IABP Intra aortic Balloon Pump by Olha Tkachuk
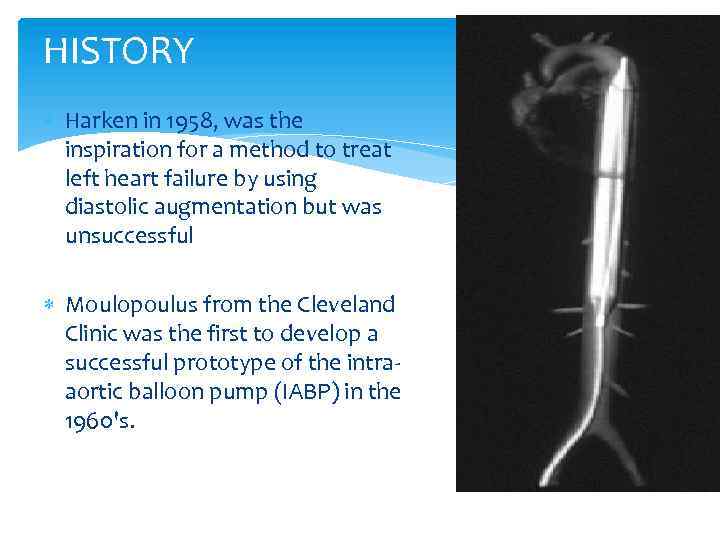
HISTORY Harken in 1958, was the inspiration for a method to treat left heart failure by using diastolic augmentation but was unsuccessful Moulopoulus from the Cleveland Clinic was the first to develop a successful prototype of the intraaortic balloon pump (IABP) in the 1960's.
HISTORY Finally, in 1968, Dr. Adrian Kantrowitz’s group began to use the IABP in clinical practice. balloon catheters were 15 French and needed to be surgically grafted into the femoral arteries. Percutaneous IAB catheters were developed in 1979
PATHO-PHYSIOLOGY Preload is defined as the amount of blood volume or pressure in the left ventricle at the end of diastole (i. e. the resting phase of the heart). Factors affecting preload include: vaortic insufficiency vcirculating blood volume vmitral valve disease vsome medications (i. e. vasoconstrictors, vasodilators)
PATHO-PHYSIOLOGY Afterload is the resistance that the heart must overcome in order to eject the blood volume from the left ventricle. Afterload can be affected by: vaortic valvular stenosis varterial vasoconstrictors and vasodilators vhypertension vperipheral arterial constriction
Myocardial Oxygen Consumption Has a linear relationship to: Systolic wall stress Intra-ventricular pressure Afterload End diastolic volume Wall thickness
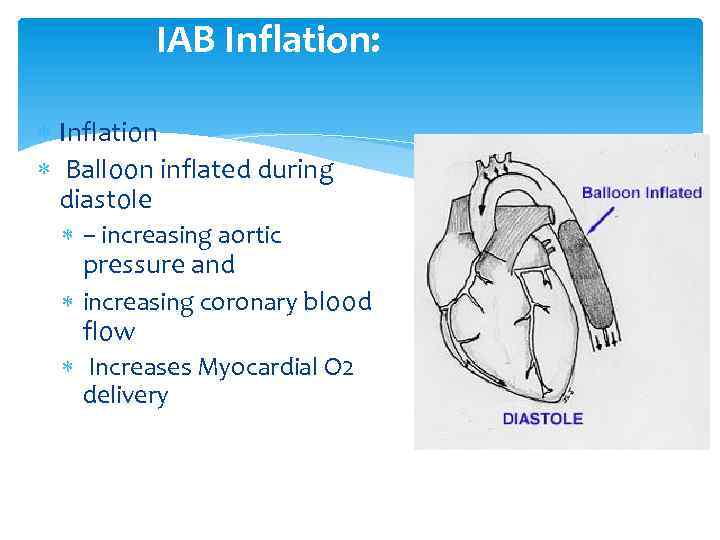
IAB Inflation: Inflation Balloon inflated during diastole – increasing aortic pressure and increasing coronary blood flow Increases Myocardial O 2 delivery
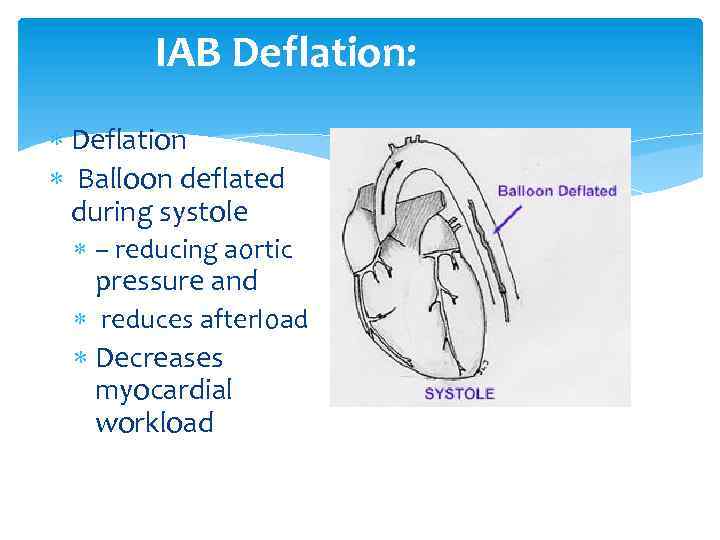
IAB Deflation: Deflation Balloon deflated during systole – reducing aortic pressure and reduces afterload Decreases myocardial workload
HEMODYNAMICS : Summary Preload (slight decrease) Afterload (decreases) Coronary flow (increases) Myocardial oxygen (decreases) Cardiac output (increases)
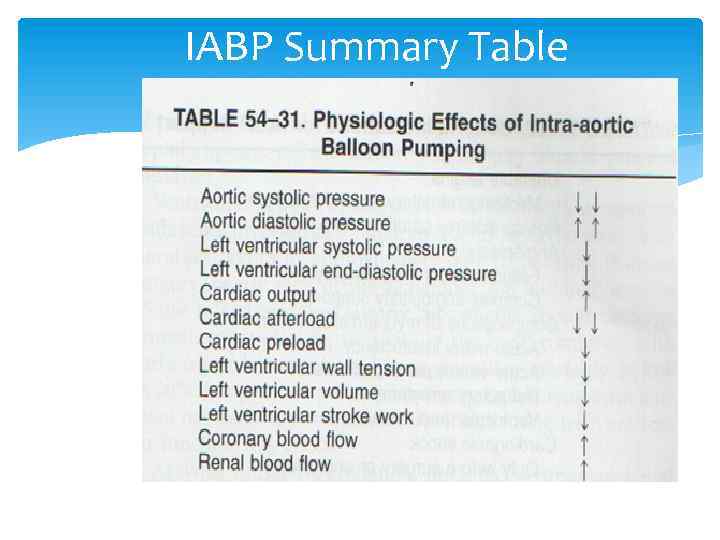
IABP Summary Table
INDICATIONS for IABP Cardiac failure after a cardiac surgical procedure Refractory angina despite maximal medical management Peri-operative treatment of complications due to myocardial infarction Failed PTCA As a bridge to cardiac transplantation High risk CABG
IABP During or After Cardiac Surgery Patients who have sustained ventricular damage preoperatively and experience harmful additional ischemia during surgery Some patients begin with relatively normal cardiac function but experienced severe, but reversible, myocardial stunning during the operation
IABP As a Bridge to Cardiac Transplantation 15 to 30 % of endstage cardiomyopathy patients awaiting transplantation need mechanical support May decrease the need for more invasive LVAD support
CONTRAINDICATIONS to IABP Severe aortic insufficiency Aortic aneurysm Aortic dissection Severe aorto-iliac occlusive disease
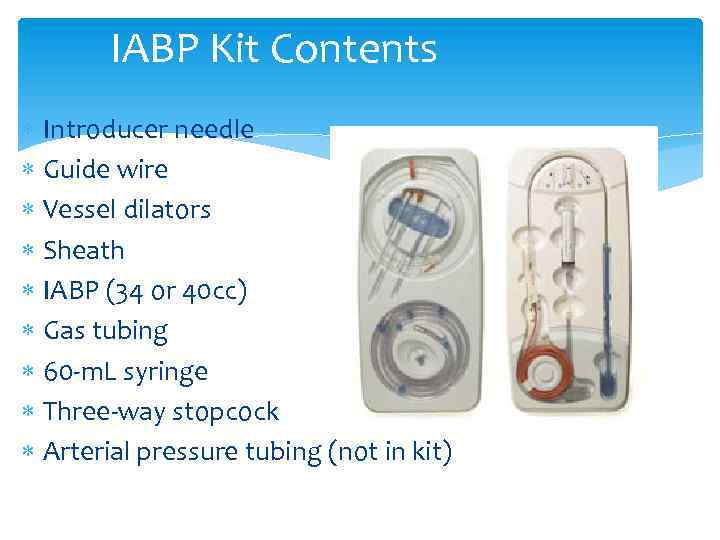
IABP Kit Contents Introducer needle Guide wire Vessel dilators Sheath IABP (34 or 40 cc) Gas tubing 60 -m. L syringe Three-way stopcock Arterial pressure tubing (not in kit)
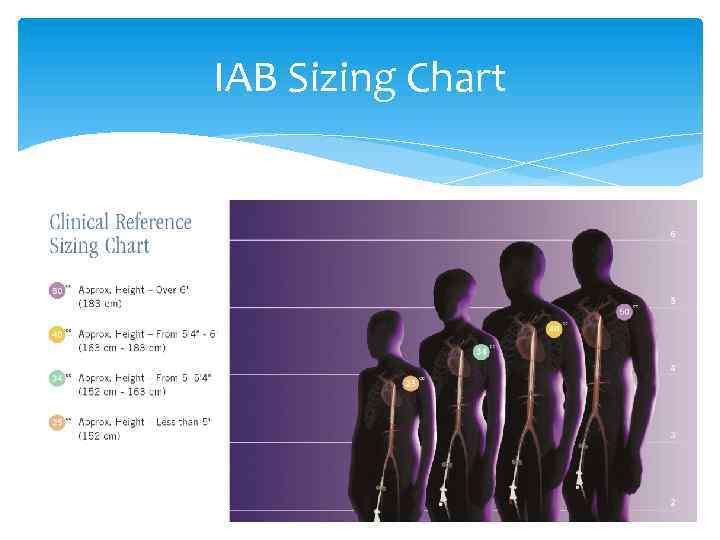
IAB Sizing Chart The IAB Should be selected according to the following chart (chart located on every box).
Why Helium? : Helium is used because its low density facilitates rapid transfer of gas from console to the balloon. It is also easily absorbed into the blood stream in case of rupture of the balloon
PRINCIPLES of IABP A flexibile catheter is inserted into the femoral artery and passed into the descending aorta. Correct positioning is critical in order to avoid blocking off the subclavian, carotid, or renal arteries. When inflated, the balloon blocks 85 -90% of the aorta. Complete occlusion would damage the walls of the aorta, red blood cells, and platelets.
INSERTION TECHNIQUE Percutaneous sheath less Surgical insertion Femoral cut down Trans-thoracic
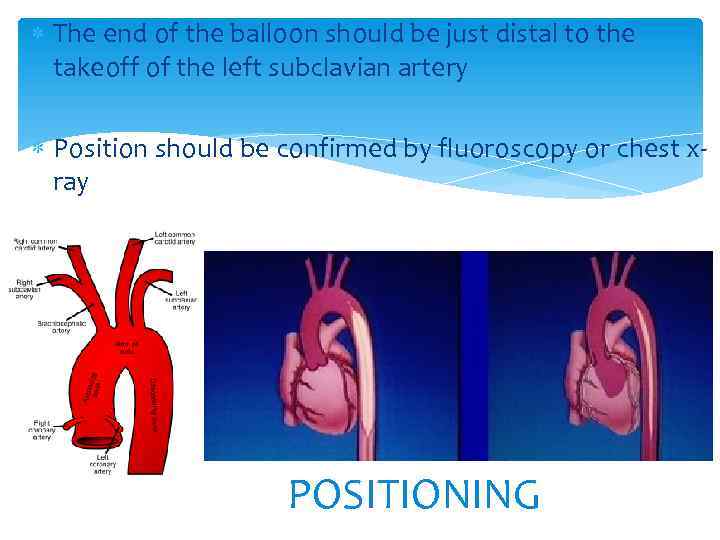
The end of the balloon should be just distal to the takeoff of the left subclavian artery Position should be confirmed by fluoroscopy or chest xray POSITIONING
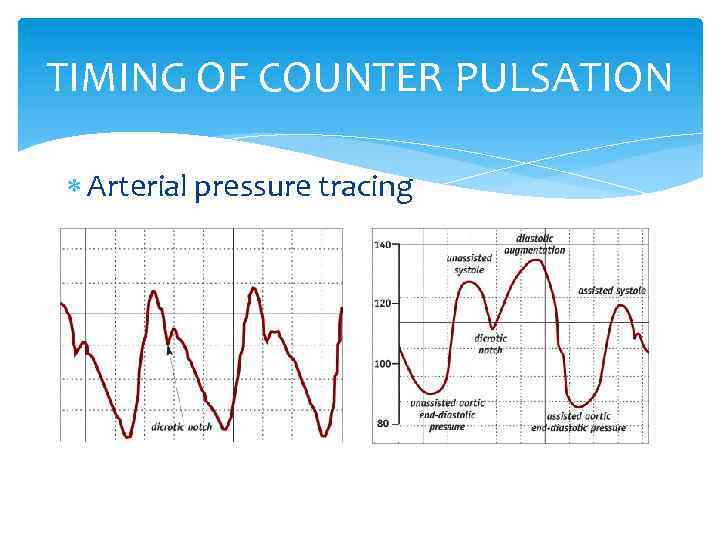
TIMING OF COUNTER PULSATION Arterial pressure tracing
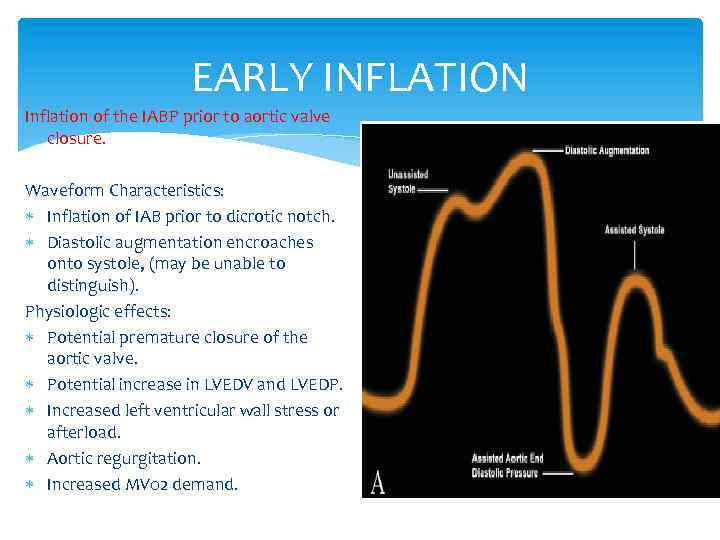
EARLY INFLATION Inflation of the IABP prior to aortic valve closure. Waveform Characteristics: Inflation of IAB prior to dicrotic notch. Diastolic augmentation encroaches onto systole, (may be unable to distinguish). Physiologic effects: Potential premature closure of the aortic valve. Potential increase in LVEDV and LVEDP. Increased left ventricular wall stress or afterload. Aortic regurgitation. Increased MV 02 demand.
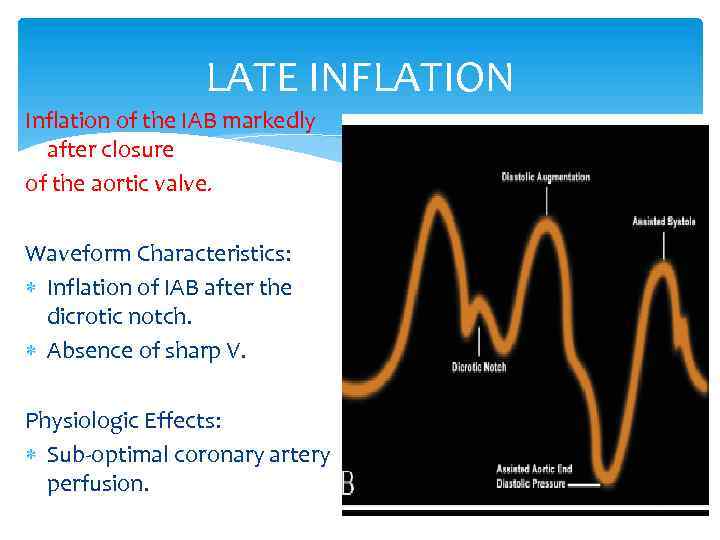
LATE INFLATION Inflation of the IAB markedly after closure of the aortic valve. Waveform Characteristics: Inflation of IAB after the dicrotic notch. Absence of sharp V. Physiologic Effects: Sub-optimal coronary artery perfusion.
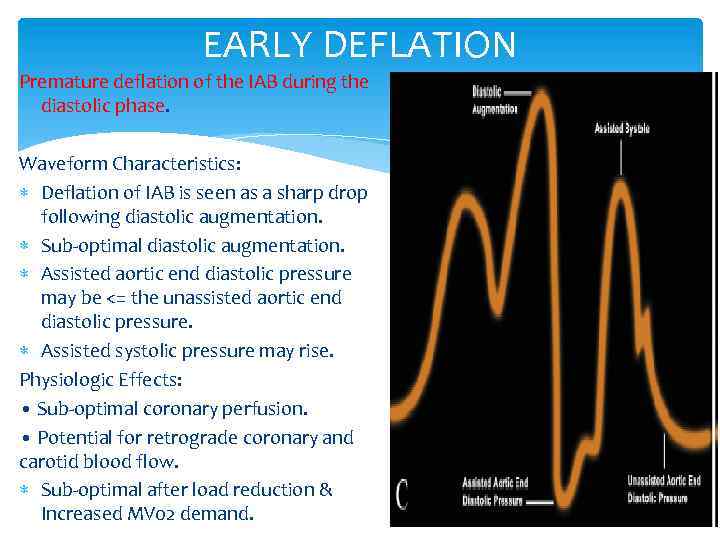
EARLY DEFLATION Premature deflation of the IAB during the diastolic phase. Waveform Characteristics: Deflation of IAB is seen as a sharp drop following diastolic augmentation. Sub-optimal diastolic augmentation. Assisted aortic end diastolic pressure may be <= the unassisted aortic end diastolic pressure. Assisted systolic pressure may rise. Physiologic Effects: • Sub-optimal coronary perfusion. • Potential for retrograde coronary and carotid blood flow. Sub-optimal after load reduction & Increased MV 02 demand.
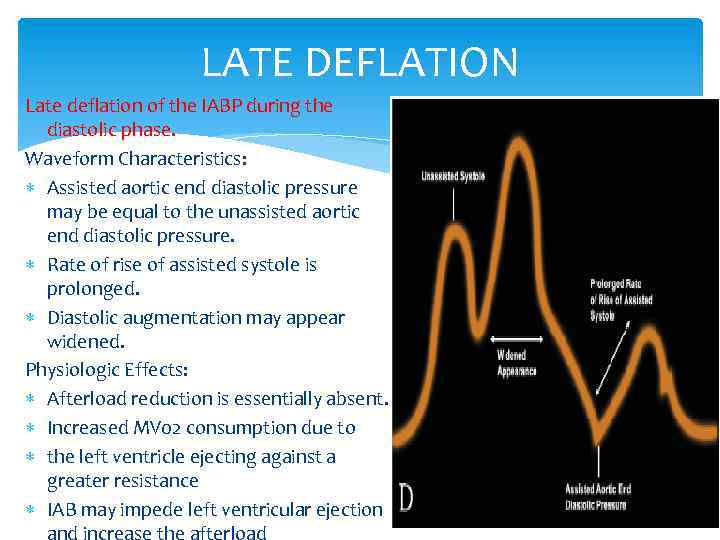
LATE DEFLATION Late deflation of the IABP during the diastolic phase. Waveform Characteristics: Assisted aortic end diastolic pressure may be equal to the unassisted aortic end diastolic pressure. Rate of rise of assisted systole is prolonged. Diastolic augmentation may appear widened. Physiologic Effects: Afterload reduction is essentially absent. Increased MV 02 consumption due to the left ventricle ejecting against a greater resistance IAB may impede left ventricular ejection and increase the afterload
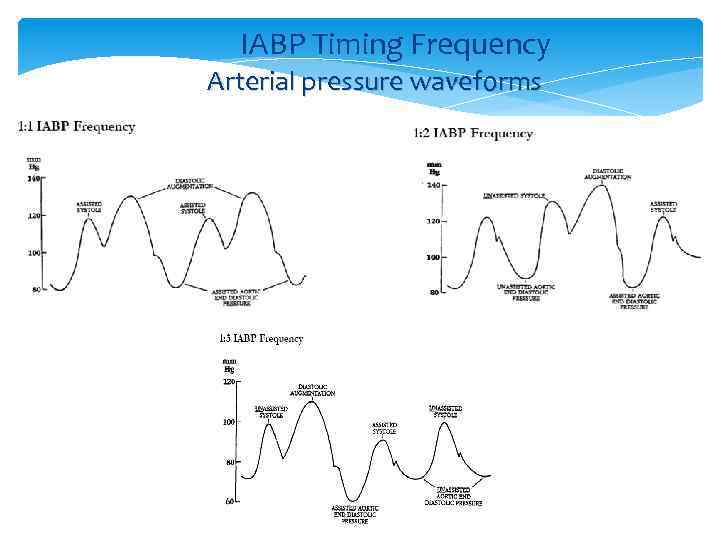
IABP Timing Frequency Arterial pressure waveforms
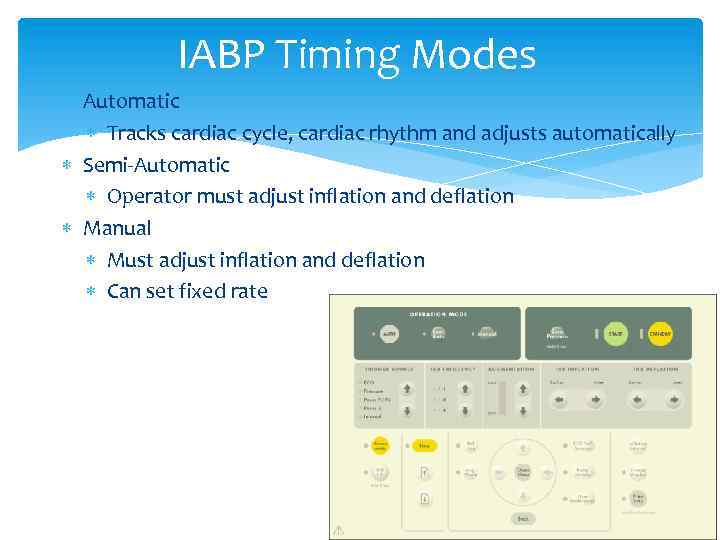
IABP Timing Modes Automatic Tracks cardiac cycle, cardiac rhythm and adjusts automatically Semi-Automatic Operator must adjust inflation and deflation Manual Must adjust inflation and deflation Can set fixed rate
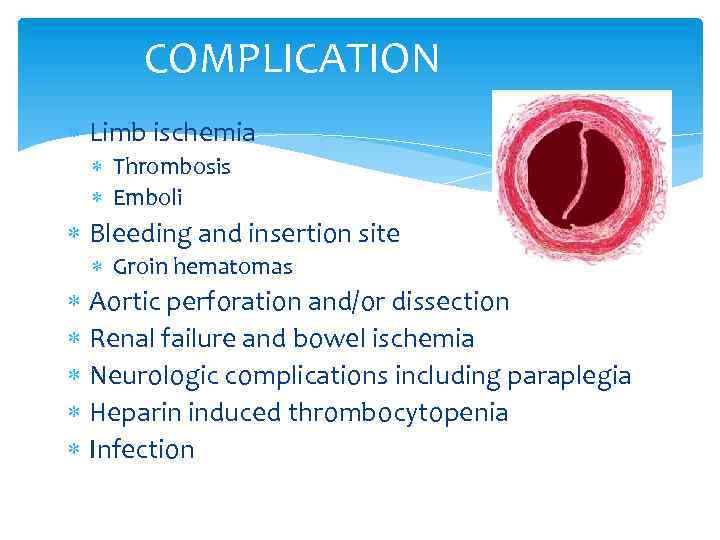
COMPLICATION Limb ischemia Thrombosis Emboli Bleeding and insertion site Groin hematomas Aortic perforation and/or dissection Renal failure and bowel ischemia Neurologic complications including paraplegia Heparin induced thrombocytopenia Infection
WEANING of IABP Timing of weaning Patient should be stable for 24 -48 hours Decreasing inotropic support Decreasing pump ratio From 1: 1 to 1: 2 or 1: 3 Decrease augmentation Monitor patient closely If patient becomes unstable, weaning should be immediately discontinued
THANK YOU