8b7af9201d778c8ff5e9719214caece8.ppt
- Количество слайдов: 31
 Immunologic mechanisms of tissue damage (hypersensitivity reactions)
Immunologic mechanisms of tissue damage (hypersensitivity reactions)
 Immunologic mechanisms of tissue damage (hypersensitivity reactions) Objectives 1 - Classify the hypersensitivity reactions (Gell & Coombs classification) 2 -Define (Illustrate) the Terms “Immediate hypersensitivity reaction, Reagin-mediated reaction, Atopy, Anaphylaxis, ". 3 - Define the term ‘allergen’ & List some common allergens that cause type I activation 4 - Discuss the pathophysiology of type I hypersensitivity reaction 5 - Discuss the immediate & late-phase responses in type-I H. S.
Immunologic mechanisms of tissue damage (hypersensitivity reactions) Objectives 1 - Classify the hypersensitivity reactions (Gell & Coombs classification) 2 -Define (Illustrate) the Terms “Immediate hypersensitivity reaction, Reagin-mediated reaction, Atopy, Anaphylaxis, ". 3 - Define the term ‘allergen’ & List some common allergens that cause type I activation 4 - Discuss the pathophysiology of type I hypersensitivity reaction 5 - Discuss the immediate & late-phase responses in type-I H. S.
 6 - List the predisposing factors to type-I H. S. reaction 7 - list the clinical manifestations of some allergic diseases 8 - Explain In-vitro & In-vivo diagnostic tests for Type-I hypersensitivity reaction 9 - Describe the complementary approaches in treating allergic diseases (Avoidance, Immunotherapy, Pharmacological treatment) 10 - Compare between Anaphylaxis & Anaphylactoid reaction
6 - List the predisposing factors to type-I H. S. reaction 7 - list the clinical manifestations of some allergic diseases 8 - Explain In-vitro & In-vivo diagnostic tests for Type-I hypersensitivity reaction 9 - Describe the complementary approaches in treating allergic diseases (Avoidance, Immunotherapy, Pharmacological treatment) 10 - Compare between Anaphylaxis & Anaphylactoid reaction
 Immunologic mechanisms of tissue damage (hypersensitivity reactions) Gell & Coombs (1963) have classified hypersensitivity reactions into four major types: Type III Type IV : Anaphylaxis H. S. : Antibody-dependent cytotoxic H. S. : Immune-complex mediated H. S. : Cell-mediated (delayed) H. S.
Immunologic mechanisms of tissue damage (hypersensitivity reactions) Gell & Coombs (1963) have classified hypersensitivity reactions into four major types: Type III Type IV : Anaphylaxis H. S. : Antibody-dependent cytotoxic H. S. : Immune-complex mediated H. S. : Cell-mediated (delayed) H. S.
 Type I hypersensitivity: Anaphylaxis H. S Immediate H. S Atopy The reaction may be mild & localized one, e. g. allergic conjunctivitis, or it may be severe generalized reaction, e. g. anaphylactic shock.
Type I hypersensitivity: Anaphylaxis H. S Immediate H. S Atopy The reaction may be mild & localized one, e. g. allergic conjunctivitis, or it may be severe generalized reaction, e. g. anaphylactic shock.
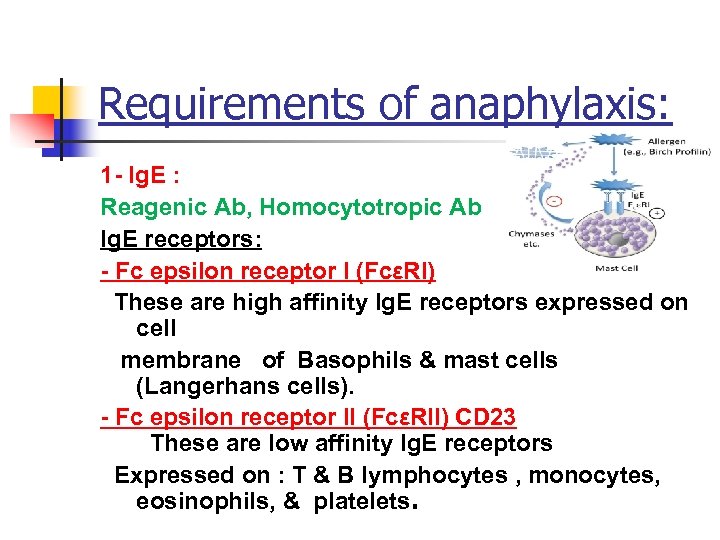 Requirements of anaphylaxis: 1 - Ig. E : Reagenic Ab, Homocytotropic Ab Ig. E receptors: - Fc epsilon receptor I (FcεRI) These are high affinity Ig. E receptors expressed on cell membrane of Basophils & mast cells (Langerhans cells). - Fc epsilon receptor II (FcεRII) CD 23 These are low affinity Ig. E receptors Expressed on : T & B lymphocytes , monocytes, eosinophils, & platelets.
Requirements of anaphylaxis: 1 - Ig. E : Reagenic Ab, Homocytotropic Ab Ig. E receptors: - Fc epsilon receptor I (FcεRI) These are high affinity Ig. E receptors expressed on cell membrane of Basophils & mast cells (Langerhans cells). - Fc epsilon receptor II (FcεRII) CD 23 These are low affinity Ig. E receptors Expressed on : T & B lymphocytes , monocytes, eosinophils, & platelets.
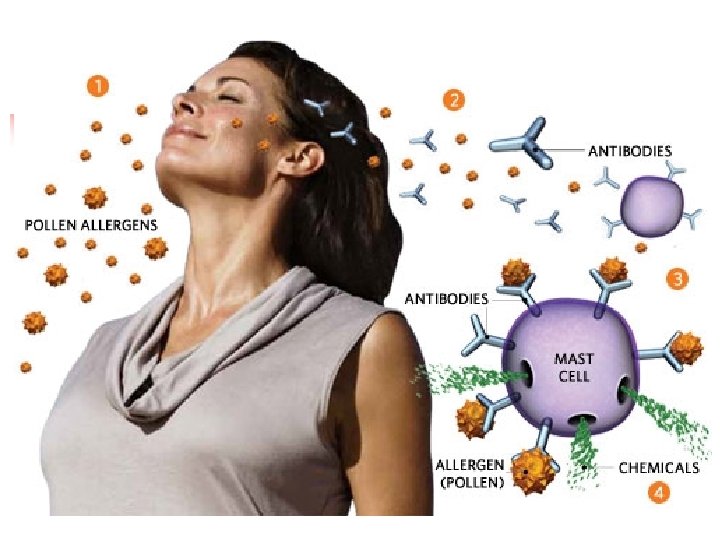
 2 - Allergens: a- Inhalants : animal danders. Plant pollens , fungal spore, house dust mites (Dermatophagoides) b- Ingestants : (foods, drugs. . . etc. ) egg albumin, fish, cheese, nuts, milk, food additive, penicillin, aspirin c- contactants: pollen, food, drugs. . . etc.
2 - Allergens: a- Inhalants : animal danders. Plant pollens , fungal spore, house dust mites (Dermatophagoides) b- Ingestants : (foods, drugs. . . etc. ) egg albumin, fish, cheese, nuts, milk, food additive, penicillin, aspirin c- contactants: pollen, food, drugs. . . etc.
 3 - Mast cells & Basophils: They represent a major source of potent chemical mediator implicated in a wide spectrum of inflammatory & immunological processes. They express membrane receptors (FcεRI) that specifically bind the Fc portion of Ig. E (binding site) Ab. Complements are not involved in this type of reaction.
3 - Mast cells & Basophils: They represent a major source of potent chemical mediator implicated in a wide spectrum of inflammatory & immunological processes. They express membrane receptors (FcεRI) that specifically bind the Fc portion of Ig. E (binding site) Ab. Complements are not involved in this type of reaction.
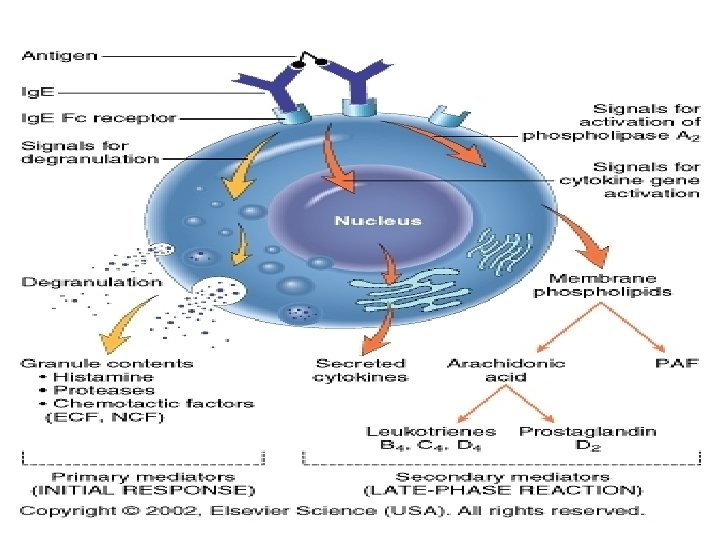
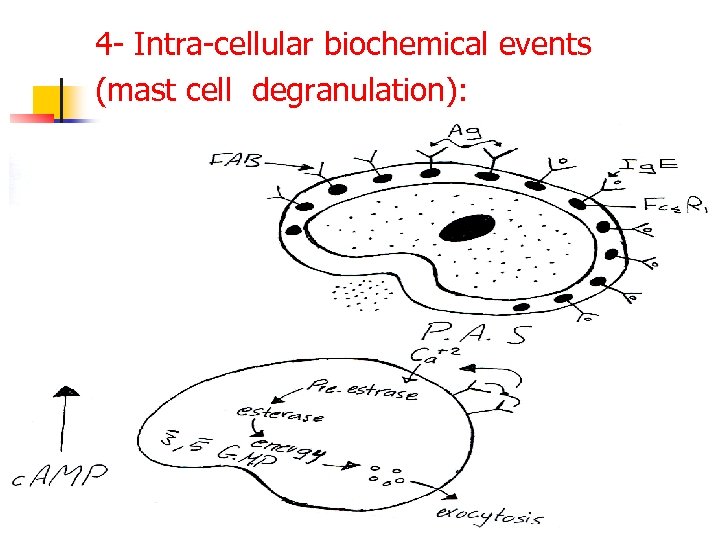 4 - Intra-cellular biochemical events (mast cell degranulation):
4 - Intra-cellular biochemical events (mast cell degranulation):
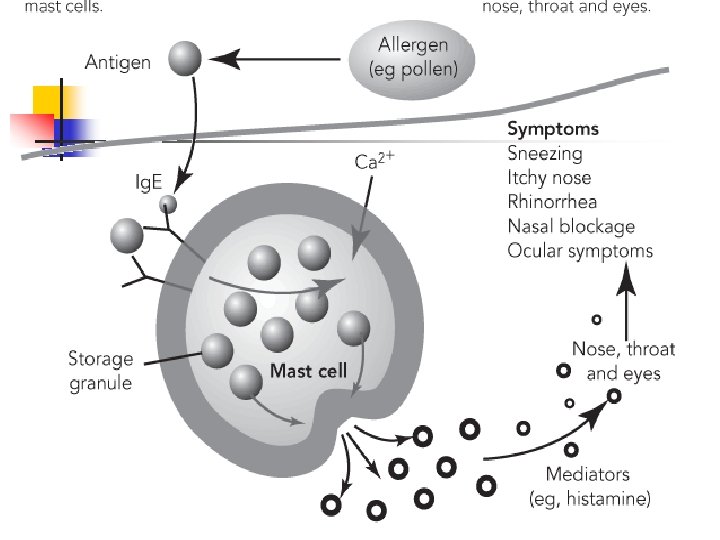
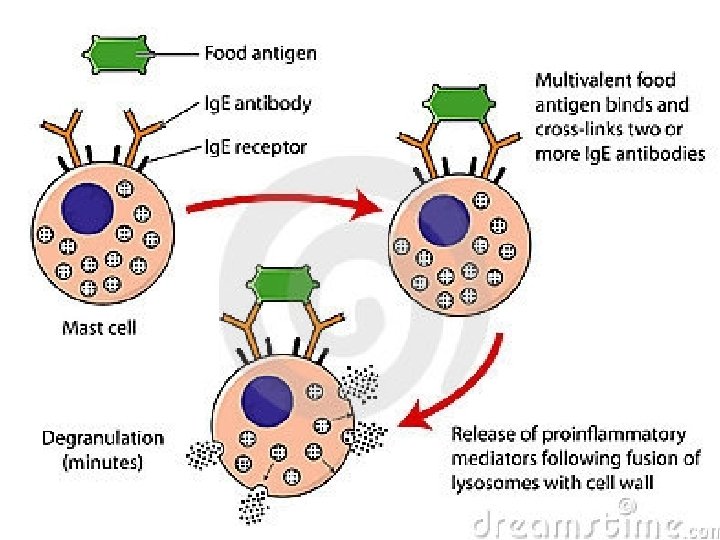
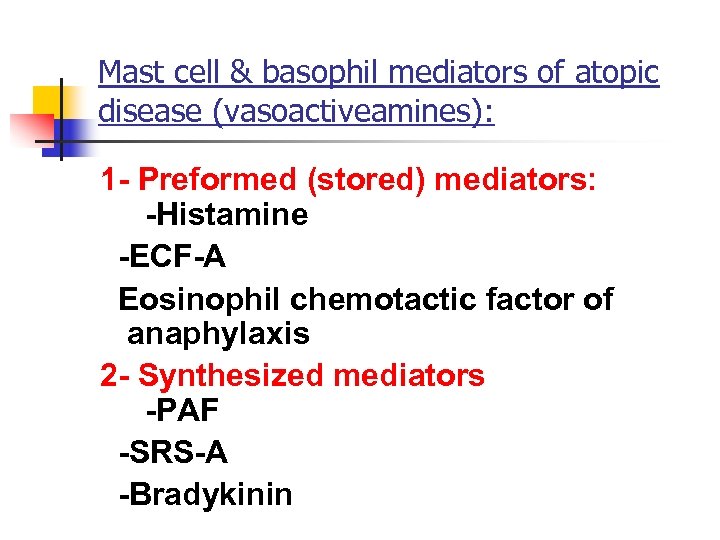 Mast cell & basophil mediators of atopic disease (vasoactiveamines): 1 - Preformed (stored) mediators: -Histamine -ECF-A Eosinophil chemotactic factor of anaphylaxis 2 - Synthesized mediators -PAF -SRS-A -Bradykinin
Mast cell & basophil mediators of atopic disease (vasoactiveamines): 1 - Preformed (stored) mediators: -Histamine -ECF-A Eosinophil chemotactic factor of anaphylaxis 2 - Synthesized mediators -PAF -SRS-A -Bradykinin
 5 - Vasoactive amines: a- Histamine: - smooth muscle contraction of human bronchioles. - increase permeability of capillaries (vasodilatation). - increase secretions by nasal & bronchial mucous glands.
5 - Vasoactive amines: a- Histamine: - smooth muscle contraction of human bronchioles. - increase permeability of capillaries (vasodilatation). - increase secretions by nasal & bronchial mucous glands.
 b- ECA-A (Eosinophil Chemotactic Factor of Anaphylaxis) - preformed in basophils & mast cells. - causes influx of eos. to area of allergic inflammation. (eosinophil chemotaxis) * role of eosinophils in allergy: They control allergic reactions by releasing histaminase and arylsulfatase , which degrade two important mediators, histamine and SRS-A, respectively. Eosinophil may therefore reduce the severity of type I response.
b- ECA-A (Eosinophil Chemotactic Factor of Anaphylaxis) - preformed in basophils & mast cells. - causes influx of eos. to area of allergic inflammation. (eosinophil chemotaxis) * role of eosinophils in allergy: They control allergic reactions by releasing histaminase and arylsulfatase , which degrade two important mediators, histamine and SRS-A, respectively. Eosinophil may therefore reduce the severity of type I response.
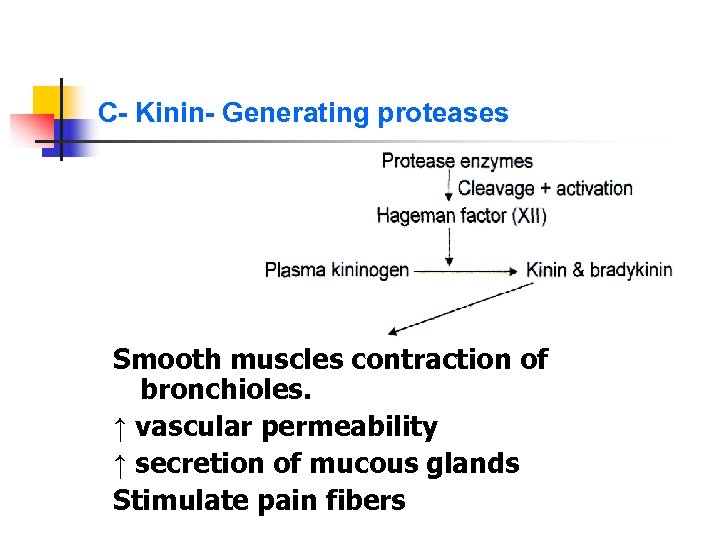 C- Kinin- Generating proteases Smooth muscles contraction of bronchioles. ↑ vascular permeability ↑ secretion of mucous glands Stimulate pain fibers
C- Kinin- Generating proteases Smooth muscles contraction of bronchioles. ↑ vascular permeability ↑ secretion of mucous glands Stimulate pain fibers
 d- PAF (Platelet Activating Factor) e- HMW-NCF (High Molecular Wt. Neutrophil Chemotactic Factor)
d- PAF (Platelet Activating Factor) e- HMW-NCF (High Molecular Wt. Neutrophil Chemotactic Factor)
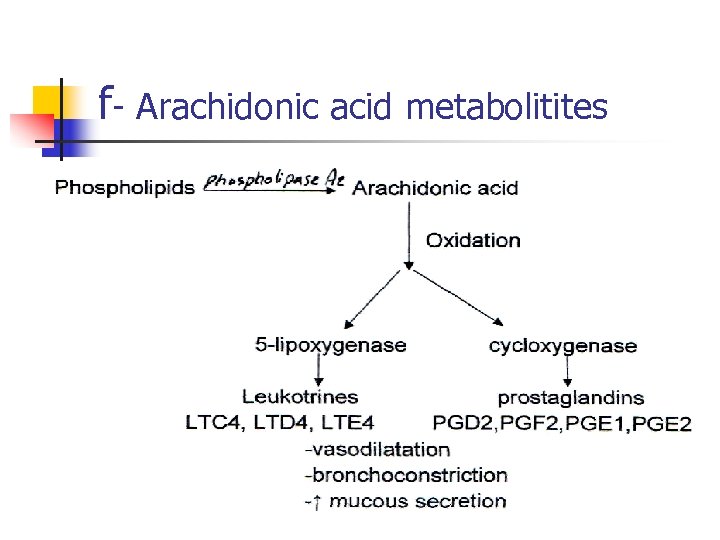 f- Arachidonic acid metabolitites
f- Arachidonic acid metabolitites
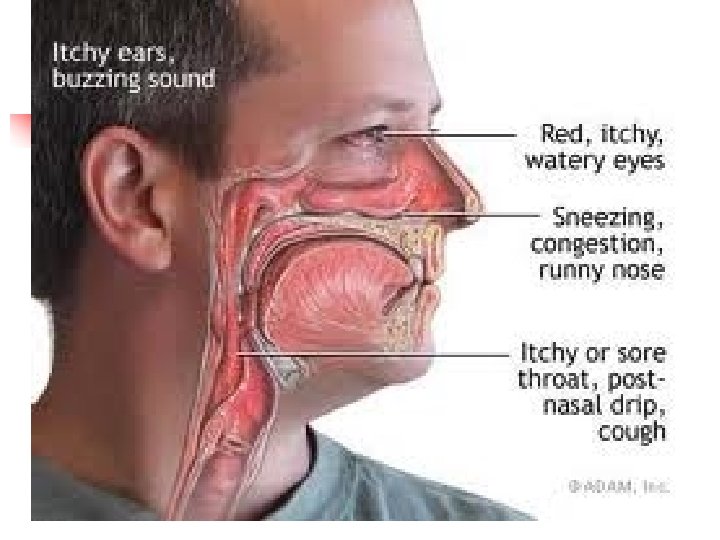
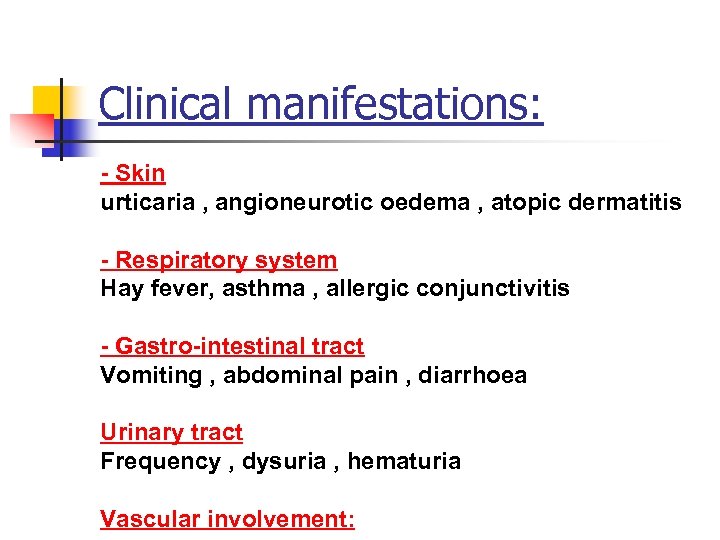 Clinical manifestations: - Skin urticaria , angioneurotic oedema , atopic dermatitis - Respiratory system Hay fever, asthma , allergic conjunctivitis - Gastro-intestinal tract Vomiting , abdominal pain , diarrhoea Urinary tract Frequency , dysuria , hematuria Vascular involvement:
Clinical manifestations: - Skin urticaria , angioneurotic oedema , atopic dermatitis - Respiratory system Hay fever, asthma , allergic conjunctivitis - Gastro-intestinal tract Vomiting , abdominal pain , diarrhoea Urinary tract Frequency , dysuria , hematuria Vascular involvement:




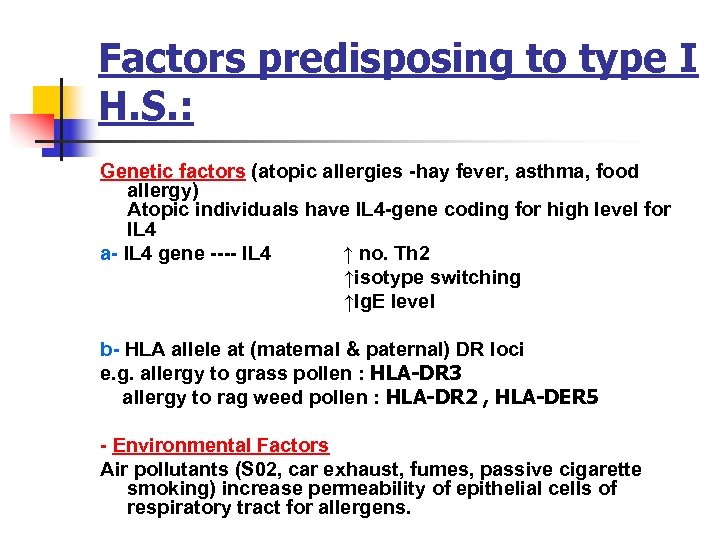 Factors predisposing to type I H. S. : Genetic factors (atopic allergies -hay fever, asthma, food allergy) Atopic individuals have IL 4 -gene coding for high level for IL 4 a- IL 4 gene ---- IL 4 ↑ no. Th 2 ↑isotype switching ↑Ig. E level b- HLA allele at (maternal & paternal) DR loci e. g. allergy to grass pollen : HLA-DR 3 allergy to rag weed pollen : HLA-DR 2 , HLA-DER 5 - Environmental Factors Air pollutants (S 02, car exhaust, fumes, passive cigarette smoking) increase permeability of epithelial cells of respiratory tract for allergens.
Factors predisposing to type I H. S. : Genetic factors (atopic allergies -hay fever, asthma, food allergy) Atopic individuals have IL 4 -gene coding for high level for IL 4 a- IL 4 gene ---- IL 4 ↑ no. Th 2 ↑isotype switching ↑Ig. E level b- HLA allele at (maternal & paternal) DR loci e. g. allergy to grass pollen : HLA-DR 3 allergy to rag weed pollen : HLA-DR 2 , HLA-DER 5 - Environmental Factors Air pollutants (S 02, car exhaust, fumes, passive cigarette smoking) increase permeability of epithelial cells of respiratory tract for allergens.
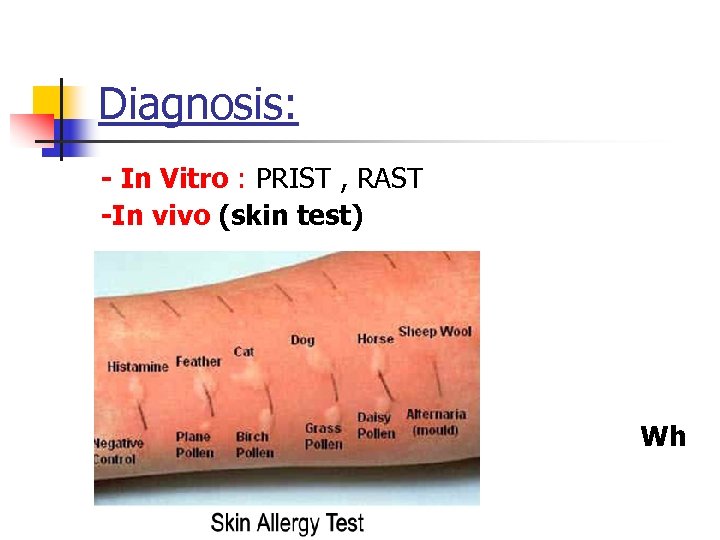 Diagnosis: - In Vitro : PRIST , RAST -In vivo (skin test) eal & flare Wh
Diagnosis: - In Vitro : PRIST , RAST -In vivo (skin test) eal & flare Wh
 Treatment & Prevention: 1 -Avoidance of responsible allergens 2 -Immunotherapy a- Desensitization , Hyposensitization (Ig. Gblocking Abs) * allergy shots(repeated inj+ dose) b- Immunotolerance
Treatment & Prevention: 1 -Avoidance of responsible allergens 2 -Immunotherapy a- Desensitization , Hyposensitization (Ig. Gblocking Abs) * allergy shots(repeated inj+ dose) b- Immunotolerance
 3 - Drugs a- Anti-histamins : Tavist-D (clemastin fumerate) b- Mast cell & basophil stabilizing drugs: Adrenaline : increase intracellular level of c. AMP Theophylline : inhibits brake down of c. AMP by phosphodiesterase Sodium chromoglycate : inhibits calcium influx c- General anti-inflammatory agents : corticosteroids
3 - Drugs a- Anti-histamins : Tavist-D (clemastin fumerate) b- Mast cell & basophil stabilizing drugs: Adrenaline : increase intracellular level of c. AMP Theophylline : inhibits brake down of c. AMP by phosphodiesterase Sodium chromoglycate : inhibits calcium influx c- General anti-inflammatory agents : corticosteroids
 Anaphylactoid reactions: The clinical manifestations of anaphylaxis can occur in the absence of any evidence for an allergen-lg. E antibody event. These reactions are believed to arise through the non-immunologic release of vasoactive & inflammatory mediators from mast cells and basophils in certain susceptible individuals. The inciting agents are: - I. V. radiographic contrast media - Aspirin - Venom - Exercise induce anaphylaxis - Other causes : Idiopathic
Anaphylactoid reactions: The clinical manifestations of anaphylaxis can occur in the absence of any evidence for an allergen-lg. E antibody event. These reactions are believed to arise through the non-immunologic release of vasoactive & inflammatory mediators from mast cells and basophils in certain susceptible individuals. The inciting agents are: - I. V. radiographic contrast media - Aspirin - Venom - Exercise induce anaphylaxis - Other causes : Idiopathic


