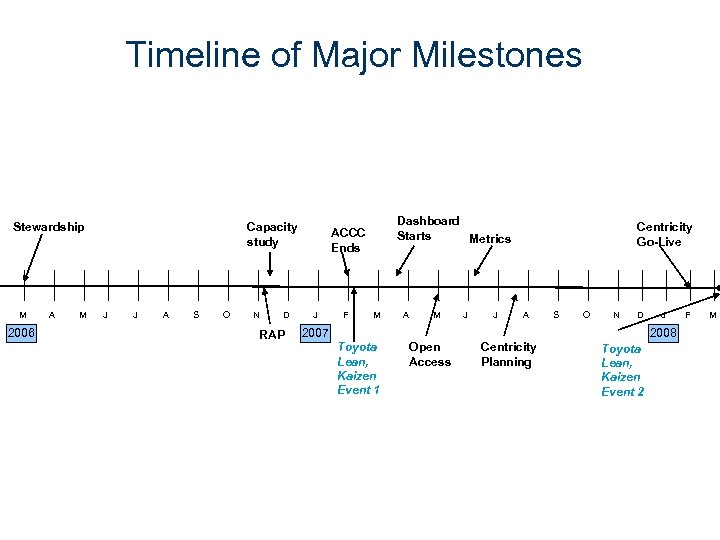 Timeline of Major Milestones Stewardship M 2006 A M Capacity study J J A S O N D RAP Dashboard Starts Metrics ACCC Ends J F M A M J J Centricity Go-Live A S O N D 2007 J 2008 Toyota Lean, Kaizen Event 1 Open Access Centricity Planning Toyota Lean, Kaizen Event 2 F M
Timeline of Major Milestones Stewardship M 2006 A M Capacity study J J A S O N D RAP Dashboard Starts Metrics ACCC Ends J F M A M J J Centricity Go-Live A S O N D 2007 J 2008 Toyota Lean, Kaizen Event 1 Open Access Centricity Planning Toyota Lean, Kaizen Event 2 F M
 Residency curriculum Health systems, administration and leadership portfolio Portfolio Goal #4: Graduates will demonstrate the process skills necessary for successful practice change and innovation.
Residency curriculum Health systems, administration and leadership portfolio Portfolio Goal #4: Graduates will demonstrate the process skills necessary for successful practice change and innovation.
 Objective #4 Each resident will demonstrate skill and knowledge in the area of change and innovation through the following: • Successfully facilitating four meetings • Successfully facilitating two groups • Successful active participation in two process improvement activities • Completion of a project management protocol • Appropriate selection of conversation strategies in Practice Design Project
Objective #4 Each resident will demonstrate skill and knowledge in the area of change and innovation through the following: • Successfully facilitating four meetings • Successfully facilitating two groups • Successful active participation in two process improvement activities • Completion of a project management protocol • Appropriate selection of conversation strategies in Practice Design Project
 Possible course content • Opportunities to learn PI processes • • • Participation in Kaizen events CCT quality efforts Sitting on FACT OPS Special task forces Residents as stakeholders in practice
Possible course content • Opportunities to learn PI processes • • • Participation in Kaizen events CCT quality efforts Sitting on FACT OPS Special task forces Residents as stakeholders in practice
 Kaizen 1 – Office flow • 3 day event • Learning principles for Toyota • Office flow • No pilots during event
Kaizen 1 – Office flow • 3 day event • Learning principles for Toyota • Office flow • No pilots during event
 Findings • Six separate process that impede smooth patient flow • • Check-In Phone System Time In Exam Room / Leaving Exam Room Vital Signs Check-Out Other miscellaneous items
Findings • Six separate process that impede smooth patient flow • • Check-In Phone System Time In Exam Room / Leaving Exam Room Vital Signs Check-Out Other miscellaneous items
 Example deliverables Time In Exam Room / Leaving Exam Room • Goal: Information will be available in the exam room (2/12 – 4/1). • Prioritize, organize, and standardize commonly used forms in all exam rooms • Install printers in all exam rooms • Install a flag system / white boards outside exam rooms so that all staff visually know the status of each exam room – provide training for staff • Goal: Clinical teams will be explored to improve communication. (2/12) • Develop and pilot clinical teams
Example deliverables Time In Exam Room / Leaving Exam Room • Goal: Information will be available in the exam room (2/12 – 4/1). • Prioritize, organize, and standardize commonly used forms in all exam rooms • Install printers in all exam rooms • Install a flag system / white boards outside exam rooms so that all staff visually know the status of each exam room – provide training for staff • Goal: Clinical teams will be explored to improve communication. (2/12) • Develop and pilot clinical teams
 Results of Kaizen 1 • • Thirty deliverables Time study as metric • Included visual cues, 5 S(Sort, Simplify, Sweep, Standardize, Self-Discipline) • • Maintained on Dashboard 30, 60, 90 and semi annually check in on status of deliverables
Results of Kaizen 1 • • Thirty deliverables Time study as metric • Included visual cues, 5 S(Sort, Simplify, Sweep, Standardize, Self-Discipline) • • Maintained on Dashboard 30, 60, 90 and semi annually check in on status of deliverables
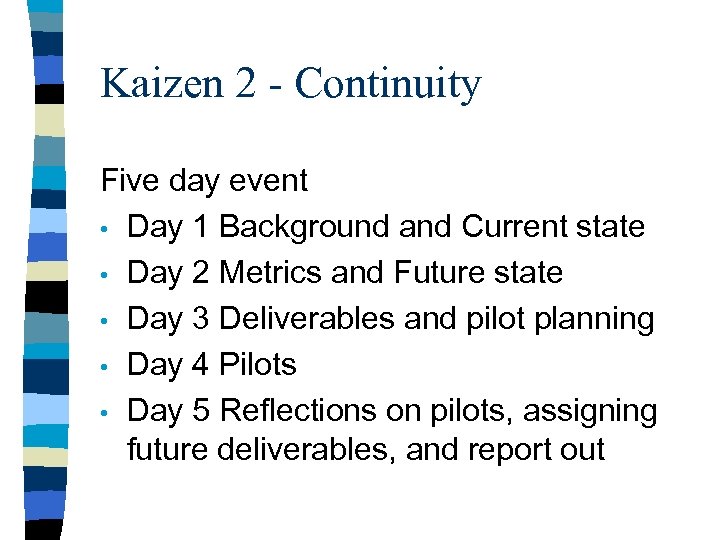 Kaizen 2 - Continuity Five day event • Day 1 Background and Current state • Day 2 Metrics and Future state • Day 3 Deliverables and pilot planning • Day 4 Pilots • Day 5 Reflections on pilots, assigning future deliverables, and report out
Kaizen 2 - Continuity Five day event • Day 1 Background and Current state • Day 2 Metrics and Future state • Day 3 Deliverables and pilot planning • Day 4 Pilots • Day 5 Reflections on pilots, assigning future deliverables, and report out
 Continuity Definition Recognizing the different choices and needs of patients with simple and complex health issues, continuity of care is the degree to which each interaction in the healthcare system over a period of time occurs as a result of the ongoing responsibility of the same care team.
Continuity Definition Recognizing the different choices and needs of patients with simple and complex health issues, continuity of care is the degree to which each interaction in the healthcare system over a period of time occurs as a result of the ongoing responsibility of the same care team.
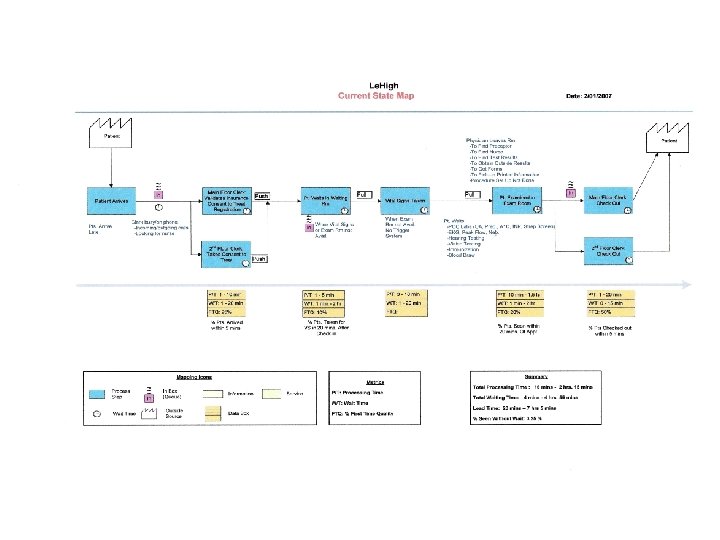
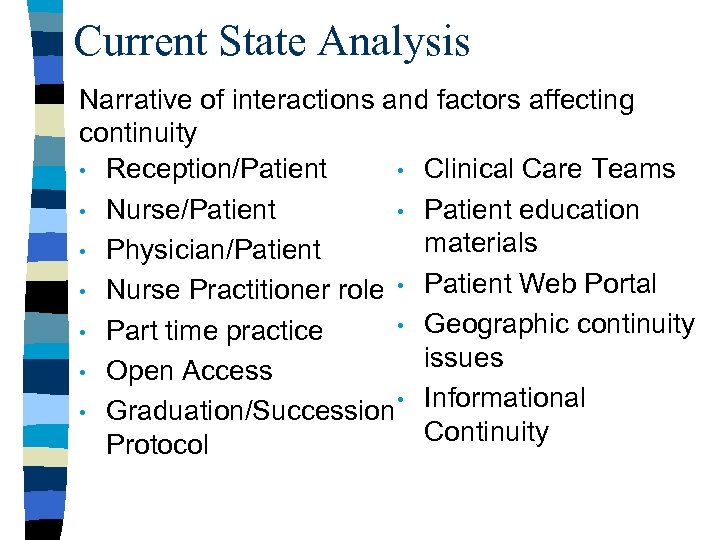 Current State Analysis Narrative of interactions and factors affecting continuity • Reception/Patient • Clinical Care Teams • Nurse/Patient • Patient education materials • Physician/Patient • Nurse Practitioner role • Patient Web Portal • Geographic continuity • Part time practice issues • Open Access • Informational • Graduation/Succession Continuity Protocol
Current State Analysis Narrative of interactions and factors affecting continuity • Reception/Patient • Clinical Care Teams • Nurse/Patient • Patient education materials • Physician/Patient • Nurse Practitioner role • Patient Web Portal • Geographic continuity • Part time practice issues • Open Access • Informational • Graduation/Succession Continuity Protocol
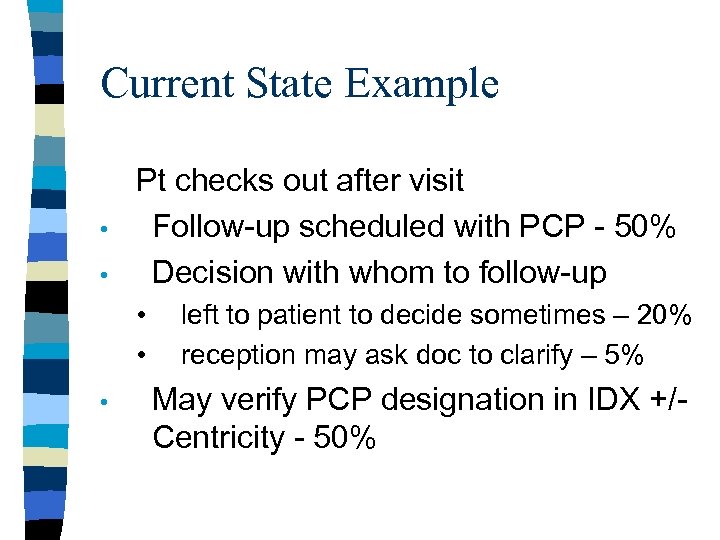 Current State Example • • Pt checks out after visit Follow-up scheduled with PCP - 50% Decision with whom to follow-up • • • left to patient to decide sometimes – 20% reception may ask doc to clarify – 5% May verify PCP designation in IDX +/Centricity - 50%
Current State Example • • Pt checks out after visit Follow-up scheduled with PCP - 50% Decision with whom to follow-up • • • left to patient to decide sometimes – 20% reception may ask doc to clarify – 5% May verify PCP designation in IDX +/Centricity - 50%
 Future State Analysis Narrative of ideal interactions and factors affecting continuity
Future State Analysis Narrative of ideal interactions and factors affecting continuity
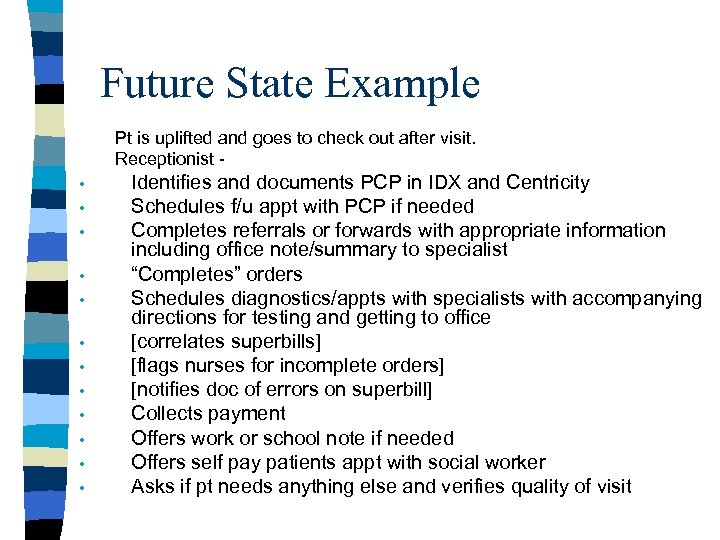 Future State Example Pt is uplifted and goes to check out after visit. Receptionist • • • Identifies and documents PCP in IDX and Centricity Schedules f/u appt with PCP if needed Completes referrals or forwards with appropriate information including office note/summary to specialist “Completes” orders Schedules diagnostics/appts with specialists with accompanying directions for testing and getting to office [correlates superbills] [flags nurses for incomplete orders] [notifies doc of errors on superbill] Collects payment Offers work or school note if needed Offers self pay patients appt with social worker Asks if pt needs anything else and verifies quality of visit
Future State Example Pt is uplifted and goes to check out after visit. Receptionist • • • Identifies and documents PCP in IDX and Centricity Schedules f/u appt with PCP if needed Completes referrals or forwards with appropriate information including office note/summary to specialist “Completes” orders Schedules diagnostics/appts with specialists with accompanying directions for testing and getting to office [correlates superbills] [flags nurses for incomplete orders] [notifies doc of errors on superbill] Collects payment Offers work or school note if needed Offers self pay patients appt with social worker Asks if pt needs anything else and verifies quality of visit
 Deliverables Idealized goals with realistic plans for initial pilot studies including measurements, accountable persons, and timeline
Deliverables Idealized goals with realistic plans for initial pilot studies including measurements, accountable persons, and timeline
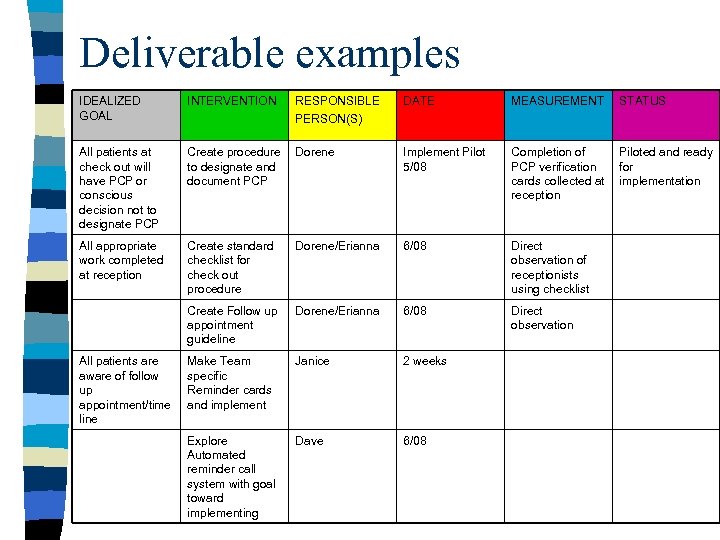 Deliverable examples IDEALIZED GOAL INTERVENTION RESPONSIBLE PERSON(S) DATE MEASUREMENT STATUS All patients at check out will have PCP or conscious decision not to designate PCP Create procedure to designate and document PCP Dorene Implement Pilot 5/08 Completion of PCP verification cards collected at reception Piloted and ready for implementation All appropriate work completed at reception Create standard checklist for check out procedure Dorene/Erianna 6/08 Direct observation of receptionists using checklist Create Follow up appointment guideline Dorene/Erianna 6/08 Direct observation Make Team specific Reminder cards and implement Janice 2 weeks Explore Automated reminder call system with goal toward implementing Dave 6/08 All patients are aware of follow up appointment/time line
Deliverable examples IDEALIZED GOAL INTERVENTION RESPONSIBLE PERSON(S) DATE MEASUREMENT STATUS All patients at check out will have PCP or conscious decision not to designate PCP Create procedure to designate and document PCP Dorene Implement Pilot 5/08 Completion of PCP verification cards collected at reception Piloted and ready for implementation All appropriate work completed at reception Create standard checklist for check out procedure Dorene/Erianna 6/08 Direct observation of receptionists using checklist Create Follow up appointment guideline Dorene/Erianna 6/08 Direct observation Make Team specific Reminder cards and implement Janice 2 weeks Explore Automated reminder call system with goal toward implementing Dave 6/08 All patients are aware of follow up appointment/time line
 Results of Kaizen 2 • • Forty-one deliverables Piloted four deliverables • • • Team appointment cards Patient education materials for PCP Reception script for scheduling patients Reception protocol for designating PCP Continuity measurements • MMCI 1 • Percent of patients seen who are from panels • Much more qualitative feel 1 Magill et al, 1987
Results of Kaizen 2 • • Forty-one deliverables Piloted four deliverables • • • Team appointment cards Patient education materials for PCP Reception script for scheduling patients Reception protocol for designating PCP Continuity measurements • MMCI 1 • Percent of patients seen who are from panels • Much more qualitative feel 1 Magill et al, 1987
 Lean Learnings • • Enhanced team efforts Allowed for candid discussion of processes rather than blaming Requires ongoing maintenance and championing Must be paired with effective communication • Communication books, email, staff meetings, practice meetings, visual reminders • Commitment to culture change, not just the tools
Lean Learnings • • Enhanced team efforts Allowed for candid discussion of processes rather than blaming Requires ongoing maintenance and championing Must be paired with effective communication • Communication books, email, staff meetings, practice meetings, visual reminders • Commitment to culture change, not just the tools
 Barriers to Implementation • • Costs 10% workforce Scheduling conflicts for events Empowerment of staff Leadership support Resident buy in to event as educationally valuable Culture changing Change management
Barriers to Implementation • • Costs 10% workforce Scheduling conflicts for events Empowerment of staff Leadership support Resident buy in to event as educationally valuable Culture changing Change management
 Future goals • Future Kaizen events • External facilitation • Integration with LVH SPPI initiative • • • Broadening resident involvement Solidification of portfolio goals for PI Development of stakeholders as owners of responsibility
Future goals • Future Kaizen events • External facilitation • Integration with LVH SPPI initiative • • • Broadening resident involvement Solidification of portfolio goals for PI Development of stakeholders as owners of responsibility
 Discussion/Questions
Discussion/Questions


