50444cf7b04011c527da2285aeb8a01e.ppt
- Количество слайдов: 54
 Immediate Life Support Revision Lecture
Immediate Life Support Revision Lecture
 Causes and Prevention of Cardiac Arrest
Causes and Prevention of Cardiac Arrest
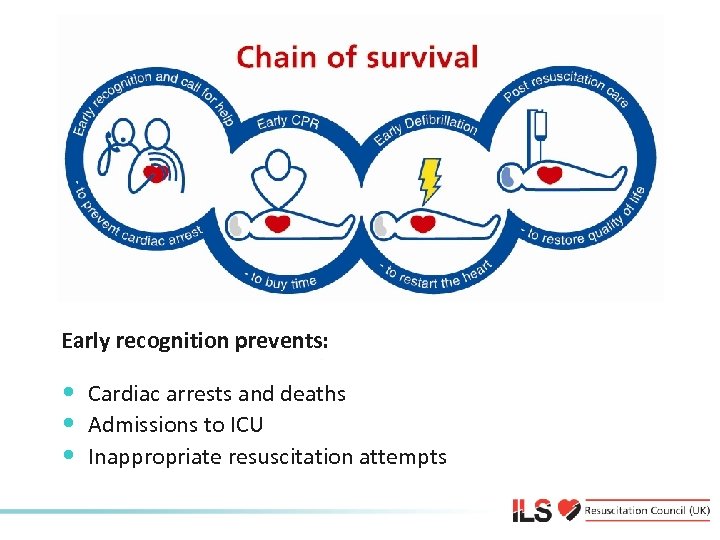 Chain of survival Early recognition prevents: • Cardiac arrests and deaths • Admissions to ICU • Inappropriate resuscitation attempts
Chain of survival Early recognition prevents: • Cardiac arrests and deaths • Admissions to ICU • Inappropriate resuscitation attempts
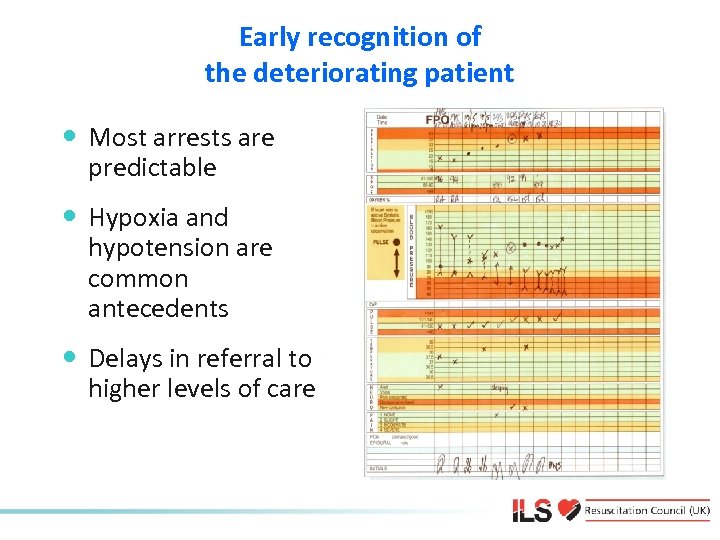 Early recognition of the deteriorating patient • Most arrests are predictable • Hypoxia and hypotension are common antecedents • Delays in referral to higher levels of care
Early recognition of the deteriorating patient • Most arrests are predictable • Hypoxia and hypotension are common antecedents • Delays in referral to higher levels of care
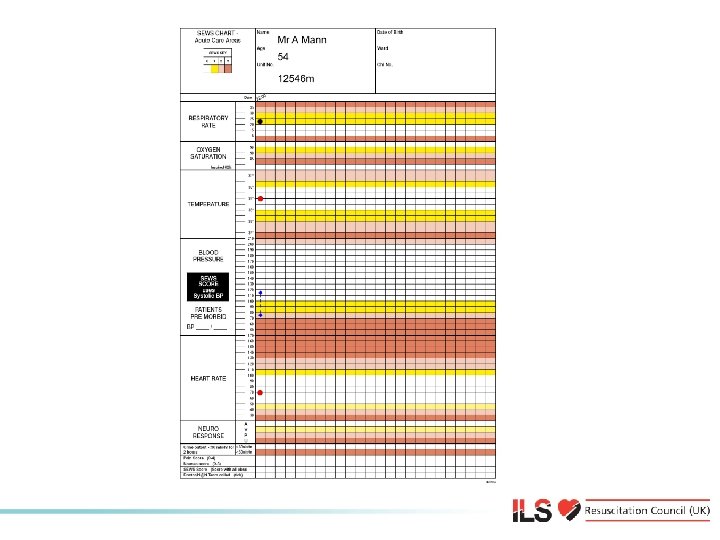
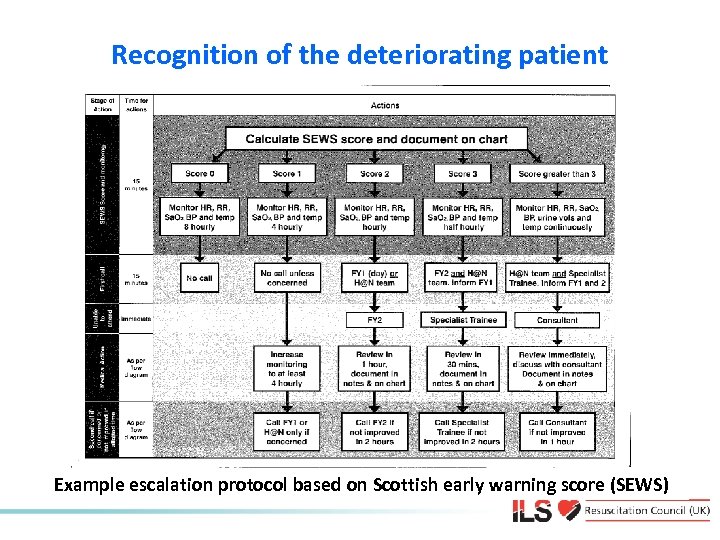 Recognition of the deteriorating patient Example escalation protocol based on Scottish early warning score (SEWS)
Recognition of the deteriorating patient Example escalation protocol based on Scottish early warning score (SEWS)
 Recognition of the deteriorating patient • Several alternative systems to cardiac arrest team • e. g. Medical emergency team (MET) • Track changes in physiology • e. g. Early warning scores • Trigger a response if abnormal values: • Call senior nurse • Call doctor • Call resuscitation team
Recognition of the deteriorating patient • Several alternative systems to cardiac arrest team • e. g. Medical emergency team (MET) • Track changes in physiology • e. g. Early warning scores • Trigger a response if abnormal values: • Call senior nurse • Call doctor • Call resuscitation team
 The ABCDE approach to the deteriorating patient Airway Breathing Circulation Disability Exposure
The ABCDE approach to the deteriorating patient Airway Breathing Circulation Disability Exposure
 ABCDE approach Underlying principles: • Complete initial assessment • Treat life-threatening problems • Reassessment • Assess effects of treatment/interventions • Call for help early
ABCDE approach Underlying principles: • Complete initial assessment • Treat life-threatening problems • Reassessment • Assess effects of treatment/interventions • Call for help early
 ABCDE approach • Personal safety • Patient responsiveness • First impression • Vital signs • Respiratory rate, Sp. O 2, pulse, BP, GCS, temperature
ABCDE approach • Personal safety • Patient responsiveness • First impression • Vital signs • Respiratory rate, Sp. O 2, pulse, BP, GCS, temperature
 ABCDE approach Airway Causes of airway obstruction: • CNS depression • Blood • Vomit • Foreign body • Trauma • Infection • Inflammation • Laryngospasm • Bronchospasm
ABCDE approach Airway Causes of airway obstruction: • CNS depression • Blood • Vomit • Foreign body • Trauma • Infection • Inflammation • Laryngospasm • Bronchospasm
 ABCDE approach Airway Recognition of airway obstruction: • Talking • Difficulty breathing, distressed, choking • Shortness of breath • Noisy breathing • Stridor, wheeze, gurgling • See-saw respiratory pattern, accessory muscles
ABCDE approach Airway Recognition of airway obstruction: • Talking • Difficulty breathing, distressed, choking • Shortness of breath • Noisy breathing • Stridor, wheeze, gurgling • See-saw respiratory pattern, accessory muscles
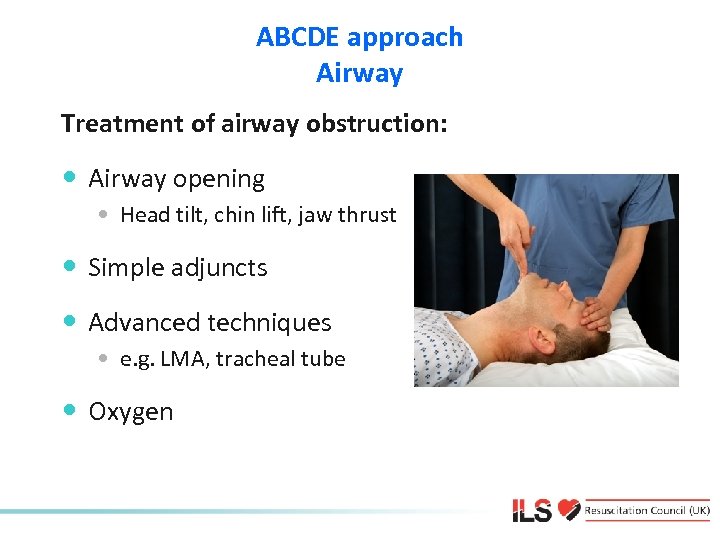 ABCDE approach Airway Treatment of airway obstruction: • Airway opening • Head tilt, chin lift, jaw thrust • Simple adjuncts • Advanced techniques • e. g. LMA, tracheal tube • Oxygen
ABCDE approach Airway Treatment of airway obstruction: • Airway opening • Head tilt, chin lift, jaw thrust • Simple adjuncts • Advanced techniques • e. g. LMA, tracheal tube • Oxygen
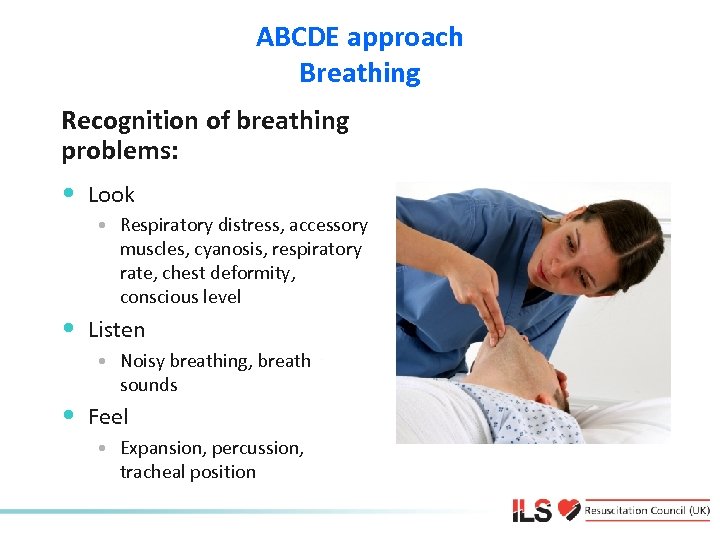 ABCDE approach Breathing Recognition of breathing problems: • Look • Respiratory distress, accessory muscles, cyanosis, respiratory rate, chest deformity, conscious level • Listen • Noisy breathing, breath sounds • Feel • Expansion, percussion, tracheal position
ABCDE approach Breathing Recognition of breathing problems: • Look • Respiratory distress, accessory muscles, cyanosis, respiratory rate, chest deformity, conscious level • Listen • Noisy breathing, breath sounds • Feel • Expansion, percussion, tracheal position
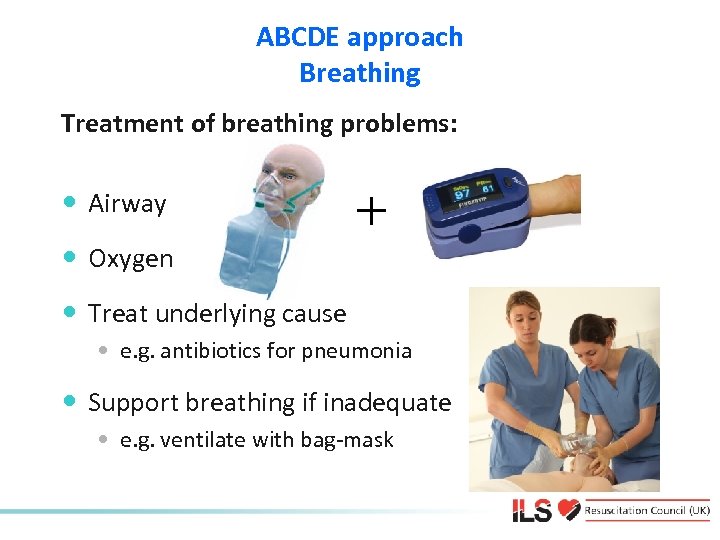 ABCDE approach Breathing Treatment of breathing problems: • Airway • Oxygen + • Treat underlying cause • e. g. antibiotics for pneumonia • Support breathing if inadequate • e. g. ventilate with bag-mask
ABCDE approach Breathing Treatment of breathing problems: • Airway • Oxygen + • Treat underlying cause • e. g. antibiotics for pneumonia • Support breathing if inadequate • e. g. ventilate with bag-mask
 ABCDE approach Circulation Causes of circulation problems: • Primary • • Acute coronary syndromes Arrhythmias Hypertensive heart disease Valve disease Drugs Inherited cardiac diseases Electrolyte/acid base abnormalities • Secondary • • • Asphyxia Hypoxaemia Blood loss Hypothermia Septic shock
ABCDE approach Circulation Causes of circulation problems: • Primary • • Acute coronary syndromes Arrhythmias Hypertensive heart disease Valve disease Drugs Inherited cardiac diseases Electrolyte/acid base abnormalities • Secondary • • • Asphyxia Hypoxaemia Blood loss Hypothermia Septic shock
 ABCDE approach Circulation Recognition of circulation problems: • Look at the patient • Pulse - tachycardia, bradycardia • Peripheral perfusion - capillary refill time • Blood pressure • Organ perfusion • Chest pain, mental state, urine output • Bleeding, fluid losses
ABCDE approach Circulation Recognition of circulation problems: • Look at the patient • Pulse - tachycardia, bradycardia • Peripheral perfusion - capillary refill time • Blood pressure • Organ perfusion • Chest pain, mental state, urine output • Bleeding, fluid losses
 ABCDE approach Circulation Treatment of circulation problems: • • • Airway, Breathing Oxygen IV/IO access, take bloods Treat cause Fluid challenge +
ABCDE approach Circulation Treatment of circulation problems: • • • Airway, Breathing Oxygen IV/IO access, take bloods Treat cause Fluid challenge +
 ABCDE approach Circulation Acute Coronary Syndromes • Unstable angina or myocardial infarction • Treatment • • Aspirin 300 mg orally (crushed/chewed) Nitroglycerine (GTN spray or tablet) Oxygen guided by pulse oximetry Morphine (or diamorphine) • Consider reperfusion therapy (PCI, thrombolysis)
ABCDE approach Circulation Acute Coronary Syndromes • Unstable angina or myocardial infarction • Treatment • • Aspirin 300 mg orally (crushed/chewed) Nitroglycerine (GTN spray or tablet) Oxygen guided by pulse oximetry Morphine (or diamorphine) • Consider reperfusion therapy (PCI, thrombolysis)
 ABCDE approach Disability Recognition • AVPU or GCS • Pupils Treatment • ABC • Treat underlying cause • Blood glucose • If < 4 mmol l-1 give glucose • Consider lateral position • Check drug chart
ABCDE approach Disability Recognition • AVPU or GCS • Pupils Treatment • ABC • Treat underlying cause • Blood glucose • If < 4 mmol l-1 give glucose • Consider lateral position • Check drug chart
 ABCDE approach Exposure • Remove clothes to enable examination • e. g. injuries, bleeding, rashes • Avoid heat loss • Maintain dignity
ABCDE approach Exposure • Remove clothes to enable examination • e. g. injuries, bleeding, rashes • Avoid heat loss • Maintain dignity
 Any questions?
Any questions?
 Summary • Early recognition of the deteriorating patient may prevent cardiac arrest • Most patients have warning symptoms and signs before cardiac arrest • Airway, breathing or circulation problems can cause cardiac arrest • ABCDE approach to recognise and treat patients at risk of cardiac arrest
Summary • Early recognition of the deteriorating patient may prevent cardiac arrest • Most patients have warning symptoms and signs before cardiac arrest • Airway, breathing or circulation problems can cause cardiac arrest • ABCDE approach to recognise and treat patients at risk of cardiac arrest
 Advanced Life Support Algorithm
Advanced Life Support Algorithm
 ALS algorithm • ILS providers should use those skills in which they are proficient • If using an AED – switch on and follow the prompts • Ensure high quality chest compressions • Ensure expert help is coming
ALS algorithm • ILS providers should use those skills in which they are proficient • If using an AED – switch on and follow the prompts • Ensure high quality chest compressions • Ensure expert help is coming
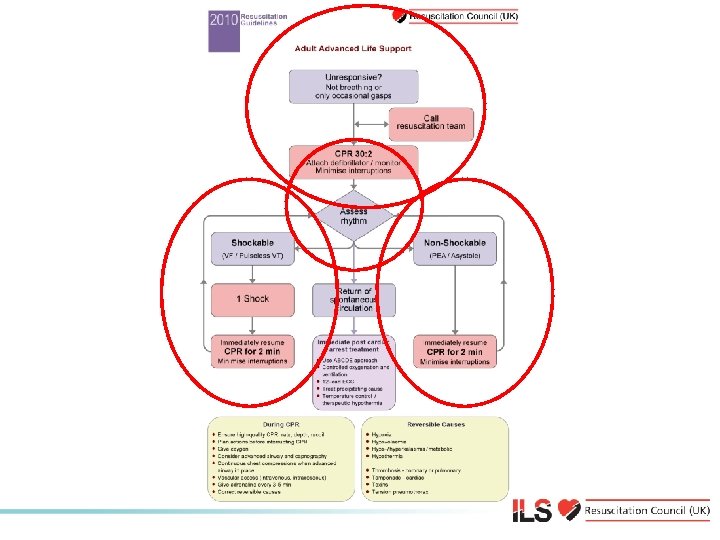 Adult ALS Algorithm
Adult ALS Algorithm
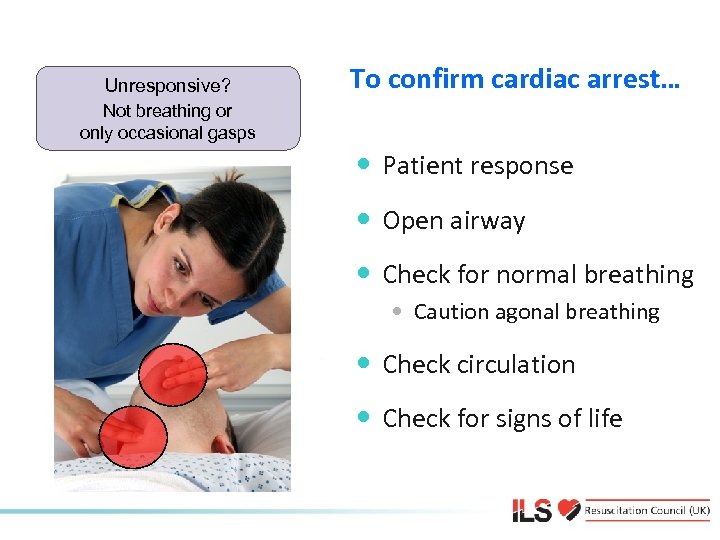 Unresponsive? Not breathing or only occasional gasps To confirm cardiac arrest… • Patient response • Open airway • Check for normal breathing • Caution agonal breathing • Check circulation • Check for signs of life
Unresponsive? Not breathing or only occasional gasps To confirm cardiac arrest… • Patient response • Open airway • Check for normal breathing • Caution agonal breathing • Check circulation • Check for signs of life
 Unresponsive? Cardiac arrest confirmed Not breathing or only occasional gasps Call resuscitation team 2222
Unresponsive? Cardiac arrest confirmed Not breathing or only occasional gasps Call resuscitation team 2222
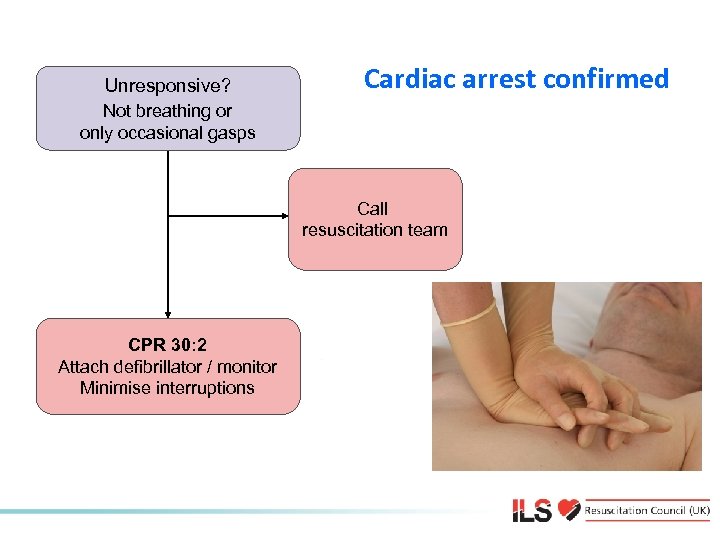 Unresponsive? Cardiac arrest confirmed Not breathing or only occasional gasps Call resuscitation team CPR 30: 2 Attach defibrillator / monitor Minimise interruptions
Unresponsive? Cardiac arrest confirmed Not breathing or only occasional gasps Call resuscitation team CPR 30: 2 Attach defibrillator / monitor Minimise interruptions
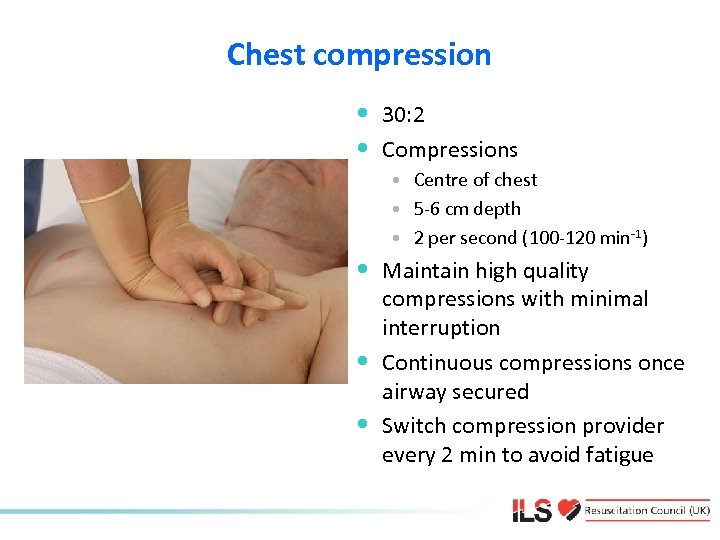 Chest compression • 30: 2 • Compressions • Centre of chest • 5 -6 cm depth • 2 per second (100 -120 min-1) • Maintain high quality • • compressions with minimal interruption Continuous compressions once airway secured Switch compression provider every 2 min to avoid fatigue
Chest compression • 30: 2 • Compressions • Centre of chest • 5 -6 cm depth • 2 per second (100 -120 min-1) • Maintain high quality • • compressions with minimal interruption Continuous compressions once airway secured Switch compression provider every 2 min to avoid fatigue
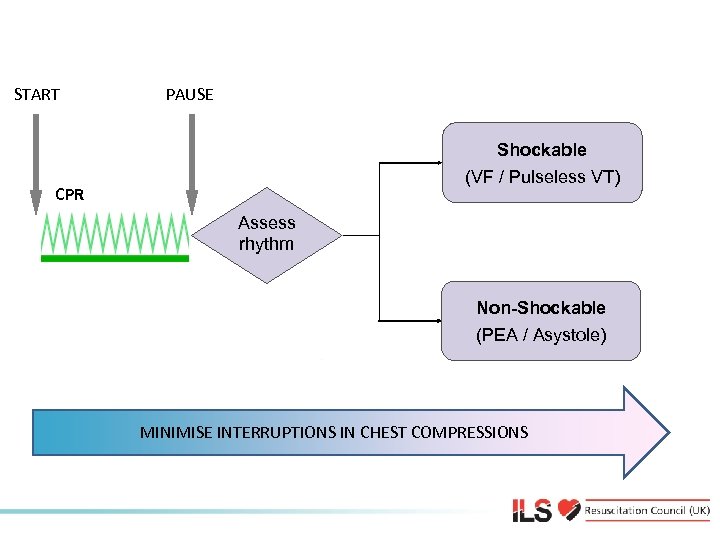 Shockable and Non-Shockable START PAUSE Shockable (VF / Pulseless VT) CPR Assess rhythm Non-Shockable (PEA / Asystole) MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
Shockable and Non-Shockable START PAUSE Shockable (VF / Pulseless VT) CPR Assess rhythm Non-Shockable (PEA / Asystole) MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
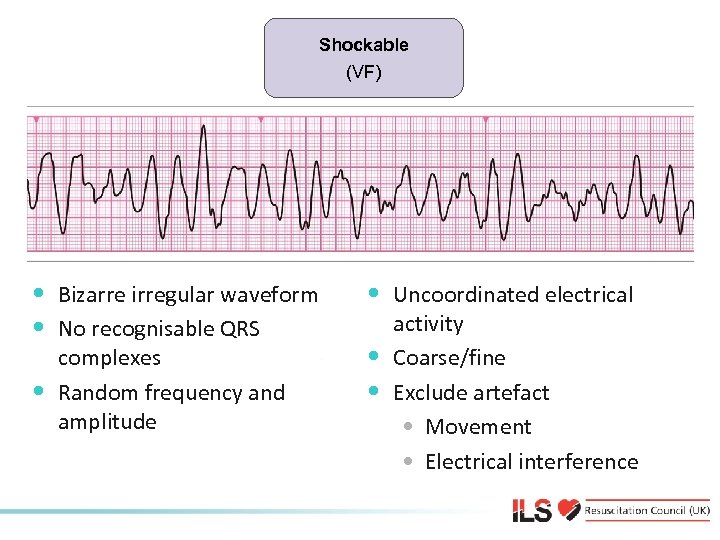 Shockable (VF) Shockable • Bizarre irregular waveform • No recognisable QRS • complexes Random frequency and amplitude • Uncoordinated electrical • • activity Coarse/fine Exclude artefact • Movement • Electrical interference
Shockable (VF) Shockable • Bizarre irregular waveform • No recognisable QRS • complexes Random frequency and amplitude • Uncoordinated electrical • • activity Coarse/fine Exclude artefact • Movement • Electrical interference
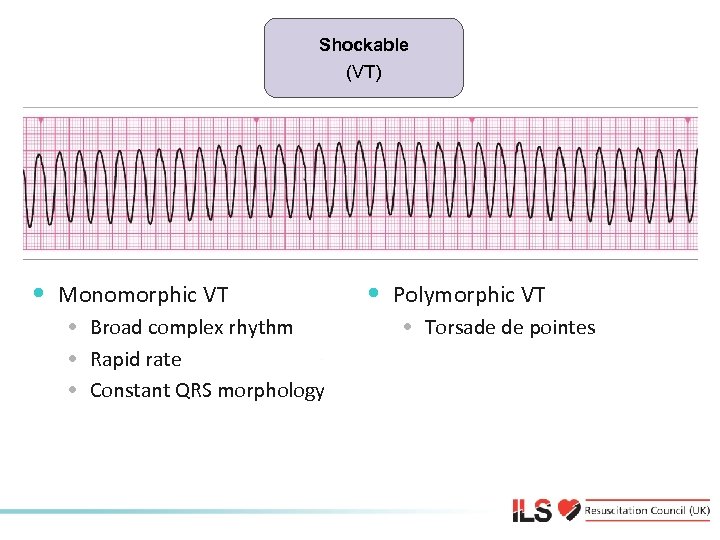 Shockable (VT) Shockable • Monomorphic VT • Broad complex rhythm • Rapid rate • Constant QRS morphology • Polymorphic VT • Torsade de pointes
Shockable (VT) Shockable • Monomorphic VT • Broad complex rhythm • Rapid rate • Constant QRS morphology • Polymorphic VT • Torsade de pointes
 Automated External Defibrillation • If not confident in rhythm recognition use an AED • Start CPR whilst awaiting AED to arrive • Switch on and follow AED prompts
Automated External Defibrillation • If not confident in rhythm recognition use an AED • Start CPR whilst awaiting AED to arrive • Switch on and follow AED prompts
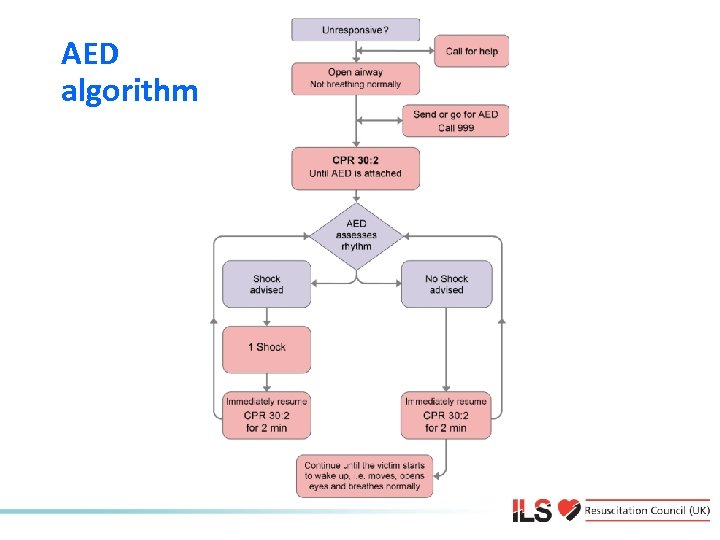 AED algorithm
AED algorithm
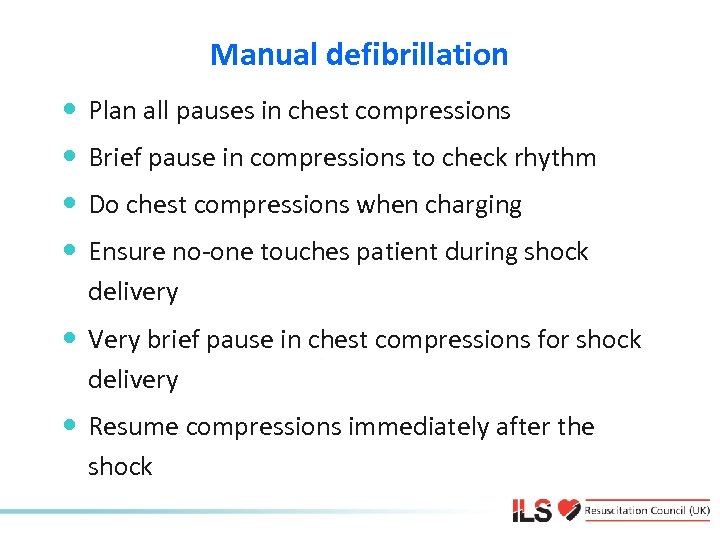 Manual defibrillation • Plan all pauses in chest compressions • Brief pause in compressions to check rhythm • Do chest compressions when charging • Ensure no-one touches patient during shock delivery • Very brief pause in chest compressions for shock delivery • Resume compressions immediately after the shock
Manual defibrillation • Plan all pauses in chest compressions • Brief pause in compressions to check rhythm • Do chest compressions when charging • Ensure no-one touches patient during shock delivery • Very brief pause in chest compressions for shock delivery • Resume compressions immediately after the shock
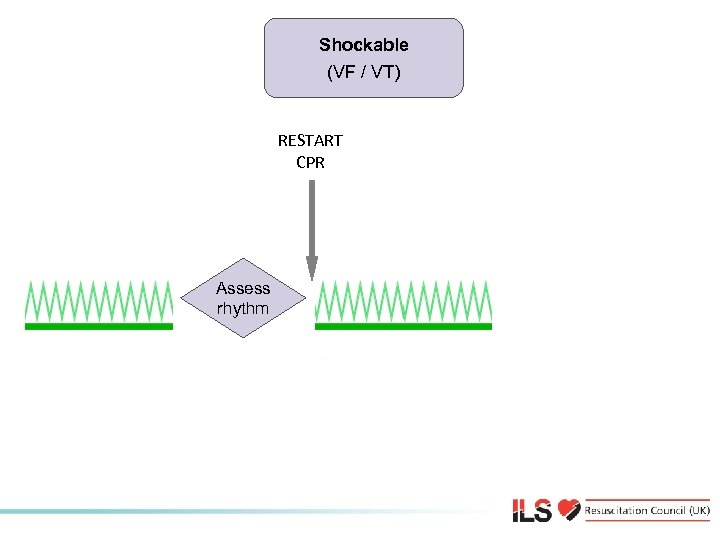 Shockable/ VT) (VF Shockable RESTART CPR Assess rhythm
Shockable/ VT) (VF Shockable RESTART CPR Assess rhythm
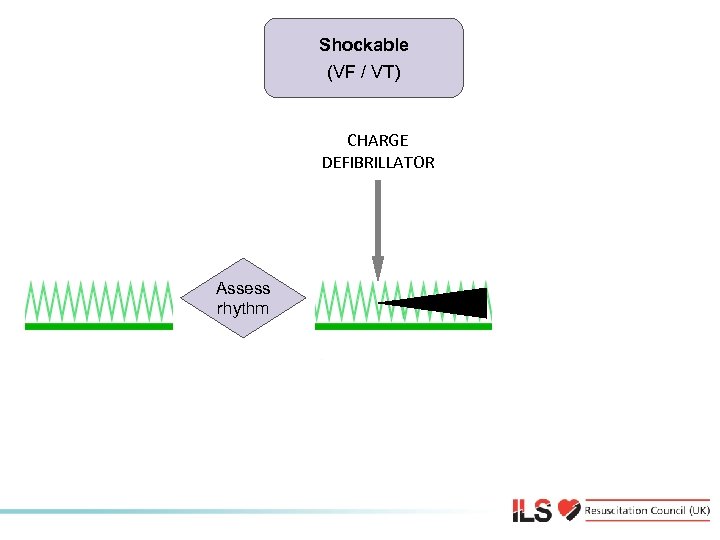 Shockable (VT) (VF / VT) Shockable CHARGE DEFIBRILLATOR Assess rhythm
Shockable (VT) (VF / VT) Shockable CHARGE DEFIBRILLATOR Assess rhythm
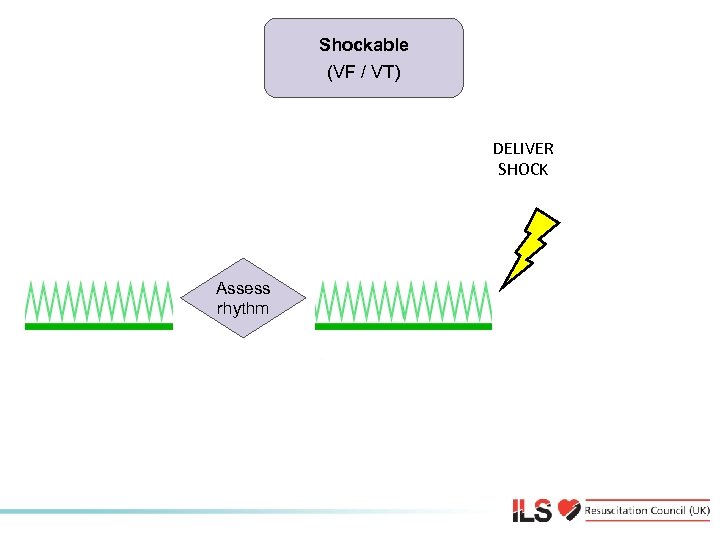 Shockable/ VT) (VF Shockable DELIVER SHOCK Assess rhythm
Shockable/ VT) (VF Shockable DELIVER SHOCK Assess rhythm
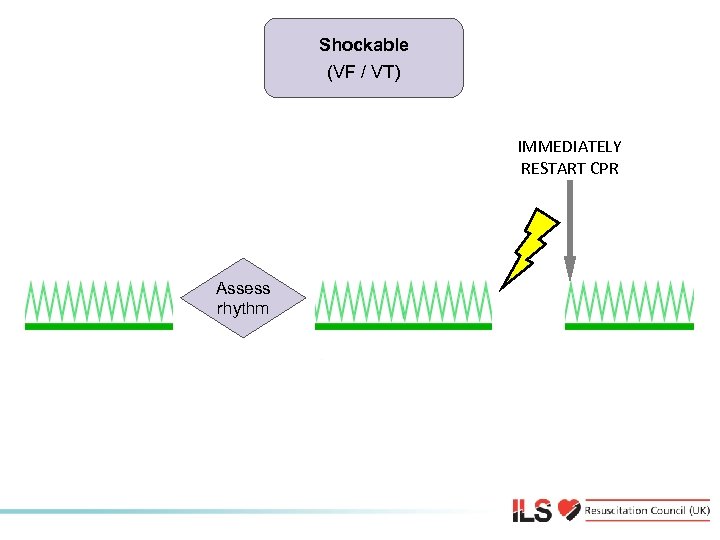 Shockable/ VT) (VF Shockable IMMEDIATELY RESTART CPR Assess rhythm
Shockable/ VT) (VF Shockable IMMEDIATELY RESTART CPR Assess rhythm
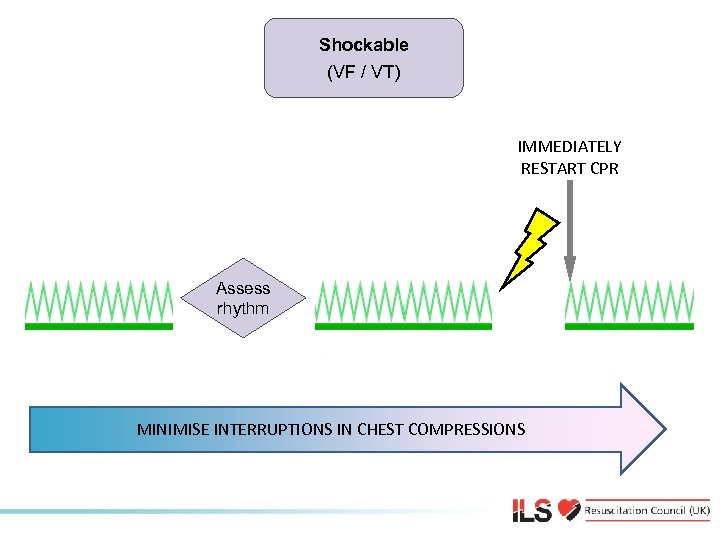 Shockable (VF / VT) IMMEDIATELY RESTART CPR Shockable (VF / VT) Assess rhythm MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
Shockable (VF / VT) IMMEDIATELY RESTART CPR Shockable (VF / VT) Assess rhythm MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
 Manual defibrillation energies • Vary with manufacturer • Check local equipment • If unsure, deliver highest available energy • DO NOT DELAY SHOCK • Energy levels for manual defibrillators on this course
Manual defibrillation energies • Vary with manufacturer • Check local equipment • If unsure, deliver highest available energy • DO NOT DELAY SHOCK • Energy levels for manual defibrillators on this course
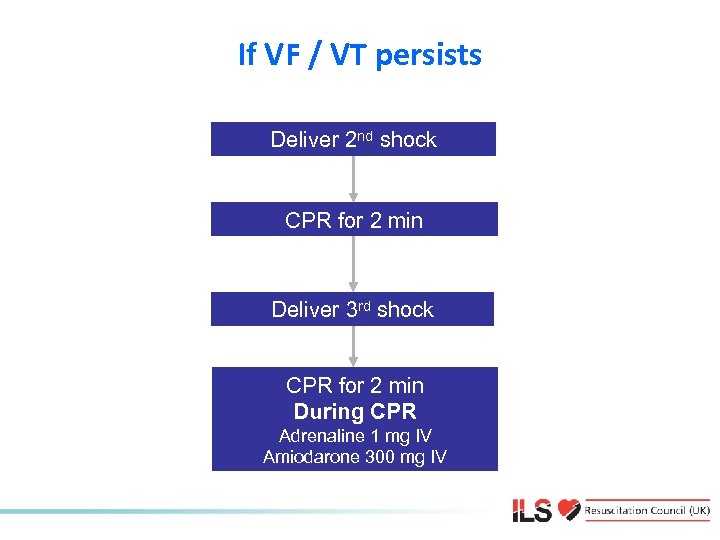 If VF / VT persists Deliver 2 nd shock CPR for 2 min Deliver 3 rd shock CPR for 2 min During CPR Adrenaline 1 mg IV Amiodarone 300 mg IV
If VF / VT persists Deliver 2 nd shock CPR for 2 min Deliver 3 rd shock CPR for 2 min During CPR Adrenaline 1 mg IV Amiodarone 300 mg IV
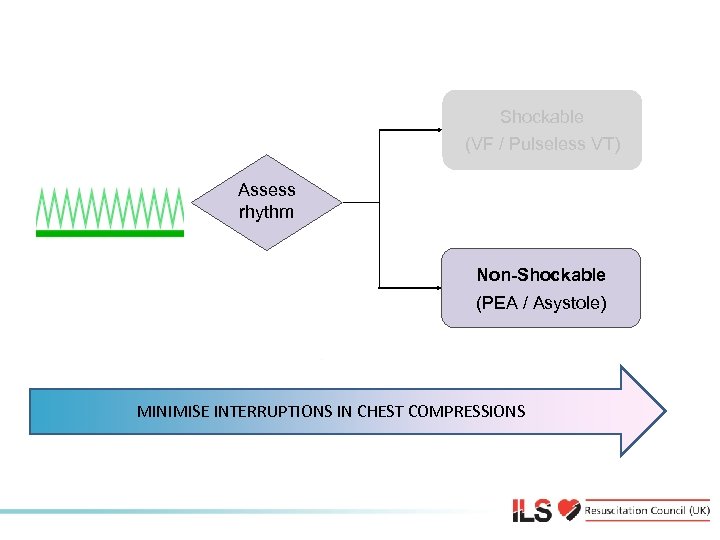 Non-Shockable (VF / Pulseless VT) Assess rhythm Non-Shockable (PEA / Asystole) MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
Non-Shockable (VF / Pulseless VT) Assess rhythm Non-Shockable (PEA / Asystole) MINIMISE INTERRUPTIONS IN CHEST COMPRESSIONS
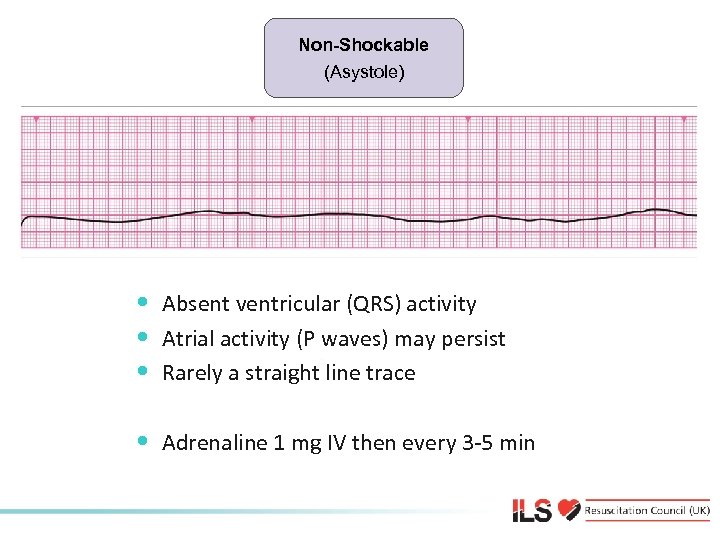 Non-shockable (Asystole) Non-Shockable • Absent ventricular (QRS) activity • Atrial activity (P waves) may persist • Rarely a straight line trace • Adrenaline 1 mg IV then every 3 -5 min
Non-shockable (Asystole) Non-Shockable • Absent ventricular (QRS) activity • Atrial activity (P waves) may persist • Rarely a straight line trace • Adrenaline 1 mg IV then every 3 -5 min
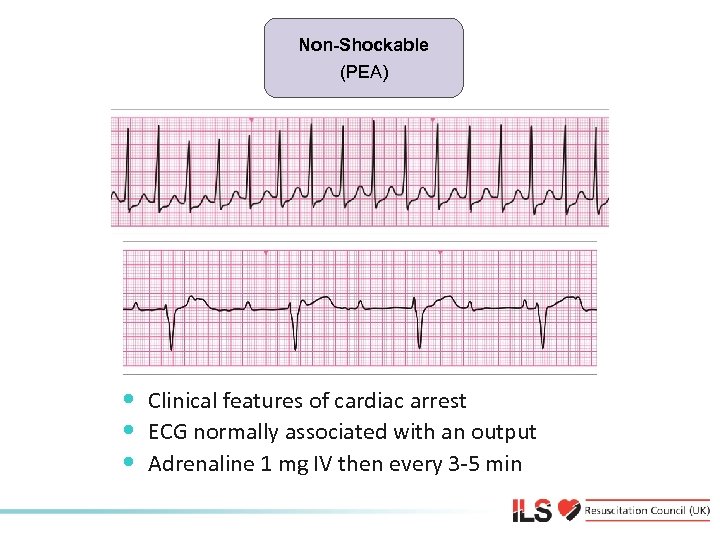 Non-shockable (Asystole) (PEA) Non-Shockable • Clinical features of cardiac arrest • ECG normally associated with an output • Adrenaline 1 mg IV then every 3 -5 min
Non-shockable (Asystole) (PEA) Non-Shockable • Clinical features of cardiac arrest • ECG normally associated with an output • Adrenaline 1 mg IV then every 3 -5 min
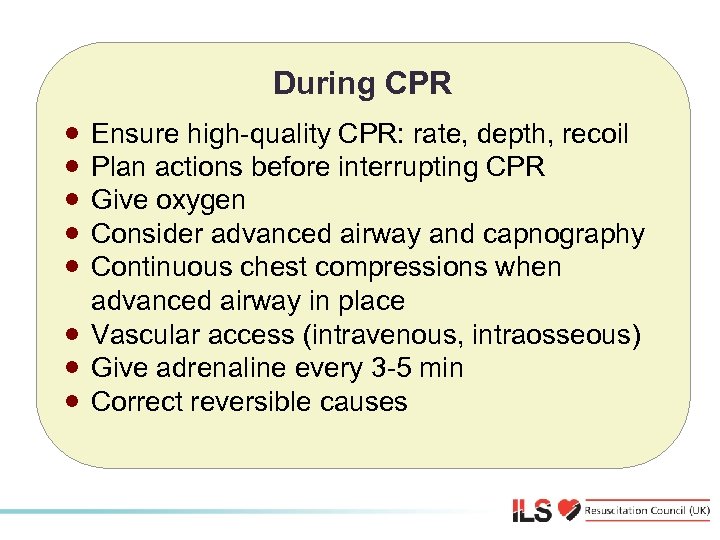 During CPR · · · · Ensure high-quality CPR: rate, depth, recoil Plan actions before interrupting CPR Give oxygen Consider advanced airway and capnography Continuous chest compressions when advanced airway in place Vascular access (intravenous, intraosseous) Give adrenaline every 3 -5 min Correct reversible causes
During CPR · · · · Ensure high-quality CPR: rate, depth, recoil Plan actions before interrupting CPR Give oxygen Consider advanced airway and capnography Continuous chest compressions when advanced airway in place Vascular access (intravenous, intraosseous) Give adrenaline every 3 -5 min Correct reversible causes
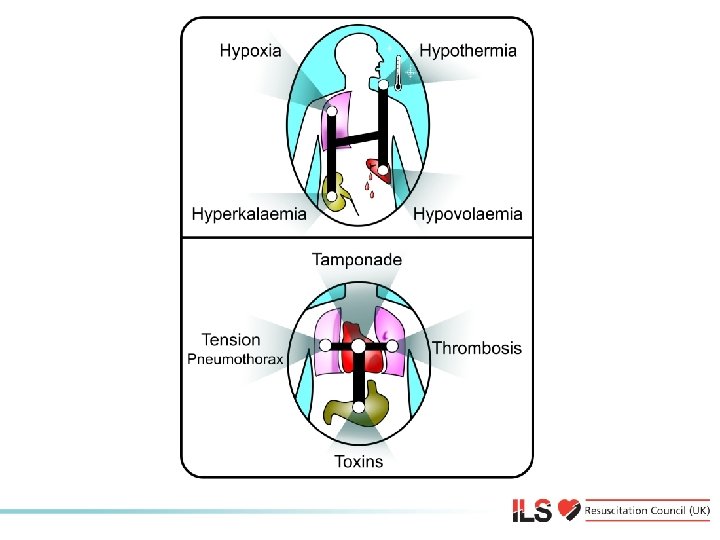 Reversible causes
Reversible causes
 Airway and ventilation • Secure airway: • Supraglottic airway device e. g. LMA, i-gel • Tracheal tube • Do not attempt intubation unless trained and competent to do so • Once airway secured, if possible, do not interrupt chest compressions for ventilation • Avoid hyperventilation • Capnography
Airway and ventilation • Secure airway: • Supraglottic airway device e. g. LMA, i-gel • Tracheal tube • Do not attempt intubation unless trained and competent to do so • Once airway secured, if possible, do not interrupt chest compressions for ventilation • Avoid hyperventilation • Capnography
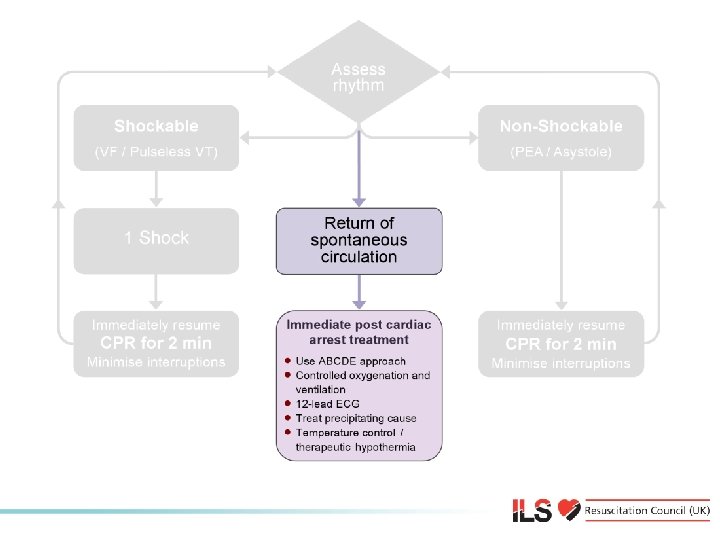 Immediate post-cardiac arrest treatment
Immediate post-cardiac arrest treatment
 Resuscitation team • Roles planned in advance • Identify team leader • Importance of non-technical skills • • Task management Team working Situational awareness Decision making • Structured communication • SBAR or RSVP
Resuscitation team • Roles planned in advance • Identify team leader • Importance of non-technical skills • • Task management Team working Situational awareness Decision making • Structured communication • SBAR or RSVP
 Any questions?
Any questions?
 Summary • Importance of high quality chest compressions • Minimise interruptions in chest compressions • Shockable rhythms are VF/pulseless VT • Non-shockable rhythms are PEA/Asystole • Use an AED if not sure about rhythms • Correct reversible causes of cardiac arrest • Role of resuscitation team
Summary • Importance of high quality chest compressions • Minimise interruptions in chest compressions • Shockable rhythms are VF/pulseless VT • Non-shockable rhythms are PEA/Asystole • Use an AED if not sure about rhythms • Correct reversible causes of cardiac arrest • Role of resuscitation team
 Immediate Life Support Course Slide set All rights reserved © Resuscitation Council (UK) 2010
Immediate Life Support Course Slide set All rights reserved © Resuscitation Council (UK) 2010


