0f80763faa7edd0bd105df1de5c3727d.ppt
- Количество слайдов: 67
Immune system, lymphoid organs for pharmacists • by Krisztina H. -Minkó Semmelweis University Department of Human Morphology and Developmental Biology 2015
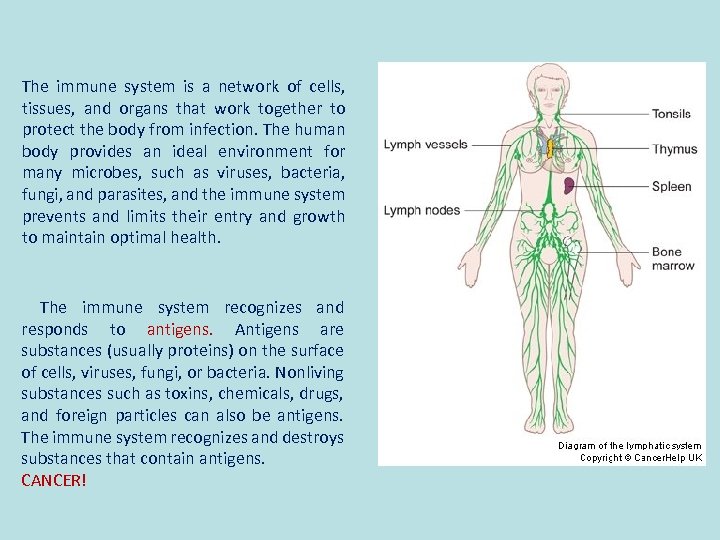
The immune system is a network of cells, tissues, and organs that work together to protect the body from infection. The human body provides an ideal environment for many microbes, such as viruses, bacteria, fungi, and parasites, and the immune system prevents and limits their entry and growth to maintain optimal health. The immune system recognizes and responds to antigens. Antigens are substances (usually proteins) on the surface of cells, viruses, fungi, or bacteria. Nonliving substances such as toxins, chemicals, drugs, and foreign particles can also be antigens. The immune system recognizes and destroys substances that contain antigens. CANCER!
INNATE IMMUNITY Innate, or nonspecific, immunity is the defense system with which you were born. It protects you against all antigens. Innate immunity involves barriers that keep harmful materials from entering your body. These barriers form the first line of defense in the immune response. Examples of innate immunity include: • Cough reflex • Enzymes in tears and skin oils • Mucus, which traps bacteria and small particles • Skin • Stomach acid Innate immunity also comes in a protein chemical form, called innate humoral immunity. Examples include the body's complement system and substances called interferon and interleukin-1 (which causes fever). If an antigen gets past these barriers, it is attacked and destroyed by other parts of the immune system. ACQUIRED IMMUNITY Acquired immunity is immunity that develops with exposure to various antigens. Your immune system builds a defense against that specific antigen.
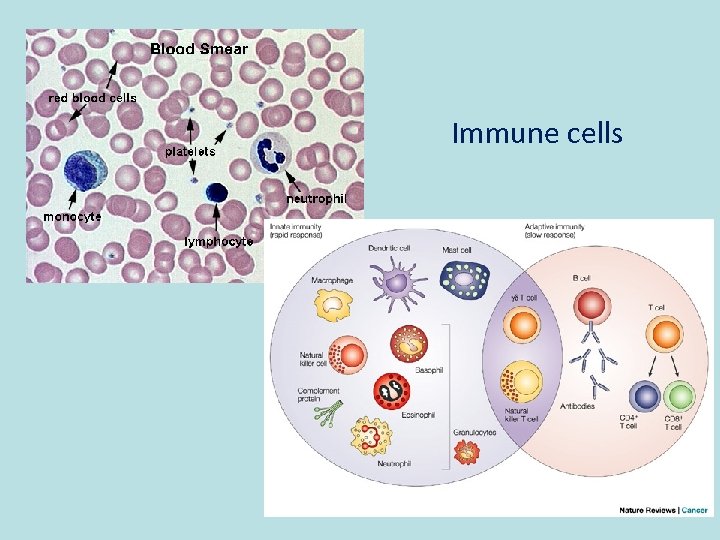
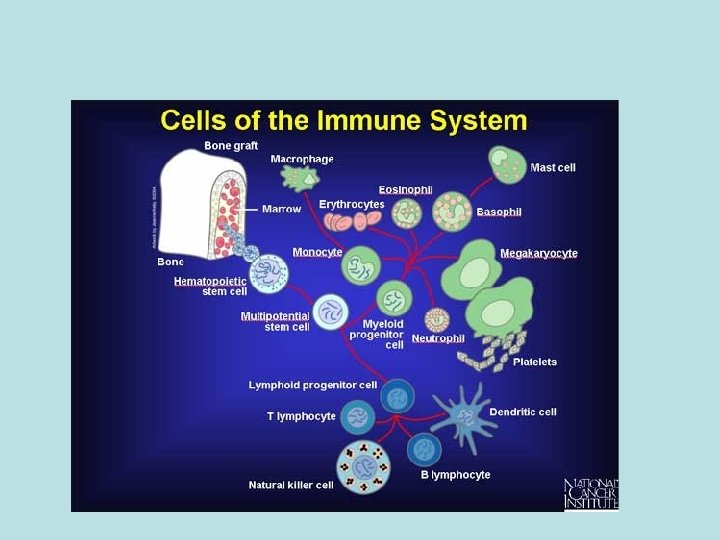
Immune cells
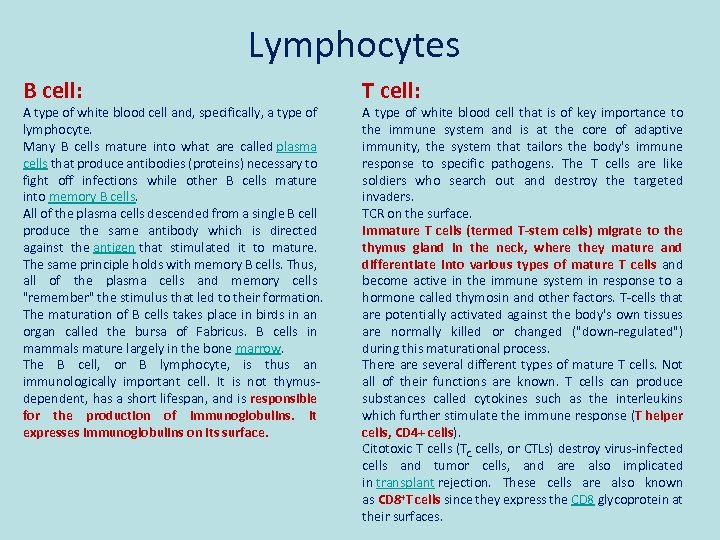
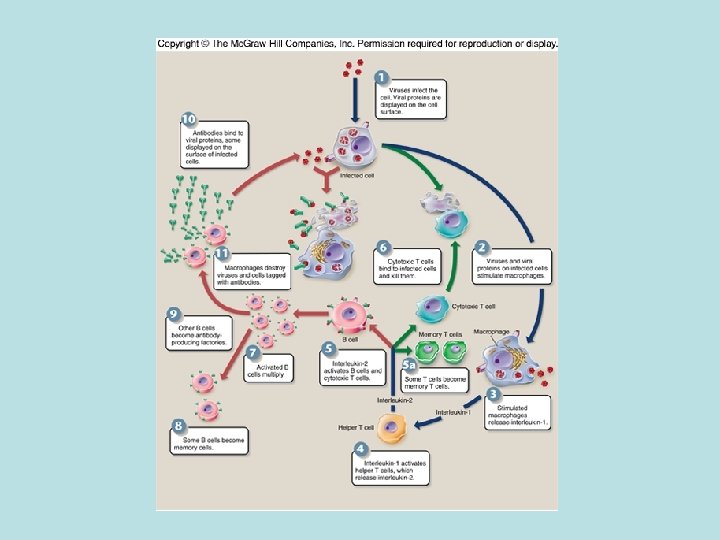
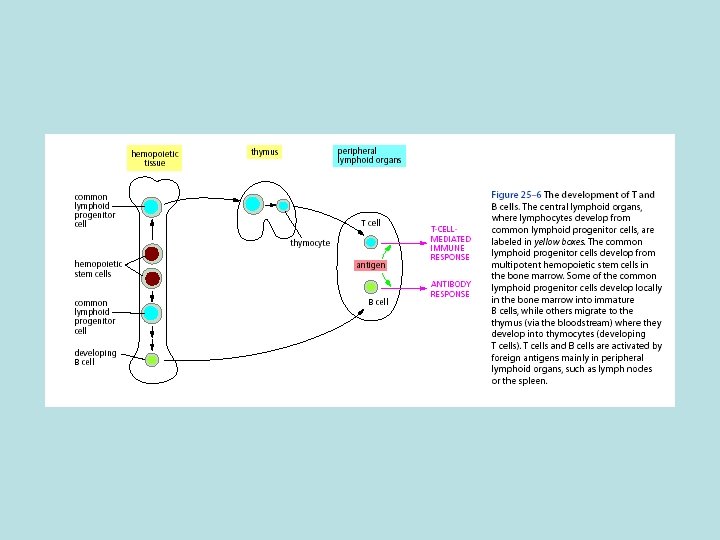
Lymphocytes B cell: A type of white blood cell and, specifically, a type of lymphocyte. Many B cells mature into what are called plasma cells that produce antibodies (proteins) necessary to fight off infections while other B cells mature into memory B cells. All of the plasma cells descended from a single B cell produce the same antibody which is directed against the antigen that stimulated it to mature. The same principle holds with memory B cells. Thus, all of the plasma cells and memory cells "remember" the stimulus that led to their formation. The maturation of B cells takes place in birds in an organ called the bursa of Fabricus. B cells in mammals mature largely in the bone marrow. The B cell, or B lymphocyte, is thus an immunologically important cell. It is not thymusdependent, has a short lifespan, and is responsible for the production of immunoglobulins. It expresses immunoglobulins on its surface. T cell: A type of white blood cell that is of key importance to the immune system and is at the core of adaptive immunity, the system that tailors the body's immune response to specific pathogens. The T cells are like soldiers who search out and destroy the targeted invaders. TCR on the surface. Immature T cells (termed T-stem cells) migrate to the thymus gland in the neck, where they mature and differentiate into various types of mature T cells and become active in the immune system in response to a hormone called thymosin and other factors. T-cells that are potentially activated against the body's own tissues are normally killed or changed ("down-regulated") during this maturational process. There are several different types of mature T cells. Not all of their functions are known. T cells can produce substances called cytokines such as the interleukins which further stimulate the immune response (T helper cells, CD 4+ cells). Citotoxic T cells (TC cells, or CTLs) destroy virus-infected cells and tumor cells, and are also implicated in transplant rejection. These cells are also known as CD 8+T cells since they express the CD 8 glycoprotein at their surfaces.
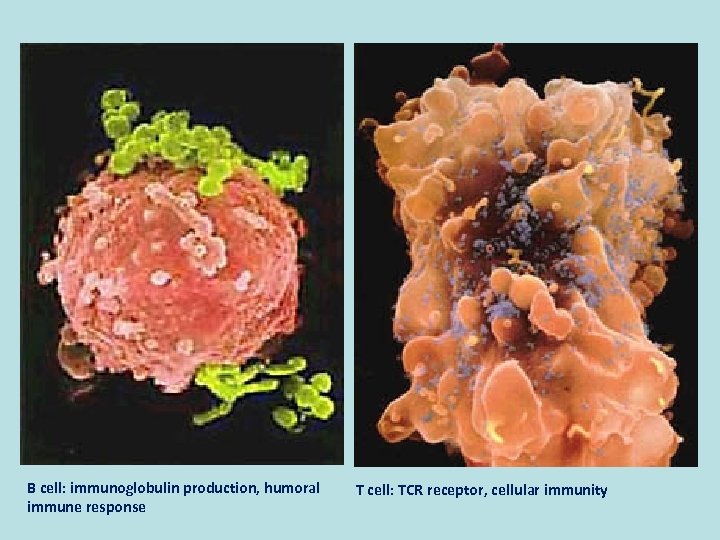
B cell: immunoglobulin production, humoral immune response T cell: TCR receptor, cellular immunity
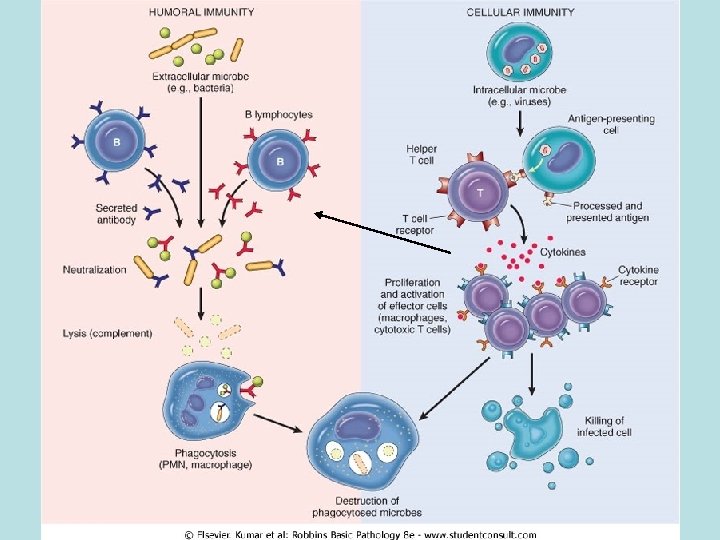
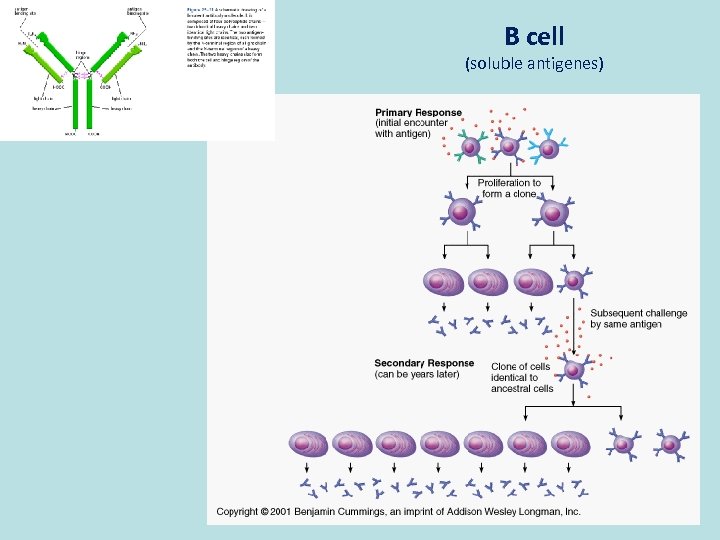
B cell (soluble antigenes)
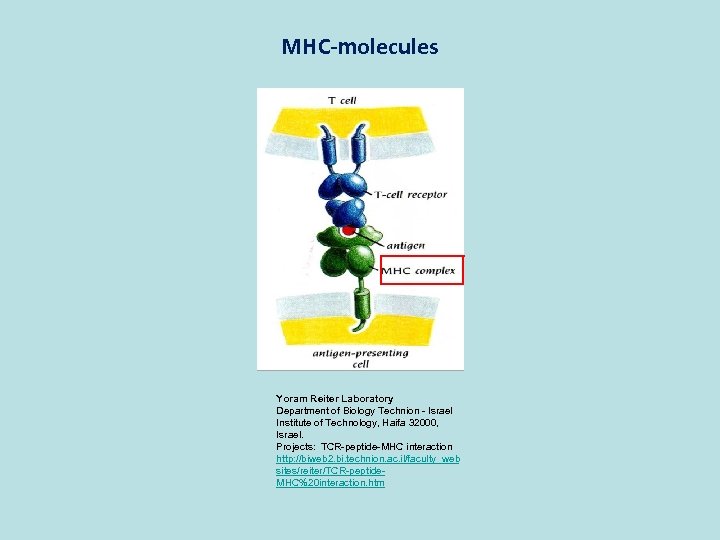
MHC-molecules Yoram Reiter Laboratory Department of Biology Technion - Israel Institute of Technology, Haifa 32000, Israel. Projects: TCR-peptide-MHC interaction http: //biweb 2. bi. technion. ac. il/faculty_web sites/reiter/TCR-peptide. MHC%20 interaction. htm
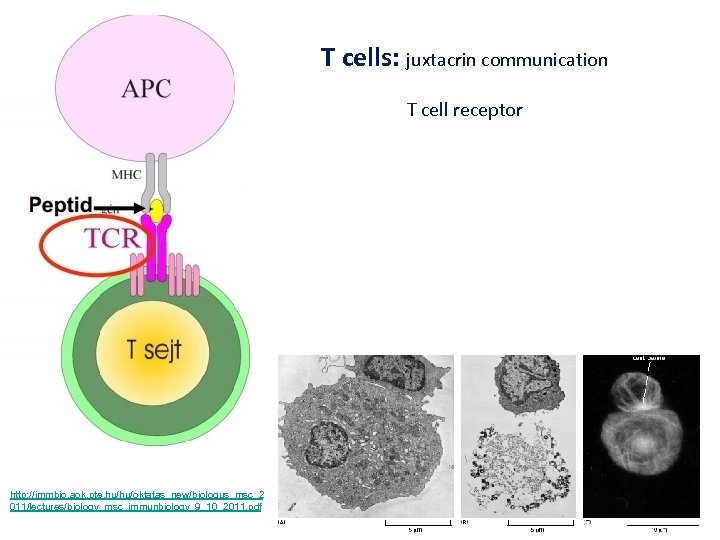
T cells: juxtacrin communication T cell receptor http: //immbio. aok. pte. hu/hu/oktatas_new/biologus_msc_2 011/lectures/biology_msc_immunbiology_9_10_2011. pdf
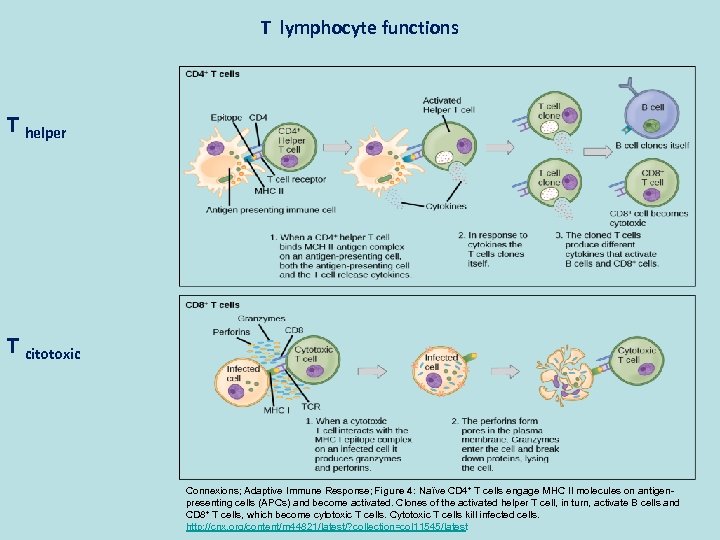
T lymphocyte functions T helper T citotoxic Connexions; Adaptive Immune Response; Figure 4: Naïve CD 4+ T cells engage MHC II molecules on antigenpresenting cells (APCs) and become activated. Clones of the activated helper T cell, in turn, activate B cells and CD 8+ T cells, which become cytotoxic T cells. Cytotoxic T cells kill infected cells. http: //cnx. org/content/m 44821/latest/? collection=col 11545/latest
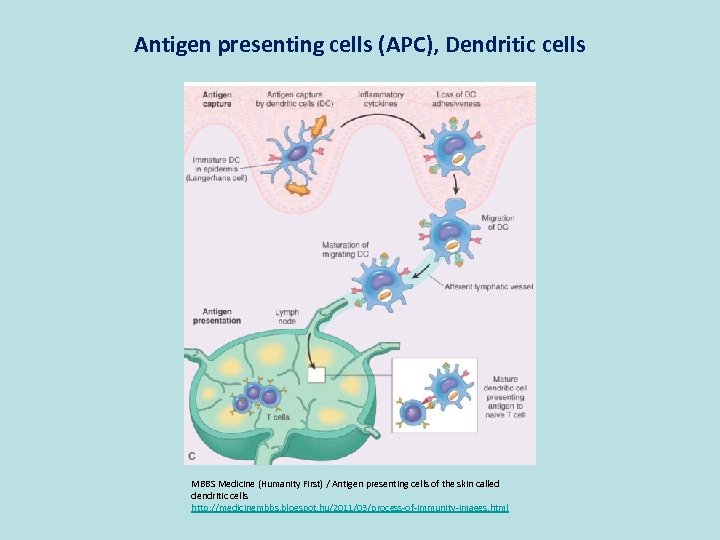
Antigen presenting cells (APC), Dendritic cells MBBS Medicine (Humanity First) / Antigen presenting cells of the skin called dendritic cells http: //medicinembbs. blogspot. hu/2011/03/process-of-immunity-images. html
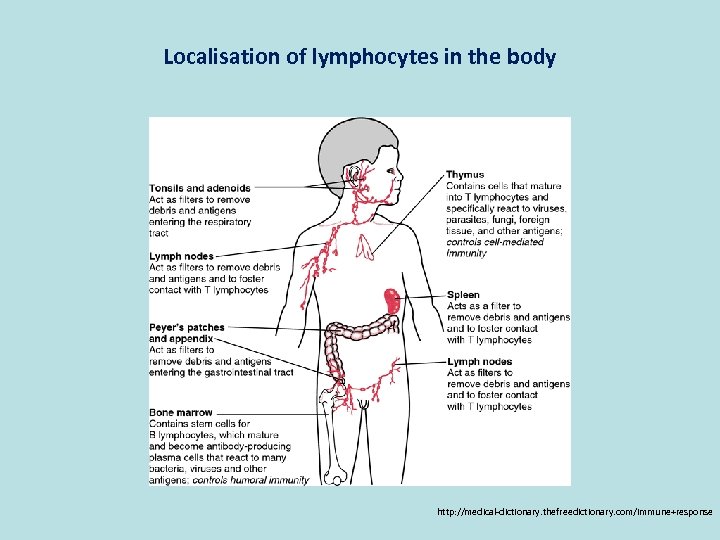
Localisation of lymphocytes in the body http: //medical-dictionary. thefreedictionary. com/immune+response
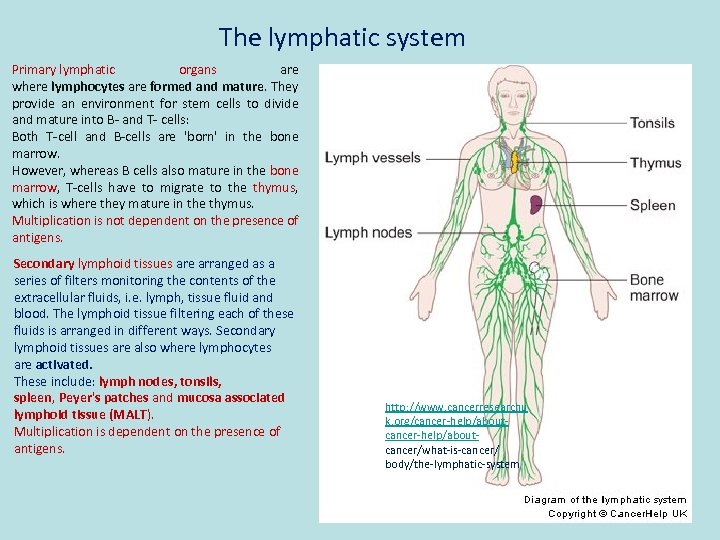
The lymphatic system Primary lymphatic organs are where lymphocytes are formed and mature. They provide an environment for stem cells to divide and mature into B- and T- cells: Both T-cell and B-cells are 'born' in the bone marrow. However, whereas B cells also mature in the bone marrow, T-cells have to migrate to the thymus, which is where they mature in the thymus. Multiplication is not dependent on the presence of antigens. Secondary lymphoid tissues are arranged as a series of filters monitoring the contents of the extracellular fluids, i. e. lymph, tissue fluid and blood. The lymphoid tissue filtering each of these fluids is arranged in different ways. Secondary lymphoid tissues are also where lymphocytes are activated. These include: lymph nodes, tonsils, spleen, Peyer's patches and mucosa associated lymphoid tissue (MALT). Multiplication is dependent on the presence of antigens. http: //www. cancerresearchu k. org/cancer-help/aboutcancer/what-is-cancer/ body/the-lymphatic-system
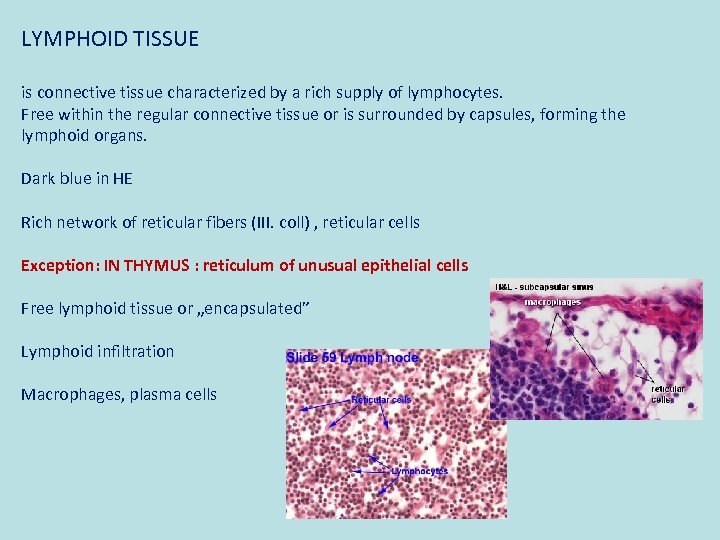
LYMPHOID TISSUE is connective tissue characterized by a rich supply of lymphocytes. Free within the regular connective tissue or is surrounded by capsules, forming the lymphoid organs. Dark blue in HE Rich network of reticular fibers (III. coll) , reticular cells Exception: IN THYMUS : reticulum of unusual epithelial cells Free lymphoid tissue or „encapsulated” Lymphoid infiltration Macrophages, plasma cells
Primary lymphoid organs (human)
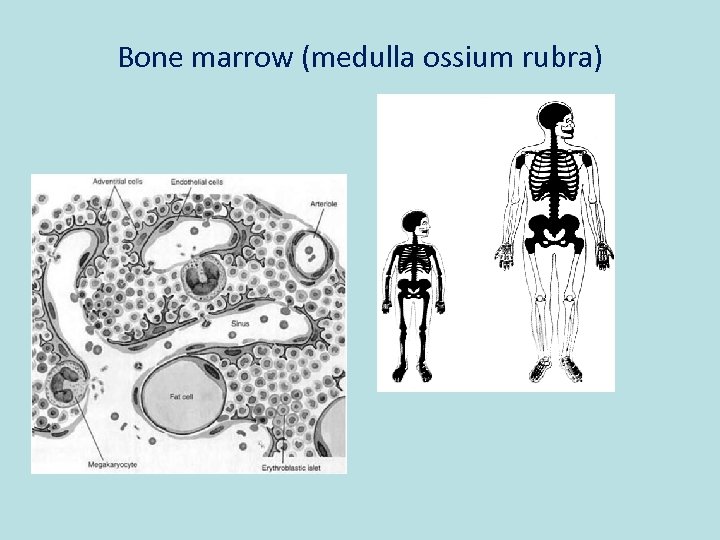
Bone marrow (medulla ossium rubra)
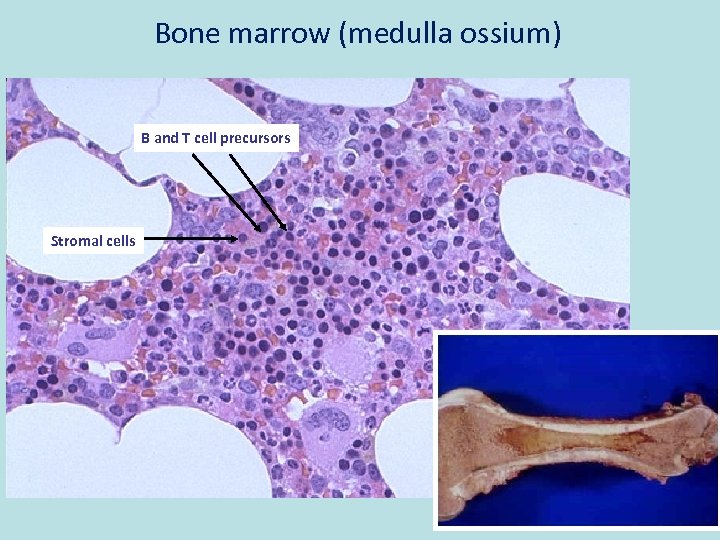
Bone marrow (medulla ossium) B and T cell precursors Stromal cells
T for thymus
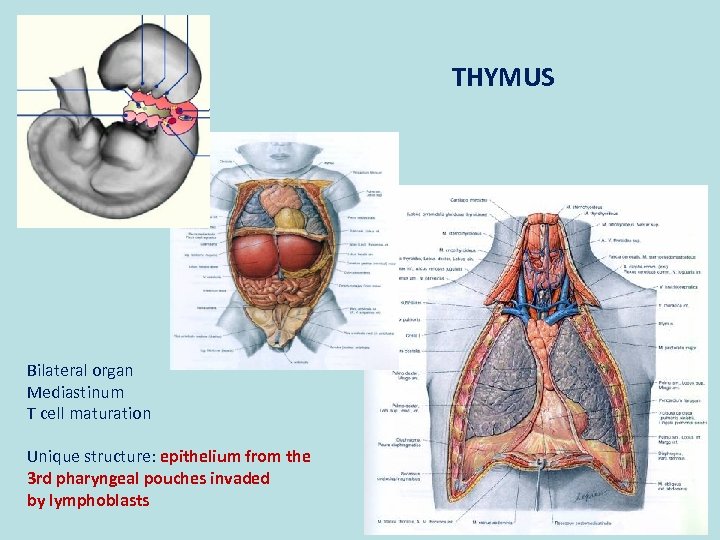
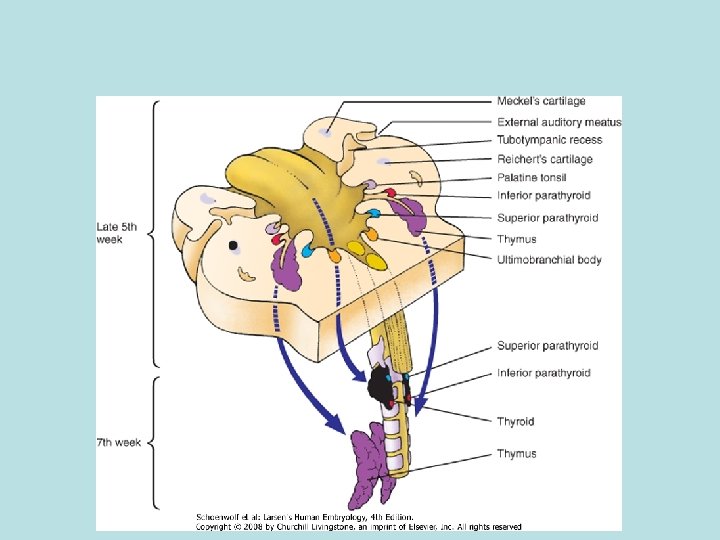
THYMUS Bilateral organ Mediastinum T cell maturation Unique structure: epithelium from the 3 rd pharyngeal pouches invaded by lymphoblasts
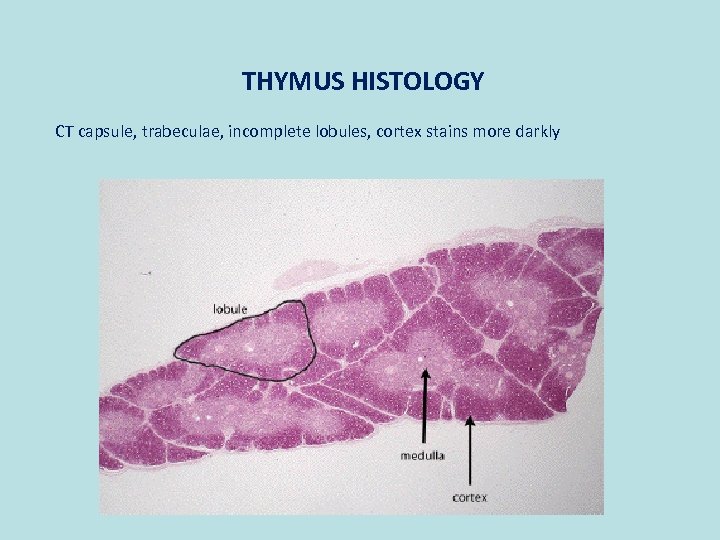
THYMUS HISTOLOGY CT capsule, trabeculae, incomplete lobules, cortex stains more darkly
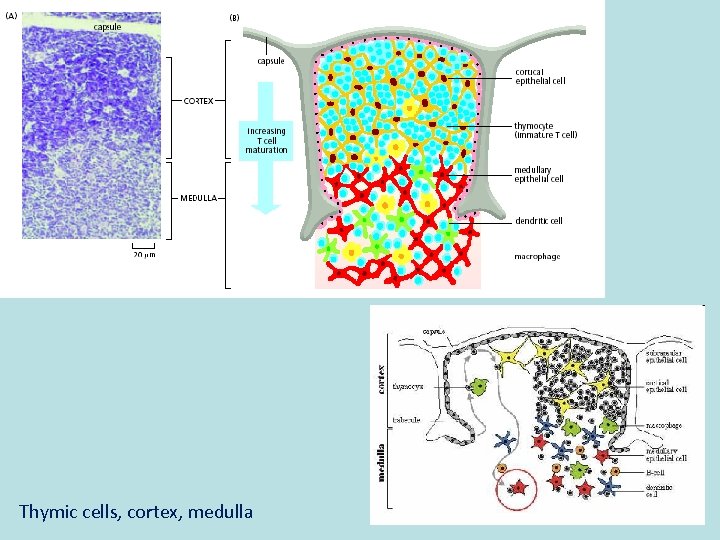
Thymic cells, cortex, medulla
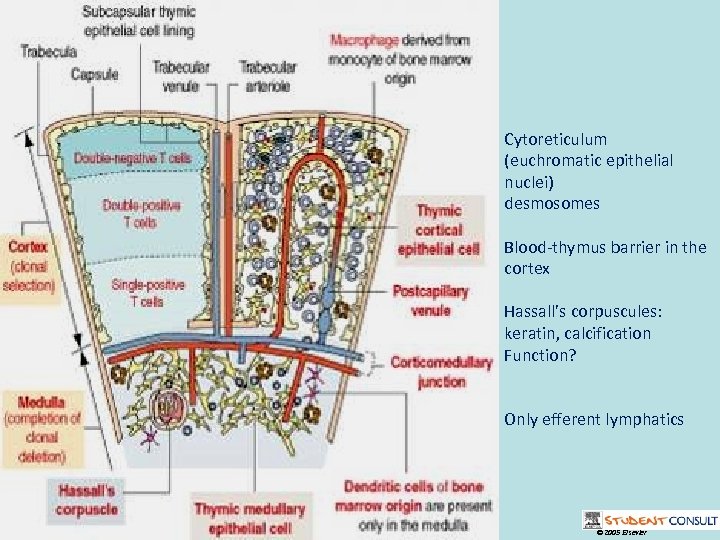
Cytoreticulum (euchromatic epithelial nuclei) desmosomes Blood-thymus barrier in the cortex Hassall’s corpuscules: keratin, calcification Function? Only efferent lymphatics © 2005 Elsevier
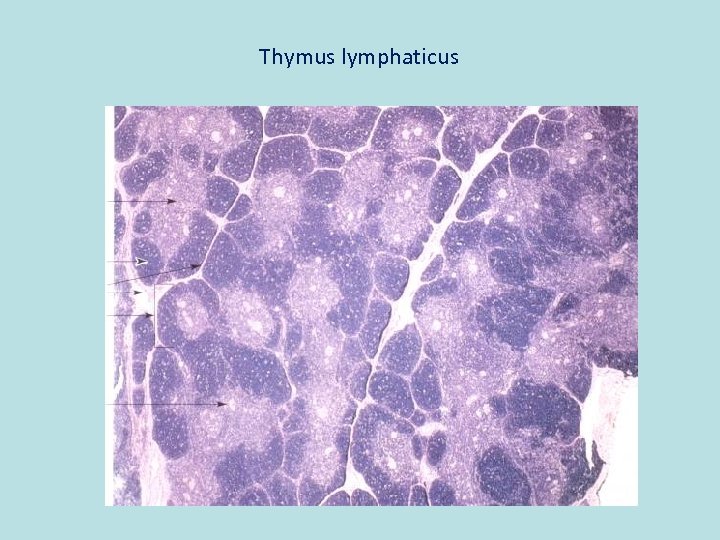
Thymus lymphaticus
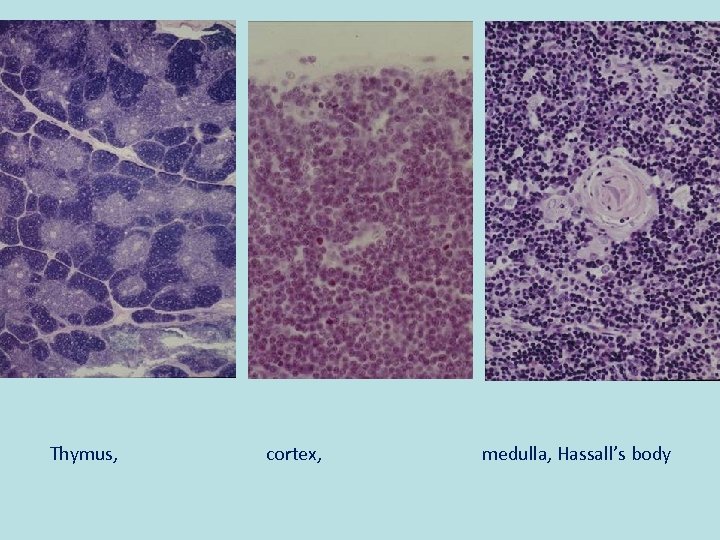
Thymus, cortex, medulla, Hassall’s body
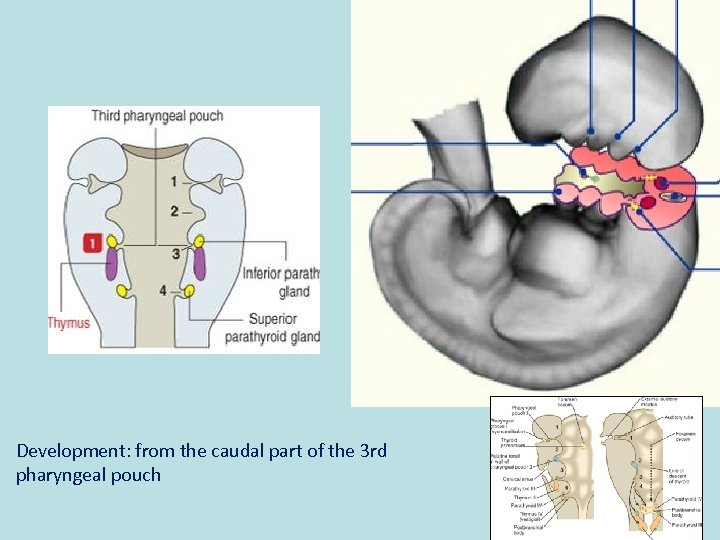
Development: from the caudal part of the 3 rd pharyngeal pouch
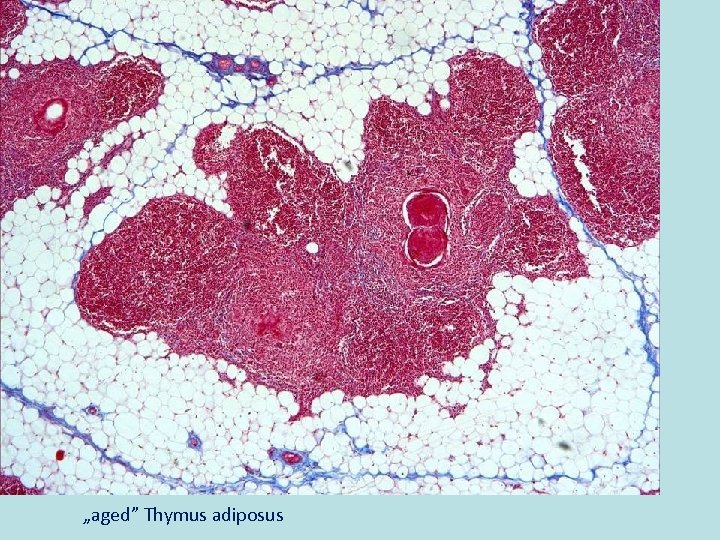
„aged” Thymus adiposus
Secondary lymphoid organs (human)
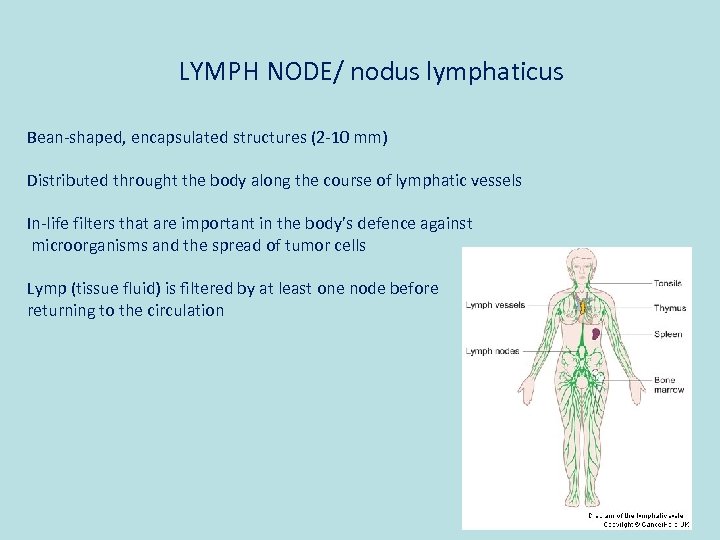
LYMPH NODE/ nodus lymphaticus Bean-shaped, encapsulated structures (2 -10 mm) Distributed throught the body along the course of lymphatic vessels In-life filters that are important in the body’s defence against microorganisms and the spread of tumor cells Lymp (tissue fluid) is filtered by at least one node before returning to the circulation
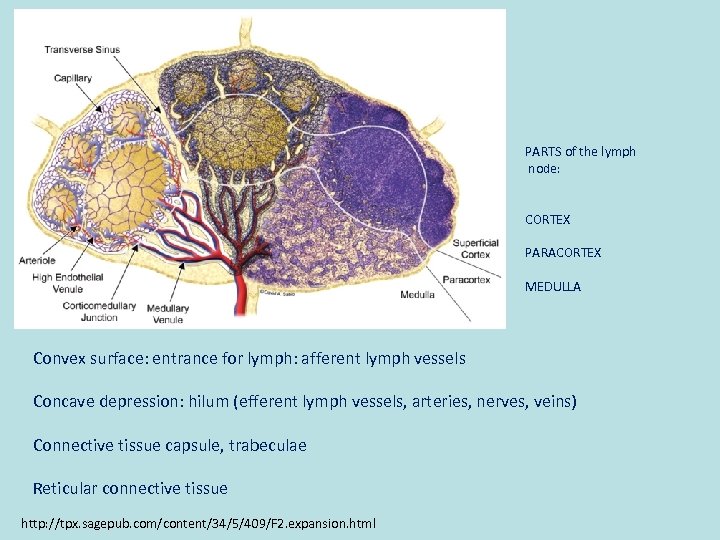
PARTS of the lymph node: CORTEX PARACORTEX MEDULLA Convex surface: entrance for lymph: afferent lymph vessels Concave depression: hilum (efferent lymph vessels, arteries, nerves, veins) Connective tissue capsule, trabeculae Reticular connective tissue http: //tpx. sagepub. com/content/34/5/409/F 2. expansion. html
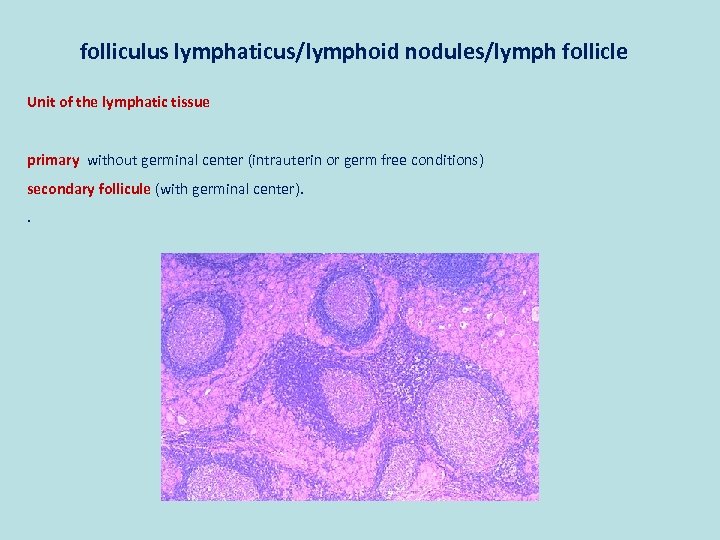
folliculus lymphaticus/lymphoid nodules/lymph follicle Unit of the lymphatic tissue primary without germinal center (intrauterin or germ free conditions) secondary follicule (with germinal center). .
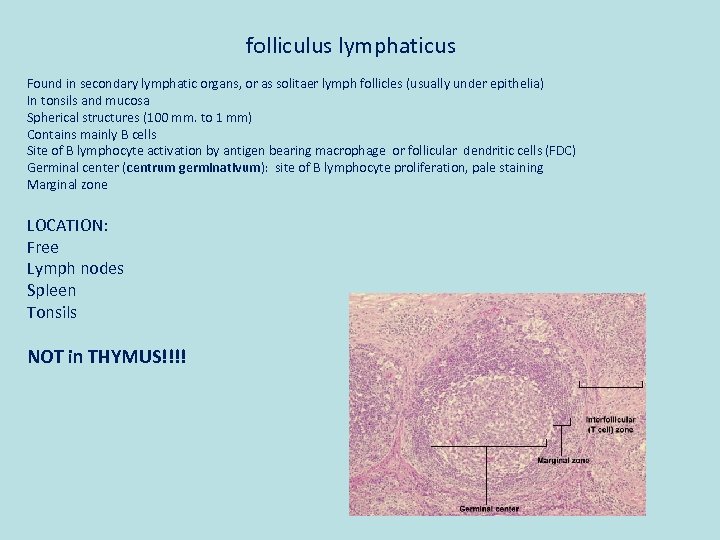
folliculus lymphaticus Found in secondary lymphatic organs, or as solitaer lymph follicles (usually under epithelia) In tonsils and mucosa Spherical structures (100 mm. to 1 mm) Contains mainly B cells Site of B lymphocyte activation by antigen bearing macrophage or follicular dendritic cells (FDC) Germinal center (centrum germinativum): site of B lymphocyte proliferation, pale staining Marginal zone LOCATION: Free Lymph nodes Spleen Tonsils NOT in THYMUS!!!!
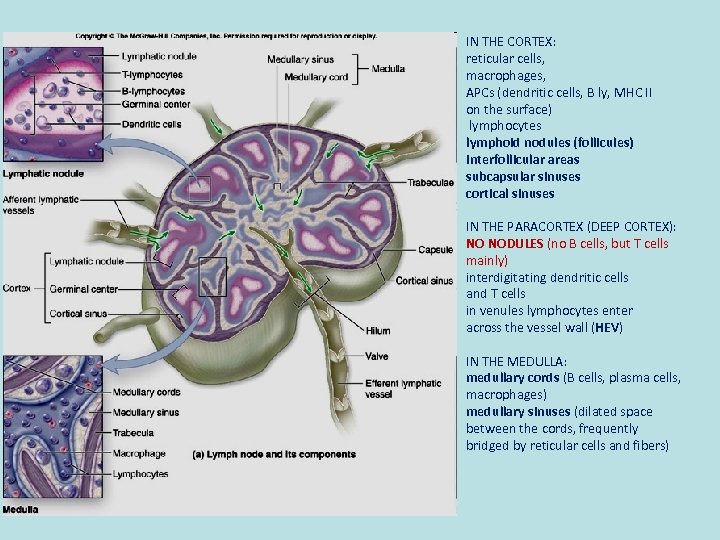
IN THE CORTEX: reticular cells, macrophages, APCs (dendritic cells, B ly, MHC II on the surface) lymphocytes lymphoid nodules (follicules) interfollicular areas subcapsular sinuses cortical sinuses IN THE PARACORTEX (DEEP CORTEX): NO NODULES (no B cells, but T cells mainly) interdigitating dendritic cells and T cells in venules lymphocytes enter across the vessel wall (HEV) IN THE MEDULLA: medullary cords (B cells, plasma cells, macrophages) medullary sinuses (dilated space between the cords, frequently bridged by reticular cells and fibers)
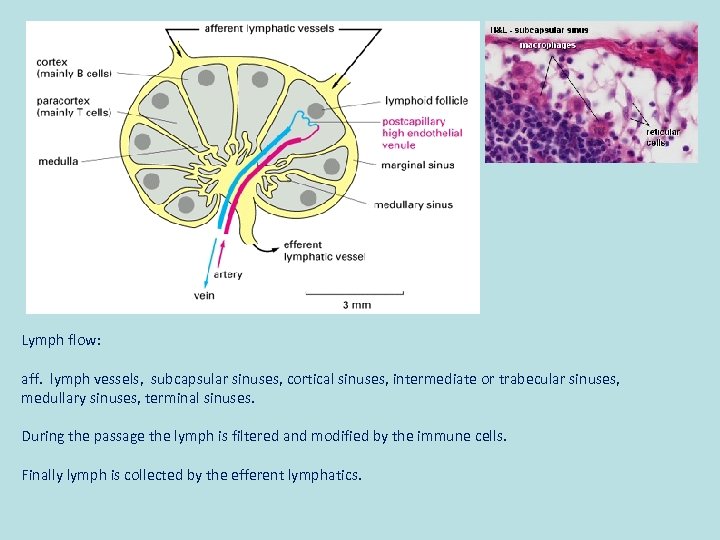
Lymph flow: aff. lymph vessels, subcapsular sinuses, cortical sinuses, intermediate or trabecular sinuses, medullary sinuses, terminal sinuses. During the passage the lymph is filtered and modified by the immune cells. Finally lymph is collected by the efferent lymphatics.
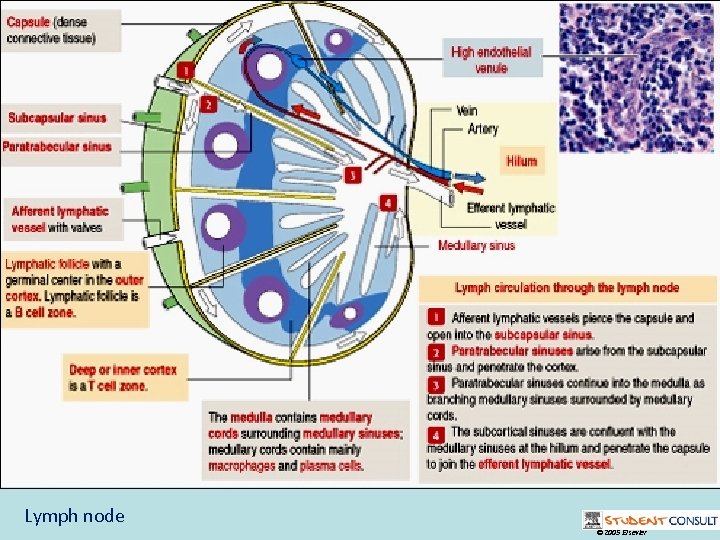
Lymph node © 2005 Elsevier
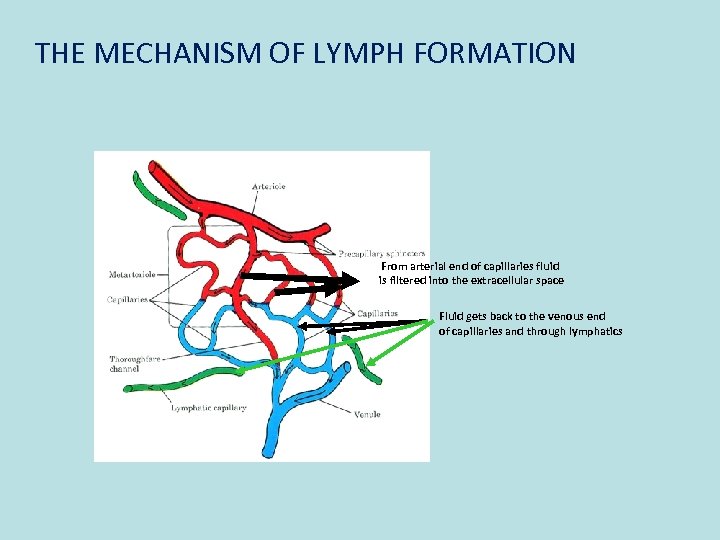
THE MECHANISM OF LYMPH FORMATION From arterial end of capillaries fluid is filtered into the extracellular space Fluid gets back to the venous end of capillaries and through lymphatics
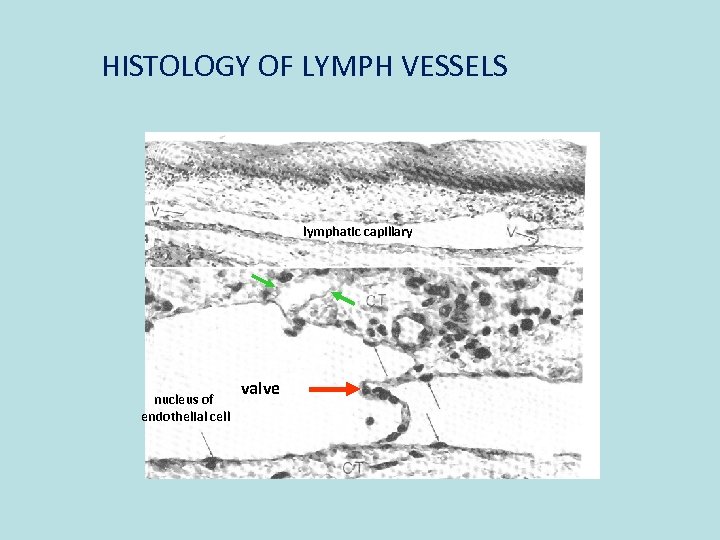
HISTOLOGY OF LYMPH VESSELS lymphatic capillary nucleus of endothelial cell valve
SPLEEN/LIEN
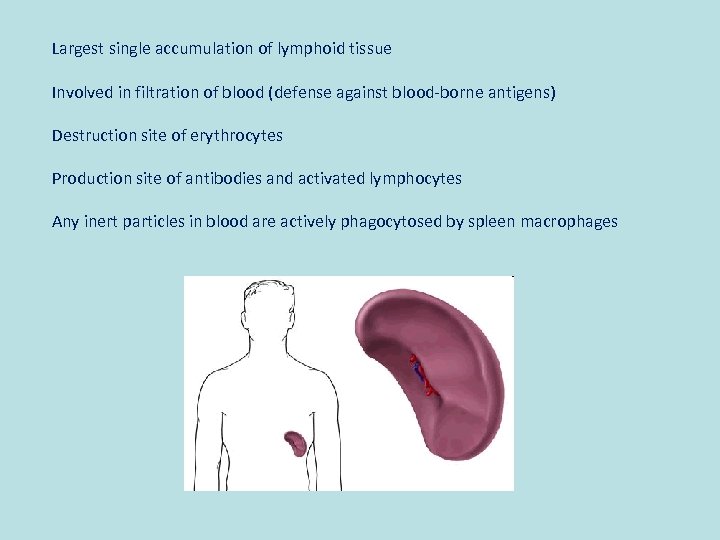
Largest single accumulation of lymphoid tissue Involved in filtration of blood (defense against blood-borne antigens) Destruction site of erythrocytes Production site of antibodies and activated lymphocytes Any inert particles in blood are actively phagocytosed by spleen macrophages
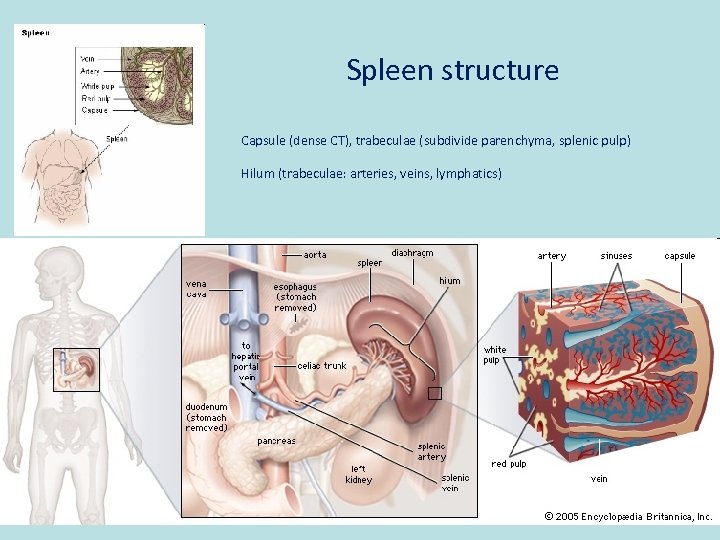
Spleen structure Capsule (dense CT), trabeculae (subdivide parenchyma, splenic pulp) Hilum (trabeculae: arteries, veins, lymphatics)
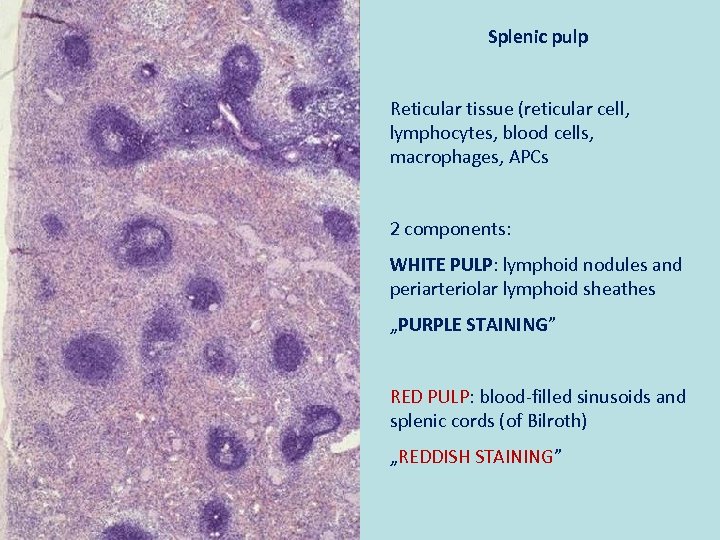
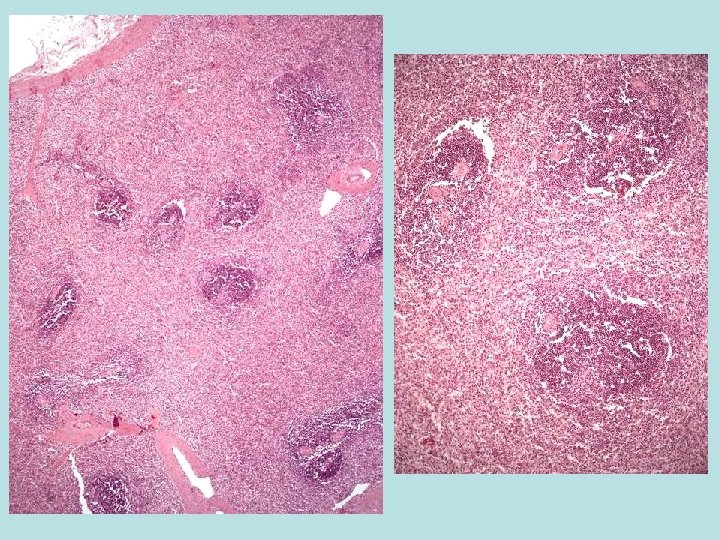
Splenic pulp Reticular tissue (reticular cell, lymphocytes, blood cells, macrophages, APCs 2 components: WHITE PULP: lymphoid nodules and periarteriolar lymphoid sheathes „PURPLE STAINING” RED PULP: blood-filled sinusoids and splenic cords (of Bilroth) „REDDISH STAINING”
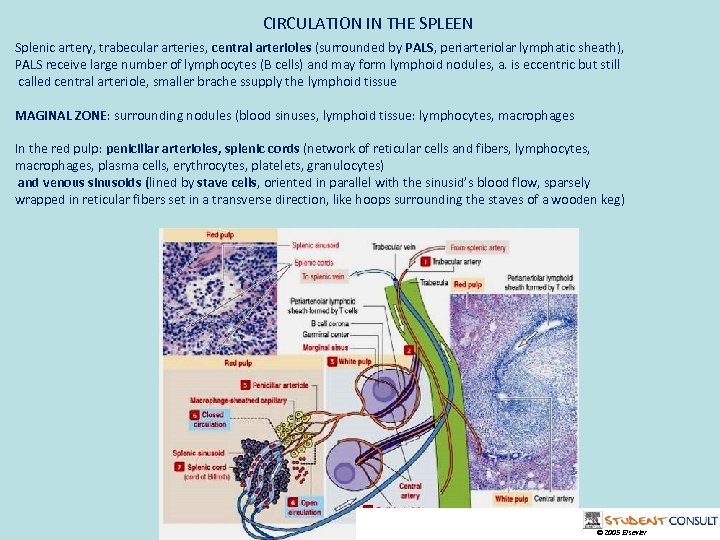
CIRCULATION IN THE SPLEEN Splenic artery, trabecular arteries, central arterioles (surrounded by PALS, periarteriolar lymphatic sheath), PALS receive large number of lymphocytes (B cells) and may form lymphoid nodules, a. is eccentric but still called central arteriole, smaller brache ssupply the lymphoid tissue MAGINAL ZONE: surrounding nodules (blood sinuses, lymphoid tissue: lymphocytes, macrophages In the red pulp: penicillar arterioles, splenic cords (network of reticular cells and fibers, lymphocytes, macrophages, plasma cells, erythrocytes, platelets, granulocytes) and venous sinusoids (lined by stave cells, oriented in parallel with the sinusid’s blood flow, sparsely wrapped in reticular fibers set in a transverse direction, like hoops surrounding the staves of a wooden keg) © 2005 Elsevier
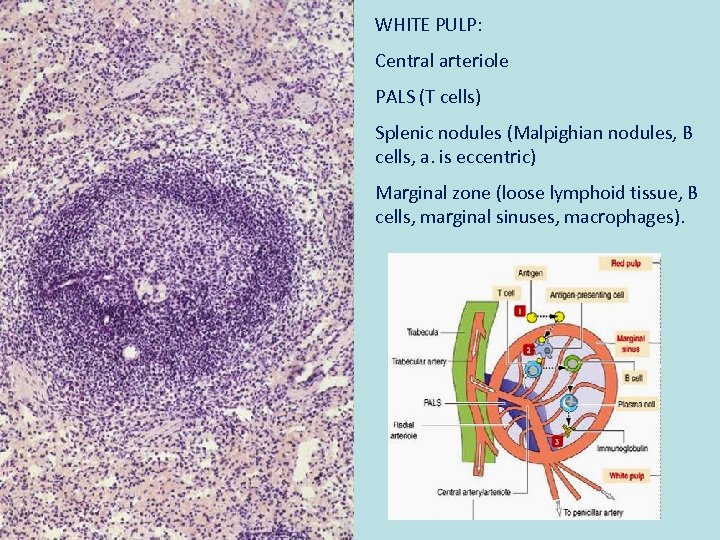
WHITE PULP: Central arteriole PALS (T cells) Splenic nodules (Malpighian nodules, B cells, a. is eccentric) Marginal zone (loose lymphoid tissue, B cells, marginal sinuses, macrophages).
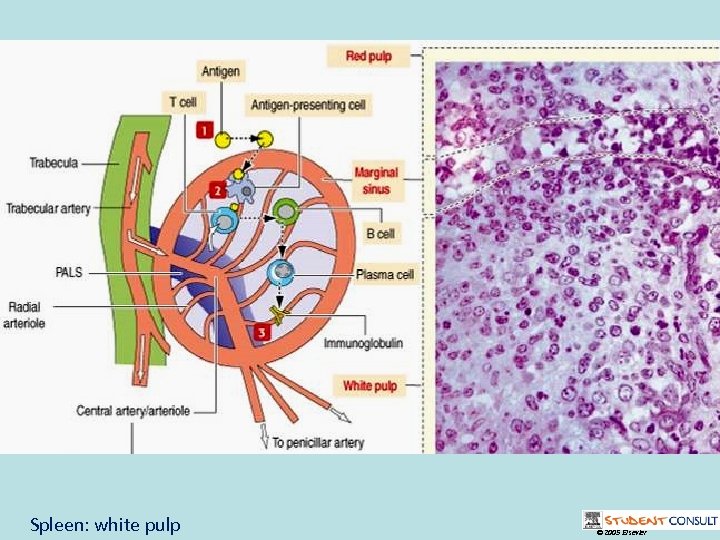
Spleen: white pulp © 2005 Elsevier
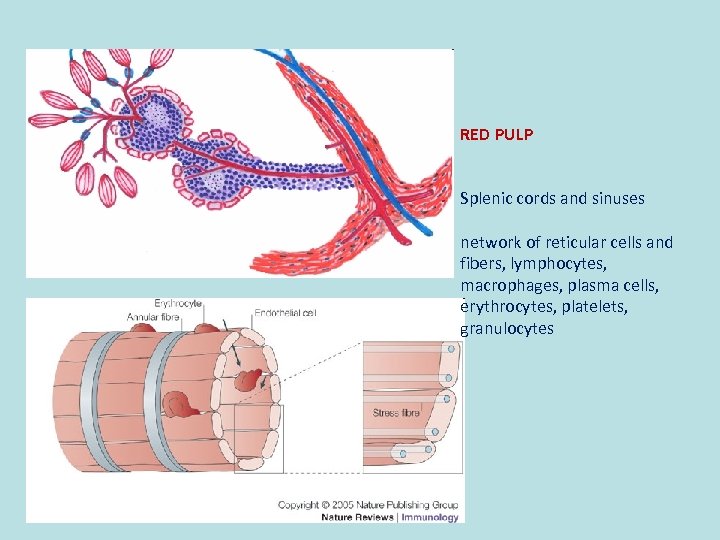
RED PULP Splenic cords and sinuses network of reticular cells and fibers, lymphocytes, macrophages, plasma cells, erythrocytes, platelets, granulocytes
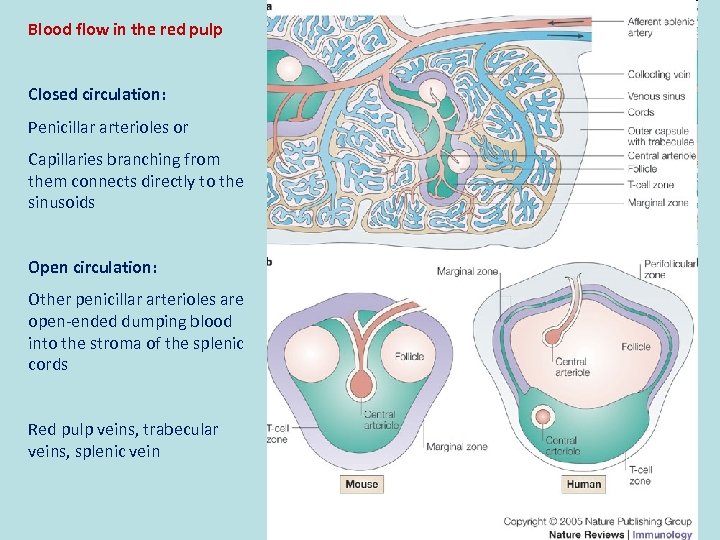
Blood flow in the red pulp Closed circulation: Penicillar arterioles or Capillaries branching from them connects directly to the sinusoids Open circulation: Other penicillar arterioles are open-ended dumping blood into the stroma of the splenic cords Red pulp veins, trabecular veins, splenic vein
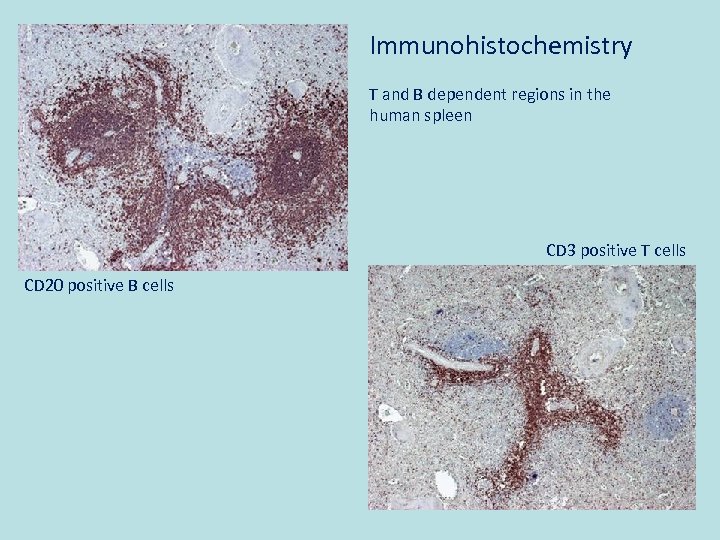
Immunohistochemistry T and B dependent regions in the human spleen CD 3 positive T cells CD 20 positive B cells
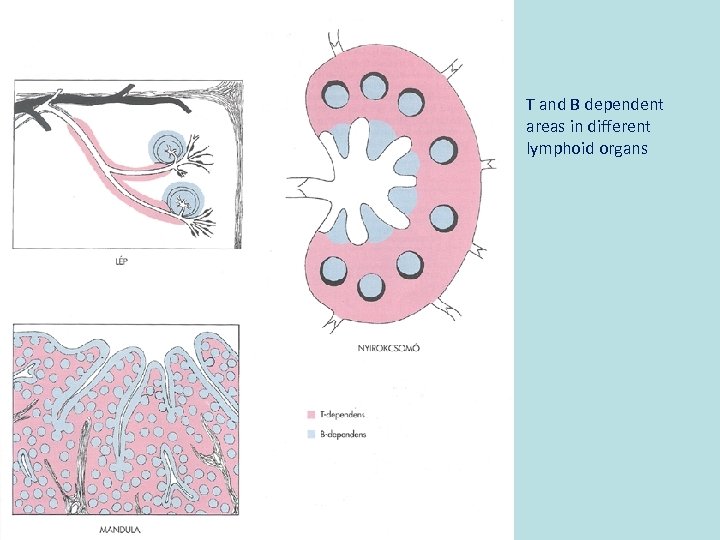
T and B dependent areas in different lymphoid organs
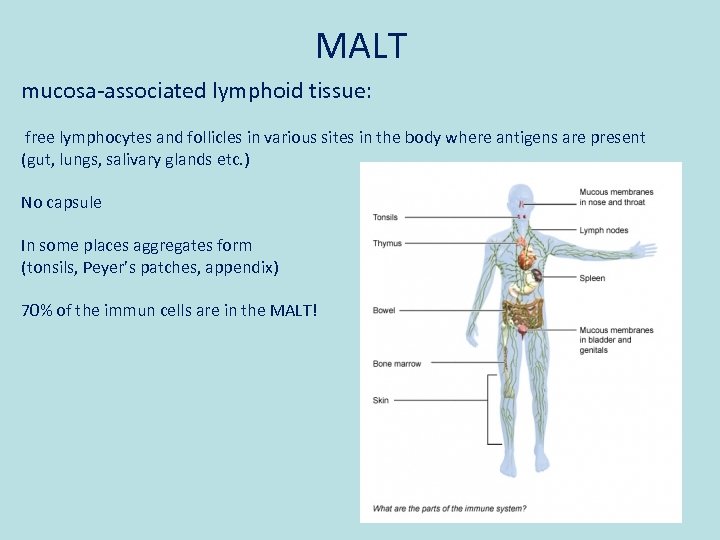
MALT mucosa-associated lymphoid tissue: free lymphocytes and follicles in various sites in the body where antigens are present (gut, lungs, salivary glands etc. ) No capsule In some places aggregates form (tonsils, Peyer’s patches, appendix) 70% of the immun cells are in the MALT!
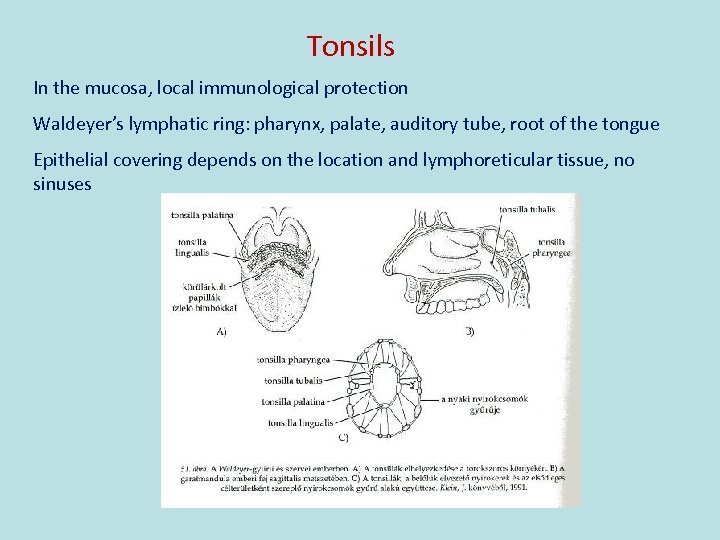
Tonsils In the mucosa, local immunological protection Waldeyer’s lymphatic ring: pharynx, palate, auditory tube, root of the tongue Epithelial covering depends on the location and lymphoreticular tissue, no sinuses
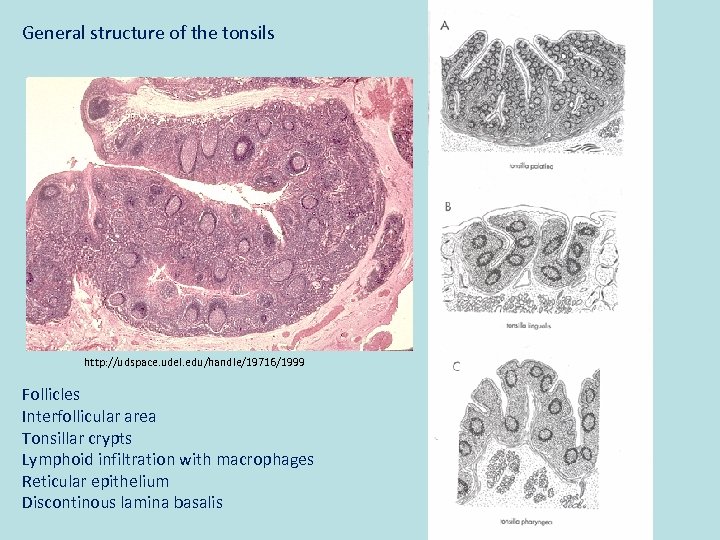
General structure of the tonsils http: //udspace. udel. edu/handle/19716/1999 Follicles Interfollicular area Tonsillar crypts Lymphoid infiltration with macrophages Reticular epithelium Discontinous lamina basalis
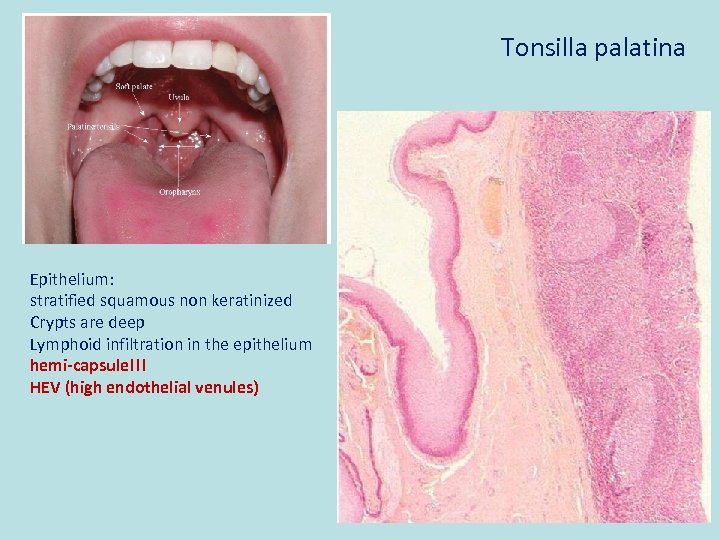
Tonsilla palatina Epithelium: stratified squamous non keratinized Crypts are deep Lymphoid infiltration in the epithelium hemi-capsule!!! HEV (high endothelial venules)
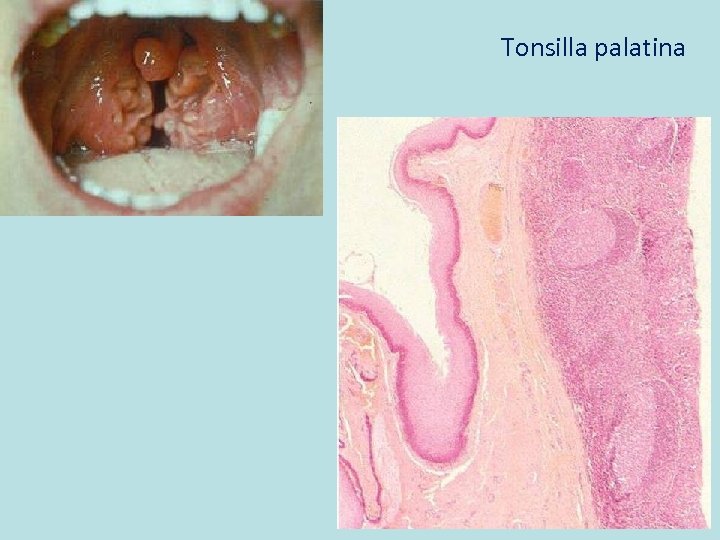
Tonsilla palatina
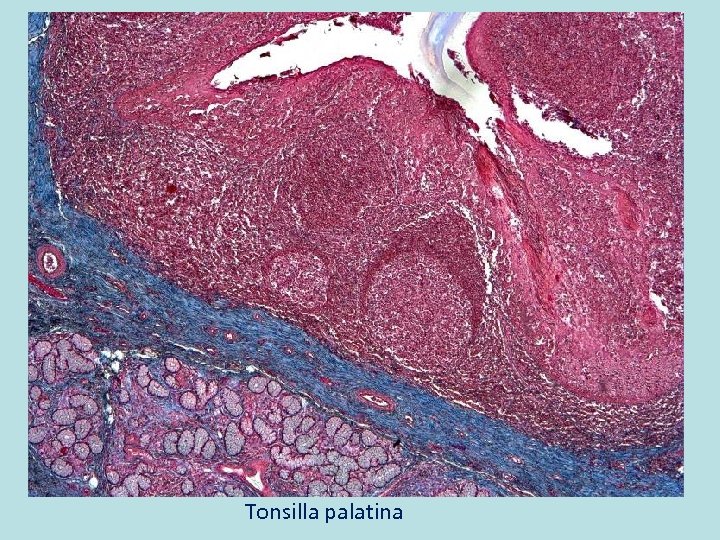
Tonsilla palatina
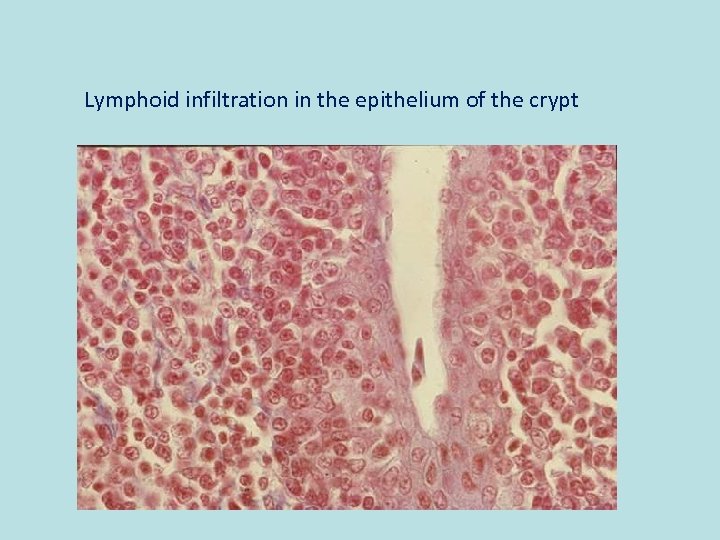
Lymphoid infiltration in the epithelium of the crypt
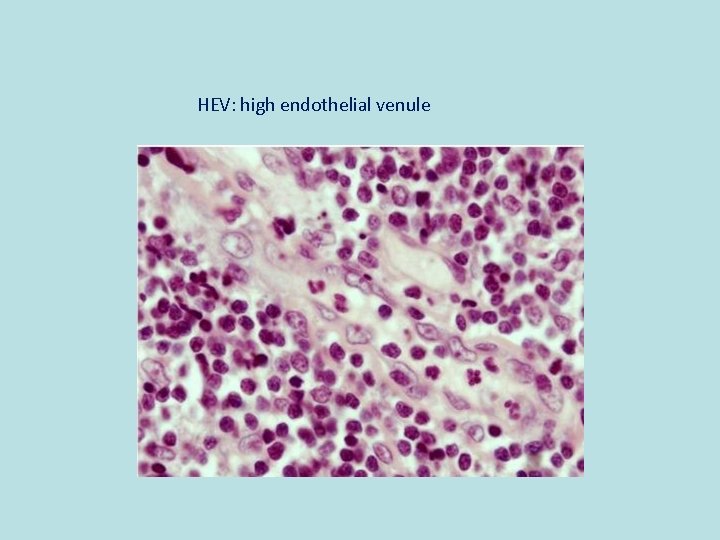
HEV: high endothelial venule
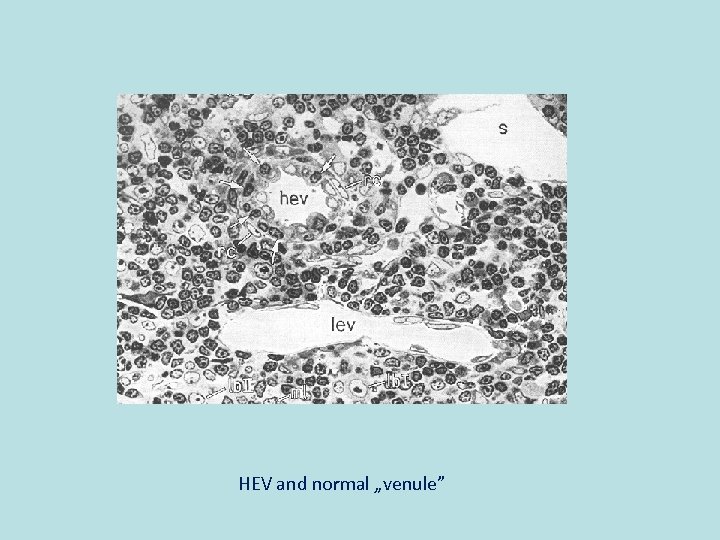
HEV and normal „venule”
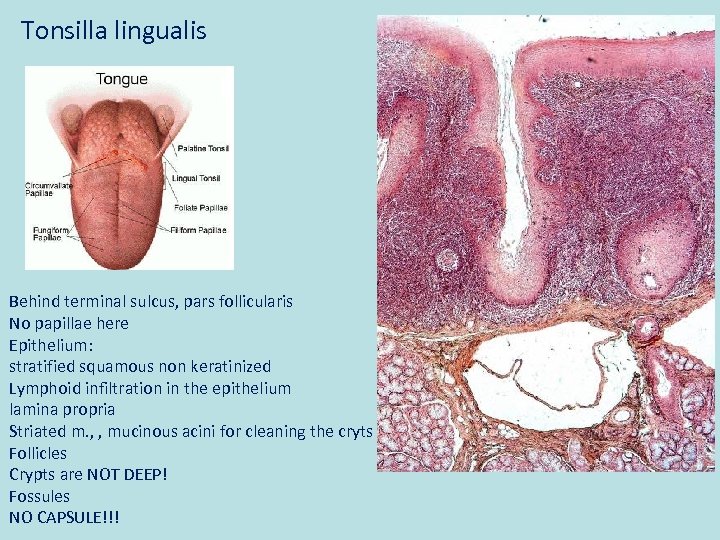
Tonsilla lingualis Behind terminal sulcus, pars follicularis No papillae here Epithelium: stratified squamous non keratinized Lymphoid infiltration in the epithelium lamina propria Striated m. , , mucinous acini for cleaning the cryts Follicles Crypts are NOT DEEP! Fossules NO CAPSULE!!!
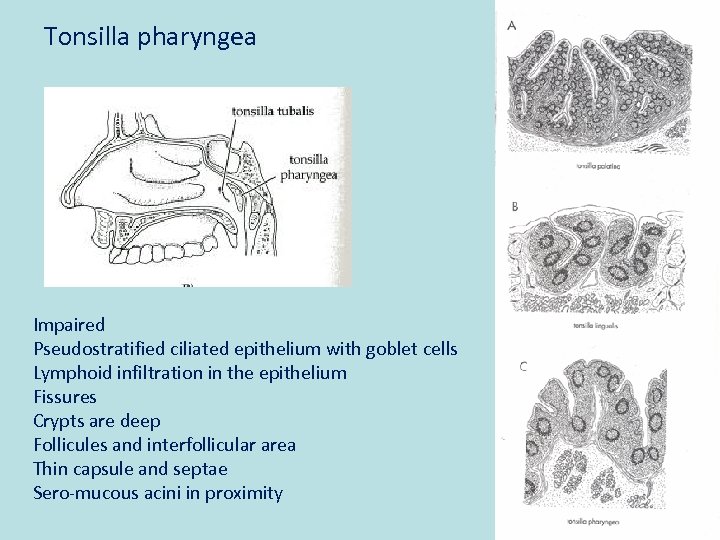
Tonsilla pharyngea Impaired Pseudostratified ciliated epithelium with goblet cells Lymphoid infiltration in the epithelium Fissures Crypts are deep Follicules and interfollicular area Thin capsule and septae Sero-mucous acini in proximity
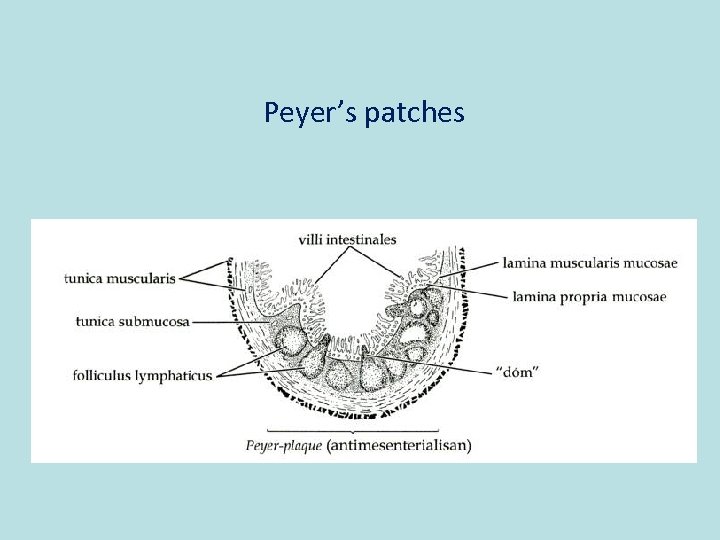
Peyer’s patches
Thank you for attention!
References: „Szövettan” edited by Röhlich Pál (SE) Molecular cell biology, Lodish et al. Molecular biology of the cell, Alberts et al. http: //www. emedinfo. com/blood-cells. html Co-authors of the lecture: Nóra Fejszák, Katalin Kocsis, Attila Magyar, Nándor Nagy
0f80763faa7edd0bd105df1de5c3727d.ppt