662b463f8d40851677f63ce843d2156a.ppt
- Количество слайдов: 55
 ICEMA Flight Nurse Orientation Local Optional Scope and ICEMA Policies and Procedures.
ICEMA Flight Nurse Orientation Local Optional Scope and ICEMA Policies and Procedures.
 OBJECTIVES • • Discuss the roll of ICEMA Discuss ICEMA specific policies Identify Trauma and Specialty Hospitals Identify the local optional scope of ICEMA paramedics.
OBJECTIVES • • Discuss the roll of ICEMA Discuss ICEMA specific policies Identify Trauma and Specialty Hospitals Identify the local optional scope of ICEMA paramedics.
 Policies & Procedures • Interfacility transfer of STEMI Patients - 8040 • • SB County Requests for Hospital Diversion - 8060 EMS Aircraft Destination Policy – 8070 Interfacility Transport Guidelines - 8010 Medical Response to Multi Casualty Incident - 5050 Medical Response to a Hazmat Incident - 5070 Physician On Scene - 9020 Responsibility For Patient Management - 9030 Guidelines for Patient Refusal Of Care – 9090/9100
Policies & Procedures • Interfacility transfer of STEMI Patients - 8040 • • SB County Requests for Hospital Diversion - 8060 EMS Aircraft Destination Policy – 8070 Interfacility Transport Guidelines - 8010 Medical Response to Multi Casualty Incident - 5050 Medical Response to a Hazmat Incident - 5070 Physician On Scene - 9020 Responsibility For Patient Management - 9030 Guidelines for Patient Refusal Of Care – 9090/9100
 • • Determination of Death on Scene – 12010 Withholding Resuscitative Measures - 12020 Requirements Radio Communication - 5040 Patient Care Records - 2010 Care of Minors In the Field - 9080 Local Medical Emergency - 9060 Guidelines on Applying Patient Restraints - 9070
• • Determination of Death on Scene – 12010 Withholding Resuscitative Measures - 12020 Requirements Radio Communication - 5040 Patient Care Records - 2010 Care of Minors In the Field - 9080 Local Medical Emergency - 9060 Guidelines on Applying Patient Restraints - 9070
 Paramedic Local Optional Scope • Transcutaneous Cardiac Pacing • Neonate and Pediatric Oral Endotracheal Intubation • CPAP • King Airway Device • Intraosseous Infusion • Nasal Tracheal Intubation • Naso/Orogastric Tube Insertion
Paramedic Local Optional Scope • Transcutaneous Cardiac Pacing • Neonate and Pediatric Oral Endotracheal Intubation • CPAP • King Airway Device • Intraosseous Infusion • Nasal Tracheal Intubation • Naso/Orogastric Tube Insertion
 The EMS System What is ICEMA? The Inland Counties Emergency Medical Agency (ICEMA) is responsible for providing the overall systems management and evaluation of the EMS Systems in San Bernardino, Inyo & Mono Counties under a joint powers agreement with each member county through the implementation of an EMS Plan. establishment and
The EMS System What is ICEMA? The Inland Counties Emergency Medical Agency (ICEMA) is responsible for providing the overall systems management and evaluation of the EMS Systems in San Bernardino, Inyo & Mono Counties under a joint powers agreement with each member county through the implementation of an EMS Plan. establishment and
 ICEMA RESPONSIBILITY MEDICAL • Medical oversight of EMS services • Designation of Base Hospitals, Trauma Centers, and STEMI centers • Development and implementation of a collaborative CQI process • Development/review and implementation of medical treatment protocols
ICEMA RESPONSIBILITY MEDICAL • Medical oversight of EMS services • Designation of Base Hospitals, Trauma Centers, and STEMI centers • Development and implementation of a collaborative CQI process • Development/review and implementation of medical treatment protocols
 ICEMA RESPONSIBILITY ADMINISTRATIVE • • • Certification and accreditation of EMS personnel Discipline of EMS providers Accountability to County citizens and Board of Supervisors
ICEMA RESPONSIBILITY ADMINISTRATIVE • • • Certification and accreditation of EMS personnel Discipline of EMS providers Accountability to County citizens and Board of Supervisors
 Criteria to Fly a Patient • When is flying a patient the appropriate method of transportation • Trauma Destination Policy • Burn Destination Policy • STEMI Destination Policy • Interfacility Transfer Policy
Criteria to Fly a Patient • When is flying a patient the appropriate method of transportation • Trauma Destination Policy • Burn Destination Policy • STEMI Destination Policy • Interfacility Transfer Policy
 ICEMA Trauma Destination Policy #15030 EMS Aircraft Indications: • An EMS aircraft may be dispatched for the following events: – Critical Trauma Patients when ground transport is greater than 30 minutes and EMS aircraft is expected to be significantly more expeditious than ground transport – MCI where multiple patients require transportation to multiple hospitals – Prolonged extrication time (> twenty (20) minutes) – Difficult ground access Do Not Delay Patient Transport waiting for an EMS aircraft
ICEMA Trauma Destination Policy #15030 EMS Aircraft Indications: • An EMS aircraft may be dispatched for the following events: – Critical Trauma Patients when ground transport is greater than 30 minutes and EMS aircraft is expected to be significantly more expeditious than ground transport – MCI where multiple patients require transportation to multiple hospitals – Prolonged extrication time (> twenty (20) minutes) – Difficult ground access Do Not Delay Patient Transport waiting for an EMS aircraft
 EMS Aircraft Transport Contraindications: • • Patients contaminated with Hazardous Material Violent or uncooperative patients Stable patients Ground transport is < 30 minutes Traumatic cardiac arrest Other safety issues as determined by pilot and/or crew Remote locations may be exempted from specific criteria upon written permission from the EMS Medical Director.
EMS Aircraft Transport Contraindications: • • Patients contaminated with Hazardous Material Violent or uncooperative patients Stable patients Ground transport is < 30 minutes Traumatic cardiac arrest Other safety issues as determined by pilot and/or crew Remote locations may be exempted from specific criteria upon written permission from the EMS Medical Director.
 Trauma Centers • Level I – Adult & Pediatric – Loma Linda University Medical Center – 24 Hour In-House Cardio-thoracic Surgery and Neurosurgery Capability • Level II – Arrowhead Regional Medical Center
Trauma Centers • Level I – Adult & Pediatric – Loma Linda University Medical Center – 24 Hour In-House Cardio-thoracic Surgery and Neurosurgery Capability • Level II – Arrowhead Regional Medical Center
 Specialty Centers • Burn Center – Arrowhead Regional Medical Center • Re-implantation Center – Loma Linda University Medical Center – (not officially designated)
Specialty Centers • Burn Center – Arrowhead Regional Medical Center • Re-implantation Center – Loma Linda University Medical Center – (not officially designated)
 Specialty Centers } STEMI Receiving Centers – Loma Linda University Medical Center – Pomona Valley Hospital Medical Center – San Antonio Community Hospital – St. Bernadine Medical Center – St. Mary Medical Center – Riverside Community Hospital • Stroke Centers – At this time the ICEMA region does not have designated Stroke Centers
Specialty Centers } STEMI Receiving Centers – Loma Linda University Medical Center – Pomona Valley Hospital Medical Center – San Antonio Community Hospital – St. Bernadine Medical Center – St. Mary Medical Center – Riverside Community Hospital • Stroke Centers – At this time the ICEMA region does not have designated Stroke Centers
 Specialty Centers • 5150 Receiving Centers – Arrowhead Regional Medical Center – Community Hospital of San Bernardino – Redlands Community Hospital • Hyperbaric Medicine – Loma Linda University Medical Center – Redlands Community Hospital
Specialty Centers • 5150 Receiving Centers – Arrowhead Regional Medical Center – Community Hospital of San Bernardino – Redlands Community Hospital • Hyperbaric Medicine – Loma Linda University Medical Center – Redlands Community Hospital
 INTERFACILITY TRANSFER OF STEMI PATIENT 8040 • This policy is for hospital to hospital STEMI transport only and shall not be used for any other requests from other entities • This policy allows hospitals without PCI capabilities to rapidly transfer patients to a STEMI Receiving Center with minimal delay.
INTERFACILITY TRANSFER OF STEMI PATIENT 8040 • This policy is for hospital to hospital STEMI transport only and shall not be used for any other requests from other entities • This policy allows hospitals without PCI capabilities to rapidly transfer patients to a STEMI Receiving Center with minimal delay.
 Requests for Hospital Diversion • Reference - 8060 • Hospitals in the ICEMA Region are not allowed to go on ED Diversion. • Types of Diversion Allowed By ICEMA – Neuro (CT) Diversion – Trauma Diversion – Internal Disaster – Bed delay is not a type of diversion
Requests for Hospital Diversion • Reference - 8060 • Hospitals in the ICEMA Region are not allowed to go on ED Diversion. • Types of Diversion Allowed By ICEMA – Neuro (CT) Diversion – Trauma Diversion – Internal Disaster – Bed delay is not a type of diversion
 EMS AIRCRAFT DESTINATION POLICY 8070 • All EMS Aircraft are dispatched by requests through San Bernardino County Comm Center • Destination is determined by Comm Center on an alternating schedule between ARMC and LLUMC. • Destination may be changed based on patient type.
EMS AIRCRAFT DESTINATION POLICY 8070 • All EMS Aircraft are dispatched by requests through San Bernardino County Comm Center • Destination is determined by Comm Center on an alternating schedule between ARMC and LLUMC. • Destination may be changed based on patient type.
 EMS AIRCRAFT DESTINATION POLICY 8070 • Every attempt should be made to continue radio contact with the original trauma base. • If the destination changes and contact is necessary with the new base, attempts should be made by the new base hospital to inform the original base to prevent confusion and activation of a trauma team unnecessarily.
EMS AIRCRAFT DESTINATION POLICY 8070 • Every attempt should be made to continue radio contact with the original trauma base. • If the destination changes and contact is necessary with the new base, attempts should be made by the new base hospital to inform the original base to prevent confusion and activation of a trauma team unnecessarily.
 Interfacility Transport Guidelines Policy # 8010 • EMT may – Monitor a saline lock or peripheral lines delivering fluids in combination/concentration of Normal Saline, Lactated Ringers, or Dextrose and Water provided: • • • No Medication is added to the IV fluid. IV maintained at a preset rate Check tubing for kinks and reposition arm if necessary Turn off IV if infiltration occurs Control bleeding at insertion site.
Interfacility Transport Guidelines Policy # 8010 • EMT may – Monitor a saline lock or peripheral lines delivering fluids in combination/concentration of Normal Saline, Lactated Ringers, or Dextrose and Water provided: • • • No Medication is added to the IV fluid. IV maintained at a preset rate Check tubing for kinks and reposition arm if necessary Turn off IV if infiltration occurs Control bleeding at insertion site.
 Interfacility Transfer Guidelines • An EMT may: – Transport a patient with a foley catheter – Transport a patient with a nasogastric tube or gastrostomy tube if they are clamped. – If the patient condition deteriorates the patient is transported to the closest facility.
Interfacility Transfer Guidelines • An EMT may: – Transport a patient with a foley catheter – Transport a patient with a nasogastric tube or gastrostomy tube if they are clamped. – If the patient condition deteriorates the patient is transported to the closest facility.
 Interfacility Transfer Guidelines • ALS Policy – If a STEMI patient refer to Policy #8040 Interfacility Transfer of STEMI Patient – Paramedics may not transport a patient with IV drips that are not in the Paramedic scope of practice – Paramedics may not transport a patient with blood or blood products.
Interfacility Transfer Guidelines • ALS Policy – If a STEMI patient refer to Policy #8040 Interfacility Transfer of STEMI Patient – Paramedics may not transport a patient with IV drips that are not in the Paramedic scope of practice – Paramedics may not transport a patient with blood or blood products.
 Interfacility Transfer Guidelines • Paramedics may – Monitor peripheral lines with any combination of Normal Saline, Lactated Ringers or Dextrose and Water – Transport IV solutions with added medications as follows: • • • Lidocaine Dopamine Procainamide Mag Sulfate Pitocin
Interfacility Transfer Guidelines • Paramedics may – Monitor peripheral lines with any combination of Normal Saline, Lactated Ringers or Dextrose and Water – Transport IV solutions with added medications as follows: • • • Lidocaine Dopamine Procainamide Mag Sulfate Pitocin
 Interfacility Transfer Guidelines • Paramedics may – Monitor and administer medications through a preexisting vascular access – Monitor IV solutions containing < 40 m. Eq/L of potassium – Monitor thoracostomy tube to water seal – Monitor NG tube
Interfacility Transfer Guidelines • Paramedics may – Monitor and administer medications through a preexisting vascular access – Monitor IV solutions containing < 40 m. Eq/L of potassium – Monitor thoracostomy tube to water seal – Monitor NG tube
 Interfacility Transfer Guidelines • Paramedics may initiate prior to contact protocols if the patient’s condition deteriorates then must contact the Base Hospital per protocol #5040, “Radio Communication Policy”.
Interfacility Transfer Guidelines • Paramedics may initiate prior to contact protocols if the patient’s condition deteriorates then must contact the Base Hospital per protocol #5040, “Radio Communication Policy”.
 Medical Response to a MCI Policy #5050 • Utilize START Triage • Incident Command System – Contact Comm. Center for bed availability Comm Center will utilize Reddinet for hospital contact – Medical Transportation Unit Leader Determines destination for patients transported
Medical Response to a MCI Policy #5050 • Utilize START Triage • Incident Command System – Contact Comm. Center for bed availability Comm Center will utilize Reddinet for hospital contact – Medical Transportation Unit Leader Determines destination for patients transported
 Medical Response to a MCI Policy #5050 • Medical Control – At the scene of a declared Multi-Casualty Incident, EMS personnel will operate within ICEMA’s “Prior to Contact Protocols”. – The Medic may contact the Trauma Base for orders if needed giving a concise report of incident and injuries. – Transport Agency will contact the receiving facility with an update on patient condition. Notification of incoming ambulances on Reddinet doesn’t give the hospital information on patient condition.
Medical Response to a MCI Policy #5050 • Medical Control – At the scene of a declared Multi-Casualty Incident, EMS personnel will operate within ICEMA’s “Prior to Contact Protocols”. – The Medic may contact the Trauma Base for orders if needed giving a concise report of incident and injuries. – Transport Agency will contact the receiving facility with an update on patient condition. Notification of incoming ambulances on Reddinet doesn’t give the hospital information on patient condition.
 Medical Response to a Haz. Mat Policy #5070 • Based on First Responder Awareness curriculum • All medical responders must function within the SUPPORT ZONE • Gross decontamination must be completed before transport • I/C will determine mode of transportation for contaminated patient
Medical Response to a Haz. Mat Policy #5070 • Based on First Responder Awareness curriculum • All medical responders must function within the SUPPORT ZONE • Gross decontamination must be completed before transport • I/C will determine mode of transportation for contaminated patient
 Physician on Scene Policy #9020 • EMT-P can only take orders from BH • Physician on-scene wanting to continue care for their patient must: – Show valid California Physician’s License – Sign statement assuming responsibility for pt care – Remain with patient at scene and during transport – Final decision regarding assumption of care will be made by BH physician
Physician on Scene Policy #9020 • EMT-P can only take orders from BH • Physician on-scene wanting to continue care for their patient must: – Show valid California Physician’s License – Sign statement assuming responsibility for pt care – Remain with patient at scene and during transport – Final decision regarding assumption of care will be made by BH physician
 Responsibility for Patient Management # 9030 • Responsibility for patient management shall rest with the highest medical authority on scene • If equally certified responders from a public and private agency are both on scene, responsibility for patient management will rest with the FIRST responder on scene
Responsibility for Patient Management # 9030 • Responsibility for patient management shall rest with the highest medical authority on scene • If equally certified responders from a public and private agency are both on scene, responsibility for patient management will rest with the FIRST responder on scene
 Patient Refusal of Care Guidelines Policy #9090/9100 • Patients can request transport to hospital other than the nearest medical appropriate facility – If requested hospital is outside of provider’s service area, transport must be offered to closest appropriate facility • Patient has right to refuse care • Documentation of refusal and other requests – Pt Care Report Form
Patient Refusal of Care Guidelines Policy #9090/9100 • Patients can request transport to hospital other than the nearest medical appropriate facility – If requested hospital is outside of provider’s service area, transport must be offered to closest appropriate facility • Patient has right to refuse care • Documentation of refusal and other requests – Pt Care Report Form
 Determination of Death on Scene Policy 12010 • Patient must be pulseless/apneic • If death is determined, – No BLS and ALS interventions initiated or continued • Patient fails to respond to initial cycle of ACLS – rhythm continues or deteriorates, – termination of efforts by Base Hospital Physician
Determination of Death on Scene Policy 12010 • Patient must be pulseless/apneic • If death is determined, – No BLS and ALS interventions initiated or continued • Patient fails to respond to initial cycle of ACLS – rhythm continues or deteriorates, – termination of efforts by Base Hospital Physician
 Withholding Resuscitative Measures Policy # 12020 • For patients in Skilled Nursing Facilities – Physician order on chart – Durable power of attorney – POLST Form • For patients in all other settings – CMA Prehospital DNR Form • DNR Report Form sent to ICEMA within 1 week – With copy of PCR
Withholding Resuscitative Measures Policy # 12020 • For patients in Skilled Nursing Facilities – Physician order on chart – Durable power of attorney – POLST Form • For patients in all other settings – CMA Prehospital DNR Form • DNR Report Form sent to ICEMA within 1 week – With copy of PCR
 Care of Minors in the Field Policy # 9080 – Any person under 18 years of age is legally a minor – Special cases not requiring parental consent • Pregnant girls when the illness is related to the pregnancy – Base hospital contact required if less than 9 yrs before leaving scene for AMA – Special cases not requiring treatment/transport
Care of Minors in the Field Policy # 9080 – Any person under 18 years of age is legally a minor – Special cases not requiring parental consent • Pregnant girls when the illness is related to the pregnancy – Base hospital contact required if less than 9 yrs before leaving scene for AMA – Special cases not requiring treatment/transport
 KING AIRWAY Adult and Pediatric Protocols # 10010 & 10020 • Treatment Indicators – Unresponsive and Apneic ( less than 6 breaths per minute) – NO Gag reflex – Do not use adult sizes in patients less than 4 foot tall – Pediatric sizes based on weight or height.
KING AIRWAY Adult and Pediatric Protocols # 10010 & 10020 • Treatment Indicators – Unresponsive and Apneic ( less than 6 breaths per minute) – NO Gag reflex – Do not use adult sizes in patients less than 4 foot tall – Pediatric sizes based on weight or height.
 KING AIRWAY Adult and Pediatric Protocols # 10010 & 10020 • Contradindications – Conscious patient with a gag reflex – Known ingestion of caustic substances – Suspected foreign body obstruction – Facial and/or esophageal trauma – Patients with known esophageal disease
KING AIRWAY Adult and Pediatric Protocols # 10010 & 10020 • Contradindications – Conscious patient with a gag reflex – Known ingestion of caustic substances – Suspected foreign body obstruction – Facial and/or esophageal trauma – Patients with known esophageal disease
 CONTINOUS POSTIVE AIRWAY PRESSURE (CPAP) • Available for all of the respiratory distress protocols (most other counties limit the usage to specific disease process) • Not used in pediatric patients • Simple process with almost immediate relief to the patients.
CONTINOUS POSTIVE AIRWAY PRESSURE (CPAP) • Available for all of the respiratory distress protocols (most other counties limit the usage to specific disease process) • Not used in pediatric patients • Simple process with almost immediate relief to the patients.
 Transcutaneous Cardiac Pacing • Protocol -10110 • Indications – Symptomatic Bradycardia – Witnessed asystole
Transcutaneous Cardiac Pacing • Protocol -10110 • Indications – Symptomatic Bradycardia – Witnessed asystole
 Transcutaneous Cardiac Pacing • Contraindications – Patients 8 and under – ICEMA protocol different than PALS recommendations
Transcutaneous Cardiac Pacing • Contraindications – Patients 8 and under – ICEMA protocol different than PALS recommendations
 Transcutaneous Cardiac Pacing • Procedure – – – Start with rate of 60 and output of 0 milliamps Increase milliamps until capture Assess pulses decrease output until capture is lost Then turn back up until capture is noted. Consider Midazolam 1 -2 mg increments up to 10 mg if patient awake and alert. – Consider Morphine Sulfate 1 -2 mg increments up to 10 mg for patients with pain and signs of adequate tissue perfusion
Transcutaneous Cardiac Pacing • Procedure – – – Start with rate of 60 and output of 0 milliamps Increase milliamps until capture Assess pulses decrease output until capture is lost Then turn back up until capture is noted. Consider Midazolam 1 -2 mg increments up to 10 mg if patient awake and alert. – Consider Morphine Sulfate 1 -2 mg increments up to 10 mg for patients with pain and signs of adequate tissue perfusion
 Oral Endotracheal Intubation Pediatric • Indicators – Non-responsive and apneic patients – Patients with agonal or failing respirations, and/or no gag reflex – Procedure may initially be contraindicated with suspected ALOC per protocol 14050 Pediatric Altered Level of Consciousness.
Oral Endotracheal Intubation Pediatric • Indicators – Non-responsive and apneic patients – Patients with agonal or failing respirations, and/or no gag reflex – Procedure may initially be contraindicated with suspected ALOC per protocol 14050 Pediatric Altered Level of Consciousness.
 Oral Endotracheal Intubation Pediatric • Support airway with appropriate adjuncts • For suspected head injury consider Lidocaine 1. 5 mg/kg IVP • Intubate with appropriate tube. • Check tube placement frequently • Medics are only allowed 2 attempts total at intubation prior to making Base Hospital contact.
Oral Endotracheal Intubation Pediatric • Support airway with appropriate adjuncts • For suspected head injury consider Lidocaine 1. 5 mg/kg IVP • Intubate with appropriate tube. • Check tube placement frequently • Medics are only allowed 2 attempts total at intubation prior to making Base Hospital contact.
 Intraosseous Infusion • Primary vascular access in cardiac arrest patients eight years of age and younger. • Any patient where vascular access is unavailable by any other means • Pick appropriate site by age • Most agencies now use the E-Z IO instead of the manual device and have had increased success rate. • Humeral head site new to ICEMA region.
Intraosseous Infusion • Primary vascular access in cardiac arrest patients eight years of age and younger. • Any patient where vascular access is unavailable by any other means • Pick appropriate site by age • Most agencies now use the E-Z IO instead of the manual device and have had increased success rate. • Humeral head site new to ICEMA region.
 Nasotracheal Intubation • INDICATORS – Possible cervical spine injury with clenched jaw and gag reflex – Trapped and inaccessible for direct laryngoscopy – Severe respiratory distress per Protocol Reference #11010, Adult Respiratory Emergencies – Patient nares can accommodate size 7. 0, 7. 5, or 8. 0 ET tube.
Nasotracheal Intubation • INDICATORS – Possible cervical spine injury with clenched jaw and gag reflex – Trapped and inaccessible for direct laryngoscopy – Severe respiratory distress per Protocol Reference #11010, Adult Respiratory Emergencies – Patient nares can accommodate size 7. 0, 7. 5, or 8. 0 ET tube.
 Nasotracheal Intubation • CONTRINDICATIONS • Apnea – Absolute contraindication. – Use alternate airway – Requires Base Hospital Contact • Relative contraindications – Significant trauma to the face or nose and/or possible basilar skull fracture – Anticoagulant therapy
Nasotracheal Intubation • CONTRINDICATIONS • Apnea – Absolute contraindication. – Use alternate airway – Requires Base Hospital Contact • Relative contraindications – Significant trauma to the face or nose and/or possible basilar skull fracture – Anticoagulant therapy
 Nasotracheal Intubation • Support ventilations • Consider prophylactic Lidocaine 1. 5 mg/kg for suspected head/brain injury • Administer metered dose 0. 5 mg Phenylephrine HCL to nostril • Place ET tube secure and monitor.
Nasotracheal Intubation • Support ventilations • Consider prophylactic Lidocaine 1. 5 mg/kg for suspected head/brain injury • Administer metered dose 0. 5 mg Phenylephrine HCL to nostril • Place ET tube secure and monitor.
 Naso/Gastric Tube • Indications – Any intubated patient where gastric distention may impede ABC’s – Oral route for patients with mid-facial trauma and all patients less than six (6) months of age.
Naso/Gastric Tube • Indications – Any intubated patient where gastric distention may impede ABC’s – Oral route for patients with mid-facial trauma and all patients less than six (6) months of age.
 Naso/Gastric Tube • Contraindications – History of esophageal strictures, varices and/or other esophageal diseases – Caustic ingestion – Significant facial or head trauma – History of bleeding disorders
Naso/Gastric Tube • Contraindications – History of esophageal strictures, varices and/or other esophageal diseases – Caustic ingestion – Significant facial or head trauma – History of bleeding disorders
 Naso/Gastric Tube • • Explain procedure if patient is alert Measure and mark Insert Confirm placement – Aspiration of gastric contents – Auscultate for sound of injected air over the epigastric area – Secure and attach to suction
Naso/Gastric Tube • • Explain procedure if patient is alert Measure and mark Insert Confirm placement – Aspiration of gastric contents – Auscultate for sound of injected air over the epigastric area – Secure and attach to suction
 Paramedic Local Optional Scope Medications • • • Ipratropium Bromide – Atrovent Magnesium Sulfate Ondansetron – Zofran Procainamide Verapamil KCL <40 meq/L of IVF for IFTs
Paramedic Local Optional Scope Medications • • • Ipratropium Bromide – Atrovent Magnesium Sulfate Ondansetron – Zofran Procainamide Verapamil KCL <40 meq/L of IVF for IFTs
 Ipratropium Bromide – Atrovent • Used in conjunction with Albuterol in all breathing treatments for respiratory emergencies. • Relative contraindication is allergy to peanuts.
Ipratropium Bromide – Atrovent • Used in conjunction with Albuterol in all breathing treatments for respiratory emergencies. • Relative contraindication is allergy to peanuts.
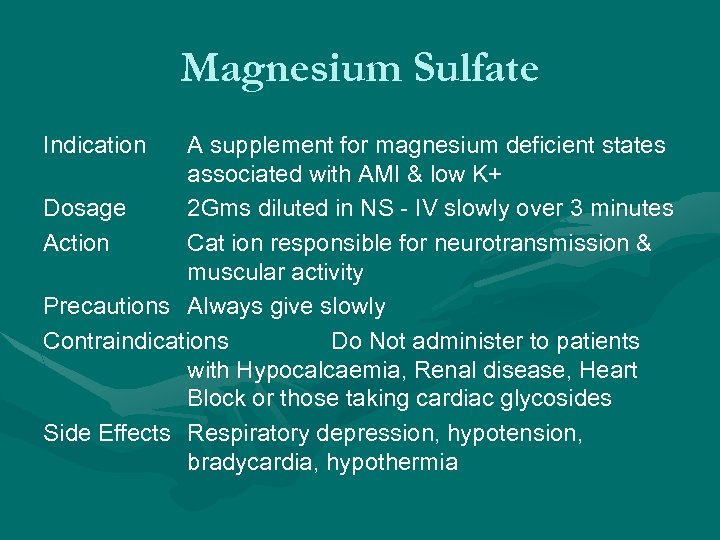 Magnesium Sulfate Indication A supplement for magnesium deficient states associated with AMI & low K+ Dosage 2 Gms diluted in NS - IV slowly over 3 minutes Action Cat ion responsible for neurotransmission & muscular activity Precautions Always give slowly Contraindications Do Not administer to patients with Hypocalcaemia, Renal disease, Heart Block or those taking cardiac glycosides Side Effects Respiratory depression, hypotension, bradycardia, hypothermia
Magnesium Sulfate Indication A supplement for magnesium deficient states associated with AMI & low K+ Dosage 2 Gms diluted in NS - IV slowly over 3 minutes Action Cat ion responsible for neurotransmission & muscular activity Precautions Always give slowly Contraindications Do Not administer to patients with Hypocalcaemia, Renal disease, Heart Block or those taking cardiac glycosides Side Effects Respiratory depression, hypotension, bradycardia, hypothermia
 Ondansetron – Zofran • • • Protocol 9120 Nausea and Vomiting Prophylactic treatment of narcotic induced nausea • Contraindications – Under 4 – Allergy to ondansetron or other 5 -Ht 3 antagonists
Ondansetron – Zofran • • • Protocol 9120 Nausea and Vomiting Prophylactic treatment of narcotic induced nausea • Contraindications – Under 4 – Allergy to ondansetron or other 5 -Ht 3 antagonists
 Procainamide • Used for Adult Tachycardias #11050 • 20 mg/min IV may be repeated till arrhythmia is suppressed or symptomatic hypotension, QRS widening by more than 50% or max dose of 17 mg/kg is given
Procainamide • Used for Adult Tachycardias #11050 • 20 mg/min IV may be repeated till arrhythmia is suppressed or symptomatic hypotension, QRS widening by more than 50% or max dose of 17 mg/kg is given
 Verapamil • Used for Atrial Fib/Flutter • Adenosine is usually used first exposing the underlying Fib/Flutter. • Verapamil is a prior to contact medication
Verapamil • Used for Atrial Fib/Flutter • Adenosine is usually used first exposing the underlying Fib/Flutter. • Verapamil is a prior to contact medication


