9e781792b6c98b3a3dba755c508752a9.ppt
- Количество слайдов: 119
 Implementing the MIHP Depression Interventions 1
Implementing the MIHP Depression Interventions 1
 Making Best Use of this Webcast • Print out the slides before you continue. • Make notes as you go along. • If you have questions after watching this webcast, contact: Joni Detwiler MIHP State Consultant 517 335 -6659 detwilerj@michigan. gov 2
Making Best Use of this Webcast • Print out the slides before you continue. • Make notes as you go along. • If you have questions after watching this webcast, contact: Joni Detwiler MIHP State Consultant 517 335 -6659 detwilerj@michigan. gov 2
 Learning Objectives 1. Review findings of MIHP Program Fidelity Study. 2. Define perinatal depression and describe its impact on the mother and her infant. 3. Discuss role of MIHP professional staff in addressing perinatal depression. 4. Discuss how to access mental health treatment and support services in your community for women suffering from perinatal depression. 3
Learning Objectives 1. Review findings of MIHP Program Fidelity Study. 2. Define perinatal depression and describe its impact on the mother and her infant. 3. Discuss role of MIHP professional staff in addressing perinatal depression. 4. Discuss how to access mental health treatment and support services in your community for women suffering from perinatal depression. 3
 MIHP PROGRAM FIDELITY STUDY 4
MIHP PROGRAM FIDELITY STUDY 4
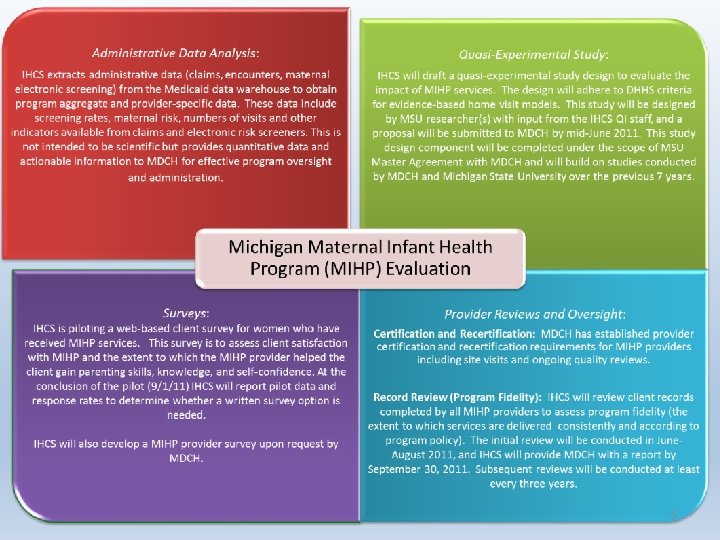 5
5
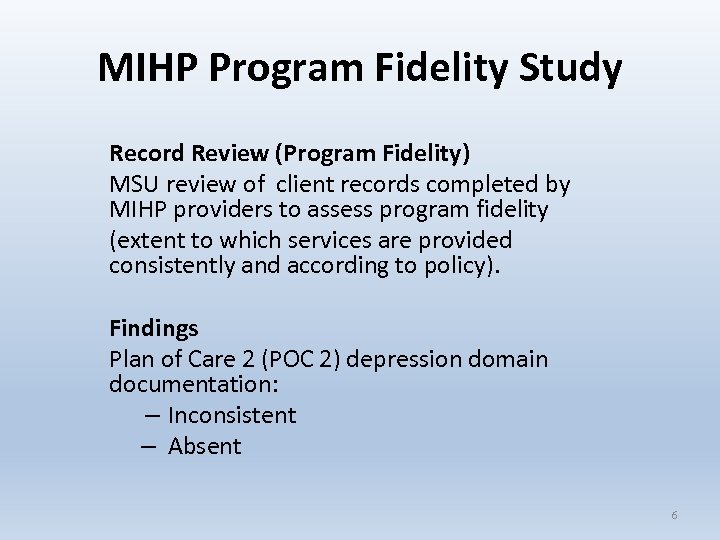 MIHP Program Fidelity Study Record Review (Program Fidelity) MSU review of client records completed by MIHP providers to assess program fidelity (extent to which services are provided consistently and according to policy). Findings Plan of Care 2 (POC 2) depression domain documentation: – Inconsistent – Absent 6
MIHP Program Fidelity Study Record Review (Program Fidelity) MSU review of client records completed by MIHP providers to assess program fidelity (extent to which services are provided consistently and according to policy). Findings Plan of Care 2 (POC 2) depression domain documentation: – Inconsistent – Absent 6
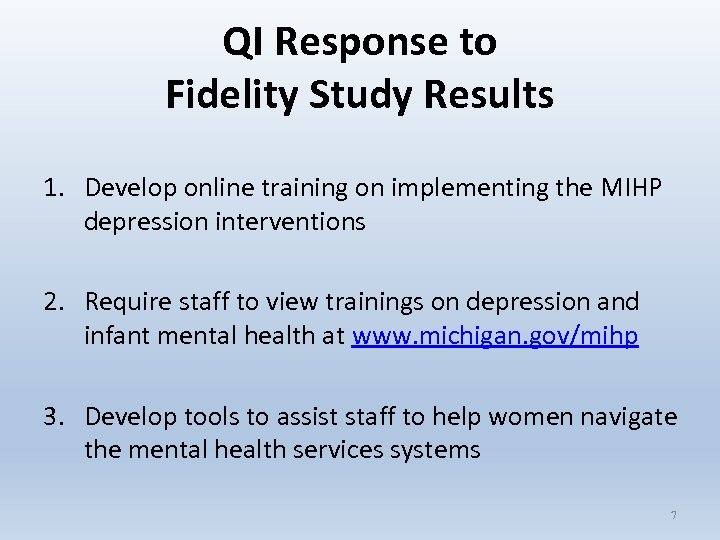 QI Response to Fidelity Study Results 1. Develop online training on implementing the MIHP depression interventions 2. Require staff to view trainings on depression and infant mental health at www. michigan. gov/mihp 3. Develop tools to assist staff to help women navigate the mental health services systems 7
QI Response to Fidelity Study Results 1. Develop online training on implementing the MIHP depression interventions 2. Require staff to view trainings on depression and infant mental health at www. michigan. gov/mihp 3. Develop tools to assist staff to help women navigate the mental health services systems 7
 PERINATAL DEPRESSION AND ITS EFFECTS ON MOTHER AND INFANT 8
PERINATAL DEPRESSION AND ITS EFFECTS ON MOTHER AND INFANT 8
 Depression Overview • Let’s start at the beginning… 9
Depression Overview • Let’s start at the beginning… 9
 Depression is a Worldwide Public Health Issue • Unipolar (clinical) depression is one of the top leading 5 causes of disability on our planet. Together with bipolar disorder (manic depression), it is costlier and more burdensome than any other ailment except cardiovascular disease. (1) • Depression affects twice as many women as men, regardless of racial and ethnic background and income. (2) • One in four women will experience severe depression at some point in life. (3) 10
Depression is a Worldwide Public Health Issue • Unipolar (clinical) depression is one of the top leading 5 causes of disability on our planet. Together with bipolar disorder (manic depression), it is costlier and more burdensome than any other ailment except cardiovascular disease. (1) • Depression affects twice as many women as men, regardless of racial and ethnic background and income. (2) • One in four women will experience severe depression at some point in life. (3) 10
 Depression in the Perinatal Period There are three types of depression women may experience during the period from start of pregnancy to 12 months after giving birth: • The Baby Blues • Perinatal Depression • Postpartum Psychosis NOTE: Prenatal Depression, Postpartum Depression, Postnatal Depression, Maternal Depression, and Perinatal Depression generally refer to the same mental health disorder. 11
Depression in the Perinatal Period There are three types of depression women may experience during the period from start of pregnancy to 12 months after giving birth: • The Baby Blues • Perinatal Depression • Postpartum Psychosis NOTE: Prenatal Depression, Postpartum Depression, Postnatal Depression, Maternal Depression, and Perinatal Depression generally refer to the same mental health disorder. 11
 Definition: Baby Blues • • Common reaction the first few days after delivery. Crying, worrying, sadness, anxiety, mood swings. Usually lifts in about 2 or 3 weeks. Experienced by 50 – 80% of women. 12
Definition: Baby Blues • • Common reaction the first few days after delivery. Crying, worrying, sadness, anxiety, mood swings. Usually lifts in about 2 or 3 weeks. Experienced by 50 – 80% of women. 12
 Definition: Perinatal Mood Disorder • Major and minor episodes of clinical depression during pregnancy or within first year after delivery. • More than the Baby Blues: – Lasts longer and is more severe • Symptoms: – – Sad, anxious, irritable Trouble concentrating, making decisions Sleeping or eating too much or too little Frequent crying and worrying 13
Definition: Perinatal Mood Disorder • Major and minor episodes of clinical depression during pregnancy or within first year after delivery. • More than the Baby Blues: – Lasts longer and is more severe • Symptoms: – – Sad, anxious, irritable Trouble concentrating, making decisions Sleeping or eating too much or too little Frequent crying and worrying 13
 Definition: Perinatal Mood Disorder • Symptoms (continued) Loss of interest in self care Loss of interest in things that used to be pleasurable Shows too much or two little concern for baby Not up to doing everyday tasks Feelings of inadequacy Suicidal thoughts • Symptoms last more than 2 weeks 14
Definition: Perinatal Mood Disorder • Symptoms (continued) Loss of interest in self care Loss of interest in things that used to be pleasurable Shows too much or two little concern for baby Not up to doing everyday tasks Feelings of inadequacy Suicidal thoughts • Symptoms last more than 2 weeks 14
 Definition: Perinatal Mood Disorder • Co-occurs with anxiety disorder for 2/3 of women: (4) – – Generalized Anxiety Disorder Panic Disorder Obsessive-compulsive Disorder Other • Often co-occurs with substance use disorder 15
Definition: Perinatal Mood Disorder • Co-occurs with anxiety disorder for 2/3 of women: (4) – – Generalized Anxiety Disorder Panic Disorder Obsessive-compulsive Disorder Other • Often co-occurs with substance use disorder 15
 Definition: Postpartum Psychosis • A rare disorder (one or two in 1, 000 women). • A severe form of perinatal depression that can be life -threatening. • Symptoms: extreme confusion, hopelessness, can’t sleep or eat, distrusts others, sees or hears things that aren’t there, thoughts of harming self, baby or others. • A medical emergency requiring urgent care. 16
Definition: Postpartum Psychosis • A rare disorder (one or two in 1, 000 women). • A severe form of perinatal depression that can be life -threatening. • Symptoms: extreme confusion, hopelessness, can’t sleep or eat, distrusts others, sees or hears things that aren’t there, thoughts of harming self, baby or others. • A medical emergency requiring urgent care. 16
 Prevalence of Perinatal Depression • 10 -20% of all women experience depression during the perinatal period. (5) • Prevalence in low-income and black women is estimated at almost double that of white women. (6) • Analysis of depression rates across 6 home visiting (HV) programs found that the % of women exceeding clinical cutoff for depression at enrollment ranged from 28. 5 – 61%. (7) 17
Prevalence of Perinatal Depression • 10 -20% of all women experience depression during the perinatal period. (5) • Prevalence in low-income and black women is estimated at almost double that of white women. (6) • Analysis of depression rates across 6 home visiting (HV) programs found that the % of women exceeding clinical cutoff for depression at enrollment ranged from 28. 5 – 61%. (7) 17
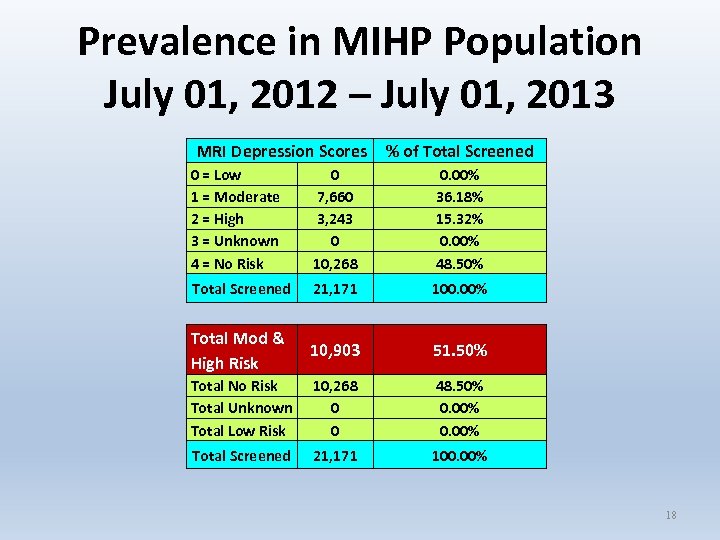 Prevalence in MIHP Population July 01, 2012 – July 01, 2013 MRI Depression Scores % of Total Screened 0 = Low 1 = Moderate 2 = High 3 = Unknown 4 = No Risk 0 7, 660 3, 243 0 10, 268 0. 00% 36. 18% 15. 32% 0. 00% 48. 50% Total Screened 21, 171 100. 00% Total Mod & High Risk 10, 903 51. 50% Total No Risk Total Unknown Total Low Risk 10, 268 0 0 48. 50% 0. 00% Total Screened 21, 171 100. 00% 18
Prevalence in MIHP Population July 01, 2012 – July 01, 2013 MRI Depression Scores % of Total Screened 0 = Low 1 = Moderate 2 = High 3 = Unknown 4 = No Risk 0 7, 660 3, 243 0 10, 268 0. 00% 36. 18% 15. 32% 0. 00% 48. 50% Total Screened 21, 171 100. 00% Total Mod & High Risk 10, 903 51. 50% Total No Risk Total Unknown Total Low Risk 10, 268 0 0 48. 50% 0. 00% Total Screened 21, 171 100. 00% 18
 Risks for Perinatal Depression • Can affect any woman regardless of age, race, income, culture, or education. • Factors that increase the risk: (8) – – – History of depression Use of alcohol and tobacco during pregnancy Unemployed/low-income Without a partner Lower level of education 19
Risks for Perinatal Depression • Can affect any woman regardless of age, race, income, culture, or education. • Factors that increase the risk: (8) – – – History of depression Use of alcohol and tobacco during pregnancy Unemployed/low-income Without a partner Lower level of education 19
 Few Pregnant Women Access Depression Treatment • U of M Depression Center study: 20% of pg women scored hi on standard depression survey, but of those, only 14% received any MH treatment. (9) • Northwestern Univ. screened 10, 000 PP women: 14% screened +; of those, 19% thought of harming selves. Recurrent episodes. Vast majority of PPD women in US not treated. (10) • Effective treatments have been identified - Cognitive Behavioral Therapy, Interpersonal Therapy, & meds. • Few women access depression treatment. 20
Few Pregnant Women Access Depression Treatment • U of M Depression Center study: 20% of pg women scored hi on standard depression survey, but of those, only 14% received any MH treatment. (9) • Northwestern Univ. screened 10, 000 PP women: 14% screened +; of those, 19% thought of harming selves. Recurrent episodes. Vast majority of PPD women in US not treated. (10) • Effective treatments have been identified - Cognitive Behavioral Therapy, Interpersonal Therapy, & meds. • Few women access depression treatment. 20
 Why Low-Income Women Don’t Access Depression Treatment 1. 2. 3. 4. 5. The illness itself gets in the way Shame about not being “strong” Guilt: “You’re supposed to be happy” when you’re pregnant. Stigma around using MH services; being seen at CMH Fear of being labeled “crazy”; lumped in with people with psychoses 6. Partner, parent or community (e. g. , faith or cultural group) prohibits it 7. Family or friends say “it’s all in your head - snap out of it” 21
Why Low-Income Women Don’t Access Depression Treatment 1. 2. 3. 4. 5. The illness itself gets in the way Shame about not being “strong” Guilt: “You’re supposed to be happy” when you’re pregnant. Stigma around using MH services; being seen at CMH Fear of being labeled “crazy”; lumped in with people with psychoses 6. Partner, parent or community (e. g. , faith or cultural group) prohibits it 7. Family or friends say “it’s all in your head - snap out of it” 21
 Why Low-Income Women Don’t Access Depression Treatment 8. Fear that she will be judged, especially if she’s young 9. Fear of taking medications, especially during pregnancy 10. Belief that psychotherapy won’t help because trauma, loss and stress are so prevalent in low-income community 11. Isolation 12. Hoops to jump and long wait times to get an appointment 13. Logistical barriers (e. g. , transportation, child care) 14. Previous negative experience with MH treatment 15. Too overwhelmed caring for infant and working 22
Why Low-Income Women Don’t Access Depression Treatment 8. Fear that she will be judged, especially if she’s young 9. Fear of taking medications, especially during pregnancy 10. Belief that psychotherapy won’t help because trauma, loss and stress are so prevalent in low-income community 11. Isolation 12. Hoops to jump and long wait times to get an appointment 13. Logistical barriers (e. g. , transportation, child care) 14. Previous negative experience with MH treatment 15. Too overwhelmed caring for infant and working 22
 Why Low-Income Women Don’t Access Depression Treatment 16. Mistrust of system 17. Fear MH treatment will be used against her in custody battle 18. Fear that confidentiality will be violated, resulting in: • CPS referral • Domestic violence Be upfront about when a CPS report is mandated, but maintain a warm relationship so that the mother feels understood and trusts that what she may say about her own MH won’t be misconstrued. 23
Why Low-Income Women Don’t Access Depression Treatment 16. Mistrust of system 17. Fear MH treatment will be used against her in custody battle 18. Fear that confidentiality will be violated, resulting in: • CPS referral • Domestic violence Be upfront about when a CPS report is mandated, but maintain a warm relationship so that the mother feels understood and trusts that what she may say about her own MH won’t be misconstrued. 23
 Adverse Effects of Untreated Perinatal Depression Untreated depression among pregnant and postpartum women is of concern due to its adverse effects on the health of the mother, the health of the infant, and the mother -infant relationship. (11) 24
Adverse Effects of Untreated Perinatal Depression Untreated depression among pregnant and postpartum women is of concern due to its adverse effects on the health of the mother, the health of the infant, and the mother -infant relationship. (11) 24
 Adverse Effects of Untreated Perinatal Depression 1. Depressed women are more likely to engage in risk taking behaviors: (12) • More likely to use substances. • Less likely to comply with prenatal care, putting self and baby at risk for complications and poor birth outcomes. • Less likely to use contraception consistently. 25
Adverse Effects of Untreated Perinatal Depression 1. Depressed women are more likely to engage in risk taking behaviors: (12) • More likely to use substances. • Less likely to comply with prenatal care, putting self and baby at risk for complications and poor birth outcomes. • Less likely to use contraception consistently. 25
 Adverse Effects of Untreated Perinatal Depression 2. Pregnant, depressed women are 3. 4 times more likely to deliver preterm and 4 times more likely to deliver a baby with low birth weight than nondepressed women. (13) 3. Undiagnosed and untreated maternal depression is associated with increased rates of maternal suicide. (14) 26
Adverse Effects of Untreated Perinatal Depression 2. Pregnant, depressed women are 3. 4 times more likely to deliver preterm and 4 times more likely to deliver a baby with low birth weight than nondepressed women. (13) 3. Undiagnosed and untreated maternal depression is associated with increased rates of maternal suicide. (14) 26
 Adverse Effects of Untreated Perinatal Depression 4. Maternal depressive symptoms in early infancy contribute to unfavorable patterns of health care seeking for children. – Increased use of acute care at 30 -33 months, including Emergency Department visits in past year. – Decreased receipt of preventive services, including ageappropriate well child visits and up-to-date immunizations. (15) 27
Adverse Effects of Untreated Perinatal Depression 4. Maternal depressive symptoms in early infancy contribute to unfavorable patterns of health care seeking for children. – Increased use of acute care at 30 -33 months, including Emergency Department visits in past year. – Decreased receipt of preventive services, including ageappropriate well child visits and up-to-date immunizations. (15) 27
 Adverse Effects of Untreated Perinatal Depression 5. Maternal depression, alone, or in combination with other risks can pose serious, but typically unrecognized barriers to healthy early development and school readiness, particularly for low-income young children. (16) The cumulative impact of depression in combination with other risks to healthy parenting (e. g. , low educational achievement) is greater. 28
Adverse Effects of Untreated Perinatal Depression 5. Maternal depression, alone, or in combination with other risks can pose serious, but typically unrecognized barriers to healthy early development and school readiness, particularly for low-income young children. (16) The cumulative impact of depression in combination with other risks to healthy parenting (e. g. , low educational achievement) is greater. 28
 Adverse Effects of Untreated Perinatal Depression 6. Postpartum depression can impair early relationships: (17) • Secure attachment, or healthy emotional bond, between an infant and primary caregiver is key to the future emotional development of the infant. • Depression threatens the mother’s emotional and physical ability to care for her child and to foster a healthy relationship with her child. 29
Adverse Effects of Untreated Perinatal Depression 6. Postpartum depression can impair early relationships: (17) • Secure attachment, or healthy emotional bond, between an infant and primary caregiver is key to the future emotional development of the infant. • Depression threatens the mother’s emotional and physical ability to care for her child and to foster a healthy relationship with her child. 29
 Still Face Experiment Video Still Face Experiment: Dr. Edward Tronick – You. Tube (2: 49) A phenomenon in which an infant, after 3 minutes of “interaction” with a non-responsive expressionless mother, “rapidly sobers and grows wary. He makes repeated attempts to get the interaction into its usual reciprocal pattern. When these attempts fail, the infant withdraws [and] orients his face and body away from his mother with a withdrawn, hopeless facial expression. ” (18) 30
Still Face Experiment Video Still Face Experiment: Dr. Edward Tronick – You. Tube (2: 49) A phenomenon in which an infant, after 3 minutes of “interaction” with a non-responsive expressionless mother, “rapidly sobers and grows wary. He makes repeated attempts to get the interaction into its usual reciprocal pattern. When these attempts fail, the infant withdraws [and] orients his face and body away from his mother with a withdrawn, hopeless facial expression. ” (18) 30
 Adverse Effects of Untreated Perinatal Depression 7. Children born to a women who suffers from postpartum depression are: (19) • More likely to lack secure attachment and are therefore at increased risk for delayed or impaired cognitive, emotional and linguistic development. • More likely to have behavioral problems. • More likely to experience worse long-term mental health problems. 31
Adverse Effects of Untreated Perinatal Depression 7. Children born to a women who suffers from postpartum depression are: (19) • More likely to lack secure attachment and are therefore at increased risk for delayed or impaired cognitive, emotional and linguistic development. • More likely to have behavioral problems. • More likely to experience worse long-term mental health problems. 31
 Adverse Effects of Untreated Perinatal Depression 8. A study of WIC mothers found that postpartum depression resulted in: (20) • • Poor nutrition Poor infant weight gain Childhood obesity and adiposity Poor mother-child interactions 32
Adverse Effects of Untreated Perinatal Depression 8. A study of WIC mothers found that postpartum depression resulted in: (20) • • Poor nutrition Poor infant weight gain Childhood obesity and adiposity Poor mother-child interactions 32
 Maternal MH Problems: A Challenge to HV Programs • Three challenges to HV programs have been consistently identified: maternal mental health, substance abuse, and intimate partner violence. (21) • Qualitative research finds that HVs identify maternal MH problems as a significant barrier to providing HV services in a consistent, continuous manner – More difficult to engage and serve – Harder to work with parents who: • Are perceived as “uncommitted” or “unmotivated” • Threaten to commit suicide 33
Maternal MH Problems: A Challenge to HV Programs • Three challenges to HV programs have been consistently identified: maternal mental health, substance abuse, and intimate partner violence. (21) • Qualitative research finds that HVs identify maternal MH problems as a significant barrier to providing HV services in a consistent, continuous manner – More difficult to engage and serve – Harder to work with parents who: • Are perceived as “uncommitted” or “unmotivated” • Threaten to commit suicide 33
 HVs Feel Inadequately Trained to Address MH Problems • In one study, 44% of HVs felt they were inadequately trained the help families with MH problems. (22) • HVs often say they are uncomfortable discussing depression with a mother because: – They don’t have the right training and are afraid they’ll say the wrong thing. – When they do bring it up and the women refuses MH services, they feel responsible. – They feel overwhelmed to be the only lifeline for a depressed and perhaps abused woman. 34
HVs Feel Inadequately Trained to Address MH Problems • In one study, 44% of HVs felt they were inadequately trained the help families with MH problems. (22) • HVs often say they are uncomfortable discussing depression with a mother because: – They don’t have the right training and are afraid they’ll say the wrong thing. – When they do bring it up and the women refuses MH services, they feel responsible. – They feel overwhelmed to be the only lifeline for a depressed and perhaps abused woman. 34
 Becoming More Comfortable Discussing Depression • If you don’t feel prepared, it’s perfectly understandable you would be uncomfortable talking about depression. • You are not going to make it worse for the mother by discussing her depression. • We’ll give you some concrete ways to frame your discussion later in this presentation. 35
Becoming More Comfortable Discussing Depression • If you don’t feel prepared, it’s perfectly understandable you would be uncomfortable talking about depression. • You are not going to make it worse for the mother by discussing her depression. • We’ll give you some concrete ways to frame your discussion later in this presentation. 35
 ROLE OF MIHP IN ADDRESSING PERINATAL DEPRESSION 36
ROLE OF MIHP IN ADDRESSING PERINATAL DEPRESSION 36
 What Can MIHP Do? • Care coordination • Education • Support and encouragement • Not therapy – Exception: Infant Mental Health Specialist can provide brief mental health interventions 37
What Can MIHP Do? • Care coordination • Education • Support and encouragement • Not therapy – Exception: Infant Mental Health Specialist can provide brief mental health interventions 37
 History of Trauma Is Related to Depression • Trauma is very common among women in MIHP. • Trauma is the personal experience of interpersonal violence including: (23) – – – sexual abuse physical abuse severe neglect loss and/or the witnessing of violence, terrorism and disasters. 38
History of Trauma Is Related to Depression • Trauma is very common among women in MIHP. • Trauma is the personal experience of interpersonal violence including: (23) – – – sexual abuse physical abuse severe neglect loss and/or the witnessing of violence, terrorism and disasters. 38
 What is Trauma-Informed Care? • An appreciation for the high prevalence of traumatic experiences among persons we serve. • A thorough understanding of the profound neurological, biological, psychological and social effects of trauma and violence on the individual, including adoption of health-risk behaviors as coping mechanisms (smoking, substance abuse [SA], self harm, sexual promiscuity, violence). • Care that addresses these effects, is collaborative, supportive and skill–based. (24) 39
What is Trauma-Informed Care? • An appreciation for the high prevalence of traumatic experiences among persons we serve. • A thorough understanding of the profound neurological, biological, psychological and social effects of trauma and violence on the individual, including adoption of health-risk behaviors as coping mechanisms (smoking, substance abuse [SA], self harm, sexual promiscuity, violence). • Care that addresses these effects, is collaborative, supportive and skill–based. (24) 39
 Learn More about Trauma-Informed Care • Trauma-informed organizations and programs are based on an understanding of the vulnerabilities or triggers of trauma survivors that traditional service delivery approaches may exacerbate, so providers can be more supportive and avoid re-traumatization. • Trauma-informed care is spreading across health and human services: MH, child welfare, health care, DV, foster care, homelessness, SA, criminal justice, military families, refugee services, and others. • http: //acesconnection. com/ for learning resources. 40
Learn More about Trauma-Informed Care • Trauma-informed organizations and programs are based on an understanding of the vulnerabilities or triggers of trauma survivors that traditional service delivery approaches may exacerbate, so providers can be more supportive and avoid re-traumatization. • Trauma-informed care is spreading across health and human services: MH, child welfare, health care, DV, foster care, homelessness, SA, criminal justice, military families, refugee services, and others. • http: //acesconnection. com/ for learning resources. 40
 Diversity-Informed Practice: Community Context Community context affects perception of depression: Many women who live in poverty or experience institutional racism may assume they’ll be depressed (or get diabetes, or be physically abused, or be sexually assaulted, etc. ) because “that’s just the way it is for the women in this neighborhood/housing project/tribal community/town. ” They feel powerless to reduce their depression (low sense of self-determination). Or, they may deny their depression. “It’s not me, it’s my life circumstances. ” 41
Diversity-Informed Practice: Community Context Community context affects perception of depression: Many women who live in poverty or experience institutional racism may assume they’ll be depressed (or get diabetes, or be physically abused, or be sexually assaulted, etc. ) because “that’s just the way it is for the women in this neighborhood/housing project/tribal community/town. ” They feel powerless to reduce their depression (low sense of self-determination). Or, they may deny their depression. “It’s not me, it’s my life circumstances. ” 41
 We met with a team of diverse MIHP providers to discuss cultural implications of depression and stress 42
We met with a team of diverse MIHP providers to discuss cultural implications of depression and stress 42
 Diversity-Informed Practice: Language and Cultural Perceptions • Be mindful of potential language barriers in approaching MH issues (e. g. , some Spanish-speakers may use the word “nervous” or “under pressure” instead of “depression”). • Stigma of mental illness affects all groups, but may be heightened in some (e. g. , some ethnic or faith-based groups). • Some groups highly respect the authority of the MD and may be more likely to accept idea of meds or a MH referral from the MD than from you; work with a woman’s MD and MHP to help her get what she needs. 43
Diversity-Informed Practice: Language and Cultural Perceptions • Be mindful of potential language barriers in approaching MH issues (e. g. , some Spanish-speakers may use the word “nervous” or “under pressure” instead of “depression”). • Stigma of mental illness affects all groups, but may be heightened in some (e. g. , some ethnic or faith-based groups). • Some groups highly respect the authority of the MD and may be more likely to accept idea of meds or a MH referral from the MD than from you; work with a woman’s MD and MHP to help her get what she needs. 43
 Diversity-Informed Practice: Cultural Affiliation Varies That said, cultural affiliation varies. YOU MUST ASK. • Not everyone in the same cultural group thinks the same way. Young parents may not be connected to their group. • The only way to really know what a particular individual believes about depression (or anything else) is to ask her. Be open to having a conversation about culture. • I don’t know how you think or feel about this – help me learn here. What do you think about people who have depression? What does your family think? What does your community think? These are very telling questions. 44
Diversity-Informed Practice: Cultural Affiliation Varies That said, cultural affiliation varies. YOU MUST ASK. • Not everyone in the same cultural group thinks the same way. Young parents may not be connected to their group. • The only way to really know what a particular individual believes about depression (or anything else) is to ask her. Be open to having a conversation about culture. • I don’t know how you think or feel about this – help me learn here. What do you think about people who have depression? What does your family think? What does your community think? These are very telling questions. 44
 Diversity-Informed Practice: Legal & Undocumented Immigrants Legal and undocumented immigrants face different realities in the United States. Persons living under political asylum and undocumented persons working in migrant camps have very different experiences here, but both may have history of trauma. Pregnant non-citizens qualify only for the MOMS program, which offers fewer benefits than other Medicaid programs. Be willing to track down info on what a particular immigrant is eligible for and what laws pertain to her. 45
Diversity-Informed Practice: Legal & Undocumented Immigrants Legal and undocumented immigrants face different realities in the United States. Persons living under political asylum and undocumented persons working in migrant camps have very different experiences here, but both may have history of trauma. Pregnant non-citizens qualify only for the MOMS program, which offers fewer benefits than other Medicaid programs. Be willing to track down info on what a particular immigrant is eligible for and what laws pertain to her. 45
 Primary MIHP Activities to Address Depression 1. Screen every pregnant and postpartum woman with infant, using standardized, validated tools embedded within MIHP Risk Identifier. (RN, SW) 2. Educate all women about Perinatal Depression utilizing POC 1. (RN, SW, RD, IMH Spec. ) 46
Primary MIHP Activities to Address Depression 1. Screen every pregnant and postpartum woman with infant, using standardized, validated tools embedded within MIHP Risk Identifier. (RN, SW) 2. Educate all women about Perinatal Depression utilizing POC 1. (RN, SW, RD, IMH Spec. ) 46
 Primary MIHP Activities to Address Depression 3. Refer women at mod or high risk to treatment (including IMH services); provide education and support; coordinate care, utilizing POC 2. (RN, SW, RD, IMH Spec. ) NOTE: RD must follow up with SW or RN to engage them in addressing depression. 4. Assess need for IMH services (depression is a factor). If parent refuses, provide brief, direct parent-infant intervention. (IMH Spec. ) 47
Primary MIHP Activities to Address Depression 3. Refer women at mod or high risk to treatment (including IMH services); provide education and support; coordinate care, utilizing POC 2. (RN, SW, RD, IMH Spec. ) NOTE: RD must follow up with SW or RN to engage them in addressing depression. 4. Assess need for IMH services (depression is a factor). If parent refuses, provide brief, direct parent-infant intervention. (IMH Spec. ) 47
 Screen for Depression and Stress The standardized MIHP Maternal Risk Identifier is administered at intake. It includes: – Edinburg Postnatal Depression Scale (EPDS) – Perceived Stress Scale 4 (PSS 4) 48
Screen for Depression and Stress The standardized MIHP Maternal Risk Identifier is administered at intake. It includes: – Edinburg Postnatal Depression Scale (EPDS) – Perceived Stress Scale 4 (PSS 4) 48
 POC 1: Educate All Women on Perinatal Depression • POC 1 documents that beneficiary received one or both of the following items from RN or SW at administration of Risk Identifier: – MIHP Maternal & Infant Education Packet: Pregnancy & Infant Health – Instructions on how to sign up for text 4 baby • Education Packet includes basic info on all of the MIHP domains to guide discussion with beneficiary: – At administration of Risk Identifier (RN, SW) – At later visit(s), depending on the beneficiary’s individual situation (RN, SW, RD, IMH Spec. ) 49
POC 1: Educate All Women on Perinatal Depression • POC 1 documents that beneficiary received one or both of the following items from RN or SW at administration of Risk Identifier: – MIHP Maternal & Infant Education Packet: Pregnancy & Infant Health – Instructions on how to sign up for text 4 baby • Education Packet includes basic info on all of the MIHP domains to guide discussion with beneficiary: – At administration of Risk Identifier (RN, SW) – At later visit(s), depending on the beneficiary’s individual situation (RN, SW, RD, IMH Spec. ) 49
 POC 1: Educate All Women on Perinatal Depression • Education Packet is a 44 -page booklet posted on the MIHP web site. • The Stress, Depression and Mental Health domain is covered on pages 22 -23. 50
POC 1: Educate All Women on Perinatal Depression • Education Packet is a 44 -page booklet posted on the MIHP web site. • The Stress, Depression and Mental Health domain is covered on pages 22 -23. 50
 Stress, Depression and MH Pregnancy & Infant Health What is perinatal depression? It’s depression that occurs during pregnancy or postpartum. Postpartum means within a year after giving birth. It is VERY common. It can be mild, moderate or severe. 51
Stress, Depression and MH Pregnancy & Infant Health What is perinatal depression? It’s depression that occurs during pregnancy or postpartum. Postpartum means within a year after giving birth. It is VERY common. It can be mild, moderate or severe. 51
 Stress, Depression and MH Pregnancy & Infant Health How do I know if I might be depressed? Women with perinatal depression usually sense that “something’s not right. ” 52
Stress, Depression and MH Pregnancy & Infant Health How do I know if I might be depressed? Women with perinatal depression usually sense that “something’s not right. ” 52
 Stress, Depression and MH Pregnancy & Infant Health Would you answer “yes” to any following statements? – I feel very sad and hopeless more days than not. – I’m not enjoying life like I used to. – I blame myself for everything. – I worry about everything. – I’m afraid and I don’t know why. – I feel overwhelmed and have a hard time coping. 53
Stress, Depression and MH Pregnancy & Infant Health Would you answer “yes” to any following statements? – I feel very sad and hopeless more days than not. – I’m not enjoying life like I used to. – I blame myself for everything. – I worry about everything. – I’m afraid and I don’t know why. – I feel overwhelmed and have a hard time coping. 53
 Stress, Depression and MH Pregnancy & Infant Health – I cry a lot. – I have trouble sleeping because I’m so unhappy. – I want to sleep all the time. – I’m confused and distracted. – I get angry very easily. – I don’t think I will be a good mother. – I have thoughts of harming myself or others. – I hear voices or see things that aren’t there. 54
Stress, Depression and MH Pregnancy & Infant Health – I cry a lot. – I have trouble sleeping because I’m so unhappy. – I want to sleep all the time. – I’m confused and distracted. – I get angry very easily. – I don’t think I will be a good mother. – I have thoughts of harming myself or others. – I hear voices or see things that aren’t there. 54
 Stress, Depression and MH Pregnancy & Infant Health If you answered “yes” to any of these statements, you may be depressed. Reiterate: You are not alone. Many pregnant women and new moms have these same thoughts and feelings. 55
Stress, Depression and MH Pregnancy & Infant Health If you answered “yes” to any of these statements, you may be depressed. Reiterate: You are not alone. Many pregnant women and new moms have these same thoughts and feelings. 55
 Stress, Depression and MH Pregnancy & Infant Health How does perinatal depression affect my baby? Your baby could: – Be born too small or too early. – Be fussy and jittery. – Have feeding or sleeping problems. – End up with learning problems. – End up with behavior problems, such as hyperactivity. 56
Stress, Depression and MH Pregnancy & Infant Health How does perinatal depression affect my baby? Your baby could: – Be born too small or too early. – Be fussy and jittery. – Have feeding or sleeping problems. – End up with learning problems. – End up with behavior problems, such as hyperactivity. 56
 Stress, Depression and MH Pregnancy & Infant Health It’s harder for you and your baby to form a strong emotional attachment to each other. Attachment is important to your baby’s development. 57
Stress, Depression and MH Pregnancy & Infant Health It’s harder for you and your baby to form a strong emotional attachment to each other. Attachment is important to your baby’s development. 57
 58
58
 Stress, Depression and MH Pregnancy & Infant Health • Where can I get more information about perinatal depression? – – Your doctor. Your MIHP worker Your Medicaid Health Plan. Online at http: //www. mededppd. org/ 59
Stress, Depression and MH Pregnancy & Infant Health • Where can I get more information about perinatal depression? – – Your doctor. Your MIHP worker Your Medicaid Health Plan. Online at http: //www. mededppd. org/ 59
 text 4 baby: Alternative to Education Packet • Free text message service to promote MCH. • Includes intermittent messages on depression similar to those in Education Packet. • Resource info is linked to mother’s zip code. • Bring Education Packet to visits for discussion purposes, even if beneficiary chose the text 4 baby alternative. • Education Packet and text 4 baby both good tools. 60
text 4 baby: Alternative to Education Packet • Free text message service to promote MCH. • Includes intermittent messages on depression similar to those in Education Packet. • Resource info is linked to mother’s zip code. • Bring Education Packet to visits for discussion purposes, even if beneficiary chose the text 4 baby alternative. • Education Packet and text 4 baby both good tools. 60
 POC 1 Documentation 1. POC 1: • Check off box (Education Packet or text 4 baby) • Signature of RN and SW within 10 business days 2. Professional Visit Progress Note: • Depression/stress written on line after education packet box checked • Other visit information 61
POC 1 Documentation 1. POC 1: • Check off box (Education Packet or text 4 baby) • Signature of RN and SW within 10 business days 2. Professional Visit Progress Note: • Depression/stress written on line after education packet box checked • Other visit information 61
 POC 2: Supporting Women at Mod-Hi Risk of Dep/Stress Next we’ll look at: – How to implement the standardized POC 2 interventions – How to document POC 2 interventions effectively 62
POC 2: Supporting Women at Mod-Hi Risk of Dep/Stress Next we’ll look at: – How to implement the standardized POC 2 interventions – How to document POC 2 interventions effectively 62
 POC 2 Services Determined in Two Ways 1. Results of the Risk Identifier 2. Woman’s situation matches risk criteria in the Risk Information column (#2) of the POC 2 63
POC 2 Services Determined in Two Ways 1. Results of the Risk Identifier 2. Woman’s situation matches risk criteria in the Risk Information column (#2) of the POC 2 63
 POC 2 Intervention Levels in Stress/Depression/MH Domain • Services stratified by anticipated intervention level • Domain intervention levels: – Moderate (scores 9 - 12 on EPDS or scores 9 - 16 on PSS 4 or is in treatment) – High (scores 13 or above on EPDS or is in treatment) – Emergency (risk of imminent harm to self or others) 64
POC 2 Intervention Levels in Stress/Depression/MH Domain • Services stratified by anticipated intervention level • Domain intervention levels: – Moderate (scores 9 - 12 on EPDS or scores 9 - 16 on PSS 4 or is in treatment) – High (scores 13 or above on EPDS or is in treatment) – Emergency (risk of imminent harm to self or others) 64
 Developing the POC 2 Stress/Depression/MH Domain 1. Once Risk Identifier is completed: – Enter data into SSO data base – Print out Score Sheet 2. Pull Stress/Depression/Mental Health POC 2 if Risk Identifier Score Sheet indicates a risk. 65
Developing the POC 2 Stress/Depression/MH Domain 1. Once Risk Identifier is completed: – Enter data into SSO data base – Print out Score Sheet 2. Pull Stress/Depression/Mental Health POC 2 if Risk Identifier Score Sheet indicates a risk. 65
 Developing the POC 2 Stress/Depression/MH Domain 3. SW and RN must sign POC 3 within 10 business days of each other. 4. No visits may be completed or billed until #2 and #3 above are done, unless an emergency arises. 66
Developing the POC 2 Stress/Depression/MH Domain 3. SW and RN must sign POC 3 within 10 business days of each other. 4. No visits may be completed or billed until #2 and #3 above are done, unless an emergency arises. 66
 Implementing the Stress/ Depression/ MH Interventions • Follow the numbered interventions based on risk level (low, mod, high, emergency). • MIHP Certification Tool Cycle 4 requires you to address any risk domain that scores out high within the first three visits. • All of the numbered interventions will not apply to every beneficiary. 67
Implementing the Stress/ Depression/ MH Interventions • Follow the numbered interventions based on risk level (low, mod, high, emergency). • MIHP Certification Tool Cycle 4 requires you to address any risk domain that scores out high within the first three visits. • All of the numbered interventions will not apply to every beneficiary. 67
 We’re Not in this Alone Medicaid Health Plans and medical care providers are active partners in MIHP services delivery. MIHP MCP 68
We’re Not in this Alone Medicaid Health Plans and medical care providers are active partners in MIHP services delivery. MIHP MCP 68
 Foundations of Intervention Delivery Use: ü ü Motivational Interviewing Coaching for Self Sufficiency Perinatal Periods of Risk Life Course Theory (See Motivational Interviewing and the Theory Behind MIHP Interventions webcast at MIHP web site) 69
Foundations of Intervention Delivery Use: ü ü Motivational Interviewing Coaching for Self Sufficiency Perinatal Periods of Risk Life Course Theory (See Motivational Interviewing and the Theory Behind MIHP Interventions webcast at MIHP web site) 69
 Be Prepared to Talk with a Woman about her Depression • Learn as much as you can about depression, its effects, and treatment. • Be extremely familiar with the HRSA booklet. Depression During & After Pregnancy: A Resource for Women, Their Families, & Friends. • Watch the MIHP online training: Depression, Mental Health, Stress (Kothari and Ludtke). • Remind yourself that talking about depression can only help – it can’t hurt. 70
Be Prepared to Talk with a Woman about her Depression • Learn as much as you can about depression, its effects, and treatment. • Be extremely familiar with the HRSA booklet. Depression During & After Pregnancy: A Resource for Women, Their Families, & Friends. • Watch the MIHP online training: Depression, Mental Health, Stress (Kothari and Ludtke). • Remind yourself that talking about depression can only help – it can’t hurt. 70
 Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score Before discussing her score: 1. Focus on her symptoms – She may shut down if you begin by using MH labels (names of disorders) and reject idea of having a MH problem, which she equates with “being crazy” 2. Focus on her experience with depression (self and others) 3. Focus on her understanding of depression 71
Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score Before discussing her score: 1. Focus on her symptoms – She may shut down if you begin by using MH labels (names of disorders) and reject idea of having a MH problem, which she equates with “being crazy” 2. Focus on her experience with depression (self and others) 3. Focus on her understanding of depression 71
 Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score 1. Ask her about her symptoms by following up on some of her EPDS responses. Remember when we asked you all those questions when you first signed up for MIHP? Fourteen of those questions asked about how you recently felt (enjoying life, anxious, sad, able to control important things in life, etc. ). Can we talk about some of your answers to the questions? Can you tell more a little more about them? 72
Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score 1. Ask her about her symptoms by following up on some of her EPDS responses. Remember when we asked you all those questions when you first signed up for MIHP? Fourteen of those questions asked about how you recently felt (enjoying life, anxious, sad, able to control important things in life, etc. ). Can we talk about some of your answers to the questions? Can you tell more a little more about them? 72
 Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score 2. Have you ever known anyone with depression or who was very stressed out? • • Was it a family member? What do you think it was like for that person? What was it like for you to be with that person? How did other people treat that person? 3. What is your understanding of depression? • Did you ever feel that you might have had depression at any time in your life? • If so, what was that time like for you? 73
Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score 2. Have you ever known anyone with depression or who was very stressed out? • • Was it a family member? What do you think it was like for that person? What was it like for you to be with that person? How did other people treat that person? 3. What is your understanding of depression? • Did you ever feel that you might have had depression at any time in your life? • If so, what was that time like for you? 73
 Low Risk Intervention 1 Review written material on stress, baby blues, and/or perinatal depression/anxiety. – Maternal/Infant Education Packet (POC 1). – HRSA booklet or other comparable booklet. (Free HRSA booklet Depression During & After Pregnancy: A Resource for Women, Their Families, & Friends, English and Spanish) Emphasize that depression is common & treatable. – Explain what intrusive thoughts are (next slide). – Explain that physical symptoms are common in depression (slide after next). 74
Low Risk Intervention 1 Review written material on stress, baby blues, and/or perinatal depression/anxiety. – Maternal/Infant Education Packet (POC 1). – HRSA booklet or other comparable booklet. (Free HRSA booklet Depression During & After Pregnancy: A Resource for Women, Their Families, & Friends, English and Spanish) Emphasize that depression is common & treatable. – Explain what intrusive thoughts are (next slide). – Explain that physical symptoms are common in depression (slide after next). 74
 Asking About Intrusive Thoughts Many women have intrusive thoughts that really bother them. “Intrusive” thoughts seem to enter your mind against your will and are very hard to get rid of. E. g. , you might find yourself worrying that you’re not doing everything right for your baby, or you might do something wrong to your baby, or something might happen to your baby. All moms worry, but it’s really hard when you’re worrying so much you can’t sleep and you just want the thoughts to stop but you can’t figure out how. Does this ever happen to you? 75
Asking About Intrusive Thoughts Many women have intrusive thoughts that really bother them. “Intrusive” thoughts seem to enter your mind against your will and are very hard to get rid of. E. g. , you might find yourself worrying that you’re not doing everything right for your baby, or you might do something wrong to your baby, or something might happen to your baby. All moms worry, but it’s really hard when you’re worrying so much you can’t sleep and you just want the thoughts to stop but you can’t figure out how. Does this ever happen to you? 75
 Post. Partum Depression Educational Video Post Partum Depression Educational Video -New Jersey – You. Tube (5. 13) Women of different ages, races, and economic backgrounds, including the First Lady of New Jersey, describe their experiences with postpartum depression. 76
Post. Partum Depression Educational Video Post Partum Depression Educational Video -New Jersey – You. Tube (5. 13) Women of different ages, races, and economic backgrounds, including the First Lady of New Jersey, describe their experiences with postpartum depression. 76
 Low Risk Intervention 2 Discuss stress reduction/coping strategies and/or selfcare skills. All moms need a self-care action plan, especially if they’re at risk for depression. There are simple, everyday things you can do to take care of yourself to feel better. Here’s a self-care action plan form that we can fill out together. It’s always better to write your plan down so you can look at it whenever you want to. 77
Low Risk Intervention 2 Discuss stress reduction/coping strategies and/or selfcare skills. All moms need a self-care action plan, especially if they’re at risk for depression. There are simple, everyday things you can do to take care of yourself to feel better. Here’s a self-care action plan form that we can fill out together. It’s always better to write your plan down so you can look at it whenever you want to. 77
 Weekly Self-Care Action Plan 1. Exercise – stay active 2. Do something pleasurable every day 3. Spend time with people who make you laugh and feel good about yourself 78
Weekly Self-Care Action Plan 1. Exercise – stay active 2. Do something pleasurable every day 3. Spend time with people who make you laugh and feel good about yourself 78
 Weekly Self-Care Action Plan 4. Lean on your family, friends and community when you’re very down or very stressed Ask about emotionally supportive people in her life: When you’re down/stressed, who can you turn to? Which family members? Which friends and neighbors? Who else (e. g. , godmother, unofficial “aunt, ” etc. )? Do you have a faith community? Anyone there? Do you belong to another kind of group? Anyone there? Do you have enough support from these people? 79
Weekly Self-Care Action Plan 4. Lean on your family, friends and community when you’re very down or very stressed Ask about emotionally supportive people in her life: When you’re down/stressed, who can you turn to? Which family members? Which friends and neighbors? Who else (e. g. , godmother, unofficial “aunt, ” etc. )? Do you have a faith community? Anyone there? Do you belong to another kind of group? Anyone there? Do you have enough support from these people? 79
 Weekly Self-Care Action Plan 5. Ask for help with the baby so you can sleep 6. Find a support group or class – connect with other women experiencing the same things you are 7. Practice relaxation (e. g. , slow, deep breathing) 8. Any other way to take care of yourself this week? 9. Give yourself some credit when you do one of the steps on this self-care action plan 80
Weekly Self-Care Action Plan 5. Ask for help with the baby so you can sleep 6. Find a support group or class – connect with other women experiencing the same things you are 7. Practice relaxation (e. g. , slow, deep breathing) 8. Any other way to take care of yourself this week? 9. Give yourself some credit when you do one of the steps on this self-care action plan 80
 Low Risk Intervention 3 Educate on symptoms of depression and/or anxiety to report to health care provider. 81
Low Risk Intervention 3 Educate on symptoms of depression and/or anxiety to report to health care provider. 81
 Physical Symptoms are Common in Depression • • Joint pain Limb pain Back pain Gastrointestinal problems Tiredness Sleep disturbances Psychomotor activity changes Appetite changes 82
Physical Symptoms are Common in Depression • • Joint pain Limb pain Back pain Gastrointestinal problems Tiredness Sleep disturbances Psychomotor activity changes Appetite changes 82
 What Does Postpartum Depression Feel Like? (25) “It feels scary. ” “It feels out of control. ” “It feels like I’m never going to feel like myself again. ” “It feels like each day is a hundred hours long. ” “It feels like no one understands. ” “It feels like my relationship cannot survive this. ” “It feels like I’m a bad mother. ” “It feels like I should never have had this baby. ” “If feels like if I could only get a good night’s sleep, everything would be better. ” “It feels like I have no patience for anything anymore. ” “It feels like I’m going crazy. ” “It feels like I will always feel like this. ” 83
What Does Postpartum Depression Feel Like? (25) “It feels scary. ” “It feels out of control. ” “It feels like I’m never going to feel like myself again. ” “It feels like each day is a hundred hours long. ” “It feels like no one understands. ” “It feels like my relationship cannot survive this. ” “It feels like I’m a bad mother. ” “It feels like I should never have had this baby. ” “If feels like if I could only get a good night’s sleep, everything would be better. ” “It feels like I have no patience for anything anymore. ” “It feels like I’m going crazy. ” “It feels like I will always feel like this. ” 83
 Low Risk Intervention 4 Provide support and encouragement. 84
Low Risk Intervention 4 Provide support and encouragement. 84
 Low Risk Intervention 5 Provide information/referral to community resources for stress reduction or problem solving. 85
Low Risk Intervention 5 Provide information/referral to community resources for stress reduction or problem solving. 85
 Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • Those 14 questions about how you felt around the time that you signed up for MIHP were a kind of quiz to find out if you could have depression or stress or both. Having both is very common. Every woman in MIHP takes this quiz. If she gets a moderate or high score on the quiz, she may be experiencing depression. • Almost HALF of all women in MIHP score moderate or high. That’s A LOT of women. This percentage is about the same across the US for low-income women with young children. 86
Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • Those 14 questions about how you felt around the time that you signed up for MIHP were a kind of quiz to find out if you could have depression or stress or both. Having both is very common. Every woman in MIHP takes this quiz. If she gets a moderate or high score on the quiz, she may be experiencing depression. • Almost HALF of all women in MIHP score moderate or high. That’s A LOT of women. This percentage is about the same across the US for low-income women with young children. 86
 Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • It makes perfect sense when you think about it. It’s very hard to raise a family when you don’t have enough money to make ends meet because you can’t find a decent job, especially if you are a single mom and you aren’t getting much support from other people, and you’re worried about keeping your children safe. No wonder so many women experience depression and stress. 87
Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • It makes perfect sense when you think about it. It’s very hard to raise a family when you don’t have enough money to make ends meet because you can’t find a decent job, especially if you are a single mom and you aren’t getting much support from other people, and you’re worried about keeping your children safe. No wonder so many women experience depression and stress. 87
 Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • Your score tells us that you may be experiencing depression, stress, or both, so it’s important for you (and your baby) that we explore this further so you can decide what to do about it. We’ll work together and figure out best way for you. 88
Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • Your score tells us that you may be experiencing depression, stress, or both, so it’s important for you (and your baby) that we explore this further so you can decide what to do about it. We’ll work together and figure out best way for you. 88
 Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • Depression makes people feel really weighed down or stressed out or both. The good news: it’s very treatable. Medications work and so does counseling. Your doctor or a mental health person can do an assessment to see if you really do have depression or stress or both. You can find out about your medication and counseling options. You can feel better, so you can be the mom you want to be. 89
Talking with a Woman about Mod/Hi EPDS or Hi PSS 4 Score • Depression makes people feel really weighed down or stressed out or both. The good news: it’s very treatable. Medications work and so does counseling. Your doctor or a mental health person can do an assessment to see if you really do have depression or stress or both. You can find out about your medication and counseling options. You can feel better, so you can be the mom you want to be. 89
 Moderate Risk Intervention 6 Discuss treatment options for treating depression (e. g. , meds, CMH, clinics, private providers, support groups, IMH Specialist). • • • Primary Care Provider or OB CMH (serious mental illness only) Medicaid HP (20 OP visits/yr for mild-mod disorder) Federally Qualified Health Center (FQHC) Private counseling agencies (e. g. , Child & Family Serv) Other (e. g. , hospital or university-based depression clinic) 90
Moderate Risk Intervention 6 Discuss treatment options for treating depression (e. g. , meds, CMH, clinics, private providers, support groups, IMH Specialist). • • • Primary Care Provider or OB CMH (serious mental illness only) Medicaid HP (20 OP visits/yr for mild-mod disorder) Federally Qualified Health Center (FQHC) Private counseling agencies (e. g. , Child & Family Serv) Other (e. g. , hospital or university-based depression clinic) 90
 Support Services • Discuss support services options for dealing with depression: – Depression support groups (e. g. , Postpartum Support International) – Other support groups (e. g. , anxiety, bereavement , etc. ) – Online support groups and communities – Web sites • See MIHP Perinatal Depression Resources for Consumers and Health Care Providers on web site 91
Support Services • Discuss support services options for dealing with depression: – Depression support groups (e. g. , Postpartum Support International) – Other support groups (e. g. , anxiety, bereavement , etc. ) – Online support groups and communities – Web sites • See MIHP Perinatal Depression Resources for Consumers and Health Care Providers on web site 91
 Moderate Risk Intervention 7 Refer for evaluation and treatment: – CMH – HP or PCP – Support Group – MIHP IMH Specialist Explain that it may take a while for treatment to work. 92
Moderate Risk Intervention 7 Refer for evaluation and treatment: – CMH – HP or PCP – Support Group – MIHP IMH Specialist Explain that it may take a while for treatment to work. 92
 If Beneficiary Has Been a CMH Client in the Past • Refer to CMH if beneficiary was previously served there. • If she refuses to return to CMH, get a release of information from her so you can discuss her status with her CMH worker. 93
If Beneficiary Has Been a CMH Client in the Past • Refer to CMH if beneficiary was previously served there. • If she refuses to return to CMH, get a release of information from her so you can discuss her status with her CMH worker. 93
 If a Woman Declines to Seek Treatment • If woman declines to seek treatment or a support group, consider using some of the ideas in the next few slides. • If she still declines, ask if she would at least be willing to keep her mind open and think about it some more. • It’s your decision, of course, but I really hope you will think about it because I’m concerned about you and want the best for you and baby. 94
If a Woman Declines to Seek Treatment • If woman declines to seek treatment or a support group, consider using some of the ideas in the next few slides. • If she still declines, ask if she would at least be willing to keep her mind open and think about it some more. • It’s your decision, of course, but I really hope you will think about it because I’m concerned about you and want the best for you and baby. 94
 Encouraging a Woman to Seek Treatment Some things you could say: • Explain that a family member or friend who says “get over it” doesn’t understand what depression is. • Ask her: If you had a friend who was depressed, what would you tell her? (Low-income women in focus groups said: “Think about the child - your kids shouldn’t suffer because of what you’re going through. ”) • Talk about how depression can make it harder for her to achieve her goals for herself and family. 95
Encouraging a Woman to Seek Treatment Some things you could say: • Explain that a family member or friend who says “get over it” doesn’t understand what depression is. • Ask her: If you had a friend who was depressed, what would you tell her? (Low-income women in focus groups said: “Think about the child - your kids shouldn’t suffer because of what you’re going through. ”) • Talk about how depression can make it harder for her to achieve her goals for herself and family. 95
 Encouraging a Woman to Seek Treatment More things you could say: (26) • “Mental illness, ” “mental disorder, ” and “behavioral disorder” are outdated terms. • New research: Depression is a brain circuit disorder. • People with depression aren’t “mentally ill” or “crazy” or “losing their minds” – their brains are “wired” differently. • A brain circuit disorder is a real physical condition. • Early treatment is always better. 96
Encouraging a Woman to Seek Treatment More things you could say: (26) • “Mental illness, ” “mental disorder, ” and “behavioral disorder” are outdated terms. • New research: Depression is a brain circuit disorder. • People with depression aren’t “mentally ill” or “crazy” or “losing their minds” – their brains are “wired” differently. • A brain circuit disorder is a real physical condition. • Early treatment is always better. 96
 Encouraging a Woman to Seek Treatment More things you could say: • Depression is a real physical problem. – It messes with your body, not just your emotions. – It’s like a broken arm, except it can’t be fixed with a cast. – It’s not going to go away by itself in a few days, like a cold does. • Many celebrities have had postpartum depression: Jennifer Lopez, Halle Berry, Gwyneth Paltrow, Courtney Cox, Bryce Dallas Howard, Brooke Shields, etc. They talk about it publicly because they want other women to know they aren’t alone, don’t need to suffer in silence, and treatment works. 97
Encouraging a Woman to Seek Treatment More things you could say: • Depression is a real physical problem. – It messes with your body, not just your emotions. – It’s like a broken arm, except it can’t be fixed with a cast. – It’s not going to go away by itself in a few days, like a cold does. • Many celebrities have had postpartum depression: Jennifer Lopez, Halle Berry, Gwyneth Paltrow, Courtney Cox, Bryce Dallas Howard, Brooke Shields, etc. They talk about it publicly because they want other women to know they aren’t alone, don’t need to suffer in silence, and treatment works. 97
 Moderate Risk Intervention 8 Re-evaluate risk later in pregnancy or postpartum (recommend re-administer the EPDS and PSS 4) and encourage beneficiary to seek treatment, if indicated. – Re-administer at any time you feel it’s appropriate. – If applicable, change and date POC 2. – EPDS and PSS 4 are on web site, separate from Risk Identifier. 98
Moderate Risk Intervention 8 Re-evaluate risk later in pregnancy or postpartum (recommend re-administer the EPDS and PSS 4) and encourage beneficiary to seek treatment, if indicated. – Re-administer at any time you feel it’s appropriate. – If applicable, change and date POC 2. – EPDS and PSS 4 are on web site, separate from Risk Identifier. 98
 Moderate Risk Intervention 9 Provide support and encouragement in adhering to mental health provider treatment recommendations including psychotropic medication and/or counseling. 99
Moderate Risk Intervention 9 Provide support and encouragement in adhering to mental health provider treatment recommendations including psychotropic medication and/or counseling. 99
 Moderate Risk Intervention 10 Discuss medication schedule and importance of taking medication as prescribed. 100
Moderate Risk Intervention 10 Discuss medication schedule and importance of taking medication as prescribed. 100
 Moderate Risk Intervention 11 Prepare postpartum support plan. How will you address stress and depression after your baby is born? 101
Moderate Risk Intervention 11 Prepare postpartum support plan. How will you address stress and depression after your baby is born? 101
 High Risk Intervention 12 Ask if beneficiary has suicidal ideation, plan or intent. 102
High Risk Intervention 12 Ask if beneficiary has suicidal ideation, plan or intent. 102
 High Risk Intervention 13 Develop and document emergency safety plan. – Discuss how mom, infant and other family members will stay safe. – Document this discussion. 103
High Risk Intervention 13 Develop and document emergency safety plan. – Discuss how mom, infant and other family members will stay safe. – Document this discussion. 103
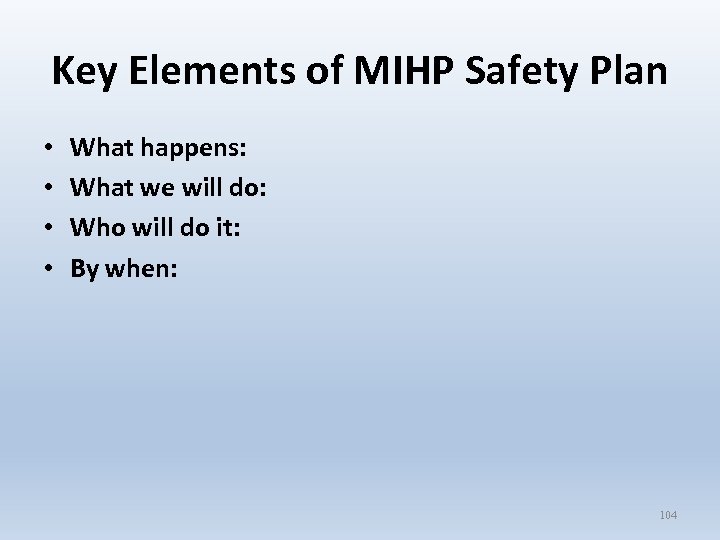 Key Elements of MIHP Safety Plan • • What happens: What we will do: Who will do it: By when: 104
Key Elements of MIHP Safety Plan • • What happens: What we will do: Who will do it: By when: 104
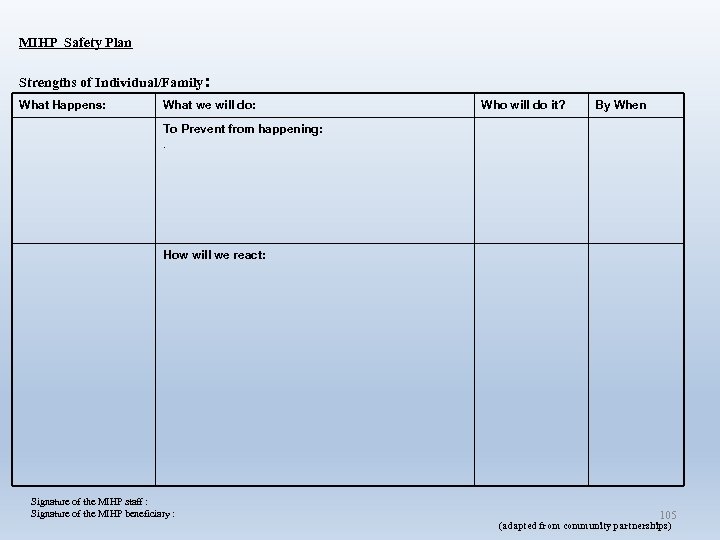 MIHP Safety Plan Strengths of Individual/Family: What Happens: What we will do: Who will do it? By When To Prevent from happening: . How will we react: Signature of the MIHP staff : Signature of the MIHP beneficiary : 105 (adapted from community partnerships)
MIHP Safety Plan Strengths of Individual/Family: What Happens: What we will do: Who will do it? By When To Prevent from happening: . How will we react: Signature of the MIHP staff : Signature of the MIHP beneficiary : 105 (adapted from community partnerships)
 Emergency Intervention 14 Assist in going to nearest Emergency Department. 106
Emergency Intervention 14 Assist in going to nearest Emergency Department. 106
 Emergency Intervention 15 Call 911. 107
Emergency Intervention 15 Call 911. 107
 Emergency Intervention 16 Inform MHP and medical care provider. 108
Emergency Intervention 16 Inform MHP and medical care provider. 108
 Demonstrations: Discussing Depression with Beneficiaries SW: Rebecca Wheeler, Consultant/Trainer, MDCH Vignette 1 Non-talkative mother (Joni) of 3 -mo old boy (Tommy); no partner; lives with mom. Joni Detwiler, MDCH Vignette 2 Talkative mother (Brenda) of 6 -mo old girl (Jasmine); lives with partner; no family support. Brenda Jegede, MDCH NOTE: V 2 picks up where V 1 leaves off; beneficiary is different to reflect varying communication styles and family situations 109
Demonstrations: Discussing Depression with Beneficiaries SW: Rebecca Wheeler, Consultant/Trainer, MDCH Vignette 1 Non-talkative mother (Joni) of 3 -mo old boy (Tommy); no partner; lives with mom. Joni Detwiler, MDCH Vignette 2 Talkative mother (Brenda) of 6 -mo old girl (Jasmine); lives with partner; no family support. Brenda Jegede, MDCH NOTE: V 2 picks up where V 1 leaves off; beneficiary is different to reflect varying communication styles and family situations 109
 ACCESSING MENTAL HEALTH TREATMENT AND SUPPORT SERVICES IN YOUR COMMUNITY 110
ACCESSING MENTAL HEALTH TREATMENT AND SUPPORT SERVICES IN YOUR COMMUNITY 110
 It’s All About Relationships • You must have strong relationships with key referral sources in order to provide quality care coordination. • Especially true in MH domain because beneficiaries are reluctant to use MH services and knowing how to access services can be difficult. 111
It’s All About Relationships • You must have strong relationships with key referral sources in order to provide quality care coordination. • Especially true in MH domain because beneficiaries are reluctant to use MH services and knowing how to access services can be difficult. 111
 Helping Beneficiary Navigate MHP Mental Health Services • Call the MHP MIHP contact person (see list on web site), who is responsible for assisting MHP members to access services. • If this does not work out for the beneficiary, inform your consultant. • If beneficiary can’t access services, explore other options. 112
Helping Beneficiary Navigate MHP Mental Health Services • Call the MHP MIHP contact person (see list on web site), who is responsible for assisting MHP members to access services. • If this does not work out for the beneficiary, inform your consultant. • If beneficiary can’t access services, explore other options. 112
 Helping Beneficiary Navigate CMH Services • If you already have a CMH contact, work through him or her. • If not, see: – CMH Contacts for Mental Health Services for Infants and their Families (including Infant Mental Health) – Using CMH Contacts to Navigate Mental Health Services for MIHP Infants and Their Families – Possible Reasons for Referral to an MIHP Infant Mental Health Specialist or to CMH for an Assessment 113
Helping Beneficiary Navigate CMH Services • If you already have a CMH contact, work through him or her. • If not, see: – CMH Contacts for Mental Health Services for Infants and their Families (including Infant Mental Health) – Using CMH Contacts to Navigate Mental Health Services for MIHP Infants and Their Families – Possible Reasons for Referral to an MIHP Infant Mental Health Specialist or to CMH for an Assessment 113
 Other Options if Beneficiary Declines MHP, PCP, CMH Services • If beneficiary does not wish to seek MH services through her MHP, primary care provider/OB or CMH, look for other options. • See MIHP web site for: MIHP Perinatal Depression Resources for Consumers and Health Care Providers • Connect her with groups (parent groups, faith-based groups, etc. ) that are not stigmatizing. 114
Other Options if Beneficiary Declines MHP, PCP, CMH Services • If beneficiary does not wish to seek MH services through her MHP, primary care provider/OB or CMH, look for other options. • See MIHP web site for: MIHP Perinatal Depression Resources for Consumers and Health Care Providers • Connect her with groups (parent groups, faith-based groups, etc. ) that are not stigmatizing. 114
 References 1. Findings Magazine, Fall/Winter 2005, Volume 21, Number 1, University of Michigan School of Public Health 2. National Institute of Mental Health 3. Ibid. 4. Wisner KL, Sit DK, Mc. Shea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013; doi: 10. 1001/JAMA Psychiatry, 2013. 87. 5. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 6. Leis JA, Mendelson T, Perry DF, Tandon D. Perceptions of mental health services among low-income, perinatal African American women. Women’s Health Issues. 2011; 21: 314 -319 7. Ammerman T, Putnam F, Bosse N, Teeters A, Van Ginkel J. Maternal depression in home visitation: A systematic review. Aggression and Violent Behavior 15: 191 -200. 8. Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. Journal of Women’s Health. 2003 May; 12(4): 373 -380. 9. Ibid. 10. Wisner KL, Sit DK, Mc. Shea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013; doi: 1001/JAMA Psychiatry, 2013. 87. 115
References 1. Findings Magazine, Fall/Winter 2005, Volume 21, Number 1, University of Michigan School of Public Health 2. National Institute of Mental Health 3. Ibid. 4. Wisner KL, Sit DK, Mc. Shea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013; doi: 10. 1001/JAMA Psychiatry, 2013. 87. 5. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 6. Leis JA, Mendelson T, Perry DF, Tandon D. Perceptions of mental health services among low-income, perinatal African American women. Women’s Health Issues. 2011; 21: 314 -319 7. Ammerman T, Putnam F, Bosse N, Teeters A, Van Ginkel J. Maternal depression in home visitation: A systematic review. Aggression and Violent Behavior 15: 191 -200. 8. Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. Journal of Women’s Health. 2003 May; 12(4): 373 -380. 9. Ibid. 10. Wisner KL, Sit DK, Mc. Shea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013; doi: 1001/JAMA Psychiatry, 2013. 87. 115
 References (continued) 11. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 12. Ibid. 13. Ibid. 14. Ibid. 15. Minkovitz C, Strobino D, Scharfstein D, et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics Vol. 115 No. 2 pp 306 -314 (doi: 10. 1542/peds. 2004 -0341) 16. Knitzer J, Theberge S, Johnson K. Reducing Maternal Depression and its Impact on Young Children: Toward a Responsive Early Childhood Policy Framework. National Center for Children and Poverty, Project Thrive, Issue Brief 2. 17. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 18. Jason Goldman, Science. Blogs. LLC, October 18, 2010 19. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 20. Pooler J, Perry D, Ghandour R. (2013). Prevanlence and risk factors for postpartum depressive symptoms among women enrolled in WIC. Maternal and Child Health Journal. Advance online publication. doi: 10. 1007/s 109956 -013 -1224 -y. 116
References (continued) 11. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 12. Ibid. 13. Ibid. 14. Ibid. 15. Minkovitz C, Strobino D, Scharfstein D, et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics Vol. 115 No. 2 pp 306 -314 (doi: 10. 1542/peds. 2004 -0341) 16. Knitzer J, Theberge S, Johnson K. Reducing Maternal Depression and its Impact on Young Children: Toward a Responsive Early Childhood Policy Framework. National Center for Children and Poverty, Project Thrive, Issue Brief 2. 17. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 18. Jason Goldman, Science. Blogs. LLC, October 18, 2010 19. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans, NIHCM Foundation Issue Brief, June 2010 20. Pooler J, Perry D, Ghandour R. (2013). Prevanlence and risk factors for postpartum depressive symptoms among women enrolled in WIC. Maternal and Child Health Journal. Advance online publication. doi: 10. 1007/s 109956 -013 -1224 -y. 116
 Referenced (continued) 21. Tandon SD, Parillo KM, Jenkins C, Duggan AK. Formative evaluation of home visitors’ role in addressing poor mental health, domestic violence, and substance abuse among low-income pregnant and parenting women. Maternal and Child Health. 2005; 9: 273 -283. 22. Ibid. 23. National Association of State Mental Health Programs Directors, 2004. 24. Jennings, A. Models for Developing Trauma-Informed Behavioral Health Systems and Trauma-Specific Services. 2004. 25. Spectrum Health Women’s Services web site 26. Thomas Insel, Mental Disorders as Brain Disorders at TEDx. Caltech, Feb. 8, 2013 117
Referenced (continued) 21. Tandon SD, Parillo KM, Jenkins C, Duggan AK. Formative evaluation of home visitors’ role in addressing poor mental health, domestic violence, and substance abuse among low-income pregnant and parenting women. Maternal and Child Health. 2005; 9: 273 -283. 22. Ibid. 23. National Association of State Mental Health Programs Directors, 2004. 24. Jennings, A. Models for Developing Trauma-Informed Behavioral Health Systems and Trauma-Specific Services. 2004. 25. Spectrum Health Women’s Services web site 26. Thomas Insel, Mental Disorders as Brain Disorders at TEDx. Caltech, Feb. 8, 2013 117
 118
118
 119
119


