c40a2794deab0aec5aee5dffa42aed09.ppt
- Количество слайдов: 53
 Immune dysfunction in trauma and sepsis: Novel aspects of ubiquitin Matthias Majetschak, MD, Ph. D De. Witt Daughtry Family Department of Surgery Div. of Trauma and Surgical Critical Care
Immune dysfunction in trauma and sepsis: Novel aspects of ubiquitin Matthias Majetschak, MD, Ph. D De. Witt Daughtry Family Department of Surgery Div. of Trauma and Surgical Critical Care
 Ubiquitin Immune dysfunction in trauma and sepsis: Novel aspects of ubiquitin Immune dysfunction Ubiquitin - intracellular: the traditional view Ubiquitin – extracellular: novel aspects systemic and local release immunological actions clinical relevant effects possible mechanism
Ubiquitin Immune dysfunction in trauma and sepsis: Novel aspects of ubiquitin Immune dysfunction Ubiquitin - intracellular: the traditional view Ubiquitin – extracellular: novel aspects systemic and local release immunological actions clinical relevant effects possible mechanism
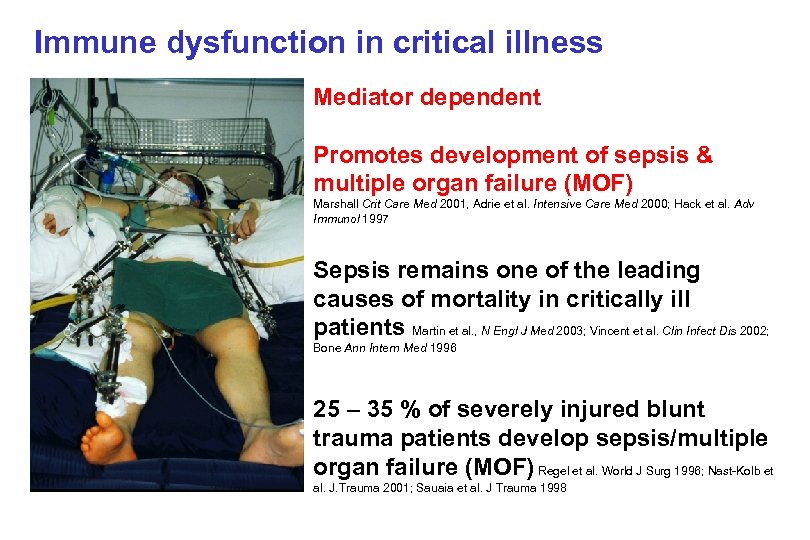 Immune dysfunction in critical illness Mediator dependent Promotes development of sepsis & multiple organ failure (MOF) Marshall Crit Care Med 2001, Adrie et al. Intensive Care Med 2000; Hack et al. Adv Immunol 1997 Sepsis remains one of the leading causes of mortality in critically ill patients Martin et al. , N Engl J Med 2003; Vincent et al. Clin Infect Dis 2002; Bone Ann Intern Med 1996 25 – 35 % of severely injured blunt trauma patients develop sepsis/multiple organ failure (MOF) Regel et al. World J Surg 1996; Nast-Kolb et al. J. Trauma 2001; Sauaia et al. J Trauma 1998
Immune dysfunction in critical illness Mediator dependent Promotes development of sepsis & multiple organ failure (MOF) Marshall Crit Care Med 2001, Adrie et al. Intensive Care Med 2000; Hack et al. Adv Immunol 1997 Sepsis remains one of the leading causes of mortality in critically ill patients Martin et al. , N Engl J Med 2003; Vincent et al. Clin Infect Dis 2002; Bone Ann Intern Med 1996 25 – 35 % of severely injured blunt trauma patients develop sepsis/multiple organ failure (MOF) Regel et al. World J Surg 1996; Nast-Kolb et al. J. Trauma 2001; Sauaia et al. J Trauma 1998
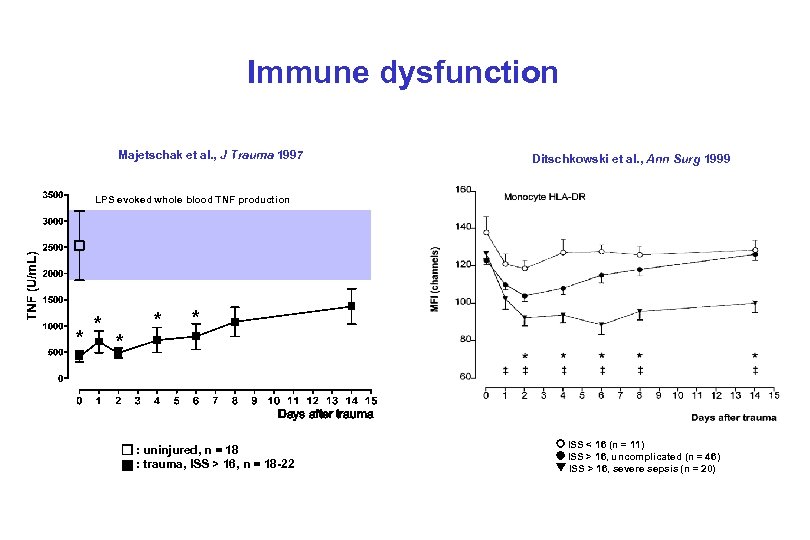 Immune dysfunction Majetschak et al. , J Trauma 1997 Ditschkowski et al. , Ann Surg 1999 LPS evoked whole blood TNF production * * * Days after trauma : : uninjured, n = 18 trauma, ISS > 16, n = 18 -22 ISS < 16 (n = 11) ISS > 16, uncomplicated (n = 46) ISS > 16, severe sepsis (n = 20)
Immune dysfunction Majetschak et al. , J Trauma 1997 Ditschkowski et al. , Ann Surg 1999 LPS evoked whole blood TNF production * * * Days after trauma : : uninjured, n = 18 trauma, ISS > 16, n = 18 -22 ISS < 16 (n = 11) ISS > 16, uncomplicated (n = 46) ISS > 16, severe sepsis (n = 20)
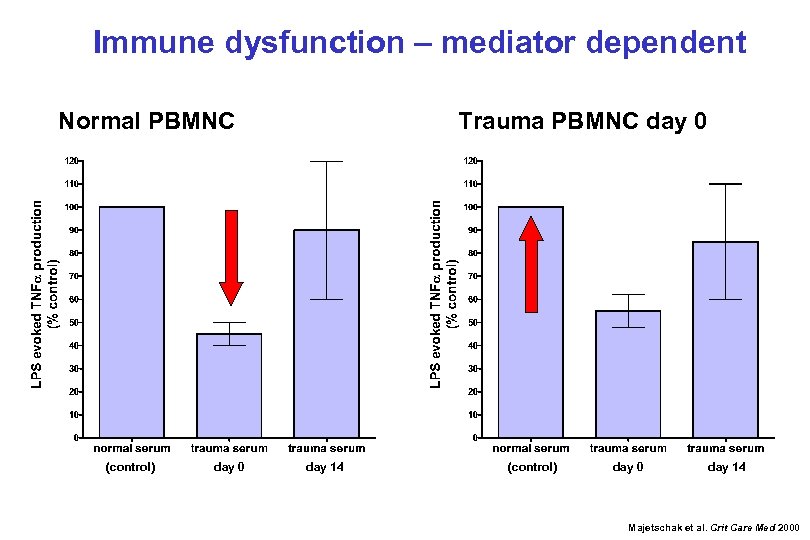 Immune dysfunction – mediator dependent Normal PBMNC (control) day 0 Trauma PBMNC day 0 day 14 (control) day 0 day 14 Majetschak et al. Crit Care Med 2000
Immune dysfunction – mediator dependent Normal PBMNC (control) day 0 Trauma PBMNC day 0 day 14 (control) day 0 day 14 Majetschak et al. Crit Care Med 2000
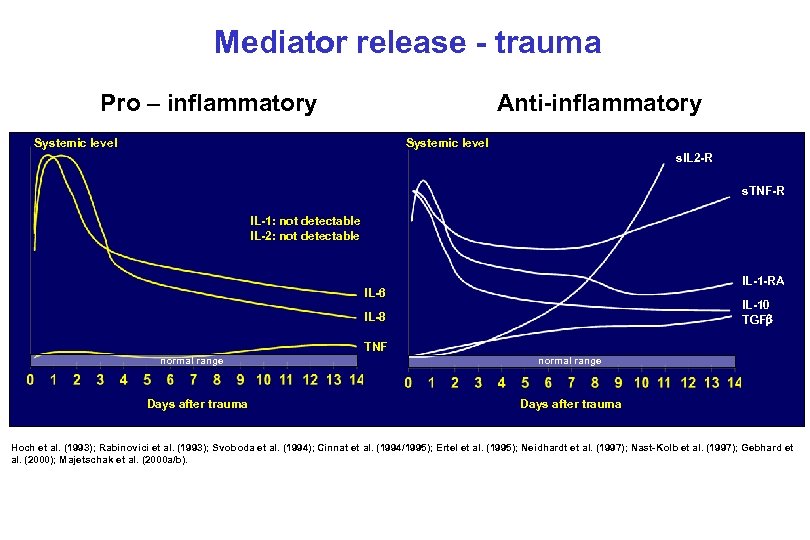 Mediator release - trauma Pro – inflammatory Anti-inflammatory Systemic level s. IL 2 -R s. TNF-R IL-1: not detectable IL-2: not detectable IL-1 -RA IL-6 IL-10 TGF IL-8 TNF normal range Days after trauma Hoch et al. (1993); Rabinovici et al. (1993); Svoboda et al. (1994); Cinnat et al. (1994/1995); Ertel et al. (1995); Neidhardt et al. (1997); Nast-Kolb et al. (1997); Gebhard et al. (2000); Majetschak et al. (2000 a/b).
Mediator release - trauma Pro – inflammatory Anti-inflammatory Systemic level s. IL 2 -R s. TNF-R IL-1: not detectable IL-2: not detectable IL-1 -RA IL-6 IL-10 TGF IL-8 TNF normal range Days after trauma Hoch et al. (1993); Rabinovici et al. (1993); Svoboda et al. (1994); Cinnat et al. (1994/1995); Ertel et al. (1995); Neidhardt et al. (1997); Nast-Kolb et al. (1997); Gebhard et al. (2000); Majetschak et al. (2000 a/b).
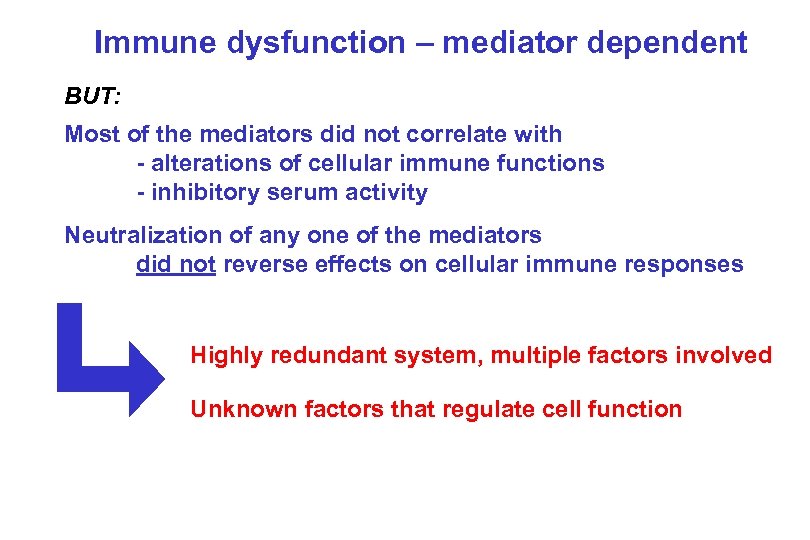 Immune dysfunction – mediator dependent BUT: Most of the mediators did not correlate with - alterations of cellular immune functions - inhibitory serum activity Neutralization of any one of the mediators did not reverse effects on cellular immune responses Highly redundant system, multiple factors involved Unknown factors that regulate cell function
Immune dysfunction – mediator dependent BUT: Most of the mediators did not correlate with - alterations of cellular immune functions - inhibitory serum activity Neutralization of any one of the mediators did not reverse effects on cellular immune responses Highly redundant system, multiple factors involved Unknown factors that regulate cell function
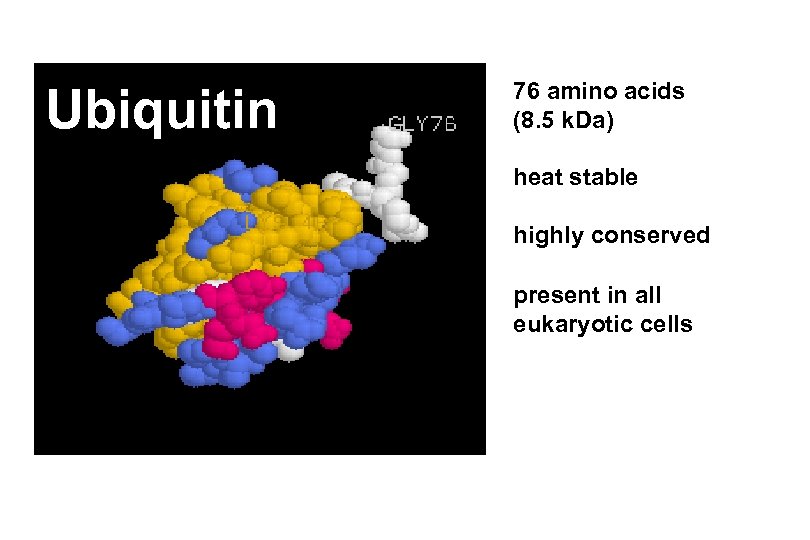 Ubiquitin 76 amino acids (8. 5 k. Da) heat stable highly conserved present in all eukaryotic cells
Ubiquitin 76 amino acids (8. 5 k. Da) heat stable highly conserved present in all eukaryotic cells
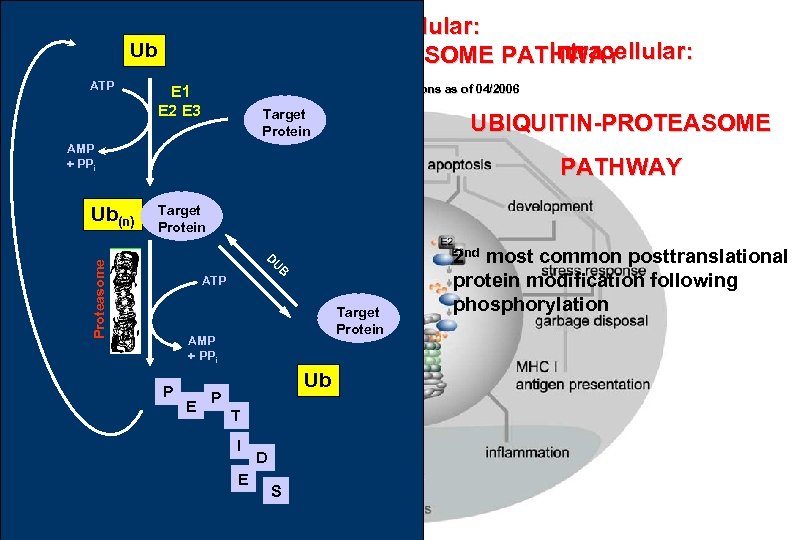 Intracellular: UBIQUITIN-PROTEASOME PATHWAY Ub ATP Pub. Med: 14, 932 citations as of 04/2006 E 1 E 2 E 3 Target Protein UBIQUITIN-PROTEASOME AMP + PPi Target Protein D U Proteasome Ub(n) PATHWAY B ATP Target Protein AMP + PPi P E Ub P T I E D S 2 nd most common posttranslational protein modification following phosphorylation
Intracellular: UBIQUITIN-PROTEASOME PATHWAY Ub ATP Pub. Med: 14, 932 citations as of 04/2006 E 1 E 2 E 3 Target Protein UBIQUITIN-PROTEASOME AMP + PPi Target Protein D U Proteasome Ub(n) PATHWAY B ATP Target Protein AMP + PPi P E Ub P T I E D S 2 nd most common posttranslational protein modification following phosphorylation
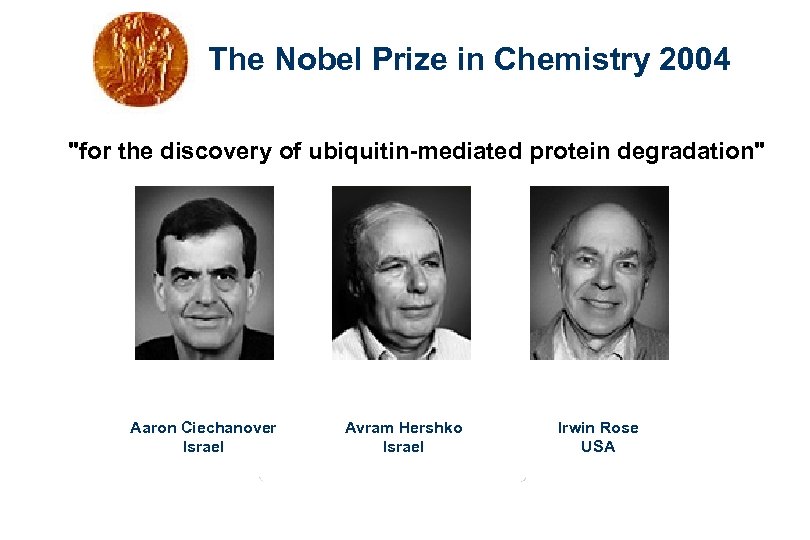 The Nobel Prize in Chemistry 2004 "for the discovery of ubiquitin-mediated protein degradation" Aaron Ciechanover Israel Avram Hershko Israel Irwin Rose USA
The Nobel Prize in Chemistry 2004 "for the discovery of ubiquitin-mediated protein degradation" Aaron Ciechanover Israel Avram Hershko Israel Irwin Rose USA
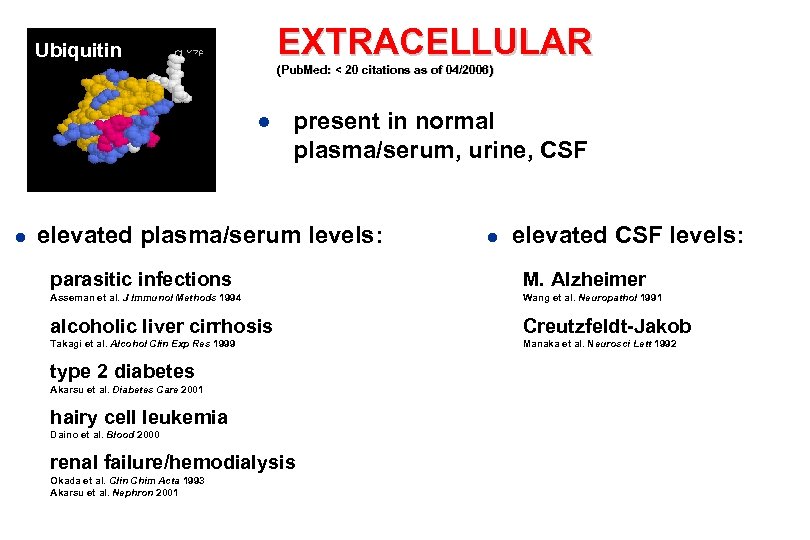 EXTRACELLULAR Ubiquitin (Pub. Med: < 20 citations as of 04/2006) ● present in normal plasma/serum, urine, CSF ● elevated plasma/serum levels: ● elevated CSF levels: parasitic infections M. Alzheimer Asseman et al. J Immunol Methods 1994 Wang et al. Neuropathol 1991 alcoholic liver cirrhosis Creutzfeldt-Jakob Takagi et al. Alcohol Clin Exp Res 1999 Manaka et al. Neurosci Lett 1992 type 2 diabetes Akarsu et al. Diabetes Care 2001 hairy cell leukemia Daino et al. Blood 2000 renal failure/hemodialysis Okada et al. Clin Chim Acta 1993 Akarsu et al. Nephron 2001
EXTRACELLULAR Ubiquitin (Pub. Med: < 20 citations as of 04/2006) ● present in normal plasma/serum, urine, CSF ● elevated plasma/serum levels: ● elevated CSF levels: parasitic infections M. Alzheimer Asseman et al. J Immunol Methods 1994 Wang et al. Neuropathol 1991 alcoholic liver cirrhosis Creutzfeldt-Jakob Takagi et al. Alcohol Clin Exp Res 1999 Manaka et al. Neurosci Lett 1992 type 2 diabetes Akarsu et al. Diabetes Care 2001 hairy cell leukemia Daino et al. Blood 2000 renal failure/hemodialysis Okada et al. Clin Chim Acta 1993 Akarsu et al. Nephron 2001
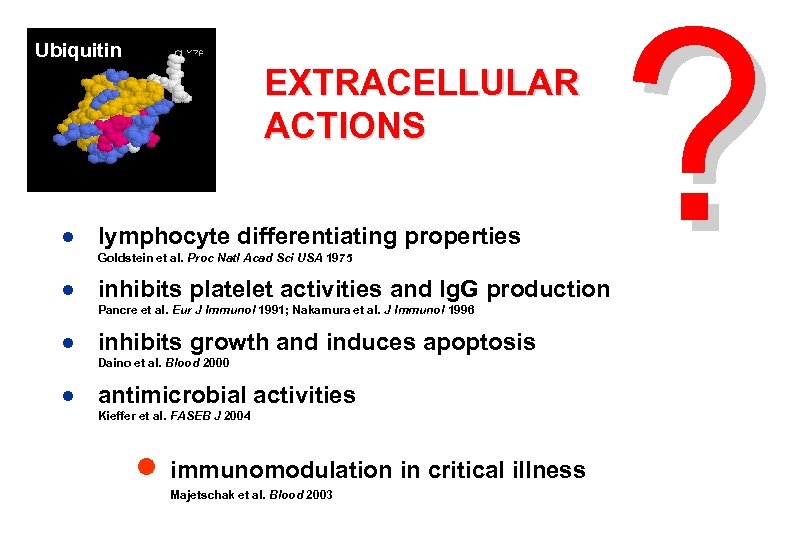 Ubiquitin EXTRACELLULAR ACTIONS ● lymphocyte differentiating properties Goldstein et al. Proc Natl Acad Sci USA 1975 ● inhibits platelet activities and Ig. G production Pancre et al. Eur J Immunol 1991; Nakamura et al. J Immunol 1996 ● inhibits growth and induces apoptosis Daino et al. Blood 2000 ● antimicrobial activities Kieffer et al. FASEB J 2004 ● immunomodulation in critical illness Majetschak et al. Blood 2003 ?
Ubiquitin EXTRACELLULAR ACTIONS ● lymphocyte differentiating properties Goldstein et al. Proc Natl Acad Sci USA 1975 ● inhibits platelet activities and Ig. G production Pancre et al. Eur J Immunol 1991; Nakamura et al. J Immunol 1996 ● inhibits growth and induces apoptosis Daino et al. Blood 2000 ● antimicrobial activities Kieffer et al. FASEB J 2004 ● immunomodulation in critical illness Majetschak et al. Blood 2003 ?
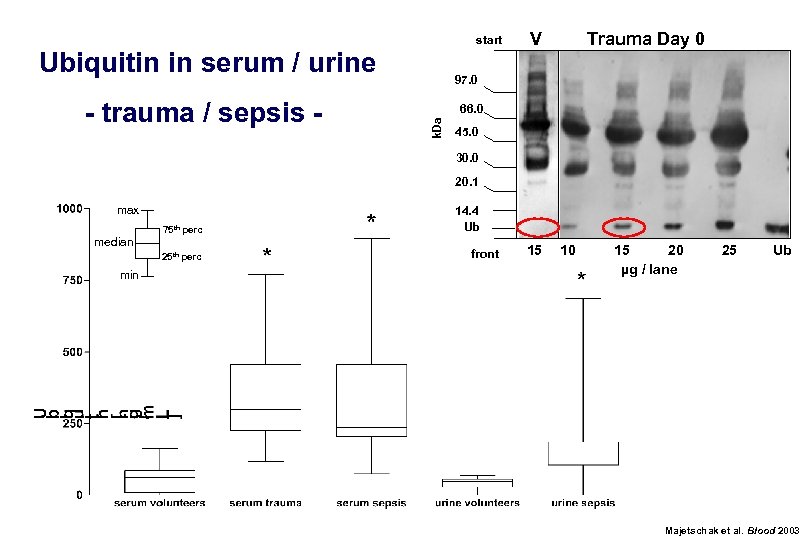 start Ubiquitin in serum / urine Trauma Day 0 97. 0 66. 0 k. Da - trauma / sepsis - V 45. 0 30. 0 20. 1 max median 75 th perc 25 th perc min 14. 4 Ub front 15 10 15 20 µg / lane 25 Ub Majetschak et al. Blood 2003
start Ubiquitin in serum / urine Trauma Day 0 97. 0 66. 0 k. Da - trauma / sepsis - V 45. 0 30. 0 20. 1 max median 75 th perc 25 th perc min 14. 4 Ub front 15 10 15 20 µg / lane 25 Ub Majetschak et al. Blood 2003
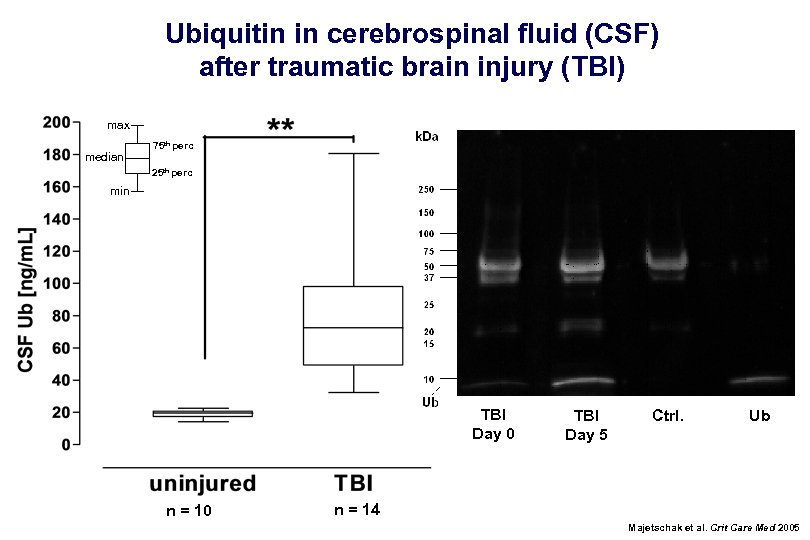 Ubiquitin in cerebrospinal fluid (CSF) after traumatic brain injury (TBI) max median 75 th perc 25 th perc min TBI Day 0 n = 10 TBI Day 5 Ctrl. Ub n = 14 Majetschak et al. Crit Care Med 2005
Ubiquitin in cerebrospinal fluid (CSF) after traumatic brain injury (TBI) max median 75 th perc 25 th perc min TBI Day 0 n = 10 TBI Day 5 Ctrl. Ub n = 14 Majetschak et al. Crit Care Med 2005
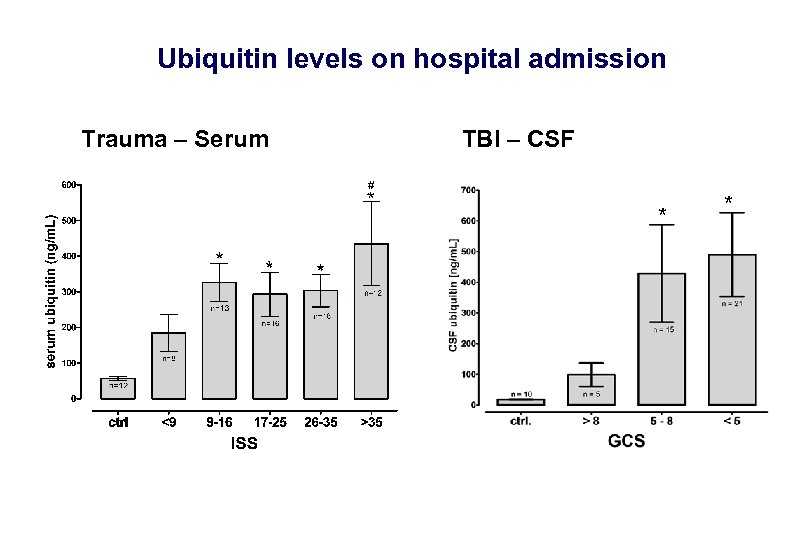 Ubiquitin levels on hospital admission Trauma – Serum TBI – CSF * *
Ubiquitin levels on hospital admission Trauma – Serum TBI – CSF * *
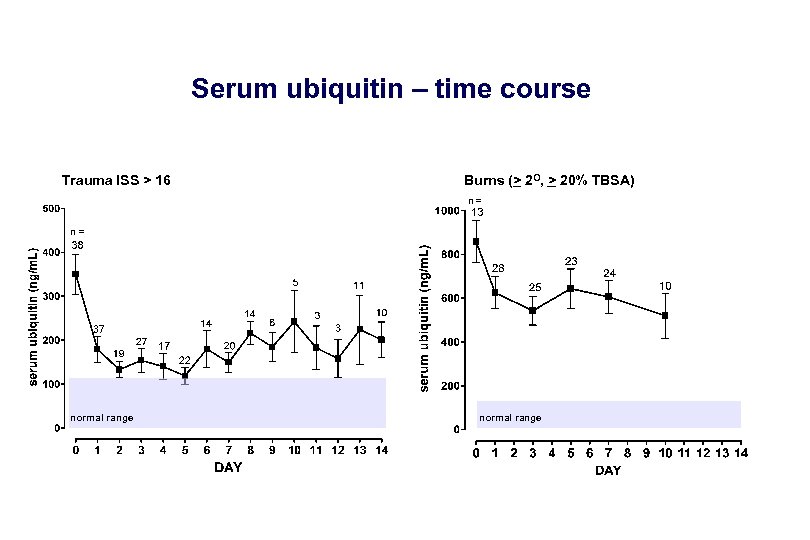 Serum ubiquitin – time course Trauma ISS > 16 Burns (> 2 O, > 20% TBSA) n= n= normal range
Serum ubiquitin – time course Trauma ISS > 16 Burns (> 2 O, > 20% TBSA) n= n= normal range
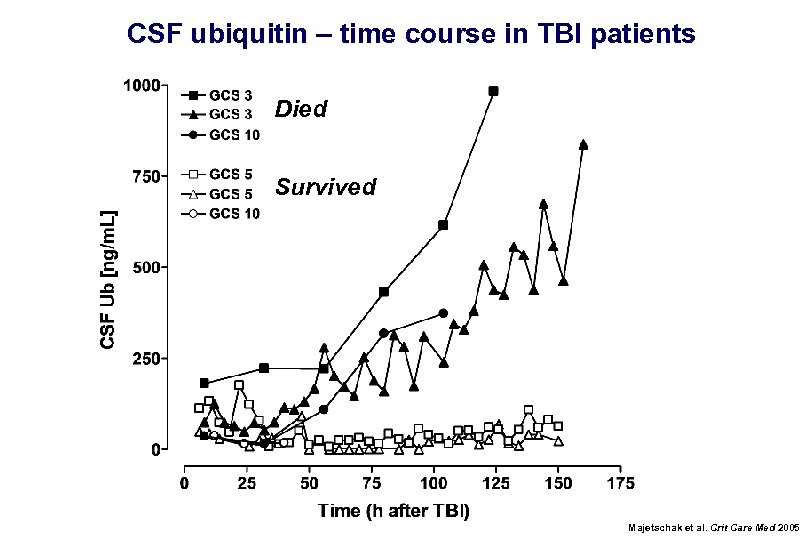 CSF ubiquitin – time course in TBI patients Died Survived Majetschak et al. Crit Care Med 2005
CSF ubiquitin – time course in TBI patients Died Survived Majetschak et al. Crit Care Med 2005
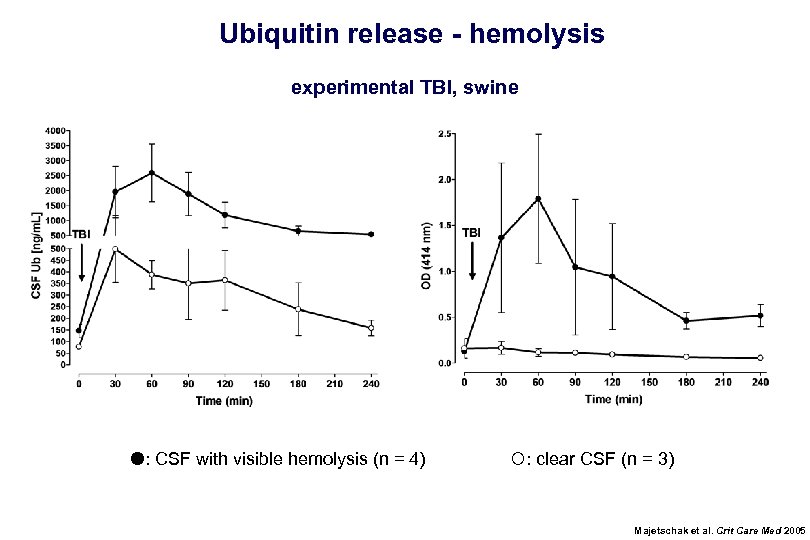 Ubiquitin release - hemolysis experimental TBI, swine : CSF with visible hemolysis (n = 4) : clear CSF (n = 3) Majetschak et al. Crit Care Med 2005
Ubiquitin release - hemolysis experimental TBI, swine : CSF with visible hemolysis (n = 4) : clear CSF (n = 3) Majetschak et al. Crit Care Med 2005
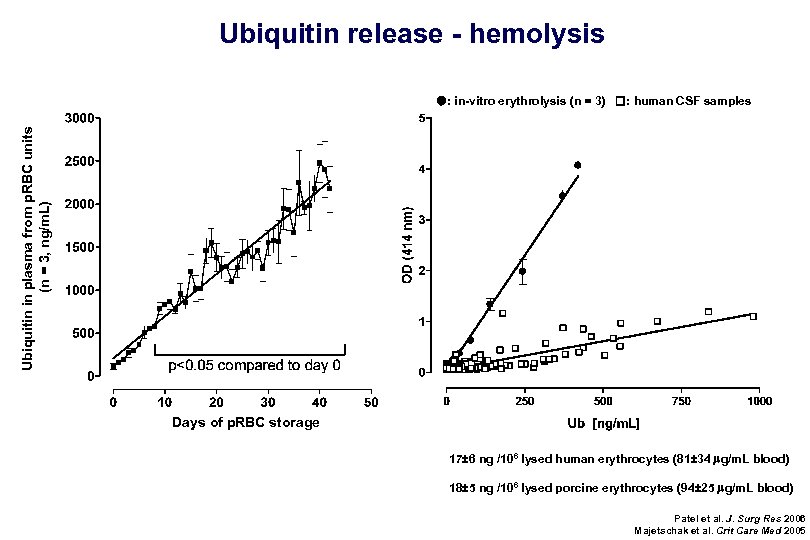 Ubiquitin release - hemolysis Ubiquitin in plasma from p. RBC units (n = 3, ng/m. L) : in-vitro erythrolysis (n = 3) : human CSF samples Days of p. RBC storage 17± 6 ng /106 lysed human erythrocytes (81± 34 mg/m. L blood) 18± 5 ng /106 lysed porcine erythrocytes (94± 25 mg/m. L blood) Patel et al. J. Surg Res 2006 Majetschak et al. Crit Care Med 2005
Ubiquitin release - hemolysis Ubiquitin in plasma from p. RBC units (n = 3, ng/m. L) : in-vitro erythrolysis (n = 3) : human CSF samples Days of p. RBC storage 17± 6 ng /106 lysed human erythrocytes (81± 34 mg/m. L blood) 18± 5 ng /106 lysed porcine erythrocytes (94± 25 mg/m. L blood) Patel et al. J. Surg Res 2006 Majetschak et al. Crit Care Med 2005
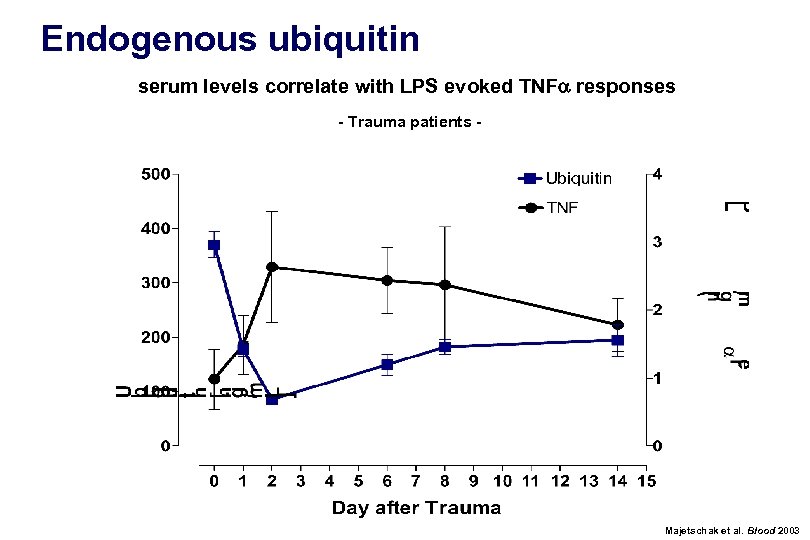 Endogenous ubiquitin serum levels correlate with LPS evoked TNFa responses - Trauma patients - Majetschak et al. Blood 2003
Endogenous ubiquitin serum levels correlate with LPS evoked TNFa responses - Trauma patients - Majetschak et al. Blood 2003
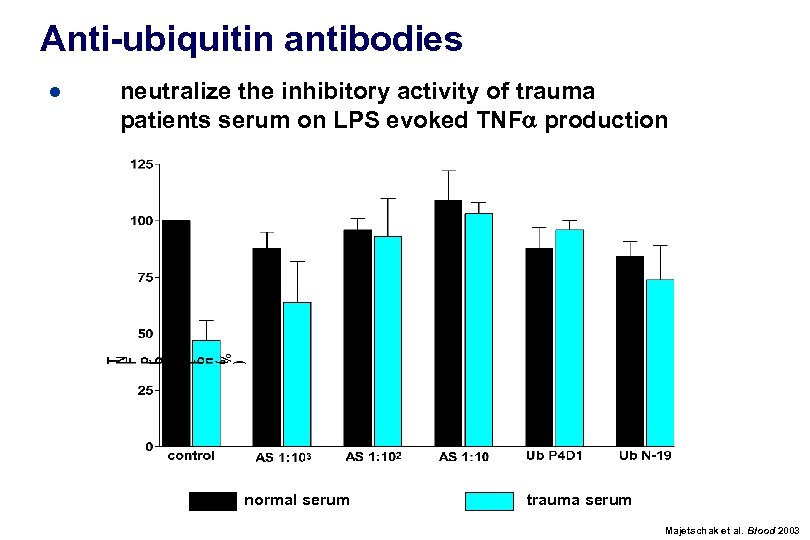 Anti-ubiquitin antibodies ● neutralize the inhibitory activity of trauma patients serum on LPS evoked TNFa production normal serum trauma serum Majetschak et al. Blood 2003
Anti-ubiquitin antibodies ● neutralize the inhibitory activity of trauma patients serum on LPS evoked TNFa production normal serum trauma serum Majetschak et al. Blood 2003
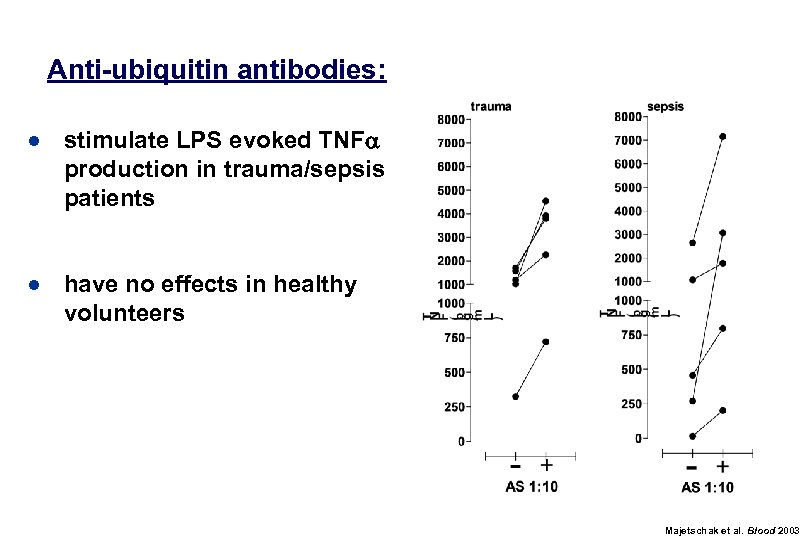 Anti-ubiquitin antibodies: ● stimulate LPS evoked TNFa production in trauma/sepsis patients ● have no effects in healthy volunteers Majetschak et al. Blood 2003
Anti-ubiquitin antibodies: ● stimulate LPS evoked TNFa production in trauma/sepsis patients ● have no effects in healthy volunteers Majetschak et al. Blood 2003
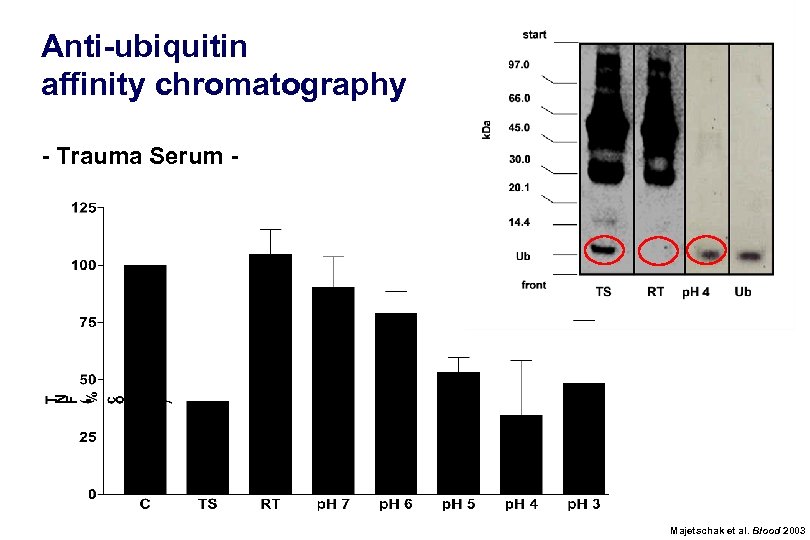 Anti-ubiquitin affinity chromatography - Trauma Serum - Majetschak et al. Blood 2003
Anti-ubiquitin affinity chromatography - Trauma Serum - Majetschak et al. Blood 2003
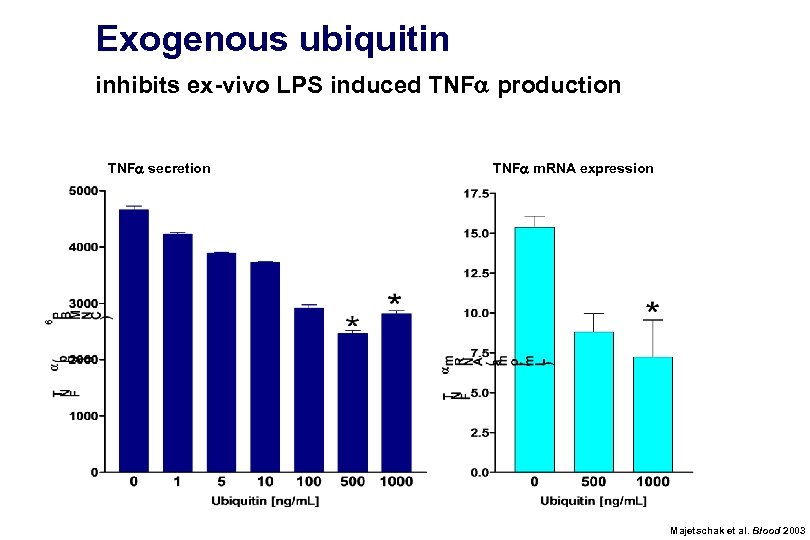 Exogenous ubiquitin inhibits ex-vivo LPS induced TNFa production TNFa secretion TNFa m. RNA expression Majetschak et al. Blood 2003
Exogenous ubiquitin inhibits ex-vivo LPS induced TNFa production TNFa secretion TNFa m. RNA expression Majetschak et al. Blood 2003
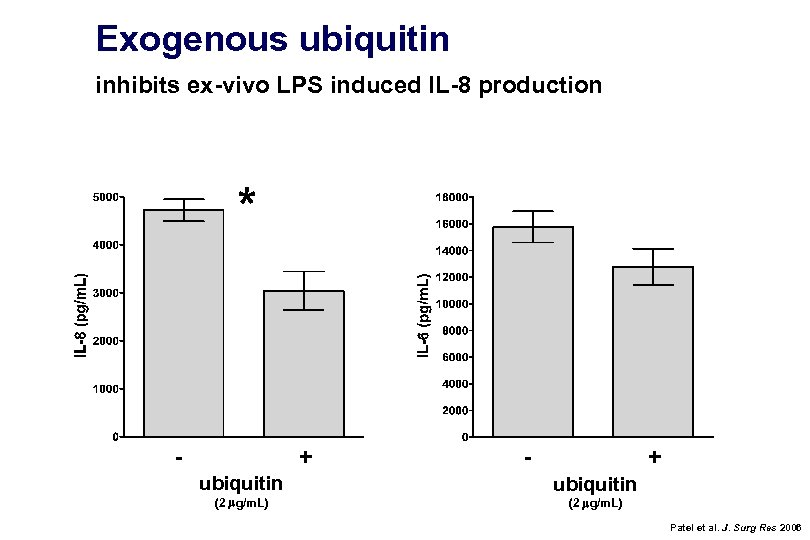 Exogenous ubiquitin inhibits ex-vivo LPS induced IL-8 production - + ubiquitin (2 mg/m. L) Patel et al. J. Surg Res 2006
Exogenous ubiquitin inhibits ex-vivo LPS induced IL-8 production - + ubiquitin (2 mg/m. L) Patel et al. J. Surg Res 2006
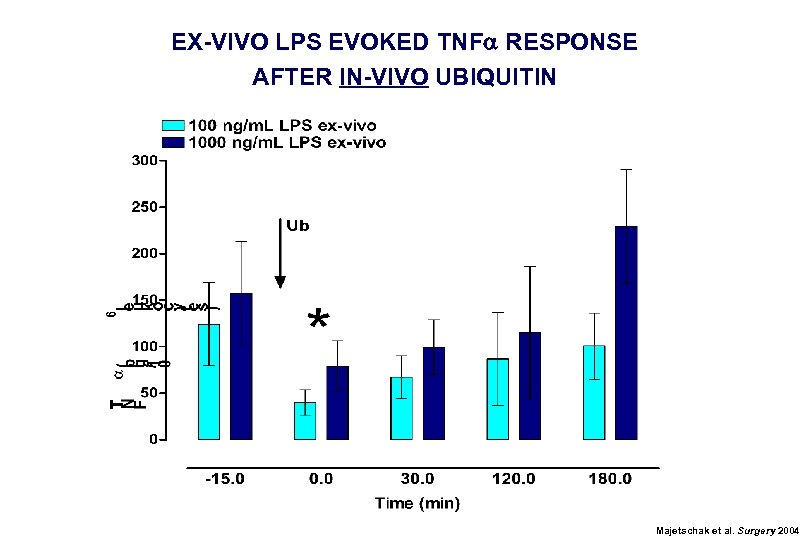 EX-VIVO LPS EVOKED TNFa RESPONSE AFTER IN-VIVO UBIQUITIN Majetschak et al. Surgery 2004
EX-VIVO LPS EVOKED TNFa RESPONSE AFTER IN-VIVO UBIQUITIN Majetschak et al. Surgery 2004
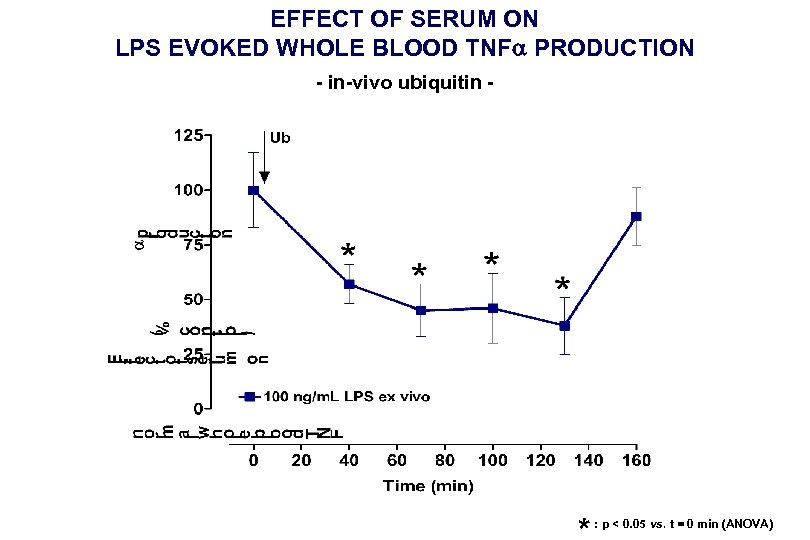 EFFECT OF SERUM ON LPS EVOKED WHOLE BLOOD TNFa PRODUCTION - in-vivo ubiquitin - : p < 0. 05 vs. t = 0 min (ANOVA)
EFFECT OF SERUM ON LPS EVOKED WHOLE BLOOD TNFa PRODUCTION - in-vivo ubiquitin - : p < 0. 05 vs. t = 0 min (ANOVA)
 Ubiquitin inhibits leukocyte function in-vitro and in-vivo clinical relevant effects ?
Ubiquitin inhibits leukocyte function in-vitro and in-vivo clinical relevant effects ?
 Exogenous ubiquitin in-vivo Swine, n = 4; 1. 3 mg/kg ubiquitin i. v. - no significant effects of ubiquitin on ● ● hemodynamics pulmonary function electrolytes, lactate or glucose levels leukocyte counts - no fluid requirement
Exogenous ubiquitin in-vivo Swine, n = 4; 1. 3 mg/kg ubiquitin i. v. - no significant effects of ubiquitin on ● ● hemodynamics pulmonary function electrolytes, lactate or glucose levels leukocyte counts - no fluid requirement
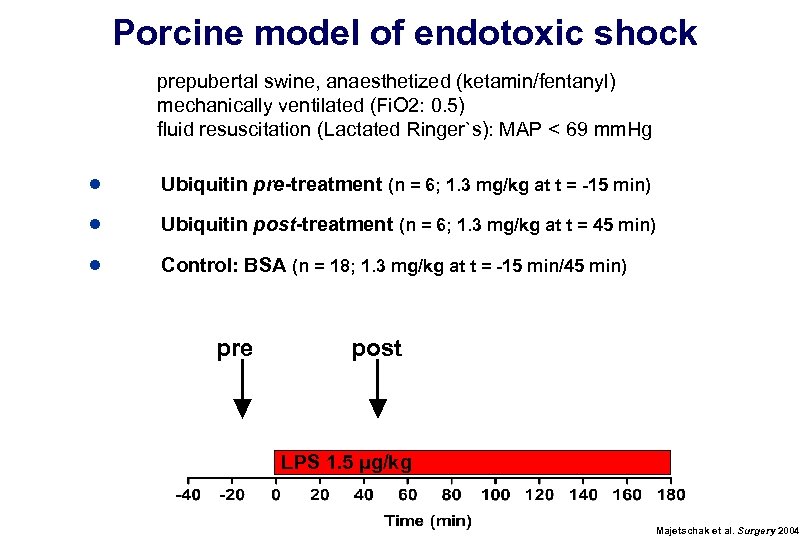 Porcine model of endotoxic shock prepubertal swine, anaesthetized (ketamin/fentanyl) mechanically ventilated (Fi. O 2: 0. 5) fluid resuscitation (Lactated Ringer`s): MAP < 69 mm. Hg ● Ubiquitin pre-treatment (n = 6; 1. 3 mg/kg at t = -15 min) ● Ubiquitin post-treatment (n = 6; 1. 3 mg/kg at t = 45 min) ● Control: BSA (n = 18; 1. 3 mg/kg at t = -15 min/45 min) pre post LPS 1. 5 µg/kg Majetschak et al. Surgery 2004
Porcine model of endotoxic shock prepubertal swine, anaesthetized (ketamin/fentanyl) mechanically ventilated (Fi. O 2: 0. 5) fluid resuscitation (Lactated Ringer`s): MAP < 69 mm. Hg ● Ubiquitin pre-treatment (n = 6; 1. 3 mg/kg at t = -15 min) ● Ubiquitin post-treatment (n = 6; 1. 3 mg/kg at t = 45 min) ● Control: BSA (n = 18; 1. 3 mg/kg at t = -15 min/45 min) pre post LPS 1. 5 µg/kg Majetschak et al. Surgery 2004
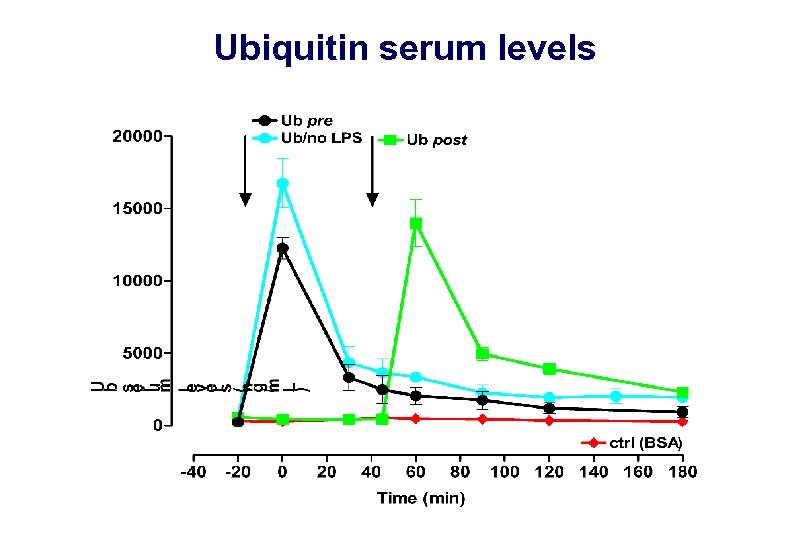 Ubiquitin serum levels
Ubiquitin serum levels
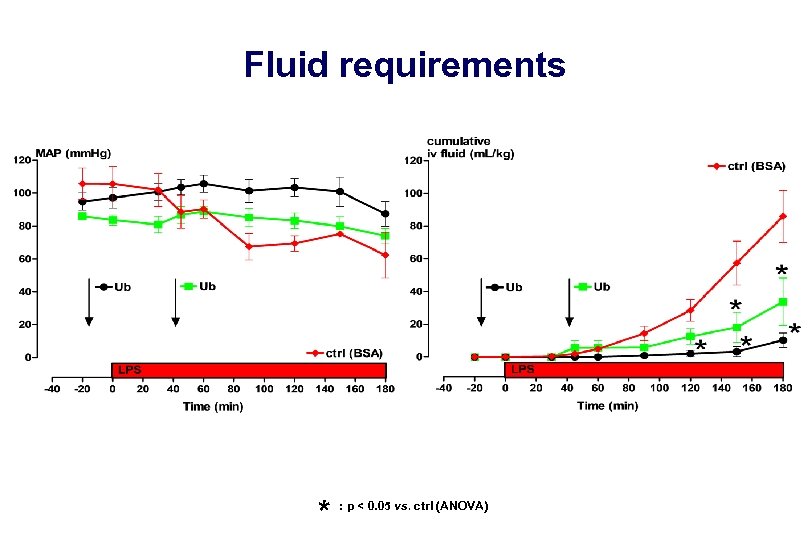 Fluid requirements * : p < 0. 05 vs. ctrl (ANOVA)
Fluid requirements * : p < 0. 05 vs. ctrl (ANOVA)
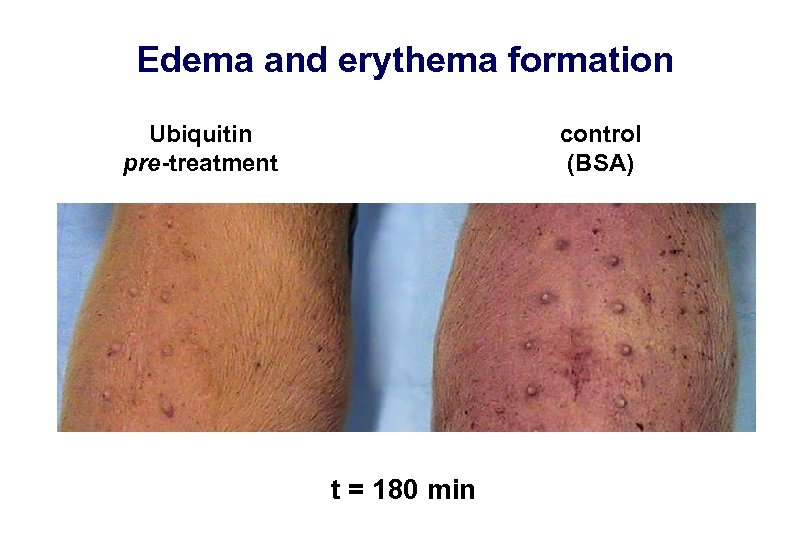 Edema and erythema formation Ubiquitin pre-treatment control (BSA) t = 180 min
Edema and erythema formation Ubiquitin pre-treatment control (BSA) t = 180 min
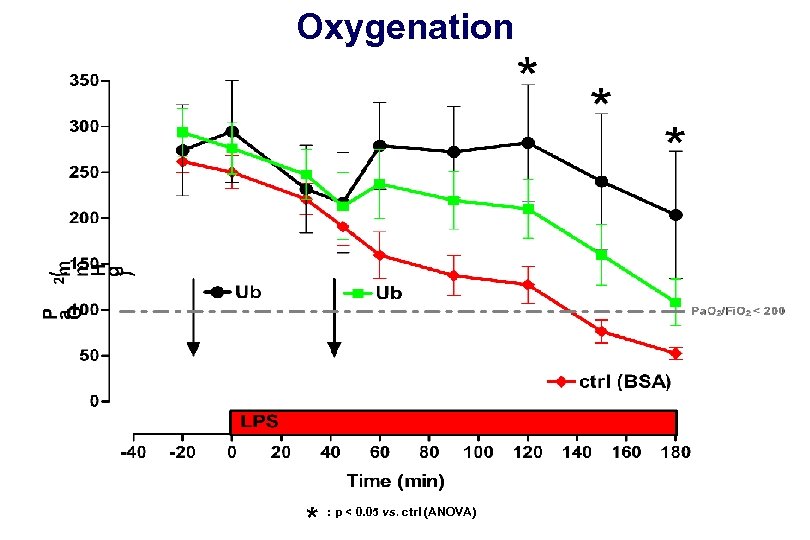 Oxygenation * : p < 0. 05 vs. ctrl (ANOVA)
Oxygenation * : p < 0. 05 vs. ctrl (ANOVA)
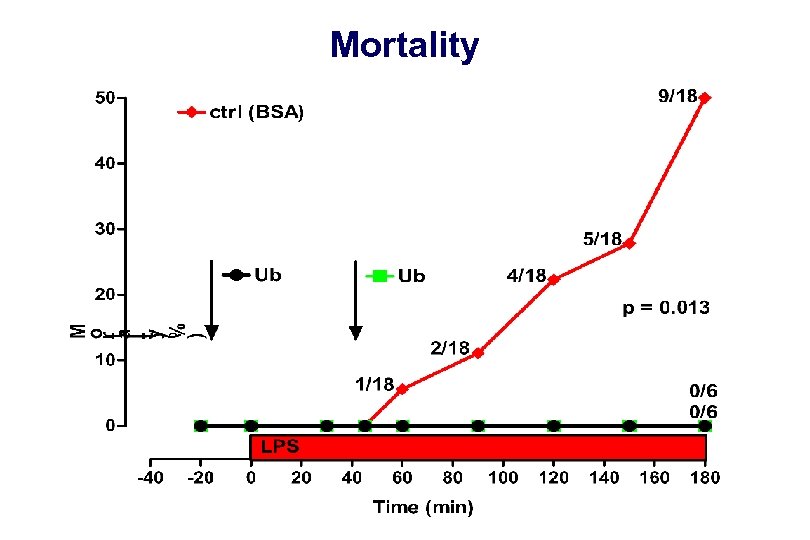 Mortality
Mortality
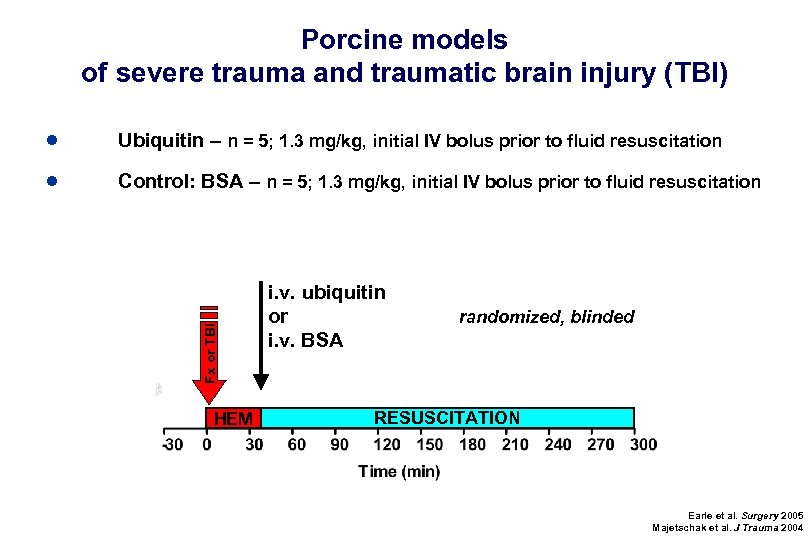 Porcine models of severe trauma and traumatic brain injury (TBI) Ubiquitin – n = 5; 1. 3 mg/kg, initial IV bolus prior to fluid resuscitation ● Control: BSA – n = 5; 1. 3 mg/kg, initial IV bolus prior to fluid resuscitation Fx or TBI ● HEM i. v. ubiquitin or i. v. BSA randomized, blinded RESUSCITATION Earle et al. Surgery 2005 Majetschak et al. J Trauma 2004
Porcine models of severe trauma and traumatic brain injury (TBI) Ubiquitin – n = 5; 1. 3 mg/kg, initial IV bolus prior to fluid resuscitation ● Control: BSA – n = 5; 1. 3 mg/kg, initial IV bolus prior to fluid resuscitation Fx or TBI ● HEM i. v. ubiquitin or i. v. BSA randomized, blinded RESUSCITATION Earle et al. Surgery 2005 Majetschak et al. J Trauma 2004
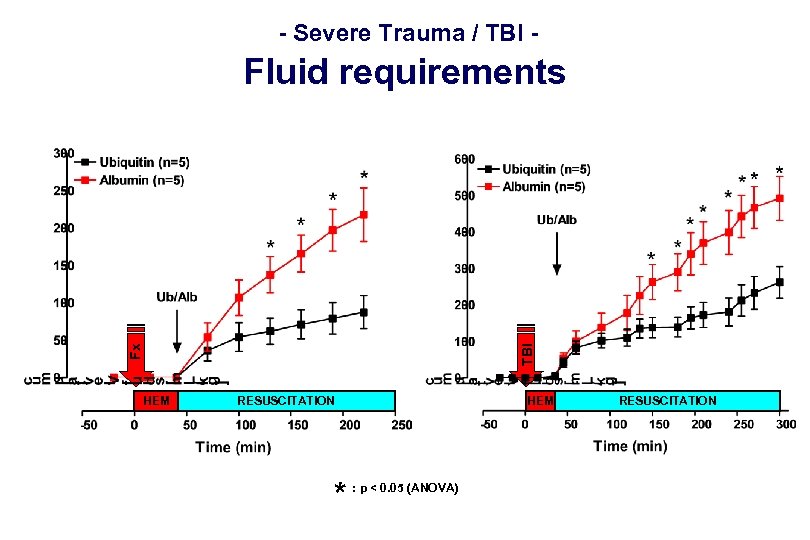 - Severe Trauma / TBI - Fx TBI Fluid requirements HEM RESUSCITATION * HEM : p < 0. 05 (ANOVA) RESUSCITATION
- Severe Trauma / TBI - Fx TBI Fluid requirements HEM RESUSCITATION * HEM : p < 0. 05 (ANOVA) RESUSCITATION
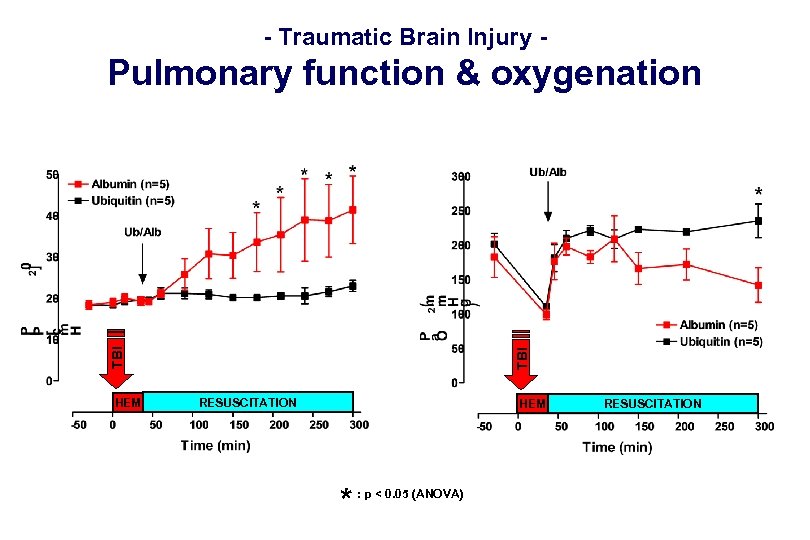 - Traumatic Brain Injury - HEM TBI Pulmonary function & oxygenation RESUSCITATION HEM * : p < 0. 05 (ANOVA) RESUSCITATION
- Traumatic Brain Injury - HEM TBI Pulmonary function & oxygenation RESUSCITATION HEM * : p < 0. 05 (ANOVA) RESUSCITATION
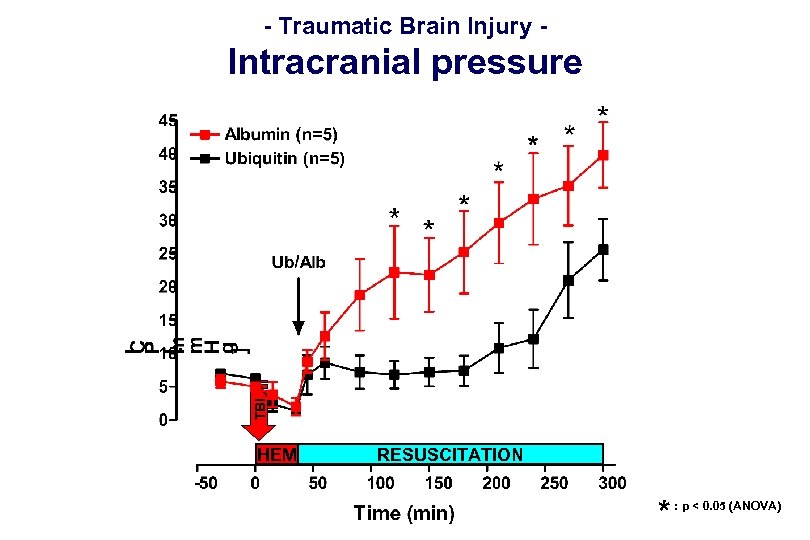 - Traumatic Brain Injury - TBI Intracranial pressure HEM RESUSCITATION * : p < 0. 05 (ANOVA)
- Traumatic Brain Injury - TBI Intracranial pressure HEM RESUSCITATION * : p < 0. 05 (ANOVA)
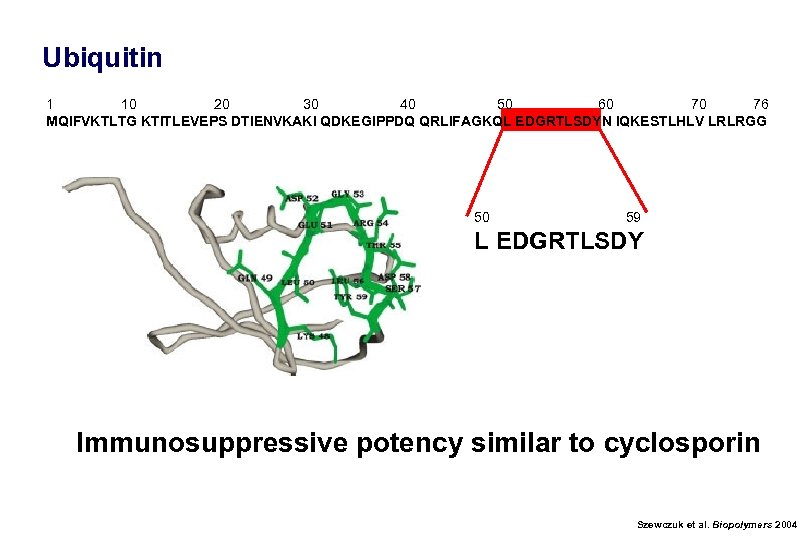 Ubiquitin 1 10 20 30 40 50 60 70 76 MQIFVKTLTG KTITLEVEPS DTIENVKAKI QDKEGIPPDQ QRLIFAGKQL EDGRTLSDYN IQKESTLHLV LRLRGG 50 59 L EDGRTLSDY Immunosuppressive potency similar to cyclosporin Szewczuk et al. Biopolymers 2004
Ubiquitin 1 10 20 30 40 50 60 70 76 MQIFVKTLTG KTITLEVEPS DTIENVKAKI QDKEGIPPDQ QRLIFAGKQL EDGRTLSDYN IQKESTLHLV LRLRGG 50 59 L EDGRTLSDY Immunosuppressive potency similar to cyclosporin Szewczuk et al. Biopolymers 2004
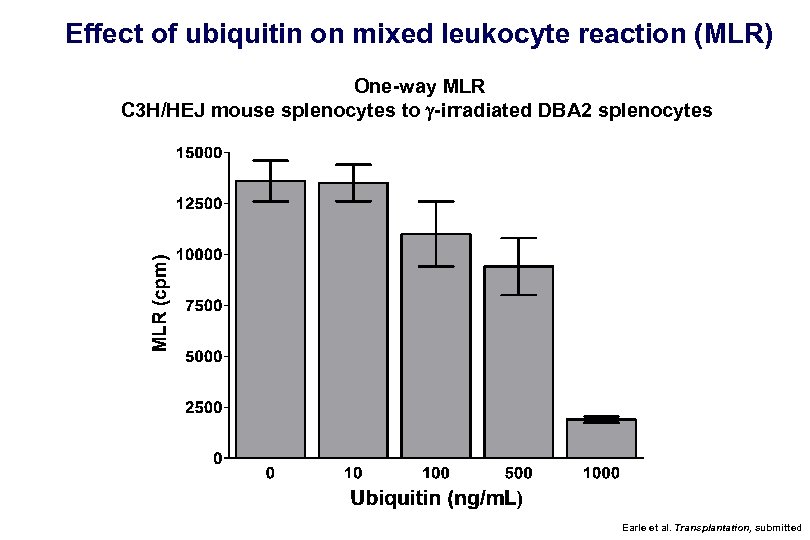 Effect of ubiquitin on mixed leukocyte reaction (MLR) One-way MLR C 3 H/HEJ mouse splenocytes to g-irradiated DBA 2 splenocytes Earle et al. Transplantation, submitted
Effect of ubiquitin on mixed leukocyte reaction (MLR) One-way MLR C 3 H/HEJ mouse splenocytes to g-irradiated DBA 2 splenocytes Earle et al. Transplantation, submitted
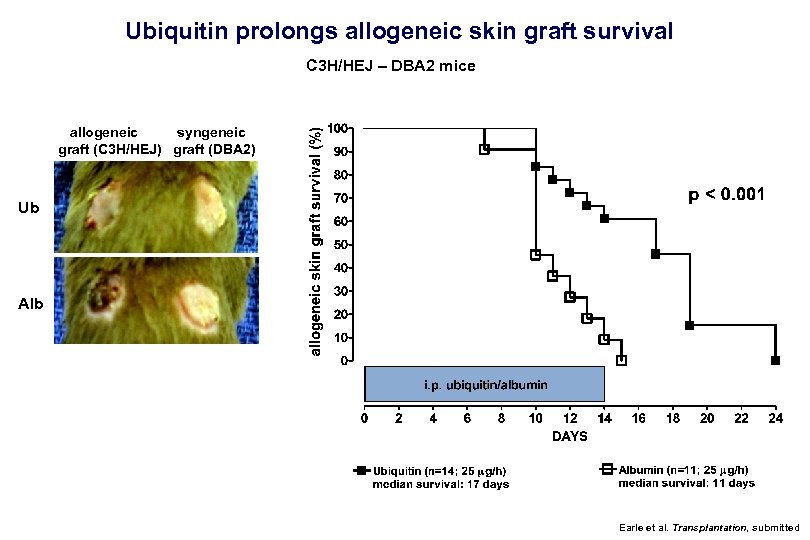 Ubiquitin prolongs allogeneic skin graft survival C 3 H/HEJ – DBA 2 mice allogeneic syngeneic graft (C 3 H/HEJ) graft (DBA 2) Ub Alb Earle et al. Transplantation, submitted
Ubiquitin prolongs allogeneic skin graft survival C 3 H/HEJ – DBA 2 mice allogeneic syngeneic graft (C 3 H/HEJ) graft (DBA 2) Ub Alb Earle et al. Transplantation, submitted
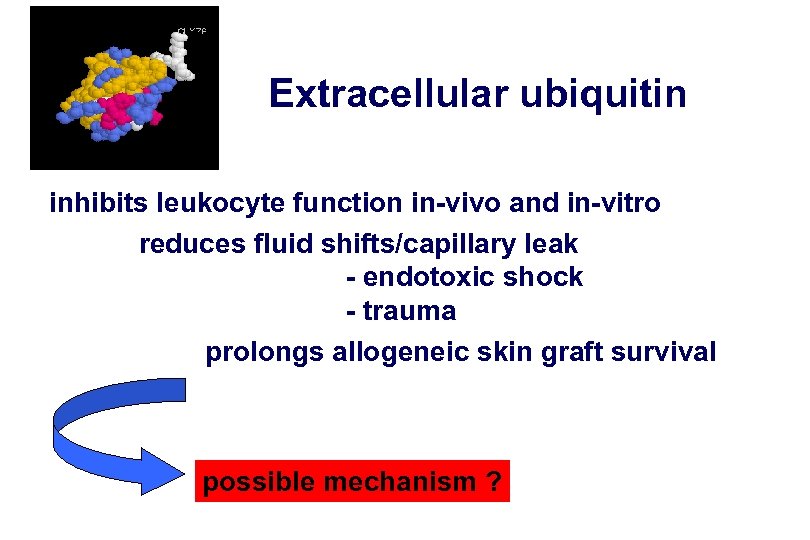 Extracellular ubiquitin inhibits leukocyte function in-vivo and in-vitro reduces fluid shifts/capillary leak - endotoxic shock - trauma prolongs allogeneic skin graft survival possible mechanism ?
Extracellular ubiquitin inhibits leukocyte function in-vivo and in-vitro reduces fluid shifts/capillary leak - endotoxic shock - trauma prolongs allogeneic skin graft survival possible mechanism ?
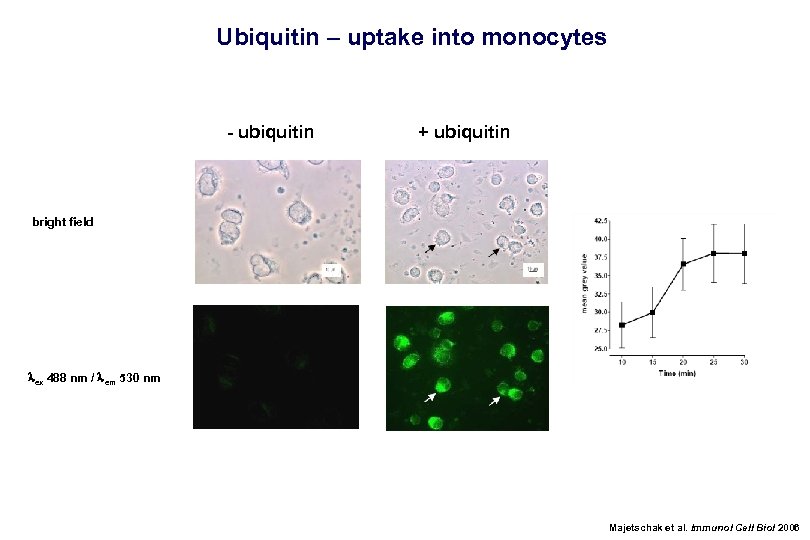 Ubiquitin – uptake into monocytes - ubiquitin + ubiquitin bright field lex 488 nm / lem 530 nm Majetschak et al. Immunol Cell Biol 2006
Ubiquitin – uptake into monocytes - ubiquitin + ubiquitin bright field lex 488 nm / lem 530 nm Majetschak et al. Immunol Cell Biol 2006
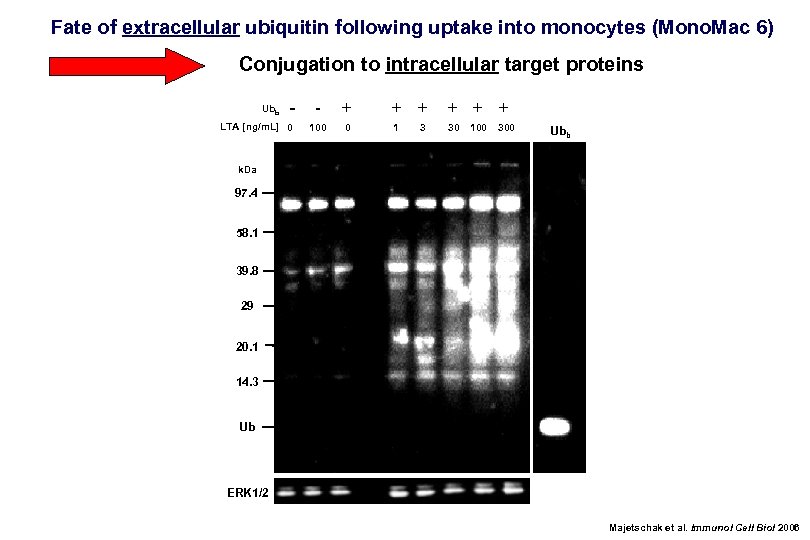 Fate of extracellular ubiquitin following uptake into monocytes (Mono. Mac 6) Conjugation to intracellular target proteins Ubb - LTA [ng/m. L] 0 - + 100 0 + + + 1 30 3 100 300 Ubb k. Da 97. 4 58. 1 39. 8 29 20. 1 14. 3 Ub ERK 1/2 Majetschak et al. Immunol Cell Biol 2006
Fate of extracellular ubiquitin following uptake into monocytes (Mono. Mac 6) Conjugation to intracellular target proteins Ubb - LTA [ng/m. L] 0 - + 100 0 + + + 1 30 3 100 300 Ubb k. Da 97. 4 58. 1 39. 8 29 20. 1 14. 3 Ub ERK 1/2 Majetschak et al. Immunol Cell Biol 2006
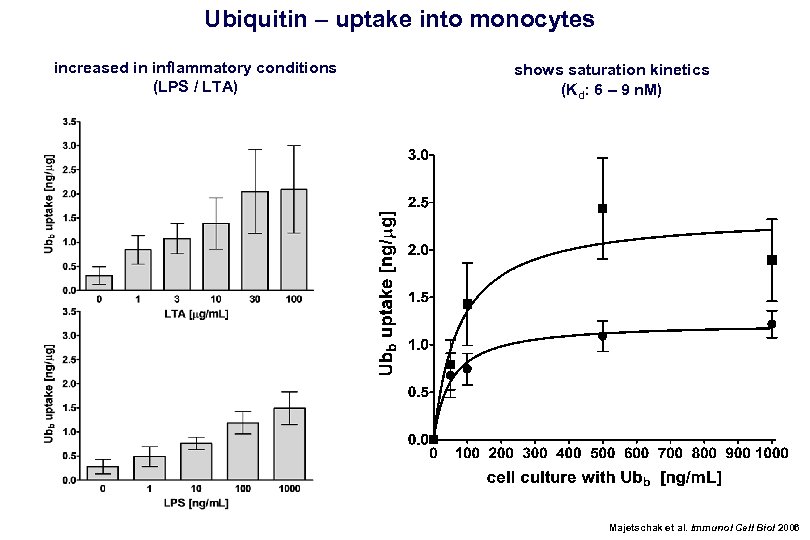 Ubiquitin – uptake into monocytes increased in inflammatory conditions (LPS / LTA) shows saturation kinetics (Kd: 6 – 9 n. M) Majetschak et al. Immunol Cell Biol 2006
Ubiquitin – uptake into monocytes increased in inflammatory conditions (LPS / LTA) shows saturation kinetics (Kd: 6 – 9 n. M) Majetschak et al. Immunol Cell Biol 2006
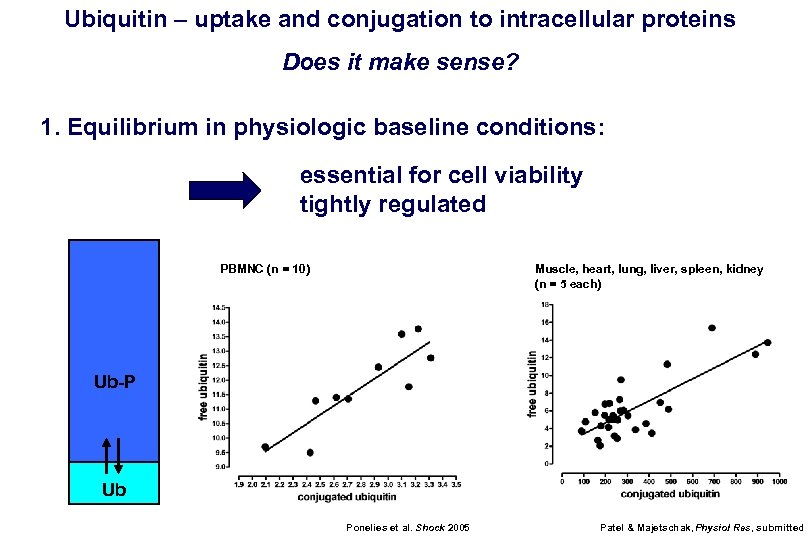 Ubiquitin – uptake and conjugation to intracellular proteins Does it make sense? 1. Equilibrium in physiologic baseline conditions: essential for cell viability tightly regulated PBMNC (n = 10) Muscle, heart, lung, liver, spleen, kidney (n = 5 each) Ub-P Ub Ponelies et al. Shock 2005 Patel & Majetschak, Physiol Res, submitted
Ubiquitin – uptake and conjugation to intracellular proteins Does it make sense? 1. Equilibrium in physiologic baseline conditions: essential for cell viability tightly regulated PBMNC (n = 10) Muscle, heart, lung, liver, spleen, kidney (n = 5 each) Ub-P Ub Ponelies et al. Shock 2005 Patel & Majetschak, Physiol Res, submitted
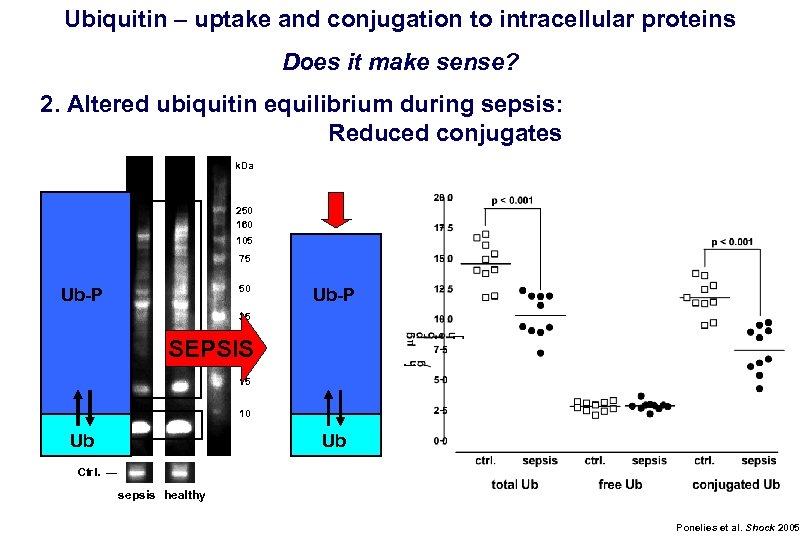 Ubiquitin – uptake and conjugation to intracellular proteins Does it make sense? 2. Altered ubiquitin equilibrium during sepsis: Reduced conjugates k. Da Ub-protein conjugates 250 160 105 75 50 Ub-P 35 30 SEPSIS 25 15 10 free Ub — Ub Ub Ctrl. — sepsis healthy Ponelies et al. Shock 2005
Ubiquitin – uptake and conjugation to intracellular proteins Does it make sense? 2. Altered ubiquitin equilibrium during sepsis: Reduced conjugates k. Da Ub-protein conjugates 250 160 105 75 50 Ub-P 35 30 SEPSIS 25 15 10 free Ub — Ub Ub Ctrl. — sepsis healthy Ponelies et al. Shock 2005
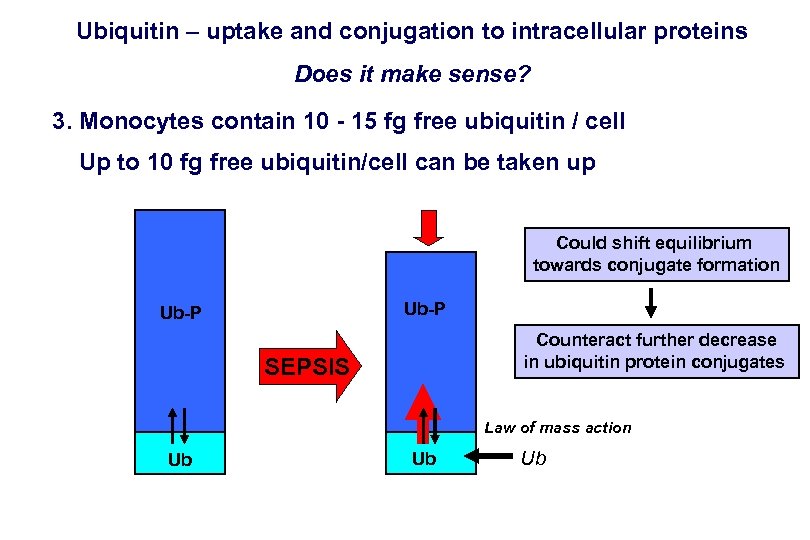 Ubiquitin – uptake and conjugation to intracellular proteins Does it make sense? 3. Monocytes contain 10 - 15 fg free ubiquitin / cell Up to 10 fg free ubiquitin/cell can be taken up Could shift equilibrium towards conjugate formation Ub-P Counteract further decrease in ubiquitin protein conjugates SEPSIS Law of mass action Ub Ub Ub
Ubiquitin – uptake and conjugation to intracellular proteins Does it make sense? 3. Monocytes contain 10 - 15 fg free ubiquitin / cell Up to 10 fg free ubiquitin/cell can be taken up Could shift equilibrium towards conjugate formation Ub-P Counteract further decrease in ubiquitin protein conjugates SEPSIS Law of mass action Ub Ub Ub
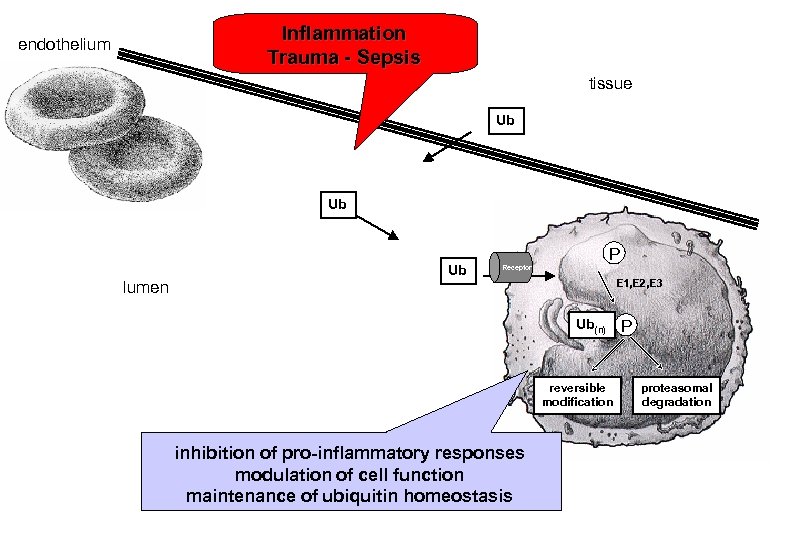 Inflammation Trauma - Sepsis endothelium tissue Ub Ub lumen Ub P Receptor E 1, E 2, E 3 Ub(n) reversible modification inhibition of pro-inflammatory responses modulation of cell function maintenance of ubiquitin homeostasis P proteasomal degradation
Inflammation Trauma - Sepsis endothelium tissue Ub Ub lumen Ub P Receptor E 1, E 2, E 3 Ub(n) reversible modification inhibition of pro-inflammatory responses modulation of cell function maintenance of ubiquitin homeostasis P proteasomal degradation
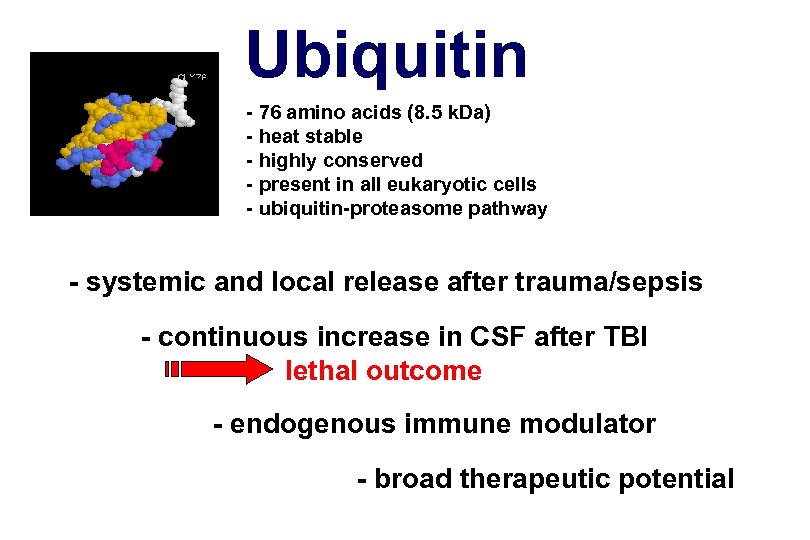 Ubiquitin - 76 amino acids (8. 5 k. Da) - heat stable - highly conserved - present in all eukaryotic cells - ubiquitin-proteasome pathway - systemic and local release after trauma/sepsis - continuous increase in CSF after TBI lethal outcome - endogenous immune modulator - broad therapeutic potential
Ubiquitin - 76 amino acids (8. 5 k. Da) - heat stable - highly conserved - present in all eukaryotic cells - ubiquitin-proteasome pathway - systemic and local release after trauma/sepsis - continuous increase in CSF after TBI lethal outcome - endogenous immune modulator - broad therapeutic potential
 Acknowledgement University of Miami University of Heidelberg Lissette T. Busby Mayur B. Patel Steven A. Earle David R. King Kenneth G. Proctor Steven M. Cohn Norbert Ponelies Thomas Hirsch Ulrich Krehmeier Udo Obertacke University of Berlin Arwed Hosstmann Andreas Oberholzer Wolfgang Ertel University of Munich Siegfried Zedler Eugen Faist Supported by: DFG (German Science Foundation) MA 2474/1 -1, MA 2474/2 -1, MA 2472/2 -2
Acknowledgement University of Miami University of Heidelberg Lissette T. Busby Mayur B. Patel Steven A. Earle David R. King Kenneth G. Proctor Steven M. Cohn Norbert Ponelies Thomas Hirsch Ulrich Krehmeier Udo Obertacke University of Berlin Arwed Hosstmann Andreas Oberholzer Wolfgang Ertel University of Munich Siegfried Zedler Eugen Faist Supported by: DFG (German Science Foundation) MA 2474/1 -1, MA 2474/2 -1, MA 2472/2 -2
 “Finally, I believe ubiquitin is a ‘lucky’ molecule. Almost everyone who has studied it has made fascinating observations. ” Martin Rechsteiner, 1988
“Finally, I believe ubiquitin is a ‘lucky’ molecule. Almost everyone who has studied it has made fascinating observations. ” Martin Rechsteiner, 1988


