57c82d80013111c4d2045f80beb8aa38.ppt
- Количество слайдов: 56
Imaging bone density Gerrit Engelbrecht
Definitions Osteopenia Poverty of bone Decreased quality or quantity of bone Radiologically identified as radiolucency Causes Diffuse Regional osteopenia Osteosclerosis Increased density of bone
Diffuse osteopenia Osteoporosis osteomalacia hyperparathyroidism multiple myeloma diffuse metastases drugs, mastocytosis osteogenesis imperfecta
Regional osteopenia Disuse osteoporosis / atrophy Etiology: local immobilization secondary to (a) fracture (more pronounced distal to fracture site) (b) neural paralysis (c) muscular paralysis Reflex sympathetic dystrophy = Sudeck dystrophy Regional migratory osteoporosis, transient regional osteoporosis of hip Rheumatologic disorders Infection: osteomyelitis, tuberculosis Osteolytic tumor Lytic phase of Paget disease Early phase of bone infarct and hemorrhage Burns + frostbite
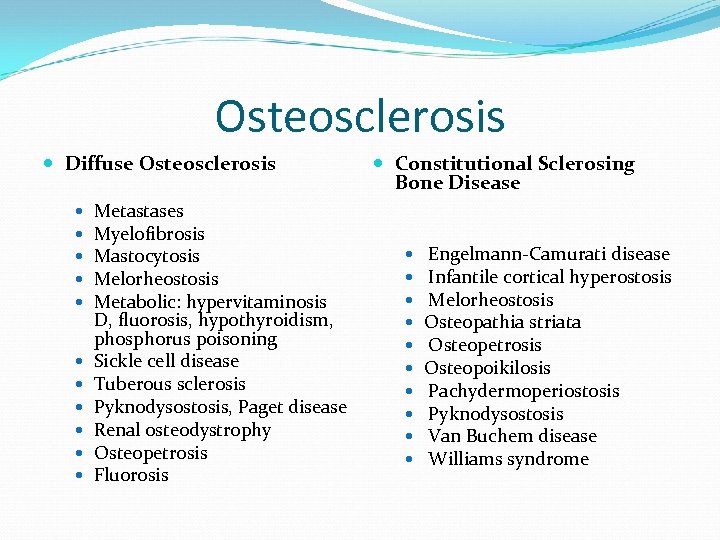
Osteosclerosis Diffuse Osteosclerosis Metastases Myelofibrosis Mastocytosis Melorheostosis Metabolic: hypervitaminosis D, fluorosis, hypothyroidism, phosphorus poisoning Sickle cell disease Tuberous sclerosis Pyknodysostosis, Paget disease Renal osteodystrophy Osteopetrosis Fluorosis Constitutional Sclerosing Bone Disease Engelmann-Camurati disease Infantile cortical hyperostosis Melorheostosis Osteopathia striata Osteopetrosis Osteopoikilosis Pachydermoperiostosis Pyknodysostosis Van Buchem disease Williams syndrome
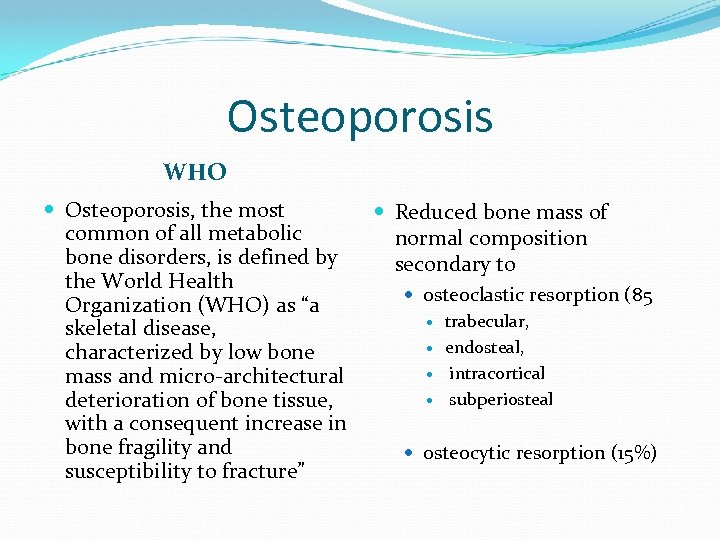
Osteoporosis WHO Osteoporosis, the most common of all metabolic bone disorders, is defined by the World Health Organization (WHO) as “a skeletal disease, characterized by low bone mass and micro-architectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture” Reduced bone mass of normal composition secondary to osteoclastic resorption (85 trabecular, endosteal, intracortical subperiosteal osteocytic resorption (15%)
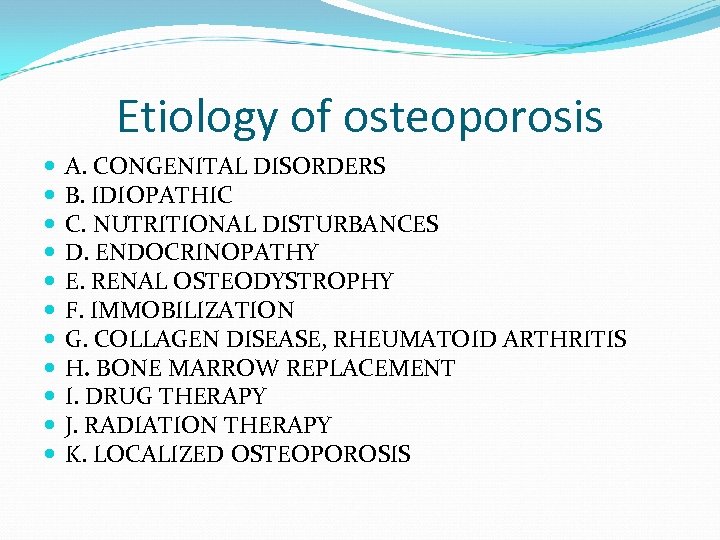
Etiology of osteoporosis A. CONGENITAL DISORDERS B. IDIOPATHIC C. NUTRITIONAL DISTURBANCES D. ENDOCRINOPATHY E. RENAL OSTEODYSTROPHY F. IMMOBILIZATION G. COLLAGEN DISEASE, RHEUMATOID ARTHRITIS H. BONE MARROW REPLACEMENT I. DRUG THERAPY J. RADIATION THERAPY K. LOCALIZED OSTEOPOROSIS
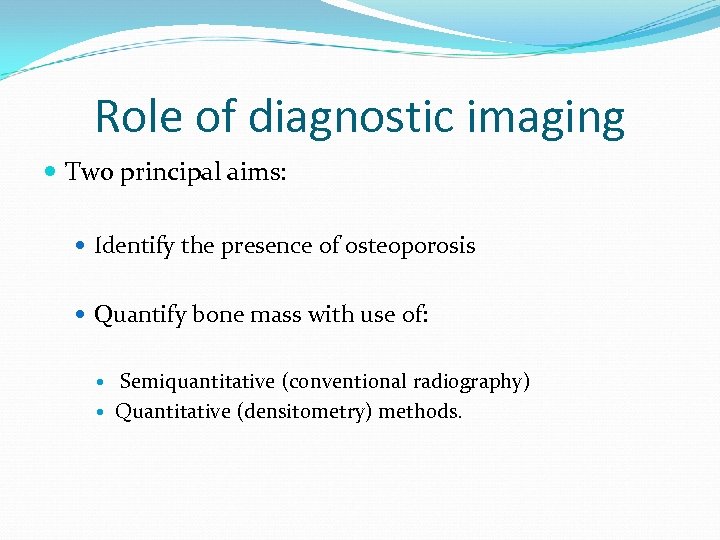
Role of diagnostic imaging Two principal aims: Identify the presence of osteoporosis Quantify bone mass with use of: Semiquantitative (conventional radiography) Quantitative (densitometry) methods.
Conventional radiography Radiologic appearance stay the same whatever the cause. Most common modality to diagnose osteoporosis Drawback: Start picking up bone loss at 30 % and more
Generalized osteoporosis Increased radiolucency Cause: resorption and thinning of trabeculae Trabeculae respond faster to metabolic bone changes Prominent Axial skeleton Ends of long bones Cortical thinning Cause: osseous resorption Endosteal Intracortical Scalloping Longitudinal striations( cortical tunneling ) Periosteal Irregular definition of the outer bone surface(Most specific for high bone turnover)
Osteoporosis in the axial skeleton Picture framing ( loss of the trabeculae in relation to cortex ) Loss of horizontal trabeculae Compression fractures Usually lumbothoracic junction Number Degree Wedge ( anterior height reduce > 4 mm : posterior height ) Endplate ( midheight : posterior height ) Crush ( all the heights in relation to neighbouring vertebrae)
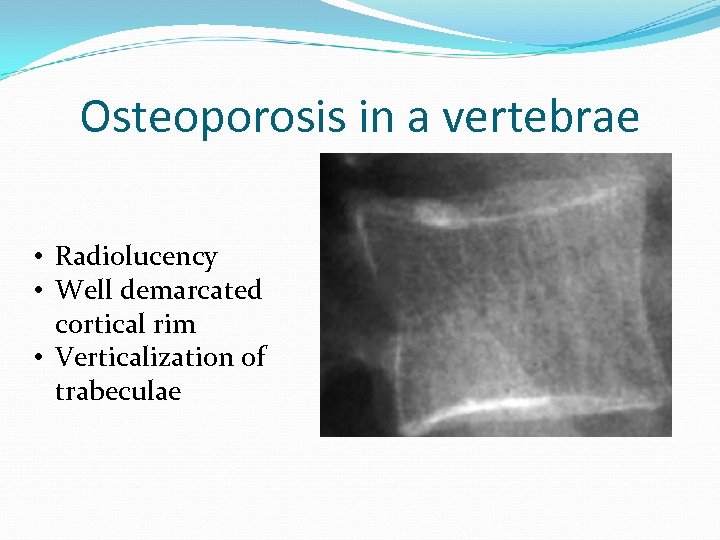
Osteoporosis in a vertebrae • Radiolucency • Well demarcated cortical rim • Verticalization of trabeculae

Saville index
Genant fracture definition Vertebral deformity between T 4 and L 4 Height loss > 20 % Area reduction 10 -20 %
Genant scoring system Severity index of vertebral fractures Grades: Grade 0: No fracture Grade 1: Mild fracture ( 20 -25 %reduction in height compared to neighbouring vertebrae ) Grade 2: Moderate fracture ( 25 -40 % reduction ) Grade 3: Severe fracture ( > 40 % ) Index = Sum Grades/ Number of vertebrae
Point to remember Isolated fractures above the T 7 level are rare in osteoporosis and should alert clinicians to a cause other than osteoporosis
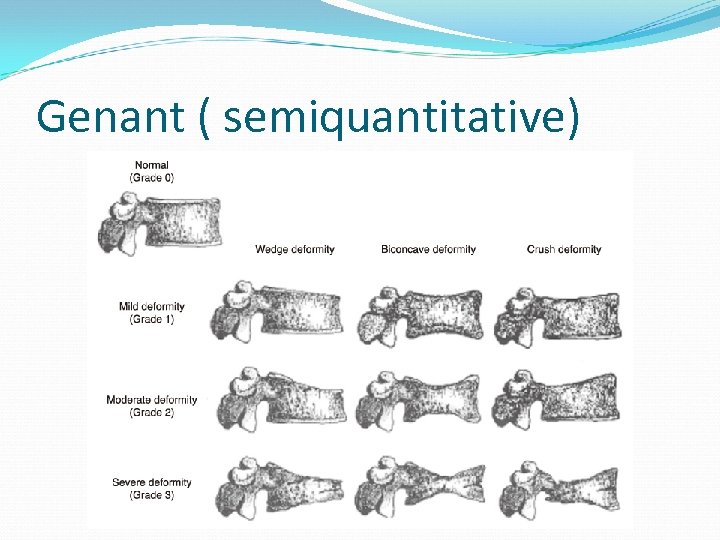
Genant ( semiquantitative)
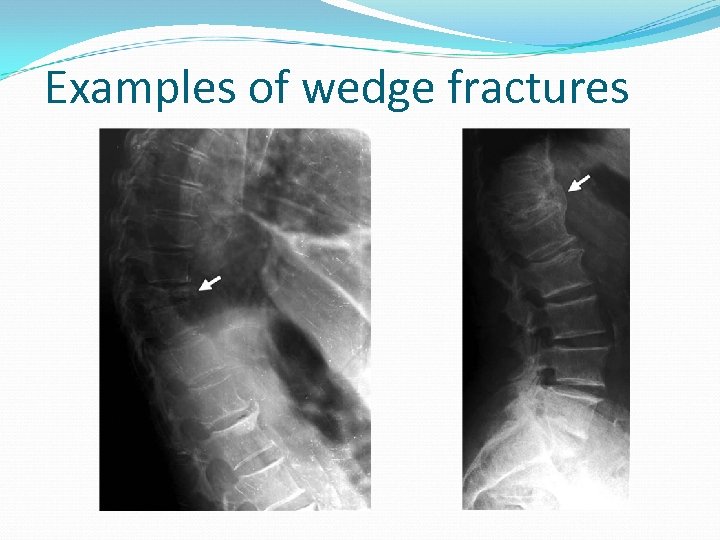
Examples of wedge fractures
Appendicular skeleton Changes first apparent : Ends of long and tubular bones Main sites: Hand Proximal femur Calcaneus
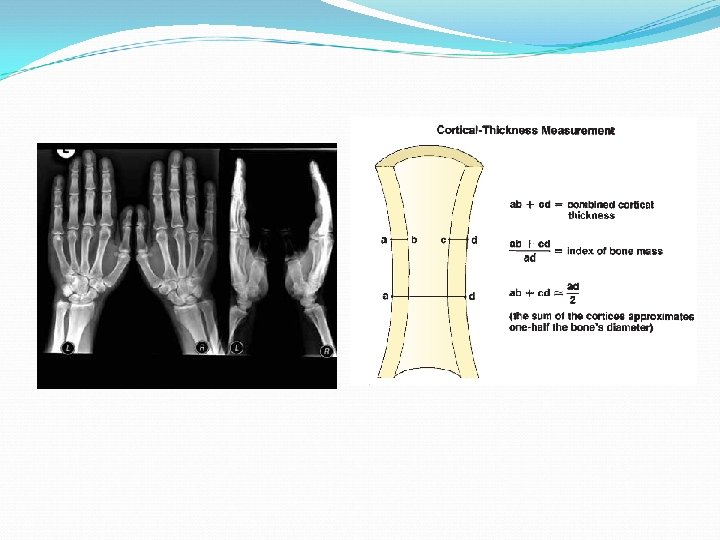
Hand Metacarpal bones ( second, third and fourth ) Corticomedullar index Second metacarpal ( accurate) Longest established quantitative methods ( > 70 years) Automated ( digital x-ray radiogrammetry)-2001 Converted to BMD High reproducibility Capacity to help predict future fracture Potential to provide a simple, widely available, and inexpensive method of assessing patients who are at risk for osteopenia or osteoporosis and might appropriately be referred for central DXA
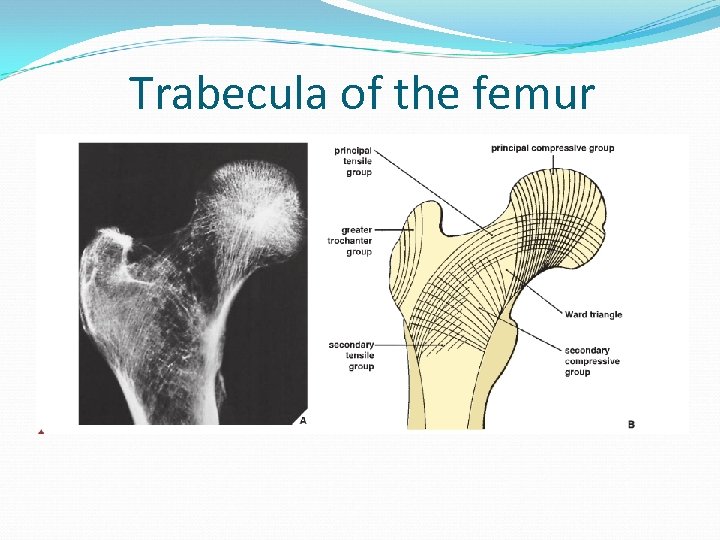
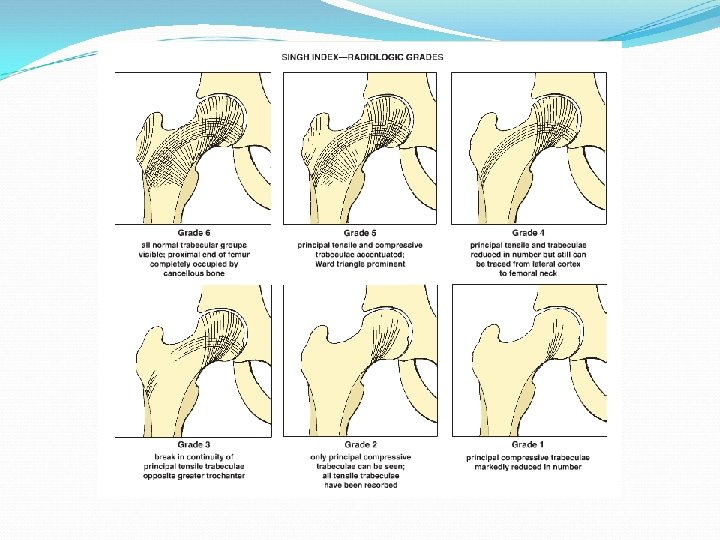
Trabecula of the femur
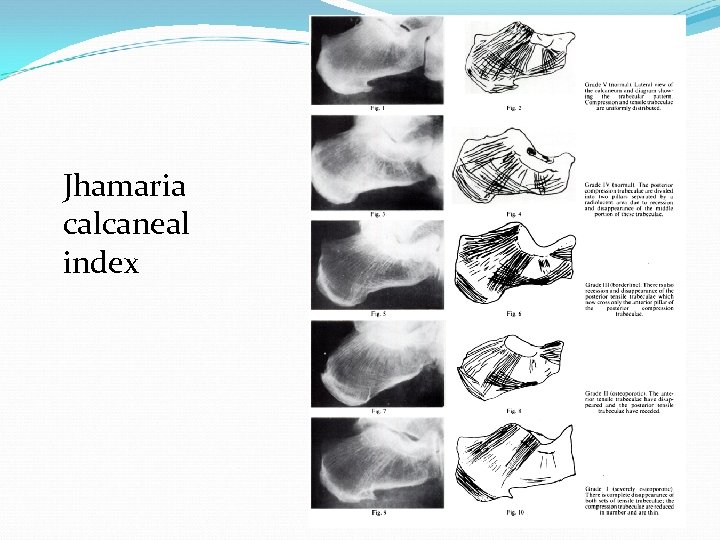
Jhamaria calcaneal index
Dual – energy Absorptiometry(DXA) In 1994, the WHO defined the threshold levels for the diagnosis of osteopenia and osteoporosis with DXA. As a consequence, DXA measurements are currently the standard of reference for the clinical diagnosis of osteoporosis with bone densitometry.
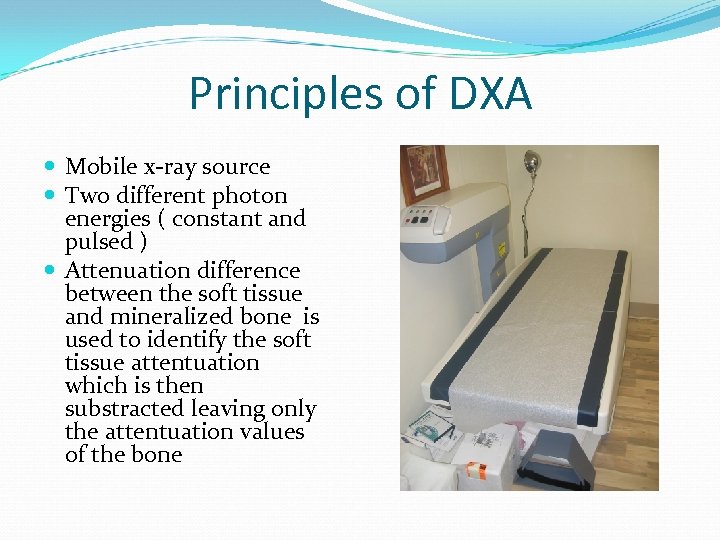
Principles of DXA Mobile x-ray source Two different photon energies ( constant and pulsed ) Attenuation difference between the soft tissue and mineralized bone is used to identify the soft tissue attentuation which is then substracted leaving only the attentuation values of the bone
Principles of DXA The attenuation is compared to known standard attenuation values from phantoms => relation between atenuation and BMD. Newer developments lateral scanners
BMD Measurements: BMD = Bone mineral content ( grams )/Projected area of the measured site ( cm 2 ) Overestimation with increased bone size Underestimation with decreased bone size
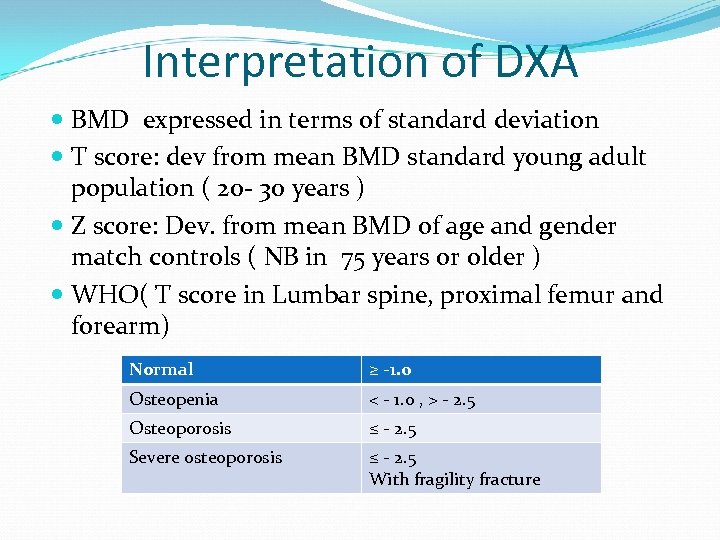
Interpretation of DXA BMD expressed in terms of standard deviation T score: dev from mean BMD standard young adult population ( 20 - 30 years ) Z score: Dev. from mean BMD of age and gender match controls ( NB in 75 years or older ) WHO( T score in Lumbar spine, proximal femur and forearm) Normal ≥ -1. 0 Osteopenia < - 1. 0 , > - 2. 5 Osteoporosis ≤ - 2. 5 Severe osteoporosis ≤ - 2. 5 With fragility fracture
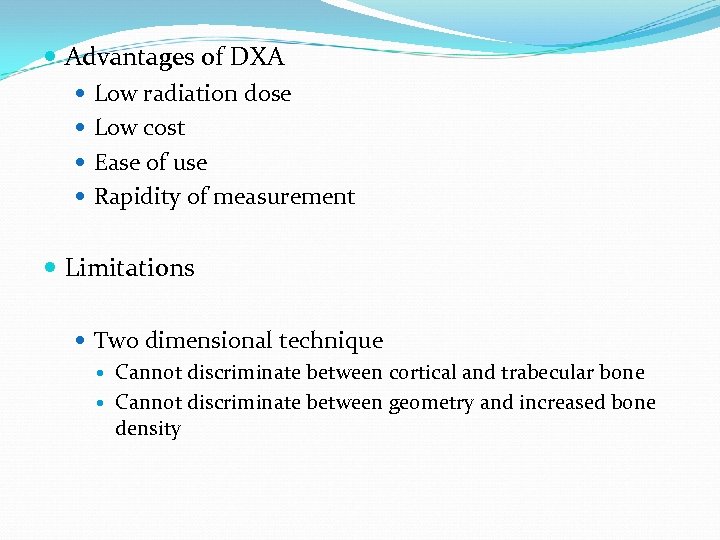
Advantages of DXA Low radiation dose Low cost Ease of use Rapidity of measurement Limitations Two dimensional technique Cannot discriminate between cortical and trabecular bone Cannot discriminate between geometry and increased bone density
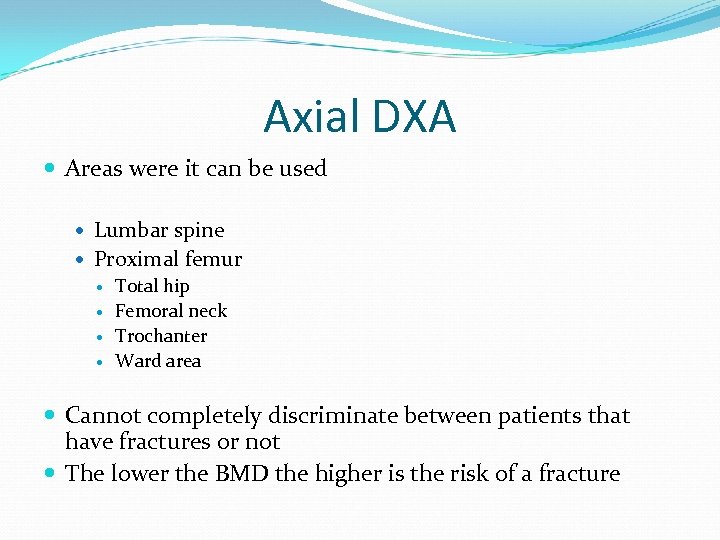
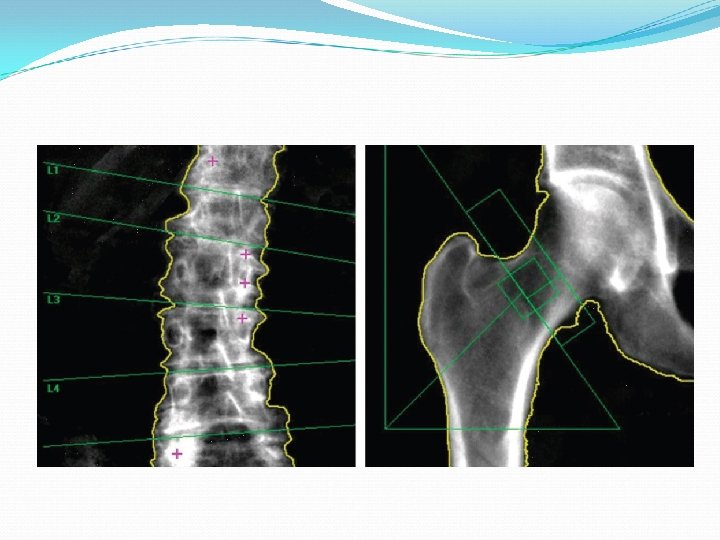
Axial DXA Areas were it can be used Lumbar spine Proximal femur Total hip Femoral neck Trochanter Ward area Cannot completely discriminate between patients that have fractures or not The lower the BMD the higher is the risk of a fracture
Pitfalls of DXA Scanner and soft ware Technologist, patient positioning, analysis of scans Patient related artefacts
Pitfalls of DXA Proper calibration: Phantoms scanned at least once a week Positioning Improper centering of the lumbar spine Abduction or external rotation of the hip Analytical pitfalls Spine Numbering of vertebrae Placement of intervertebral markers Detection of bone edges Hip Placement of ROI Detection of bone edges
Pitfalls of DXA Anatomic artefacts Degenerative disk disease Compression fractures Post surgical defects Atherosclerotic artefacts Motion artefacts Medical devices: Prosthesis, cement etc Personal belongings and clothes: wallets, coins Results from different machines not interchangeable.
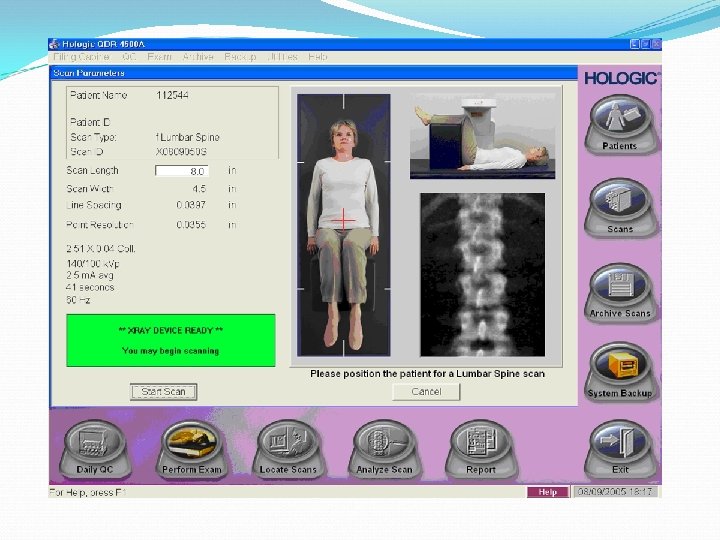
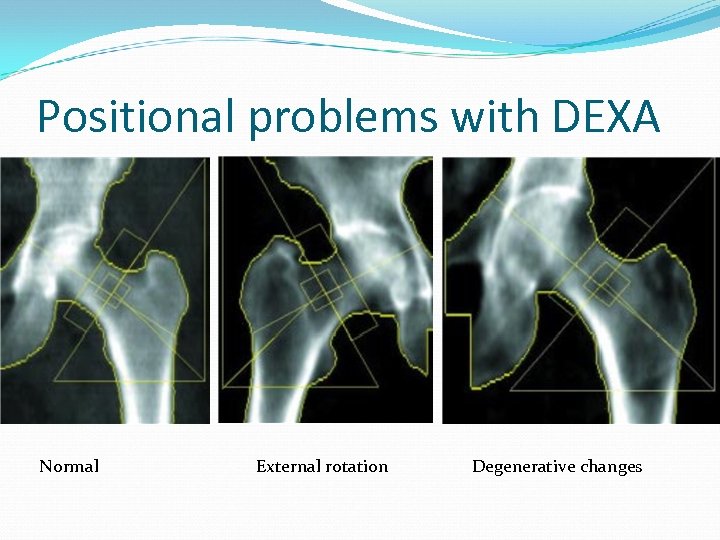
Positional problems with DEXA Normal External rotation Degenerative changes
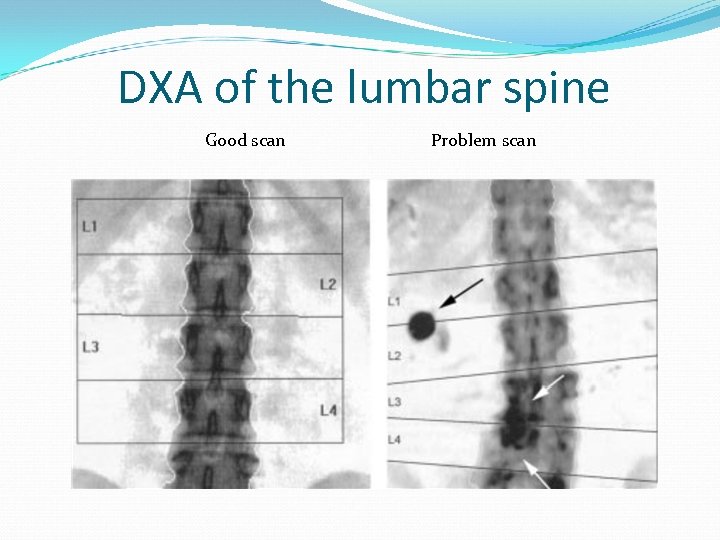
DXA of the lumbar spine Good scan Problem scan
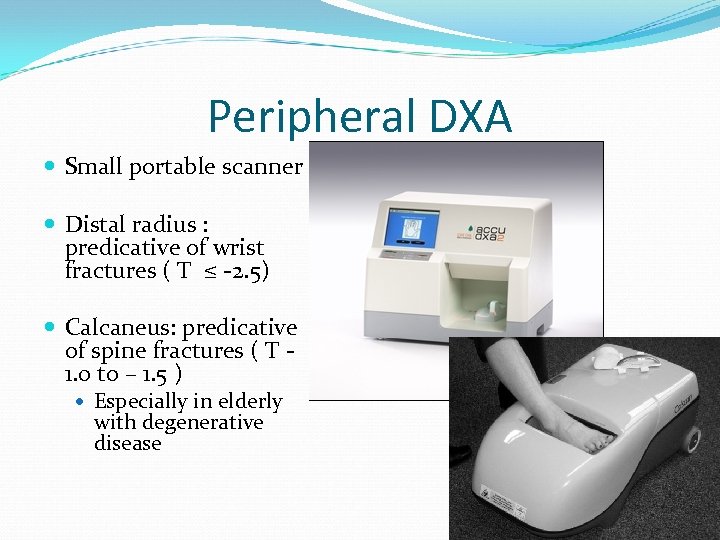
Peripheral DXA Small portable scanner Distal radius : predicative of wrist fractures ( T ≤ -2. 5) Calcaneus: predicative of spine fractures ( T 1. 0 to – 1. 5 ) Especially in elderly with degenerative disease
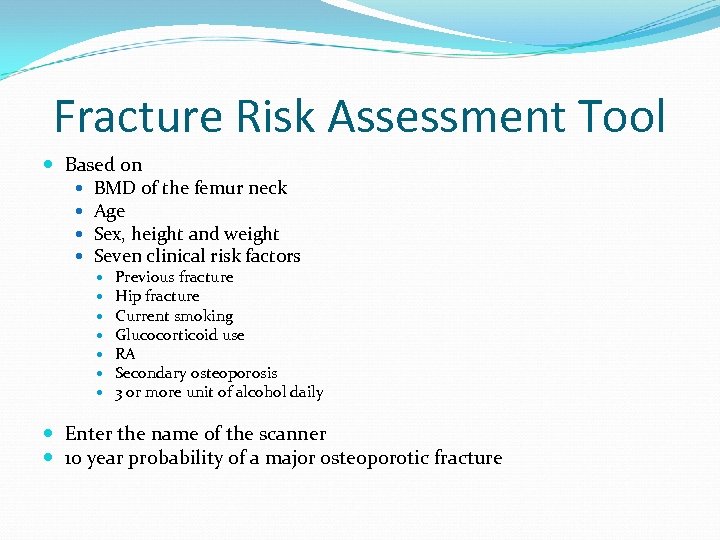
Fracture Risk Assessment Tool Based on BMD of the femur neck Age Sex, height and weight Seven clinical risk factors Previous fracture Hip fracture Current smoking Glucocorticoid use RA Secondary osteoporosis 3 or more unit of alcohol daily Enter the name of the scanner 10 year probability of a major osteoporotic fracture
Quantitative CT Separate estimates of Cortical BMD Trabecular BMD True volumetric density in mg/cm 3
Axial Quantitative CT 2 to 4 consecutive vertebrae ( T 12 – L 4 ) Commercial CT scanners Bone mineral reference standard 8 -10 mm thick slices, parallel to vertebral endplate Midplane of each vertebrae ROI anterior portion of trabecular bone in vertebral body. Automatic edge detection software then takes over and calculate the correct ROI with anatomical landmarks Compare attenuation values to a calibration standard Conversion to calcium hydroxy apatite/ cm 3
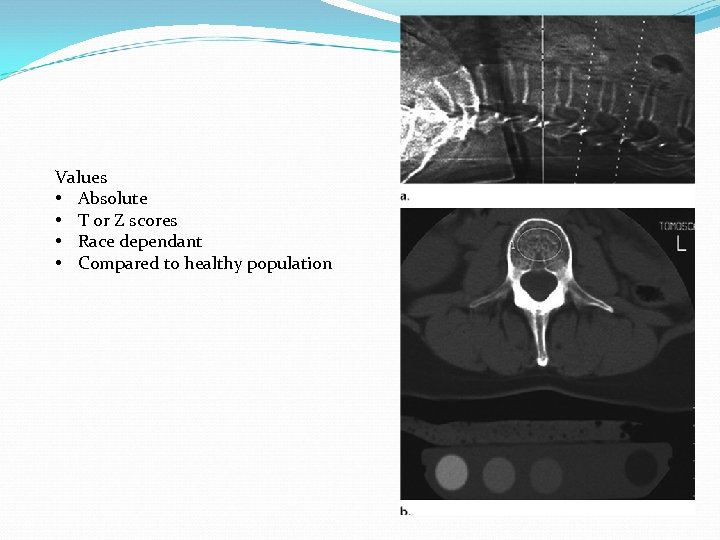
Values • Absolute • T or Z scores • Race dependant • Compared to healthy population
Advantages of Axial Quantitative CT Better than DXA at predicting vertebral fractures Good sensitivity measurement of age related bone loss after menopause Exclude measurement of structures that does not contribute to spine mechanical resistance but to BMD values Selective measurement of trabeculae which is the most metabolic active part of bone and main determinant of the compressive strength of bone Allow evaluation of the macro architecture of the vertebrae
New developments of quantitative CT Volumetric quantitative CT encompass the entire object of interest with stacked sections or spiral CT BMD of entire structure Separate analysis of trabecular and cortical components Dual energy CT is currently used to study the bone marrow adipocytes for effects of aging, drugs and disease.
Disadvantages of axial quantitative CT High radiation dose Poor precision for objects that is complex instead of longitudinal. High costs Operator dependance Space Limited scanner access.
Peripheral quantitative CT Separate accessments of cortical and trabecular bone Bone geometry at appendicular sites. Indexes of bone stability in response to bending and torsion which are the most important biomechanical measures of susceptibility fracture and may improve accuracy in the prediction of fractures.

Peripheral quantitative CT
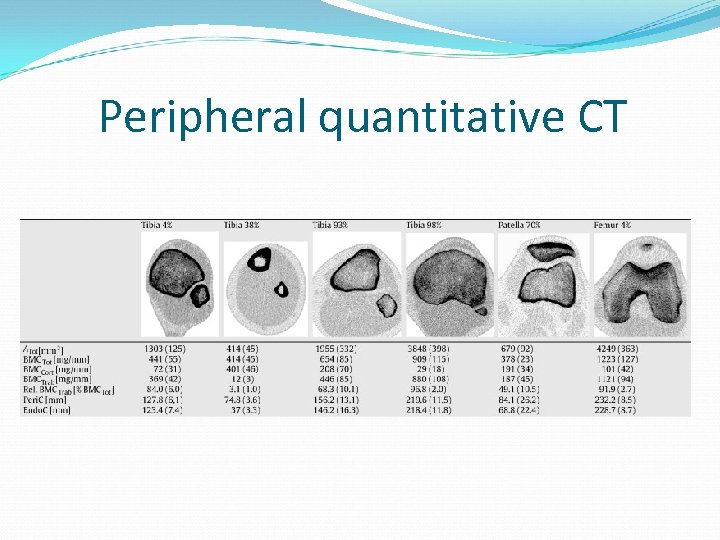
Peripheral quantitative CT
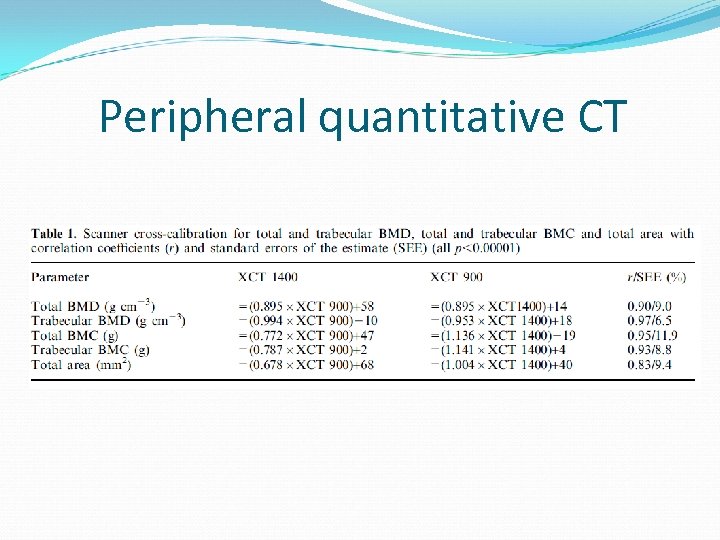
Peripheral quantitative CT
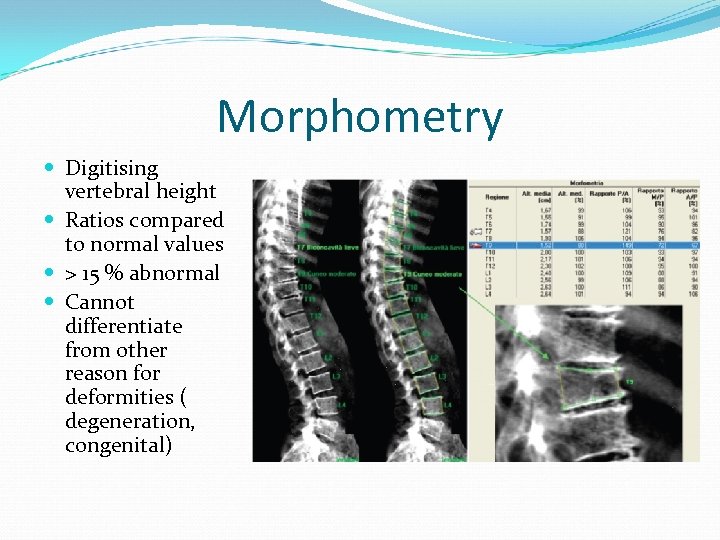
Morphometry Digitising vertebral height Ratios compared to normal values > 15 % abnormal Cannot differentiate from other reason for deformities ( degeneration, congenital)
Ultrasound Screening tool with confirmation by DXA Not sensitive enough for long term followup of osteoporosis. Calcaneus, distal metaphysis of the phalanx, radius and tibia
Newer advances Aim to better identify the macro and micro anatomy of bone to improve prediction of fracture risk. ( imaging of trabeculae ) MRI 3 tesla systems Calcaneus, knee and wrist Several studies but no clinical guidelines yet CT clinical systems not yet able to detect true trabecular networks but the texture Micro CT with resolutions of 6 micrometer currently used with in vitro studies.
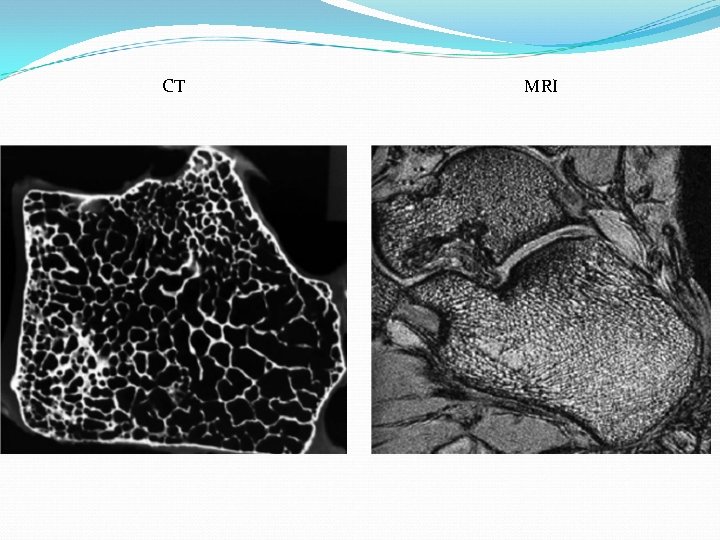
CT MRI
References Ortopedic imaging, A practical approach, Adam Greenspan Fundamentals of Diagnostic Radiology, Brant and Helms Integrated imaging approach to osteoporosis: State of the art review and update. Guiseppe Guglielmi et al, Radiographics 2011; 31: 1343 The trabecular pattern of the calcaneus as index of osteoporosis; NL Jhamaria et al. , British editorial society of bone and joint surgery, vol 65 -B, No 2 March 1983
57c82d80013111c4d2045f80beb8aa38.ppt