b271610447bee27429ccca982aca8f2b.ppt
- Количество слайдов: 49
 Immune deviation in atopic eczema is crucial Johannes Ring, Kilian Eyerich, Stephan Weidinger, Ulf Darsow Klinik und Poliklinik für Dermatologie und Allergologie am Biederstein Technische Universität München, Munich, Bavaria, Germany GA 2 LEN Center of Excellence EU frame program Christine Kühne Center for Allergy Research and Education (CKCARE) XXII World Allergy Congress (WAC)
Immune deviation in atopic eczema is crucial Johannes Ring, Kilian Eyerich, Stephan Weidinger, Ulf Darsow Klinik und Poliklinik für Dermatologie und Allergologie am Biederstein Technische Universität München, Munich, Bavaria, Germany GA 2 LEN Center of Excellence EU frame program Christine Kühne Center for Allergy Research and Education (CKCARE) XXII World Allergy Congress (WAC)
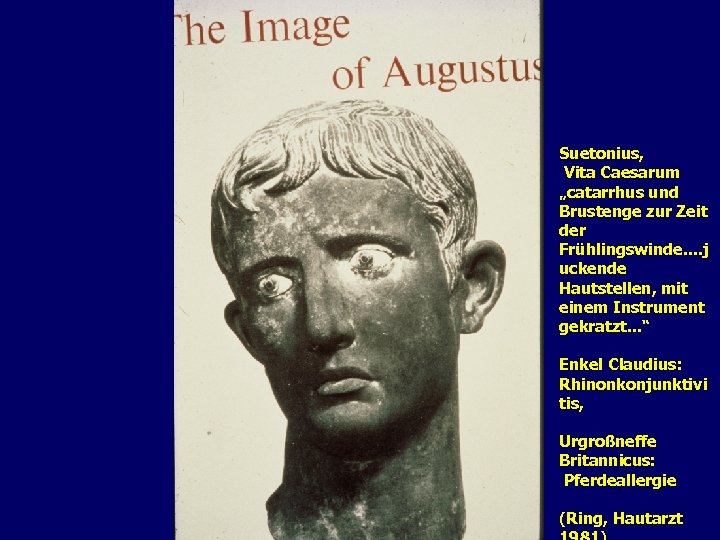 Suetonius, Vita Caesarum „catarrhus und Brustenge zur Zeit der Frühlingswinde. . j uckende Hautstellen, mit einem Instrument gekratzt. . . “ Enkel Claudius: Rhinonkonjunktivi tis, Urgroßneffe Britannicus: Pferdeallergie (Ring, Hautarzt
Suetonius, Vita Caesarum „catarrhus und Brustenge zur Zeit der Frühlingswinde. . j uckende Hautstellen, mit einem Instrument gekratzt. . . “ Enkel Claudius: Rhinonkonjunktivi tis, Urgroßneffe Britannicus: Pferdeallergie (Ring, Hautarzt
 Atopic Eczema: History • • • Imperator Octavian (Augustus) Aetius from Amida: „ekzem “ (ek zeo = aufkochen, 600 AD) Mercuriali: „Lactumen“ (like burnt mild in a pot) (1571) Willan: „Eczema“ (1808) Brocq, Jacquet: „Neurodermite“ (1892) Besnier: „Prurigo diathésique“ (1901) Coca, Cooke: „Atopy“ (1923) Wise, Sulzberger: „Atopic dermatitis/atopic eczema“ (1933) Schnyder, Borelli: „Neurodermitis constitutionalis sive atopica“ (1968) • Atopic eczema/dermatitis syndrome AEDS (EAACI 2001) • Eczema (WAO nomenclature 2004)
Atopic Eczema: History • • • Imperator Octavian (Augustus) Aetius from Amida: „ekzem “ (ek zeo = aufkochen, 600 AD) Mercuriali: „Lactumen“ (like burnt mild in a pot) (1571) Willan: „Eczema“ (1808) Brocq, Jacquet: „Neurodermite“ (1892) Besnier: „Prurigo diathésique“ (1901) Coca, Cooke: „Atopy“ (1923) Wise, Sulzberger: „Atopic dermatitis/atopic eczema“ (1933) Schnyder, Borelli: „Neurodermitis constitutionalis sive atopica“ (1968) • Atopic eczema/dermatitis syndrome AEDS (EAACI 2001) • Eczema (WAO nomenclature 2004)
 “Atopy” = Familial tendency to develop certain diseases (asthma, rhinoconjunctivitis, atopic eczema) based on hypersensitivity of skin and mucous membranes against environmental substances together with increased Ig. E production and/or altered non-specific reactivity Ring J, Handbook of Atopic Eczema 1991
“Atopy” = Familial tendency to develop certain diseases (asthma, rhinoconjunctivitis, atopic eczema) based on hypersensitivity of skin and mucous membranes against environmental substances together with increased Ig. E production and/or altered non-specific reactivity Ring J, Handbook of Atopic Eczema 1991
 WAO Task Force on Allergy Nomenclature: “Atopy” : = Familial tendency to produce Ig. E immune response to low doses of allergens and to develop typical symptoms such as asthma, rhinoconjunctivitis or eczema (Johansson et al JACI 2004)
WAO Task Force on Allergy Nomenclature: “Atopy” : = Familial tendency to produce Ig. E immune response to low doses of allergens and to develop typical symptoms such as asthma, rhinoconjunctivitis or eczema (Johansson et al JACI 2004)
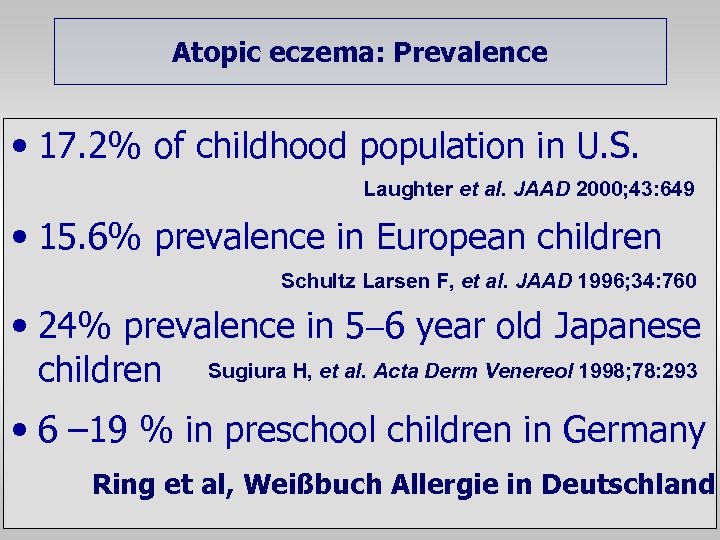 Atopic eczema: Prevalence • 17. 2% of childhood population in U. S. Laughter et al. JAAD 2000; 43: 649 • 15. 6% prevalence in European children Schultz Larsen F, et al. JAAD 1996; 34: 760 • 24% prevalence in 5 6 year old Japanese children Sugiura H, et al. Acta Derm Venereol 1998; 78: 293 • 6 – 19 % in preschool children in Germany Ring et al, Weißbuch Allergie in Deutschland
Atopic eczema: Prevalence • 17. 2% of childhood population in U. S. Laughter et al. JAAD 2000; 43: 649 • 15. 6% prevalence in European children Schultz Larsen F, et al. JAAD 1996; 34: 760 • 24% prevalence in 5 6 year old Japanese children Sugiura H, et al. Acta Derm Venereol 1998; 78: 293 • 6 – 19 % in preschool children in Germany Ring et al, Weißbuch Allergie in Deutschland
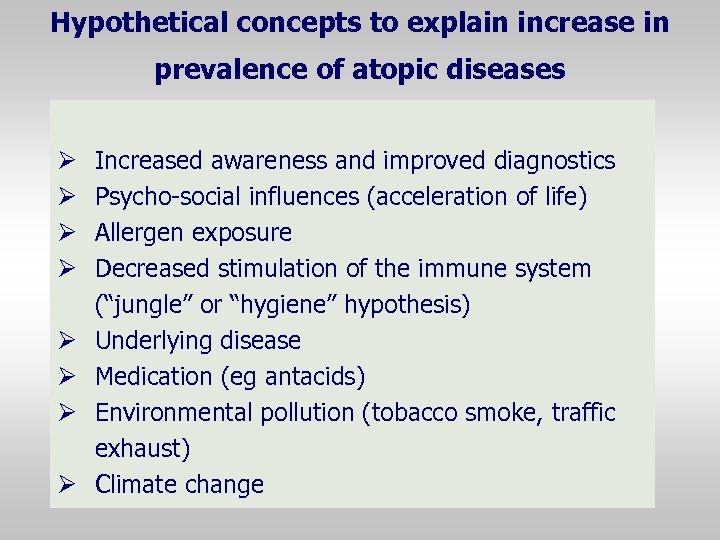 Hypothetical concepts to explain increase in prevalence of atopic diseases Ø Ø Ø Ø Increased awareness and improved diagnostics Psycho-social influences (acceleration of life) Allergen exposure Decreased stimulation of the immune system (“jungle” or “hygiene” hypothesis) Underlying disease Medication (eg antacids) Environmental pollution (tobacco smoke, traffic exhaust) Climate change
Hypothetical concepts to explain increase in prevalence of atopic diseases Ø Ø Ø Ø Increased awareness and improved diagnostics Psycho-social influences (acceleration of life) Allergen exposure Decreased stimulation of the immune system (“jungle” or “hygiene” hypothesis) Underlying disease Medication (eg antacids) Environmental pollution (tobacco smoke, traffic exhaust) Climate change
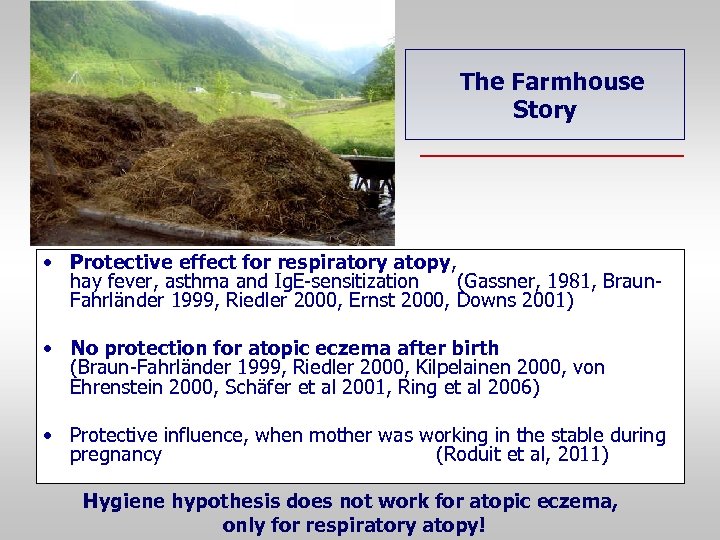 The Farmhouse Story • Protective effect for respiratory atopy, hay fever, asthma and Ig. E-sensitization (Gassner, 1981, Braun. Fahrländer 1999, Riedler 2000, Ernst 2000, Downs 2001) • No protection for atopic eczema after birth (Braun-Fahrländer 1999, Riedler 2000, Kilpelainen 2000, von Ehrenstein 2000, Schäfer et al 2001, Ring et al 2006) • Protective influence, when mother was working in the stable during pregnancy (Roduit et al, 2011) Hygiene hypothesis does not work for atopic eczema, only for respiratory atopy!
The Farmhouse Story • Protective effect for respiratory atopy, hay fever, asthma and Ig. E-sensitization (Gassner, 1981, Braun. Fahrländer 1999, Riedler 2000, Ernst 2000, Downs 2001) • No protection for atopic eczema after birth (Braun-Fahrländer 1999, Riedler 2000, Kilpelainen 2000, von Ehrenstein 2000, Schäfer et al 2001, Ring et al 2006) • Protective influence, when mother was working in the stable during pregnancy (Roduit et al, 2011) Hygiene hypothesis does not work for atopic eczema, only for respiratory atopy!
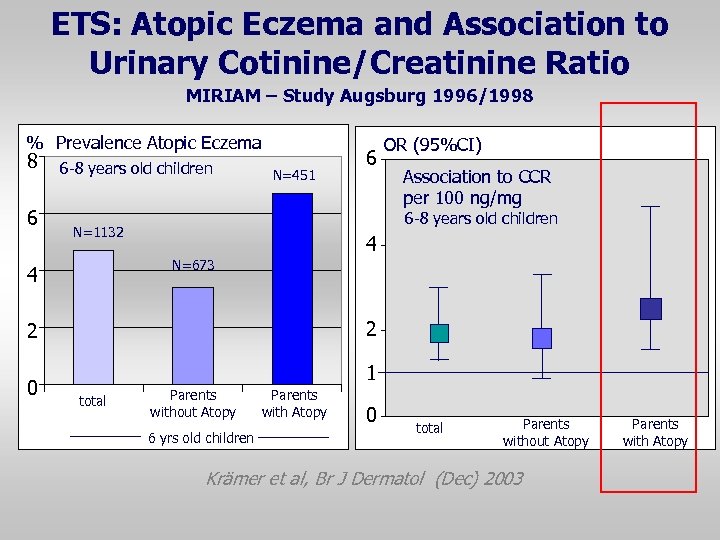 ETS: Atopic Eczema and Association to Urinary Cotinine/Creatinine Ratio MIRIAM – Study Augsburg 1996/1998 % Prevalence Atopic Eczema 8 6 6 -8 years old children N=451 Association to CCR per 100 ng/mg 6 -8 years old children N=1132 4 N=673 4 2 2 0 6 OR (95%CI) 1 total Parents without Atopy 6 yrs old children Parents with Atopy 0 total Parents without Atopy Krämer et al, Br J Dermatol (Dec) 2003 Parents with Atopy
ETS: Atopic Eczema and Association to Urinary Cotinine/Creatinine Ratio MIRIAM – Study Augsburg 1996/1998 % Prevalence Atopic Eczema 8 6 6 -8 years old children N=451 Association to CCR per 100 ng/mg 6 -8 years old children N=1132 4 N=673 4 2 2 0 6 OR (95%CI) 1 total Parents without Atopy 6 yrs old children Parents with Atopy 0 total Parents without Atopy Krämer et al, Br J Dermatol (Dec) 2003 Parents with Atopy
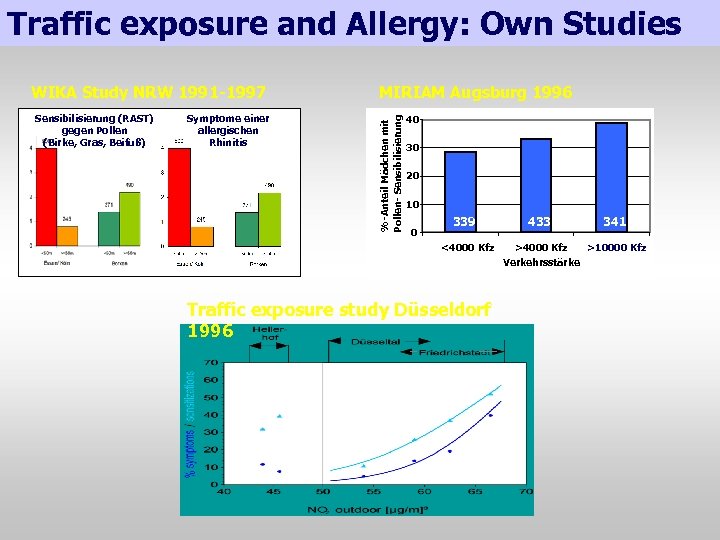 Traffic exposure and Allergy: Own Studies Sensibilisierung (RAST) gegen Pollen (Birke, Gras, Beifuß) Symptome einer allergischen Rhinitis MIRIAM Augsburg 1996 %-Anteil Mädchen mit Pollen- Sensibilisierung WIKA Study NRW 1991 -1997 40 30 20 10 0 339 <4000 Kfz 433 341 >4000 Kfz >10000 Kfz Verkehrsstärke Traffic exposure study Düsseldorf 1996
Traffic exposure and Allergy: Own Studies Sensibilisierung (RAST) gegen Pollen (Birke, Gras, Beifuß) Symptome einer allergischen Rhinitis MIRIAM Augsburg 1996 %-Anteil Mädchen mit Pollen- Sensibilisierung WIKA Study NRW 1991 -1997 40 30 20 10 0 339 <4000 Kfz 433 341 >4000 Kfz >10000 Kfz Verkehrsstärke Traffic exposure study Düsseldorf 1996
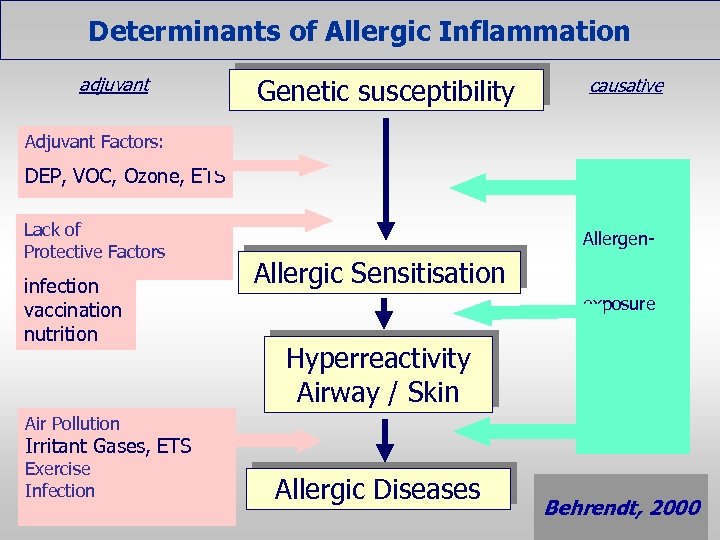 Determinants of Allergic Inflammation adjuvant Genetic susceptibility causative Adjuvant Factors: DEP, VOC, Ozone, ETS Lack of Protective Factors infection vaccination nutrition Allergen- Allergic Sensitisation exposure Hyperreactivity Airway / Skin Air Pollution Irritant Gases, ETS Exercise Infection Allergic Diseases Behrendt, 2000
Determinants of Allergic Inflammation adjuvant Genetic susceptibility causative Adjuvant Factors: DEP, VOC, Ozone, ETS Lack of Protective Factors infection vaccination nutrition Allergen- Allergic Sensitisation exposure Hyperreactivity Airway / Skin Air Pollution Irritant Gases, ETS Exercise Infection Allergic Diseases Behrendt, 2000
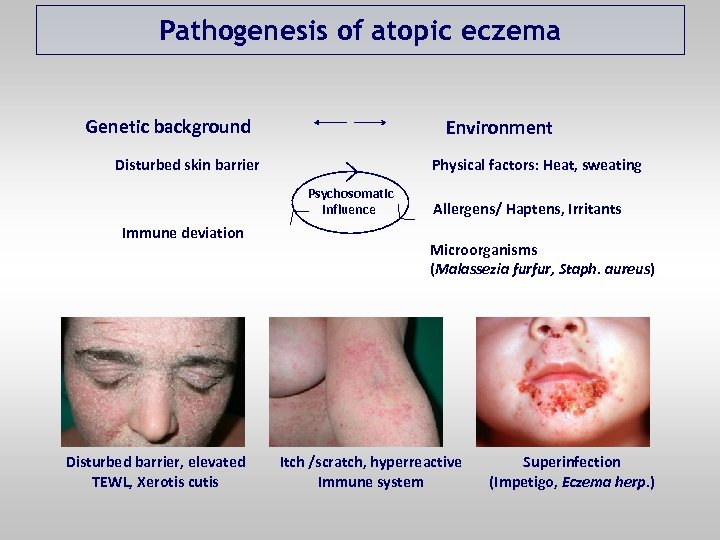 Pathogenesis of atopic eczema Genetic background Environment Disturbed skin barrier Physical factors: Heat, sweating Psychosomatic influence Immune deviation Disturbed barrier, elevated TEWL, Xerotis cutis Allergens/ Haptens, Irritants Microorganisms (Malassezia furfur, Staph. aureus) Itch /scratch, hyperreactive Immune system Superinfection (Impetigo, Eczema herp. )
Pathogenesis of atopic eczema Genetic background Environment Disturbed skin barrier Physical factors: Heat, sweating Psychosomatic influence Immune deviation Disturbed barrier, elevated TEWL, Xerotis cutis Allergens/ Haptens, Irritants Microorganisms (Malassezia furfur, Staph. aureus) Itch /scratch, hyperreactive Immune system Superinfection (Impetigo, Eczema herp. )
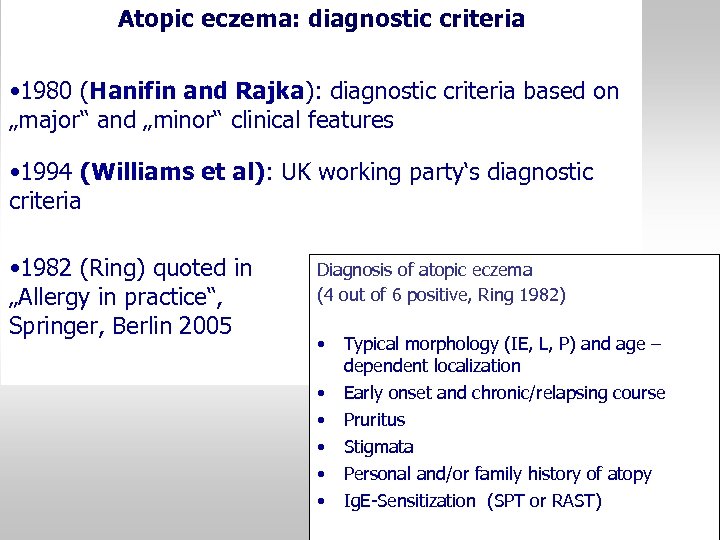 Atopic eczema: diagnostic criteria • 1980 (Hanifin and Rajka): diagnostic criteria based on „major“ and „minor“ clinical features • 1994 (Williams et al): UK working party‘s diagnostic criteria • 1982 (Ring) quoted in „Allergy in practice“, Springer, Berlin 2005 Diagnosis of atopic eczema (4 out of 6 positive, Ring 1982) • • • Typical morphology (IE, L, P) and age – dependent localization Early onset and chronic/relapsing course Pruritus Stigmata Personal and/or family history of atopy Ig. E-Sensitization (SPT or RAST)
Atopic eczema: diagnostic criteria • 1980 (Hanifin and Rajka): diagnostic criteria based on „major“ and „minor“ clinical features • 1994 (Williams et al): UK working party‘s diagnostic criteria • 1982 (Ring) quoted in „Allergy in practice“, Springer, Berlin 2005 Diagnosis of atopic eczema (4 out of 6 positive, Ring 1982) • • • Typical morphology (IE, L, P) and age – dependent localization Early onset and chronic/relapsing course Pruritus Stigmata Personal and/or family history of atopy Ig. E-Sensitization (SPT or RAST)
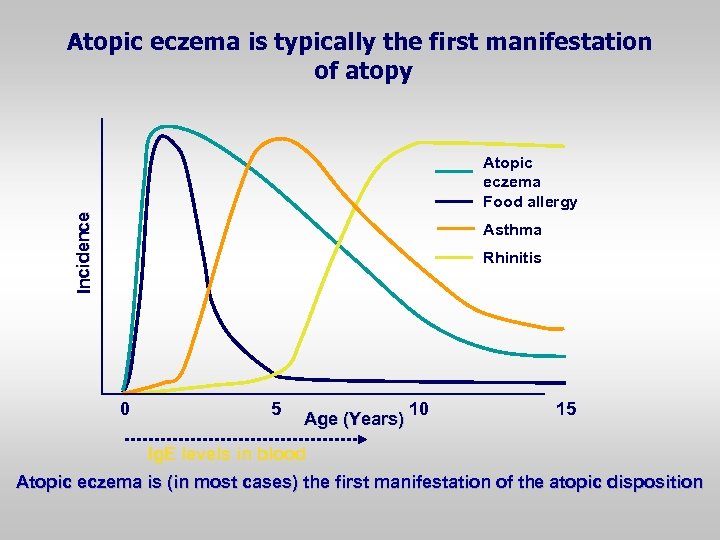 Atopic eczema is typically the first manifestation of atopy Incidence Atopic eczema Food allergy Asthma Rhinitis 0 5 Age (Years) 10 15 Ig. E levels in blood Atopic eczema is (in most cases) the first manifestation of the atopic disposition
Atopic eczema is typically the first manifestation of atopy Incidence Atopic eczema Food allergy Asthma Rhinitis 0 5 Age (Years) 10 15 Ig. E levels in blood Atopic eczema is (in most cases) the first manifestation of the atopic disposition
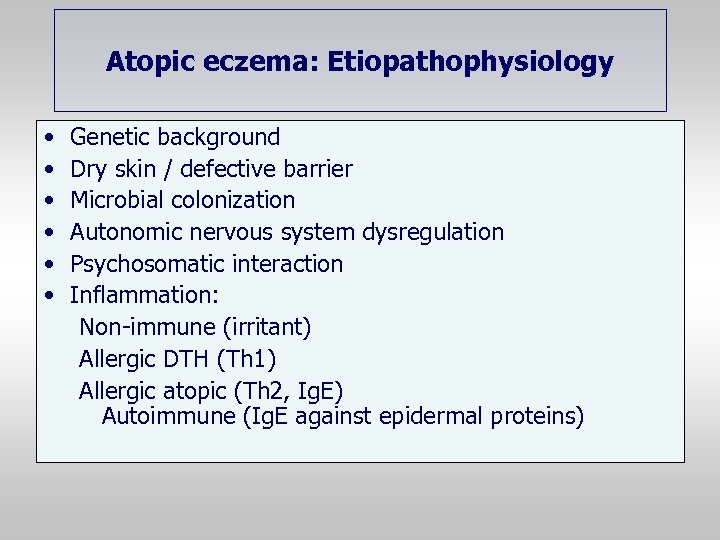 Atopic eczema: Etiopathophysiology • • • Genetic background Dry skin / defective barrier Microbial colonization Autonomic nervous system dysregulation Psychosomatic interaction Inflammation: Non-immune (irritant) Allergic DTH (Th 1) Allergic atopic (Th 2, Ig. E) Autoimmune (Ig. E against epidermal proteins)
Atopic eczema: Etiopathophysiology • • • Genetic background Dry skin / defective barrier Microbial colonization Autonomic nervous system dysregulation Psychosomatic interaction Inflammation: Non-immune (irritant) Allergic DTH (Th 1) Allergic atopic (Th 2, Ig. E) Autoimmune (Ig. E against epidermal proteins)
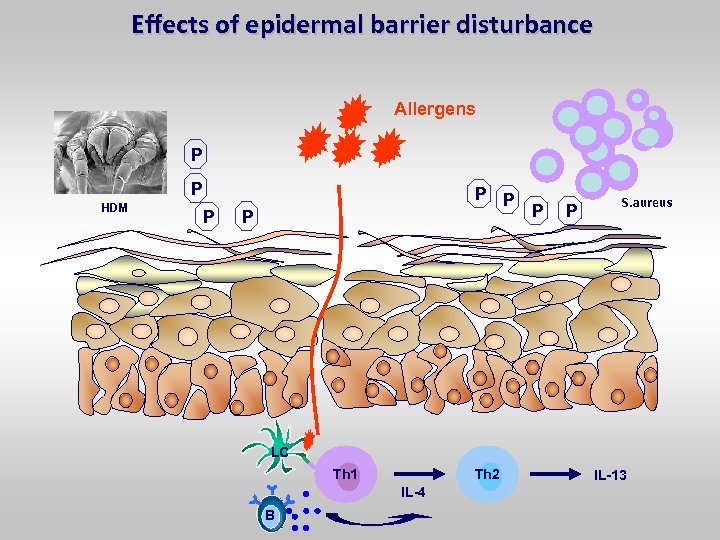 Effects of epidermal barrier disturbance Allergens P P HDM P P P S. aureus LC Th 1 Th 2 IL-4 B IL-13
Effects of epidermal barrier disturbance Allergens P P HDM P P P S. aureus LC Th 1 Th 2 IL-4 B IL-13
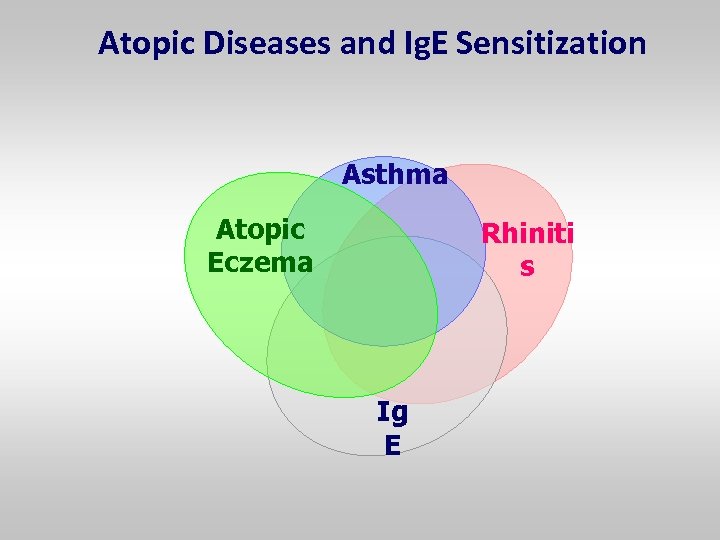 Atopic Diseases and Ig. E Sensitization Asthma Atopic Eczema Rhiniti s Ig E
Atopic Diseases and Ig. E Sensitization Asthma Atopic Eczema Rhiniti s Ig E
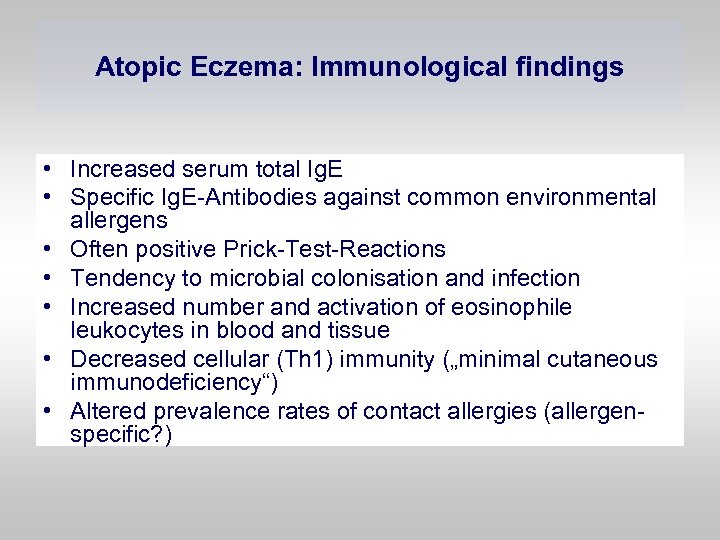 Atopic Eczema: Immunological findings • Increased serum total Ig. E • Specific Ig. E-Antibodies against common environmental allergens • Often positive Prick-Test-Reactions • Tendency to microbial colonisation and infection • Increased number and activation of eosinophile leukocytes in blood and tissue • Decreased cellular (Th 1) immunity („minimal cutaneous immunodeficiency“) • Altered prevalence rates of contact allergies (allergenspecific? )
Atopic Eczema: Immunological findings • Increased serum total Ig. E • Specific Ig. E-Antibodies against common environmental allergens • Often positive Prick-Test-Reactions • Tendency to microbial colonisation and infection • Increased number and activation of eosinophile leukocytes in blood and tissue • Decreased cellular (Th 1) immunity („minimal cutaneous immunodeficiency“) • Altered prevalence rates of contact allergies (allergenspecific? )
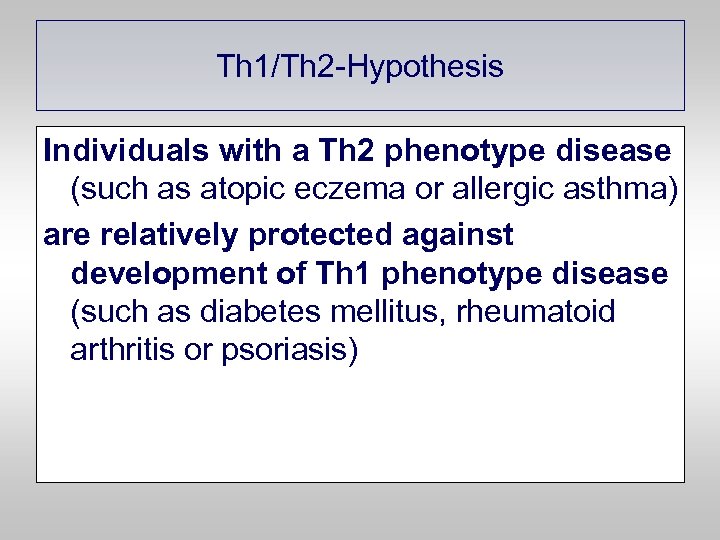 Th 1/Th 2 -Hypothesis Individuals with a Th 2 phenotype disease (such as atopic eczema or allergic asthma) are relatively protected against development of Th 1 phenotype disease (such as diabetes mellitus, rheumatoid arthritis or psoriasis)
Th 1/Th 2 -Hypothesis Individuals with a Th 2 phenotype disease (such as atopic eczema or allergic asthma) are relatively protected against development of Th 1 phenotype disease (such as diabetes mellitus, rheumatoid arthritis or psoriasis)
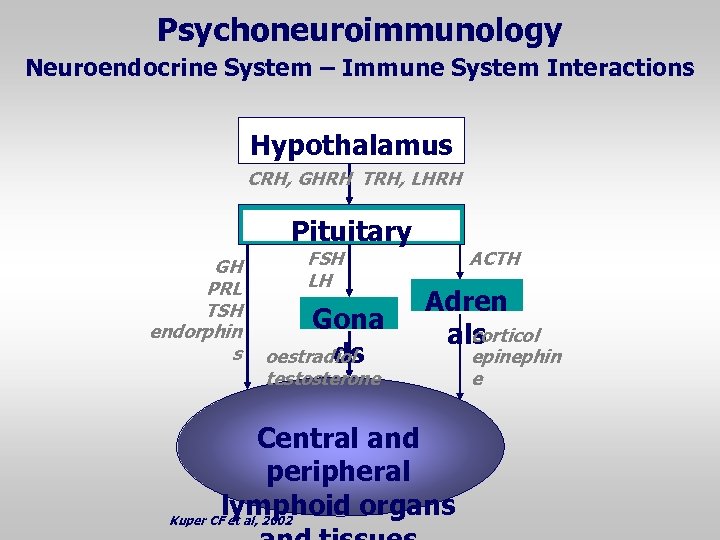 Psychoneuroimmunology Neuroendocrine System – Immune System Interactions Hypothalamus CRH, GHRH TRH, LHRH Pituitary GH PRL TSH endorphin s FSH LH Gona ds oestradiol ACTH Adren corticol als testosterone Central and peripheral lymphoid organs Kuper CF et al, 2002 epinephin e
Psychoneuroimmunology Neuroendocrine System – Immune System Interactions Hypothalamus CRH, GHRH TRH, LHRH Pituitary GH PRL TSH endorphin s FSH LH Gona ds oestradiol ACTH Adren corticol als testosterone Central and peripheral lymphoid organs Kuper CF et al, 2002 epinephin e
 Mechanisms of disturbed skin barrier function • Abnormal lipid patterns (eg ceramides) • Abnormal lipid synthesis and metabolism (eg sphingomyelinase, glucocerebrosidase) • Increased protease activity (eg SCCE) • Serin protease inhibitor defect (eg LEKTI 1) • Structural mutations (eg filaggrin, hornerin? )
Mechanisms of disturbed skin barrier function • Abnormal lipid patterns (eg ceramides) • Abnormal lipid synthesis and metabolism (eg sphingomyelinase, glucocerebrosidase) • Increased protease activity (eg SCCE) • Serin protease inhibitor defect (eg LEKTI 1) • Structural mutations (eg filaggrin, hornerin? )
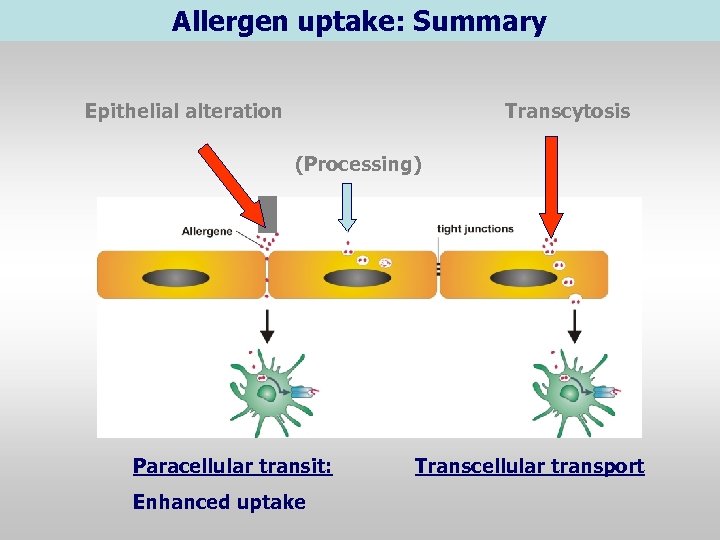 Allergen uptake: Summary Epithelial alteration Transcytosis (Processing) Paracellular transit: Enhanced uptake Transcellular transport
Allergen uptake: Summary Epithelial alteration Transcytosis (Processing) Paracellular transit: Enhanced uptake Transcellular transport
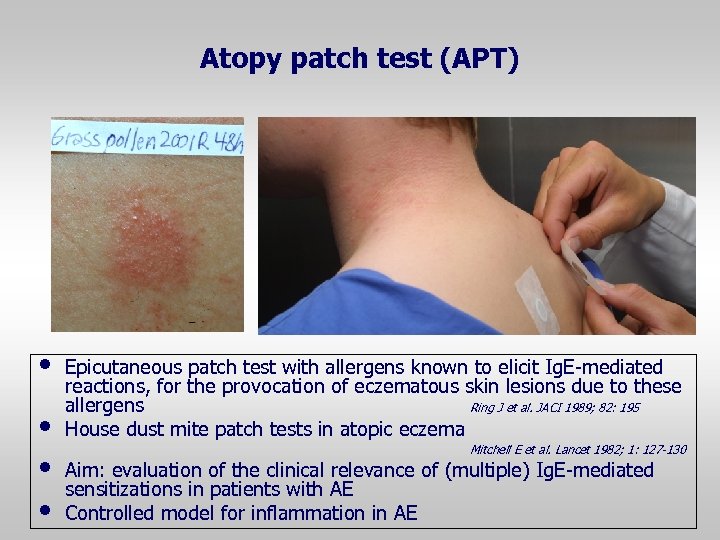 Atopy patch test (APT) • • Epicutaneous patch test with allergens known to elicit Ig. E-mediated reactions, for the provocation of eczematous skin lesions due to these allergens Ring J et al. JACI 1989; 82: 195 House dust mite patch tests in atopic eczema Mitchell E et al. Lancet 1982; 1: 127 -130 Aim: evaluation of the clinical relevance of (multiple) Ig. E-mediated sensitizations in patients with AE Controlled model for inflammation in AE
Atopy patch test (APT) • • Epicutaneous patch test with allergens known to elicit Ig. E-mediated reactions, for the provocation of eczematous skin lesions due to these allergens Ring J et al. JACI 1989; 82: 195 House dust mite patch tests in atopic eczema Mitchell E et al. Lancet 1982; 1: 127 -130 Aim: evaluation of the clinical relevance of (multiple) Ig. E-mediated sensitizations in patients with AE Controlled model for inflammation in AE
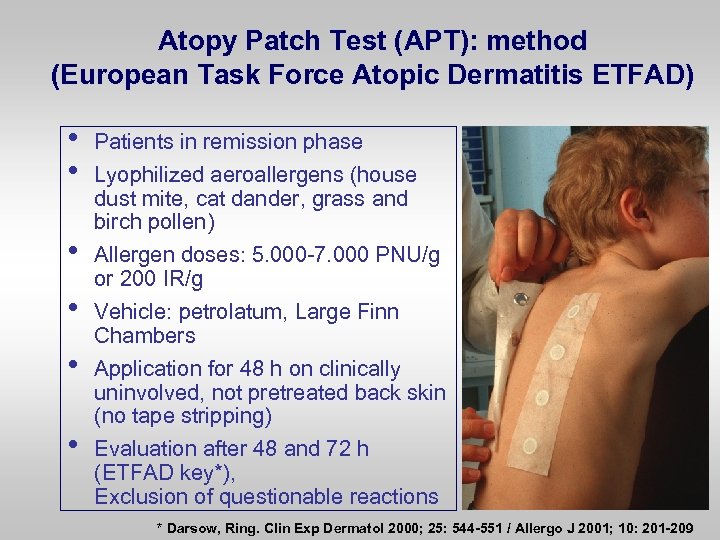 Atopy Patch Test (APT): method (European Task Force Atopic Dermatitis ETFAD) • • • Patients in remission phase Lyophilized aeroallergens (house dust mite, cat dander, grass and birch pollen) Allergen doses: 5. 000 -7. 000 PNU/g or 200 IR/g Vehicle: petrolatum, Large Finn Chambers Application for 48 h on clinically uninvolved, not pretreated back skin (no tape stripping) Evaluation after 48 and 72 h (ETFAD key*), Exclusion of questionable reactions * Darsow, Ring. Clin Exp Dermatol 2000; 25: 544 -551 / Allergo J 2001; 10: 201 -209
Atopy Patch Test (APT): method (European Task Force Atopic Dermatitis ETFAD) • • • Patients in remission phase Lyophilized aeroallergens (house dust mite, cat dander, grass and birch pollen) Allergen doses: 5. 000 -7. 000 PNU/g or 200 IR/g Vehicle: petrolatum, Large Finn Chambers Application for 48 h on clinically uninvolved, not pretreated back skin (no tape stripping) Evaluation after 48 and 72 h (ETFAD key*), Exclusion of questionable reactions * Darsow, Ring. Clin Exp Dermatol 2000; 25: 544 -551 / Allergo J 2001; 10: 201 -209
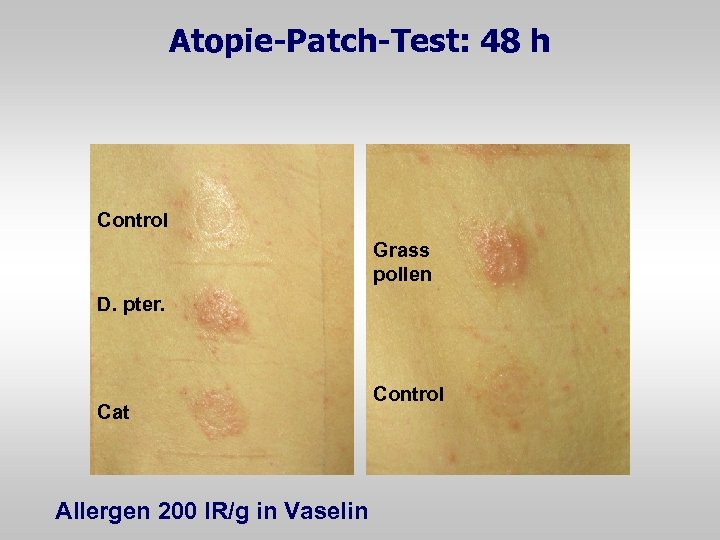 Atopie-Patch-Test: 48 h Control Grass pollen D. pter. Cat Allergen 200 IR/g in Vaselin Control
Atopie-Patch-Test: 48 h Control Grass pollen D. pter. Cat Allergen 200 IR/g in Vaselin Control
 APT in Europe
APT in Europe

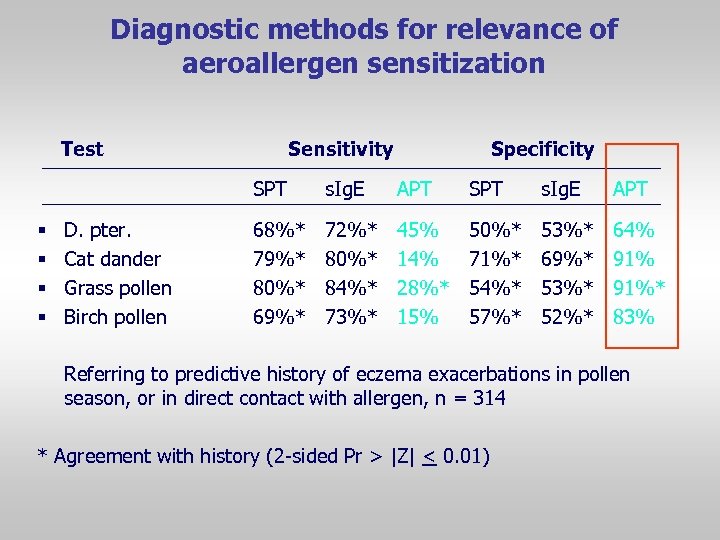 Diagnostic methods for relevance of aeroallergen sensitization Test Sensitivity Specificity SPT § § D. pter. Cat dander Grass pollen Birch pollen s. Ig. E APT SPT s. Ig. E APT 68%* 79%* 80%* 69%* 72%* 80%* 84%* 73%* 45% 14% 28%* 15% 50%* 71%* 54%* 57%* 53%* 69%* 53%* 52%* 64% 91%* 83% Referring to predictive history of eczema exacerbations in pollen season, or in direct contact with allergen, n = 314 * Agreement with history (2 -sided Pr > |Z| < 0. 01)
Diagnostic methods for relevance of aeroallergen sensitization Test Sensitivity Specificity SPT § § D. pter. Cat dander Grass pollen Birch pollen s. Ig. E APT SPT s. Ig. E APT 68%* 79%* 80%* 69%* 72%* 80%* 84%* 73%* 45% 14% 28%* 15% 50%* 71%* 54%* 57%* 53%* 69%* 53%* 52%* 64% 91%* 83% Referring to predictive history of eczema exacerbations in pollen season, or in direct contact with allergen, n = 314 * Agreement with history (2 -sided Pr > |Z| < 0. 01)
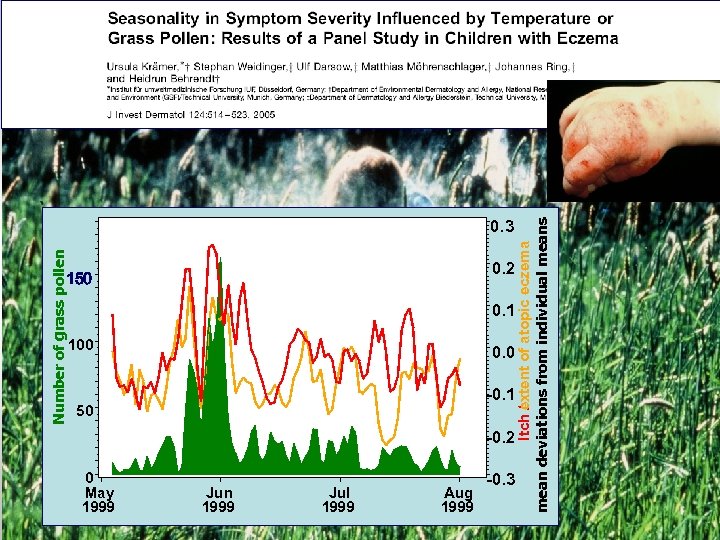 Number of grass pollen 150 0 May 1999 0. 2 0. 1 100 0. 0 50 -0. 1 -0. 2 Jun 1999 Jul 1999 Aug 1999 -0. 3 Itch extent of atopic eczema / mean deviations from individual means 0. 3
Number of grass pollen 150 0 May 1999 0. 2 0. 1 100 0. 0 50 -0. 1 -0. 2 Jun 1999 Jul 1999 Aug 1999 -0. 3 Itch extent of atopic eczema / mean deviations from individual means 0. 3
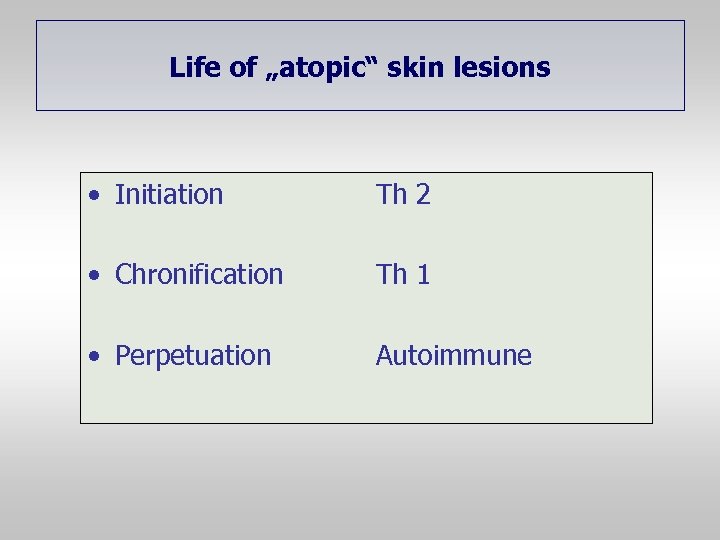 Life of „atopic“ skin lesions • Initiation Th 2 • Chronification Th 1 • Perpetuation Autoimmune
Life of „atopic“ skin lesions • Initiation Th 2 • Chronification Th 1 • Perpetuation Autoimmune
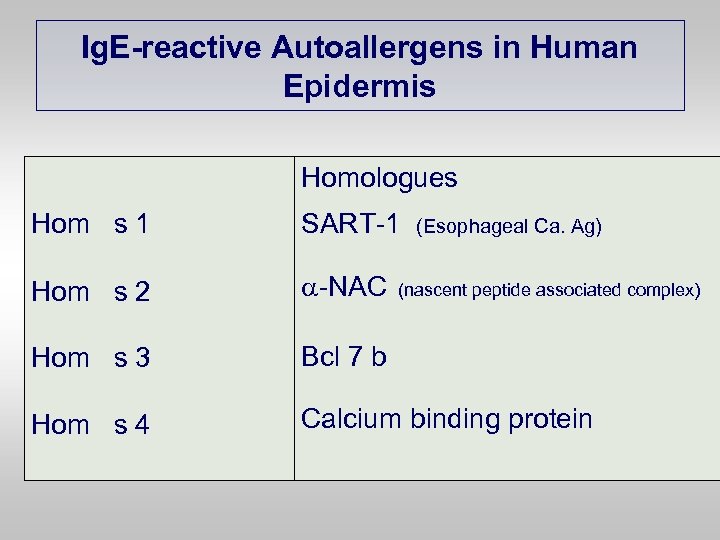 Ig. E-reactive Autoallergens in Human Epidermis Homologues Hom s 1 SART-1 Hom s 2 -NAC Hom s 3 Bcl 7 b Hom s 4 Calcium binding protein (Esophageal Ca. Ag) (nascent peptide associated complex)
Ig. E-reactive Autoallergens in Human Epidermis Homologues Hom s 1 SART-1 Hom s 2 -NAC Hom s 3 Bcl 7 b Hom s 4 Calcium binding protein (Esophageal Ca. Ag) (nascent peptide associated complex)
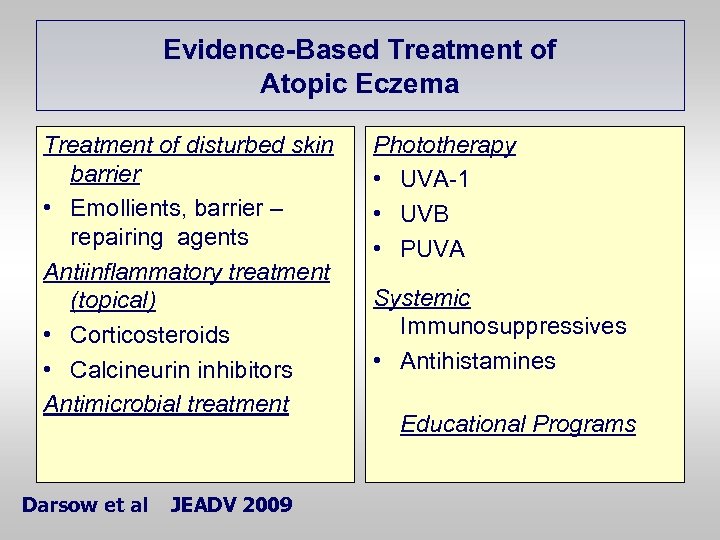 Evidence-Based Treatment of Atopic Eczema Treatment of disturbed skin barrier • Emollients, barrier – repairing agents Antiinflammatory treatment (topical) • Corticosteroids • Calcineurin inhibitors Antimicrobial treatment Darsow et al JEADV 2009 Phototherapy • UVA-1 • UVB • PUVA Systemic Immunosuppressives • Antihistamines Educational Programs
Evidence-Based Treatment of Atopic Eczema Treatment of disturbed skin barrier • Emollients, barrier – repairing agents Antiinflammatory treatment (topical) • Corticosteroids • Calcineurin inhibitors Antimicrobial treatment Darsow et al JEADV 2009 Phototherapy • UVA-1 • UVB • PUVA Systemic Immunosuppressives • Antihistamines Educational Programs
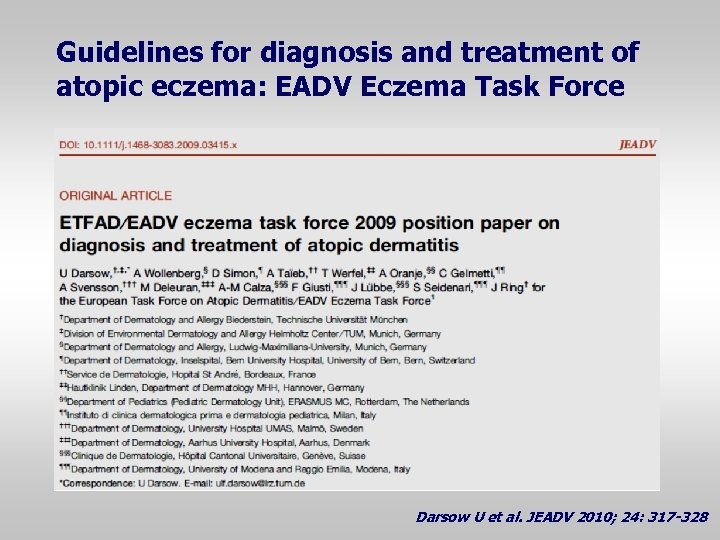 Guidelines for diagnosis and treatment of atopic eczema: EADV Eczema Task Force Darsow U et al. JEADV 2010; 24: 317 -328
Guidelines for diagnosis and treatment of atopic eczema: EADV Eczema Task Force Darsow U et al. JEADV 2010; 24: 317 -328
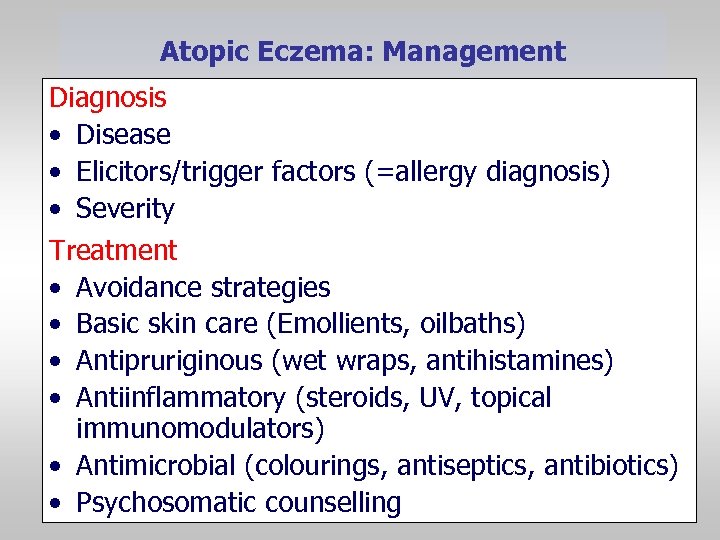 Atopic Eczema: Management Diagnosis • Disease • Elicitors/trigger factors (=allergy diagnosis) • Severity Treatment • Avoidance strategies • Basic skin care (Emollients, oilbaths) • Antipruriginous (wet wraps, antihistamines) • Antiinflammatory (steroids, UV, topical immunomodulators) • Antimicrobial (colourings, antiseptics, antibiotics) • Psychosomatic counselling
Atopic Eczema: Management Diagnosis • Disease • Elicitors/trigger factors (=allergy diagnosis) • Severity Treatment • Avoidance strategies • Basic skin care (Emollients, oilbaths) • Antipruriginous (wet wraps, antihistamines) • Antiinflammatory (steroids, UV, topical immunomodulators) • Antimicrobial (colourings, antiseptics, antibiotics) • Psychosomatic counselling
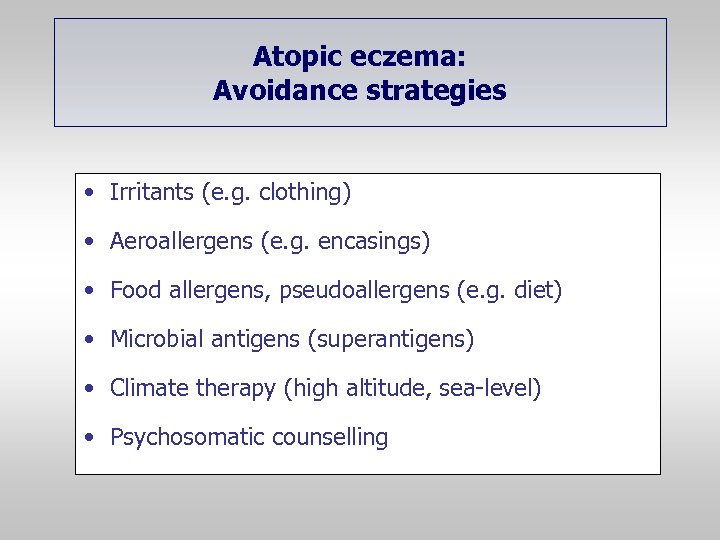 Atopic eczema: Avoidance strategies • Irritants (e. g. clothing) • Aeroallergens (e. g. encasings) • Food allergens, pseudoallergens (e. g. diet) • Microbial antigens (superantigens) • Climate therapy (high altitude, sea-level) • Psychosomatic counselling
Atopic eczema: Avoidance strategies • Irritants (e. g. clothing) • Aeroallergens (e. g. encasings) • Food allergens, pseudoallergens (e. g. diet) • Microbial antigens (superantigens) • Climate therapy (high altitude, sea-level) • Psychosomatic counselling
 Davos, Progress in Allergy, Dermatology and Immunology Congress 8 – 10 September 2012
Davos, Progress in Allergy, Dermatology and Immunology Congress 8 – 10 September 2012
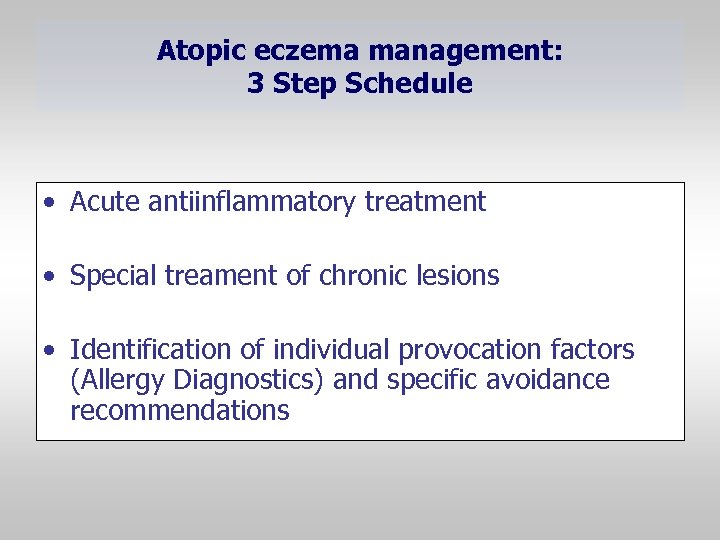 Atopic eczema management: 3 Step Schedule • Acute antiinflammatory treatment • Special treament of chronic lesions • Identification of individual provocation factors (Allergy Diagnostics) and specific avoidance recommendations
Atopic eczema management: 3 Step Schedule • Acute antiinflammatory treatment • Special treament of chronic lesions • Identification of individual provocation factors (Allergy Diagnostics) and specific avoidance recommendations
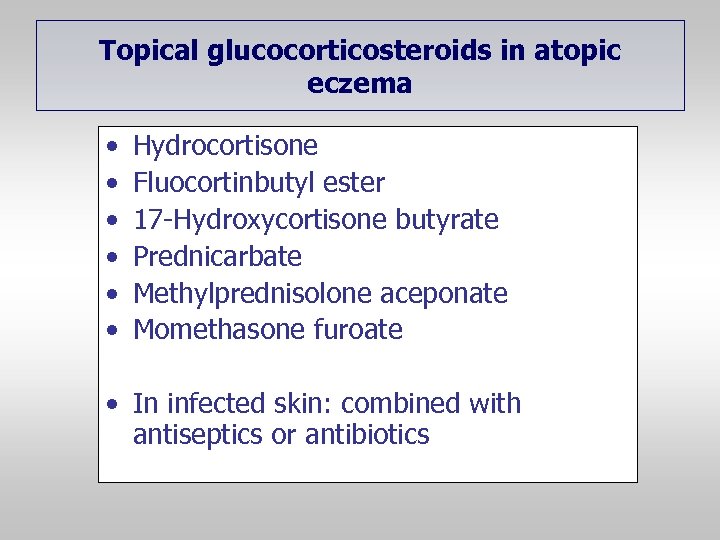 Topical glucocorticosteroids in atopic eczema • • • Hydrocortisone Fluocortinbutyl ester 17 -Hydroxycortisone butyrate Prednicarbate Methylprednisolone aceponate Momethasone furoate • In infected skin: combined with antiseptics or antibiotics
Topical glucocorticosteroids in atopic eczema • • • Hydrocortisone Fluocortinbutyl ester 17 -Hydroxycortisone butyrate Prednicarbate Methylprednisolone aceponate Momethasone furoate • In infected skin: combined with antiseptics or antibiotics
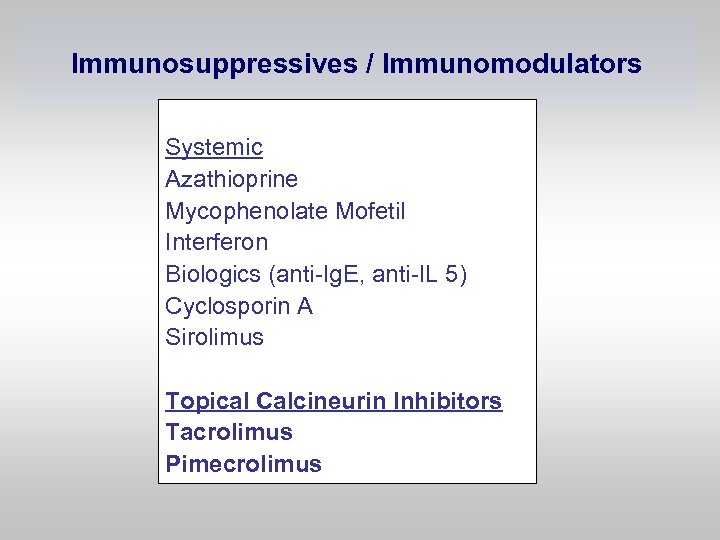 Immunosuppressives / Immunomodulators Systemic Azathioprine Mycophenolate Mofetil Interferon Biologics (anti-Ig. E, anti-IL 5) Cyclosporin A Sirolimus Topical Calcineurin Inhibitors Tacrolimus Pimecrolimus
Immunosuppressives / Immunomodulators Systemic Azathioprine Mycophenolate Mofetil Interferon Biologics (anti-Ig. E, anti-IL 5) Cyclosporin A Sirolimus Topical Calcineurin Inhibitors Tacrolimus Pimecrolimus
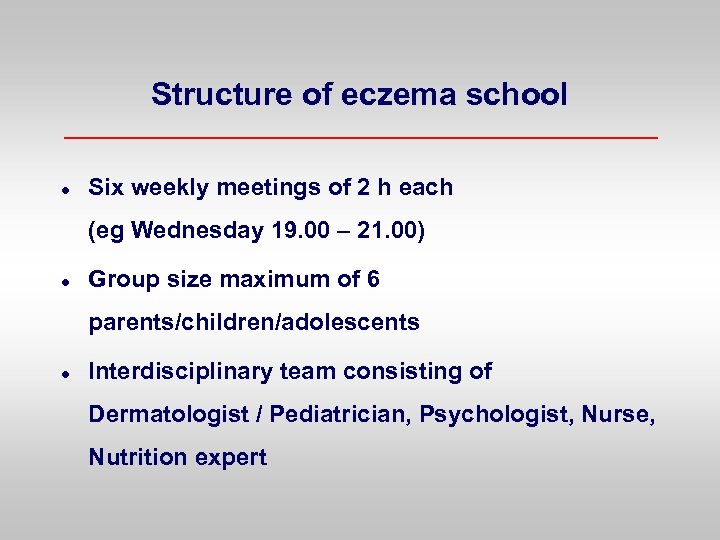 Structure of eczema school l Six weekly meetings of 2 h each (eg Wednesday 19. 00 – 21. 00) l Group size maximum of 6 parents/children/adolescents l Interdisciplinary team consisting of Dermatologist / Pediatrician, Psychologist, Nurse, Nutrition expert
Structure of eczema school l Six weekly meetings of 2 h each (eg Wednesday 19. 00 – 21. 00) l Group size maximum of 6 parents/children/adolescents l Interdisciplinary team consisting of Dermatologist / Pediatrician, Psychologist, Nurse, Nutrition expert
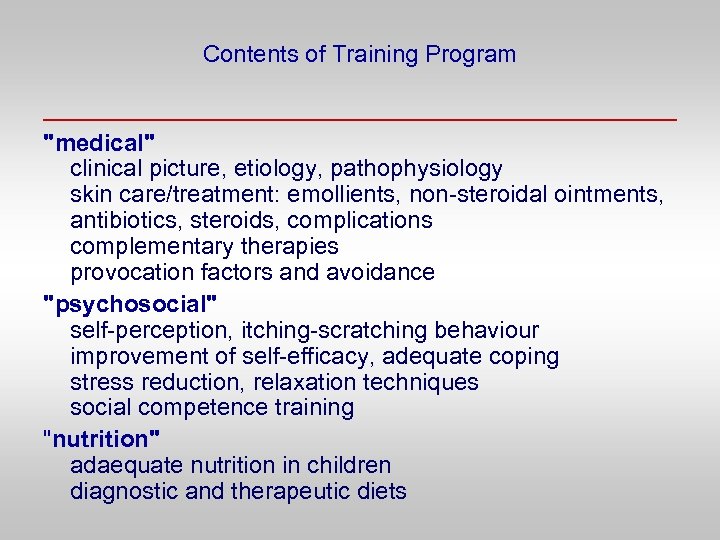 Contents of Training Program "medical" clinical picture, etiology, pathophysiology skin care/treatment: emollients, non-steroidal ointments, antibiotics, steroids, complications complementary therapies provocation factors and avoidance "psychosocial" self-perception, itching-scratching behaviour improvement of self-efficacy, adequate coping stress reduction, relaxation techniques social competence training "nutrition" adaequate nutrition in children diagnostic and therapeutic diets
Contents of Training Program "medical" clinical picture, etiology, pathophysiology skin care/treatment: emollients, non-steroidal ointments, antibiotics, steroids, complications complementary therapies provocation factors and avoidance "psychosocial" self-perception, itching-scratching behaviour improvement of self-efficacy, adequate coping stress reduction, relaxation techniques social competence training "nutrition" adaequate nutrition in children diagnostic and therapeutic diets
 "train the trainer" • Block 1 30 h: Medizin, Psychologie, Pädagogik, Ernährung • Block 2 10 h: Teilnahme an einer Schulung, eine Sitzung mit Supervision www. disa. de (allinfo, AG- Neurodermitis)
"train the trainer" • Block 1 30 h: Medizin, Psychologie, Pädagogik, Ernährung • Block 2 10 h: Teilnahme an einer Schulung, eine Sitzung mit Supervision www. disa. de (allinfo, AG- Neurodermitis)
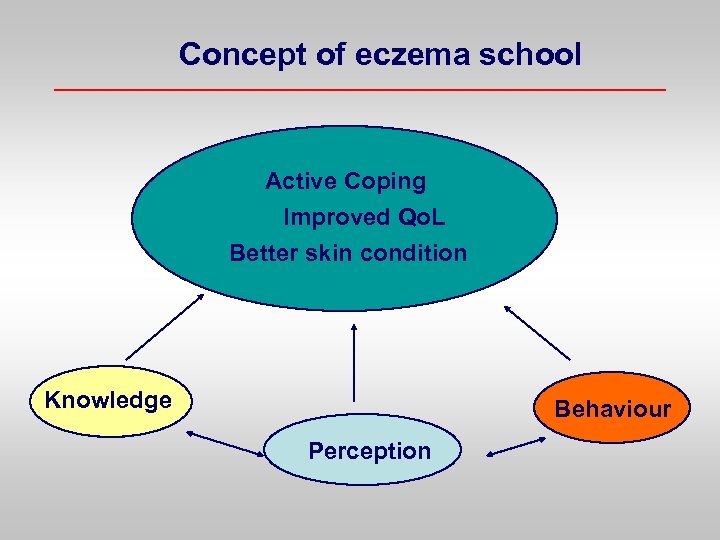 Concept of eczema school Active Coping Improved Qo. L Better skin condition Knowledge Behaviour Perception
Concept of eczema school Active Coping Improved Qo. L Better skin condition Knowledge Behaviour Perception
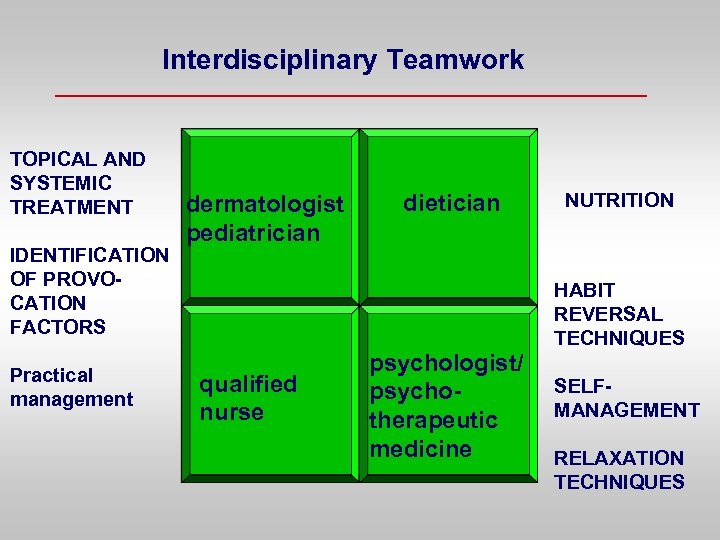 Interdisciplinary Teamwork TOPICAL AND SYSTEMIC TREATMENT IDENTIFICATION OF PROVOCATION FACTORS Practical management dermatologist pediatrician dietician NUTRITION HABIT REVERSAL TECHNIQUES qualified nurse psychologist/ psychotherapeutic medicine SELFMANAGEMENT RELAXATION TECHNIQUES
Interdisciplinary Teamwork TOPICAL AND SYSTEMIC TREATMENT IDENTIFICATION OF PROVOCATION FACTORS Practical management dermatologist pediatrician dietician NUTRITION HABIT REVERSAL TECHNIQUES qualified nurse psychologist/ psychotherapeutic medicine SELFMANAGEMENT RELAXATION TECHNIQUES
 The A B C of patient management in allergy (Ring 2006) • • • A B C D E = = = Avoidance strategies Basic antiinflammatory treatment Care (skin, airways) Direct symptom relief Empowerment of patient (Educational programs eg „Eczema school“)
The A B C of patient management in allergy (Ring 2006) • • • A B C D E = = = Avoidance strategies Basic antiinflammatory treatment Care (skin, airways) Direct symptom relief Empowerment of patient (Educational programs eg „Eczema school“)
 Trust yourself and your suggestive power! • Talk more about desired effects than about side-effects • Give hope • Illustrate your message with real experience – even if only anecdotal • Motivate patient to take own responsibility („you will be your own skin doctor“) • Turn off the clock!
Trust yourself and your suggestive power! • Talk more about desired effects than about side-effects • Give hope • Illustrate your message with real experience – even if only anecdotal • Motivate patient to take own responsibility („you will be your own skin doctor“) • Turn off the clock!
 Thanks to Heidrun Behrendt Carsten Schmidt-Weber U. Darsow K. Brockow K. Eyerich J. Gutermuth M. Mempel M. Ollert F. Pfab C. Schnopp C. Traidl-Hoffmann S. Weidinger
Thanks to Heidrun Behrendt Carsten Schmidt-Weber U. Darsow K. Brockow K. Eyerich J. Gutermuth M. Mempel M. Ollert F. Pfab C. Schnopp C. Traidl-Hoffmann S. Weidinger
 7 th Georg Rajka International Symposium on Atopic Dermatitis, Moshi, Tansania 15 – 18 January 2012
7 th Georg Rajka International Symposium on Atopic Dermatitis, Moshi, Tansania 15 – 18 January 2012


