3a9e161cdbbcea96796b86c330bcf245.ppt
- Количество слайдов: 35
 Implementation Support Pack 6 th March 2008 The objective of this pack is to provide a summary of key materials to support SHA Flu Leads, PCT Flu Co-ordinators and key contacts in Acute and Mental Health trusts with Pandemic Flu Preparedness work Note: Information is correct at the time of publishing. The programme will endeavour to update documentation regularly, however if you have any queries relating to the content of this document please email: pandemicflu@dh. gsi. gov. uk This document is not in the public domain. Please restrict circulation to those involved with flu planning. Assurance Strategy and Audit
Implementation Support Pack 6 th March 2008 The objective of this pack is to provide a summary of key materials to support SHA Flu Leads, PCT Flu Co-ordinators and key contacts in Acute and Mental Health trusts with Pandemic Flu Preparedness work Note: Information is correct at the time of publishing. The programme will endeavour to update documentation regularly, however if you have any queries relating to the content of this document please email: pandemicflu@dh. gsi. gov. uk This document is not in the public domain. Please restrict circulation to those involved with flu planning. Assurance Strategy and Audit
 An Introduction to Pandemic Flu • Influenza pandemics are natural phenomena that have occurred three times in the last century. "Most experts believe that it is not a question of whethere will be another severe influenza pandemic but when” Chief Medical Officer 2002. • It is recognised that the likelihood of a high pathogenic human influenza virus, capable of causing a pandemic, evolving in the near term is real but unquantifiable. • This unquantifiable probability must be set against the possible huge impact of a pandemic. In the worst case a pandemic would have a massive impact, with many millions of people worldwide becoming ill and a proportion of these dying. In the UK this could mean up to half the population may become ill and up to 750, 000 additional deaths. • A pandemic will impact on all aspects of UK society. In the worst case scenario, with no interventions taken, the possible cumulative costs of a pandemic to society have been estimated to be up to £ 1, 242 billion. • The World Health Organization (WHO) currently advise that, out of six levels of alert, we are in the pandemic alert period at phase 3, where there are human infections with a new type of virus, but there is not efficient and sustained transmission from person to person. Phase 6 would be the start of a pandemic. • As a pandemic flu virus has yet to emerge, we do not know how infectious it will be, or the severity of the illness it will cause. We do know that it is likely to take only a few weeks between a pandemic virus emerging somewhere in the world and it reaching the UK, and that it will spread quickly to all parts of the UK. As it will be too late to secure stocks of countermeasures once the pandemic virus has emerged, we need to allow some time to procure stocks and to ensure a response strategy can be implemented in the NHS. Therefore, decisions need to be taken in the pandemic alert period, before a pandemic emerges. This is supported by the WHO state “in view of the immediacy of the threat, WHO recommends that all countries undertake urgent action to prepare for a pandemic”*. *Responding to the avian influenza pandemic threat. Recommended strategic actions. WHO. Page 1 Page │ 1
An Introduction to Pandemic Flu • Influenza pandemics are natural phenomena that have occurred three times in the last century. "Most experts believe that it is not a question of whethere will be another severe influenza pandemic but when” Chief Medical Officer 2002. • It is recognised that the likelihood of a high pathogenic human influenza virus, capable of causing a pandemic, evolving in the near term is real but unquantifiable. • This unquantifiable probability must be set against the possible huge impact of a pandemic. In the worst case a pandemic would have a massive impact, with many millions of people worldwide becoming ill and a proportion of these dying. In the UK this could mean up to half the population may become ill and up to 750, 000 additional deaths. • A pandemic will impact on all aspects of UK society. In the worst case scenario, with no interventions taken, the possible cumulative costs of a pandemic to society have been estimated to be up to £ 1, 242 billion. • The World Health Organization (WHO) currently advise that, out of six levels of alert, we are in the pandemic alert period at phase 3, where there are human infections with a new type of virus, but there is not efficient and sustained transmission from person to person. Phase 6 would be the start of a pandemic. • As a pandemic flu virus has yet to emerge, we do not know how infectious it will be, or the severity of the illness it will cause. We do know that it is likely to take only a few weeks between a pandemic virus emerging somewhere in the world and it reaching the UK, and that it will spread quickly to all parts of the UK. As it will be too late to secure stocks of countermeasures once the pandemic virus has emerged, we need to allow some time to procure stocks and to ensure a response strategy can be implemented in the NHS. Therefore, decisions need to be taken in the pandemic alert period, before a pandemic emerges. This is supported by the WHO state “in view of the immediacy of the threat, WHO recommends that all countries undertake urgent action to prepare for a pandemic”*. *Responding to the avian influenza pandemic threat. Recommended strategic actions. WHO. Page 1 Page │ 1
 Useful reference documents There are two useful reference documents that help build an understanding of the subject of pandemic flu. Pandemic Flu Frequently Asked Questions To open double click on the icon below Pandemic Flu Key Facts To open double click on the box below Page │ 2
Useful reference documents There are two useful reference documents that help build an understanding of the subject of pandemic flu. Pandemic Flu Frequently Asked Questions To open double click on the icon below Pandemic Flu Key Facts To open double click on the box below Page │ 2
 The programme’s intervention strategy is based on the need for ‘defence in depth’. This strategy aims to • Reduce amount of illness caused by pandemic flu • Reduce number of deaths which result from pandemic flu • Manage the increased pressure on the NHS and Social Care Services The programme is building up capability in several areas to deliver to the above programme objectives • Clinical countermeasure stockpiles are being built up e. g. Antivirals, antibiotics, face masks etc • Infrastructure to deliver the pandemic response across the NHS and Social care is being built e. g. the national flu line service, surveillance mechanisms • Processes are being put in place to ensure the right information is available to inform management of a pandemic emergency situation, such as identifying key information required by Ministers • Public preparation and confidence is being built up through a public health and hygiene campaign • A programme of public engagement is testing how the public will respond to proposed policy The programme is also helping the NHS and the Social Care field prepare • Health and social care service planning and preparation work is underway in the NHS The programme is also liaising with the wider business continuity work being undertaken by the Department, in the Emergency Preparedness Division Page │ 3
The programme’s intervention strategy is based on the need for ‘defence in depth’. This strategy aims to • Reduce amount of illness caused by pandemic flu • Reduce number of deaths which result from pandemic flu • Manage the increased pressure on the NHS and Social Care Services The programme is building up capability in several areas to deliver to the above programme objectives • Clinical countermeasure stockpiles are being built up e. g. Antivirals, antibiotics, face masks etc • Infrastructure to deliver the pandemic response across the NHS and Social care is being built e. g. the national flu line service, surveillance mechanisms • Processes are being put in place to ensure the right information is available to inform management of a pandemic emergency situation, such as identifying key information required by Ministers • Public preparation and confidence is being built up through a public health and hygiene campaign • A programme of public engagement is testing how the public will respond to proposed policy The programme is also helping the NHS and the Social Care field prepare • Health and social care service planning and preparation work is underway in the NHS The programme is also liaising with the wider business continuity work being undertaken by the Department, in the Emergency Preparedness Division Page │ 3
 Summary of outputs from the Programme Guidance Position on countermeasures Communications and training materials Contact details Assurance Strategy and Audit
Summary of outputs from the Programme Guidance Position on countermeasures Communications and training materials Contact details Assurance Strategy and Audit
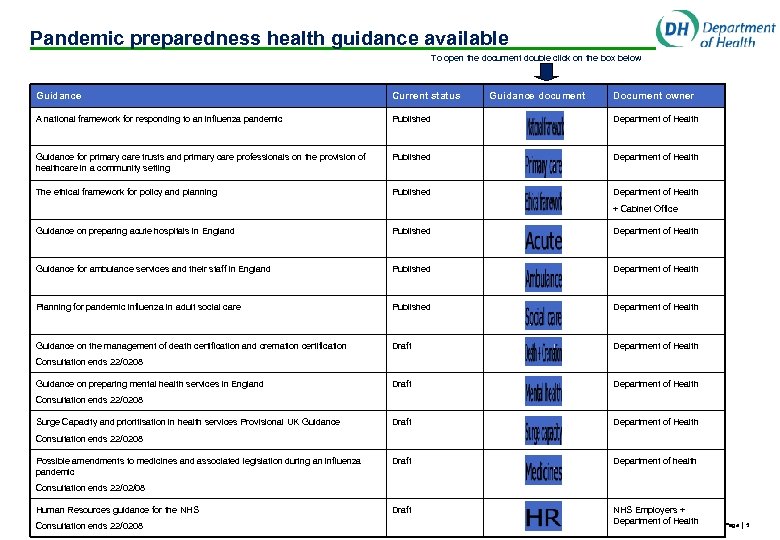 Pandemic preparedness health guidance available To open the document double click on the box below Guidance Current status Guidance document Document owner A national framework for responding to an influenza pandemic Published Department of Health Guidance for primary care trusts and primary care professionals on the provision of healthcare in a community setting Published Department of Health The ethical framework for policy and planning Published Department of Health + Cabinet Office Guidance on preparing acute hospitals in England Published Department of Health Guidance for ambulance services and their staff in England Published Department of Health Planning for pandemic influenza in adult social care Published Department of Health Guidance on the management of death certification and cremation certification Draft Department of Health Draft Department of health Draft NHS Employers + Department of Health Consultation ends 22/0208 Guidance on preparing mental health services in England Consultation ends 22/0208 Surge Capacity and prioritisation in health services Provisional UK Guidance Consultation ends 22/0208 Possible amendments to medicines and associated legislation during an influenza pandemic Consultation ends 22/02/08 Human Resources guidance for the NHS Consultation ends 22/0208 Page │ 5
Pandemic preparedness health guidance available To open the document double click on the box below Guidance Current status Guidance document Document owner A national framework for responding to an influenza pandemic Published Department of Health Guidance for primary care trusts and primary care professionals on the provision of healthcare in a community setting Published Department of Health The ethical framework for policy and planning Published Department of Health + Cabinet Office Guidance on preparing acute hospitals in England Published Department of Health Guidance for ambulance services and their staff in England Published Department of Health Planning for pandemic influenza in adult social care Published Department of Health Guidance on the management of death certification and cremation certification Draft Department of Health Draft Department of health Draft NHS Employers + Department of Health Consultation ends 22/0208 Guidance on preparing mental health services in England Consultation ends 22/0208 Surge Capacity and prioritisation in health services Provisional UK Guidance Consultation ends 22/0208 Possible amendments to medicines and associated legislation during an influenza pandemic Consultation ends 22/02/08 Human Resources guidance for the NHS Consultation ends 22/0208 Page │ 5
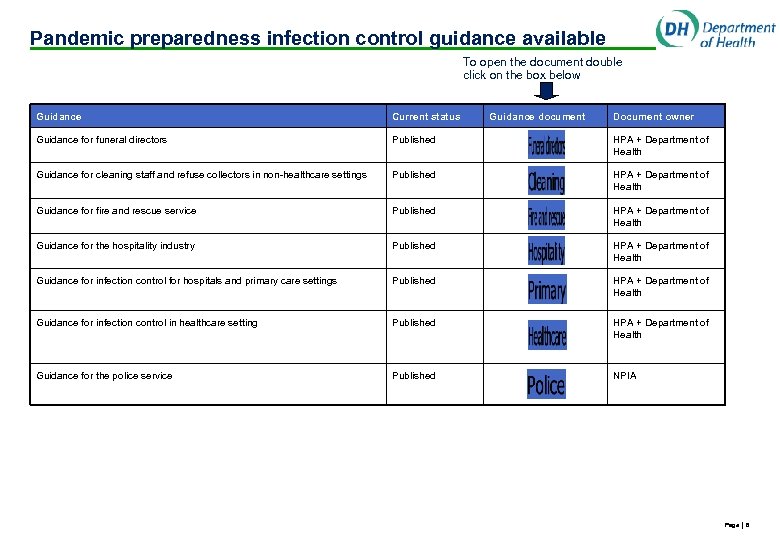 Pandemic preparedness infection control guidance available To open the document double click on the box below Guidance Current status Guidance document Document owner Guidance for funeral directors Published HPA + Department of Health Guidance for cleaning staff and refuse collectors in non-healthcare settings Published HPA + Department of Health Guidance for fire and rescue service Published HPA + Department of Health Guidance for the hospitality industry Published HPA + Department of Health Guidance for infection control for hospitals and primary care settings Published HPA + Department of Health Guidance for infection control in healthcare setting Published HPA + Department of Health Guidance for the police service Published NPIA Page │ 6
Pandemic preparedness infection control guidance available To open the document double click on the box below Guidance Current status Guidance document Document owner Guidance for funeral directors Published HPA + Department of Health Guidance for cleaning staff and refuse collectors in non-healthcare settings Published HPA + Department of Health Guidance for fire and rescue service Published HPA + Department of Health Guidance for the hospitality industry Published HPA + Department of Health Guidance for infection control for hospitals and primary care settings Published HPA + Department of Health Guidance for infection control in healthcare setting Published HPA + Department of Health Guidance for the police service Published NPIA Page │ 6
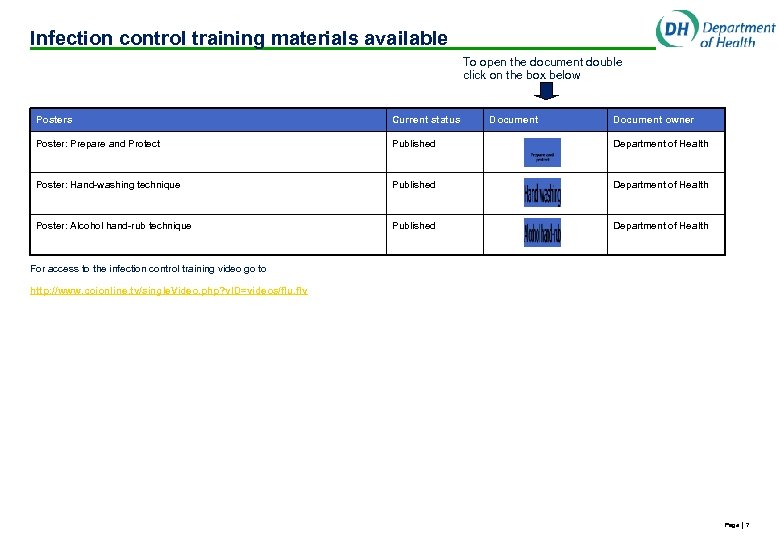 Infection control training materials available To open the document double click on the box below Posters Current status Document owner Poster: Prepare and Protect Published Department of Health Poster: Hand-washing technique Published Department of Health Poster: Alcohol hand-rub technique Published Department of Health For access to the infection control training video go to http: //www. coionline. tv/single. Video. php? v. ID=videos/flu. flv Page │ 7
Infection control training materials available To open the document double click on the box below Posters Current status Document owner Poster: Prepare and Protect Published Department of Health Poster: Hand-washing technique Published Department of Health Poster: Alcohol hand-rub technique Published Department of Health For access to the infection control training video go to http: //www. coionline. tv/single. Video. php? v. ID=videos/flu. flv Page │ 7
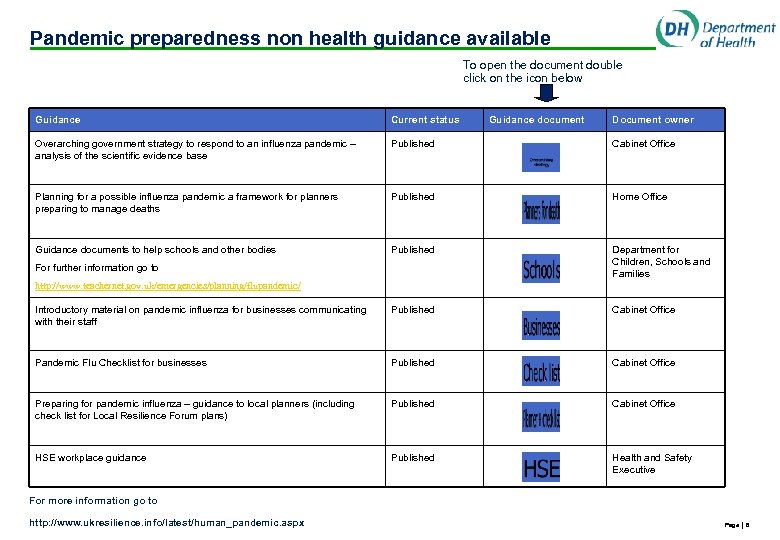 Pandemic preparedness non health guidance available To open the document double click on the icon below Guidance Current status Overarching government strategy to respond to an influenza pandemic – analysis of the scientific evidence base Published Cabinet Office Planning for a possible influenza pandemic a framework for planners preparing to manage deaths Published Home Office Guidance documents to help schools and other bodies Published Department for Children, Schools and Families Introductory material on pandemic influenza for businesses communicating with their staff Published Cabinet Office Pandemic Flu Checklist for businesses Published Cabinet Office Preparing for pandemic influenza – guidance to local planners (including check list for Local Resilience Forum plans) Published Cabinet Office HSE workplace guidance Published Health and Safety Executive For further information go to Guidance document Document owner http: //www. teachernet. gov. uk/emergencies/planning/flupandemic/ For more information go to http: //www. ukresilience. info/latest/human_pandemic. aspx Page │ 8
Pandemic preparedness non health guidance available To open the document double click on the icon below Guidance Current status Overarching government strategy to respond to an influenza pandemic – analysis of the scientific evidence base Published Cabinet Office Planning for a possible influenza pandemic a framework for planners preparing to manage deaths Published Home Office Guidance documents to help schools and other bodies Published Department for Children, Schools and Families Introductory material on pandemic influenza for businesses communicating with their staff Published Cabinet Office Pandemic Flu Checklist for businesses Published Cabinet Office Preparing for pandemic influenza – guidance to local planners (including check list for Local Resilience Forum plans) Published Cabinet Office HSE workplace guidance Published Health and Safety Executive For further information go to Guidance document Document owner http: //www. teachernet. gov. uk/emergencies/planning/flupandemic/ For more information go to http: //www. ukresilience. info/latest/human_pandemic. aspx Page │ 8
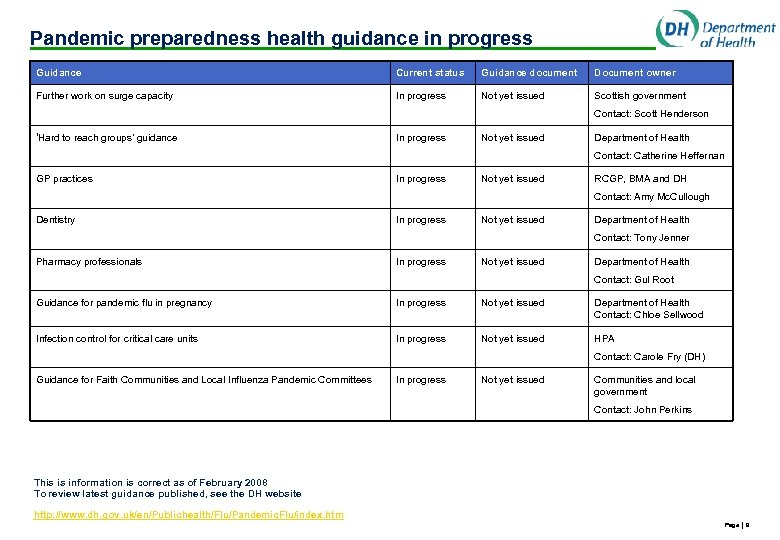 Pandemic preparedness health guidance in progress Guidance Current status Guidance document Document owner Further work on surge capacity In progress Not yet issued Scottish government Contact: Scott Henderson ‘Hard to reach groups’ guidance In progress Not yet issued Department of Health Contact: Catherine Heffernan GP practices In progress Not yet issued RCGP, BMA and DH Contact: Amy Mc. Cullough Dentistry In progress Not yet issued Department of Health Contact: Tony Jenner Pharmacy professionals In progress Not yet issued Department of Health Contact: Gul Root Guidance for pandemic flu in pregnancy In progress Not yet issued Department of Health Contact: Chloe Sellwood Infection control for critical care units In progress Not yet issued HPA Contact: Carole Fry (DH) Guidance for Faith Communities and Local Influenza Pandemic Committees In progress Not yet issued Communities and local government Contact: John Perkins This is information is correct as of February 2008 To review latest guidance published, see the DH website http: //www. dh. gov. uk/en/Publichealth/Flu/Pandemic. Flu/index. htm Page │ 9
Pandemic preparedness health guidance in progress Guidance Current status Guidance document Document owner Further work on surge capacity In progress Not yet issued Scottish government Contact: Scott Henderson ‘Hard to reach groups’ guidance In progress Not yet issued Department of Health Contact: Catherine Heffernan GP practices In progress Not yet issued RCGP, BMA and DH Contact: Amy Mc. Cullough Dentistry In progress Not yet issued Department of Health Contact: Tony Jenner Pharmacy professionals In progress Not yet issued Department of Health Contact: Gul Root Guidance for pandemic flu in pregnancy In progress Not yet issued Department of Health Contact: Chloe Sellwood Infection control for critical care units In progress Not yet issued HPA Contact: Carole Fry (DH) Guidance for Faith Communities and Local Influenza Pandemic Committees In progress Not yet issued Communities and local government Contact: John Perkins This is information is correct as of February 2008 To review latest guidance published, see the DH website http: //www. dh. gov. uk/en/Publichealth/Flu/Pandemic. Flu/index. htm Page │ 9
 Summary of key sources • Guidance published by the Department can be found http: //www. dh. gov. uk/en/Publichealth/Flu/Pandemic. Flu/index. htm • Guidance published by the Cabinet Office can be found http: //www. ukresilience. info/latest/human_pandemic. aspx • Guidance published by HPA can be found http: //www. hpa. org. uk/infections/topics_az/influenza/pandemic/default. htm • Guidance published by HSE can be found http: //www. hse. gov. uk/biosafety/diseases/pandemic. htm Page │ 10
Summary of key sources • Guidance published by the Department can be found http: //www. dh. gov. uk/en/Publichealth/Flu/Pandemic. Flu/index. htm • Guidance published by the Cabinet Office can be found http: //www. ukresilience. info/latest/human_pandemic. aspx • Guidance published by HPA can be found http: //www. hpa. org. uk/infections/topics_az/influenza/pandemic/default. htm • Guidance published by HSE can be found http: //www. hse. gov. uk/biosafety/diseases/pandemic. htm Page │ 10
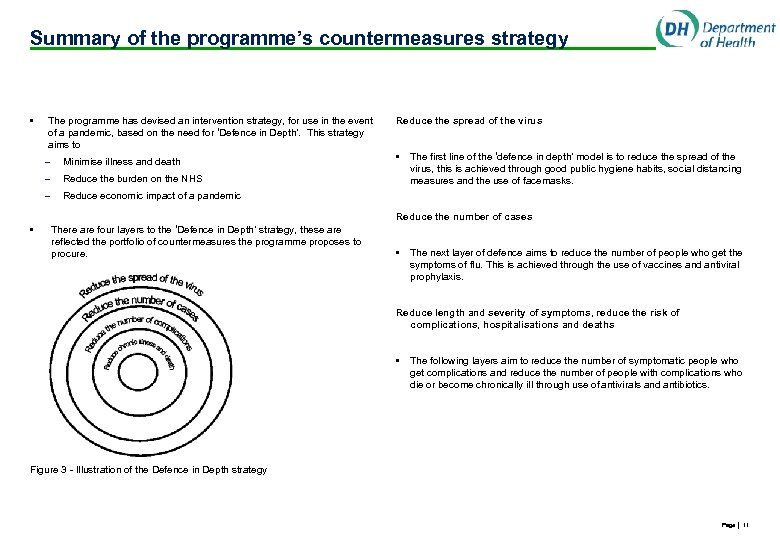 Summary of the programme’s countermeasures strategy • The programme has devised an intervention strategy, for use in the event of a pandemic, based on the need for ‘Defence in Depth’. This strategy aims to – – Reduce the burden on the NHS – • Minimise illness and death Reduce the spread of the virus • The first line of the ‘defence in depth’ model is to reduce the spread of the virus, this is achieved through good public hygiene habits, social distancing measures and the use of facemasks. Reduce economic impact of a pandemic Reduce the number of cases There are four layers to the ‘Defence in Depth’ strategy, these are reflected the portfolio of countermeasures the programme proposes to procure. • The next layer of defence aims to reduce the number of people who get the symptoms of flu. This is achieved through the use of vaccines and antiviral prophylaxis. Reduce length and severity of symptoms, reduce the risk of complications, hospitalisations and deaths • The following layers aim to reduce the number of symptomatic people who get complications and reduce the number of people with complications who die or become chronically ill through use of antivirals and antibiotics. Figure 3 - Illustration of the Defence in Depth strategy Page │ 11
Summary of the programme’s countermeasures strategy • The programme has devised an intervention strategy, for use in the event of a pandemic, based on the need for ‘Defence in Depth’. This strategy aims to – – Reduce the burden on the NHS – • Minimise illness and death Reduce the spread of the virus • The first line of the ‘defence in depth’ model is to reduce the spread of the virus, this is achieved through good public hygiene habits, social distancing measures and the use of facemasks. Reduce economic impact of a pandemic Reduce the number of cases There are four layers to the ‘Defence in Depth’ strategy, these are reflected the portfolio of countermeasures the programme proposes to procure. • The next layer of defence aims to reduce the number of people who get the symptoms of flu. This is achieved through the use of vaccines and antiviral prophylaxis. Reduce length and severity of symptoms, reduce the risk of complications, hospitalisations and deaths • The following layers aim to reduce the number of symptomatic people who get complications and reduce the number of people with complications who die or become chronically ill through use of antivirals and antibiotics. Figure 3 - Illustration of the Defence in Depth strategy Page │ 11
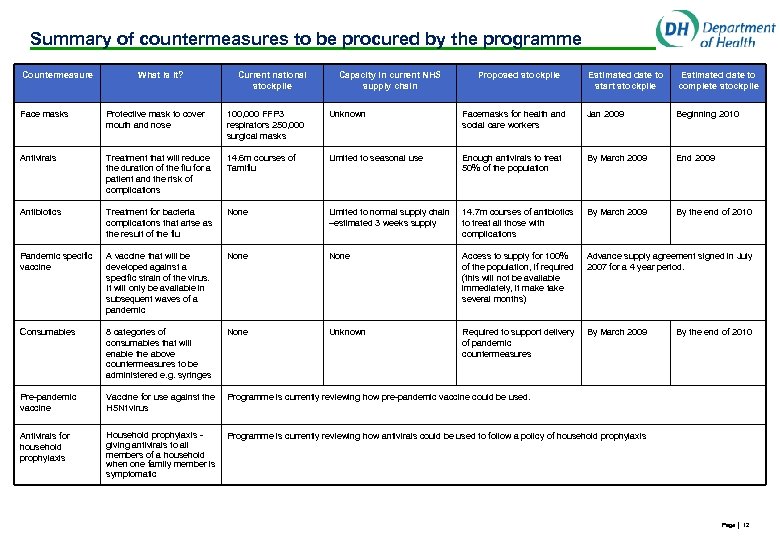 Summary of countermeasures to be procured by the programme Countermeasure What is it? Current national stockpile Capacity in current NHS supply chain Proposed stockpile Estimated date to start stockpile Estimated date to complete stockpile Face masks Protective mask to cover mouth and nose 100, 000 FFP 3 respirators 250, 000 surgical masks Unknown Facemasks for health and social care workers Jan 2009 Beginning 2010 Antivirals Treatment that will reduce the duration of the flu for a patient and the risk of complications 14. 6 m courses of Tamiflu Limited to seasonal use Enough antivirals to treat 50% of the population By March 2009 End 2009 Antibiotics Treatment for bacteria complications that arise as the result of the flu None Limited to normal supply chain –estimated 3 weeks supply 14. 7 m courses of antibiotics to treat all those with complications By March 2009 By the end of 2010 Pandemic specific vaccine A vaccine that will be developed against a specific strain of the virus. It will only be available in subsequent waves of a pandemic None Access to supply for 100% of the population, if required (this will not be available immediately, it make take several months) Advance supply agreement signed in July 2007 for a 4 year period. Consumables 8 categories of consumables that will enable the above countermeasures to be administered e. g. syringes None Unknown Required to support delivery of pandemic countermeasures By March 2009 Pre-pandemic vaccine Vaccine for use against the H 5 N 1 virus Programme is currently reviewing how pre-pandemic vaccine could be used. Antivirals for household prophylaxis Household prophylaxis giving antivirals to all members of a household when one family member is symptomatic Programme is currently reviewing how antivirals could be used to follow a policy of household prophylaxis By the end of 2010 Page │ 12
Summary of countermeasures to be procured by the programme Countermeasure What is it? Current national stockpile Capacity in current NHS supply chain Proposed stockpile Estimated date to start stockpile Estimated date to complete stockpile Face masks Protective mask to cover mouth and nose 100, 000 FFP 3 respirators 250, 000 surgical masks Unknown Facemasks for health and social care workers Jan 2009 Beginning 2010 Antivirals Treatment that will reduce the duration of the flu for a patient and the risk of complications 14. 6 m courses of Tamiflu Limited to seasonal use Enough antivirals to treat 50% of the population By March 2009 End 2009 Antibiotics Treatment for bacteria complications that arise as the result of the flu None Limited to normal supply chain –estimated 3 weeks supply 14. 7 m courses of antibiotics to treat all those with complications By March 2009 By the end of 2010 Pandemic specific vaccine A vaccine that will be developed against a specific strain of the virus. It will only be available in subsequent waves of a pandemic None Access to supply for 100% of the population, if required (this will not be available immediately, it make take several months) Advance supply agreement signed in July 2007 for a 4 year period. Consumables 8 categories of consumables that will enable the above countermeasures to be administered e. g. syringes None Unknown Required to support delivery of pandemic countermeasures By March 2009 Pre-pandemic vaccine Vaccine for use against the H 5 N 1 virus Programme is currently reviewing how pre-pandemic vaccine could be used. Antivirals for household prophylaxis Household prophylaxis giving antivirals to all members of a household when one family member is symptomatic Programme is currently reviewing how antivirals could be used to follow a policy of household prophylaxis By the end of 2010 Page │ 12
 Template for Consumables A framework of the consumable items that may be in short supply to trusts / health care providers during an influenza pandemic was drafted in Autumn 2007 and shared with SHA Flu Leads. The Department of Health is not creating a complete, comprehensive list of items that all trusts / health care providers will need. However the below list is provided as a guide to stimulate local discussion with local experts as to what items are required and in what quantities. Click the icon below to open up the consumables template Page │ 13
Template for Consumables A framework of the consumable items that may be in short supply to trusts / health care providers during an influenza pandemic was drafted in Autumn 2007 and shared with SHA Flu Leads. The Department of Health is not creating a complete, comprehensive list of items that all trusts / health care providers will need. However the below list is provided as a guide to stimulate local discussion with local experts as to what items are required and in what quantities. Click the icon below to open up the consumables template Page │ 13
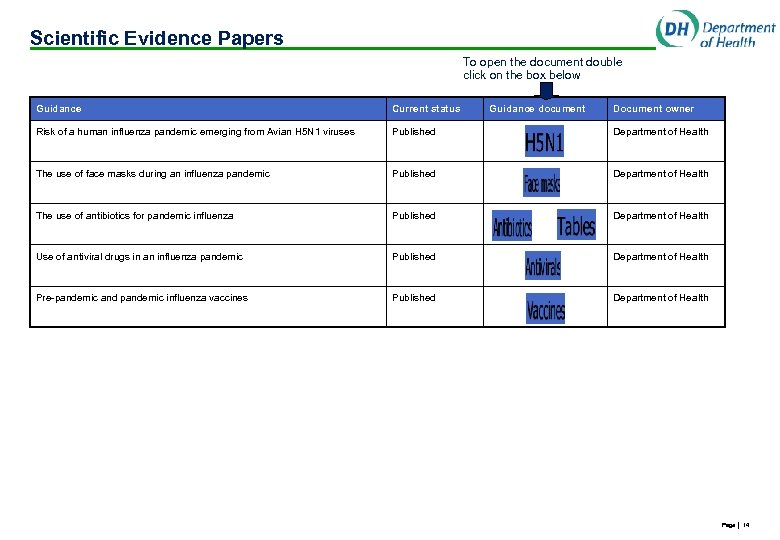 Scientific Evidence Papers To open the document double click on the box below Guidance Current status Guidance document Document owner Risk of a human influenza pandemic emerging from Avian H 5 N 1 viruses Published Department of Health The use of face masks during an influenza pandemic Published Department of Health The use of antibiotics for pandemic influenza Published Department of Health Use of antiviral drugs in an influenza pandemic Published Department of Health Pre-pandemic and pandemic influenza vaccines Published Department of Health Page │ 14
Scientific Evidence Papers To open the document double click on the box below Guidance Current status Guidance document Document owner Risk of a human influenza pandemic emerging from Avian H 5 N 1 viruses Published Department of Health The use of face masks during an influenza pandemic Published Department of Health The use of antibiotics for pandemic influenza Published Department of Health Use of antiviral drugs in an influenza pandemic Published Department of Health Pre-pandemic and pandemic influenza vaccines Published Department of Health Page │ 14
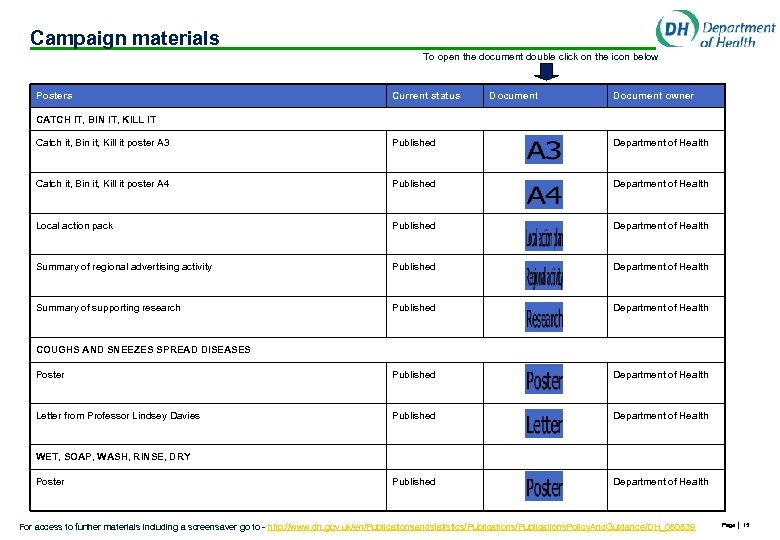 Campaign materials To open the document double click on the icon below Posters Current status Document owner CATCH IT, BIN IT, KILL IT Catch it, Bin it, Kill it poster A 3 Published Department of Health Catch it, Bin it, Kill it poster A 4 Published Department of Health Local action pack Published Department of Health Summary of regional advertising activity Published Department of Health Summary of supporting research Published Department of Health Poster Published Department of Health Letter from Professor Lindsey Davies Published Department of Health COUGHS AND SNEEZES SPREAD DISEASES WET, SOAP, WASH, RINSE, DRY Poster For access to further materials including a screensaver go to - http: //www. dh. gov. uk/en/Publicationsandstatistics/Publications. Policy. And. Guidance/DH_080839 Page │ 15
Campaign materials To open the document double click on the icon below Posters Current status Document owner CATCH IT, BIN IT, KILL IT Catch it, Bin it, Kill it poster A 3 Published Department of Health Catch it, Bin it, Kill it poster A 4 Published Department of Health Local action pack Published Department of Health Summary of regional advertising activity Published Department of Health Summary of supporting research Published Department of Health Poster Published Department of Health Letter from Professor Lindsey Davies Published Department of Health COUGHS AND SNEEZES SPREAD DISEASES WET, SOAP, WASH, RINSE, DRY Poster For access to further materials including a screensaver go to - http: //www. dh. gov. uk/en/Publicationsandstatistics/Publications. Policy. And. Guidance/DH_080839 Page │ 15
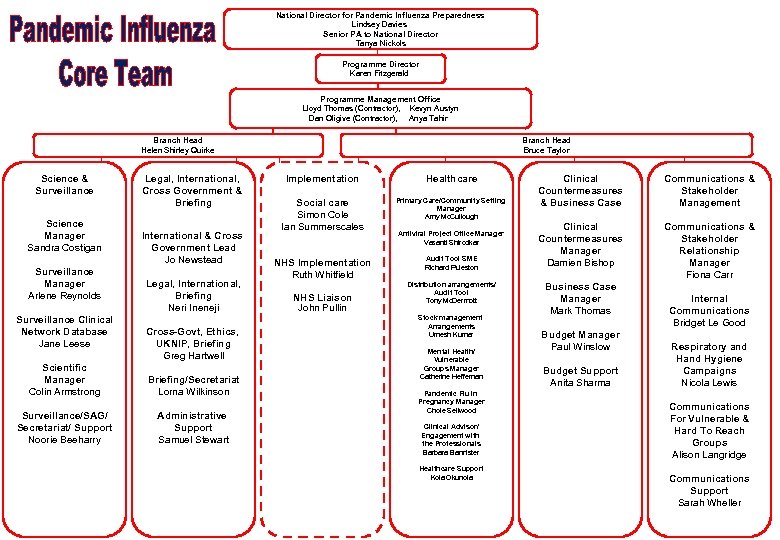 National Director for Pandemic Influenza Preparedness Lindsey Davies Senior PA to National Director Tanya Nickols Programme Director Karen Fitzgerald Programme Management Office Lloyd Thomas (Contractor), Kevyn Austyn Dan Oligive (Contractor), Anya Tahir Branch Head Bruce Taylor Branch Head Helen Shirley Quirke Science & Surveillance Science Manager Sandra Costigan Surveillance Manager Arlene Reynolds Surveillance Clinical Network Database Jane Leese Legal, International, Cross Government & Briefing International & Cross Government Lead Jo Newstead Legal, International, Briefing Neri Ineneji Cross-Govt, Ethics, UKNIP, Briefing Greg Hartwell Scientific Manager Colin Armstrong Briefing/Secretariat Lorna Wilkinson Surveillance/SAG/ Secretariat/ Support Noorie Beeharry Administrative Support Samuel Stewart Implementation Healthcare Social care Simon Cole Ian Summerscales Primary Care/Community Setting Manager Amy Mc. Cullough NHS Implementation Ruth Whitfield Audit Tool SME Richard Puleston NHS Liaison John Pullin Antiviral Project Office Manager Vasanti Shirodkar Distribution arrangements/ Audit Tool Tony Mc. Dermott Stock management Arrangements Umesh Kumar Mental Health/ Vulnerable Groups Manager Catherine Heffernan Pandemic Flu in Pregnancy Manager Chole Sellwood Clinical Advisor/ Engagement with the Professionals Barbara Bannister Healthcare Support Kola Okunola Clinical Countermeasures & Business Case Communications & Stakeholder Management Clinical Countermeasures Manager Damien Bishop Communications & Stakeholder Relationship Manager Fiona Carr Business Case Manager Mark Thomas Budget Manager Paul Winslow Budget Support Anita Sharma Internal Communications Bridget Le Good Respiratory and Hygiene Campaigns Nicola Lewis Communications For Vulnerable & Hard To Reach Groups Alison Langridge Communications Assurance Strategy Support and Sarah Wheller Audit
National Director for Pandemic Influenza Preparedness Lindsey Davies Senior PA to National Director Tanya Nickols Programme Director Karen Fitzgerald Programme Management Office Lloyd Thomas (Contractor), Kevyn Austyn Dan Oligive (Contractor), Anya Tahir Branch Head Bruce Taylor Branch Head Helen Shirley Quirke Science & Surveillance Science Manager Sandra Costigan Surveillance Manager Arlene Reynolds Surveillance Clinical Network Database Jane Leese Legal, International, Cross Government & Briefing International & Cross Government Lead Jo Newstead Legal, International, Briefing Neri Ineneji Cross-Govt, Ethics, UKNIP, Briefing Greg Hartwell Scientific Manager Colin Armstrong Briefing/Secretariat Lorna Wilkinson Surveillance/SAG/ Secretariat/ Support Noorie Beeharry Administrative Support Samuel Stewart Implementation Healthcare Social care Simon Cole Ian Summerscales Primary Care/Community Setting Manager Amy Mc. Cullough NHS Implementation Ruth Whitfield Audit Tool SME Richard Puleston NHS Liaison John Pullin Antiviral Project Office Manager Vasanti Shirodkar Distribution arrangements/ Audit Tool Tony Mc. Dermott Stock management Arrangements Umesh Kumar Mental Health/ Vulnerable Groups Manager Catherine Heffernan Pandemic Flu in Pregnancy Manager Chole Sellwood Clinical Advisor/ Engagement with the Professionals Barbara Bannister Healthcare Support Kola Okunola Clinical Countermeasures & Business Case Communications & Stakeholder Management Clinical Countermeasures Manager Damien Bishop Communications & Stakeholder Relationship Manager Fiona Carr Business Case Manager Mark Thomas Budget Manager Paul Winslow Budget Support Anita Sharma Internal Communications Bridget Le Good Respiratory and Hygiene Campaigns Nicola Lewis Communications For Vulnerable & Hard To Reach Groups Alison Langridge Communications Assurance Strategy Support and Sarah Wheller Audit
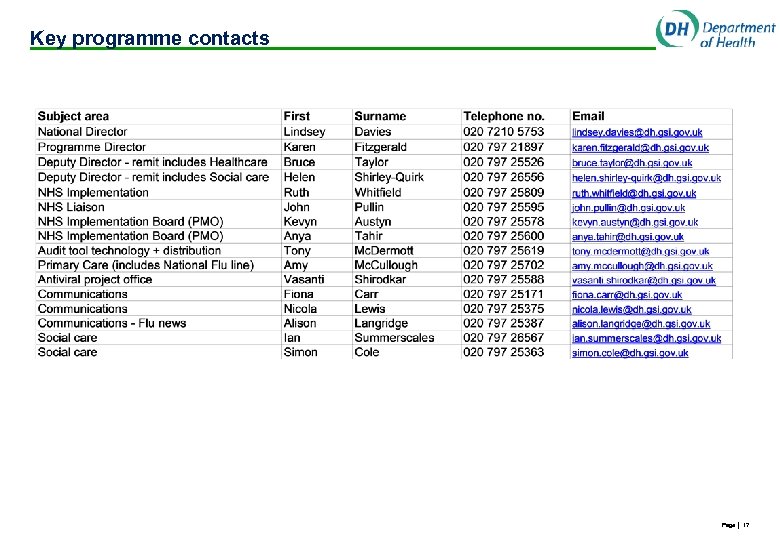 Key programme contacts Page │ 17
Key programme contacts Page │ 17
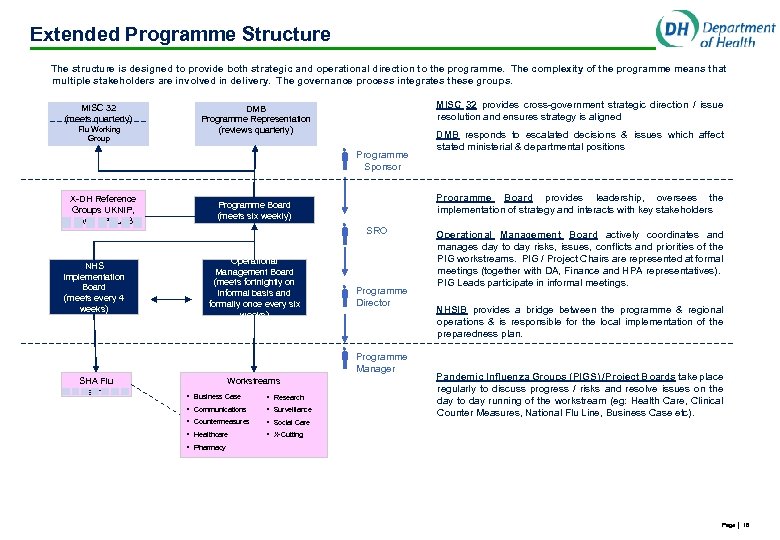 Extended Programme Structure The structure is designed to provide both strategic and operational direction to the programme. The complexity of the programme means that multiple stakeholders are involved in delivery. The governance process integrates these groups. MISC 32 (meets quarterly) Flu Working Group MISC 32 provides cross-government strategic direction / issue resolution and ensures strategy is aligned DMB Programme Representation (reviews quarterly) Programme Sponsor X-DH Reference Groups UKNIP, SAG, EPCLAG NHS Implementation Board (meets every 4 weeks) Programme Board provides leadership, oversees the implementation of strategy and interacts with key stakeholders Programme Board (meets six weekly) Operational Management Board (meets fortnightly on informal basis and formally once every six weeks) SRO Programme Director Programme Manager SHA Flu Teams Workstreams • Business Case • Research • Communications • Surveillance • Countermeasures Operational Management Board actively coordinates and manages day to day risks, issues, conflicts and priorities of the PIG workstreams. PIG / Project Chairs are represented at formal meetings (together with DA, Finance and HPA representatives). PIG Leads participate in informal meetings. NHSIB provides a bridge between the programme & regional operations & is responsible for the local implementation of the preparedness plan. Pandemic Influenza Groups (PIGS) /Project Boards take place regularly to discuss progress / risks and resolve issues on the day to day running of the workstream (eg: Health Care, Clinical Counter Measures, National Flu Line, Business Case etc). • Social Care • Healthcare DMB responds to escalated decisions & issues which affect stated ministerial & departmental positions • X-Cutting • Pharmacy Page │ 18
Extended Programme Structure The structure is designed to provide both strategic and operational direction to the programme. The complexity of the programme means that multiple stakeholders are involved in delivery. The governance process integrates these groups. MISC 32 (meets quarterly) Flu Working Group MISC 32 provides cross-government strategic direction / issue resolution and ensures strategy is aligned DMB Programme Representation (reviews quarterly) Programme Sponsor X-DH Reference Groups UKNIP, SAG, EPCLAG NHS Implementation Board (meets every 4 weeks) Programme Board provides leadership, oversees the implementation of strategy and interacts with key stakeholders Programme Board (meets six weekly) Operational Management Board (meets fortnightly on informal basis and formally once every six weeks) SRO Programme Director Programme Manager SHA Flu Teams Workstreams • Business Case • Research • Communications • Surveillance • Countermeasures Operational Management Board actively coordinates and manages day to day risks, issues, conflicts and priorities of the PIG workstreams. PIG / Project Chairs are represented at formal meetings (together with DA, Finance and HPA representatives). PIG Leads participate in informal meetings. NHSIB provides a bridge between the programme & regional operations & is responsible for the local implementation of the preparedness plan. Pandemic Influenza Groups (PIGS) /Project Boards take place regularly to discuss progress / risks and resolve issues on the day to day running of the workstream (eg: Health Care, Clinical Counter Measures, National Flu Line, Business Case etc). • Social Care • Healthcare DMB responds to escalated decisions & issues which affect stated ministerial & departmental positions • X-Cutting • Pharmacy Page │ 18
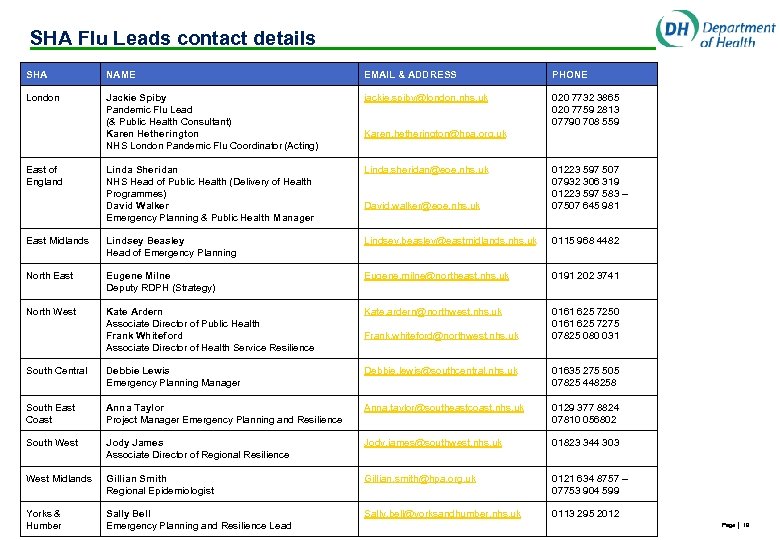 SHA Flu Leads contact details SHA NAME EMAIL & ADDRESS PHONE London Jackie Spiby Pandemic Flu Lead (& Public Health Consultant) Karen Hetherington NHS London Pandemic Flu Coordinator (Acting) jackie. spiby@london. nhs. uk 020 7732 3865 020 7759 2813 07790 708 559 Linda Sheridan NHS Head of Public Health (Delivery of Health Programmes) David Walker Emergency Planning & Public Health Manager Linda. sheridan@eoe. nhs. uk David. walker@eoe. nhs. uk 01223 597 507 07932 306 319 01223 597 583 – 07507 645 981 East Midlands Lindsey Beasley Head of Emergency Planning Lindsey. beasley@eastmidlands. nhs. uk 0115 968 4482 North East Eugene Milne Deputy RDPH (Strategy) Eugene. milne@northeast. nhs. uk 0191 202 3741 North West Kate Ardern Associate Director of Public Health Frank Whiteford Associate Director of Health Service Resilience Kate. ardern@northwest. nhs. uk 0161 625 7250 0161 625 7275 07825 080 031 South Central Debbie Lewis Emergency Planning Manager Debbie. lewis@southcentral. nhs. uk 01635 275 505 07825 448258 South East Coast Anna Taylor Project Manager Emergency Planning and Resilience Anna. taylor@southeastcoast. nhs. uk 0129 377 8824 07810 056802 South West Jody James Associate Director of Regional Resilience Jody. james@southwest. nhs. uk 01823 344 303 West Midlands Gillian Smith Regional Epidemiologist Gillian. smith@hpa. org. uk 0121 634 8757 – 07753 904 599 Yorks & Humber Sally Bell Emergency Planning and Resilience Lead Sally. bell@yorksandhumber. nhs. uk 0113 295 2012 East of England Karen. hetherington@hpa. org. uk Frank. whiteford@northwest. nhs. uk Page │ 19
SHA Flu Leads contact details SHA NAME EMAIL & ADDRESS PHONE London Jackie Spiby Pandemic Flu Lead (& Public Health Consultant) Karen Hetherington NHS London Pandemic Flu Coordinator (Acting) jackie. spiby@london. nhs. uk 020 7732 3865 020 7759 2813 07790 708 559 Linda Sheridan NHS Head of Public Health (Delivery of Health Programmes) David Walker Emergency Planning & Public Health Manager Linda. sheridan@eoe. nhs. uk David. walker@eoe. nhs. uk 01223 597 507 07932 306 319 01223 597 583 – 07507 645 981 East Midlands Lindsey Beasley Head of Emergency Planning Lindsey. beasley@eastmidlands. nhs. uk 0115 968 4482 North East Eugene Milne Deputy RDPH (Strategy) Eugene. milne@northeast. nhs. uk 0191 202 3741 North West Kate Ardern Associate Director of Public Health Frank Whiteford Associate Director of Health Service Resilience Kate. ardern@northwest. nhs. uk 0161 625 7250 0161 625 7275 07825 080 031 South Central Debbie Lewis Emergency Planning Manager Debbie. lewis@southcentral. nhs. uk 01635 275 505 07825 448258 South East Coast Anna Taylor Project Manager Emergency Planning and Resilience Anna. taylor@southeastcoast. nhs. uk 0129 377 8824 07810 056802 South West Jody James Associate Director of Regional Resilience Jody. james@southwest. nhs. uk 01823 344 303 West Midlands Gillian Smith Regional Epidemiologist Gillian. smith@hpa. org. uk 0121 634 8757 – 07753 904 599 Yorks & Humber Sally Bell Emergency Planning and Resilience Lead Sally. bell@yorksandhumber. nhs. uk 0113 295 2012 East of England Karen. hetherington@hpa. org. uk Frank. whiteford@northwest. nhs. uk Page │ 19
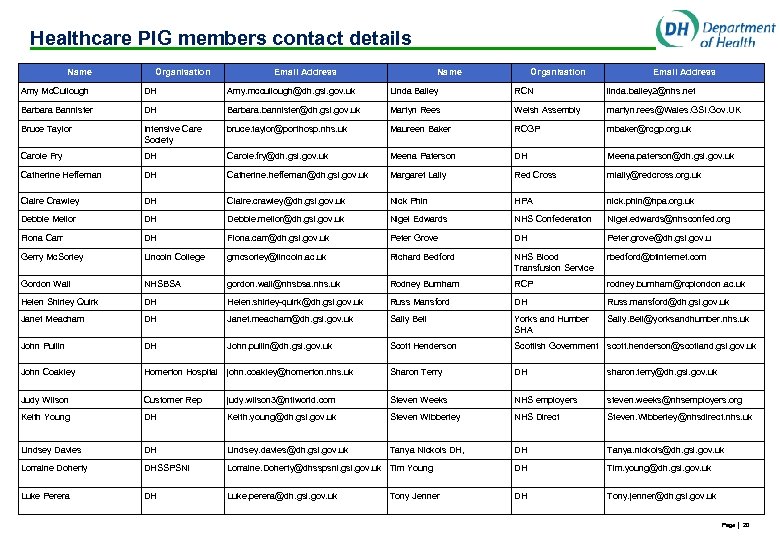 Healthcare PIG members contact details Name Organisation Email Address Amy Mc. Cullough DH Amy. mccullough@dh. gsi. gov. uk Linda Bailey RCN linda. bailey 2@nhs. net Barbara Bannister DH Barbara. bannister@dh. gsi. gov. uk Martyn Rees Welsh Assembly martyn. rees@Wales. GSI. Gov. UK Bruce Taylor Intensive Care Society bruce. taylor@porthosp. nhs. uk Maureen Baker RCGP mbaker@rcgp. org. uk Carole Fry DH Carole. fry@dh. gsi. gov. uk Meena Paterson DH Meena. paterson@dh. gsi. gov. uk Catherine Heffernan DH Catherine. heffernan@dh. gsi. gov. uk Margaret Lally Red Cross mlally@redcross. org. uk Claire Crawley DH Claire. crawley@dh. gsi. gov. uk Nick Phin HPA nick. phin@hpa. org. uk Debbie Mellor DH Debbie. mellor@dh. gsi. gov. uk Nigel Edwards NHS Confederation Nigel. edwards@nhsconfed. org Fiona Carr DH Fiona. carr@dh. gsi. gov. uk Peter Grove DH Peter. grove@dh. gsi. gov. u Gerry Mc. Sorley Lincoln College gmcsorley@lincoln. ac. uk Richard Bedford NHS Blood Transfusion Service rbedford@btinternet. com Gordon Wall NHSBSA gordon. wall@nhsbsa. nhs. uk Rodney Burnham RCP rodney. burnham@rcplondon. ac. uk Helen Shirley Quirk DH Helen. shirley-quirk@dh. gsi. gov. uk Russ Mansford DH Russ. mansford@dh. gsi. gov. uk Janet Meacham DH Janet. meacham@dh. gsi. gov. uk Sally Bell Yorks and Humber SHA Sally. Bell@yorksandhumber. nhs. uk John Pullin DH John. pullin@dh. gsi. gov. uk Scott Henderson Scottish Government scott. henderson@scotland. gsi. gov. uk John Coakley Homerton Hospital john. coakley@homerton. nhs. uk Sharon Terry DH sharon. terry@dh. gsi. gov. uk Judy Wilson Customer Rep judy. wilson 3@ntlworld. com Steven Weeks NHS employers steven. weeks@nhsemployers. org Keith Young DH Keith. young@dh. gsi. gov. uk Steven Wibberley NHS Direct Steven. Wibberley@nhsdirect. nhs. uk Lindsey Davies DH Lindsey. davies@dh. gsi. gov. uk Tanya Nickols DH, DH Tanya. nickols@dh. gsi. gov. uk Lorraine Doherty DHSSPSNI Lorraine. Doherty@dhsspsni. gsi. gov. uk Tim Young DH Tim. young@dh. gsi. gov. uk Luke Perera DH Luke. perera@dh. gsi. gov. uk DH Tony. jenner@dh. gsi. gov. uk Tony Jenner Page │ 20
Healthcare PIG members contact details Name Organisation Email Address Amy Mc. Cullough DH Amy. mccullough@dh. gsi. gov. uk Linda Bailey RCN linda. bailey 2@nhs. net Barbara Bannister DH Barbara. bannister@dh. gsi. gov. uk Martyn Rees Welsh Assembly martyn. rees@Wales. GSI. Gov. UK Bruce Taylor Intensive Care Society bruce. taylor@porthosp. nhs. uk Maureen Baker RCGP mbaker@rcgp. org. uk Carole Fry DH Carole. fry@dh. gsi. gov. uk Meena Paterson DH Meena. paterson@dh. gsi. gov. uk Catherine Heffernan DH Catherine. heffernan@dh. gsi. gov. uk Margaret Lally Red Cross mlally@redcross. org. uk Claire Crawley DH Claire. crawley@dh. gsi. gov. uk Nick Phin HPA nick. phin@hpa. org. uk Debbie Mellor DH Debbie. mellor@dh. gsi. gov. uk Nigel Edwards NHS Confederation Nigel. edwards@nhsconfed. org Fiona Carr DH Fiona. carr@dh. gsi. gov. uk Peter Grove DH Peter. grove@dh. gsi. gov. u Gerry Mc. Sorley Lincoln College gmcsorley@lincoln. ac. uk Richard Bedford NHS Blood Transfusion Service rbedford@btinternet. com Gordon Wall NHSBSA gordon. wall@nhsbsa. nhs. uk Rodney Burnham RCP rodney. burnham@rcplondon. ac. uk Helen Shirley Quirk DH Helen. shirley-quirk@dh. gsi. gov. uk Russ Mansford DH Russ. mansford@dh. gsi. gov. uk Janet Meacham DH Janet. meacham@dh. gsi. gov. uk Sally Bell Yorks and Humber SHA Sally. Bell@yorksandhumber. nhs. uk John Pullin DH John. pullin@dh. gsi. gov. uk Scott Henderson Scottish Government scott. henderson@scotland. gsi. gov. uk John Coakley Homerton Hospital john. coakley@homerton. nhs. uk Sharon Terry DH sharon. terry@dh. gsi. gov. uk Judy Wilson Customer Rep judy. wilson 3@ntlworld. com Steven Weeks NHS employers steven. weeks@nhsemployers. org Keith Young DH Keith. young@dh. gsi. gov. uk Steven Wibberley NHS Direct Steven. Wibberley@nhsdirect. nhs. uk Lindsey Davies DH Lindsey. davies@dh. gsi. gov. uk Tanya Nickols DH, DH Tanya. nickols@dh. gsi. gov. uk Lorraine Doherty DHSSPSNI Lorraine. Doherty@dhsspsni. gsi. gov. uk Tim Young DH Tim. young@dh. gsi. gov. uk Luke Perera DH Luke. perera@dh. gsi. gov. uk DH Tony. jenner@dh. gsi. gov. uk Tony Jenner Page │ 20
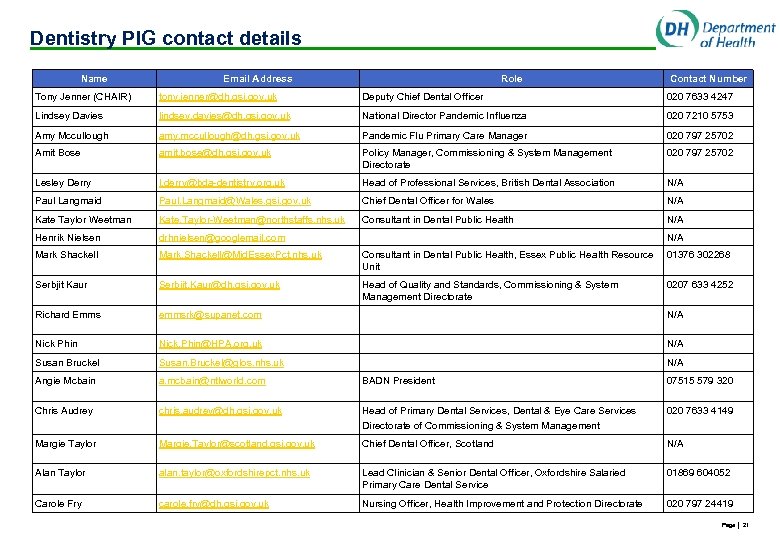 Dentistry PIG contact details Name Email Address Role Contact Number Tony Jenner (CHAIR) tony. jenner@dh. gsi. gov. uk Deputy Chief Dental Officer 020 7633 4247 Lindsey Davies lindsey. davies@dh. gsi. gov. uk National Director Pandemic Influenza 020 7210 5753 Amy Mccullough amy. mccullough@dh. gsi. gov. uk Pandemic Flu Primary Care Manager 020 797 25702 Amit Bose amit. bose@dh. gsi. gov. uk Policy Manager, Commissioning & System Management Directorate 020 797 25702 Lesley Derry l. derry@bda-dentistry. org. uk Head of Professional Services, British Dental Association N/A Paul Langmaid Paul. Langmaid@Wales. gsi. gov. uk Chief Dental Officer for Wales N/A Kate Taylor Weetman Kate. Taylor-Weetman@northstaffs. nhs. uk Consultant in Dental Public Health N/A Henrik Nielsen drhnielsen@googlemail. com Mark Shackell Mark. Shackell@Mid. Essex. Pct. nhs. uk Consultant in Dental Public Health, Essex Public Health Resource Unit 01376 302268 Serbjit Kaur Serbjit. Kaur@dh. gsi. gov. uk Head of Quality and Standards, Commissioning & System Management Directorate 0207 633 4252 Richard Emms emmsrk@supanet. com N/A Nick Phin Nick. Phin@HPA. org. uk N/A Susan Bruckel Susan. Bruckel@glos. nhs. uk N/A Angie Mcbain a. mcbain@ntlworld. com BADN President 07515 579 320 Chris Audrey chris. audrey@dh. gsi. gov. uk Head of Primary Dental Services, Dental & Eye Care Services Directorate of Commissioning & System Management 020 7633 4149 Margie Taylor Margie. Taylor@scotland. gsi. gov. uk Chief Dental Officer, Scotland N/A Alan Taylor alan. taylor@oxfordshirepct. nhs. uk Lead Clinician & Senior Dental Officer, Oxfordshire Salaried Primary Care Dental Service 01869 604052 Carole Fry carole. fry@dh. gsi. gov. uk Nursing Officer, Health Improvement and Protection Directorate 020 797 24419 N/A Page │ 21
Dentistry PIG contact details Name Email Address Role Contact Number Tony Jenner (CHAIR) tony. jenner@dh. gsi. gov. uk Deputy Chief Dental Officer 020 7633 4247 Lindsey Davies lindsey. davies@dh. gsi. gov. uk National Director Pandemic Influenza 020 7210 5753 Amy Mccullough amy. mccullough@dh. gsi. gov. uk Pandemic Flu Primary Care Manager 020 797 25702 Amit Bose amit. bose@dh. gsi. gov. uk Policy Manager, Commissioning & System Management Directorate 020 797 25702 Lesley Derry l. derry@bda-dentistry. org. uk Head of Professional Services, British Dental Association N/A Paul Langmaid Paul. Langmaid@Wales. gsi. gov. uk Chief Dental Officer for Wales N/A Kate Taylor Weetman Kate. Taylor-Weetman@northstaffs. nhs. uk Consultant in Dental Public Health N/A Henrik Nielsen drhnielsen@googlemail. com Mark Shackell Mark. Shackell@Mid. Essex. Pct. nhs. uk Consultant in Dental Public Health, Essex Public Health Resource Unit 01376 302268 Serbjit Kaur Serbjit. Kaur@dh. gsi. gov. uk Head of Quality and Standards, Commissioning & System Management Directorate 0207 633 4252 Richard Emms emmsrk@supanet. com N/A Nick Phin Nick. Phin@HPA. org. uk N/A Susan Bruckel Susan. Bruckel@glos. nhs. uk N/A Angie Mcbain a. mcbain@ntlworld. com BADN President 07515 579 320 Chris Audrey chris. audrey@dh. gsi. gov. uk Head of Primary Dental Services, Dental & Eye Care Services Directorate of Commissioning & System Management 020 7633 4149 Margie Taylor Margie. Taylor@scotland. gsi. gov. uk Chief Dental Officer, Scotland N/A Alan Taylor alan. taylor@oxfordshirepct. nhs. uk Lead Clinician & Senior Dental Officer, Oxfordshire Salaried Primary Care Dental Service 01869 604052 Carole Fry carole. fry@dh. gsi. gov. uk Nursing Officer, Health Improvement and Protection Directorate 020 797 24419 N/A Page │ 21
 Summary of planning support materials Implementation timings Planning assumptions Exercise feedback Assurance Strategy and Audit
Summary of planning support materials Implementation timings Planning assumptions Exercise feedback Assurance Strategy and Audit
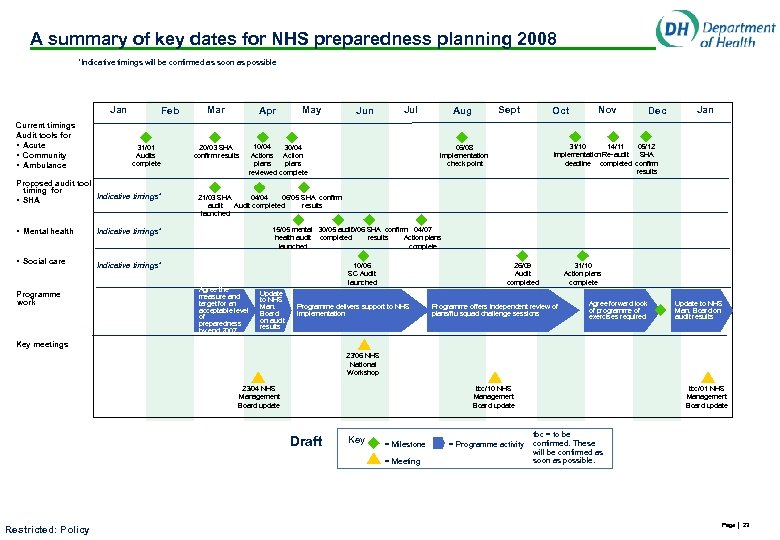 A summary of key dates for NHS preparedness planning 2008 *Indicative timings will be confirmed as soon as possible Jan Current timings Audit tools for • Acute • Community • Ambulance Feb 31/01 Audits complete Proposed audit tool timing for Indicative timings* • SHA • Mental health Apr 20/03 SHA confirm results May Jul Sept Aug Oct Nov Dec Jan 05/12 31/10 14/11 SHA Implementation Re-audit deadline completed confirm results 06/08 Implementation check point 21/03 SHA 04/04 06/05 SHA confirm audit Audit completed results launched 15/05 mental 30/05 audit 10/06 SHA confirm 04/07 health audit completed results Action plans launched complete Indicative timings* Programme work Jun 10/04 30/04 Actions Action plans reviewed complete Indicative timings* • Social care Mar Agree the measure and target for an acceptable level of preparedness by end 2007 10/06 SC Audit launched Update to NHS Man. Board on audit results 26/09 Audit completed Programme delivers support to NHS Implementation Programme offers independent review of plans/flu squad challenge sessions 31/10 Action plans complete Agree forward look of programme of exercises required Update to NHS Man. Board on audit results Key meetings 23/06 NHS National Workshop 23/04 NHS Management Board update tbc/10 NHS Management Board update Draft Key = Milestone = Meeting Restricted: Policy = Programme activity tbc/01 NHS Management Board update tbc = to be confirmed. These will be confirmed as soon as possible. Page │ 23
A summary of key dates for NHS preparedness planning 2008 *Indicative timings will be confirmed as soon as possible Jan Current timings Audit tools for • Acute • Community • Ambulance Feb 31/01 Audits complete Proposed audit tool timing for Indicative timings* • SHA • Mental health Apr 20/03 SHA confirm results May Jul Sept Aug Oct Nov Dec Jan 05/12 31/10 14/11 SHA Implementation Re-audit deadline completed confirm results 06/08 Implementation check point 21/03 SHA 04/04 06/05 SHA confirm audit Audit completed results launched 15/05 mental 30/05 audit 10/06 SHA confirm 04/07 health audit completed results Action plans launched complete Indicative timings* Programme work Jun 10/04 30/04 Actions Action plans reviewed complete Indicative timings* • Social care Mar Agree the measure and target for an acceptable level of preparedness by end 2007 10/06 SC Audit launched Update to NHS Man. Board on audit results 26/09 Audit completed Programme delivers support to NHS Implementation Programme offers independent review of plans/flu squad challenge sessions 31/10 Action plans complete Agree forward look of programme of exercises required Update to NHS Man. Board on audit results Key meetings 23/06 NHS National Workshop 23/04 NHS Management Board update tbc/10 NHS Management Board update Draft Key = Milestone = Meeting Restricted: Policy = Programme activity tbc/01 NHS Management Board update tbc = to be confirmed. These will be confirmed as soon as possible. Page │ 23
 Pandemic preparedness planning principles The National Framework articulates the planning principles upon which the health and social care response to a pandemic should be planned • Response arrangements should be based on strengthening and supplementing normal delivery mechanisms as far as is practicable • Plans should be developed on an integrated multi-agency basis with risk sharing and cross-cover between all organisations • Plans should encourage pan-organisational working, seeking to mobilise capacity and skills of all public and private sector healthcare staff, contractors and volunteers • Response measures should maintain public confidence and ‘feel fair’ Source: National Framework, p 94, 95 Page │ 24
Pandemic preparedness planning principles The National Framework articulates the planning principles upon which the health and social care response to a pandemic should be planned • Response arrangements should be based on strengthening and supplementing normal delivery mechanisms as far as is practicable • Plans should be developed on an integrated multi-agency basis with risk sharing and cross-cover between all organisations • Plans should encourage pan-organisational working, seeking to mobilise capacity and skills of all public and private sector healthcare staff, contractors and volunteers • Response measures should maintain public confidence and ‘feel fair’ Source: National Framework, p 94, 95 Page │ 24
 Plans should account for the following assumptions on how healthcare will be delivered during a pandemic The National Framework explains that the NHS should plan on the basis that normal patient pathways and service delivery arrangements will need to be adapted. It suggests that plans should assume use of the following 1. From WHO Phase 6, UK Alert Level 2 a National Flu Line Service is activated to enable symptomatic patients rapid access to a assessment, advice and, if appropriate, antiviral medicine treatment and onward referral. This includes triage to another healthcare professional where further advice and care is required. The Flu Line Service is intended to help preserve primary healthcare capacity for seeing those people that most need their services, as well as facilitating rapid access to antiviral treatment 2. Provision of a wider range of treatments by health professionals other than GPs e. g. nurses following agreed guidelines 3. Care of patients, who under normal circumstances would be admitted to hospital, in their own home/residential settings 4. Treatment of severely ill patients in areas of a hospital not normally used for providing acute medical care by medical and nursing teams who do not normally manage such patients 5. Treatment of patients in private healthcare facilities not normally used for acute medical care by healthcare teams that do not normally manage such patients 6. Managing surge demand during the pandemic will require a focus on delivering essential services 7. Note: 8. DH is currently consulting on necessary changes to medicines or other legislation that may be required to implement these alternative operational arrangements Source: National Framework, p 97 Page │ 25
Plans should account for the following assumptions on how healthcare will be delivered during a pandemic The National Framework explains that the NHS should plan on the basis that normal patient pathways and service delivery arrangements will need to be adapted. It suggests that plans should assume use of the following 1. From WHO Phase 6, UK Alert Level 2 a National Flu Line Service is activated to enable symptomatic patients rapid access to a assessment, advice and, if appropriate, antiviral medicine treatment and onward referral. This includes triage to another healthcare professional where further advice and care is required. The Flu Line Service is intended to help preserve primary healthcare capacity for seeing those people that most need their services, as well as facilitating rapid access to antiviral treatment 2. Provision of a wider range of treatments by health professionals other than GPs e. g. nurses following agreed guidelines 3. Care of patients, who under normal circumstances would be admitted to hospital, in their own home/residential settings 4. Treatment of severely ill patients in areas of a hospital not normally used for providing acute medical care by medical and nursing teams who do not normally manage such patients 5. Treatment of patients in private healthcare facilities not normally used for acute medical care by healthcare teams that do not normally manage such patients 6. Managing surge demand during the pandemic will require a focus on delivering essential services 7. Note: 8. DH is currently consulting on necessary changes to medicines or other legislation that may be required to implement these alternative operational arrangements Source: National Framework, p 97 Page │ 25
 Plans must take account of the following surge management assumptions Introduction At WHO Phase 6, Alert Level 2 respective health departments will need to make decisions to reduce or change NHS services and, where appropriate, to modify or suspend some normal performance targets. Health and social care organisations need to ensure their plans include provision for enhancing, scaling down, or ceasing some services at the pandemic threat increases. Their planning should be based on the following surge assumptions Severity of illness assumptions* • Up to 50% of the population may show clinical symptoms, up to 25% of those may develop complications • Up to 2. 5% of those who become symptomatic may die • Up to 22% of cases can be expected in the ‘peak week’ of a pandemic wave • A short epidemic would be greater strain on services than a lower-level but more sustained one • Hospitalisations and deaths are likely to be greatest if the highest attack rates are in older people, lowest burden if highest attack rates are in adults aged 15 -64 • Up to 28. 5% of symptomatic patients will require assessment and treatment by a general medical practitioner or experience nurse • Up to 4% of those symptomatic may require hospital admission, average length of stay for those with complications may be 6 days (10 if in intensive care) Source: National Framework, p 95, 96 Health and social care demand assumptions* • Total healthcare contacts for influenza –like illness could be up to 30 million • Peak demand could last for 1 -2 weeks, local epidemic waves 6 -8 weeks • Most patients will be treated at home with antiviral medicines initially * All statistics are based on national planning assumption attack rate of 50% Further information can be found in the Primary care guidance and managing surge guidance Page │ 26
Plans must take account of the following surge management assumptions Introduction At WHO Phase 6, Alert Level 2 respective health departments will need to make decisions to reduce or change NHS services and, where appropriate, to modify or suspend some normal performance targets. Health and social care organisations need to ensure their plans include provision for enhancing, scaling down, or ceasing some services at the pandemic threat increases. Their planning should be based on the following surge assumptions Severity of illness assumptions* • Up to 50% of the population may show clinical symptoms, up to 25% of those may develop complications • Up to 2. 5% of those who become symptomatic may die • Up to 22% of cases can be expected in the ‘peak week’ of a pandemic wave • A short epidemic would be greater strain on services than a lower-level but more sustained one • Hospitalisations and deaths are likely to be greatest if the highest attack rates are in older people, lowest burden if highest attack rates are in adults aged 15 -64 • Up to 28. 5% of symptomatic patients will require assessment and treatment by a general medical practitioner or experience nurse • Up to 4% of those symptomatic may require hospital admission, average length of stay for those with complications may be 6 days (10 if in intensive care) Source: National Framework, p 95, 96 Health and social care demand assumptions* • Total healthcare contacts for influenza –like illness could be up to 30 million • Peak demand could last for 1 -2 weeks, local epidemic waves 6 -8 weeks • Most patients will be treated at home with antiviral medicines initially * All statistics are based on national planning assumption attack rate of 50% Further information can be found in the Primary care guidance and managing surge guidance Page │ 26
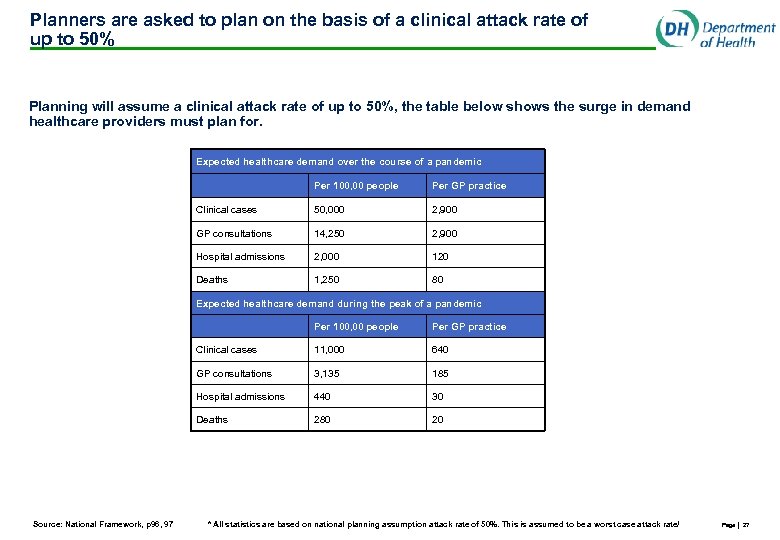 Planners are asked to plan on the basis of a clinical attack rate of up to 50% Planning will assume a clinical attack rate of up to 50%, the table below shows the surge in demand healthcare providers must plan for. Expected healthcare demand over the course of a pandemic Per 100, 00 people Per GP practice Clinical cases 50, 000 2, 900 GP consultations 14, 250 2, 900 Hospital admissions 2, 000 120 Deaths 1, 250 80 Expected healthcare demand during the peak of a pandemic Per 100, 00 people Clinical cases 11, 000 640 GP consultations 3, 135 185 Hospital admissions 440 30 Deaths Source: National Framework, p 96, 97 Per GP practice 280 20 * All statistics are based on national planning assumption attack rate of 50%. This is assumed to be a worst case attack rate/ Page │ 27
Planners are asked to plan on the basis of a clinical attack rate of up to 50% Planning will assume a clinical attack rate of up to 50%, the table below shows the surge in demand healthcare providers must plan for. Expected healthcare demand over the course of a pandemic Per 100, 00 people Per GP practice Clinical cases 50, 000 2, 900 GP consultations 14, 250 2, 900 Hospital admissions 2, 000 120 Deaths 1, 250 80 Expected healthcare demand during the peak of a pandemic Per 100, 00 people Clinical cases 11, 000 640 GP consultations 3, 135 185 Hospital admissions 440 30 Deaths Source: National Framework, p 96, 97 Per GP practice 280 20 * All statistics are based on national planning assumption attack rate of 50%. This is assumed to be a worst case attack rate/ Page │ 27
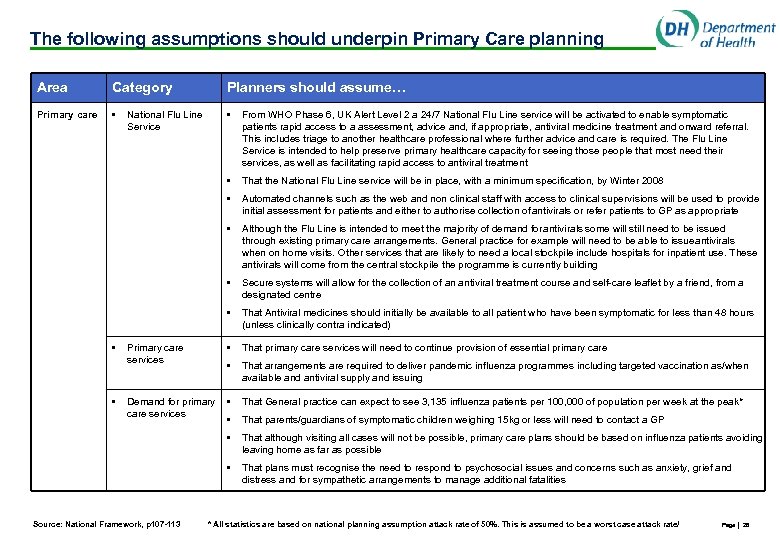 The following assumptions should underpin Primary Care planning Area Category Planners should assume… Primary care • • From WHO Phase 6, UK Alert Level 2 a 24/7 National Flu Line service will be activated to enable symptomatic patients rapid access to a assessment, advice and, if appropriate, antiviral medicine treatment and onward referral. This includes triage to another healthcare professional where further advice and care is required. The Flu Line Service is intended to help preserve primary healthcare capacity for seeing those people that most need their services, as well as facilitating rapid access to antiviral treatment • That the National Flu Line service will be in place, with a minimum specification, by Winter 2008 • Automated channels such as the web and non clinical staff with access to clinical supervisions will be used to provide initial assessment for patients and either to authorise collection of antivirals or refer patients to GP as appropriate • Although the Flu Line is intended to meet the majority of demand for antivirals some will still need to be issued through existing primary care arrangements. General practice for example will need to be able to issue antivirals when on home visits. Other services that are likely to need a local stockpile include hospitals for inpatient use. These antivirals will come from the central stockpile the programme is currently building • Secure systems will allow for the collection of an antiviral treatment course and self-care leaflet by a friend, from a designated centre • That Antiviral medicines should initially be available to all patient who have been symptomatic for less than 48 hours (unless clinically contra indicated) Primary care services • That primary care services will need to continue provision of essential primary care • That arrangements are required to deliver pandemic influenza programmes including targeted vaccination as/when available and antiviral supply and issuing Demand for primary care services • That General practice can expect to see 3, 135 influenza patients per 100, 000 of population per week at the peak* • That parents/guardians of symptomatic children weighing 15 kg or less will need to contact a GP • That although visiting all cases will not be possible, primary care plans should be based on influenza patients avoiding leaving home as far as possible • That plans must recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities • • National Flu Line Service Source: National Framework, p 107 -113 * All statistics are based on national planning assumption attack rate of 50%. This is assumed to be a worst case attack rate/ Page │ 28
The following assumptions should underpin Primary Care planning Area Category Planners should assume… Primary care • • From WHO Phase 6, UK Alert Level 2 a 24/7 National Flu Line service will be activated to enable symptomatic patients rapid access to a assessment, advice and, if appropriate, antiviral medicine treatment and onward referral. This includes triage to another healthcare professional where further advice and care is required. The Flu Line Service is intended to help preserve primary healthcare capacity for seeing those people that most need their services, as well as facilitating rapid access to antiviral treatment • That the National Flu Line service will be in place, with a minimum specification, by Winter 2008 • Automated channels such as the web and non clinical staff with access to clinical supervisions will be used to provide initial assessment for patients and either to authorise collection of antivirals or refer patients to GP as appropriate • Although the Flu Line is intended to meet the majority of demand for antivirals some will still need to be issued through existing primary care arrangements. General practice for example will need to be able to issue antivirals when on home visits. Other services that are likely to need a local stockpile include hospitals for inpatient use. These antivirals will come from the central stockpile the programme is currently building • Secure systems will allow for the collection of an antiviral treatment course and self-care leaflet by a friend, from a designated centre • That Antiviral medicines should initially be available to all patient who have been symptomatic for less than 48 hours (unless clinically contra indicated) Primary care services • That primary care services will need to continue provision of essential primary care • That arrangements are required to deliver pandemic influenza programmes including targeted vaccination as/when available and antiviral supply and issuing Demand for primary care services • That General practice can expect to see 3, 135 influenza patients per 100, 000 of population per week at the peak* • That parents/guardians of symptomatic children weighing 15 kg or less will need to contact a GP • That although visiting all cases will not be possible, primary care plans should be based on influenza patients avoiding leaving home as far as possible • That plans must recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities • • National Flu Line Service Source: National Framework, p 107 -113 * All statistics are based on national planning assumption attack rate of 50%. This is assumed to be a worst case attack rate/ Page │ 28
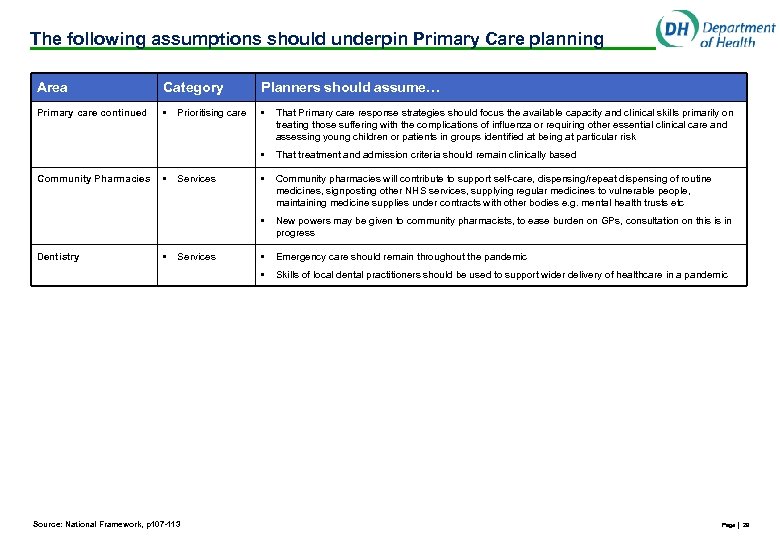 The following assumptions should underpin Primary Care planning Area Category Planners should assume… Primary care continued • • That Primary care response strategies should focus the available capacity and clinical skills primarily on treating those suffering with the complications of influenza or requiring other essential clinical care and assessing young children or patients in groups identified at being at particular risk • That treatment and admission criteria should remain clinically based • Community pharmacies will contribute to support self-care, dispensing/repeat dispensing of routine medicines, signposting other NHS services, supplying regular medicines to vulnerable people, maintaining medicine supplies under contracts with other bodies e. g. mental health trusts etc • New powers may be given to community pharmacists, to ease burden on GPs, consultation on this is in progress • Emergency care should remain throughout the pandemic • Skills of local dental practitioners should be used to support wider delivery of healthcare in a pandemic Community Pharmacies Dentistry • • Prioritising care Services Source: National Framework, p 107 -113 Page │ 29
The following assumptions should underpin Primary Care planning Area Category Planners should assume… Primary care continued • • That Primary care response strategies should focus the available capacity and clinical skills primarily on treating those suffering with the complications of influenza or requiring other essential clinical care and assessing young children or patients in groups identified at being at particular risk • That treatment and admission criteria should remain clinically based • Community pharmacies will contribute to support self-care, dispensing/repeat dispensing of routine medicines, signposting other NHS services, supplying regular medicines to vulnerable people, maintaining medicine supplies under contracts with other bodies e. g. mental health trusts etc • New powers may be given to community pharmacists, to ease burden on GPs, consultation on this is in progress • Emergency care should remain throughout the pandemic • Skills of local dental practitioners should be used to support wider delivery of healthcare in a pandemic Community Pharmacies Dentistry • • Prioritising care Services Source: National Framework, p 107 -113 Page │ 29
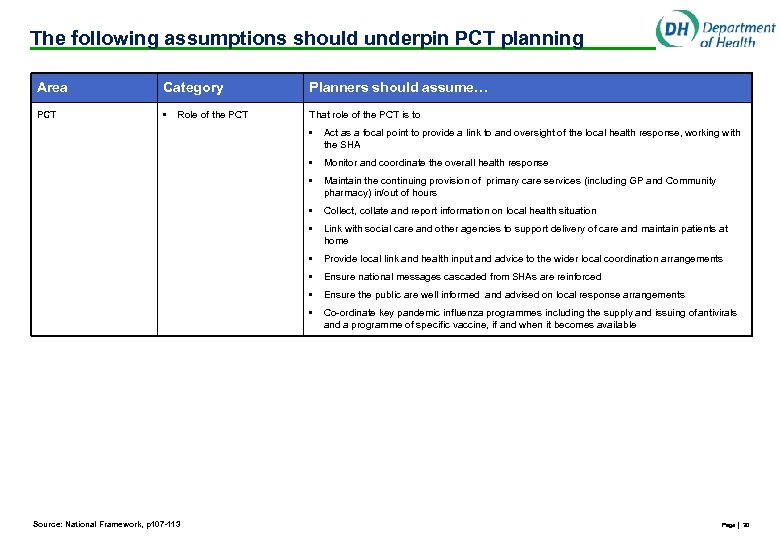 The following assumptions should underpin PCT planning Area Category Planners should assume… PCT • That role of the PCT is to Role of the PCT • • Monitor and coordinate the overall health response • Maintain the continuing provision of primary care services (including GP and Community pharmacy) in/out of hours • Collect, collate and report information on local health situation • Link with social care and other agencies to support delivery of care and maintain patients at home • Provide local link and health input and advice to the wider local coordination arrangements • Ensure national messages cascaded from SHAs are reinforced • Ensure the public are well informed and advised on local response arrangements • Source: National Framework, p 107 -113 Act as a focal point to provide a link to and oversight of the local health response, working with the SHA Co-ordinate key pandemic influenza programmes including the supply and issuing of antivirals and a programme of specific vaccine, if and when it becomes available Page │ 30
The following assumptions should underpin PCT planning Area Category Planners should assume… PCT • That role of the PCT is to Role of the PCT • • Monitor and coordinate the overall health response • Maintain the continuing provision of primary care services (including GP and Community pharmacy) in/out of hours • Collect, collate and report information on local health situation • Link with social care and other agencies to support delivery of care and maintain patients at home • Provide local link and health input and advice to the wider local coordination arrangements • Ensure national messages cascaded from SHAs are reinforced • Ensure the public are well informed and advised on local response arrangements • Source: National Framework, p 107 -113 Act as a focal point to provide a link to and oversight of the local health response, working with the SHA Co-ordinate key pandemic influenza programmes including the supply and issuing of antivirals and a programme of specific vaccine, if and when it becomes available Page │ 30
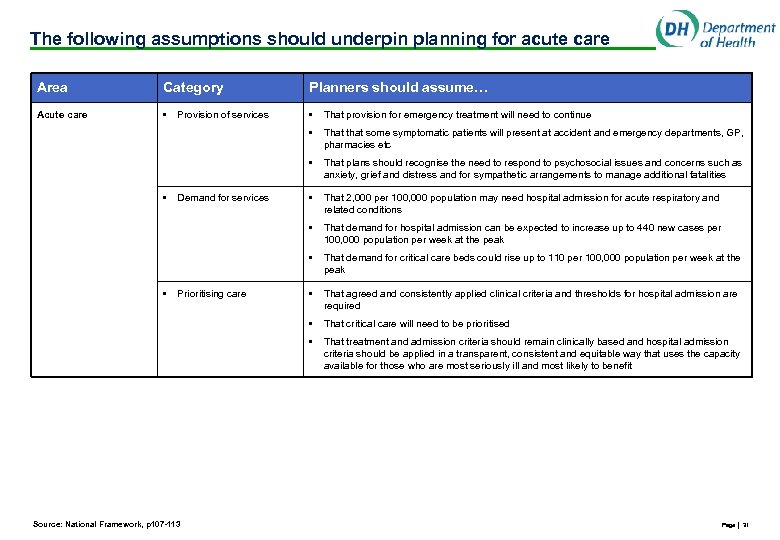 The following assumptions should underpin planning for acute care Area Category Planners should assume… Acute care • • That provision for emergency treatment will need to continue • That that some symptomatic patients will present at accident and emergency departments, GP, pharmacies etc • That plans should recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities • That 2, 000 per 100, 000 population may need hospital admission for acute respiratory and related conditions • That demand for hospital admission can be expected to increase up to 440 new cases per 100, 000 population per week at the peak • That demand for critical care beds could rise up to 110 per 100, 000 population per week at the peak • That agreed and consistently applied clinical criteria and thresholds for hospital admission are required • That critical care will need to be prioritised • That treatment and admission criteria should remain clinically based and hospital admission criteria should be applied in a transparent, consistent and equitable way that uses the capacity available for those who are most seriously ill and most likely to benefit • • Provision of services Demand for services Prioritising care Source: National Framework, p 107 -113 Page │ 31
The following assumptions should underpin planning for acute care Area Category Planners should assume… Acute care • • That provision for emergency treatment will need to continue • That that some symptomatic patients will present at accident and emergency departments, GP, pharmacies etc • That plans should recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities • That 2, 000 per 100, 000 population may need hospital admission for acute respiratory and related conditions • That demand for hospital admission can be expected to increase up to 440 new cases per 100, 000 population per week at the peak • That demand for critical care beds could rise up to 110 per 100, 000 population per week at the peak • That agreed and consistently applied clinical criteria and thresholds for hospital admission are required • That critical care will need to be prioritised • That treatment and admission criteria should remain clinically based and hospital admission criteria should be applied in a transparent, consistent and equitable way that uses the capacity available for those who are most seriously ill and most likely to benefit • • Provision of services Demand for services Prioritising care Source: National Framework, p 107 -113 Page │ 31
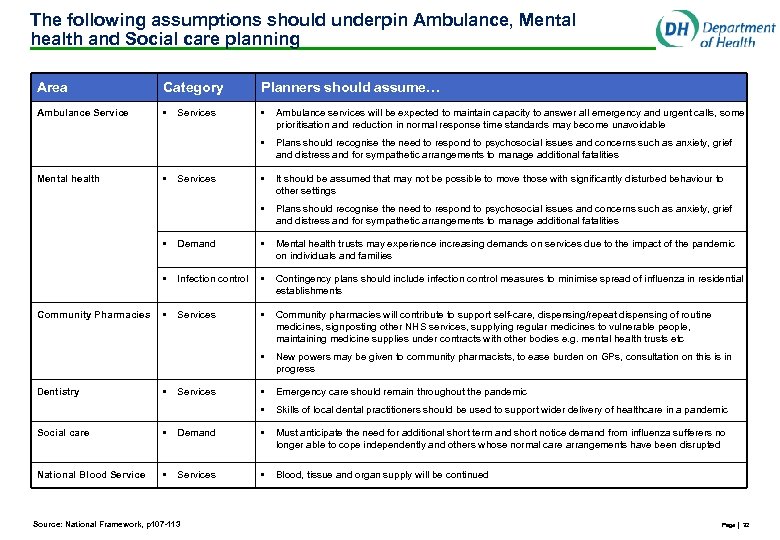 The following assumptions should underpin Ambulance, Mental health and Social care planning Area Category Planners should assume… Ambulance Service • • Ambulance services will be expected to maintain capacity to answer all emergency and urgent calls, some prioritisation and reduction in normal response time standards may become unavoidable • Plans should recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities • It should be assumed that may not be possible to move those with significantly disturbed behaviour to other settings • Plans should recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities Mental health • Services • Mental health trusts may experience increasing demands on services due to the impact of the pandemic on individuals and families Infection control • Contingency plans should include infection control measures to minimise spread of influenza in residential establishments • Services • Community pharmacies will contribute to support self-care, dispensing/repeat dispensing of routine medicines, signposting other NHS services, supplying regular medicines to vulnerable people, maintaining medicine supplies under contracts with other bodies e. g. mental health trusts etc • New powers may be given to community pharmacists, to ease burden on GPs, consultation on this is in progress • Emergency care should remain throughout the pandemic • Dentistry • • Community Pharmacies Demand Skills of local dental practitioners should be used to support wider delivery of healthcare in a pandemic • Services Social care • Demand • Must anticipate the need for additional short term and short notice demand from influenza sufferers no longer able to cope independently and others whose normal care arrangements have been disrupted National Blood Service • Services • Blood, tissue and organ supply will be continued Source: National Framework, p 107 -113 Page │ 32
The following assumptions should underpin Ambulance, Mental health and Social care planning Area Category Planners should assume… Ambulance Service • • Ambulance services will be expected to maintain capacity to answer all emergency and urgent calls, some prioritisation and reduction in normal response time standards may become unavoidable • Plans should recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities • It should be assumed that may not be possible to move those with significantly disturbed behaviour to other settings • Plans should recognise the need to respond to psychosocial issues and concerns such as anxiety, grief and distress and for sympathetic arrangements to manage additional fatalities Mental health • Services • Mental health trusts may experience increasing demands on services due to the impact of the pandemic on individuals and families Infection control • Contingency plans should include infection control measures to minimise spread of influenza in residential establishments • Services • Community pharmacies will contribute to support self-care, dispensing/repeat dispensing of routine medicines, signposting other NHS services, supplying regular medicines to vulnerable people, maintaining medicine supplies under contracts with other bodies e. g. mental health trusts etc • New powers may be given to community pharmacists, to ease burden on GPs, consultation on this is in progress • Emergency care should remain throughout the pandemic • Dentistry • • Community Pharmacies Demand Skills of local dental practitioners should be used to support wider delivery of healthcare in a pandemic • Services Social care • Demand • Must anticipate the need for additional short term and short notice demand from influenza sufferers no longer able to cope independently and others whose normal care arrangements have been disrupted National Blood Service • Services • Blood, tissue and organ supply will be continued Source: National Framework, p 107 -113 Page │ 32
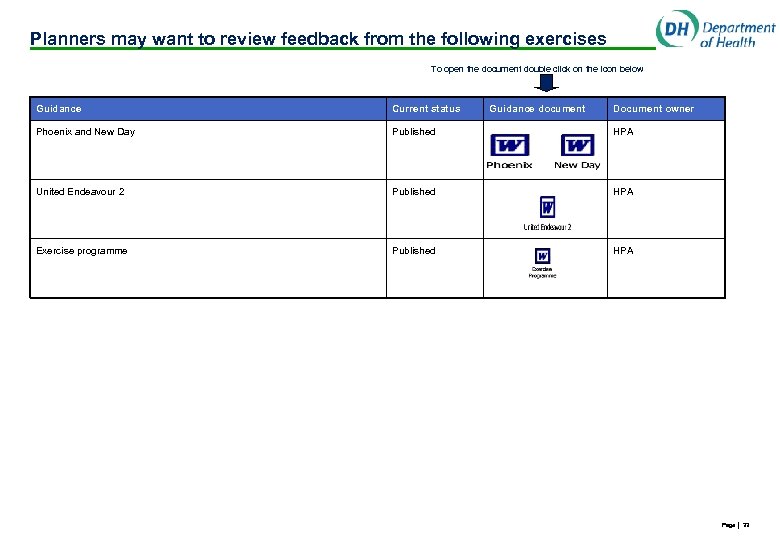 Planners may want to review feedback from the following exercises To open the document double click on the icon below Guidance Current status Guidance document Document owner Phoenix and New Day Published HPA United Endeavour 2 Published HPA Exercise programme Published HPA Page │ 33
Planners may want to review feedback from the following exercises To open the document double click on the icon below Guidance Current status Guidance document Document owner Phoenix and New Day Published HPA United Endeavour 2 Published HPA Exercise programme Published HPA Page │ 33
 Disclaimer In carrying out our work and preparing our report, we have worked solely on the instructions of Department of Health and for Department of Health’s purposes. It should not be provided to any third party without prior written consent. Our report may not have considered issues relevant to any third parties, any use such third parties may choose to make of our report is entirely at their own risk and we shall have no responsibility whatsoever in relation to any such use. The information in this pack is intended to provide only a general outline of the subjects covered. It should not be regarded as comprehensive or sufficient for making decisions, nor should it be used in place of professional advice. Accordingly, Assurance Strategy and Audit accepts no responsibility for loss arising from any action taken or not taken by anyone using this pack. The information in this presentation pack will have been supplemented by matters arising from any oral presentation by us, and should be considered in light of this additional information. Page │ 34
Disclaimer In carrying out our work and preparing our report, we have worked solely on the instructions of Department of Health and for Department of Health’s purposes. It should not be provided to any third party without prior written consent. Our report may not have considered issues relevant to any third parties, any use such third parties may choose to make of our report is entirely at their own risk and we shall have no responsibility whatsoever in relation to any such use. The information in this pack is intended to provide only a general outline of the subjects covered. It should not be regarded as comprehensive or sufficient for making decisions, nor should it be used in place of professional advice. Accordingly, Assurance Strategy and Audit accepts no responsibility for loss arising from any action taken or not taken by anyone using this pack. The information in this presentation pack will have been supplemented by matters arising from any oral presentation by us, and should be considered in light of this additional information. Page │ 34


