c0280486cee6bc2e29441b8bdeb73baf.ppt
- Количество слайдов: 62
 Imaging in Dementia: Options for Clinical Practice 2014 2015+ John A. Bertelson, MD Clinical Chief of Neurology, Seton Brain and Spine Institute Assistant Professor of Medicine, Dell Medical School, UT Austin Clinical Assistant Professor of Psychology, UT Austin
Imaging in Dementia: Options for Clinical Practice 2014 2015+ John A. Bertelson, MD Clinical Chief of Neurology, Seton Brain and Spine Institute Assistant Professor of Medicine, Dell Medical School, UT Austin Clinical Assistant Professor of Psychology, UT Austin
 Disclosures n None
Disclosures n None
 Outline n Early Imaging n Indications for Imaging in Dementia n Imaging Techniques n n MRI PET n Imaging of Alzheimer’s Disease n Future Directions
Outline n Early Imaging n Indications for Imaging in Dementia n Imaging Techniques n n MRI PET n Imaging of Alzheimer’s Disease n Future Directions
 Early Imaging Modality What am I? n Initially described in 1918 1 n Low resolution n High morbidity, including: n Meningeal irritation, 6 hrs: n n n Headache Nausea Emesis Elevation in BP Became obsolete in 1971 1: AJNR 2012
Early Imaging Modality What am I? n Initially described in 1918 1 n Low resolution n High morbidity, including: n Meningeal irritation, 6 hrs: n n n Headache Nausea Emesis Elevation in BP Became obsolete in 1971 1: AJNR 2012
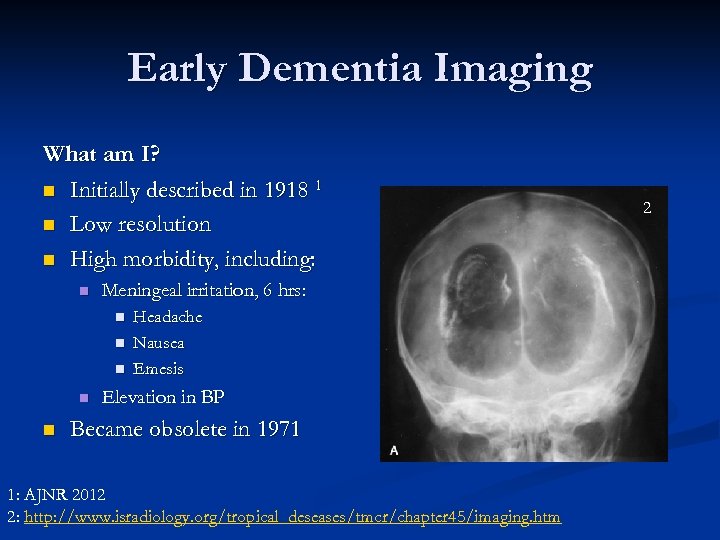 Early Dementia Imaging What am I? n Initially described in 1918 1 n Low resolution n High morbidity, including: n Meningeal irritation, 6 hrs: n n n Headache Nausea Emesis Elevation in BP Became obsolete in 1971 1: AJNR 2012 2: http: //www. isradiology. org/tropical_deseases/tmcr/chapter 45/imaging. htm 2
Early Dementia Imaging What am I? n Initially described in 1918 1 n Low resolution n High morbidity, including: n Meningeal irritation, 6 hrs: n n n Headache Nausea Emesis Elevation in BP Became obsolete in 1971 1: AJNR 2012 2: http: //www. isradiology. org/tropical_deseases/tmcr/chapter 45/imaging. htm 2
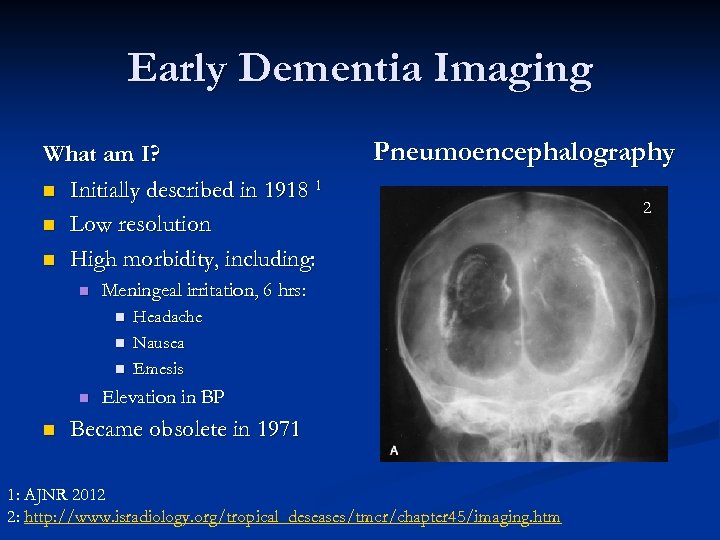 Early Dementia Imaging What am I? n Initially described in 1918 1 n Low resolution n High morbidity, including: n Meningeal irritation, 6 hrs: n n n Pneumoencephalography Headache Nausea Emesis Elevation in BP Became obsolete in 1971 1: AJNR 2012 2: http: //www. isradiology. org/tropical_deseases/tmcr/chapter 45/imaging. htm 2
Early Dementia Imaging What am I? n Initially described in 1918 1 n Low resolution n High morbidity, including: n Meningeal irritation, 6 hrs: n n n Pneumoencephalography Headache Nausea Emesis Elevation in BP Became obsolete in 1971 1: AJNR 2012 2: http: //www. isradiology. org/tropical_deseases/tmcr/chapter 45/imaging. htm 2
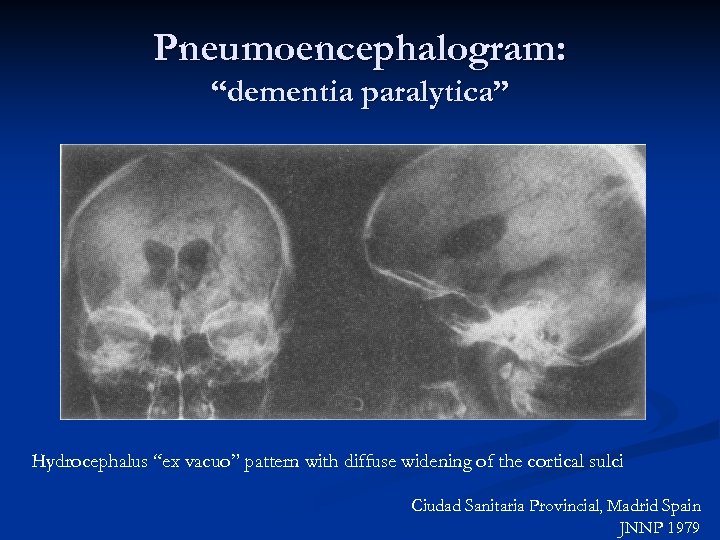 Pneumoencephalogram: “dementia paralytica” Hydrocephalus “ex vacuo” pattern with diffuse widening of the cortical sulci Ciudad Sanitaria Provincial, Madrid Spain JNNP 1979
Pneumoencephalogram: “dementia paralytica” Hydrocephalus “ex vacuo” pattern with diffuse widening of the cortical sulci Ciudad Sanitaria Provincial, Madrid Spain JNNP 1979
 Modern Imaging
Modern Imaging
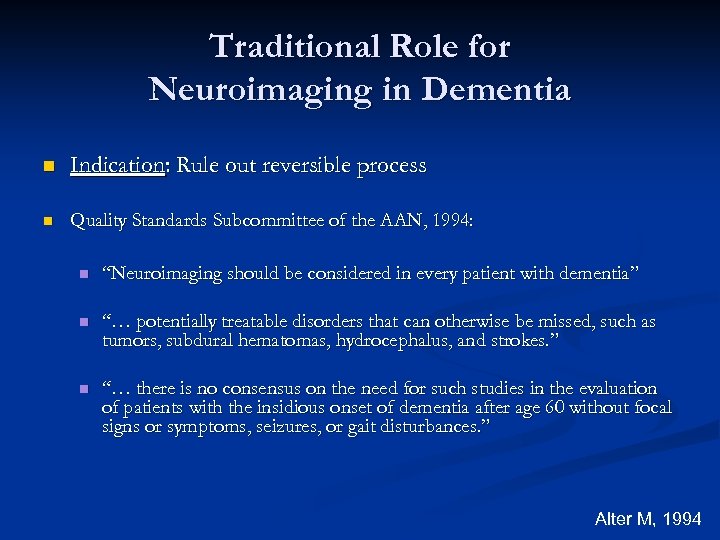 Traditional Role for Neuroimaging in Dementia n Indication: Rule out reversible process n Quality Standards Subcommittee of the AAN, 1994: n “Neuroimaging should be considered in every patient with dementia” n “… potentially treatable disorders that can otherwise be missed, such as tumors, subdural hematomas, hydrocephalus, and strokes. ” n “… there is no consensus on the need for such studies in the evaluation of patients with the insidious onset of dementia after age 60 without focal signs or symptoms, seizures, or gait disturbances. ” Alter M, 1994
Traditional Role for Neuroimaging in Dementia n Indication: Rule out reversible process n Quality Standards Subcommittee of the AAN, 1994: n “Neuroimaging should be considered in every patient with dementia” n “… potentially treatable disorders that can otherwise be missed, such as tumors, subdural hematomas, hydrocephalus, and strokes. ” n “… there is no consensus on the need for such studies in the evaluation of patients with the insidious onset of dementia after age 60 without focal signs or symptoms, seizures, or gait disturbances. ” Alter M, 1994
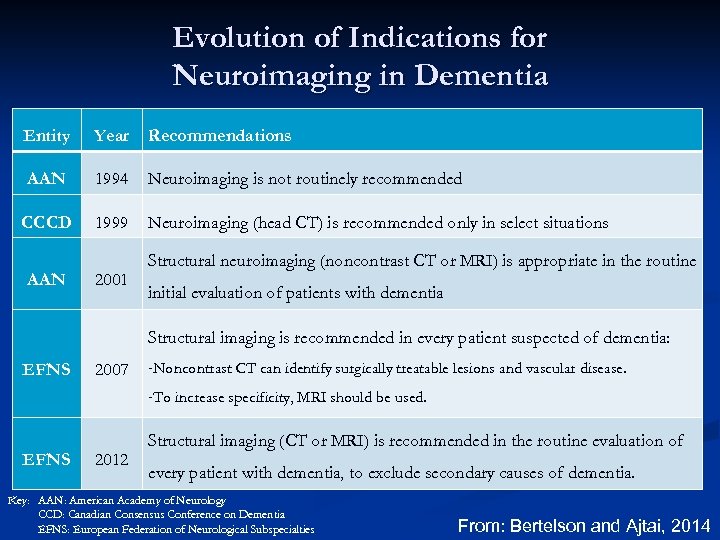 Evolution of Indications for Neuroimaging in Dementia Entity Year Recommendations AAN 1994 Neuroimaging is not routinely recommended CCCD 1999 Neuroimaging (head CT) is recommended only in select situations AAN 2001 Structural neuroimaging (noncontrast CT or MRI) is appropriate in the routine initial evaluation of patients with dementia Structural imaging is recommended in every patient suspected of dementia: EFNS 2007 -Noncontrast CT can identify surgically treatable lesions and vascular disease. -To increase specificity, MRI should be used. EFNS 2012 Structural imaging (CT or MRI) is recommended in the routine evaluation of every patient with dementia, to exclude secondary causes of dementia. Key: AAN: American Academy of Neurology CCD: Canadian Consensus Conference on Dementia EFNS: European Federation of Neurological Subspecialties From: Bertelson and Ajtai, 2014
Evolution of Indications for Neuroimaging in Dementia Entity Year Recommendations AAN 1994 Neuroimaging is not routinely recommended CCCD 1999 Neuroimaging (head CT) is recommended only in select situations AAN 2001 Structural neuroimaging (noncontrast CT or MRI) is appropriate in the routine initial evaluation of patients with dementia Structural imaging is recommended in every patient suspected of dementia: EFNS 2007 -Noncontrast CT can identify surgically treatable lesions and vascular disease. -To increase specificity, MRI should be used. EFNS 2012 Structural imaging (CT or MRI) is recommended in the routine evaluation of every patient with dementia, to exclude secondary causes of dementia. Key: AAN: American Academy of Neurology CCD: Canadian Consensus Conference on Dementia EFNS: European Federation of Neurological Subspecialties From: Bertelson and Ajtai, 2014
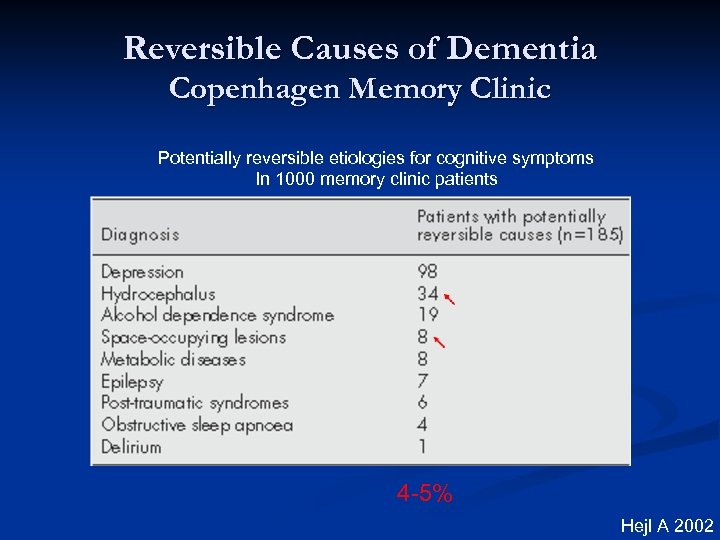 Reversible Causes of Dementia Copenhagen Memory Clinic Potentially reversible etiologies for cognitive symptoms In 1000 memory clinic patients 4 -5% Hejl A 2002
Reversible Causes of Dementia Copenhagen Memory Clinic Potentially reversible etiologies for cognitive symptoms In 1000 memory clinic patients 4 -5% Hejl A 2002
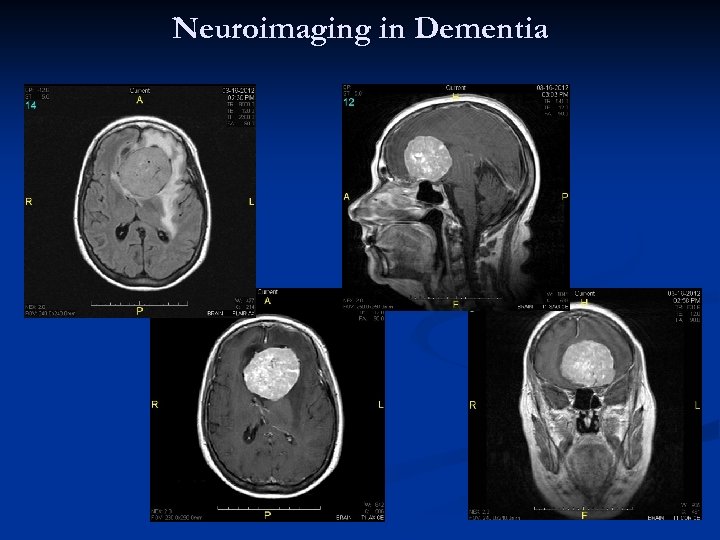 Neuroimaging in Dementia
Neuroimaging in Dementia
 Imaging Modalities Magnetic Resonance Imaging Positron Emission Tomography
Imaging Modalities Magnetic Resonance Imaging Positron Emission Tomography
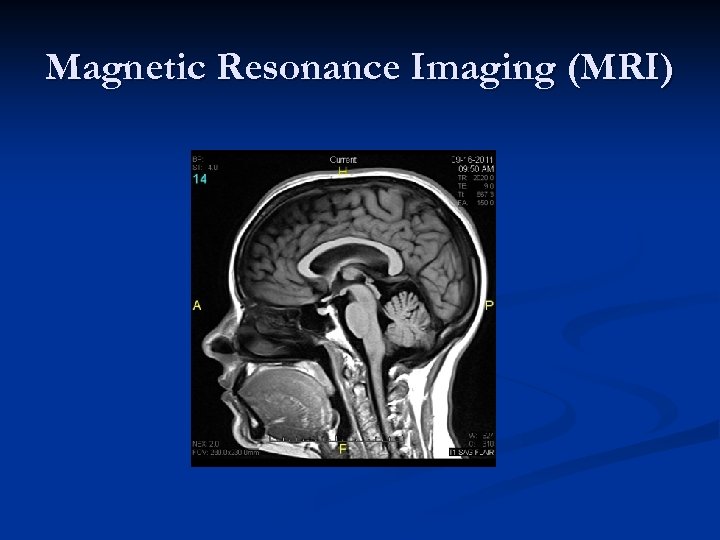 Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI)
 Minimum MRI Sequences for Dementia Evaluation n Multiplanar Imaging n n Multiple Modalities n n T 1 W, T 2 W, FLAIR, DWI Screening for Abnormal Blood Products n n Axial, coronal, sagittal GRE or SWI Contrast-Enhanced (select situations)
Minimum MRI Sequences for Dementia Evaluation n Multiplanar Imaging n n Multiple Modalities n n T 1 W, T 2 W, FLAIR, DWI Screening for Abnormal Blood Products n n Axial, coronal, sagittal GRE or SWI Contrast-Enhanced (select situations)
 Other MR Modalities n Volumetric MRI n CSF flow studies n MR spectroscopy n f. MRI n Diffusion tensor (DTI) n MR perfusion
Other MR Modalities n Volumetric MRI n CSF flow studies n MR spectroscopy n f. MRI n Diffusion tensor (DTI) n MR perfusion
 Other MR Modalities n Volumetric MRI n CSF flow studies n MR spectroscopy n f. MRI n Diffusion tensor (DTI) n MR perfusion Semi-routinely utilized for clinical assessment of dementia
Other MR Modalities n Volumetric MRI n CSF flow studies n MR spectroscopy n f. MRI n Diffusion tensor (DTI) n MR perfusion Semi-routinely utilized for clinical assessment of dementia
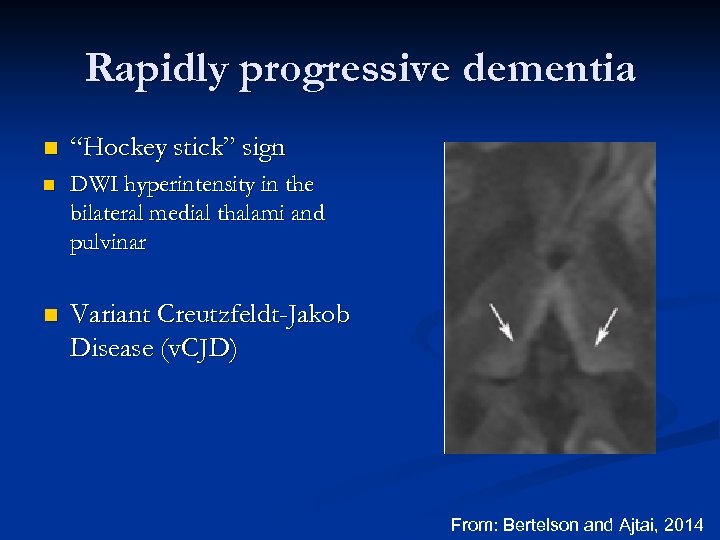 Rapidly progressive dementia n “Hockey stick” sign n DWI hyperintensity in the bilateral medial thalami and pulvinar n Variant Creutzfeldt-Jakob Disease (v. CJD) From: Bertelson and Ajtai, 2014
Rapidly progressive dementia n “Hockey stick” sign n DWI hyperintensity in the bilateral medial thalami and pulvinar n Variant Creutzfeldt-Jakob Disease (v. CJD) From: Bertelson and Ajtai, 2014
 Positron Emission Tomography (PET)
Positron Emission Tomography (PET)
 FDG PET Medicare Coverage Dementia and Neurodegenerative Diseases n Effective 9/15/2004, n “An FDG PET scan is considered reasonable and necessary in patients with: n a recent diagnosis of dementia, n documented cognitive decline of at least 6 months, n meet diagnostic criteria for both AD and FTD. ” http: //www. cms. gov/Regulations-and-Guidance/Manuals/downloads/ncd 103 c 1_Part 4. pdf
FDG PET Medicare Coverage Dementia and Neurodegenerative Diseases n Effective 9/15/2004, n “An FDG PET scan is considered reasonable and necessary in patients with: n a recent diagnosis of dementia, n documented cognitive decline of at least 6 months, n meet diagnostic criteria for both AD and FTD. ” http: //www. cms. gov/Regulations-and-Guidance/Manuals/downloads/ncd 103 c 1_Part 4. pdf
 FDG PET Medicare Coverage Dementia and Neurodegenerative Diseases n Additional prerequisites include: n Comprehensive evaluation already completed, including brain CT or MRI n Evaluation by “a physician experienced in the diagnosis and assessment of dementia” n Evaluation is indeterminate and FDG PET is reasonably expected to clarify the diagnosis between FTD and AD n SPECT or PET have not already been obtained in the past 12 months AND significant clinical changes have occurred
FDG PET Medicare Coverage Dementia and Neurodegenerative Diseases n Additional prerequisites include: n Comprehensive evaluation already completed, including brain CT or MRI n Evaluation by “a physician experienced in the diagnosis and assessment of dementia” n Evaluation is indeterminate and FDG PET is reasonably expected to clarify the diagnosis between FTD and AD n SPECT or PET have not already been obtained in the past 12 months AND significant clinical changes have occurred
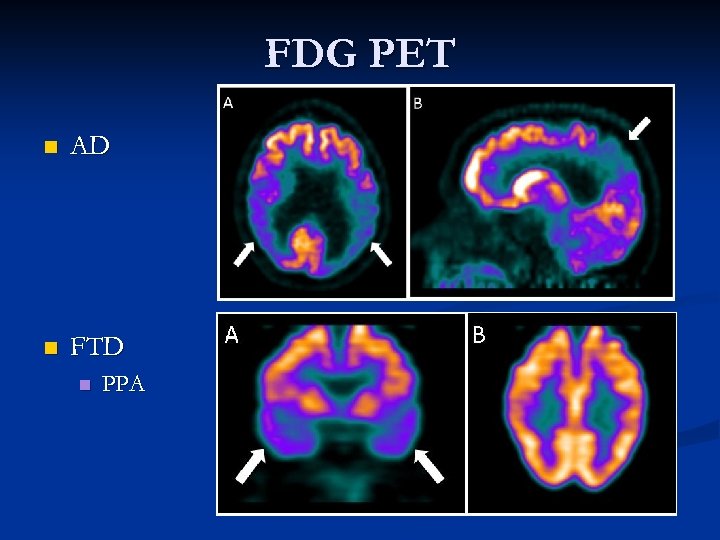 FDG PET n AD n FTD n PPA
FDG PET n AD n FTD n PPA
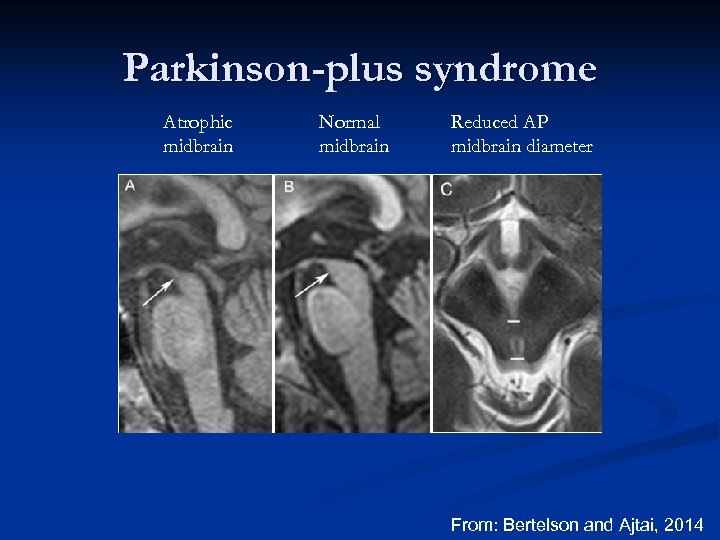 Parkinson-plus syndrome Atrophic midbrain Normal midbrain Reduced AP midbrain diameter From: Bertelson and Ajtai, 2014
Parkinson-plus syndrome Atrophic midbrain Normal midbrain Reduced AP midbrain diameter From: Bertelson and Ajtai, 2014
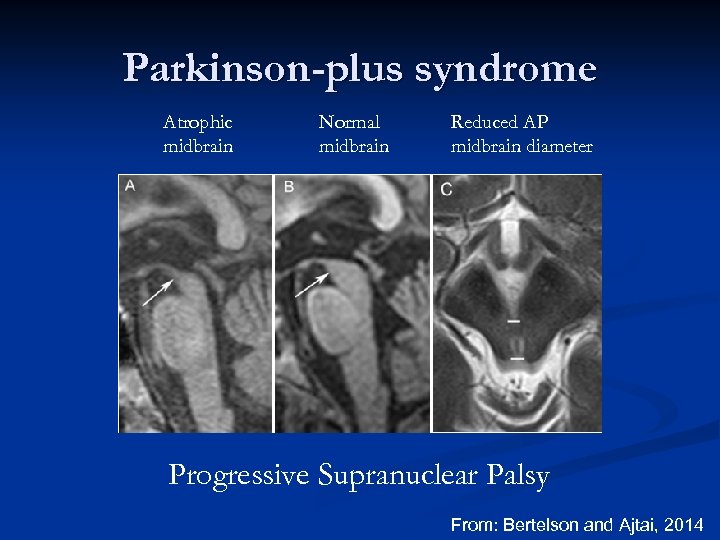 Parkinson-plus syndrome Atrophic midbrain Normal midbrain Reduced AP midbrain diameter Progressive Supranuclear Palsy From: Bertelson and Ajtai, 2014
Parkinson-plus syndrome Atrophic midbrain Normal midbrain Reduced AP midbrain diameter Progressive Supranuclear Palsy From: Bertelson and Ajtai, 2014
 Alzheimer’s Disease (AD)
Alzheimer’s Disease (AD)
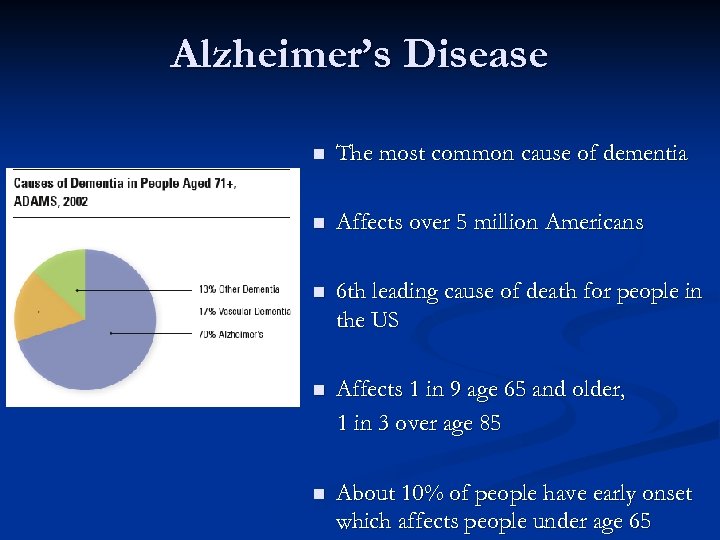 Alzheimer’s Disease n The most common cause of dementia n Affects over 5 million Americans n 6 th leading cause of death for people in the US n Affects 1 in 9 age 65 and older, 1 in 3 over age 85 n About 10% of people have early onset which affects people under age 65
Alzheimer’s Disease n The most common cause of dementia n Affects over 5 million Americans n 6 th leading cause of death for people in the US n Affects 1 in 9 age 65 and older, 1 in 3 over age 85 n About 10% of people have early onset which affects people under age 65
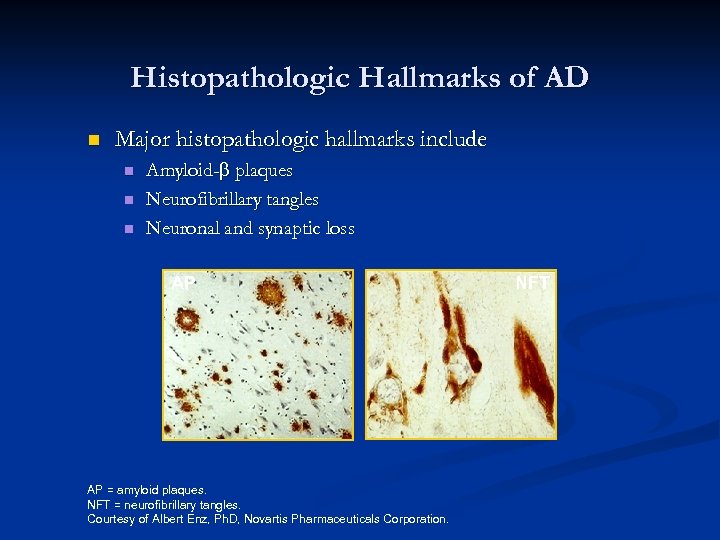 Histopathologic Hallmarks of AD n Major histopathologic hallmarks include n n n Amyloid- plaques Neurofibrillary tangles Neuronal and synaptic loss AP AP = amyloid plaques. NFT = neurofibrillary tangles. Courtesy of Albert Enz, Ph. D, Novartis Pharmaceuticals Corporation. NFT
Histopathologic Hallmarks of AD n Major histopathologic hallmarks include n n n Amyloid- plaques Neurofibrillary tangles Neuronal and synaptic loss AP AP = amyloid plaques. NFT = neurofibrillary tangles. Courtesy of Albert Enz, Ph. D, Novartis Pharmaceuticals Corporation. NFT
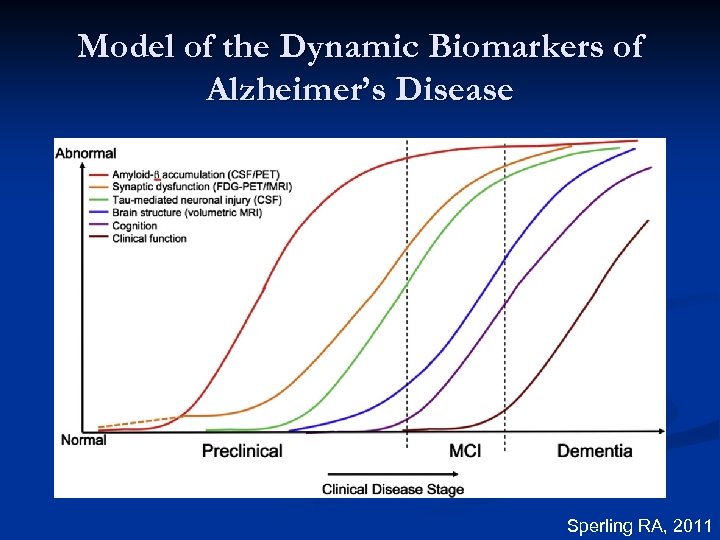 Model of the Dynamic Biomarkers of Alzheimer’s Disease Sperling RA, 2011
Model of the Dynamic Biomarkers of Alzheimer’s Disease Sperling RA, 2011
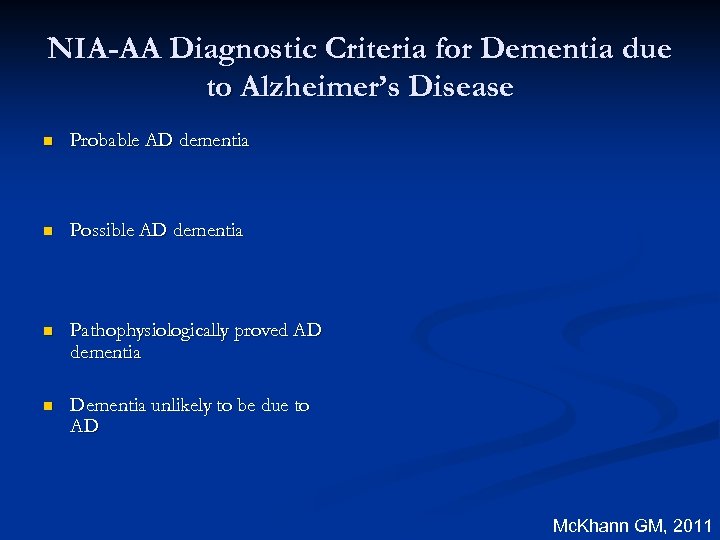 NIA-AA Diagnostic Criteria for Dementia due to Alzheimer’s Disease n Probable AD dementia n Possible AD dementia n Pathophysiologically proved AD dementia n Dementia unlikely to be due to AD Mc. Khann GM, 2011
NIA-AA Diagnostic Criteria for Dementia due to Alzheimer’s Disease n Probable AD dementia n Possible AD dementia n Pathophysiologically proved AD dementia n Dementia unlikely to be due to AD Mc. Khann GM, 2011
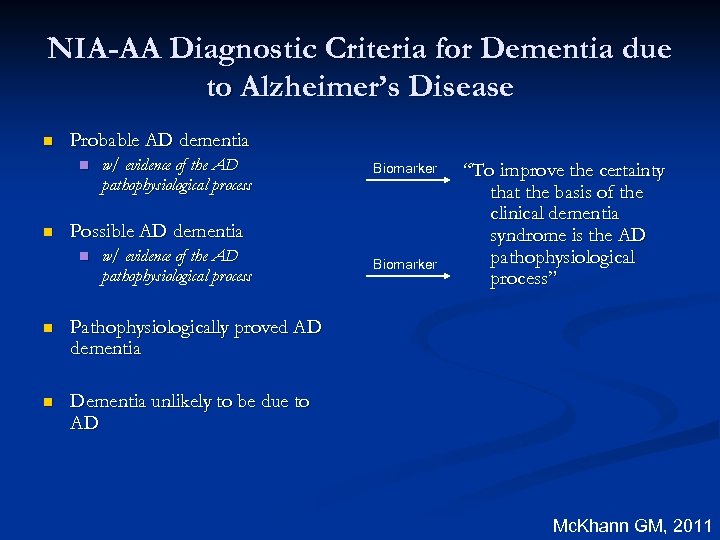 NIA-AA Diagnostic Criteria for Dementia due to Alzheimer’s Disease n Probable AD dementia n n w/ evidence of the AD pathophysiological process Biomarker Possible AD dementia n w/ evidence of the AD pathophysiological process n Pathophysiologically proved AD dementia n Biomarker “To improve the certainty that the basis of the clinical dementia syndrome is the AD pathophysiological process” Dementia unlikely to be due to AD Mc. Khann GM, 2011
NIA-AA Diagnostic Criteria for Dementia due to Alzheimer’s Disease n Probable AD dementia n n w/ evidence of the AD pathophysiological process Biomarker Possible AD dementia n w/ evidence of the AD pathophysiological process n Pathophysiologically proved AD dementia n Biomarker “To improve the certainty that the basis of the clinical dementia syndrome is the AD pathophysiological process” Dementia unlikely to be due to AD Mc. Khann GM, 2011
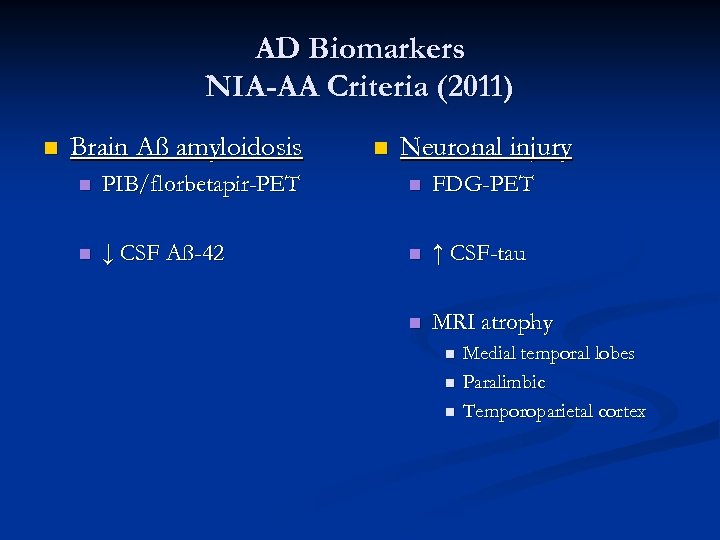 AD Biomarkers NIA-AA Criteria (2011) n Brain Aß amyloidosis n Neuronal injury n PIB/florbetapir-PET n FDG-PET n ↓ CSF Aß-42 n ↑ CSF-tau n MRI atrophy n n n Medial temporal lobes Paralimbic Temporoparietal cortex
AD Biomarkers NIA-AA Criteria (2011) n Brain Aß amyloidosis n Neuronal injury n PIB/florbetapir-PET n FDG-PET n ↓ CSF Aß-42 n ↑ CSF-tau n MRI atrophy n n n Medial temporal lobes Paralimbic Temporoparietal cortex
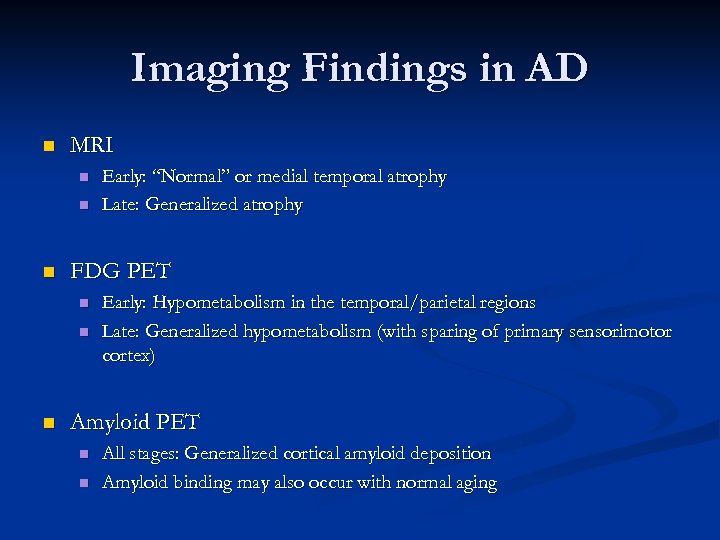 Imaging Findings in AD n MRI n n n FDG PET n n n Early: “Normal” or medial temporal atrophy Late: Generalized atrophy Early: Hypometabolism in the temporal/parietal regions Late: Generalized hypometabolism (with sparing of primary sensorimotor cortex) Amyloid PET n n All stages: Generalized cortical amyloid deposition Amyloid binding may also occur with normal aging
Imaging Findings in AD n MRI n n n FDG PET n n n Early: “Normal” or medial temporal atrophy Late: Generalized atrophy Early: Hypometabolism in the temporal/parietal regions Late: Generalized hypometabolism (with sparing of primary sensorimotor cortex) Amyloid PET n n All stages: Generalized cortical amyloid deposition Amyloid binding may also occur with normal aging
 MRI and AD
MRI and AD
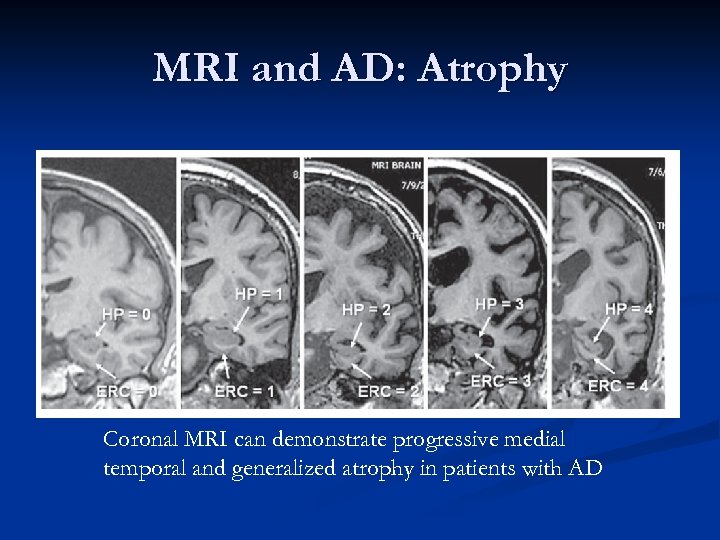 MRI and AD: Atrophy Coronal MRI can demonstrate progressive medial temporal and generalized atrophy in patients with AD
MRI and AD: Atrophy Coronal MRI can demonstrate progressive medial temporal and generalized atrophy in patients with AD
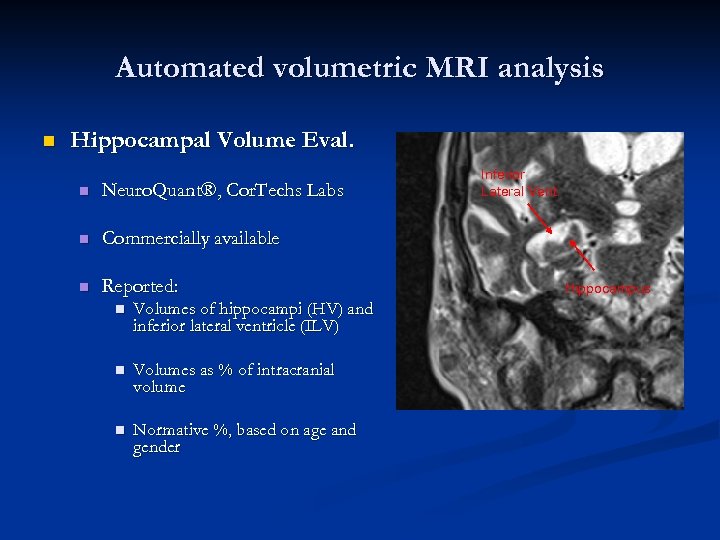 Automated volumetric MRI analysis n Hippocampal Volume Eval. n Neuro. Quant®, Cor. Techs Labs n Commercially available n Reported: Inferior Lateral Vent. n Volumes of hippocampi (HV) and inferior lateral ventricle (ILV) n Volumes as % of intracranial volume n Normative %, based on age and gender Hippocampus
Automated volumetric MRI analysis n Hippocampal Volume Eval. n Neuro. Quant®, Cor. Techs Labs n Commercially available n Reported: Inferior Lateral Vent. n Volumes of hippocampi (HV) and inferior lateral ventricle (ILV) n Volumes as % of intracranial volume n Normative %, based on age and gender Hippocampus
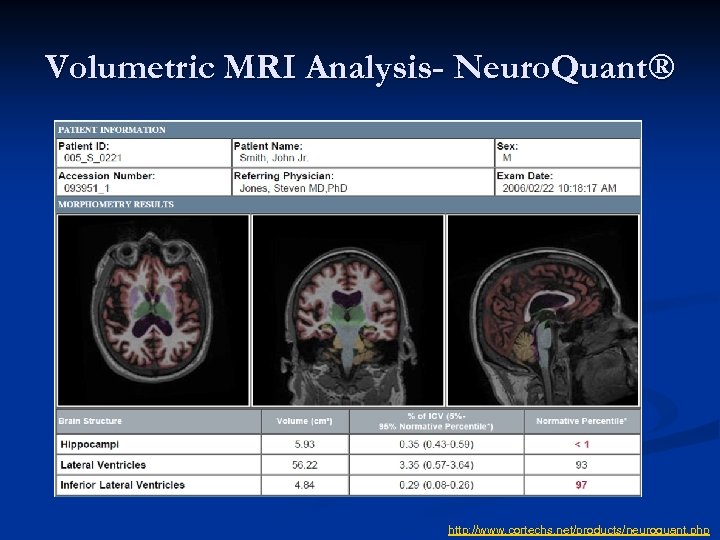 Volumetric MRI Analysis- Neuro. Quant® http: //www. cortechs. net/products/neuroquant. php
Volumetric MRI Analysis- Neuro. Quant® http: //www. cortechs. net/products/neuroquant. php
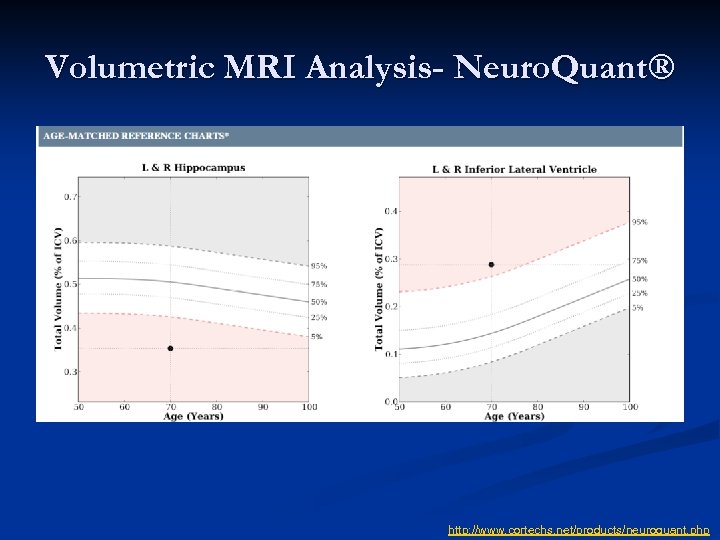 Volumetric MRI Analysis- Neuro. Quant® http: //www. cortechs. net/products/neuroquant. php
Volumetric MRI Analysis- Neuro. Quant® http: //www. cortechs. net/products/neuroquant. php
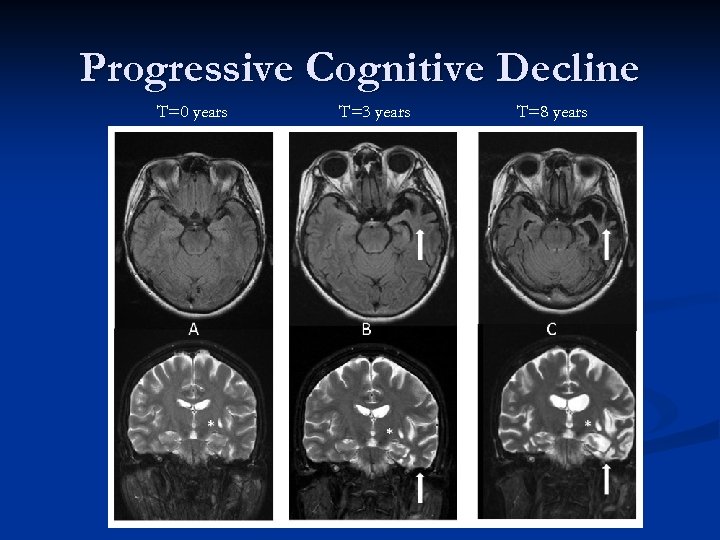 Progressive Cognitive Decline T=0 years T=3 years T=8 years
Progressive Cognitive Decline T=0 years T=3 years T=8 years
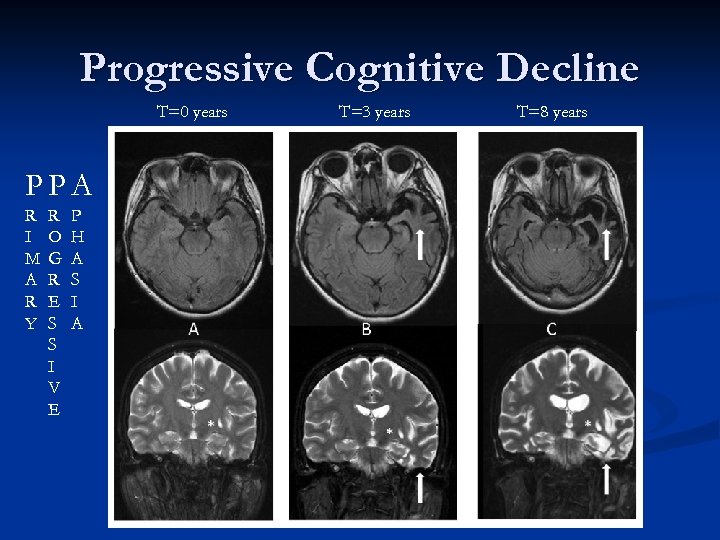 Progressive Cognitive Decline T=0 years PPA R I M A R Y R O G R E S S I V E P H A S I A T=3 years T=8 years
Progressive Cognitive Decline T=0 years PPA R I M A R Y R O G R E S S I V E P H A S I A T=3 years T=8 years
 “PET” and Dementia n FDG PET n Amyloid PET
“PET” and Dementia n FDG PET n Amyloid PET
![FDG PET in AD Profoundly diminished [18 F]FDG uptake in the temporoparietal and parietal FDG PET in AD Profoundly diminished [18 F]FDG uptake in the temporoparietal and parietal](https://present5.com/presentation/c0280486cee6bc2e29441b8bdeb73baf/image-41.jpg) FDG PET in AD Profoundly diminished [18 F]FDG uptake in the temporoparietal and parietal regions bilaterally (arrows), seen on (A) axial and (B) parasagittal images From: Bertelson and Ajtai, 2014
FDG PET in AD Profoundly diminished [18 F]FDG uptake in the temporoparietal and parietal regions bilaterally (arrows), seen on (A) axial and (B) parasagittal images From: Bertelson and Ajtai, 2014
![Amyloid Imaging: Pittsburgh Compound-B PET T 1 W-MRI Pittsburgh Compound-B (PIB) n [N-methyl-(11)C]2 -(4’methylaminophenyl)-6 Amyloid Imaging: Pittsburgh Compound-B PET T 1 W-MRI Pittsburgh Compound-B (PIB) n [N-methyl-(11)C]2 -(4’methylaminophenyl)-6](https://present5.com/presentation/c0280486cee6bc2e29441b8bdeb73baf/image-42.jpg) Amyloid Imaging: Pittsburgh Compound-B PET T 1 W-MRI Pittsburgh Compound-B (PIB) n [N-methyl-(11)C]2 -(4’methylaminophenyl)-6 hydroxybenzothiazole n Selectively binds to amyloid plaque and cerebrovascular amyloid n Significant retention seen in: n n Control Radiolabeled thioflavin derivative AD n PIB- PET 90+% AD patients 60% patients with MCI 30% “normal” elderly Very short half life: 20 minutes Mathis J Med Chem 2003; 46(13) Applied Neurology, Nov. 2005 (suppl) Mosconi J Alzheimer’s Dis 2010
Amyloid Imaging: Pittsburgh Compound-B PET T 1 W-MRI Pittsburgh Compound-B (PIB) n [N-methyl-(11)C]2 -(4’methylaminophenyl)-6 hydroxybenzothiazole n Selectively binds to amyloid plaque and cerebrovascular amyloid n Significant retention seen in: n n Control Radiolabeled thioflavin derivative AD n PIB- PET 90+% AD patients 60% patients with MCI 30% “normal” elderly Very short half life: 20 minutes Mathis J Med Chem 2003; 46(13) Applied Neurology, Nov. 2005 (suppl) Mosconi J Alzheimer’s Dis 2010
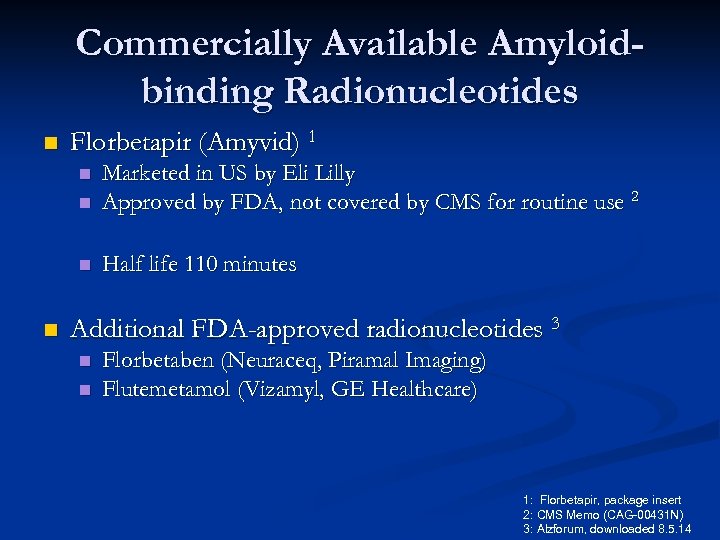 Commercially Available Amyloidbinding Radionucleotides n Florbetapir (Amyvid) 1 n Marketed in US by Eli Lilly Approved by FDA, not covered by CMS for routine use 2 n Half life 110 minutes n n Additional FDA-approved radionucleotides 3 n n Florbetaben (Neuraceq, Piramal Imaging) Flutemetamol (Vizamyl, GE Healthcare) 1: Florbetapir, package insert 2: CMS Memo (CAG-00431 N) 3: Alzforum, downloaded 8. 5. 14
Commercially Available Amyloidbinding Radionucleotides n Florbetapir (Amyvid) 1 n Marketed in US by Eli Lilly Approved by FDA, not covered by CMS for routine use 2 n Half life 110 minutes n n Additional FDA-approved radionucleotides 3 n n Florbetaben (Neuraceq, Piramal Imaging) Flutemetamol (Vizamyl, GE Healthcare) 1: Florbetapir, package insert 2: CMS Memo (CAG-00431 N) 3: Alzforum, downloaded 8. 5. 14
 But… Aẞ burden as assessed by positron emission tomography(PET) does not strongly correlate with cognitive impairment in AD patients
But… Aẞ burden as assessed by positron emission tomography(PET) does not strongly correlate with cognitive impairment in AD patients
 Tau Imaging n Human postmortem studies have shown that it is the density of NFTs and not of Aẞ insoluble plaques that strongly correlates with neurodegeneration and cognitive deficits. Villemagne 2014
Tau Imaging n Human postmortem studies have shown that it is the density of NFTs and not of Aẞ insoluble plaques that strongly correlates with neurodegeneration and cognitive deficits. Villemagne 2014
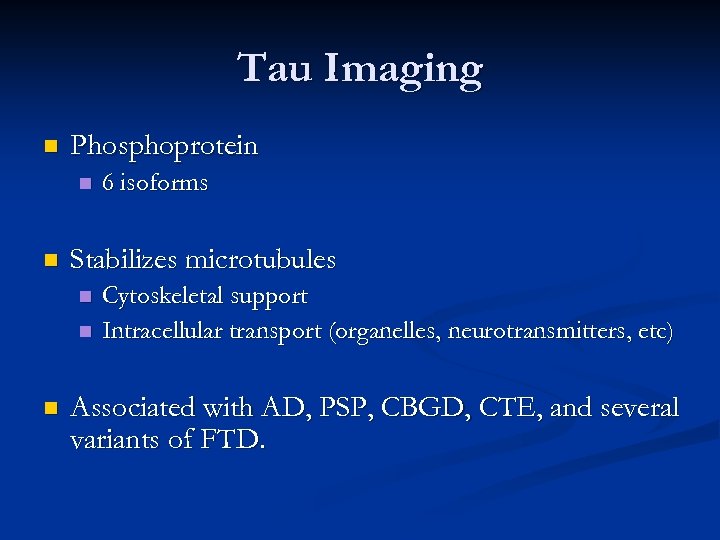 Tau Imaging n Phosphoprotein n n Stabilizes microtubules n n n 6 isoforms Cytoskeletal support Intracellular transport (organelles, neurotransmitters, etc) Associated with AD, PSP, CBGD, CTE, and several variants of FTD.
Tau Imaging n Phosphoprotein n n Stabilizes microtubules n n n 6 isoforms Cytoskeletal support Intracellular transport (organelles, neurotransmitters, etc) Associated with AD, PSP, CBGD, CTE, and several variants of FTD.
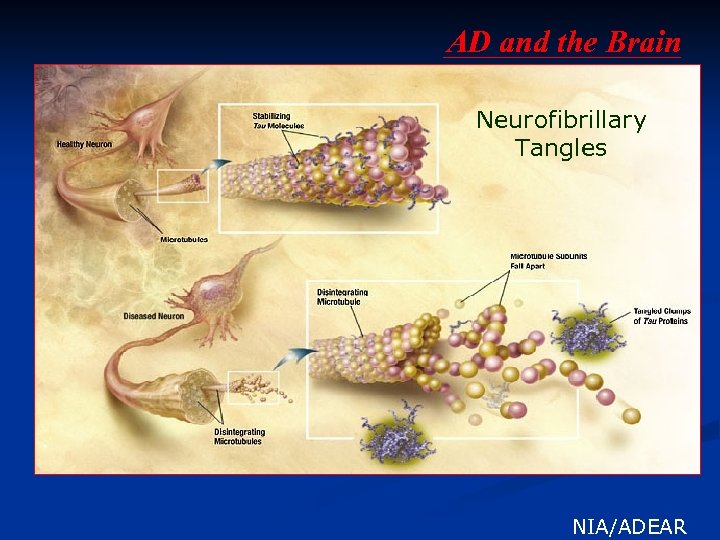 AD and the Brain Neurofibrillary Tangles . NIA/ADEAR
AD and the Brain Neurofibrillary Tangles . NIA/ADEAR
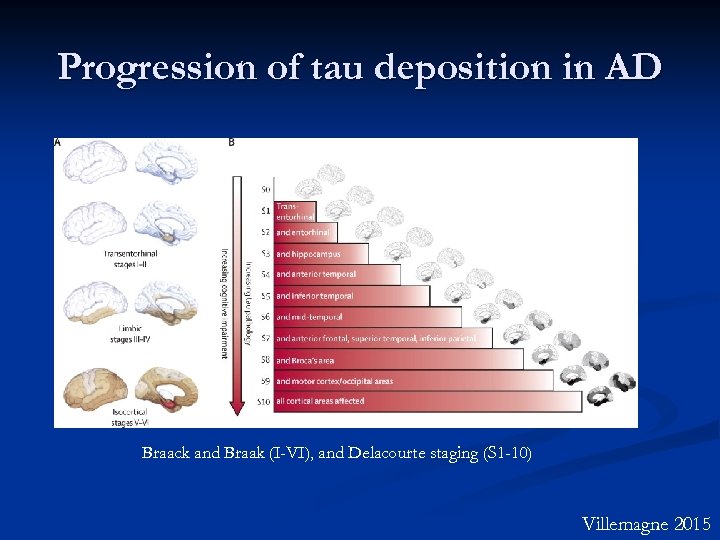 Progression of tau deposition in AD Braack and Braak (I-VI), and Delacourte staging (S 1 -10) Villemagne 2015
Progression of tau deposition in AD Braack and Braak (I-VI), and Delacourte staging (S 1 -10) Villemagne 2015
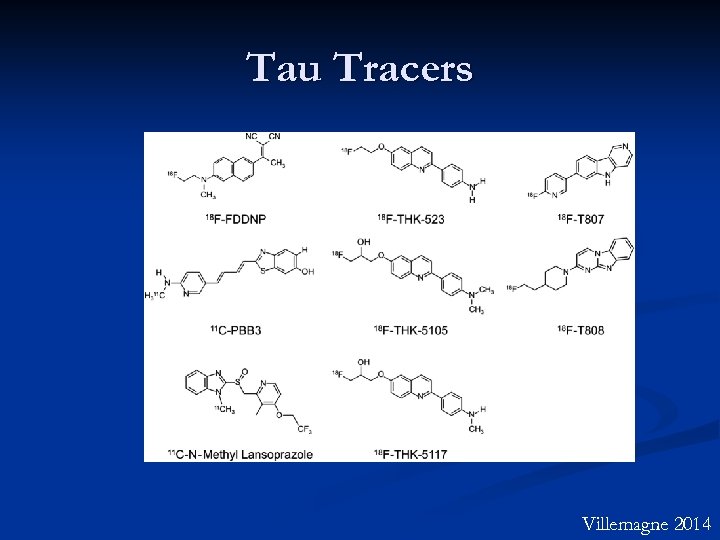 Tau Tracers Villemagne 2014
Tau Tracers Villemagne 2014
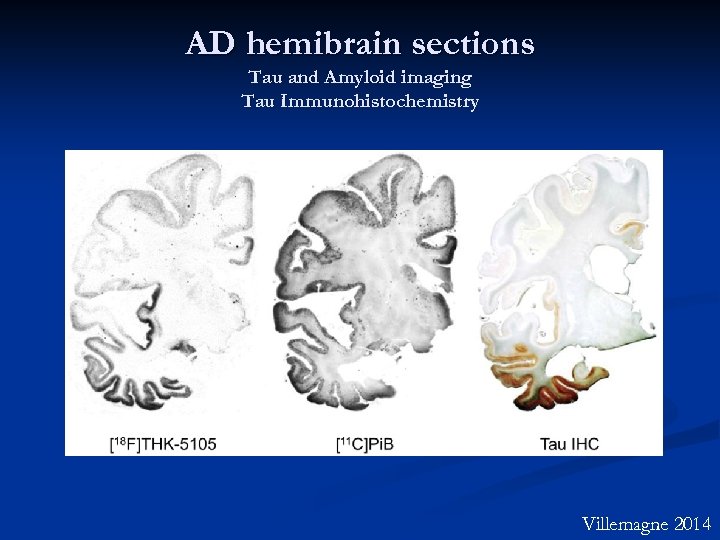 AD hemibrain sections Tau and Amyloid imaging Tau Immunohistochemistry Villemagne 2014
AD hemibrain sections Tau and Amyloid imaging Tau Immunohistochemistry Villemagne 2014
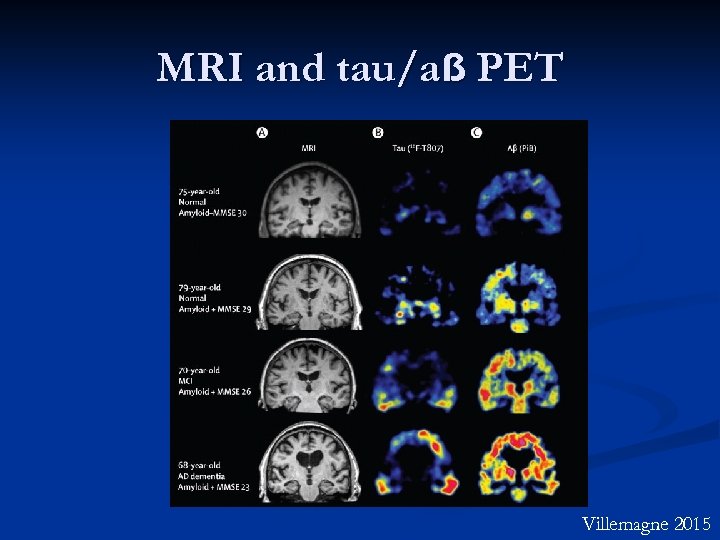 MRI and tau/aẞ PET Villemagne 2015
MRI and tau/aẞ PET Villemagne 2015
 Other Degenerative Dementias Frontotemporal dementia (FTD) n Vascular dementia (VAD) n Chronic traumatic encephalopathy (CTE) n Lewy Body dementia (LBD) n Parkinson’s disease dementia (PDD) n Etc n
Other Degenerative Dementias Frontotemporal dementia (FTD) n Vascular dementia (VAD) n Chronic traumatic encephalopathy (CTE) n Lewy Body dementia (LBD) n Parkinson’s disease dementia (PDD) n Etc n
 What’s next? ? n Wider utilization of biomarkers to: n n Clarify the diagnosis Monitor response to disease modifying agents n Greater implementation of multimodal imaging n Limitations n n n Cost Access to advanced imaging Inadequacy of response to disease modifying agents
What’s next? ? n Wider utilization of biomarkers to: n n Clarify the diagnosis Monitor response to disease modifying agents n Greater implementation of multimodal imaging n Limitations n n n Cost Access to advanced imaging Inadequacy of response to disease modifying agents
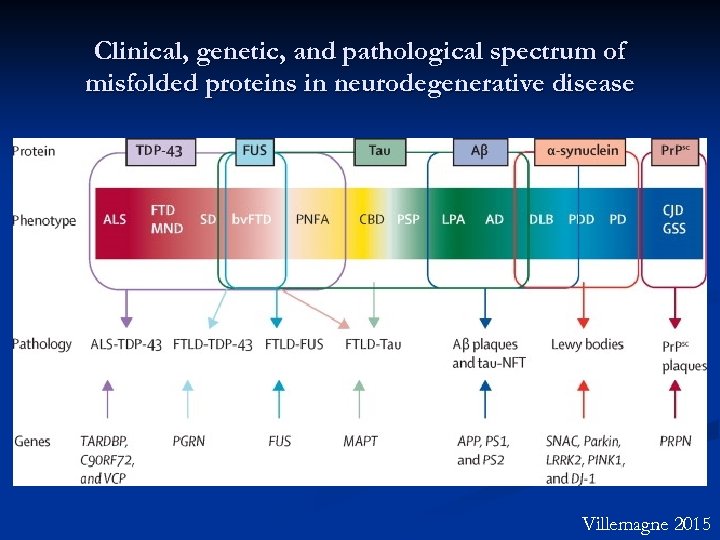 Clinical, genetic, and pathological spectrum of misfolded proteins in neurodegenerative disease Villemagne 2015
Clinical, genetic, and pathological spectrum of misfolded proteins in neurodegenerative disease Villemagne 2015
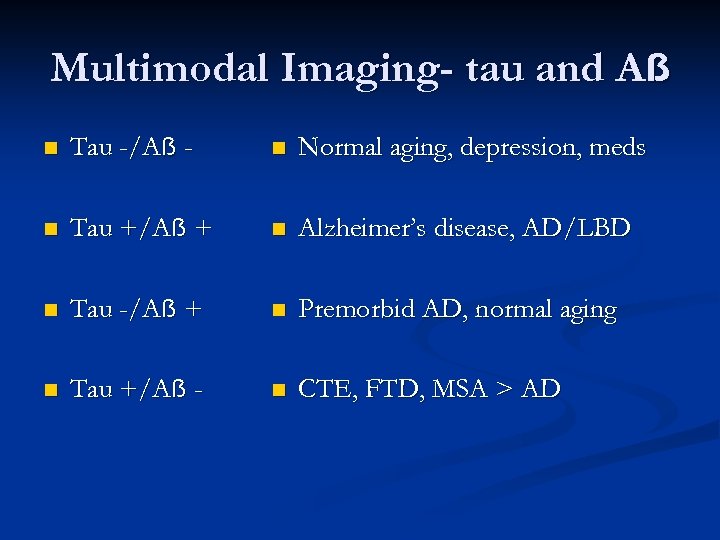 Multimodal Imaging- tau and Aẞ n Tau -/Aẞ - n Normal aging, depression, meds n Tau +/Aẞ + n Alzheimer’s disease, AD/LBD n Tau -/Aẞ + n Premorbid AD, normal aging n Tau +/Aẞ - n CTE, FTD, MSA > AD
Multimodal Imaging- tau and Aẞ n Tau -/Aẞ - n Normal aging, depression, meds n Tau +/Aẞ + n Alzheimer’s disease, AD/LBD n Tau -/Aẞ + n Premorbid AD, normal aging n Tau +/Aẞ - n CTE, FTD, MSA > AD
 What should I do today? ? ? n I want to work up a patient with cognitive symptoms. What imaging modality should I order? n “I'm sorry, my responses are limited. You must ask the right question. ” n n Hologram of Dr. Lanning (James Cromwell) to Det. Spooner (Will Smith): From: I, Robot n n Film released by 20 th Century Fox in 2004 Based on a series of short stories by Isaac Asimov
What should I do today? ? ? n I want to work up a patient with cognitive symptoms. What imaging modality should I order? n “I'm sorry, my responses are limited. You must ask the right question. ” n n Hologram of Dr. Lanning (James Cromwell) to Det. Spooner (Will Smith): From: I, Robot n n Film released by 20 th Century Fox in 2004 Based on a series of short stories by Isaac Asimov
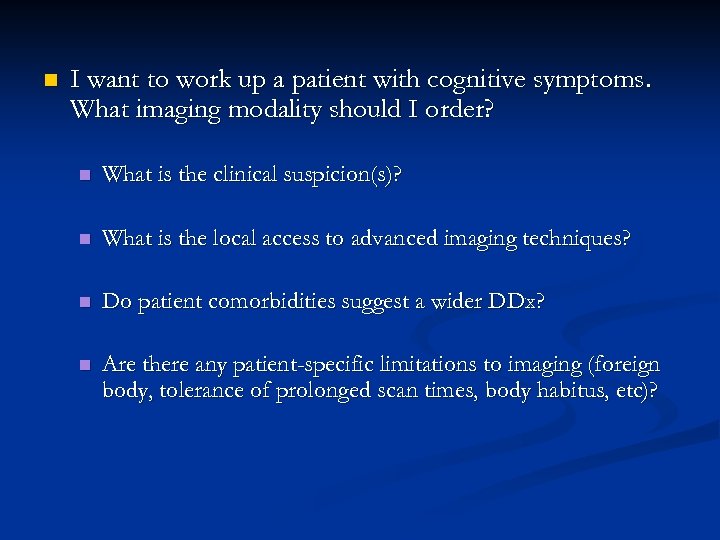 n I want to work up a patient with cognitive symptoms. What imaging modality should I order? n What is the clinical suspicion(s)? n What is the local access to advanced imaging techniques? n Do patient comorbidities suggest a wider DDx? n Are there any patient-specific limitations to imaging (foreign body, tolerance of prolonged scan times, body habitus, etc)?
n I want to work up a patient with cognitive symptoms. What imaging modality should I order? n What is the clinical suspicion(s)? n What is the local access to advanced imaging techniques? n Do patient comorbidities suggest a wider DDx? n Are there any patient-specific limitations to imaging (foreign body, tolerance of prolonged scan times, body habitus, etc)?
 n “That, detective, is the right question” n Dr. Lanning to Det. Spooner n From: I, Robot Thank You
n “That, detective, is the right question” n Dr. Lanning to Det. Spooner n From: I, Robot Thank You
 References n Villemagne, VL et al. Tau imaging: early progress and future directions. Lancet Neurology 14 : 1(2015) 114 -24. n Villemagne VL and Okamura N. In vivo tau imaging: Obstacles and progress. Alzheimer’s and Dementia 10(2014) S 254 -64.
References n Villemagne, VL et al. Tau imaging: early progress and future directions. Lancet Neurology 14 : 1(2015) 114 -24. n Villemagne VL and Okamura N. In vivo tau imaging: Obstacles and progress. Alzheimer’s and Dementia 10(2014) S 254 -64.
 References n Alter, M et al (Quality Standards Subcommittee of the AAN). Practice parameter for diagnosis and evaluation of dementia. Neurology 1994; 44: 2203 -6. n Knopman DS et al. Practice Parameter: diagnosis of dementia (an evidence-based review). Neurology 2001; 56: 1143 -53. n Kalkonde YV et al. Difference between clinical subspecialties in the outpatient evaluation and treatment of dementia in an academic medical center. Dement Geriatr Cogn Disord 2010; 29: 38 -36. n Hejl A et al. Potentially reversible conditions in 1000 consecutive memory clinic patients. J Neurosurg Psychiatry 2002; 73(4): 390 -4. n Jack CR Jr, Albert M, Knopman D, Mc. Khann G, Sperling R, Carrillo M, et al. Introduction to the revised criteria for the diagnosis of Alzheimer’s disease: National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 25762. n Mc. Khann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 263 -69. n Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. Towards defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 280 -92. n Albert M, De. Kosky ST, Dickson D, Dubois B, Feldman H, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: report of the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 270 -9.
References n Alter, M et al (Quality Standards Subcommittee of the AAN). Practice parameter for diagnosis and evaluation of dementia. Neurology 1994; 44: 2203 -6. n Knopman DS et al. Practice Parameter: diagnosis of dementia (an evidence-based review). Neurology 2001; 56: 1143 -53. n Kalkonde YV et al. Difference between clinical subspecialties in the outpatient evaluation and treatment of dementia in an academic medical center. Dement Geriatr Cogn Disord 2010; 29: 38 -36. n Hejl A et al. Potentially reversible conditions in 1000 consecutive memory clinic patients. J Neurosurg Psychiatry 2002; 73(4): 390 -4. n Jack CR Jr, Albert M, Knopman D, Mc. Khann G, Sperling R, Carrillo M, et al. Introduction to the revised criteria for the diagnosis of Alzheimer’s disease: National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 25762. n Mc. Khann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 263 -69. n Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. Towards defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 280 -92. n Albert M, De. Kosky ST, Dickson D, Dubois B, Feldman H, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: report of the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement 2011; 7: 270 -9.
 References n Borghesani PR et al. Neuroimaging in the clinical diagnosis of dementia: observations from a memory disorders clinic. Journal of the American Geriatrics Society 2010; 58(8): 1453 -8. n Heister D et al. Predicting MCI outcome with clinically available MRI and CSF biomarkers. Neurology 2011; 77: 1619 -28. n Dickerson BC et al. Alzheimer-signature MRI biomarker predicts AD dementia in cognitively normal adults. Neurology 2011; 76: 1395 -402. n Dickerson BC et al. MRI cortical thickness biomarker predicts AD-like CSF and cognitive decline in normal adults. Neurology 2012; 78: 84 -90. n Petersen RC. New clinical criteria for the Alzheimer’s Disease Spectrum. Minnesota Medicine 2012. n Price DL et al. “Investigation of acoustic noise on 15 MRI scanners from 0. 2 T to 3 T. ” J Magn Reson Imaging 2001; 13(2): 288 -93.
References n Borghesani PR et al. Neuroimaging in the clinical diagnosis of dementia: observations from a memory disorders clinic. Journal of the American Geriatrics Society 2010; 58(8): 1453 -8. n Heister D et al. Predicting MCI outcome with clinically available MRI and CSF biomarkers. Neurology 2011; 77: 1619 -28. n Dickerson BC et al. Alzheimer-signature MRI biomarker predicts AD dementia in cognitively normal adults. Neurology 2011; 76: 1395 -402. n Dickerson BC et al. MRI cortical thickness biomarker predicts AD-like CSF and cognitive decline in normal adults. Neurology 2012; 78: 84 -90. n Petersen RC. New clinical criteria for the Alzheimer’s Disease Spectrum. Minnesota Medicine 2012. n Price DL et al. “Investigation of acoustic noise on 15 MRI scanners from 0. 2 T to 3 T. ” J Magn Reson Imaging 2001; 13(2): 288 -93.
 References n Rabinovici GD, Rosen HJ, etal. Amyloid vs. FDG-PET in the differential diagnosis of AD and FTLD. Neurology 2011; 77: 203442. n Suárez J et al. Characterizing radiology reports in patients with frontotemporal dementia. Neurology 2009; 73(13): 1073 -4. n Kerholz K et al. “Positron emission tomography imaging in dementia. ” British Journal of Radiology 2007; 80: S 160 -7. n Mosconi L et al. “Pre-clinical detection of Alzheimer’s disease using FDG-PET with or without amyloid imaging. ” J Alzheimers Dis. 2010; 20(3): 843 -54. n Laino C Two radioactive tracers detect amyloid, may aid in AD diagnosis. Neurology Today 2012; 12(10): 16 -7. n Li TQ and Wahlund LO. The search for neuroimaging biomarkers of Alzheimer's disease with advanced MRI techniques. Acta Radiologica. 2011; Vol. 52 (2): 211 -22. n Gorno-Tempini ML et al. “Classification of primary progressive aphasia and its variants. ” Neurology 2011; 76: 1006 -14. n Snowden JS et al. Distinct behavioural profiles in frontotemporal dementia and semantic dementia. J Neurol Neurosurg Psychiatry 2001; 70: 323 -32.
References n Rabinovici GD, Rosen HJ, etal. Amyloid vs. FDG-PET in the differential diagnosis of AD and FTLD. Neurology 2011; 77: 203442. n Suárez J et al. Characterizing radiology reports in patients with frontotemporal dementia. Neurology 2009; 73(13): 1073 -4. n Kerholz K et al. “Positron emission tomography imaging in dementia. ” British Journal of Radiology 2007; 80: S 160 -7. n Mosconi L et al. “Pre-clinical detection of Alzheimer’s disease using FDG-PET with or without amyloid imaging. ” J Alzheimers Dis. 2010; 20(3): 843 -54. n Laino C Two radioactive tracers detect amyloid, may aid in AD diagnosis. Neurology Today 2012; 12(10): 16 -7. n Li TQ and Wahlund LO. The search for neuroimaging biomarkers of Alzheimer's disease with advanced MRI techniques. Acta Radiologica. 2011; Vol. 52 (2): 211 -22. n Gorno-Tempini ML et al. “Classification of primary progressive aphasia and its variants. ” Neurology 2011; 76: 1006 -14. n Snowden JS et al. Distinct behavioural profiles in frontotemporal dementia and semantic dementia. J Neurol Neurosurg Psychiatry 2001; 70: 323 -32.


