651195be6fef1a95b5cf058f78268082.ppt
- Количество слайдов: 26
 IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Adapted for Regional Training Course on RP of Patients for Radiographers Accra, Ghana, 11 -15 July 2011 RADIATION PROTECTION IN DIAGNOSTIC AND INTERVENTIONAL RADIOLOGY L 14: Radiation exposure in pregnancy IAEA International Atomic Energy Agency
IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Adapted for Regional Training Course on RP of Patients for Radiographers Accra, Ghana, 11 -15 July 2011 RADIATION PROTECTION IN DIAGNOSTIC AND INTERVENTIONAL RADIOLOGY L 14: Radiation exposure in pregnancy IAEA International Atomic Energy Agency
 Topics • • Introduction Effects and risks of in utero exposure Typical doses Practical implementation IAEA 14: Radiation exposure in pregnancy 2
Topics • • Introduction Effects and risks of in utero exposure Typical doses Practical implementation IAEA 14: Radiation exposure in pregnancy 2
 IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 1: Introduction IAEA International Atomic Energy Agency
IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 1: Introduction IAEA International Atomic Energy Agency
 Introduction • Thousands of pregnant women are exposed to ionizing radiation each year • Lack of knowledge is responsible for much anxiety and possibly unnecessary termination of pregnancies • For most patients, the radiation exposure was medically appropriate and the radiation risk was minimal IAEA 14: Radiation exposure in pregnancy 4
Introduction • Thousands of pregnant women are exposed to ionizing radiation each year • Lack of knowledge is responsible for much anxiety and possibly unnecessary termination of pregnancies • For most patients, the radiation exposure was medically appropriate and the radiation risk was minimal IAEA 14: Radiation exposure in pregnancy 4
 Situation analysis • Exposure of females of reproductive capacity: • Intended medical exposure: • Patients needing radiological procedures while pregnant • Unintended or accidental medical exposure: • Pregnancy not known or not declared • Occupational exposure IAEA 14: Radiation exposure in pregnancy 5
Situation analysis • Exposure of females of reproductive capacity: • Intended medical exposure: • Patients needing radiological procedures while pregnant • Unintended or accidental medical exposure: • Pregnancy not known or not declared • Occupational exposure IAEA 14: Radiation exposure in pregnancy 5
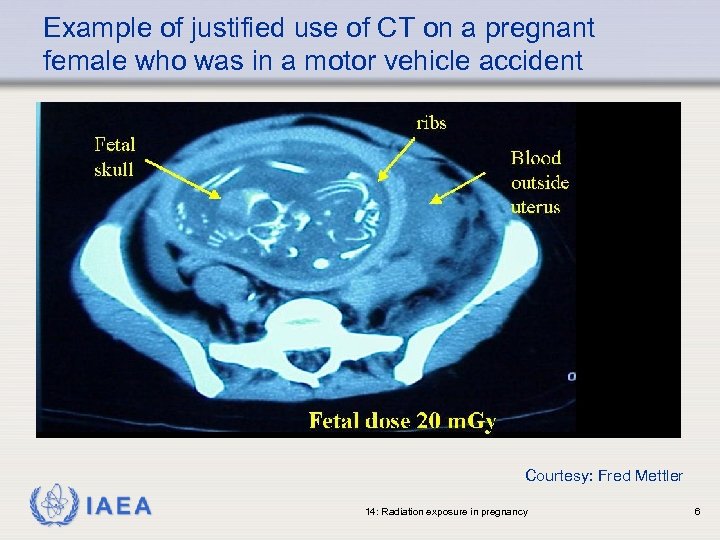 Example of justified use of CT on a pregnant female who was in a motor vehicle accident Courtesy: Fred Mettler IAEA 14: Radiation exposure in pregnancy 6
Example of justified use of CT on a pregnant female who was in a motor vehicle accident Courtesy: Fred Mettler IAEA 14: Radiation exposure in pregnancy 6
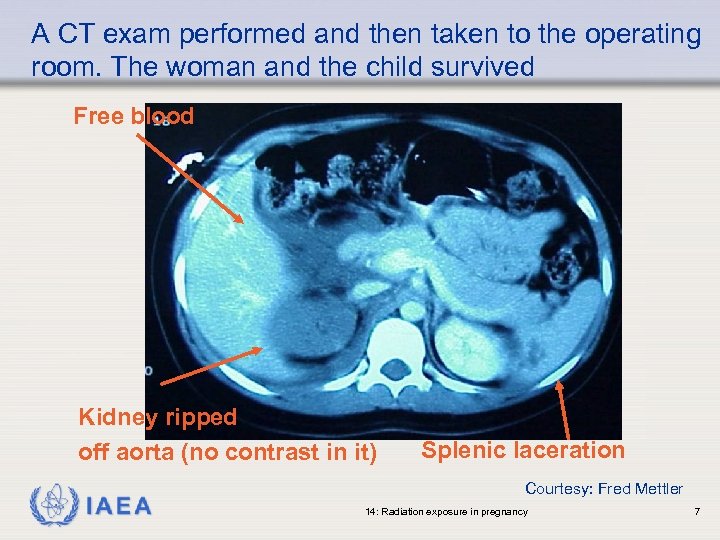 A CT exam performed and then taken to the operating room. The woman and the child survived Free blood Kidney ripped off aorta (no contrast in it) IAEA Splenic laceration Courtesy: Fred Mettler 14: Radiation exposure in pregnancy 7
A CT exam performed and then taken to the operating room. The woman and the child survived Free blood Kidney ripped off aorta (no contrast in it) IAEA Splenic laceration Courtesy: Fred Mettler 14: Radiation exposure in pregnancy 7
 IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 2: Effects and risks of in utero exposure IAEA International Atomic Energy Agency
IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 2: Effects and risks of in utero exposure IAEA International Atomic Energy Agency
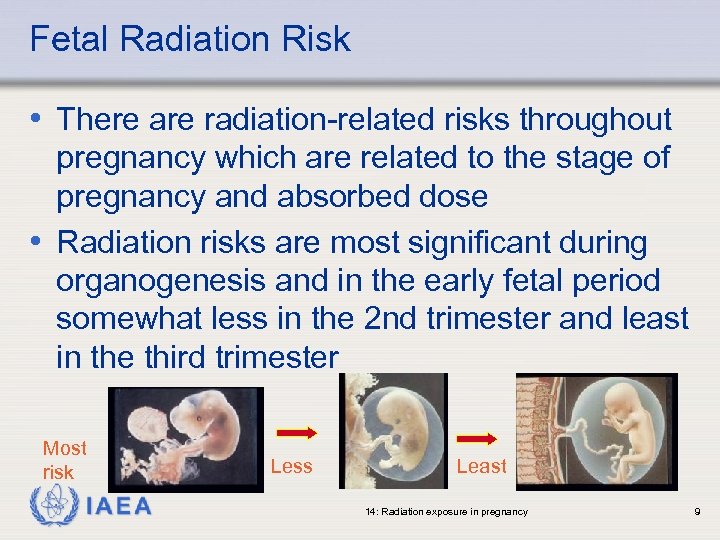 Fetal Radiation Risk • There are radiation-related risks throughout pregnancy which are related to the stage of pregnancy and absorbed dose • Radiation risks are most significant during organogenesis and in the early fetal period somewhat less in the 2 nd trimester and least in the third trimester Most risk IAEA Less Least 14: Radiation exposure in pregnancy 9
Fetal Radiation Risk • There are radiation-related risks throughout pregnancy which are related to the stage of pregnancy and absorbed dose • Radiation risks are most significant during organogenesis and in the early fetal period somewhat less in the 2 nd trimester and least in the third trimester Most risk IAEA Less Least 14: Radiation exposure in pregnancy 9
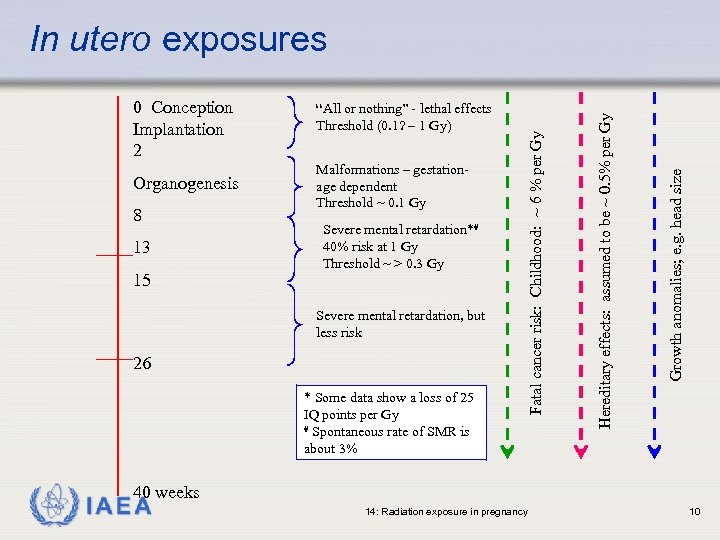 8 13 15 Malformations – gestationage dependent Threshold ~ 0. 1 Gy Severe mental retardation*# 40% risk at 1 Gy Threshold ~ > 0. 3 Gy Severe mental retardation, but less risk 26 * Some data show a loss of 25 IQ points per Gy # Spontaneous rate of SMR is about 3% Growth anomalies; e. g. head size Organogenesis “All or nothing” - lethal effects Threshold (0. 1? – 1 Gy) Hereditary effects: assumed to be ~ 0. 5% per Gy 0 Conception Implantation 2 Fatal cancer risk: Childhood: ~ 6 % per Gy In utero exposures 40 weeks IAEA 14: Radiation exposure in pregnancy 10
8 13 15 Malformations – gestationage dependent Threshold ~ 0. 1 Gy Severe mental retardation*# 40% risk at 1 Gy Threshold ~ > 0. 3 Gy Severe mental retardation, but less risk 26 * Some data show a loss of 25 IQ points per Gy # Spontaneous rate of SMR is about 3% Growth anomalies; e. g. head size Organogenesis “All or nothing” - lethal effects Threshold (0. 1? – 1 Gy) Hereditary effects: assumed to be ~ 0. 5% per Gy 0 Conception Implantation 2 Fatal cancer risk: Childhood: ~ 6 % per Gy In utero exposures 40 weeks IAEA 14: Radiation exposure in pregnancy 10
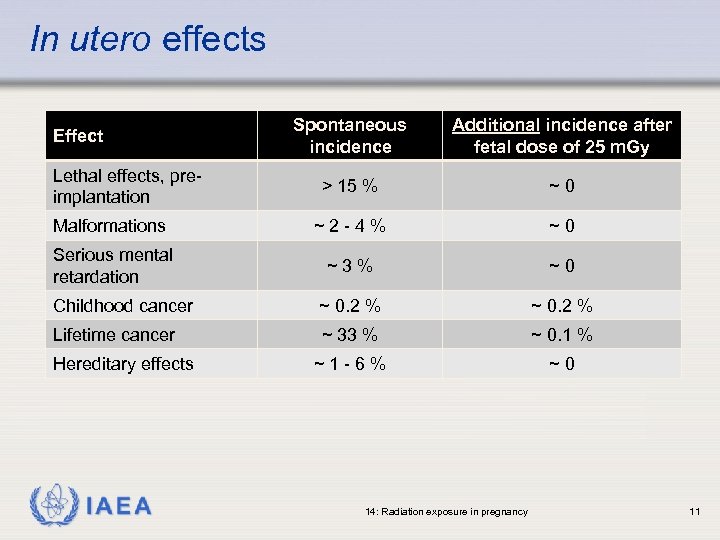 In utero effects Spontaneous incidence Additional incidence after fetal dose of 25 m. Gy > 15 % ~0 Malformations ~2 -4% ~0 Serious mental retardation ~3% ~0 Childhood cancer ~ 0. 2 % Lifetime cancer ~ 33 % ~ 0. 1 % ~1 -6% ~0 Effect Lethal effects, preimplantation Hereditary effects IAEA 14: Radiation exposure in pregnancy 11
In utero effects Spontaneous incidence Additional incidence after fetal dose of 25 m. Gy > 15 % ~0 Malformations ~2 -4% ~0 Serious mental retardation ~3% ~0 Childhood cancer ~ 0. 2 % Lifetime cancer ~ 33 % ~ 0. 1 % ~1 -6% ~0 Effect Lethal effects, preimplantation Hereditary effects IAEA 14: Radiation exposure in pregnancy 11
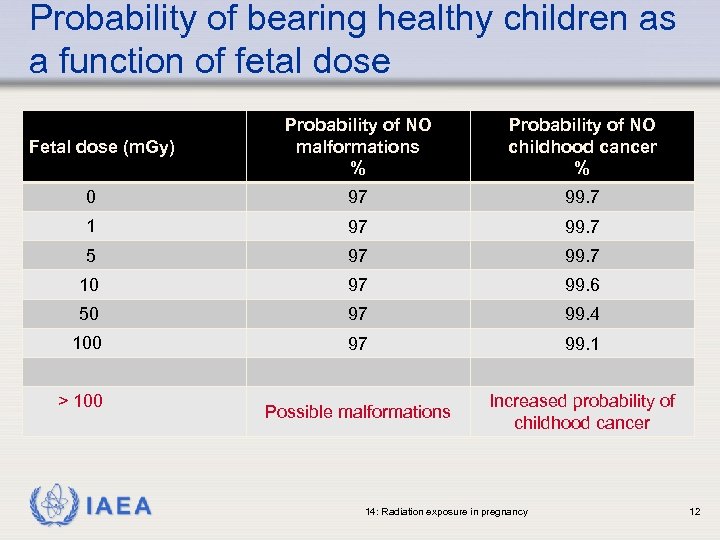 Probability of bearing healthy children as a function of fetal dose Probability of NO malformations % Probability of NO childhood cancer % 0 97 99. 7 1 97 99. 7 5 97 99. 7 10 97 99. 6 50 97 99. 4 100 97 99. 1 Possible malformations Increased probability of childhood cancer Fetal dose (m. Gy) > 100 IAEA 14: Radiation exposure in pregnancy 12
Probability of bearing healthy children as a function of fetal dose Probability of NO malformations % Probability of NO childhood cancer % 0 97 99. 7 1 97 99. 7 5 97 99. 7 10 97 99. 6 50 97 99. 4 100 97 99. 1 Possible malformations Increased probability of childhood cancer Fetal dose (m. Gy) > 100 IAEA 14: Radiation exposure in pregnancy 12
 IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 3: Typical doses IAEA International Atomic Energy Agency
IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 3: Typical doses IAEA International Atomic Energy Agency
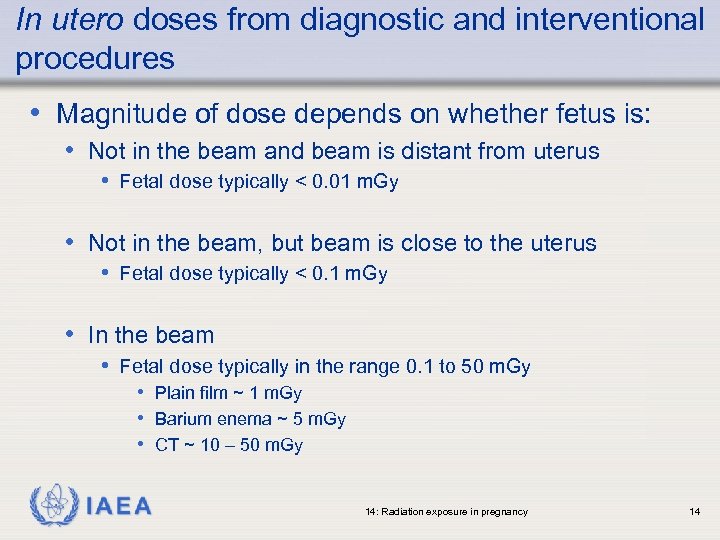 In utero doses from diagnostic and interventional procedures • Magnitude of dose depends on whether fetus is: • Not in the beam and beam is distant from uterus • Fetal dose typically < 0. 01 m. Gy • Not in the beam, but beam is close to the uterus • Fetal dose typically < 0. 1 m. Gy • In the beam • Fetal dose typically in the range 0. 1 to 50 m. Gy • Plain film ~ 1 m. Gy • Barium enema ~ 5 m. Gy • CT ~ 10 – 50 m. Gy IAEA 14: Radiation exposure in pregnancy 14
In utero doses from diagnostic and interventional procedures • Magnitude of dose depends on whether fetus is: • Not in the beam and beam is distant from uterus • Fetal dose typically < 0. 01 m. Gy • Not in the beam, but beam is close to the uterus • Fetal dose typically < 0. 1 m. Gy • In the beam • Fetal dose typically in the range 0. 1 to 50 m. Gy • Plain film ~ 1 m. Gy • Barium enema ~ 5 m. Gy • CT ~ 10 – 50 m. Gy IAEA 14: Radiation exposure in pregnancy 14
 IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 4: Practical implementation IAEA International Atomic Energy Agency
IAEA Training Material on Radiation Protection in Diagnostic and Interventional Radiology Part 14: Radiation exposure in pregnancy Topic 4: Practical implementation IAEA International Atomic Energy Agency
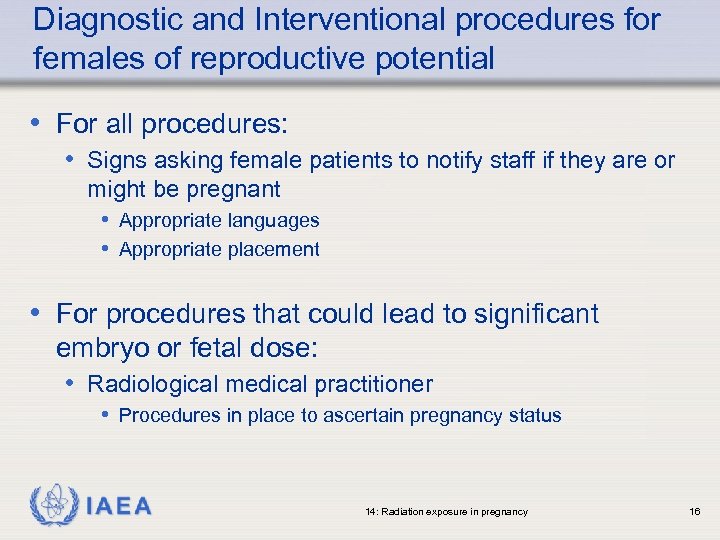 Diagnostic and Interventional procedures for females of reproductive potential • For all procedures: • Signs asking female patients to notify staff if they are or might be pregnant • Appropriate languages • Appropriate placement • For procedures that could lead to significant embryo or fetal dose: • Radiological medical practitioner • Procedures in place to ascertain pregnancy status IAEA 14: Radiation exposure in pregnancy 16
Diagnostic and Interventional procedures for females of reproductive potential • For all procedures: • Signs asking female patients to notify staff if they are or might be pregnant • Appropriate languages • Appropriate placement • For procedures that could lead to significant embryo or fetal dose: • Radiological medical practitioner • Procedures in place to ascertain pregnancy status IAEA 14: Radiation exposure in pregnancy 16
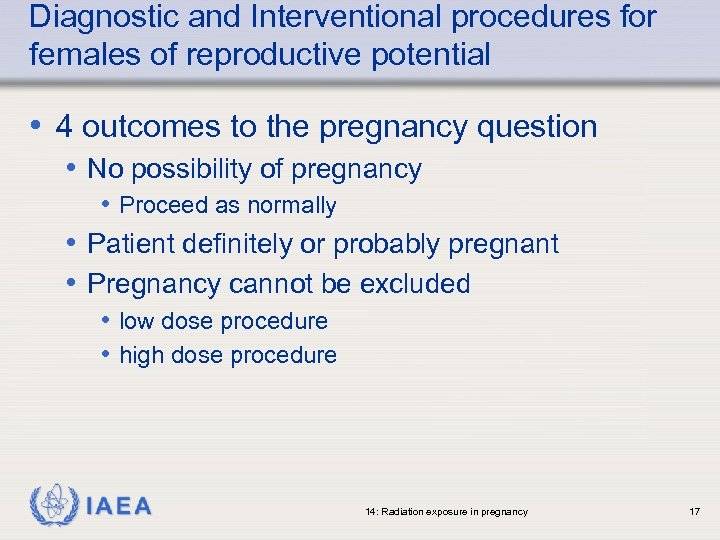 Diagnostic and Interventional procedures for females of reproductive potential • 4 outcomes to the pregnancy question • No possibility of pregnancy • Proceed as normally • Patient definitely or probably pregnant • Pregnancy cannot be excluded • low dose procedure • high dose procedure IAEA 14: Radiation exposure in pregnancy 17
Diagnostic and Interventional procedures for females of reproductive potential • 4 outcomes to the pregnancy question • No possibility of pregnancy • Proceed as normally • Patient definitely or probably pregnant • Pregnancy cannot be excluded • low dose procedure • high dose procedure IAEA 14: Radiation exposure in pregnancy 17
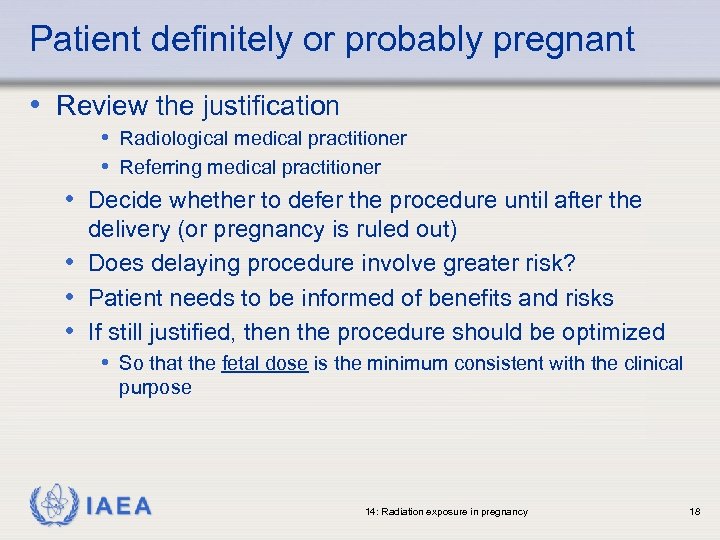 Patient definitely or probably pregnant • Review the justification • Radiological medical practitioner • Referring medical practitioner • Decide whether to defer the procedure until after the delivery (or pregnancy is ruled out) • Does delaying procedure involve greater risk? • Patient needs to be informed of benefits and risks • If still justified, then the procedure should be optimized • So that the fetal dose is the minimum consistent with the clinical purpose IAEA 14: Radiation exposure in pregnancy 18
Patient definitely or probably pregnant • Review the justification • Radiological medical practitioner • Referring medical practitioner • Decide whether to defer the procedure until after the delivery (or pregnancy is ruled out) • Does delaying procedure involve greater risk? • Patient needs to be informed of benefits and risks • If still justified, then the procedure should be optimized • So that the fetal dose is the minimum consistent with the clinical purpose IAEA 14: Radiation exposure in pregnancy 18
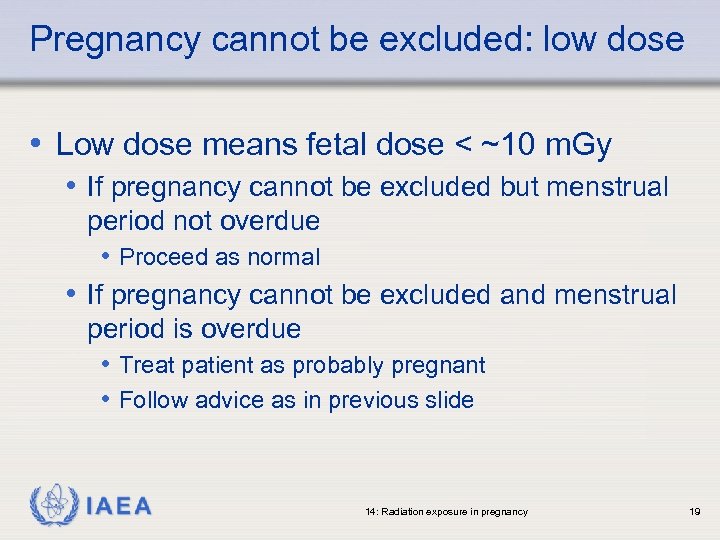 Pregnancy cannot be excluded: low dose • Low dose means fetal dose < ~10 m. Gy • If pregnancy cannot be excluded but menstrual period not overdue • Proceed as normal • If pregnancy cannot be excluded and menstrual period is overdue • Treat patient as probably pregnant • Follow advice as in previous slide IAEA 14: Radiation exposure in pregnancy 19
Pregnancy cannot be excluded: low dose • Low dose means fetal dose < ~10 m. Gy • If pregnancy cannot be excluded but menstrual period not overdue • Proceed as normal • If pregnancy cannot be excluded and menstrual period is overdue • Treat patient as probably pregnant • Follow advice as in previous slide IAEA 14: Radiation exposure in pregnancy 19
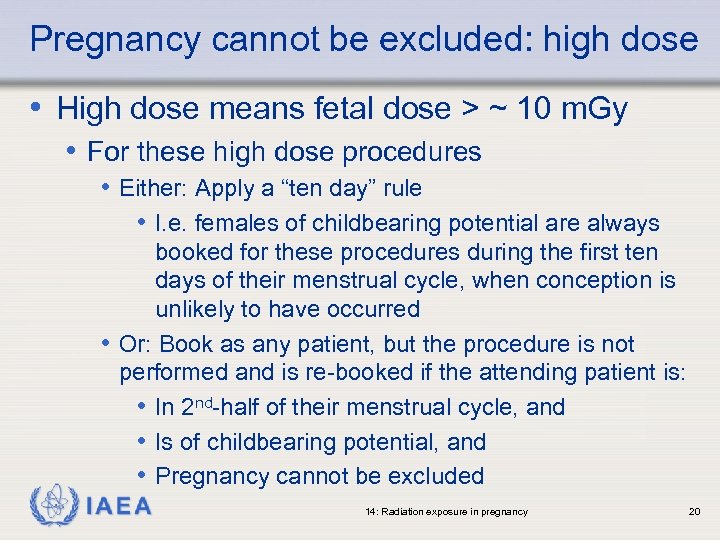 Pregnancy cannot be excluded: high dose • High dose means fetal dose > ~ 10 m. Gy • For these high dose procedures • Either: Apply a “ten day” rule • I. e. females of childbearing potential are always booked for these procedures during the first ten days of their menstrual cycle, when conception is unlikely to have occurred • Or: Book as any patient, but the procedure is not performed and is re-booked if the attending patient is: • In 2 nd-half of their menstrual cycle, and • Is of childbearing potential, and • Pregnancy cannot be excluded IAEA 14: Radiation exposure in pregnancy 20
Pregnancy cannot be excluded: high dose • High dose means fetal dose > ~ 10 m. Gy • For these high dose procedures • Either: Apply a “ten day” rule • I. e. females of childbearing potential are always booked for these procedures during the first ten days of their menstrual cycle, when conception is unlikely to have occurred • Or: Book as any patient, but the procedure is not performed and is re-booked if the attending patient is: • In 2 nd-half of their menstrual cycle, and • Is of childbearing potential, and • Pregnancy cannot be excluded IAEA 14: Radiation exposure in pregnancy 20
 Inadvertent exposure in pregnancy • Can occur in two ways: • A pregnant patient is asked whether she is or might be pregnant and denies it • Either deliberately or in ignorance of her condition; and • Procedure takes place • A pregnant patient is NOT asked and the procedure takes place regardless • Revised BSS requires the licensee to investigate any inadvertent exposure of the embryo or fetus • Dose and risk estimation • Patient and referring doctor informed IAEA 14: Radiation exposure in pregnancy 21
Inadvertent exposure in pregnancy • Can occur in two ways: • A pregnant patient is asked whether she is or might be pregnant and denies it • Either deliberately or in ignorance of her condition; and • Procedure takes place • A pregnant patient is NOT asked and the procedure takes place regardless • Revised BSS requires the licensee to investigate any inadvertent exposure of the embryo or fetus • Dose and risk estimation • Patient and referring doctor informed IAEA 14: Radiation exposure in pregnancy 21
 Termination of pregnancy • Termination of pregnancy for fetal doses of less than 100 m. Gy is NOT justified based solely upon radiation risk • For fetal doses in excess of 100 m. Gy, there can be fetal damage, the magnitude and type of which is a function of dose and stage of pregnancy • In these cases decisions on termination should be based upon individual circumstances IAEA 14: Radiation exposure in pregnancy 22
Termination of pregnancy • Termination of pregnancy for fetal doses of less than 100 m. Gy is NOT justified based solely upon radiation risk • For fetal doses in excess of 100 m. Gy, there can be fetal damage, the magnitude and type of which is a function of dose and stage of pregnancy • In these cases decisions on termination should be based upon individual circumstances IAEA 14: Radiation exposure in pregnancy 22
 Occupational Exposure of Pregnant Workers • Pregnant medical radiation workers may work in a radiation environment as long as there is reasonable assurance that the fetal dose can be kept below 1 m. Gy during the pregnancy • Typically 3 options for pregnant workers • No change in assigned work duties • Change to an area where the radiation exposure may be lower • Change to a role that has no radiation exposure • Discussions are needed • Pregnant worker must be informed of potential risks, local policies and the dose limits IAEA 14: Radiation exposure in pregnancy 23
Occupational Exposure of Pregnant Workers • Pregnant medical radiation workers may work in a radiation environment as long as there is reasonable assurance that the fetal dose can be kept below 1 m. Gy during the pregnancy • Typically 3 options for pregnant workers • No change in assigned work duties • Change to an area where the radiation exposure may be lower • Change to a role that has no radiation exposure • Discussions are needed • Pregnant worker must be informed of potential risks, local policies and the dose limits IAEA 14: Radiation exposure in pregnancy 23
 Occupational Exposure of Pregnant Workers • From an occupational dose perspective there are few situations in diagnostic and interventional radiology where a pregnant worker would actually need to change their duties • “Front line” operators in image guided interventional procedures are a possible exception • Need to use previous monitoring history to establish likely levels of exposure • Need to be confident that accidents with the potential for occupational exposure are unlikely • There will be other concerns of the pregnant worker that will need to be taken into account IAEA 14: Radiation exposure in pregnancy 24
Occupational Exposure of Pregnant Workers • From an occupational dose perspective there are few situations in diagnostic and interventional radiology where a pregnant worker would actually need to change their duties • “Front line” operators in image guided interventional procedures are a possible exception • Need to use previous monitoring history to establish likely levels of exposure • Need to be confident that accidents with the potential for occupational exposure are unlikely • There will be other concerns of the pregnant worker that will need to be taken into account IAEA 14: Radiation exposure in pregnancy 24
 Summary • The radiation dose to the embryo or fetus from any diagnostic or interventional procedure in current use should present no risk of causing fetal death, malformation, growth retardation or impairment of mental development • For the majority of diagnostic procedures, giving fetal doses up to about a milligray, the associated risks of childhood cancer are very low • For high fetal dose procedures, systems must be in place to ascertain pregnancy status, with ensuing review of the justification for each patient, and appropriate optimization if the procedure is performed IAEA 14: Radiation exposure in pregnancy 25
Summary • The radiation dose to the embryo or fetus from any diagnostic or interventional procedure in current use should present no risk of causing fetal death, malformation, growth retardation or impairment of mental development • For the majority of diagnostic procedures, giving fetal doses up to about a milligray, the associated risks of childhood cancer are very low • For high fetal dose procedures, systems must be in place to ascertain pregnancy status, with ensuing review of the justification for each patient, and appropriate optimization if the procedure is performed IAEA 14: Radiation exposure in pregnancy 25
 Where to Get More Information • ICRP Publication 84. Pregnancy and Medical Radiation (1999). • ICRP Publication 90. Biological Effects after Prenatal Irradiation (Embryo and Fetus)(2003) • ICRP Publication 103. The 2007 Recommendations of the International Commission on Radiological Protection (2007) • Protection of Pregnant Patients during Diagnostic Medical Exposures to Ionizing Radiation. Advice from the HPA, RCR and Co. R (2009) IAEA 14: Radiation exposure in pregnancy 26
Where to Get More Information • ICRP Publication 84. Pregnancy and Medical Radiation (1999). • ICRP Publication 90. Biological Effects after Prenatal Irradiation (Embryo and Fetus)(2003) • ICRP Publication 103. The 2007 Recommendations of the International Commission on Radiological Protection (2007) • Protection of Pregnant Patients during Diagnostic Medical Exposures to Ionizing Radiation. Advice from the HPA, RCR and Co. R (2009) IAEA 14: Radiation exposure in pregnancy 26


